Commonly Used Types and Recent Development of Ankle-Foot Orthosis: A Narrative Review
Abstract
:1. Introduction
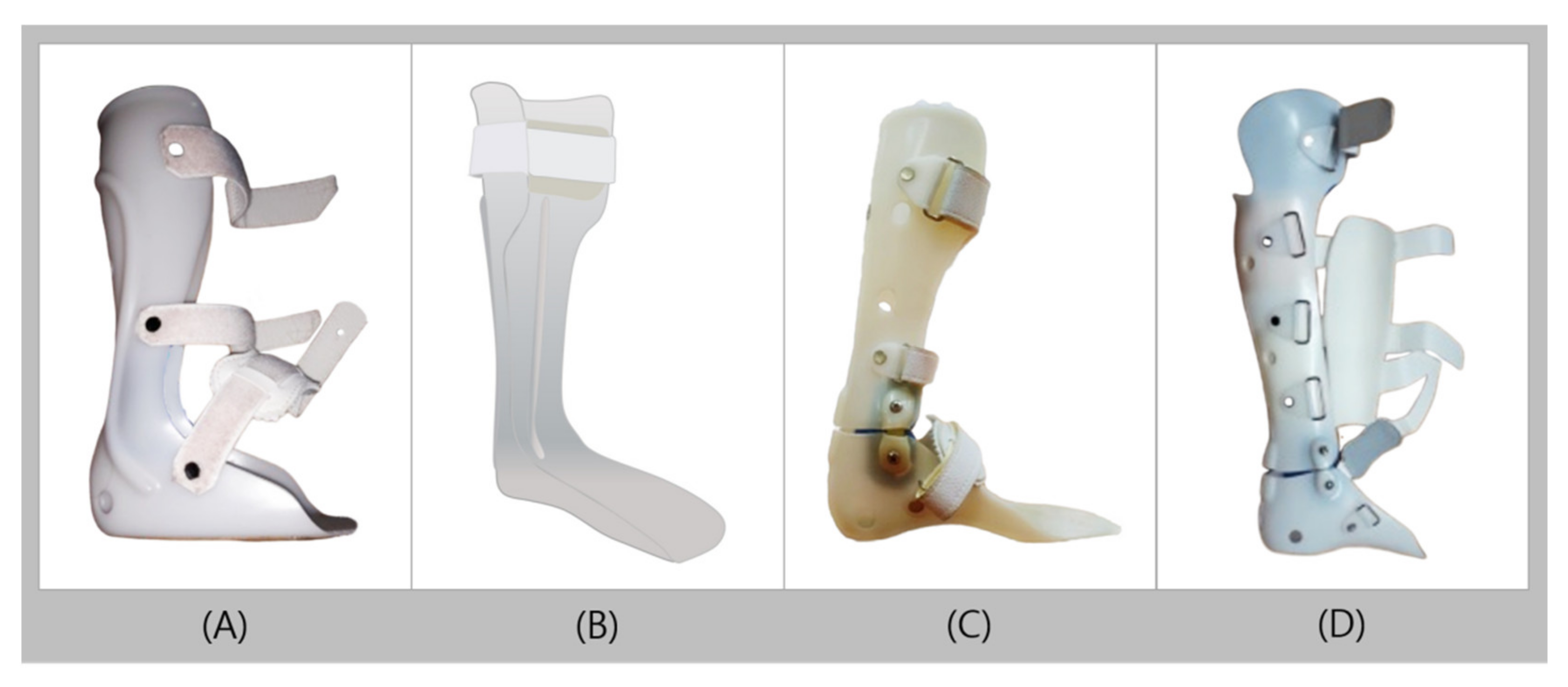
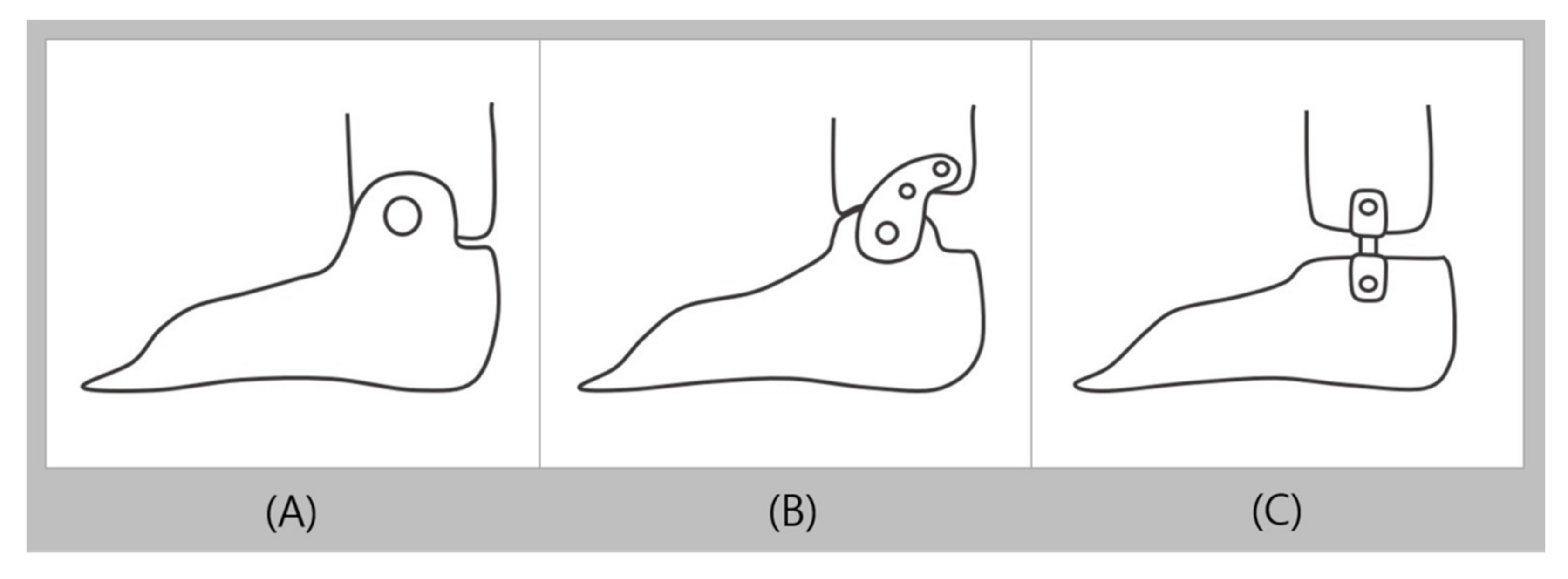
2. Conventional AFO Used in Clinical Practice
2.1. Typical Plastic AFO
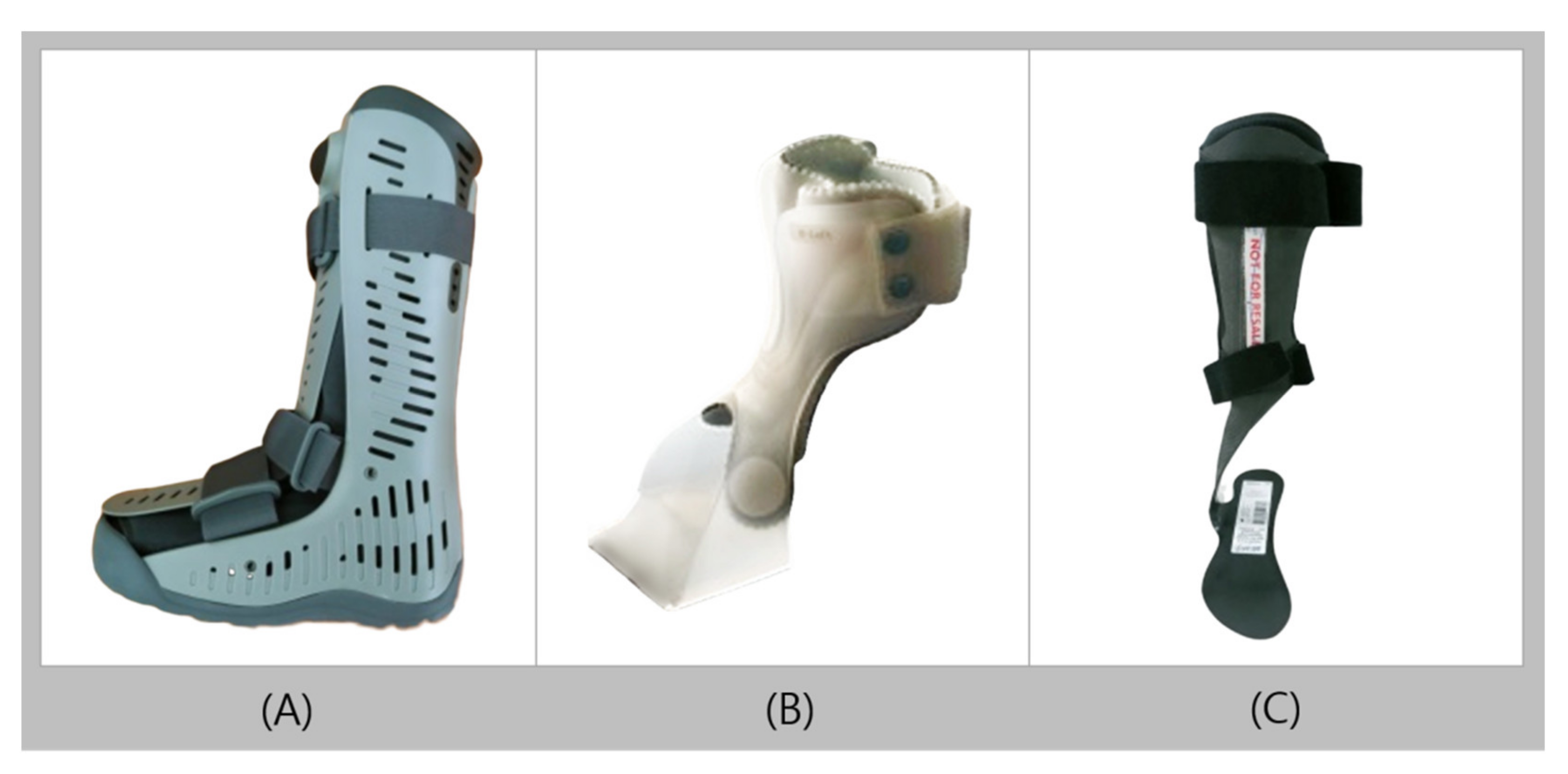
2.2. Walking Boot (Controlled Ankle Movement Walker, Aircast)
2.3. UD-Flex
2.4. Carbon Fiber AFO
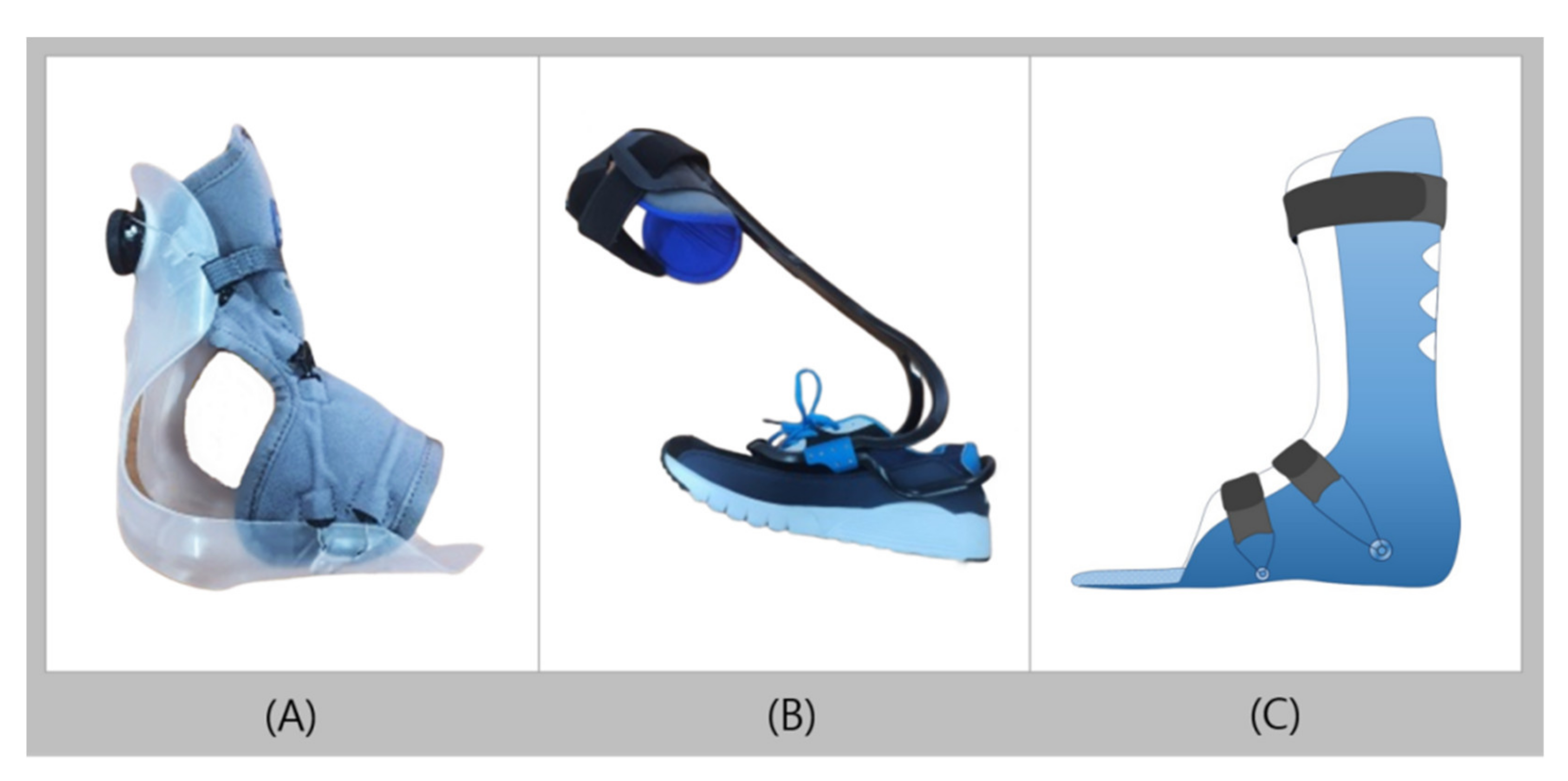
3. Recent Trends of AFO
3.1. AF Servo
3.2. TurboMed
3.3. D Printed AFO
3.4. Kenaf Composites
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Balaban, B.; Yasar, E.; Dal, U.; Yazicioglu, K.; Mohur, H.; Kalyon, T.A. The effect of hinged ankle-foot orthosis on gait and energy expenditure in spastic hemiplegic cerebral palsy. Disabil. Rehabil. 2007, 29, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Bregman, D.J.; De Groot, V.; Van Diggele, P.; Meulman, H.; Houdijk, H.; Harlaar, J. Polypropylene ankle foot orthoses to overcome drop-foot gait in central neurological patients: A mechanical and functional evaluation. Prosthet. Orthot. Int. 2010, 34, 293–304. [Google Scholar] [CrossRef]
- Kim, C.M.; Eng, J.J.; Whittaker, M.W. Effects of a simple functional electric system and/or a hinged ankle-foot orthosis on walking in persons with incomplete spinal cord injury. Arch. Phys. Med. Rehabil. 2004, 85, 1718–1723. [Google Scholar] [CrossRef]
- Pourhosseingholi, E.; Farahmand, B.; Bagheri, A.; Kamali, M.; Saeb, M. Efficacy of different techniques of AFO construction for hemiplegia patients: A systematic review. Med. J. Islam. Repub. Iran 2019, 33, 50. [Google Scholar] [CrossRef] [PubMed]
- Simkin, A.; Leichter, I.; Giladi, M.; Stein, M.; Milgrom, C. Combined effect of foot arch structure and an orthotic device on stress fractures. Foot Ankle 1989, 10, 25–29. [Google Scholar] [CrossRef]
- Woodburn, J.; Barker, S.; Helliwell, P.S. A randomized controlled trial of foot orthoses in rheumatoid arthritis. J. Rheumatol. 2002, 29, 1377–1383. [Google Scholar]
- Fatone, S.; Gard, S.A.; Malas, B.S. Effect of ankle-foot orthosis alignment and foot-plate length on the gait of adults with poststroke hemiplegia. Arch. Phys. Med. Rehabil. 2009, 90, 810–818. [Google Scholar] [CrossRef] [PubMed]
- Ploeger, H.E.; Bus, S.A.; Brehm, M.A.; Nollet, F. Ankle-foot orthoses that restrict dorsiflexion improve walking in polio survivors with calf muscle weakness. Gait Posture 2014, 40, 391–398. [Google Scholar] [CrossRef]
- Alam, M.; Choudhury, I.A.; Bin Mamat, A. Mechanism and design analysis of articulated ankle foot orthoses for drop-foot. Sci. World J. 2014, 2014, 867869. [Google Scholar] [CrossRef] [Green Version]
- Danielsson, A.; Sunnerhagen, K.S. Energy expenditure in stroke subjects walking with a carbon composite ankle foot orthosis. J. Rehabil. Med. 2004, 36, 165–168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, M.; Chun, M. The effects of a short ankle-foot orthosis on gait in patients with post-stroke hemiplegia. Neurol. Asia 2019, 24, 103–107. [Google Scholar]
- Kwon, J.; Park, J.; Ku, S.; Jeong, Y.; Paik, N.; Park, Y. A Soft Wearable Robotic Ankle-Foot-Orthosis for Post-Stroke Patients. IEEE Robot. Autom. Lett. 2019, 4, 2547–2552. [Google Scholar] [CrossRef]
- Adiputra, D.; Nazmi, N.; Bahiuddin, I.; Ubaidillah, U.; Imaduddin, F.; Abdul Rahman, M.A.; Mazlan, S.A.; Zamzuri, H. A Review on the Control of the Mechanical Properties of Ankle Foot Orthosis for Gait Assistance. Actuators 2019, 8, 10. [Google Scholar] [CrossRef] [Green Version]
- Agrawal, A.; Sangwan, V.; Banala, S.K.; Agrawal, S.K.; Binder-Macleod, S.A. Design of a Novel Two Degree-of-Freedom Ankle-Foot Orthosis. J. Mech. Design 2006, 129, 1137–1143. [Google Scholar] [CrossRef]
- Arvin, M.; Kamyab, M.; Moradi, V.; Hajiaghaei, B.; Maroufi, N. Influence of modified solid ankle-foot orthosis to be used with and without shoe on dynamic balance and gait characteristic in asymptomatic people. Prosthet. Orthot. Int. 2013, 37, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, J.F.; Esselman, P.C.; Ko, M.J.; Smith, J.C.; Dralle, A.J. Plastic ankle-foot orthoses: Evaluation of function. Arch. Phys. Med. Rehabil. 1983, 64, 402–407. [Google Scholar] [PubMed]
- Sobel, E.; Levitz, S.J.; Caselli, M.A. Orthoses in the treatment of rearfoot problems. J. Am. Podiatr. Med. Assoc. 1999, 89, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Cikajlo, I.; Osrečki, K.; Burger, H. The effects of different types of ankle-foot orthoses on postural responses in individuals with walking impairments. Int. J. Rehabil. Res. 2016, 39, 313–319. [Google Scholar] [CrossRef]
- Degelean, M.; De Borre, L.; Salvia, P.; Pelc, K.; Kerckhofs, E.; De Meirleir, L.; Cheron, G.; Dan, B. Effect of ankle-foot orthoses on trunk sway and lower limb intersegmental coordination in children with bilateral cerebral palsy. J. Pediatr. Rehabil. Med. 2012, 5, 171–179. [Google Scholar] [CrossRef]
- Stott, N.S. Chapter 8—Cerebral Palsy. In Management of Chronic Conditions in the Foot and Lower Leg; Rome, K., McNair, P., Eds.; Churchill Livingstone: Edinburgh, UK, 2015; pp. 214–250. [Google Scholar]
- Sabolich, J. Modification of The Posterior Leaf-Spring Orthosis. Orthot. Prosthet. 1976, 30, 35–36. [Google Scholar]
- Dalvand, H.; Dehghan, L.; Feizi, A.; Hosseini, S.A.; Amirsalari, S. The impacts of hinged and solid ankle-foot orthoses on standing and walking in children with spastic diplegia. Iran J. Child Neurol. 2013, 7, 12–19. [Google Scholar]
- Rha, D.W.; Kim, D.J.; Park, E.S. Effect of hinged ankle-foot orthoses on standing balance control in children with bilateral spastic cerebral palsy. Yonsei Med. J. 2010, 51, 746–752. [Google Scholar] [CrossRef] [Green Version]
- Son, I.; Lee, D.; Hong, S.; Lee, K.; Lee, G. Comparison of Gait Ability of a Child with Cerebral Palsy According to the Difference of Dorsiflexion Angle of Hinged Ankle-Foot Orthosis: A Case Report. Am. J. Case Rep. 2019, 20, 1454–1459. [Google Scholar] [CrossRef] [PubMed]
- Alimerzaloo, F.; Kashani, R.V.; Saeedi, H.; Farzi, M.; Fallahian, N. Patellar tendon bearing brace: Combined effect of heel clearance and ankle status on foot plantar pressure. Prosthet. Orthot. Int. 2014, 38, 34–38. [Google Scholar] [CrossRef]
- Trepman, E.; Donnelly, P. Patellar tendon-bearing, patten-bottom caliper suspension orthosis in active Charcot arthropathy: Crutch-free ambulation with no weight bearing in the foot. Foot Ankle Int. 2002, 23, 335–339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abe, H.; Michimata, A.; Sugawara, K.; Sugaya, N.; Izumi, S. Improving gait stability in stroke hemiplegic patients with a plastic ankle-foot orthosis. Tohoku J. Exp. Med. 2009, 218, 193–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, K.D. Ankle Mechanism of Ankle Foot Orthoses. J. Korean Soc. Prosthet. Orthot. 2007, 1, 30–37. [Google Scholar]
- Agochukwu, N.B.; Solomon, B.D.; Benson, L.J.; Muenke, M. Talocalcaneal coalition in Muenke syndrome: Report of a patient, review of the literature in FGFR-related craniosynostoses, and consideration of mechanism. Am. J. Med. Genet. A 2013, 161, 453–460. [Google Scholar] [CrossRef] [Green Version]
- Akizuki, K.H.; Gartman, E.J.; Nisonson, B.; Ben-Avi, S.; McHugh, M.P. The relative stress on the Achilles tendon during ambulation in an ankle immobiliser: Implications for rehabilitation after Achilles tendon repair. Br. J. Sports Med. 2001, 35, 329–333, discussion 333–324. [Google Scholar] [CrossRef] [Green Version]
- Ready, L.V.; Fisk, E.G.; Ciurylo, W.; Chiodo, C.P.; Bluman, E.M.; Smith, J.T. Associated Joint Pain With Controlled Ankle Movement Walker Boot Wear. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2018, 2, e044. [Google Scholar] [CrossRef]
- Blanchette, M.A.; Grenier, J.M. Fracture of the lateral tubercle of the posterior talar process caused by a rock-climbing fall: A case report. J. Can. Chiropr. Assoc. 2014, 58, 286–290. [Google Scholar]
- Laporta, G.; Bock, F.; Ghate, N. Posterior approach for subtalar joint distraction arthrodesis by compact external fixation: A technique guide. J. Foot Ankle Surg. 2013, 52, 547–552. [Google Scholar] [CrossRef] [PubMed]
- Ritz, G.; Rowland, W.D.; Rowland, J.W. Use of the Cam Walker in treating diabetic ulcers. A case report. J. Am. Podiatr. Med. Assoc. 1996, 86, 253–256. [Google Scholar] [CrossRef]
- Schiffman, E.D.; McCarthy, J.C.; Kwon, J.Y. Ankle fracture following hip arthroscopy. Orthopedics 2012, 35, e1290–e1292. [Google Scholar] [CrossRef] [Green Version]
- Amaha, K.; Arimoto, T.; Saito, M.; Tasaki, A.; Tsuji, S. Shorter recovery can be achieved from using walking boot after operative treatment of an ankle fracture. Asia Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 2017, 7, 10–14. [Google Scholar] [CrossRef] [Green Version]
- Bae, D.Y.; Shin, J.H.; Kim, J.S. Effects of dorsiflexor functional electrical stimulation compared to an ankle/foot orthosis on stroke-related genu recurvatum gait. J. Phys. Ther. Sci. 2019, 31, 865–868. [Google Scholar] [CrossRef]
- Alimusaj, M.; Knie, I.; Wolf, S.; Fuchs, A.; Braatz, F.; Döderlein, L. Functional impact of carbon fiber springs in ankle-foot orthoses. Orthopade 2007, 36, 752–756. [Google Scholar] [CrossRef] [PubMed]
- Hachisuka, K.; Makino, K.; Wada, F.; Saeki, S.; Yoshimoto, N.; Arai, M. Clinical application of carbon fibre reinforced plastic leg orthosis for polio survivors and its advantages and disadvantages. Prosthet. Orthot. Int. 2006, 30, 129–135. [Google Scholar] [CrossRef] [Green Version]
- Mnatsakanian, A.; Kissel, J.T.; Terry, P.; King, W.M. One clinic’s experience with carbon fiber orthoses in neuromuscular disease. Muscle Nerve 2017, 55, 202–205. [Google Scholar] [CrossRef] [PubMed]
- Shearin, S.M.; Bauzaite, E.; Hall, H.; McCain, K.J. Application of Carbon Fiber Ankle Foot Orthoses to Enhance Gait Outcomes for Individuals with Neurologic Gait Dysfunction. Phys. Med. Rehabil. Int. 2017, 4, 1123. [Google Scholar]
- Steinfeldt, F.; Seifert, W.; Günther, K.P. Modern carbon fibre orthoses in the management of polio patients--a critical evaluation of the functional aspects. Z. Orthop. Ihre Grenzgeb. 2003, 141, 357–361. [Google Scholar] [CrossRef] [PubMed]
- Wolf, S.I.; Alimusaj, M.; Rettig, O.; Döderlein, L. Dynamic assist by carbon fiber spring AFOs for patients with myelomeningocele. Gait Posture 2008, 28, 175–177. [Google Scholar] [CrossRef]
- Dufek, J.S.; Neumann, E.S.; Hawkins, M.C.; O’Toole, B. Functional and dynamic response characteristics of a custom composite ankle foot orthosis for Charcot-Marie-Tooth patients. Gait Posture 2014, 39, 308–313. [Google Scholar] [CrossRef]
- Malas, B.S. What variables influence the ability of an AFO to improve function and when are they indicated? Clin. Orthop. Relat. Res. 2011, 469, 1308–1314. [Google Scholar] [CrossRef] [Green Version]
- Desloovere, K.; Molenaers, G.; Van Gestel, L.; Huenaerts, C.; Van Campenhout, A.; Callewaert, B.; Van de Walle, P.; Seyler, J. How can push-off be preserved during use of an ankle foot orthosis in children with hemiplegia? A prospective controlled study. Gait Posture 2006, 24, 142–151. [Google Scholar] [CrossRef]
- Moriello, G.; Frear, M.; Seaburg, K. The recovery of running ability in an adolescent male after traumatic brain injury: A case study. J. Neurol. Phys. Ther. 2009, 33, 111–120. [Google Scholar] [CrossRef]
- Introduction of AFSERVO. Available online: https://www.afservo.com/ (accessed on 15 June 2021).
- Introduction of TurboMed. Available online: https://turbomed.co.uk/ (accessed on 15 June 2021).
- Products introduction of TurboMed. Available online: https://turbomedorthotics.com/ (accessed on 15 June 2021).
- Bair, M.O. The Design and Testing of a Powered Exoskeleton to Reduce the Metabolic Cost of Walking in Individuals with Cerebral Palsy. Masters’s Thesis, Northern Arizona University, San Francisco, CA, USA, 2018. [Google Scholar]
- Ladlow, P.; Bennett, N.; Phillip, R.; Dharm-Datta, S.; McMenemy, L.; Bennett, A.N. Passive-dynamic ankle-foot orthosis improves medium-term clinical outcomes after severe lower extremity trauma. J. R. Army Med. Corps 2019, 165, 330–337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wojciechowski, E.; Chang, A.Y.; Balassone, D.; Ford, J.; Cheng, T.L.; Little, D.; Menezes, M.P.; Hogan, S.; Burns, J. Feasibility of designing, manufacturing and delivering 3D printed ankle-foot orthoses: A systematic review. J. Foot Ankle Res. 2019, 12, 11. [Google Scholar] [CrossRef] [PubMed]
- Buonamici, F.; Carfagni, M.; Furferi, R.; Lazzeri, S.; Servi, M.; Talanti, E.; Volpe, Y. Automatic CAD Modeling of Ventilation Holes for 3D Printed Wrist Orthoses. Comput. Aided Des. Appl. 2019, 17, 325–336. [Google Scholar] [CrossRef]
- Li, J.; Tanaka, H. Feasibility study applying a parametric model as the design generator for 3D-printed orthosis for fracture immobilization. 3D Print Med. 2018, 4, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cha, Y.H.; Lee, K.H.; Ryu, H.J.; Joo, I.W.; Seo, A.; Kim, D.H.; Kim, S.J. Ankle-Foot Orthosis Made by 3D Printing Technique and Automated Design Software. Appl. Bionics Biomech. 2017, 2017, 9610468. [Google Scholar] [CrossRef] [Green Version]
- Chen, R.K.; Jin, Y.-A.; Wensman, J.; Shih, A. Additive manufacturing of custom orthoses and prostheses—A review. Addit. Manuf. 2016, 12, 77–89. [Google Scholar] [CrossRef] [Green Version]
- Xu, R.; Wang, Z.; Ma, T.; Ren, Z.; Jin, H. Effect of 3D Printing Individualized Ankle-Foot Orthosis on Plantar Biomechanics and Pain in Patients with Plantar Fasciitis: A Randomized Controlled Trial. Med. Sci. Monit. 2019, 25, 1392–1400. [Google Scholar] [CrossRef] [PubMed]
- Shahar, F.S.; Hameed Sultan, M.T.; Lee, S.H.; Jawaid, M.; Md Shah, A.U.; Safri, S.N.A.; Sivasankaran, P.N. A review on the orthotics and prosthetics and the potential of kenaf composites as alternative materials for ankle-foot orthosis. J. Mech. Behav. Biomed. Mater. 2019, 99, 169–185. [Google Scholar] [CrossRef]
- Razak, N.I.; Ibrahim, N.A.; Zainuddin, N.; Rayung, M.; Saad, W.Z. The influence of chemical surface modification of kenaf fiber using hydrogen peroxide on the mechanical properties of biodegradable kenaf fiber/poly(lactic acid) composites. Molecules 2014, 19, 2957–2968. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mohd Radzuan, N.A.; Ismail, N.F.; Fadzly Md Radzi, M.K.; Razak, Z.B.; Tharizi, I.B.; Sulong, A.B.; Che Haron, C.H.; Muhamad, N. Kenaf Composites for Automotive Components: Enhancement in Machinability and Moldability. Polymers 2019, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choo, Y.J.; Chang, M.C. Commonly Used Types and Recent Development of Ankle-Foot Orthosis: A Narrative Review. Healthcare 2021, 9, 1046. https://doi.org/10.3390/healthcare9081046
Choo YJ, Chang MC. Commonly Used Types and Recent Development of Ankle-Foot Orthosis: A Narrative Review. Healthcare. 2021; 9(8):1046. https://doi.org/10.3390/healthcare9081046
Chicago/Turabian StyleChoo, Yoo Jin, and Min Cheol Chang. 2021. "Commonly Used Types and Recent Development of Ankle-Foot Orthosis: A Narrative Review" Healthcare 9, no. 8: 1046. https://doi.org/10.3390/healthcare9081046
APA StyleChoo, Y. J., & Chang, M. C. (2021). Commonly Used Types and Recent Development of Ankle-Foot Orthosis: A Narrative Review. Healthcare, 9(8), 1046. https://doi.org/10.3390/healthcare9081046






