The Impact of Prophylactic Polishing Pastes on the Surface Roughness, Color, and Stain Resistance of CAD/CAM Restorative Materials
Abstract
1. Introduction
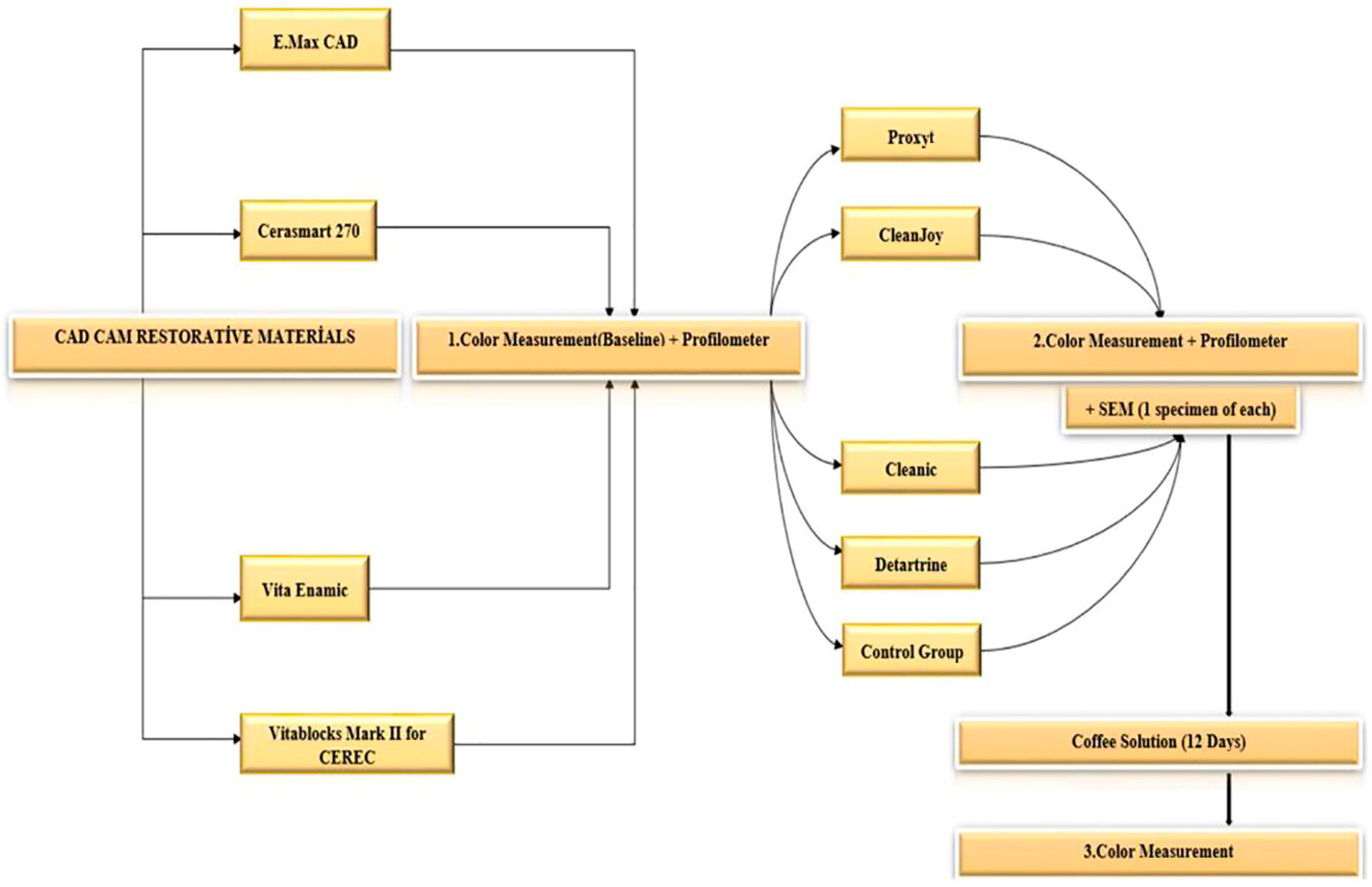
2. Material and Methods
Statistical Analysis
3. Results
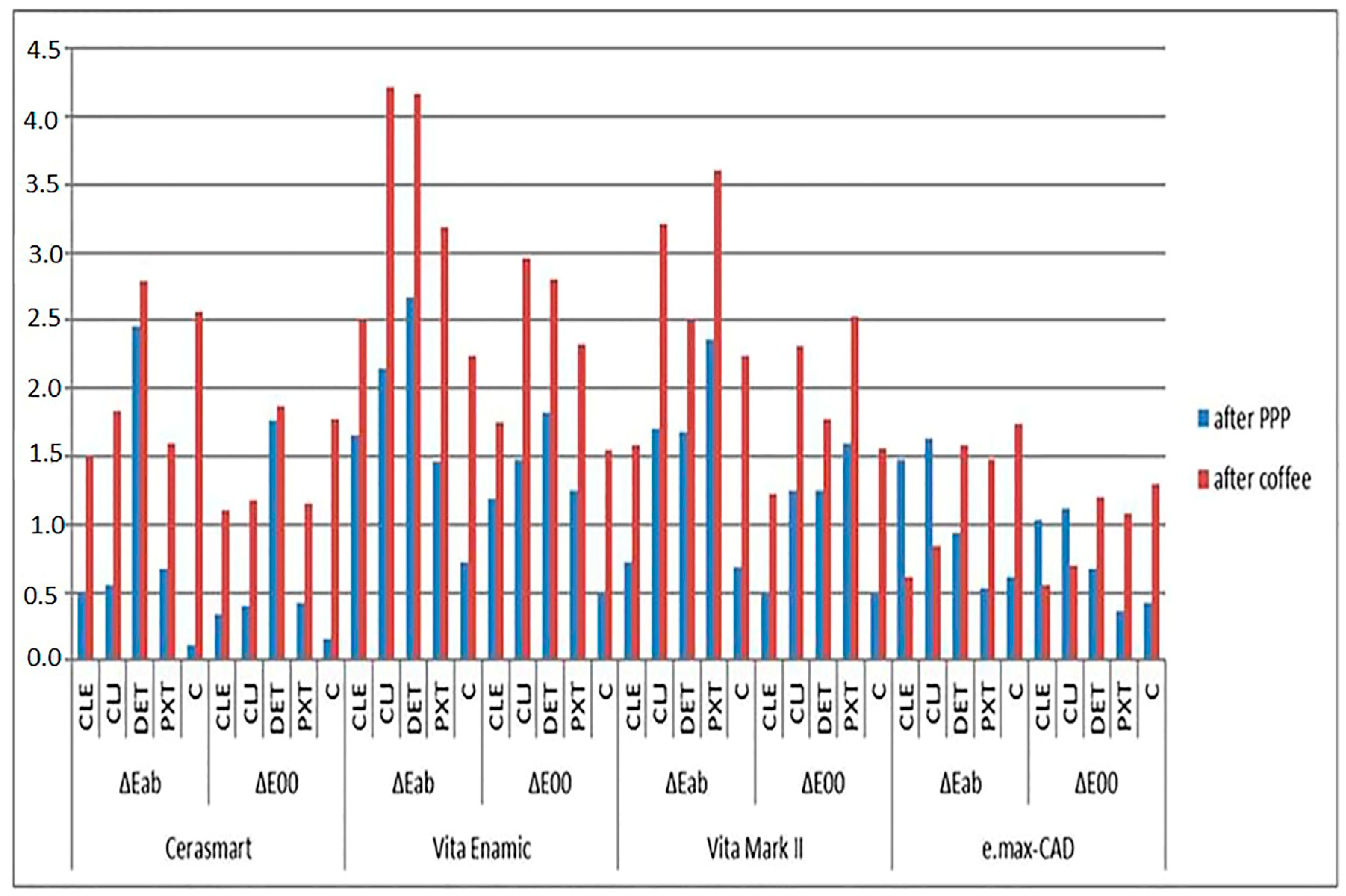
3.1. Color Change Across Groups
3.2. Prophylaxis Paste Impact on Color Differences
3.3. Whiteness Differences Across Pastes
3.4. Clinically Acceptable Thresholds After PPP
3.5. Color and Whiteness Changes After Immersion in Coffee Solution
3.6. Clinically Acceptable Thresholds After Coffee
3.7. Surface Roughness (Ra Parameter) Analysis
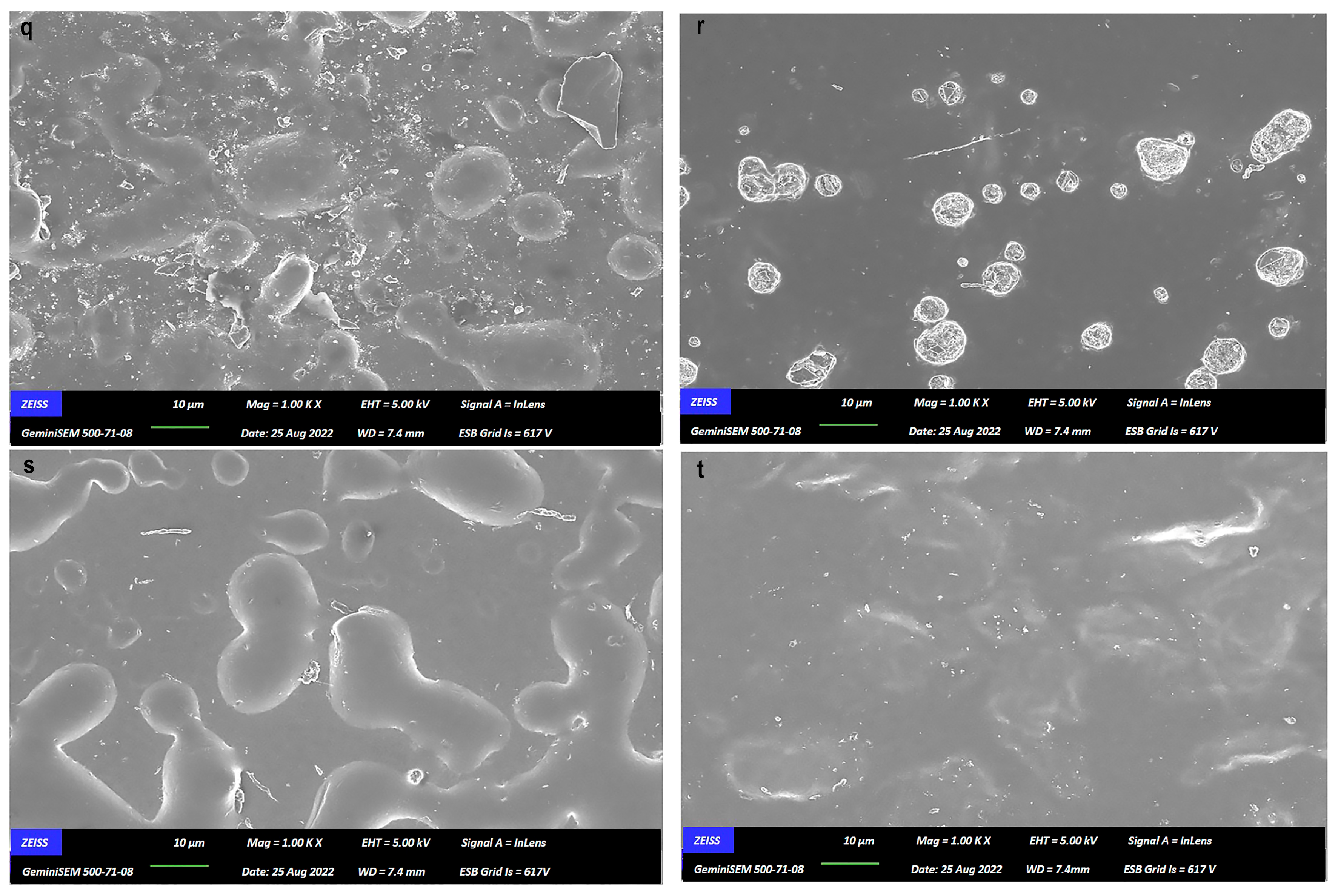
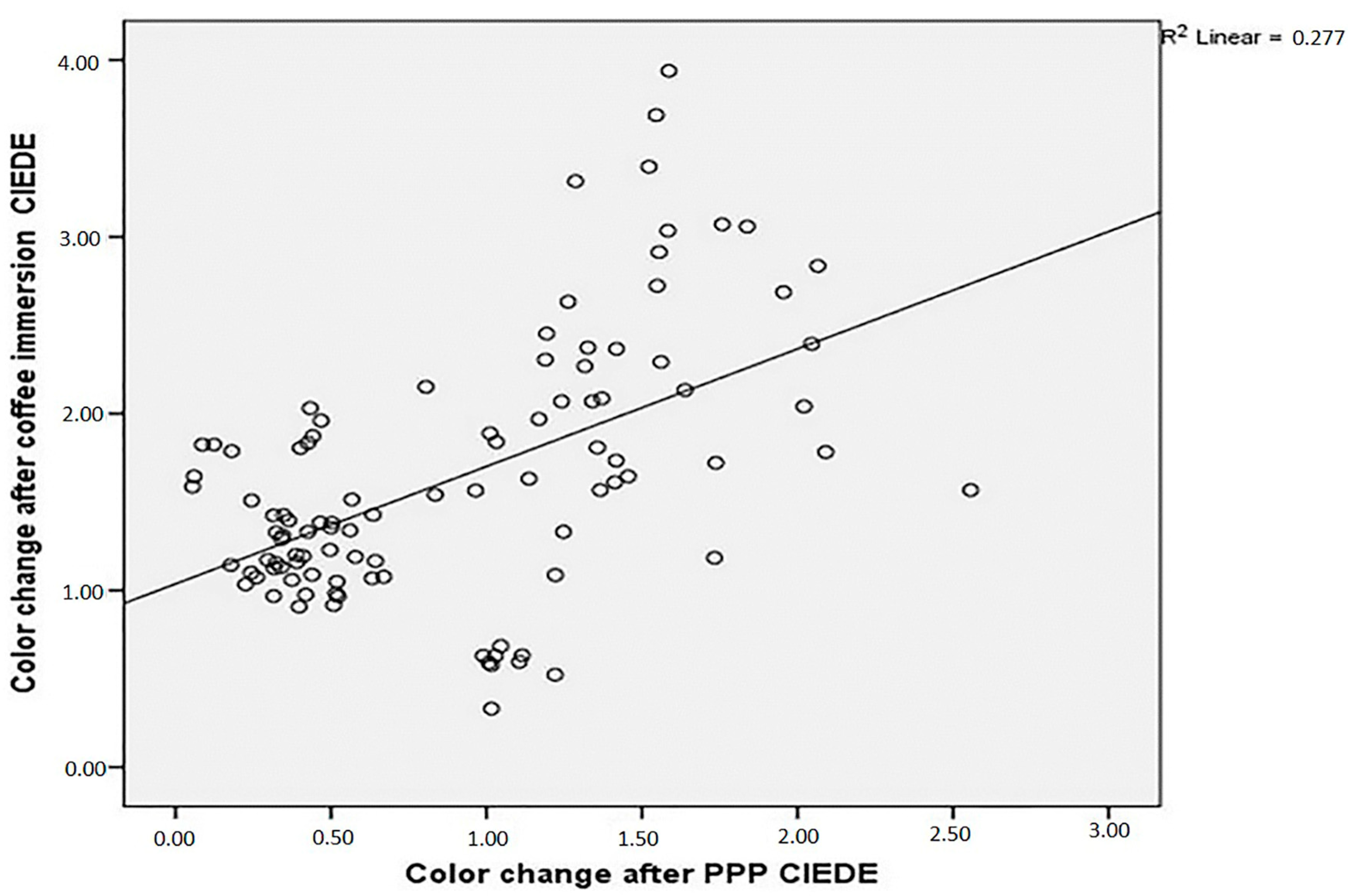
3.8. SEM Microphotographs and Correlations
3.9. Effect of Single vs. Multi-Stage Pastes
4. Discussion
5. Conclusions
- CAD/CAM restorative materials show a material-specific response to the influence of prophylactic polishing pastes on color and surface roughness.
- There was no discernible relationship found between the surface roughness resulting from the application of prophylactic polishing pastes and the discoloration of CAD/CAM materials.
- According to both approaches for color measurement, a moderate positive correlation was noted between ΔE1 and ΔE2.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bona, A.D.; Pecho, O.E.; Ghinea, R.; Cardona, J.C.; Pérez, M.M. Colour parameters and shade correspondence of CAD-CAM ceramic systems. J. Dent. 2015, 43, 726–734. [Google Scholar] [CrossRef] [PubMed]
- Colombo, M.; Poggio, C.; Lasagna, A.; Chiesa, M.; Scribante, A. Vickers micro-hardness of new restorative CAD/CAM dental materials: Evaluation and comparison after exposure to acidic drink. Materials 2019, 12, 1246. [Google Scholar] [CrossRef] [PubMed]
- Alessandretti, R.; Borba, M.; Benetti, P.; Corazza, P.H.; Ribeiro, R.; Bona, A.D. Reliability and mode of failure of bonded monolithic and multilayer ceramics. Dent. Mater. 2017, 33, 191–197. [Google Scholar] [CrossRef]
- Tinastepe, N.; Malkondu, O.; Iscan, I.; Kazazoglu, E. Effect of home and over the contour bleaching on stainability of CAD/CAM esthetic restorative materials. J. Esthet. Restor. Dent. 2021, 33, 303–313. [Google Scholar] [CrossRef]
- Wang, F.; Takahashi, H.; Iwasaki, N. Translucency of dental ceramics with different thicknesses. J. Prosthet. Dent. 2013, 110, 14–20. [Google Scholar] [CrossRef]
- Liebermann, A.; Spintzyk, S.; Reymus, M.; Schweizer, E.; Stawarczyk, B. Nine prophylactic polishing pastes: Impact on discoloration, gloss, and surface properties of a CAD/CAM resin composite. Clin. Oral Investig. 2019, 23, 327–335. [Google Scholar] [CrossRef]
- Neme, A.L.; Frazier, K.B.; Roeder, L.B.; Debner, T.L. Effect of prophylactic polishing protocols on the surface roughness of esthetic restorative materials. Oper. Dent. 2002, 27, 50–58. [Google Scholar] [PubMed]
- Patil, S.S.; Rakhewar, P.S.; Limaye, P.S.; Chaudhari, N.P. A comparative evaluation of plaque-removing efficacy of air polishing and rubber-cup, bristle brush with paste polishing on oral hygiene status: A clinical study. J. Int. Soc. Prev. Community Dent. 2015, 5, 457–462. [Google Scholar] [CrossRef]
- Can Say, E.; Yurdagüven, H.; Malkondu, Ö.; Ünlü, N.; Soyman, M.; Kazazoğlu, E. The effect of prophylactic polishing pastes on surface roughness of indirect restorative materials. Sci. World J. 2014, 2014, 962764. [Google Scholar] [CrossRef]
- Lutz, F.; Sener, B.; Imfeld, T.; Barbakow, F.; Schüpbach, P. Self-adjusting abrasiveness: A new technology for prophylaxis pastes. Quintessence Int. 1993, 24, 53–63. [Google Scholar]
- Setcos, J.C.; Tarim, B.; Suzuki, S. Surface finish produced on resin composites by new polishing systems. Quintessence Int. 1999, 30, 169–173. [Google Scholar] [PubMed]
- Pecho, E.O.; Ghinea, R.; Alessandretti, R.; Pérez, M.M.; Bona, A.D. Visual and instrumental shade matching using CIELAB and CIEDE2000 color difference formulas. Dent. Mater. 2016, 32, 82–92. [Google Scholar] [CrossRef] [PubMed]
- Pérez, M.M.; Ghinea, R.; Rivas, M.J.; Yebra, A.; Ionescu, A.M.; Paravina, R.D.; Herrera, L.J. Development of a customized whiteness index for dentistry based on CIELAB color space. Dent. Mater. 2016, 32, 461–467. [Google Scholar] [CrossRef]
- Paravina, R.D.; Pérez, M.M.; Ghinea, R. Acceptability and perceptibility thresholds in dentistry: A comprehensive review of clinical and research applications. J. Esthet. Restor. Dent. 2019, 31, 103–112. [Google Scholar] [CrossRef]
- Yurdaguven, H.; Aykor, A.; Ozel, E.; Soyman, M. Influence of a prophylaxis paste on surface roughness of different composites, porcelain, enamel and dentin surfaces. Eur. J. Dent. 2012, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Fratolin, M.M.; Bianco, V.C.; Santos, M.J.; Rizkalla, A.S.; Santos, G.C., Jr. The effect of prophylactic powders on the surface roughness of enamel. Compend. Contin. Educ. Dent. 2014, 35, e31–e35. [Google Scholar]
- Monaco, C.; Arena, A.; Ozcan, M. Effect of prophylactic polishing pastes on roughness and translucency of lithium disilicate ceramic. Int. J. Periodontics Restor. Dent. 2014, 34, e26–e29. [Google Scholar] [CrossRef]
- Monaco, C.; Arena, A.; Scheda, L.; Fiore, D.A.; Zucchelli, G. In vitro 2D and 3D roughness and spectrophotometric and gloss analyses of ceramic materials after polishing with different prophylactic pastes. J. Prosthet. Dent. 2020, 124, 787.e1–787.e8. [Google Scholar] [CrossRef]
- Abu-Obaid, A.; AlMawash, A.; Alyabis, N.; Alzaaqi, N. An in vitro evaluation of the effect of polishing on the stainability of different CAD/CAM ceramic materials. Saudi Dent. J. 2020, 32, 135–141. [Google Scholar] [CrossRef]
- CIE. Colorimetry. Report No.: CIE Pub. No. 15; CIE Central Bureau: Vienna, Austria, 2004. [Google Scholar]
- Koller, M.; Arnetzl, G.V.; Holly, L.; Arnetzl, G. Lava ultimate resin nano ceramic for CAD/CAM: Customization case study. Int. J. Comput. Dent. 2012, 15, 159–164. [Google Scholar]
- Koizumi, H.; Saiki, O.; Nogawa, H.; Hiraba, H.; Okazaki, T.; Matsumura, H. Surface roughness and gloss of current CAD/CAM resin composites before and after toothbrush abrasion. Dent. Mater. J. 2015, 34, 881–887. [Google Scholar] [CrossRef]
- Kilinc, H.; Turgut, S. Optical behaviors of esthetic CAD-CAM restorations after different surface finishing and polishing procedures and UV aging: An in vitro study. J. Prosthet. Dent. 2017, 120, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Turker, S.B.; Biskin, T. The effect of bleaching agents on the microhardness of dental aesthetic restorative materials. J. Oral Rehabil. 2002, 29, 657–661. [Google Scholar] [CrossRef] [PubMed]
- Turker, S.B.; Biskin, T. Effect of three bleaching agents on the surface properties of three different esthetic restorative materials. J. Prosthet. Dent. 2003, 89, 466–473. [Google Scholar] [CrossRef] [PubMed]
- Bona, A.D.; Corazza, P.H.; Zhang, Y. Characterization of a polymer-infiltrated ceramic-network material. Dent. Mater. 2014, 30, 564–569. [Google Scholar] [CrossRef]
- Acar, O.; Yılmaz, B.; Altıntas, S.H.; Chandrasekaran, I.; Johnston, W.M. Color stainability of CAD/CAM and nanocomposite resin materials. J. Prosthet. Dent. 2016, 115, 71–75. [Google Scholar] [CrossRef]
- Barutçugil, B.; Bilgili, D.; Barutcigil, K.; Dündar, A.; Büyükkaplan, U.S.; Yılmaz, B. Discoloration and translucency changes of CAD-CAM materials after exposure to beverages. J. Prosthet. Dent. 2019, 122, 325–331. [Google Scholar] [CrossRef]
- Lawson, N.C.; Burgess, J.O. Gloss and stain resistance of ceramic-polymer CAD/CAM restorative blocks. J. Esthet. Restor. Dent. 2021, 28, 40–45. [Google Scholar] [CrossRef]
- Kanat-Ertürk, B. Color Stability of CAD/CAM Ceramics Prepared with Different Surface Finishing Procedures. J. Prosthodont. 2020, 29, 166–172. [Google Scholar] [CrossRef]
- Adawi, H.; Mialeem, M.; Ahmari, N.; Shariff, M.; Qahhar, M.; Muharraq, S.; Alghazali, N. Assessment of Color Stainability of Computer-Aided Design and Computer-Aided Manufacturing (CAD/CAM) Ceramic Materials After Hot and Cold Coffee Immersion at Different Time Intervals. Med. Sci. Monit. 2021, 27, e932745. [Google Scholar] [CrossRef]
- Covey, D.A.; Barnes, C.; Watanabe, H.; Johnson, W.W. Effects of pastefree prophylaxis polishing cup and various prophylaxis polishing pastes on tooth enamel and restorative materials. Gen. Dent. 2011, 59, 466–473. [Google Scholar] [PubMed]
- Kuzu, T.E.; Karatas, O. The effect of prophylaxis paste and air-powder polishing on color stability and surface roughness of different composite resins. J. Oral Res. Rev. 2023, 15, 34. [Google Scholar] [CrossRef]
- Kursoglu, P.; Motro, P.F.; Kazazoglu, E. Correlation of surface texture with the stainability of ceramics. J. Prosthet. Dent. 2014, 112, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Ghinea, R.; Pérez, M.M.; Herrera, L.J.; Rivas, M.J.; Yebra, A.; Paravina, R.D. Color difference thresholds in dental ceramics. J. Dent. 2010, 38, S57–S64. [Google Scholar] [CrossRef]
- Lee, Y.K. Comparison of CIELAB DeltaE* and CIEDE2000 color-differences after polymerization and thermocycling of resin composites. Dent. Mater. 2005, 21, 678–682. [Google Scholar] [CrossRef]
- Ertaş, M.; Yıldız, E.; Ünlü, E.; Aydın, S. The effect of coffee on the color stability of dental restorative materials. J. Dent. Mater. 2006, 22, 56–62. [Google Scholar]



| Material | Type | Chemical Content (Weight %) | Color | Particle Size | Manufacturer |
|---|---|---|---|---|---|
| Cerasmart 270 | Nanoceramic | Bis-MEPP, UDMA, DMA Silicon dioxide (SiO2), barium glass | A2 HT (High translucent) | GC Corp., Tokyo, Japan | |
| IPS Emax CAD | Lithium disilicate based glass-matrix ceramic | 58–80% SiO2, 11–19% Li2O, 0–13% K2O, 0–8% ZrO2, 0–5% Al2O3 | A2-HT | Ivoclar Vivadent | |
| Vita Enamic | Hybrid ceramic | 86% inorganic (58–63% SiO2, 20–23% Al2O3, 9–11% Na2O, 4–6% K2O, 0.1% ZrO2), 14% organic | 2M2-C-HT | VITA Zahnfabrik | |
| VITABLOCS Mark II for Cerec | Feldspathic glass-matrix ceramic | 56–64% SiO2, 20–23% Al2O3,6–9% Na2O, 6–8% K2O | 2M2-C | VITA Zahnfabrik, Bad Säckingen, Germany | |
| Cleanic | Prophylactic polishing paste (PPP) | Titanium dioxide, glycerine, sodium fluoride < 0.25%, ethanol < 1% | RDA 21 | Kerr, Rastatt, Germany | |
| CleanJoy | Prophylactic polishing paste (PPP) | Surfactant < 2.5%, peppermint flavor < 2.5%, natriumfluoride < 2.5% | Coarse RDA 195; Medium RDA 127; Fine RDA 16 | Voco, Cuxhaven, Germany | |
| Detartrine | Prophylactic polishing paste (PPP) | Quartz 25–50%, glycerine 10–25%, ethanol < 2.5%, zircon in silicate | RDA 150 | Septodont, Saint-Maur-des-Fosses, France | |
| Proxyt | Prophylactic polishing paste (PPP) | Water, glycerine 41.0; sorbite, xylit 21.0; inorganic fillers 35.0; excipients 1.2; natriumfluoride 0.12 | Coarse RDA 83; Medium RDA 36; Fine RDA 7 | Ivoclar Vivadent, Schaan, Liechtenstein |
| Material | Prophylactic Polishing Paste (PPP) | Code |
|---|---|---|
| VITABLOCS Mark II for Cerec | Cleanic | VM-CLE |
| VITABLOCS Mark II for Cerec | CleanJoy | VM-CLJ |
| VITABLOCS Mark II for Cerec | Detartrine | VM-DET |
| VITABLOCS Mark II for Cerec | Proxyt | VM-PXT |
| VITABLOCS Mark II for Cerec | Control | VM-C |
| IPS Emax CAD | Cleanic | E.MAX-CLE |
| IPS Emax CAD | CleanJoy | E.MAX-CLJ |
| IPS Emax CAD | Detartrine | E.MAX-DET |
| IPS Emax CAD | Proxyt | E.MAX-PXT |
| IPS Emax CAD | Control | E.MAX-C |
| Vita Enamic | Cleanic | VE-CLE |
| Vita Enamic | CleanJoy | VE-CLJ |
| Vita Enamic | Detartrine | VE-DET |
| Vita Enamic | Proxyt | VE- PXT |
| Vita Enamic | Control | VE-C |
| Cerasmart 270 | Cleanic | CS-CLE |
| Cerasmart 270 | CleanJoy | CS-CLJ |
| Cerasmart 270 | Detartrine | CS-DET |
| Cerasmart 270 | Proxyt | CS-PXT |
| Cerasmart 270 | Control | CS-C |
| ∆E*ab1 | Type III Sum of Squares | df | Mean Square | F | p |
|---|---|---|---|---|---|
| Material | 11,571 | 3 | 3857 | 24,944 | 0.001 * |
| Polishing Method | 21,624 | 4 | 5406 | 34,963 | 0.001 * |
| Material * Polishing | 21,345 | 12 | 1779 | 11,504 | 0.001 * |
| ∆E001 | Type III Sum of Squares | df | Mean Square | F | p |
|---|---|---|---|---|---|
| Material | 12,063 | 3 | 402 | 53,967 | 0.001 * |
| Polishing Method | 4659 | 4 | 1165 | 15,632 | 0.001 * |
| Material * Polishing | 11,203 | 12 | 0.934 | 12,530 | 0.001 * |
| ∆WID1 | Type III Sum of Squares | df | Mean Square | F | p |
|---|---|---|---|---|---|
| Material | 20,701 | 3 | 6900 | 11,744 | 0.001 * |
| Polishing Method | 35,265 | 4 | 8816 | 15,005 | 0.001 * |
| Material * Polishing | 26,110 | 12 | 2176 | 3703 | 0.001 * |
| ∆E*ab2 | Type III Sum of Squares | df | Mean Square | F | p |
|---|---|---|---|---|---|
| Material | 55,072 | 3 | 18,357 | 60,091 | 0.001 * |
| Polishing Method | 17,313 | 4 | 4328 | 14,168 | 0.001 * |
| Material * Polishing | 23,966 | 12 | 1997 | 6538 | 0.001 * |
| ∆E002 | Type III Sum of Squares | df | Mean Square | F | p |
|---|---|---|---|---|---|
| Material | 10,939 | 3 | 3646 | 38,540 | 0.001 * |
| Polishing Method | 4738 | 4 | 1185 | 12,521 | 0.001 * |
| Material * Polishing | 10,670 | 12 | 0.889 | 9398 | 0.001 * |
| ∆WID2 | Type III Sum of Squares | df | Mean Square | F | p |
|---|---|---|---|---|---|
| Material | 65,777 | 3 | 21,926 | 14,926 | 0.001 * |
| Polishing Method | 29,317 | 4 | 732 | 4989 | 0.001 * |
| Material * Polishing | 76,726 | 12 | 639 | 4353 | 0.001 * |
| ∆Ra | ||||||
|---|---|---|---|---|---|---|
| Cleanic | Cleanjoy | Detartrine | Proxyt | Control | p | |
| Material | Mean ± S D | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |
| Cerasmart | 0.021 ± 0.004 | 0.031 ± 0.002 | 0.049 ± 0.004 | 0.023 ± 0.003 | 0.001 ± 0.001 | 0.001 * |
| VitaEnamic | 0.003 ± 0.002 | 0.006 ± 0.002 | 0.005 ± 0.002 | 0.006 ± 0.002 | 0 ± 0.001 | 0.001 * |
| Vita Mark 2 | 0.005 ± 0.002 | 0.008 ± 0.005 | 0.006 ± 0.001 | 0.009 ± 0.003 | 0.001 ± 0.001 | 0.002 * |
| E.Max | 0.003 ± 0.002 | 0.007 ± 0.001 | 0.010 ± 0.003 | 0.010 ± 0.002 | 0 ± 0 | 0.001 * |
| p | 0.001 * | 0.001 * | 0.001 * | 0.001 * | 0.412 | |
| ∆Ra | Type III Sum of Squares | df | Mean Square | F | p |
|---|---|---|---|---|---|
| Material | 0.007 | 3 | 0.002 | 415,948 | 0.001 * |
| Polishing Method | 0.004 | 4 | 0.001 | 146,690 | 0.001 * |
| Material * Polishing | 0.003 | 12 | 0 | 48,215 | 0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arkan, B.; Iscan, I.; Tinastepe, N. The Impact of Prophylactic Polishing Pastes on the Surface Roughness, Color, and Stain Resistance of CAD/CAM Restorative Materials. Dent. J. 2025, 13, 212. https://doi.org/10.3390/dj13050212
Arkan B, Iscan I, Tinastepe N. The Impact of Prophylactic Polishing Pastes on the Surface Roughness, Color, and Stain Resistance of CAD/CAM Restorative Materials. Dentistry Journal. 2025; 13(5):212. https://doi.org/10.3390/dj13050212
Chicago/Turabian StyleArkan, Betul, Ipek Iscan, and Neslihan Tinastepe. 2025. "The Impact of Prophylactic Polishing Pastes on the Surface Roughness, Color, and Stain Resistance of CAD/CAM Restorative Materials" Dentistry Journal 13, no. 5: 212. https://doi.org/10.3390/dj13050212
APA StyleArkan, B., Iscan, I., & Tinastepe, N. (2025). The Impact of Prophylactic Polishing Pastes on the Surface Roughness, Color, and Stain Resistance of CAD/CAM Restorative Materials. Dentistry Journal, 13(5), 212. https://doi.org/10.3390/dj13050212





