Current Perspectives on Rehabilitation Following Return of Spontaneous Circulation After Sudden Cardiac Arrest: A Narrative Review
Abstract
1. Introduction
Objectives of the Review
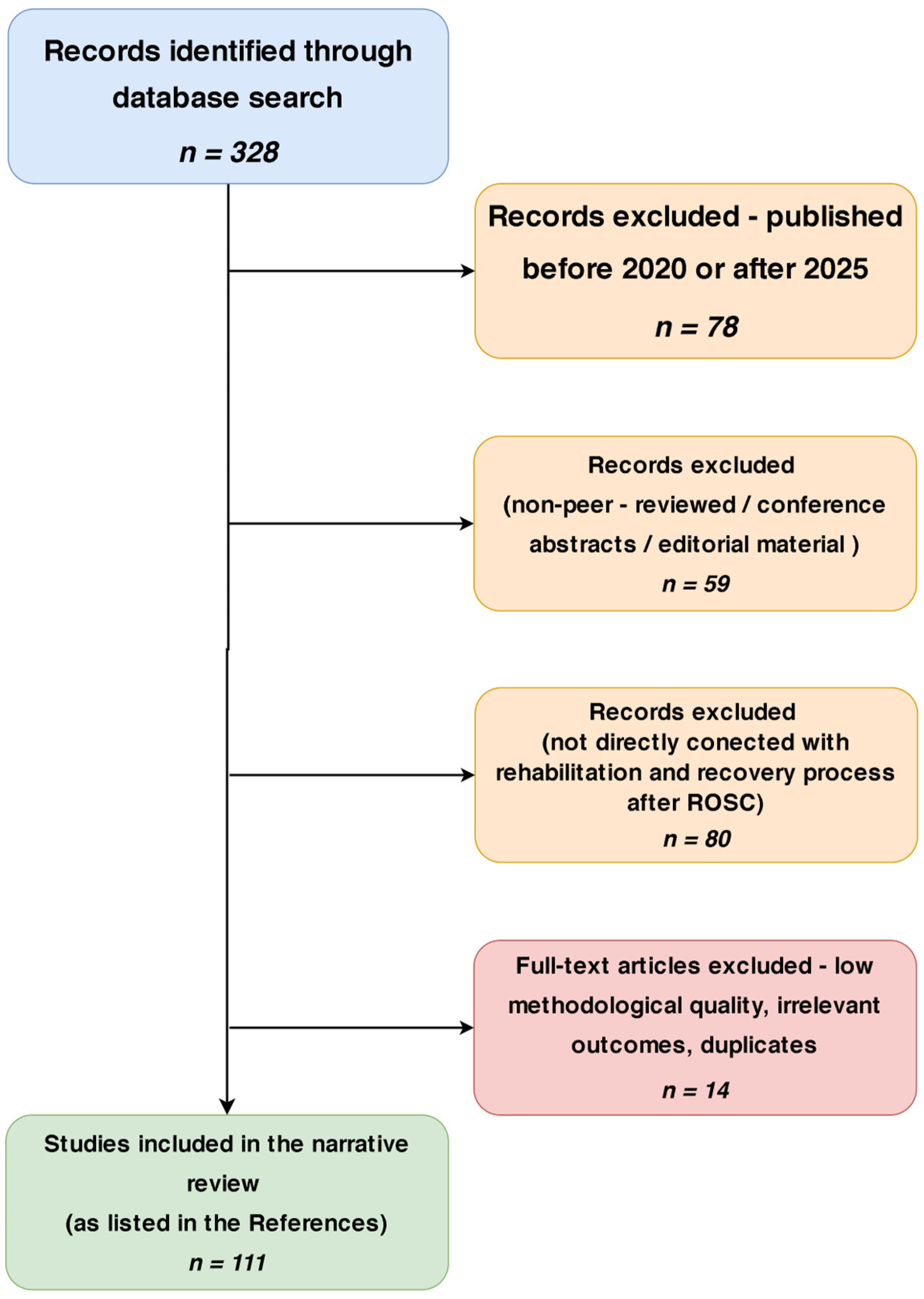
2. Materials and Methods
3. Results
3.1. Epidemiology
3.2. The Fourth Link in the Survival Chain
3.3. Post Cardiac Arrest Syndrome-PCAS
3.4. Early Neurological Assessment Significance
3.5. Metabolic Profiling and Secondary Risk in Cardiac Arrest Survivors
3.6. Physiotherapy and Early Rehabilitation Interventions in ROSC
3.6.1. Acute Phase (0–72 h)
3.6.2. Early Phase (3–7 Days)
3.6.3. Functional Phase
3.6.4. Long-Term Rehabilitation Phase
3.7. The Role of the Interdisciplinary Team
3.8. The Importance of Assessing Cognitive Function and Activities of Daily Living in Cardiac Arrest Survivors
3.9. Education and Support of the Patient’s Family After Return of Spontaneous Circulation (ROSC)
3.10. Clinical Barriers and Complications Affecting Early Rehabilitation After ROSC
3.10.1. Urgent Percutaneous Coronary Intervention (PCI)
3.10.2. Hemodynamic Instability and Vasoactive Support
3.10.3. Surgical Revascularization (CABG/OPCAB) and Postoperative Recovery
3.10.4. Mechanical Complications of Myocardial Infarction
3.10.5. Mechanical Circulatory Support (ECMO, IABP, IMPELLA)
3.11. Neurocognitive Therapy After Hypoxia Following ROSC
3.12. Limitations of Neurocognitive Assessment Tools in Post-ROSC Patients’ Recovery
3.13. Individualization of Physiotherapy Protocols After ROSC
3.14. The Role of Physiotherapy in the Prevention of Pulmonary and Orthopedic Complications After ROSC
3.15. Pulmonary Complications and Respiratory Physiotherapy
3.16. Orthopedic Complications and Mobilization Therapy
3.17. Model for Implementing an Interdisciplinary Rehabilitation Approach After ROSC Across Variations in Healthcare Systems
3.18. Timing of Cardiac Interventions in Neurologically Uncertain Post-ROSC Patients: Implications for Rehabilitation and Prognosis
3.19. Organ Donation Following ROSC: Management and Clinical Outcomes

3.20. Clinical Indications, Timing, and Reversal Strategies in Targeted Temperature Management (TTM)
4. Discussion
4.1. Contrasting Perspectives on Targeted Temperature Management (TTM) Post-ROSC
4.2. Interdisciplinary Integration and Monitoring
4.3. Inequalities in Access to Post-Cardiac Arrest Rehabilitation Across Europe
4.4. Variability in the Implementation of Integrated Care Pathways After Cardiac Arrest
4.5. The Need for Randomized Controlled Trials Evaluating Rehabilitation Protocols After ROSC
- optimal timing of initiation, such as comparing outcomes of rehabilitation started within 24 h post-ROSC versus after ICU discharge
- determination of ideal intensity and frequency for mobilization protocols to prevent deconditioning while avoiding physiological stress
- comparative effectiveness of home-based rehabilitation models versus structured inpatient programs in terms of adherence, function, and reintegration
- validation of neurocognitive therapy algorithms stratified by baseline cognitive profiles using tools like the Montreal Cognitive Assessment or EEG patterns
- assessment of virtual and digital cognitive–motor rehabilitation platforms in improving cognitive outcomes and access to therapy, particularly in patients with limited mobility or rural access barriers.
4.6. Developing Pathways for Return to Work and Social Reintegration After Cardiac Arrest
4.7. Innovations in Brain Function Assessment
4.8. Gaps of Knowledge
4.9. Limitations of Study
4.10. Future Research
5. Conclusions
- Return of spontaneous circulation following sudden cardiac arrest initiates a prolonged and multifaceted recovery that demands continuous interdisciplinary involvement. While advances in resuscitation have improved survival rates, attention must now prioritize post-discharge outcomes. Rehabilitation plays a critical role in shaping neurological prognosis, functional autonomy, and reintegration into society.
- Evidence across all stages of recovery—from ICU to community-based follow-up—consistently supports individualized, structured, and multidisciplinary rehabilitation as foundational. Through targeted interventions, rehabilitation enables restoration of motor skills, cognitive function, emotional regulation, and daily participation.
- Optimal recovery requires coordinated efforts among cardiologists, neurologists, physiotherapists, occupational therapists, and neuropsychologists, integrated within a unified care framework. Family involvement is equally vital; informed and supported caregivers are central to ensuring adherence and long-term continuity of care.
- Significant disparities in rehabilitation access persist. Variability in service provision and the absence of standardized pathways undermine recovery potential. These inequities necessitate systemic reforms, including the implementation of care-integrated protocols and equitable investment in rehabilitation resources.
- Recovery after cardiac arrest should be redefined as an active process of reestablishing physical, cognitive, vocational, and social identity. Rehabilitation must be viewed not as ancillary, but as an indispensable extension of resuscitation. A coordinated, patient-centered approach is essential to translating survival into a meaningful return to life.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AED | automated external defibrillator |
| AHA | American Heart Association |
| ALS | advanced life support |
| AMI | acute myocardial infarction |
| BLS | basic life support |
| CAD | coronary artery disease |
| CBT | cognitive–behavioral therapy |
| COACT | coronary angiography after cardiac arrest |
| COMACARE | corticosteroid or macrolide therapy in critically Ill patients with community-acquired pneumonia |
| CoSTR | Consensus on Science and Treatment Recommendations |
| CPR | cardiopulmonary resuscitation |
| CT | computed tomography |
| EEG | electroencephalography |
| EQ-5D | EuroQol 5-Dimension |
| ERC | European Resuscitation Council |
| EU | European Union |
| FCT | functional cognitive therapy |
| GFAP | glial fibrillary acidic protein |
| ICU | intensive care unit |
| IHCA | in-hospital cardiac arrest |
| IL-6 | interleukin-6 |
| ILCOR | International Liaison Committee On Resuscitation |
| JAMA | Journal of the American Medical Association |
| NfL | neurofilament light chain |
| NNT | number needed to treat |
| OHCA | out-of-hospital cardiac arrest |
| PCAS | post-cardiac arrest syndrome |
| QALYs | quality-adjusted life years |
| ROCK | relevance of outcome consensus knowledge |
| ROSC | return of spontaneous circulation |
| SCA | sudden cardiac arrest |
| SCARF | SCAling recovery after cardiac arrest framework |
| TNF | tumor necrosis factor |
| TTM | targeted temperature management |
| UCH-L1 | ubiquitin carboxy-terminal hydrolase L1 |
| WHO | World Health Organization |
| WHODAS | World Health Organization Disability Assessment Schedule |
| WHODAS 2.0 | World Health Organization Disability Assessment Schedule, version 2.0 |
References
- Babu, A.S. Rehabilitation following return of spontaneous circulation (ROSC-Rehab): A new role for rehabilitation professionals in post-resuscitation care. Resuscitation 2021, 159, 38–39. [Google Scholar] [CrossRef] [PubMed]
- Nolan, J.P.; Sandroni, C.; Böttiger, B.W.; Cariou, A.; Cronberg, T.; Friberg, H.; Genbrugge, C.; Haywood, K.; Lilja, G.; Moulaert, V.R.M.M.; et al. European Resuscitation Council and European Society of Intensive Care Medicine guidelines 2021: Post-resuscitation care. Resuscitation 2021, 16, 220–269. [Google Scholar] [CrossRef] [PubMed]
- Gräsner, J.-T.; Herlitz, J.; Tjelmeland, I.B.; Wnent, J.; Masterson, S.; Lilja, G.; Bein, B.; Böttiger, B.W.; Rosell-Ortiz, F.; Nolan, J.P.; et al. European Resuscitation Council Guidelines 2021: Epidemiology of cardiac arrest in Europe. Resuscitation 2021, 161, 61–79. [Google Scholar] [CrossRef] [PubMed]
- Perkins, G.D.; Neumar, R.; Monsieurs, K.G.; Lim, S.H.; Castren, M.; Nolan, J.P.; Nadkarni, V.; Montgomery, B.; Steen, P.; Cummins, R.; et al. The International Liaison Committee on Resuscitation—Review of the last 25 years and vision for the future. Resuscitation 2017, 121, 104–116. [Google Scholar] [CrossRef] [PubMed]
- Böttiger, B.W.; Van Aken, H. Training children in cardiopulmonary resuscitation worldwide. Lancet 2015, 385, 2353. [Google Scholar] [CrossRef] [PubMed]
- Perkins, G.D.; Gräsner, J.-T.; Semeraro, F.; Olasveengen, T.; Soar, J.; Lott, C.; Van de Voorde, P.; Madar, J.; Zideman, D.; Mentzelopoulos, S.; et al. European Resuscitation Council Guidelines 2021: Executive summary. Resuscitation 2021, 161, 1–60. [Google Scholar] [CrossRef] [PubMed]
- Bednarz, K.; Goniewicz, K.; Al-Wathinani, A.M.; Goniewicz, M. Emergency Medicine Perspectives: The Importance of Bystanders and Their Impact on On-Site Resuscitation Measures and Immediate Outcomes of Out-of-Hospital Cardiac Arrest. J. Clin. Med. 2023, 12, 6815. [Google Scholar] [CrossRef] [PubMed]
- Ludhwani, D.; Goyal, A.; Jagtap, M. Ventricular Fibrillation. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK537120/ (accessed on 30 May 2025). [PubMed]
- Dejby, E.; Bhatt, D.L.; Skoglund, K.; Rawshani, A.; Omerovic, E.; Redfors, B.; Myredal, A.; Petursson, P.; Angerås, O.; Gustafsson, A. Left-sided valvular heart disease and survival in out-of-hospital cardiac arrest: A nationwide registry-based study. Sci Rep. 2023, 13, 12662. [Google Scholar] [CrossRef] [PubMed]
- Tran, D.T.; St Pierre Schneider, B.; McGinnis, G.R. Circadian Rhythms in Sudden Cardiac Arrest: A Review. Nurs. Res. 2021, 70, 298–309. [Google Scholar] [CrossRef] [PubMed]
- Chikatimalla, R.; Trivedi, Y.V.; Chigurupati, H.D.; Muhammed, A.N.; Sattar, Y.; Rana, J.S.; Neppala, S. From Prediction to Precision: The Impact of AI on the Future of Cardiopulmonary Resuscitation. preprints 2025. Available online: https://www.preprints.org/manuscript/202503.0207/v1 (accessed on 30 May 2025).
- Brady, W.J.; Singh, A. Cardiac Arrest. An Issue of Emergency Medicine Clinics of North America; Elsevier Health Sciences: Amsterdam, The Netherlands, 2023; Available online: https://books.google.com/books?id=jf7KEAAAQBAJ (accessed on 30 May 2025).
- Joshi, V.L.; Tang, L.H.; Kim, Y.J.; Wagner, M.K.; Nielsen, J.F.; Tjoernlund, M.; Zwisler, A.D. Promising results from a residential rehabilitation intervention focused on fatigue and the secondary psychological and physical consequences of cardiac arrest: The SCARF feasibility study. Resuscitation 2022, 173, 12–22. [Google Scholar] [CrossRef] [PubMed]
- Berg, K.M.; Cheng, A.; Panchal, A.R.; Topjian, A.A.; Aziz, K.; Bhanji, F.; Bigham, B.L.; Hirsch, K.G.; Hoover, A.V.; Kurz, M.C.; et al. Part 7: Systems of Care: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142 (16 Suppl. S2), S580–S604. [Google Scholar] [CrossRef] [PubMed]
- Dalessio, L. Post-Cardiac Arrest Syndrome. AACN Adv. Crit. Care 2020, 31, 383–393. [Google Scholar] [CrossRef] [PubMed]
- Taccone, F.S.; Picetti, E.; Vincent, J.-L. High quality targeted temperature management (TTM) after cardiac arrest. Crit. Care 2020, 24, 6. [Google Scholar] [CrossRef] [PubMed]
- Bakhsh, A.; Bakhashwain, W.; Alhazmi, M.; Bahwireth, S.; Binmahfooz, S.; Alghamdi, R.; Bakhribah, A.; Alsufyani, H. Fever Prevention and Neurological Recovery in In-Hospital Cardiac Arrest Survivors at a Limited-Resource Setting. Ther. Hypothermia Temp. Manag. 2025. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhang, H.; Wang, T.; Liu, G.; Teng, Y.; Wang, J.; Zhang, Q.; Yan, S.; Ji, B. What’s the optimal temperature control strategy in patients receiving ECPR after cardiac arrest? A network meta-analysis. Am. J. Emerg. Med. 2025, 87, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Feitosa-Filho, G.S.; Sena, J.P.; Guimarães, H.P.; Lopes, R.D. Hipotermia terapêutica pós-reanimação cardiorrespiratória: Evidências e aspectos práticos. Rev. Bras. Ter. Intensiv. 2009, 21, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Belur, A.D.; Sedhai, Y.R.; Truesdell, A.G.; Khanna, A.K.; Mishkin, J.D.; Belford, P.M.; Zhao, D.X.; Vallabhajosyula, S. Targeted Temperature Management in Cardiac Arrest: An Updated Narrative Review. Cardiol. Ther. 2023, 12, 65–84. [Google Scholar] [CrossRef] [PubMed]
- Hsu, T.-H.; Huang, W.C.; Lin, K.C.; Huang, C.L.; Tai, H.Y.; Tsai, Y.C.; Wu, M.C.; Chang, Y.T. Impact of a targeted temperature management quality improvement project on survival and neurologic outcomes in cardiac arrest patients. J. Chin. Med. Assoc. 2023, 86, 672–681. [Google Scholar] [CrossRef] [PubMed]
- Sandroni, C.; Natalini, D.; Nolan, J.P. Temperature control after cardiac arrest. Crit. Care 2022, 26, 361. [Google Scholar] [CrossRef] [PubMed]
- De Giorgio, D. Treatment with Inhaled Medical Gases to Improve Myocardial and Neurological Outcome after Cardiac Arrest. Ph.D. Dissertation, The Open University, Milton Keynes, UK, 2025. [Google Scholar] [CrossRef]
- Johnsen, H.M.; Hiorth, M.; Klaveness, J. Molecular hydrogen therapy—A review on clinical studies and outcomes. Molecules 2023, 28, 7785. [Google Scholar] [CrossRef] [PubMed]
- Chandiramani, A.; Ali, J.M. Frailty in cardiac surgery—Assessment tools, impact on outcomes, and optimisation strategies: A narrative review. J. Cardiovasc. Dev. Dis. 2025, 12, 127. [Google Scholar] [CrossRef] [PubMed]
- Yacine, A.; Zain Ali, M.; Alharbi, A.B.; Qubayl Alanaz, H.; Saud Alrahili, A.; Alkhdairi, A.A. Chronic Inflammation: A Multidisciplinary Analysis of Shared Pathways in Autoimmune, Infectious, and Degenerative Diseases. Cureus 2025, 17, e82579. [Google Scholar] [CrossRef] [PubMed]
- Sindewald, D.A. Behavioral Symptoms, Inflammation and Cortisol: Relationship to Cardiac Health and Quality of Life in Cardiac Rehabilitation Patients. Ph.D. Dissertation, Loyola University Chicago, Chicago, IL, USA, 2020. Available online: https://ecommons.luc.edu/luc_diss/3867 (accessed on 30 May 2025).
- Popazova, O.; Belenichev, I.; Bukhtiyarova, N.; Ryzhenko, V.; Gorchakova, N.; Oksenych, V.; Kamyshnyi, O. Molecular and Biochemical Mechanisms of Cardiomyopathy Development Following Prenatal Hypoxia-Focus on the NO System. Antioxidants 2025, 14, 743. [Google Scholar] [CrossRef] [PubMed]
- Christensen, J.; Winkel, B.G.; Kirkeskov, L.; Berg, S.K.; Gjedsted, J.; Soholm, H.; Melchiorsen, H.; Dreyer, P.; Rasmussen, L.S.; Moons, P.; et al. The ROCK trial—A multidisciplinary Rehabilitation intervention for sudden Out-of-hospital Cardiac arrest survivors focusing on return-to-work: A pragmatic randomized controlled trial protocol. Trials 2024, 25, 99. [Google Scholar] [CrossRef] [PubMed]
- Siegel, S.; Zhang, J.; Bandyopadhyay, S.; Nerella, S.; Silva, B.; Baslanti, T.; Bihorac, A.; Rashidi, P. Leveraging computer vision in the in-tensive care unit (ICU) for examining visitation and mobility. arXiv 2024, arXiv:2403.06322v2. [Google Scholar] [CrossRef]
- Davoudi, A.; Corbett, D.B.; Ozrazgat-Baslanti, T.; Bihorac, A.; Rashidi, P.; Mayaud, L.; Solomon, S.; Futoma, J.; Luke, A.; Potes, C.; et al. Activity and circadian rhythm of sepsis patients in the intensive care unit. In Proceedings of the 2018 IEEE EMBS International Conference on Biomedical & Health Informatics (BHI), Las Vegas, NV, USA, 4–7 March 2018; pp. 17–20. [Google Scholar] [CrossRef] [PubMed]
- Ren, Y.; Balch, J.; Abbott, K.L.; Loftus, T.J.; Shickel, B.; Rashidi, P.; Bihorac, A.; Ozrazgat-Baslanti, T. Computable Phenotypes of Patient Acuity in the Intensive Care Unit. arXiv 2020, arXiv:2005.05163v2. [Google Scholar]
- Contreras, M.; Sena, J.; Davidson, A.; Zhang, J.; Ozrazgat-Baslanti, T.; Ren, Y.; Guan, Z.; Balch, J.; Loftus, T.; Nerella, S.; et al. Mixture-of-Experts Framework for Dynamic Delirium and Coma Prediction in ICU Patients: Development and Validation of an Acute Brain Dysfunction Prediction Model. arXiv 2025, arXiv:2503.06059v1. [Google Scholar]
- Kristensen, L.Q.; Eiskjær, H.; van Tulder, M.; Wæhrens, E.E.E.; Sørensen, L.; Bro-Jeppesen, J.; Eastwood, G.; Oestergaard, L.G. Early ADL ability assessment and cognitive screening as markers of post-discharge outcomes after surviving an out-of-hospital cardiac arrest: A prospective cohort study. Resuscitation 2025, 214, 110653. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.; Elmer, J.; Chen, G.H.; Weiner, J.; Huang, S.; Drashner, M.; Callaway, C.W.; Morabito, D.; Kim, J.; Kymissis, I.; et al. Neurological prognostication of post-cardiac-arrest coma patients using EEG data: A dynamic survival analysis framework with competing risks. arXiv 2023, arXiv:2308.11645. [Google Scholar] [CrossRef]
- Mion, M.; Keeble, T.R. Supporting patients and families following an out-of-hospital cardiac arrest: Developing a multidisciplinary care pathway and the role of neuropsychology. Neuropsychologist 2023, 1, 52. [Google Scholar] [CrossRef]
- Košir, M. Predictive Value of Cerebral and Skeletal Muscle Oxygen Saturation During Resuscitation to Restore Spontaneous Circulation in Cardiac Arrest. Ph.D. Thesis, University of Ljubljana, Ljubljana, Slovenia, 2024. Available online: https://repozitorij.uni-lj.si/IzpisGradiva.php?id=164113 (accessed on 30 May 2025).
- The European Resuscitation Council. European Heart Network. The European Cardiac Arrest Research Strategy 2023–2030. Available online: https://ehnheart.org/wp-content/uploads/2023/10/06892-EHN-Strategic-Plan-2023_External_updated_26.10.pdf (accessed on 30 May 2025).
- Giuvară, S.; Suciu, A.V.; Postoiu, R.L.; Aurelian, S.M.; Daia, C.O.; Băilă, M.; And One, I.; Popescu, C.; Mălăelea, A.D.; Spînu, A.; et al. Rehabilitation challenges in a case of a female patient with cardio-respiratory arrest resuscitated in an intra-hospital environment, associating multiple cardiovascular comorbidities and metabolic pathology—case report. Rom. J. Med. Rehabil. 2024, 1, 181–186. [Google Scholar] [CrossRef]
- Christensen, J.; Eskildsen, S.J.; Winkel, B.G.; Iversen, H.K.; Høgenhaven, H.; Møller, S.; Krøigård, T.; Ravn, H.B.; Rasmussen, L.S.; Madsen, P.L.; et al. Motor and process skills in activities of daily living in survivors of out-of-hospital cardiac arrest: A cross-sectional study at hospital discharge. Eur. J. Cardiovasc. Nurs. 2021, 20, 775–781. [Google Scholar] [CrossRef] [PubMed]
- Henry, T.D.; Tomey, M.I.; Tamis-Holland, J.E.; Thiele, H.; Rao, S.V.; Menon, V.; Klein, D.G.; Naka, Y.; Piña, I.L.; Kapur, N.K.; et al. Invasive management of acute myocardial infarction complicated by cardiogenic shock: A scientific statement from the American Heart Association. Circulation 2021, 143, e815–e829. [Google Scholar] [CrossRef] [PubMed]
- Chahdi, H.O.; Berbach, L.; Boivin-Proulx, L.A.; Xue, Y.; Zahrani, M.; Alkhalfan, S.; Lemor, A.; Garan, A.R.; Mebazaa, A.; Afilalo, J.; et al. Percutaneous mechanical circulatory support in post—Myocardial infarction cardiogenic shock: A systematic review and meta-analysis. Can. J. Cardiol. 2022, 38, 1525–1538. [Google Scholar] [CrossRef] [PubMed]
- Bray, J.E.; Grasner, J.T.; Nolan, J.P.; Iwami, T.; Ong, M.E.H.; Finn, J.; McNally, B.; Nehme, Z.; Sasson, C.; Tijssen, J.; et al. Cardiac Arrest and Cardiopulmonary Resuscitation Outcome Reports: 2024 Update of the Utstein Out-of-Hospital Cardiac Arrest Registry Template. Circulation 2024, 150, e203–e223. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Montfort, J.; Sinha, S.S.; Thayer, K.L.; Hernandez-Suarez, D.F.; Sandhu, A.; Rosner, C.; Mori, M.; Batchelor, W.; Masoudi, F.A.; Carnicelli, A.P.; et al. Clinical outcomes associated with acute mechanical circulatory support utilization in heart failure related cardiogenic shock. Circ. Heart Fail. 2021, 14, e007924. [Google Scholar] [CrossRef] [PubMed]
- Mahtta, D.; Mohammed, I.; Elgendy, I.Y.; Pepine, C.J.; Nicholson, W.J.; Bavry, A.A.; Gulati, M.; Mamas, M.A.; Bhatt, D.L.; Pepine, C.J.; et al. Overview of prevalence, trends, and outcomes of post myocardial infarction mechanical complications. Ann. Cardiothorac. Surg. 2022, 11, 322–324. [Google Scholar] [CrossRef] [PubMed]
- Mowbray, F.I.; Manlongat, D.; Correia, R.H.; Drennan, I.R.; Fernando, S.M.; Toma, A.; MacRedmond, R.; Munshi, L.; Scales, D.C.; Naskou, S.; et al. Prognostic association of frailty with post-arrest outcomes following cardiac arrest: A systematic review and meta-analysis. Resuscitation 2021, 167, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Tweet, M.S.; Gulati, R.; Best, P.J.M.; Hayes, S.N.; Rose, C.H.; Kovacic, J.C.; Codsi, E.; Pellikka, P.A.; Gochanour, B.R.; Bar-rett-O’Keefe, Z.; et al. Pregnancy-associated myocardial infarction: Prevalence, causes, and interventional management. Circ. Cardiovasc. Interv. 2020, 13, e008687. [Google Scholar] [CrossRef] [PubMed]
- Hart, I.; Bhat, V.; Kyazimzade, S.; Taylor, E.; Patel, A.; Nguyen, T.; Johnson, L.; Smith, M.; Williams, R.; Garcia, P.; et al. Incidence and Characteristics of ST-Elevation Myocardial Infarction in Patients with Previous Coronary Artery Bypass Grafting: A Single-Center Experience. Cureus 2025, 17, e363697. [Google Scholar] [CrossRef]
- Blumer, V.; Hanff, T.C.; Gage, A.; Schrage, B.; Kanwar, M.K.; Truesdell, A.G.; Morrow, D.A.; Thiele, H.; Kapur, N.K.; Garan, A.R.; et al. Cardiogenic Shock Teams: Past, Present, and Future Directions. Circ Heart Fail. 2025, 18, e011630. [Google Scholar] [CrossRef] [PubMed]
- Perkins, G.D.; Callaway, C.W.; Haywood, K.; Bradley, P.; Drennan, I.R.; Hazinski, M.F.; Morley, P.T.; Olasveengen, T.M.; Wang, T.L.; Nolan, J.P.; et al. Brain injury after cardiac arrest. Lancet 2021, 398, 1269–1278. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, C.; Bhatty, A.; Batra, G.; Andell, P.; Storey, R.F.; Valgimigli, M.; Halvorsen, S.; Timmis, A.; Bueno, H.; Jernberg, T.; et al. Definitions of clinical study outcome measures for cardiovascular diseases: The European Unified Registries for Heart Care Evaluation and Randomized Trials (EuroHeart). Eur. Heart J. 2025, 46, 190–214. [Google Scholar] [CrossRef] [PubMed]
- Mathews, L.M.; Brewer, L.C. A Review of Disparities in Cardiac Rehabilitation: Evidence, Drivers, and Solutions. J. Cardiopulm. Rehabil. Prev. 2021, 41, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Lazzarin, T.; Tonon, C.R.; Martins, D.; Fávero, E.L.; Baumgratz, T.D.; Pereira, F.W.L.; Pinheiro, V.R.; Ballarin, R.S.; Queiroz, D.A.R.; Azevedo, P.S.; et al. Post-Cardiac Arrest: Mechanisms, Management, and Future Perspectives. J. Clin. Med. 2022, 12, 259. [Google Scholar] [CrossRef] [PubMed]
- Zook, N.; Voss, S.; Nordström, E.B.; Grewe, T.; Lilja, G.; Chocron, R.; Wibrandt, I.; Cronberg, T.; Beiser, D.G.; Moseby-Knappe, M.; et al. Neurocognitive function following out-of-hospital cardiac arrest: A systematic review. Resuscitation 2022, 170, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Chocron, R.; Fahrenbruch, C.; Yin, L.; Guan, S.; Drucker, C.; Shin, J.; Eisenberg, M.; Chatterjee, N.A.; Kudenchuk, P.J.; Rea, T.; et al. Association between functional status at hospital discharge and long-term survival after out-of-hospital cardiac arrest. Resuscitation 2021, 164, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Rajajee, V.; Muehlschlegel, S.; Wartenberg, K.E.; Greer, D.M.; Geocadin, R.G.; Seder, D.B.; Fischbein, N.; Lurie, K.G.; McNett, M.M.; Dhakar, M.B.; et al. Guidelines for neuroprognostication in comatose adult survivors of cardiac arrest. Neurocrit. Care 2023, 38, 533–563. [Google Scholar] [CrossRef] [PubMed]
- Admiraal, M.M.; Ramos, L.A.; Delgado Olabarriaga, S.D.; Marquering, H.A.; Horn, J.; van Rootselaar, A.F. Quantitative analysis of EEG reactivity for neurological prognostication after cardiac arrest. Clin. Neurophysiol. 2021, 132, 2240–2247. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.F.; Wang, T.Y.; Chen, D.S.; Tsai, Y.T.; Lin, T.Y.; Huang, H.C.; Hsieh, M.J.; Wang, C.C.; Cheng, Y.L.; Chao, Y.K.; et al. The effects of mechanical insufflation-exsufflation on lung function and complications in cardiac surgery patients: A pilot study. J. Cardiothorac. Surg. 2021, 16, 202. [Google Scholar] [CrossRef] [PubMed]
- Mayaz, H.; Shrief, S.E.; Elsisi, A.; Elpasiony, N.M.A. Influence of Range of Motion Exercises on Hemodynamic Parameters for Patients on Mechanical Ventilation. J. Health Care Res. 2025, 2, 137–158. Available online: https://journals.ekb.eg/article_409262.html (accessed on 30 May 2025). [CrossRef]
- Carides, M.K. Nurse’s Knowledge of Early Ambulation of the Postoperative Patient and Complication Prevention: A Quality Improvement Project. Master’s Dissertation, Rhode Island College, Providence, RI, USA, 2021. [Google Scholar] [CrossRef]
- Sawyer, K.N. Surviving cardiac arrest—what do we know about recovery & survivorship? Curr. Opin. Crit. Care 2022, 28, 256–261. [Google Scholar] [CrossRef]
- Sepúlveda, P.; Gallardo, A.; Arriagada, R.; González, E.; Rocco, P.R.M.; Battaglini, D. Protocolized strategies to encourage early mobilization of critical care patients: Challenges and success. Crit Care Sci. 2025, 37, e20250128. [Google Scholar] [CrossRef] [PubMed]
- Kazemi, M.; Froutan, R.; Bagheri Moghadam, A. Impact of Inspiratory Muscle Training and Positive Expiratory Pressure on Lung Function and Extubation Success of ICU Patients: A Randomized Controlled Trial. Arch. Acad. Emerg. Med. 2024, 12, e59. [Google Scholar] [CrossRef] [PubMed]
- Semsar-Kazerooni, K.; Dima, D.; Valiquette, J.; Berube-Dufour, J.; Goldfarb, M. Early Mobilization in People with Acute Cardiovascular Disease. Can. J. Cardiol. 2021, 37, 232–240. [Google Scholar] [CrossRef] [PubMed]
- 43rd International Symposium on Intensive Care & Emergency Medicine. Meeting Abstracts. Crit Care 2024, 28, 68. Available online: https://link.springer.com/content/pdf/10.1186/s13054-024-04822-5.pdf (accessed on 30 May 2025).
- 44th International Symposium on Intensive Care & Emergency Medicine. Meeting Abstracts. Crit. Care 2025, 29, 97. Available online: https://link.springer.com/content/pdf/10.1186/s13054-025-05304-y.pdf (accessed on 30 May 2025).
- Panchal, A.R.; Bartos, J.A.; Cabañas, J.G.; Donnino, M.W.; Drennan, I.R.; Hirsch, K.G.; Kudenchuk, P.J.; Kurz, M.C.; Lavonas, E.J.; Morley, P.T.; et al. Part 3: Adult basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2020, 142 (Suppl. 2), S366–S468. [Google Scholar] [CrossRef] [PubMed]
- Elmer, J.; Callaway, C.W. The brain after cardiac arrest. Semin. Neurol. 2017, 37, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Presciutti, A.; Siry-Bove, B.; Newman, M.M.; Cruz, J.; Blewer, A.L.; Morrison, L.J.; Coute, R.A.; Shofer, F.S.; Becker, L.B.; Guerra, K.; et al. Qualitative study of long-term cardiac arrest survivors’ challenges and recommendations for improving survivorship. J. Am. Heart Assoc. 2022, 11, e025713. [Google Scholar] [CrossRef] [PubMed]
- Jonsson, H.; Piscator, E.; Israelsson, J.; Backman, A.; Strömberg, A.; Engerström, L.; Djärv, T.; Claesson, A.; Ring, M.; Samuels-son, C.; et al. Is frailty associated with long-term survival, neurological function and patient-reported outcomes after in-hospital cardiac arrest?—A Swedish cohort study. Resuscitation 2022, 179, 233–242. [Google Scholar] [CrossRef] [PubMed]
- Desch, S.; Freund, A.; Akin, I.; Behnes, M.; Preusch, M.R.; Zelniker, T.A.; Skurk, C.; Landmesser, U.; Graf, T.; Eitel, I.; et al. Angiography after out-of-hospital cardiac arrest without ST-segment elevation. N. Engl. J. Med. 2021, 385, 2544–2553. [Google Scholar] [CrossRef] [PubMed]
- Fasolino, A.; Compagnoni, S.; Baldi, E.; Ristagno, G.; Grieco, D.L.; Scquizzato, T.; Sandroni, C.; Dell’Anna, A.; Mura, P.; Contri, E.; et al. Updates on Post-Resuscitation Care. After the return of spontaneous circulation beyond the 2021 guidelines. Rev. Cardiovasc. Med. 2022, 23, 373. [Google Scholar] [CrossRef] [PubMed]
- Al Lawati, K.; Forestell, B.; Binbraik, Y.; Alsamawi, M.; Pannu, N.; Al Badaai, Y.; Redfern, R.; Pannu, A.; Stanger, J.; Bagshaw, S.M.; et al. Early versus delayed coronary angiography after out-of-hospital cardiac arrest without ST-segment elevation—A systematic review and meta-analysis of randomized controlled trials. Crit. Care Explor. 2023, 5, e0874. [Google Scholar] [CrossRef] [PubMed]
- Bougouin, W.; Lascarrou, J.B.; Chelly, J.; Benghanem, S.; Geri, G.; Maizel, J.; Mira, J.P.; Pelle, J.; Pruvost-Robieux, E.; Vigneron, C.; et al. Performance of the ERC/ESICM-recommendations for neuroprognostication after cardiac arrest: Insights from a prospective multicenter cohort. Resuscitation 2024, 202, 110362. [Google Scholar] [CrossRef] [PubMed]
- Wyckoff, M.H.; Greif, R.; Morley, P.T.; Ng, K.C.; Olasveengen, T.M.; Singletary, E.M.; Smyth, M.A.; Soar, J.; Travers, A.H.; Ve-lazquez, O.; et al. 2022 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations: Summary from the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid task forces. Pediatrics 2023, 151, e2022060463. [Google Scholar] [CrossRef] [PubMed]
- Sandiumenge, A.; Domínguez-Gil, B.; Pont, T.; López-Navidad, A.; Len, O.; Meneu, J.C.; Cañón, J.F.; Cervera, C.; Matesanz, R.; Oppenheimer, F.; et al. Critical pathway for deceased tissue donation: A novel adaptative European systematic approach. Transpl. Int. 2021, 34, 865–871. [Google Scholar] [CrossRef] [PubMed]
- Yuan, F.; Li, H.; Pan, T.; Wen, W.; Wang, L.; Wu, S.; Zhao, H.; Qian, S.; Liu, Z.; Liu, H.; et al. Variability across countries for brain death determination in adults. Brain Inj. 2023, 37, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Drost, G.; Absalom, A.R.; Kuiper, M.A.; van der Jagt, M.; Herold, I.; Pölzleitner, L.; Meijer, F.; Greuters, S.; Verhoeven, F.; Smits, M.; et al. Brain death/death by neurologic criteria determination: An update. Curr. Opin. Anesthesiol. 2021, 35, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Gil, B.; Ascher, N.; Capron, A.M.; Gardiner, D.; Manara, A.R.; Bernat, J.L.; Miñambres, E.; Singh, J.M.; Porte, R.J.; Markmann, J.F.; et al. Expanding controlled donation after the circulatory determination of death: Statement from an international collaborative. Intensiv. Care Med. 2021, 47, 265–281. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Gil, B.; Fernández-Ruiz, M.; Hernández, D.; Crespo, M.; Colmenero, J.; Coll, E.; Rubio, J.J. Organ donation and transplantation during the COVID-19 pandemic: A summary of the Spanish experience. Transplantation 2021, 105, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Bonizzoni, M.A.; Scquizzato, T.; Pieri, M.; Delrio, S.; Nardelli, P.; Ortalda, A.; Dell’Acqua, A.; Scandroglio, A.M.; Turla, O.G.; Francescon, C.; et al. Organ donation after extracorporeal cardiopulmonary resuscitation for refractory out-of-hospital cardiac arrest in a metropolitan cardiac arrest centre in Milan, Italy. Resuscitation 2024, 200, 110214. [Google Scholar] [CrossRef] [PubMed]
- Miranda, L.M.; De Lima, P.E.C.; Miranda, N.D.C.D.; Margraf, G.Z.; Riella, J.; Olandoski, M.; Noronha, I.L.; Garcia, V.D.; Felipe, C.R.; Franco, R.P.; et al. Donor’s therapeutic hypothermia vs. normothermia in kidney transplantation: A meta-analysis of randomized controlled trials. Front. Transplant. 2025, 4, 1564460. [Google Scholar] [CrossRef] [PubMed]
- Morrison, L.J.; Sandroni, C.; Grunau, B.; Parr, M.; Macneil, F.; Perkins, G.D.; Aibiki, M.; Censullo, E.; Lin, S.; Neumar, R.W.; et al. Organ donation after out-of-hospital cardiac arrest: A scientific statement from the International Liaison Committee on Resuscitation. Circulation 2023, 148, e120–e146. [Google Scholar] [CrossRef] [PubMed]
- Freeborn, H.J. Implementing the American Heart Association 2020 Guidelines for Cardiac Arrest in an Urgent Care Setting. Ph.D. Dissertation, Montana State University, Bozeman, MT, USA, 2022. Available online: https://scholarworks.montana.edu/items/2c7d31f4-27cd-4cec-9123-432adf6b6822 (accessed on 30 May 2025).
- Szarpak, L.; Filipiak, K.J.; Mosteller, L.; Jaguszewski, M.; Smereka, J.; Ruetzler, K.; Ahuja, S.; Ladny, J.R.; Surani, S.; Ulaszewski, B.; et al. Survival, neurological and safety outcomes after out-of-hospital cardiac arrests treated by using prehospital therapeutic hypothermia: A systematic review and meta-analysis. Am. J. Emerg. Med. 2021, 42, 168–177. [Google Scholar] [CrossRef] [PubMed]
- Dankiewicz, J.; Cronberg, T.; Lilja, G.; Horn, J.; Friberg, H.; Stammet, P.; Ondruschka, B.; Wanscher, M.; Osorio, M.J.; Callaway, C.W.; et al. Hypothermia versus normothermia after out-of-hospital cardiac arrest. N. Engl. J. Med. 2021, 384, 2283–2294. [Google Scholar] [CrossRef] [PubMed]
- Penketh, J.; Nolan, J.P. Post-Cardiac Arrest Syndrome. J. Neurosurg. Anesthesiol. 2023, 35, 260–264. [Google Scholar] [CrossRef] [PubMed]
- Xiao, A.; Callaway, C.W.; Coppler, P.J.; Dimalanta, C.I.; Dezfulian, C.; Elmer, J.; Frisch, A.; Guyette, F.X.; Jasti, H.; Kilgannon, H.J.; et al. Long-term outcomes of post-cardiac arrest patients with severe neurological and functional impairments at hospital discharge. Resuscitation 2022, 174, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Shin, M.; Fujita, M.; Hifumi, T.; Inoue, A.; Sawano, H.; Kuroda, Y.; Yonemoto, N.; Kawakita, K.; Tahara, Y.; Nishioka, K.; et al. Rapid rewarming rate associated with favorable neurological outcomes in patients with post—Cardiac arrest syndrome patients treated with targeted temperature management. Acute Med. Surg. 2023, 10, e897. [Google Scholar] [CrossRef] [PubMed]
- Sandroni, C.; Nolan, J.P.; Andersen, L.W.; Cariou, A.; Cronberg, T.; Friberg, H.; Lemiale, V.; Soar, J.; Taccone, F.S.; Cariou, A.; et al. ERC-ESICM guidelines on temperature control after cardiac arrest in adults. Intensiv. Care Med. 2022, 48, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Lilja, G.; Ullén, S.; Dankiewicz, J.; Friberg, H.; Levin, H.; Nordström, E.B.; Heimburg, K.; Jakobsen, J.C.; Ahlqvist, M.; Bass, F.; et al. Effects of hypothermia vs normothermia on societal participation and cognitive function at 6 months in survivors after out-of-hospital cardiac arrest: A predefined analysis of the TTM2 randomized clinical trial. JAMA Neurol. 2023, 80, 1070–1079. [Google Scholar] [CrossRef] [PubMed]
- Tajlil, A.; Abdelradi, A.; Mosleh, W.; Kattel, S.; Al Jebaje, Z.; Sharma, U. Abstract Su1205: The effect of targeted temperature management on five-year mortality in comatose out-of-hospital cardiac arrest survivors: A real-world experience. Circulation 2024, 150 (Suppl. 1), ASu1205. [Google Scholar] [CrossRef]
- Abdel Jawad, M.; Gosch, K.; O’Keefe, E. Abstract Su1203: Temporal trends in post-resuscitation fever after in-hospital cardiac arrest. Circulation 2024, 150 (Suppl. 1), ASu1203. [Google Scholar] [CrossRef]
- European Resuscitation Council. EuReCa THREE: European Registry of Cardiac Arrest; European Resuscitation Council: Niel, Belgium, 2022; Available online: https://www.eureca-three.eu (accessed on 30 May 2025).
- Joshi, V.L.; Christensen, J.; Lejsgaard, E.; Rajabally, Y.A.; Dainty, K.N.; Haywood, K.; Moulaert, V.R.M.P.; Lilja, G.; Wilder Schaaf, K.; Elliott, J.; et al. Effectiveness of rehabilitation interventions on the secondary consequences of surviving a cardiac arrest: A systematic review and meta-analysis. BMJ Open 2021, 11, e047251. [Google Scholar] [CrossRef] [PubMed]
- Austenå, M.; Rustøen, T.; Småstuen, M.C.; Valsø, Å.; Sunde, K.; Tøien, K. Return to work during first year after intensive care treatment and the impact of demographic, clinical and psycho-social factors. Intensiv. Crit. Care Nurs. 2023, 76, 103384. [Google Scholar] [CrossRef] [PubMed]
- ESC Working Group on Cardiac Arrest Survivorship. Reintegration Guidelines 2023. European Society of Cardiology. 2023. Available online: https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Acute-Coronary-Syndromes-ACS-Guidelines (accessed on 30 May 2025).
- Amoo, M.; Henry, J.; O’Halloran, P.J.; Whyte, T.; Mcloughlin, S.; Mccreary, C.; Mcdaid, D.; Rawlinson, J.; Williams, D.J.; Nelson, D.W.; et al. S100B, GFAP, UCH-L1 and NSE as predic-tors of abnormalities on CT imaging following mild traumatic brain injury: A systematic review and meta-analysis of diagnostic test accuracy. Neurosurg. Rev. 2022, 45, 1171–1193. [Google Scholar] [CrossRef] [PubMed]
- Harding, L.; Greer, N.; Stacey, W.; Sanderson, T.; Neumar, R.; Mergos, J.; Tiba, M.; Cramer, T.; Hsu, C.; Sandroni, C. Abstract Sa506: Early serial somatosensory evoked potentials can assess brain injury severity and recovery in swine cardiac arrest models. Circulation 2024, 150 (Suppl. 1), Sa506. [Google Scholar] [CrossRef]
- Moseby-Knappe, M.; Cronberg, T. Blood biomarkers of brain injury after cardiac arrest—A dynamic field. Resuscitation 2020, 156, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Wihersaari, L.; Ashton, N.J.; Reinikainen, M.; Jakkula, P.; Pettilä, V.; Hästbacka, J.; Tynkkynen, J.; Tiainen, M.; Häppölä, O.; van Gils, M.; et al. Neurofilament light as an outcome predictor after cardiac arrest: A post hoc analysis of the COMAC-ARE trial. Intensive Care Med. 2021, 47, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Klitholm, M.; Jeppesen, A.N.; Christensen, S.; Parkner, T.; Tybirk, L.; Kirkegaard, H.; Sandfeld-Paulsen, B.; Grejs, A.M. Neurofilament Light Chain and Glial Fibrillary Acidic Protein as early prognostic biomarkers after out-of-hospital cardiac arrest. Resuscitation 2023, 193, 109983. [Google Scholar] [CrossRef] [PubMed]
- Wagner, M.K.; Berg, S.K.; Hassager, C.; Borregaard, B.; Rasmussen, T.B.; Ekholm, O.; Stenbæk, D.S. Cognitive impairment and psychopathology in sudden out-of-hospital cardiac arrest survivors: Results from the REVIVAL cohort study. Resuscitation 2023, 192, 109984. [Google Scholar] [CrossRef] [PubMed]
- Amacher, S.A.; Bohren, C.; Blatter, R.; Becker, C.; Beck, K.; Mueller, J.; Loretz, N.; Gross, S.; Tisljar, K.; Sutter, R.; et al. Long-term survival after out-of-hospital cardiac arrest: A systematic review and meta-analysis. JAMA Cardiol. 2022, 7, 633–643. [Google Scholar] [CrossRef] [PubMed]
- Secher, N.; Adelborg, K.; Szentkúti, P.; Schmidt, M.; Søholm, H.; Kjærgaard, J.; Rørth, R.; Torp-Pedersen, C.; Kragholm, K.; Gerds, T.A.; et al. Evaluation of neurologic and psychiatric outcomes after hospital discharge among adult survivors of cardiac arrest. JAMA Netw. Open 2022, 5, e2213546. [Google Scholar] [CrossRef] [PubMed]
- Morrison, L.J.; Hunt, E.A.; Grunau, B.; Neumar, R.W.; Becker, L.B.; Aufderheide, T.P.; Bobrow, B.J.; Callaway, C.W.; Yannopoulos, D.; Girotra, S.; et al. International Consensus on Evidence Gaps and Research Opportunities in Extracorporeal Cardiopulmonary Resuscitation for Refractory Out-of-Hospital Cardiac Arrest: A report from the National Heart, Lung, and Blood Institute workshop. J. Am. Heart Assoc. 2025, 14, e036108. [Google Scholar] [CrossRef] [PubMed]
- Merchant, R.M.; Becker, L.B.; Brooks, S.C.; Chan, P.S.; Del Rios, M.; McBride, M.E.; Neumar, R.W.; Previdi, J.K.; Uzendu, A.; Sasson, C.; et al. The American Heart Association Emergency Cardiovascular Care 2030 Impact Goals and Call to Action to Improve Cardiac Arrest Outcomes: A Scientific Statement From the American Heart Association. Circulation 2024, 149, e914–e933. [Google Scholar] [CrossRef] [PubMed]
- Wagner, M.K.; Kikkenborg Berg, S.; Hassager, C.; Borregaard, B.; Rorth, R.; Zierau, L.; Brogaard, J.B. Feeling understood for the first time: Experiences of participation in rehabilitation after out-of-hospital sudden cardiac arrest. Eur. J. Cardiovasc. Nurs. 2021, 20, 767–774. [Google Scholar] [CrossRef] [PubMed]
- Haywood, K.L.; Southern, C.; Tutton, E.; Swindell, P.; Ellard, D.; Pearson, N.A.; Parsons, H.; Couper, K.; Daintyi, K.N.; Agarwal, S.; et al. An international collaborative study to co-produce a patient-reported outcome measure of cardiac arrest survivorship and health-related quality of life (CASHQoL): A protocol for developing the long-form measure. Resusc. Plus 2022, 11, 100288. [Google Scholar] [CrossRef] [PubMed]
- Allen, M.B.; Orkaby, A.R.; Justice, S.; Wang, E.Y.; Pieracci, F.M.; Arya, S.; Qian, F.; Brown, C.V.R.; Shah, A.S.; Cooper, Z.; et al. Frailty and outcomes following cardiopulmonary resuscitation for perioperative cardiac arrest. JAMA Netw. Open 2023, 6, e2321465. [Google Scholar] [CrossRef] [PubMed]
- Buckley, B.J.R.; Harrison, S.L.; Fazio-Eynullayeva, E.; Darby, S.C.; Lane, D.A.; Packer, M.; Petrie, M.C.; Poppe, K.K.; Sarma, S.; Lewsey, J.D.; et al. Cardiac rehabilitation and all-cause mortality in patients with heart failure: A retrospective cohort study. Eur. J. Prev. Cardiol. 2021, 28, 1704–1710. [Google Scholar] [CrossRef] [PubMed]

| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Peer-reviewed articles published between 2020 and 2025 | Articles published prior to 2020 or after 2025 |
| Publications subjected to editorial and peer review processes | Non-peer-reviewed works, editorials, letters to the editor, or conference abstracts lacking full-text availability |
| Studies explicitly addressing rehabilitation following return of spontaneous circulation (ROSC) after SCA | Studies not related to post-ROSC rehabilitation or focusing exclusively on acute or resuscitative care |
| Articles aligned with evidence-based official and newest clinical guidelines. | Articles omitting or disregarding contemporary resuscitation or rehabilitation guidelines |
| Original research: randomized controlled trials, cohort studies, observational analyses, and structured reviews | Publications with low methodological quality, lacking a clearly defined study design or analytical rigor |
| Studies addressing neurological, cardiopulmonary, neurocognitive, or psychosocial rehabilitation domains | Articles solely focusing on preclinical, pharmacological, or procedural resuscitation measures |
| Articles published in the English language | Publications in languages other than English |
| Full-text availability for critical appraisal and synthesis | Articles without accessible full text, with limited eligibility for methodological evaluation |
| No. | Author (Year) | Population (N) | Intervention | Outcome | CPC/mRS | Rehabilitation Stage | Notes |
|---|---|---|---|---|---|---|---|
| 1 | Harding L et al. (2024) [99] | 20 (animal model) | SEP measurement after ROSC | Lower SEP amplitudes correlated with more severe brain injury. | Experimental model—no CPC assessment. | Early post-ROSC phase (0–72 h) | Indicates the utility of SEP as a prognostic tool. |
| 2 | Bakhsh A et al. (2024) [17] | 86 in-hospital cardiac arrest patients | Fever prevention vs. no temperature control. | CPC 1–2: 52% vs. 31% (p = 0.03) | CPC | Acute phase of intensive care | Statistically significant difference —better neurological outcomes. |
| 3 | Sepúlveda P et al. (2025) [62] | ICU patients (narrative review) | Protocolized early mobilization (screening, PT-led activity within ~72 h) | Reduced duration of mechanical ventilation and ICU stay | Not assessed | Early mobilization phase | Emphasizes multidisciplinary teamwork, education, safety screening (hemodynamic, respiratory, neurological), func-tional mobilization and outcome documentation |
| 4 | Shen X et al. (2023) [35] | 93 coma patients after cardiac arrest | EEG analysis combined with a dynamic risk model. | EEG variability correlated with CPC 1–2 at 6 months. | CPC | 0–7 days (prognostic phase) | Potential for individualized rehabilitation based on EEG findings. |
| 5 | Nolan JP et al. (2021) [2] | Pooled data from RCTs and registries | ERC guidelines: rehabilitation, neuro-observation, TTM. | CPC 1–2 in 48–55% of patients after OHCA. | CPC | In-hospital and post-discharge | Strong recommendation for a multidisciplinary approach. |
| 6 | Gräsner J-T et al. (2021) [3] | EU registry: >250,000 OHCA cases | Observation: contribution of rehabilitation to survival. | ROSC: 27%; Survival to discharge: 9.4% | No data available, mortality only. | No intervention, population-based analysis. | Data support the need for post-ROSC care. |
| 7 | Christensen J et al. (2024) [29] | Planned: 300 OHCA survivors | Multidisciplinary rehabilitation focused on RTW. | Study protocol —results unpublished. | Planned: mRS, RTW. | Post-discharge (long-term RTW) | To be utilized upon the publication of results. |
| 8 | Wang J et al. (2024) [18] | 786 patients from 12 studies (ECPR + TTM). | Comparison of TTM: 32 °C, 33 °C, 36 °C, no temperature control. | TTM at 33 °C: CPC 1–2 in 56% vs. no TTM: 42%. | CPC | Intensive care phase (24–72 h) | Best outcomes observed at 33 °C; meta-analysis. |
| 9 | Joshi VL et al. (2022) [13] | 82 post-cardiac arrest survivors referred to residential rehab | Structured residential rehabilitation targeting fatigue, cognition, and psychological sequelae | 88% program completion; significant reduction in fatigue (mean improvement: 13.5 points, p < 0.001); improved MoCA and HADS scores | MoCA, HADS; no CPC | Post-discharge (residential, subacute phase) | Demonstrated feasibility and clinical benefit of residential multimodal rehabilitation; supports implementation in recovery pathways. |
| 10 | Giuvară S et al. (2024) [39] | 1 female OHCA patient with comorbidities | Physiotherapy, mobilization, and dietary education. | After 4 weeks: improved limb strength, increased independence (Barthel + 20%). | No numerical CPC data available. | Post-hospital rehabilitation | Single case—clinical illustration. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salwa, K.; Kaziród-Wolski, K.; Rębak, D.; Sielski, J. Current Perspectives on Rehabilitation Following Return of Spontaneous Circulation After Sudden Cardiac Arrest: A Narrative Review. Healthcare 2025, 13, 1865. https://doi.org/10.3390/healthcare13151865
Salwa K, Kaziród-Wolski K, Rębak D, Sielski J. Current Perspectives on Rehabilitation Following Return of Spontaneous Circulation After Sudden Cardiac Arrest: A Narrative Review. Healthcare. 2025; 13(15):1865. https://doi.org/10.3390/healthcare13151865
Chicago/Turabian StyleSalwa, Kamil, Karol Kaziród-Wolski, Dorota Rębak, and Janusz Sielski. 2025. "Current Perspectives on Rehabilitation Following Return of Spontaneous Circulation After Sudden Cardiac Arrest: A Narrative Review" Healthcare 13, no. 15: 1865. https://doi.org/10.3390/healthcare13151865
APA StyleSalwa, K., Kaziród-Wolski, K., Rębak, D., & Sielski, J. (2025). Current Perspectives on Rehabilitation Following Return of Spontaneous Circulation After Sudden Cardiac Arrest: A Narrative Review. Healthcare, 13(15), 1865. https://doi.org/10.3390/healthcare13151865






