Tailored Rehabilitation Program and Dynamic Ultrasonography After Surgical Repair of Bilateral Simultaneous Quadriceps Tendon Rupture in a Patient Affected by Gout: A Case Report
Abstract
1. Introduction
2. Materials and Methods
2.1. Case Presentation
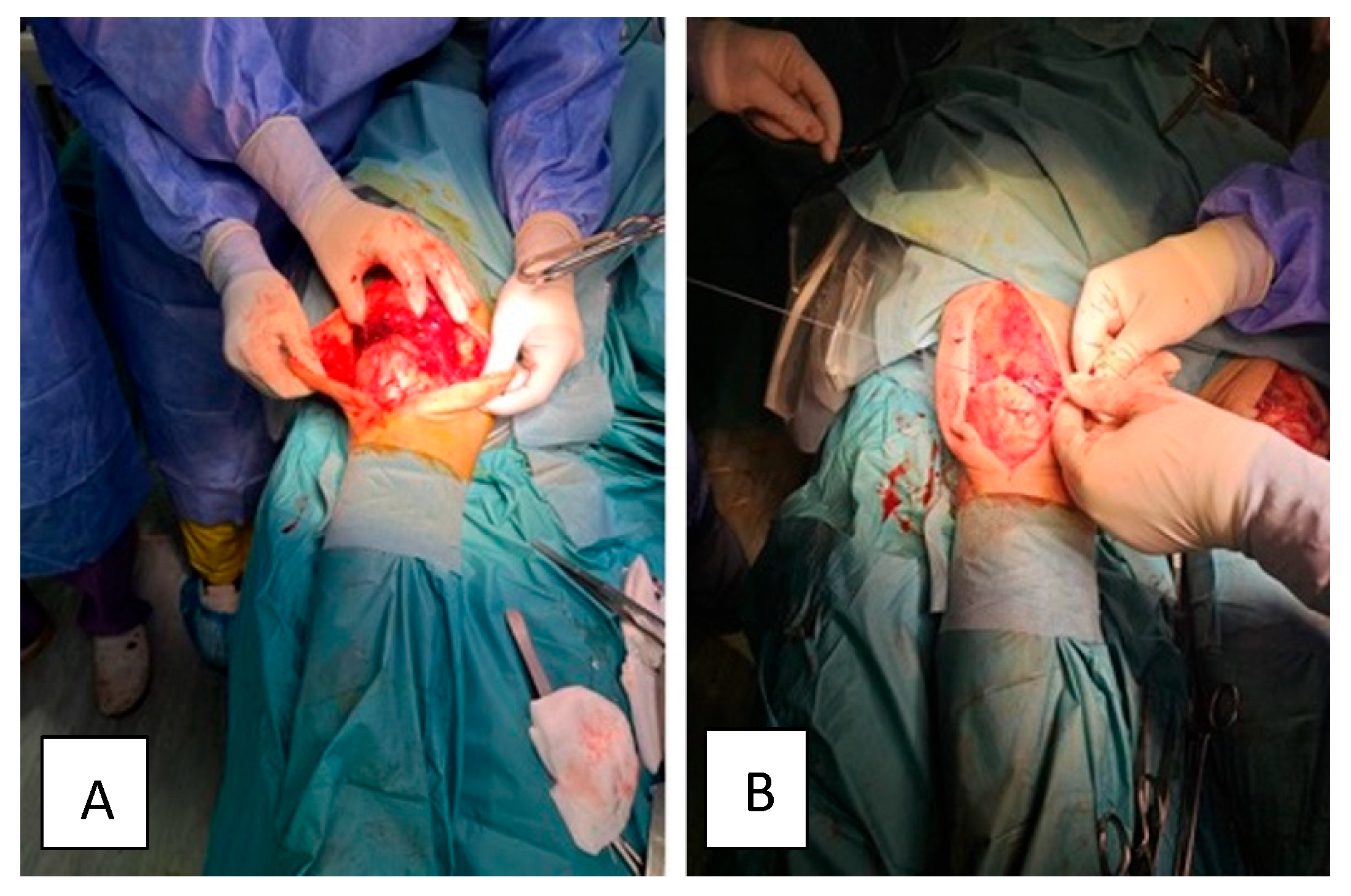
2.2. Surgical Treatment
2.3. Post-Surgical Rehabilitation Program
2.4. Dynamic Sonography for Optimizing Post-Rehabilitation Program
2.5. Single Lateral Hip Joint Manipulation at Six Months Considering Better Biomechanical Support and Neuromuscular Aspects
3. Discussion
Take-Home Messages
- Prompt referral and MRI confirmation can reduce misdiagnosis and improve surgical timing and outcomes;
- Timely surgical intervention is essential to prevent tendon retraction and irreversible muscle atrophy;
- A dynamic and individualized rehabilitation program guided by serial dynamic musculoskeletal ultrasound and thorough clinical evaluation ensures that therapy adapts to the patient’s healing trajectory; continuous monitoring supports tissue healing, muscle reactivation, and safe progression in mobility, strength, and function;
- Home-based and long-term recovery strategies extend functional gains beyond inpatient care, promoting independence and reducing healthcare burden;
- The role of manual therapy in functional reintegration after a single high-velocity, low-amplitude hip manipulation, strategically applied at 6 months post-surgery, may facilitate neuromuscular activation and improve biomechanical alignment; when used selectively, manual therapy can enhance proprioception and support return to ADLs;
- Active goal-setting and multidisciplinary involvement: engaging the patient in active goal-setting fosters motivation and promotes recovery; close collaboration between surgical and physical and rehabilitation medicine teams enables comprehensive care that addresses strength, function, and stability.
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADL | Activities of daily living |
| AROM | Active range of motion |
| BSQTR | Bilateral simultaneous quadriceps tendon rupture |
| FAC | Functional ambulation categories |
| QoL | Quality of life |
| RCT | Randomized controlled trial |
| ROM | Range of motion |
| SEBT | Star Excursion Balance Test |
| TUG | Timed Up and Go Test |
| VAS | Visual Analogue Scale |
References
- Vasiliadis, A.V.; Maris, A.; Tsoupli, A.; Saridis, A. Rehabilitation exercise program after surgical treatment of quadriceps tendon rupture: A case report. Phys. Ther. Sport 2019, 39, 82–89. [Google Scholar] [CrossRef]
- Portugal, D.M.; Capelo, J.A.; Martins, B.D.; Ribeiro, I.M.; Ataíde, S.R.; Vera-Cruz, C.V. Rehabilitation Approach After Surgical Repair of Spontaneous Bilateral Quadriceps Tendon Rupture in a Healthy Mason. Am. J. Phys. Med. Rehabil. 2019, 98, e43–e46. [Google Scholar] [CrossRef]
- Arras, C.; Krause, M.; Frosch, K.H. Quadriceps Tendon and Patellar Tendon Rupture. Z. Orthop. Unfall. 2025, 163, 181–194. (In German) [Google Scholar] [CrossRef]
- Moura, D.L.; Marques, J.P.; Pinheiro, J.P.; Fonseca, F. Total bilateral ruptures of the knee extensor apparatus. Rev. Bras Ortop. 2016, 52, 663–669. [Google Scholar] [CrossRef]
- Onuoha, K.M.; Ajiboye, O.K.; Kumar, R. Spontaneous bilateral quadriceps tendon rupture: A case report. Pan Afr. Med. J. 2020, 37, 84. [Google Scholar] [CrossRef]
- Mishra, B.; Raj, M.; Behera, S.; Bhadani, J.S.; Kumar, R.; Kumar, P. Bilateral Traumatic Rupture of the Quadriceps Tendon—A Case Report. J. Orthop. Case Rep. 2024, 14, 36–40. [Google Scholar] [CrossRef]
- Ellanti, P.; Davarinos, N.; Morris, S.; Rice, J. Bilateral synchronous rupture of the quadriceps tendon. Ir. J. Med. Sci. 2012, 181, 423–425. [Google Scholar] [CrossRef]
- Allata, Y.; Chouhani, B.; El Bardai, G.; Kabbali, N.; Houssaini, T.S. A Spontaneous Bilateral Quadriceps Tendon Rupture in a Patient Undergoing Long-Term Hemodialysis. Cureus 2023, 15, e36059. [Google Scholar] [CrossRef]
- Perfitt, J.S.; Petrie, M.J.; Blundell, C.M.; Davies, M.B. Acute quadriceps tendon rupture: A pragmatic approach to diagnostic imaging. Eur. J. Orthop. Surg. Traumatol. 2014, 24, 1237–1241. [Google Scholar] [CrossRef]
- Thermann, H.; Reimer, P.; Milbradt, H.; Zwipp, H.; Hoffmann, R.; Wippermann, B. Primary sonographic diagnosis and follow-up of muscular and tendon injuries of the lower extremity. Unfallchirurg 1992, 95, 412–418. [Google Scholar]
- Richman, M.; Kieffer, A.; Moss, R.; Dexeus, D. Patella Fracture Identified Using Point-of-care Ultrasound. Prague Med. Rep. 2021, 122, 308–312. [Google Scholar] [CrossRef]
- Pope, J.D.; El Bitar, Y.; Mabrouk, A.; Plexousakis, M.P. Quadriceps Tendon Rupture. In StatPearls Publishing; StatPearls: Treasure Island, FL, USA, 2025. [Google Scholar] [PubMed]
- Sánchez Romero, E.A.; Pollet, J.; Martín Pérez, S.; Alonso Pérez, J.L.; Muñoz Fernández, A.C.; Pedersini, P.; Barragán Carballar, C.; Villafañe, J.H. Lower Limb Tendinopathy Tissue Changes Assessed through Ultrasound: A Narrative Review. Medicina 2020, 56, 378. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Muñoz-Fernández, A.C.; Barragán-Carballar, C.; Villafañe, J.H.; Martín-Pérez, S.; Alonso-Pérez, J.L.; Díaz-Meco, R.; García-Jiménez, D.; Sánchez-Romero, E.A. A new ultrasound-guided percutaneous electrolysis and exercise treatment in patellar tendinopathy: Three case reports. Front. Biosci. (Landmark Ed.) 2021, 26, 1166–1175, Erratum in Front. Biosci. (Landmark Ed.) 2022, 27, 109. [Google Scholar] [CrossRef]
- Runge, N.; Aina, A.; May, S. The benefits of adding manual therapy to exercise therapy for improving pain and function in patients with knee or hip osteoarthritis: A systematic review with meta-analysis. J. Orthop. Sports Phys. Ther. 2022, 52, 675-A13. [Google Scholar] [CrossRef]
- Motealleh, A.; Gheysari, E.; Shokri, E.; Sobhani, S. The Immediate Effect of Lumbopelvic Manipulation on EMG Activity of Vasti and Gluteus Medius in Athletes with Patellofemoral Pain Syndrome: A Randomized Controlled Trial. Man. Ther. 2016, 22, 16–21. [Google Scholar] [CrossRef]
- Gao, X.; Shao, Z.; Liu, S.; Xiang, J. A case report of spontaneous rupture of the quadriceps tendon. Clin. Case Rep. 2017, 5, 1477–1481. [Google Scholar] [CrossRef]
- Arumilli, B.; Adeyemo, F.; Samarji, R. Bilateral simultaneous complete quadriceps rupture following chronic symptomatic tendinopathy: A case report. J. Med. Case Rep. 2009, 3, 9031. [Google Scholar] [CrossRef]
- Abduljabbar, F.H.; Aljurayyan, A.; Ghalimah, B.; Lincoln, L. Bilateral Simultaneous Quadriceps Tendon Rupture in a 24-Year-Old Obese Patient: A Case Report and Review of the Literature. Case Rep. Orthop. 2016, 2016, 4713137. [Google Scholar] [CrossRef]
- Yan, J. Acute unilateral rupture of the quadriceps tendon. Univ. West. Ont. Med. J. 2012, 81, 5e7. [Google Scholar]
- Saito, H.; Shimada, Y.; Yamamura, T.; Yamada, S.; Sato, T.; Nozaka, K.; Sato, T.; Nozaka, K.; Kijima, H.; Saito, K. Arthroscopic quadriceps tendon repair: Two case reports. Case Rep. Orthop. 2015, 2025, 937581. [Google Scholar] [CrossRef]
- Manent, A.; Lopez, L.; Vilanova, J.; Mota, T.; Alvarez, J.; Santamaría, A.; Oliva, X.M. Assessment of the resistance of several suture techniques in human cadaver achilles tendons. J. Foot Ankle Surg. 2017, 56, 954e959. [Google Scholar] [CrossRef]
- McKeon, B.P.; Heming, J.F.; Fulkerson, J.; Langeland, R. The Krackow stitch: A biomechanical evaluation of changing the number of loops versus the number of sutures. Arthroscopy 2006, 22, 33–37. [Google Scholar] [CrossRef]
- Ortiz, C.; Wagner, E.; Mococain, P.; Labarca, G.; Keller, A.; Del Buono, A.; Maffulli, N. Biomechanical comparison of four methods of repair of the Achilles tendon. J. Bone Jt. Surg. Am. 2012, 94, 663e667. [Google Scholar] [CrossRef]
- Gao, M.F.; Yang, H.L.; Shi, W.D. Simultaneous bilateral quadriceps tendon rupture in a patient with hyperparathyroidism undergoing long-term haemodialysis: A case report and literature review. J. Int. Med. Res. 2013, 41, 1378–1383. [Google Scholar] [CrossRef]
- Assiotis, A.; Pengas, I.; Vemulapalli, K. Bilateral quadriceps tendon rupture in a seasoned marathon runner with patellar spurs. Grand Rounds 2011, 11, 77–80. [Google Scholar] [CrossRef]
- Levinson, J.; Mixon, A. Delayed Diagnosis of Quadriceps Tendon Rupture. Cureus 2024, 16, e71270. [Google Scholar] [CrossRef]
- Fanchini, M.; Impellizzeri, F.M.; Silbernagel, K.G.; Combi, F.; Benazzo, F.; Bizzini, M. Return to competition after an achilles tendon rupture using both on and off the field load monitoring as guidance: A case report of a top-level soccer player. Phys. Ther. Sport 2018, 29, 70–78. [Google Scholar] [CrossRef]
- Toker, S.; Oak, N.; Williams, A.; Ipaktchi, K.; Ozer, K. Adherence to therapy after flexor tendon surgery at a level 1 trauma center. Hand 2014, 9, 175–178. [Google Scholar] [CrossRef]
- Lyu, K.; Liu, X.; Jiang, L.; Chen, Y.; Lu, J.; Zhu, B.; Liu, X.; Li, Y.; Wang, D.; Li, S. The Functions and Mechanisms of Low-Level Laser Therapy in Tendon Repair (Review). Front. Physiol. 2022, 13, 808374. [Google Scholar] [CrossRef]
- Poorpezeshk, N.; Ghoreishi, S.K.; Bayat, M.; Pouriran, R.; Yavari, M. Early Low-Level Laser Therapy Improves the Passive Range of Motion and Decreases Pain in Patients with Flexor Tendon Injury. Photomed. Laser Surg. 2018, 36, 530–535. [Google Scholar] [CrossRef]
- Bolgla, L.A.; Boling, M.C. An update for the conservative management of patellofemoral pain syndrome: A systematic review of the literature from 2000 to 2010. Int. J. Sports Phys. Ther. 2011, 6, 112–125. [Google Scholar]
- Studnicki, R.; Sochaj, M.; Skup, K.; Niespodziński, B.; Aschenbrenner, P.; Laskowski, R.; Łuczkiewicz, P. The Impact of a Single Hip Manipulation on Quadriceps Activity and Performance: A Randomized Study. Biomedicines 2025, 13, 900. [Google Scholar] [CrossRef]
- Lepley, A.S.; Gribble, P.A.; Thomas, A.C.; Tevald, M.A.; Sohn, D.H.; Pietrosimone, B.G. Quadriceps neural alterations in anterior cruciate ligament reconstructed patients: A 6-month longitudinal investigation. Scand. J. Med. Sci. Sports 2015, 25, 828–839. [Google Scholar] [CrossRef]
- Khella, C.M.; Horvath, J.M.; Asgarian, R.; Rolauffs, B.; Hart, M.L. Anti-Inflammatory Therapeutic Approaches to Prevent or Delay Post-Traumatic Osteoarthritis (PTOA) of the Knee Joint with a Focus on Sustained Delivery Approaches. Int. J. Mol. Sci. 2021, 22, 8005. [Google Scholar] [CrossRef]
- Blasimann, A.; Koenig, I.; Baert, I.; Baur, H.; Vissers, D. Which assessments are used to analyze neuromuscular control by electromyography after an anterior cruciate ligament injury to determine readiness to return to sports? A systematic review. BMC Sports Sci. Med. Rehabil. 2021, 13, 142. [Google Scholar] [CrossRef]
- Studnicki, R.; Tomaszewsk, U.; Hansdorfer-Korzon, R.; Kawczyński, A. Comparing the Acute Effects of Diagonal Mobilization and Nordic Hamstring Curls on Knee Flexion and Extension Strength: A Randomized, Double-Blinded Parallel Study in Young Soccer Players. Appl. Sci. 2024, 14, 8610. [Google Scholar] [CrossRef]
- Niazi, I.K.; Navid, M.S.; Merkle, C.; Amjad, I.; Kumari, N.; Trager, R.J.; Holt, K.; Haavik, H. A randomized controlled trial comparing different sites of high-velocity low amplitude thrust on sensorimotor integration parameters. Sci. Rep. 2024, 14, 1159. [Google Scholar] [CrossRef]



| Phase | Timeline | Key Goals | Interventions | Measurements |
|---|---|---|---|---|
| Phase 1 | Weeks 1–4 | Pain management; wound healing and surgical protection; maintain ROM, muscle strength, and overall function | Knee braces locked in full extension; LLLT therapy; Cardiovascular support; Passive ROM; Muscle activation. | VAS, ROM, ADL, FAC |
| Phase 2 | Weeks 5–7 | Regain motion; initiate muscle strengthening exercises; cardiovascular rehabilitation | Braces (until week 6); Passive mobilization; Begin active strengthening; | VAS, ROM, ADL, FAC |
| Phase 3 | Weeks 8–9 | Normalize gait; increase strength and ROM; regain ADL independence | Progressive strengthening; Walking on even and uneven surfaces; Stair training. | VAS, ROM, ADL, FAC |
| Phase 4 | Week 10 onward | Social and work reintegration; sport resumption | Tailored home-rehabilitation program; Printed handout; Mild aerobic exercises. | Follow-up ROM; ADL; return-to-work and non-contact sport activities |
| Outcome Measures | T0 | T1 | T2 | T3 | T4 |
|---|---|---|---|---|---|
| Right Knee AROM (degrees) | 0 | 25 | 55 | 95 | Full |
| Left Knee AROM (degrees) | 0 | 20 | 60 | 90 | Full |
| VAS | 7 | 4 | 3 | 1 | 0 |
| FAC | 0 | 0 | 1 | 5 | 5 |
| ADL | 6 | 6 | 7 | 10 | 10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mihai, E.E.; Teodorescu, M.; Iordache, S.; Cirstoiu, C.; Berteanu, M. Tailored Rehabilitation Program and Dynamic Ultrasonography After Surgical Repair of Bilateral Simultaneous Quadriceps Tendon Rupture in a Patient Affected by Gout: A Case Report. Healthcare 2025, 13, 1830. https://doi.org/10.3390/healthcare13151830
Mihai EE, Teodorescu M, Iordache S, Cirstoiu C, Berteanu M. Tailored Rehabilitation Program and Dynamic Ultrasonography After Surgical Repair of Bilateral Simultaneous Quadriceps Tendon Rupture in a Patient Affected by Gout: A Case Report. Healthcare. 2025; 13(15):1830. https://doi.org/10.3390/healthcare13151830
Chicago/Turabian StyleMihai, Emanuela Elena, Matei Teodorescu, Sergiu Iordache, Catalin Cirstoiu, and Mihai Berteanu. 2025. "Tailored Rehabilitation Program and Dynamic Ultrasonography After Surgical Repair of Bilateral Simultaneous Quadriceps Tendon Rupture in a Patient Affected by Gout: A Case Report" Healthcare 13, no. 15: 1830. https://doi.org/10.3390/healthcare13151830
APA StyleMihai, E. E., Teodorescu, M., Iordache, S., Cirstoiu, C., & Berteanu, M. (2025). Tailored Rehabilitation Program and Dynamic Ultrasonography After Surgical Repair of Bilateral Simultaneous Quadriceps Tendon Rupture in a Patient Affected by Gout: A Case Report. Healthcare, 13(15), 1830. https://doi.org/10.3390/healthcare13151830






