Immediate Loading of Implants-Supported Fixed Partial Prostheses in Posterior Regions: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Quality Assessment
2.3. Data Extraction
3. Results
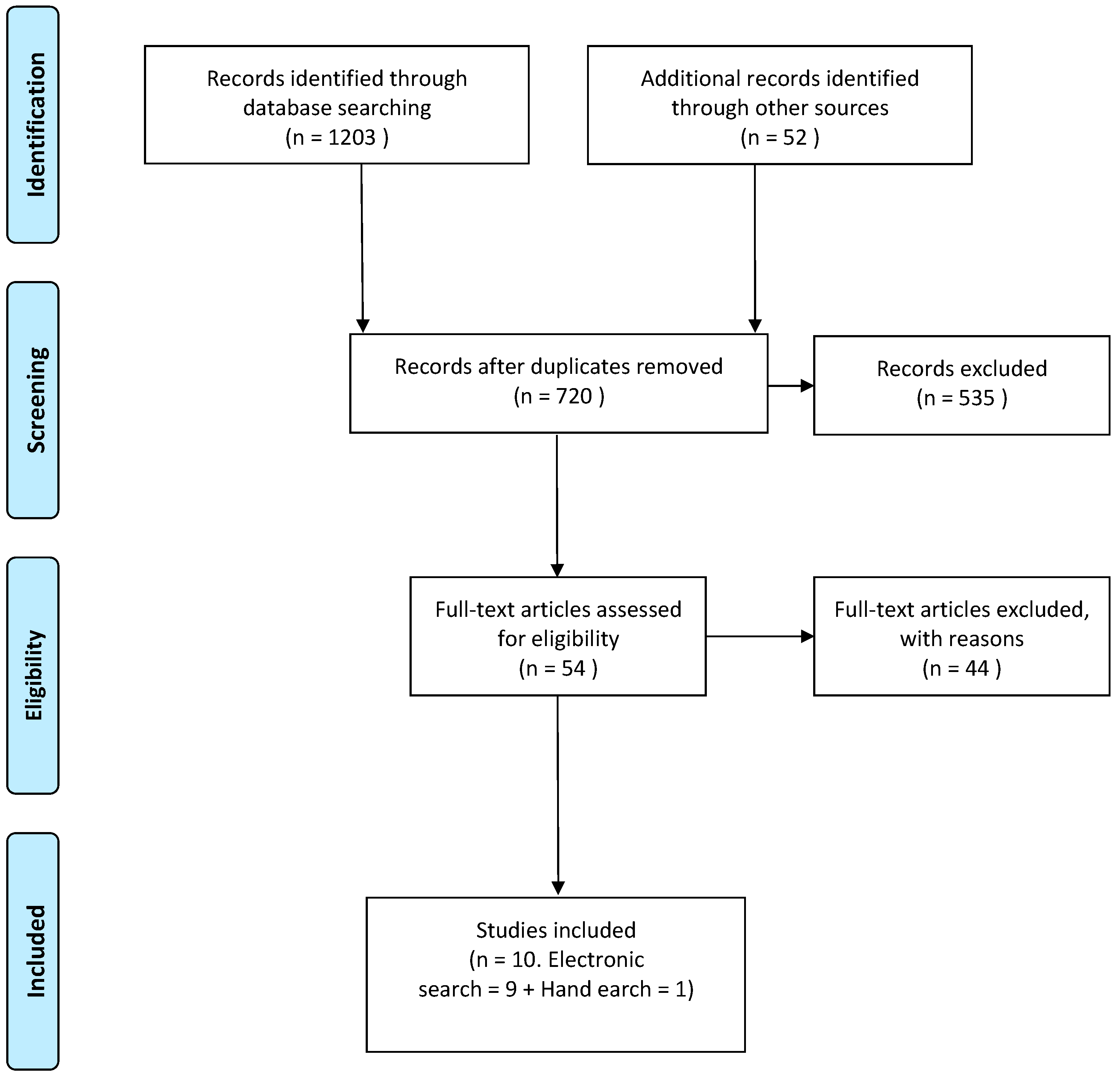
3.1. Study Selection
3.2. Risk of Bias
3.3. Data Synthesis
3.4. Incidence of Complications
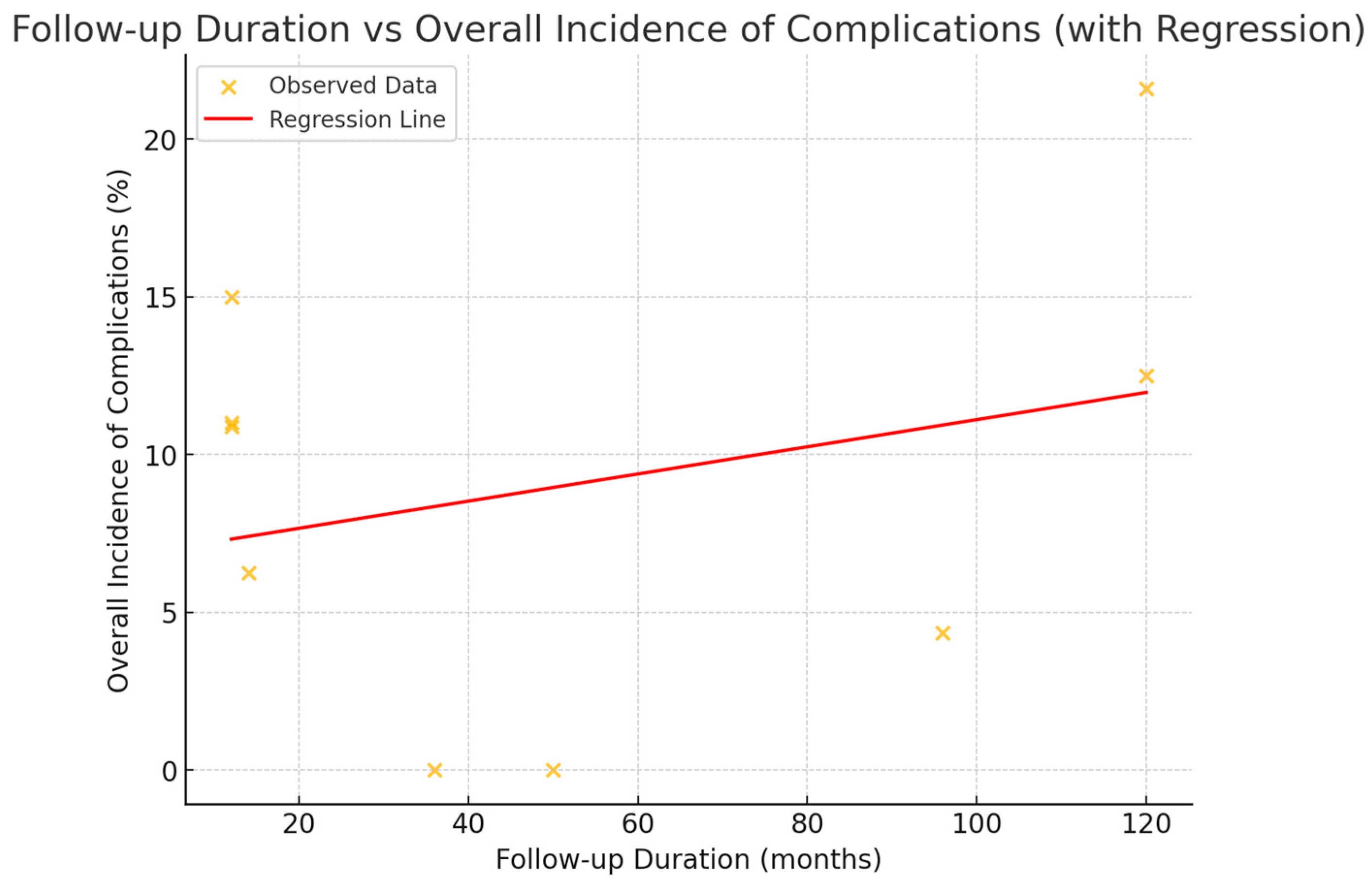
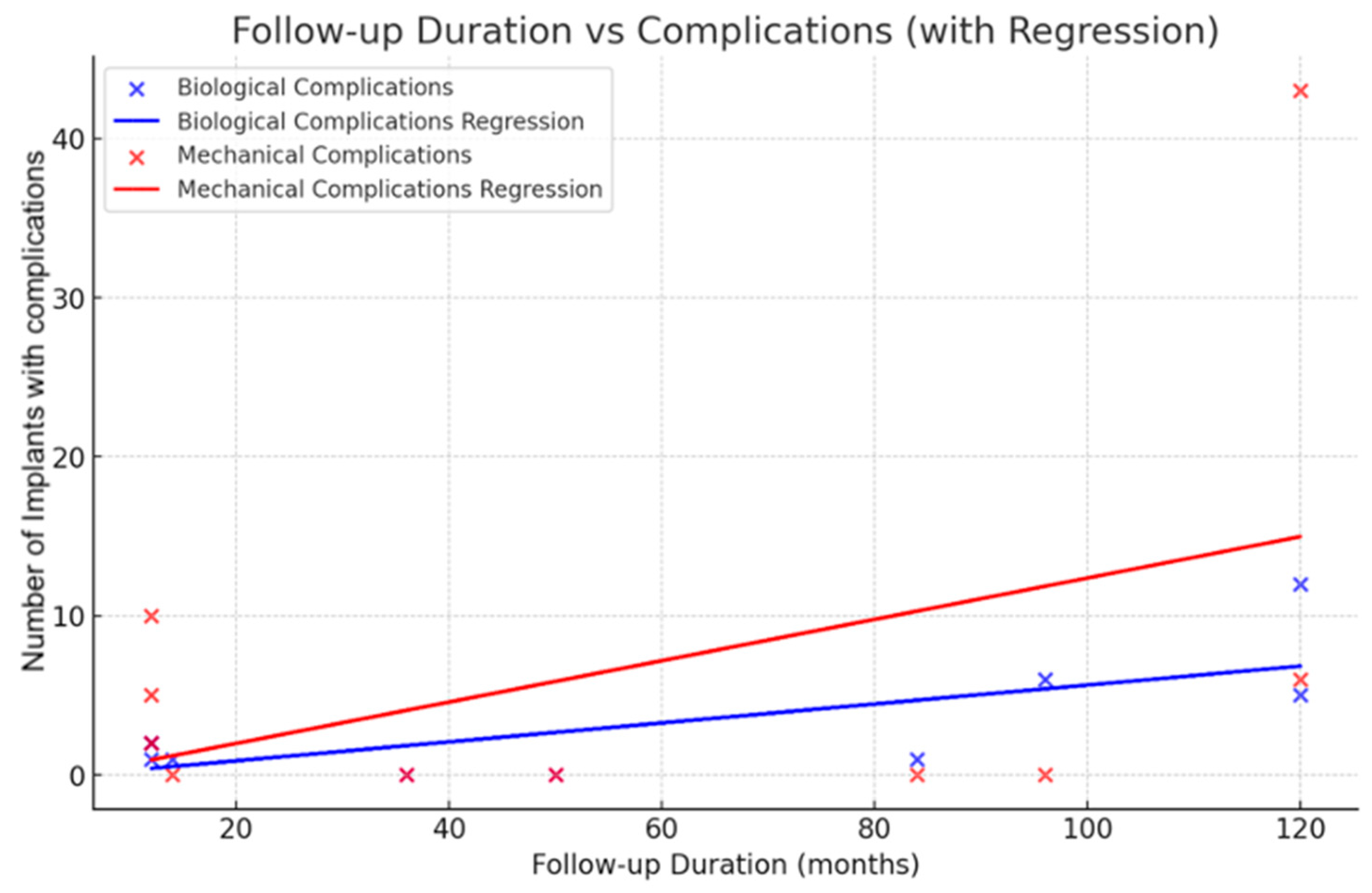
3.5. Analysis of Complications Based on Follow-Up Duration
- Slope (0.0595): For each additional month of follow-up, the rate of biological complications increases by approximately 0.0595. This indicates a gradual rise in complications over time, reflecting a steady accumulation of biological challenges.
- Intercept (−0.309): At 0 months of follow-up, the theoretical baseline level of biological complications is nearly negligible (−0.309), suggesting minimal initial complications at the start of observation.
- R2 (0.522): The R2 value of 0.522 indicates that 52.2% of the variability found in biological complications is explained by the duration of follow-up. This suggests a relationship between the duration of follow-up and the incidence of biological complications.
- Slope (0.1299): The mechanical complications show a steeper increase than the biological ones, with a slope of 0.1299 for each additional month of follow-up. This shows that the rate of increase in incidence with time is higher for mechanical issues.
- Intercept (−0.624): At the initial follow-up period of 0 months, the predicted baseline rate of mechanical complications is almost negligible (−0.624), showing a very low prevalence of mechanical issues at that time.
- The R2 value of 0.199 indicates that the follow-up duration explains only 19.9% of the variation seen in mechanical complications. This result implies that other factors, other than the follow-up duration, have significant effects on the development of mechanical complications.
3.6. Primary Stability
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Romandini, M.; Ruales-Carrera, E.; Sadilina, S.; Hämmerle, C.H.F.; Sanz, M. Minimal invasiveness at dental implant placement: A systematic review with meta-analyses on flapless fully guided surgery. Periodontology 2000 2023, 91, 89–112. [Google Scholar] [CrossRef] [PubMed]
- Nicolescu, M.I. Regenerative Perspective in Modern Dentistry. Dent. J. 2016, 4, 10. [Google Scholar] [CrossRef] [PubMed]
- Al-Sawai, A.A.; Labib, H. Success of immediate loading implants compared to conventionally-loaded implants: A literature review. J. Investig. Clin. Dent. 2016, 7, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; He, F.; Zhao, Y.; Sun, Q.; Xia, H.; Xia, D.; Bai, Y. Immediate Versus Non-immediate Loading Protocols for Reduced-Diameter Implants Supporting Overdentures: A Systematic Review and Meta-analysis. Int. J. Oral Maxillofac. Implant 2024, 39, 657–664. [Google Scholar] [CrossRef]
- Chen, J.; Cai, M.; Yang, J.; Aldhohrah, T.; Wang, Y. Immediate versus early or conventional loading dental implants with fixed prostheses: A systematic review and meta-analysis of randomized controlled clinical trials. J. Prosthet. Dent. 2019, 122, 516–536. [Google Scholar] [CrossRef]
- Javed, F.; Romanos, G.E. The role of primary stability for successful immediate loading of dental implants. A literature review. J. Dent. 2010, 38, 612–620. [Google Scholar] [CrossRef]
- Pitman, J.; Seyssens, L.; Christiaens, V.; Cosyn, J. Immediate implant placement with or without immediate provisionalization: A systematic review and meta-analysis. J. Clin. Periodontol. 2022, 49, 1012–1023. [Google Scholar] [CrossRef]
- Sadilina, S.; Park, S.H.; Chantler, J.; Park, J.Y.; Thoma, D.; Cha, J.K.; Strauss, F.J. Immediate loading of definitive restorations in partially edentulous patients requiring an implant-supported prosthesis: A scoping review. J. Prosthet. Dent. 2024; in press. [Google Scholar] [CrossRef]
- Hamilton, A.; Gonzaga, L.; Amorim, K.; Wittneben, J.G.; Martig, L.; Morton, D.; Martin, W.; Gallucci, G.O.; Wismeijer, D. Selection criteria for immediate implant placement and immediate loading for single tooth replacement in the maxillary esthetic zone: A systematic review and meta-analysis. Clin. Oral Implant Res. 2023, 34 (Suppl. S26), 304–348. [Google Scholar] [CrossRef] [PubMed]
- La Monaca, G.; Pranno, N.; Annibali, S.; Di Carlo, S.; Pompa, G.; Cristalli, M.P. Immediate flapless full-arch rehabilitation of edentulous jaws on 4 or 6 implants according to the prosthetic-driven planning and guided implant surgery: A retrospective study on clinical and radiographic outcomes up to 10 years of follow-up. Clin. Implant Dent Relat. Res. 2022, 24, 831–844. [Google Scholar] [CrossRef]
- Norré, D.; Att, W. STAR concept: A technique to improve the predictability of immediate implant placement and loading in edentulous arches. Int. J. Comput. Dent. 2022, 25, 303–323. [Google Scholar] [CrossRef]
- Tirone, F.; Salzano, S.; Rolando, E.; Pozzatti, L.; Rodi, D. Framework Fracture of Zirconia Supported Full Arch Implant Rehabilitation: A Retrospective Evaluation of Cantilever Length and Distal Cross-Sectional Connection Area in 140 Patients Over an Up-To-7 Year Follow-Up Period. J. Prosthodont. 2022, 31, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Methley, A.M.; Campbell, S.; Chew-Graham, C.; McNally, R.; Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv. Res. 2014, 14, 579. [Google Scholar] [CrossRef]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef]
- Schünemann, H.J.; Cuello, C.; Akl, E.A.; Mustafa, R.A.; Meerpohl, J.J.; Thayer, K.; Morgan, R.L.; Gartlehner, G.; Kunz, R.; Katikireddi, S.V.; et al. GRAD Eguidelines: 18 How ROBINS-I, other tools to assess risk of bias in nonrandomized studies should be used to rate the certainty of a body of evidence. J. Clin. Epidemiol. 2019, 111, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Minozzi, S.; Cinquini, M.; Gianola, S.; Gonzalez-Lorenzo, M.; Banzi, R. The revised Cochrane risk of bias tool for randomized trials (RoB 2) showed low interrater reliability and challenges in its application. J. Clin. Epidemiol. 2020, 126, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Perelli, M.; Abundo, R.; Corrente, G.; Saccone, C.; Sarmiento, H.; Chang, Y.C.; Fiorellini, J.P. The Long-Term Evaluation of Two-Unit Fixed Partial Dentures on Short, Threaded Implants: Delayed Versus Immediate Loading. Int. J. Periodontics Restor. Dent. 2020, 40, e157–e162. [Google Scholar] [CrossRef]
- Anitua, E.; Flores, C.; Flores, J.; Alkhraisat, M.H. Clinical Effectiveness of 6.5-mm-Long Implants to Support Two-Implant Fixed Prostheses in Premolar-Molar Region: The Influence of Immediate Loading and the Length of Splinting Implant. J. Prosthodont. 2019, 28, e688–e693. [Google Scholar] [CrossRef]
- Maló, P.; de Araújo Nobre, M.; Lopes, A.; Queridinha, B.; Ferro, A.; Gravito, I. Axial Implants in Immediate Function for Partial Rehabilitation in the Maxilla and Mandible: A Retrospective Clinical Study Evaluating the Long-Term Outcome (Up to 10 Years). Implant. Dent. 2015, 24, 557–564. [Google Scholar] [CrossRef]
- Cesaretti, G.; Botticelli, D.; Renzi, A.; Rossi, M.; Rossi, R.; Lang, N.P. Radiographic evaluation of immediately loaded implants supporting 2-3 units fixed bridges in the posterior maxilla: A 3-year follow-up prospective randomized controlled multicenter clinical study. Clin. Oral Implant Res. 2016, 27, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Weerapong, K.; Sirimongkolwattana, S.; Sastraruji, T.; Khongkhunthian, P. Comparative study of immediate loading on short dental implants and conventional dental implants in the posterior mandible: A randomized clinical trial. Int. J. Oral Maxillofac. Implant 2019, 34, 141–149. [Google Scholar] [CrossRef]
- Agliardi, E.L.; Tetè, S.; Romeo, D.; Malchiodi, L.; Gherlone, E. Immediate function of partial fixed rehabilitation with axial and tilted implants having intrasinus insertion. J. Craniofac. Surg. 2014, 25, 851–855. [Google Scholar] [CrossRef] [PubMed]
- Amato, F.; Spedicato, G.A. Immediate Loading of 3-Unit Posterior Fixed Dental Prostheses on 3 Vs 2 Implants, Comparison and Evaluation with up to 10-Year Follow-up. Int. J. Prosthodont. 2025, 25, 175–184. [Google Scholar] [CrossRef]
- Daher, F.I.; Abi-Aad, H.L.; Dimassi, H.I.; Cordioli, G.; Majzoub, Z.A.K. Immediate versus conventional loading of variable-thread tapered implants supporting three- to four-unit fixed partial dentures in the posterior maxilla: 3-year results of a split-mouth randomised controlled trial. Int. J. Oral Implant. 2019, 12, 449–466. [Google Scholar] [PubMed]
- Esposito, M.; Grufferty, B.; Papavasiliou, G.; Dominiak, M.; Xhanari, E.; Buti, J.; Heinemann, F. Immediate loading of occluding definitive partial fixed prostheses versus nonoccluding provisional prostheses: 10-year post-loading results from a multicentre randomized controlled trial. Clin. Trials. Dent. 2023, 5, 2–16. [Google Scholar] [CrossRef]
- Kim, Y.Y.; Song, Y.W.; Kim, M.J.; Cha, J.K.; Park, J.M.; Kim, J.H.; Jung, U.W. Immediate loading of fixed partial prostheses reconstructed using either tapered or straight implants in the posterior area: A randomized clinical trial. Clin. Implant Dent. Relat. Res. 2021, 23, 703–715. [Google Scholar] [CrossRef]
- Cappare, P.; Sannino, G.; Minoli, M.; Montemezzi, P.; Ferrini, F. Conventional versus Digital Impressions for Full Arch Screw-Retained Maxillary Rehabilitations: A Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2019, 16, 829. [Google Scholar] [CrossRef]
- Pardal-Peláez, B.; Flores-Fraile, J.; Pardal-Refoyo, J.L.; Montero, J. Implant loss and crestal bone loss in early loading versus delayed and immediate loading in edentulous mandibles. A systematic review and meta-analysis. J. Clin. Exp. Dent. 2021, 13, e397–e405. [Google Scholar] [CrossRef]
- Yari, A.; Fasih, P.; Alborzi, S.; Nikzad, H.; Romoozi, E. Risk factors associated with early implant failure: A retrospective review. J. Stomatol. Oral Maxillofac. Surg. 2024, 125, 101749. [Google Scholar] [CrossRef]
- Corsalini, M.; Di Venere, D.; Stefanachi, G.; Muci, G.; Palminteri, A.; Laforgia, A.; Pettini, F. Maxillary Overdenture Retained with an Implant Support CAD-CAM Bar: A 4 Years Follow Up Case. Open Dent. J. 2017, 11, 247–256. [Google Scholar] [CrossRef] [PubMed]
- D’Albis, G.; D’Albis, V.; Susca, B.; Palma, M.; Al Krenawi, N. Implant-supported zirconia fixed partial dentures cantilevered in the lateral-posterior area: A 4-year clinical results. J. Dent. Res. Dent. Clin. Dent. Prospects. 2022, 16, 258–263. [Google Scholar] [CrossRef]
- Corsalini, M.; D’Agostino, S.; Favia, G.; Dolci, M.; Tempesta, A.; Di Venere, D.; Limongelli, L.; Capodiferro, S. A Minimally Invasive Technique for Short Spiral Implant Insertion with Contextual Crestal Sinus Lifting in the Atrophic Maxilla: A Preliminary Report. Healthcare 2020, 9, 11. [Google Scholar] [CrossRef]
- Rameh, S.; Menhall, A.; Younes, R. Key factors influencing short implant success. Oral Maxillofac. Surg. 2020, 24, 263–275. [Google Scholar] [CrossRef]
- Altaib, F.H.; Alqutaibi, A.Y.; Al-Fahd, A.; Eid, S. Short dental implant as alternative to long implant with bone augmentation of the atrophic posterior ridge: A systematic review and meta-analysis of RCTs. Quintessence Int. 2019, 50, 636–650. [Google Scholar] [CrossRef]
- Schwartz, S.R. Short implants: Are they a viable option in implant dentistry? Dent. Clin. N. Am. 2015, 59, 317–328. [Google Scholar] [CrossRef]
- Huang, Y.C.; Huang, Y.C.; Ding, S.J. Primary stability of implant placement and loading related to dental implant materials and designs: A literature review. J. Dent. Sci. 2023, 18, 1467–1476. [Google Scholar] [CrossRef]
- Bergamo, E.T.P.; Zahoui, A.; Barrera, R.B.; Huwais, S.; Coelho, P.G.; Karateew, E.D.; Bonfante, E.A. Osseodensification effect on implants primary and secondary stability: Multicenter controlled clinical trial. Clin. Implant Dent. Relat. Res. 2021, 23, 317–328. [Google Scholar] [CrossRef]
- Akhlaghi, P.; Khorshidparast, S.; Rouhi, G. Investigation on primary stability of dental implants through considering peri-implant bone damage, caused by small and large deformations: A validated non-linear micro finite element study. J. Mech. Behav. Biomed. Mater. 2023, 146, 106062. [Google Scholar] [CrossRef] [PubMed]
- Ruales-Carrera, E.; Pauletto, P.; Apaza-Bedoya, K.; Volpato, C.A.M.; Özcan, M.; Benfatti, C.A.M. Peri-implant tissue management after immediate implant placement using a customized healing abutment. J. Esthet. Restor. Dent. 2019, 31, 533–541. [Google Scholar] [CrossRef]
- Ghoul, W.E.; Chidiac, J.J. Prosthetic requirements for immediate implant loading: A review. J. Prosthodont. 2012, 21, 141–154. [Google Scholar] [CrossRef]
- Ribeiro, A.K.C.; Costa, R.T.F.; Vasconcelos, B.C.D.E.; de Moraes, S.L.D.; Carreiro, A.D.F.P.; Pellizzer, E.P. Patient-reported outcome measures and prosthetic events in implant-supported mandibular overdenture patients after immediate versus delayed loading: A systematic review and meta-analysis. J. Prosthet. Dent. 2024, 131, 833–840. [Google Scholar] [CrossRef]
- Nkenke, E.; Fenner, M. Indications for immediate loading of implants and implant success. Clin. Oral Implant Res. 2006, 17 (Suppl. S2), 19–34. [Google Scholar] [CrossRef]
- Delben, J.A.; Goiato, M.C.; Pellizzer, E.P.; Magro Filho, O. Planning for immediate loading of implant-supported prostheses: Literature review. J. Oral Implant 2012, 38, 504–508. [Google Scholar] [CrossRef]
- Buser, D.; Sennerby, L.; De Bruyn, H. Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontology 2000 2017, 73, 7–21. [Google Scholar] [CrossRef]
- Gamborena, I.; Sasaki, Y.; Blatz, M.B. Predictable immediate implant placement and restoration in the esthetic zone. J. Esthet. Restor. Dent. 2021, 33, 158–172. [Google Scholar] [CrossRef]
- Pesce, P.; Pera, F.; Setti, P.; Menini, M. Precision and Accuracy of a Digital Impression Scanner in Full-Arch Implant Rehabilitation. Int. J. Prosthodont. 2018, 31, 171–175. [Google Scholar] [CrossRef]
- Morton, D.; Gallucci, G.; Lin, W.S.; Pjetursson, B.; Polido, W.; Roehling, S.; Sailer, I.; Aghaloo, T.; Albera, H.; Bohner, L.; et al. Group 2 ITI Consensus Report: Prosthodontics and implant dentistry. Clin. Oral Implant Res. 2018, 29 (Suppl. S16), 215–223. [Google Scholar] [CrossRef]
- Uesugi, T.; Shimoo, Y.; Munakata, M.; Sato, D.; Yamaguchi, K.; Fujimaki, M.; Nakayama, K.; Watanabe, T.; Malo, P. The All-on-four concept for fixed full-arch rehabilitation of the edentulous maxilla and mandible: A longitudinal study in Japanese patients with 3–17-year follow-up and analysis of risk factors for survival rate. Int. J. Implant Dent. 2023, 9, 43. [Google Scholar] [CrossRef]
- Schwarz, F.; Ramanauskaite, A. It is all about peri-implant tissue health. Periodontology 2000 2022, 88, 9–12. [Google Scholar] [CrossRef]
- Chiam, S.Y.; Liu, H.P.; Oh, W.S. Mechanical and biological complications of angled versus straight screw channel implant-supported prostheses: A systematic review and meta-analysis. J. Prosthet. Dent. 2024; in press. [Google Scholar] [CrossRef]
- Benic, G.I.; Mir-Mari, J.; Hämmerle, C.H. Loading protocols for single-implant crowns: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Implant 2014, 29 (Suppl. S38), 222. [Google Scholar] [CrossRef]
- Macrì, M.; D’Albis, V.; D’Albis, G.; Forte, M.; Capodiferro, S.; Favia, G.; Alrashadah, A.O.; García, V.D.; Festa, F. The Role and Applications of Artificial Intelligence in Dental Implant Planning: A Systematic Review. Bioengineering 2024, 11, 778. [Google Scholar] [CrossRef]
- Davies, S.J. Occlusal considerations in implantology: Good occlusal practice in implantology. Dent. Update 2010, 37, 619–620. [Google Scholar] [CrossRef]
- Bertolini, M.M.; Del Bel Cury, A.A.; Pizzoloto, L.; Acapa, I.R.H.; Shibli, J.A.; Bordin, D. Does traumatic occlusal forces lead to peri-implant bone loss? A systematic review. Braz. Oral Res. 2019, 33 (Suppl. S1), e069. [Google Scholar] [CrossRef]
- Debortoli, C.; Afota, F.; Latreche, S.; Zammillo, F.; Boujenah, O.; Savoldelli, C. Stackable guide in implantology: A technical note. J. Stomatol. Oral Maxillofac. Surg. 2023, 124, 101459. [Google Scholar] [CrossRef]
- Khan, M.W.; Inayat, N.; Zafar, M.S.; Zaigham, A.M. A resonance frequency analysis to investigate the impact of implant size on primary and secondary stability. Pak. J. Med. Sci. 2024, 40, 1261–1266. [Google Scholar] [CrossRef]
- Huang, H.; Wu, G.; Hunziker, E. The clinical significance of implant stability quotient (ISQ) measurements: A literature review. J. Oral Biol. Craniofac. Res. 2020, 10, 629–638. [Google Scholar] [CrossRef]
- Salian, S.S.; Subhadarsanee, C.P.; Patil, R.T.; Dhadse, P.V. Radiographic Evaluation in Implant Patients: A Review. Cureus 2024, 16, e54783. [Google Scholar] [CrossRef]
| Focused Question (PICO) | What is the Current Knowledge about Immediate Loading Implants in the Posterior Region of Fixed Partial Prosthesis? | |
|---|---|---|
| Search | Strategy | Partially edentulous patients in the posterior regions, in the mandible or maxilla. |
| Population | ||
| Intervention or Exposure | Placement of implants and simultaneous positioning of the provisional prosthesis. | |
| Comparison | Implant rehabilitations of partially edentulous regions without immediate prosthesis. | |
| Outcome | Survival rate, complication rate. | |
| Database Electronic search | PubMed Medline, Web of Science databases, manual search. | |
| Journals | Periodontology 2000, Clinical Advances in Periodontics, Dentistry Journal of Oral Pathology and Medicine, Journal of Clinical Periodontology, Frontiers in Oral Health, International Journal of Periodontics and Restorative Dentistry, Lasers in Dental Science, Journal of Periodontal Research. | |
| Selection criteria | Inclusion criteria | Studies at all levels of evidence, except expert opinion; articles published in English; articles published in the last 10 years. |
| Exclusion criteria | Review articles, animal studies, in vitro studies. Multiple publications on the same patient population. Letters to editors. Full text not available/accessible. | |
| D1 | D2 | D3 | D4 | D5 | Overall | |
|---|---|---|---|---|---|---|
| Cesaretti G. (2015) [21] |  |  |  |  |  |  |
| Weerapong K. et al. (2019) [22] |  |  |  |  |  |  |
| Daher FI et al. (2020) [25] |  |  |  |  |  |  |
| Esposito et al. (2024) [26] |  |  |  |  |  |  |
| Kim YY et al. (2021) [27] |  |  |  |  |  |  |
 Some concerns;
Some concerns;  Low.
Low.| D1 | D2 | D3 | D4 | D5 | D6 | D7 | Overall | |
|---|---|---|---|---|---|---|---|---|
| Perelli M. et al. (2020) [18] |  |  |  |  |  |  |  |  |
| Anitua E. et al. (2019) [19] |  |  |  |  |  |  |  |  |
| Maló P. et al. (2015) [20] |  |  |  |  |  |  |  |  |
| Agliardi et al. (2014) [23] |  |  |  |  |  |  |  |  |
| Amato F. et al. (2024) [24] |  |  |  |  |  |  |  |  |
 Some concerns;
Some concerns;  Low.
Low.| Reference, Year, Country | Study Design | N° Implants | Implant Type | Prosthesis Haracteristics | Implant Lost |
|---|---|---|---|---|---|
| Perelli M. et al. (2020) [18] Italy | Prospective study | Max: 46 Mand: 23 | Short, cylindrical, threaded implants, 7.0 mm or 8.5 mm in length. | Provisional: Acrylic resin, screw-retained. Definitive: Metal–ceramic materials screw-retained and cement-retained. | 6 implants lost in maxillary region |
| Anitua E. et al. (2019) [19] Spain | Retrospective clinical study | 48 | Extra-short implants (6.5 mm) by BTI Biotechnology Institute, Vitoria, Spain. | Provisional: Acrylic resin, screw-retained. Definitive: Metal–ceramic materials, screw-retained. | - |
| Maló P et al. (2015) [20] Portugal | Retrospective Clinical Study | Max: 215 Mand: 266 | Cylindrical, 7–15 mm length, TiUnite surface, immediate function protocol. | Provisional: Acrylic resin screw-retained Definitive: Metal–ceramic materials, screw-retained. | Maxilla: 6 lost— Mandible: 2 lost. |
| Cesaretti G. (2015) [21] Cuba | Randomized controlled multicenter clinical trial. | Max: 71 | Straumann SLA, 4.1 mm diameter, 8–12 mm length. | Provisional: Acrylic resin, screw-retained. Definitive: Metal–ceramic materials, screw-retained. | - |
| Weerapong K. Et al. (2019) [22] Thailand | Randomized clinical trial | Mand: 46 | PW+ Implant, 6–10 mm. | Provisional Prosthesis: Hybrid ceramic, fabricated using CAD/CAM technology, screw-retained. Definitive Prosthesis: Not specified | 2 short, 1 standard implant lost. |
| Agliardi et al. (2014) [23] Italy | Prospective Clinical Study | Max: 20 | NobelSpeedy Groovy (Nobel Biocare), axial and tilted, 11.5–25 mm length, TiUnite surface. | Provisional: Acrylic resin, screw-retained. Definitive: CAD/CAM framework with titanium and acrylic teeth, screw-retained. | - |
| Amato F. et al. (2024) [24] Italy | Prospective study | Max: 128 Mand: 50 | - | Provisional: Acrylic resin, screw-retained. Definitive: Not specified | One implant failure. |
| Daher FI et al. (2020) [25] Lebanon | Split-mouth randomized controlled trial. | Max:120 | NobelActive implants (Nobel Biocare), variable-thread tapered, 10–15 mm length, dual acid-etched. | Provisional: Acrylic resin, screw-retained. Definitive: Metal–ceramic materials, screw-retained. | - |
| Esposito et al. (2024) [26] Italy | Multicenter randomized controlled trial | 72 implants: 34 occlusion, 38 non-occlusion | T3 Certain Tapered Prevail implants (ZimVie Dental), dual acid-etched, 8.5–13 mm length. | Provisional: Acrylic resin, screw-retained. Definitive: Metal–ceramic materials, screw-retained. | 2 implants lost (occlusion group), 0 lost (non-occlusion group) |
| Kim YY et al. (2021) [27] South Korea | Randomized clinical trial | Max: 46 Mand: 56 | Tapered implants (TI) (Luna, Shinhung) and Straight implants (SI) (Straumann Bone Level), SLA surface, 8–10 mm length. | Provisional: Polymethyl methacrylate (PMMA), screw-retained. Definitive: Metal–ceramic or zirconia-based materials, likely screw-retained or cement-retained. | 2 TI, 7 SI implants lost |
| Reference, Year, Country | N° of Implants | Follow-Up Duration | Biological Complications | Mechanical Complications | Survival Rate % | Complications (%) |
|---|---|---|---|---|---|---|
| Perelli M. et al. (2020) [18] Italy | 69 | 8 years | 6 maxillary implants failed during first year | No prosthetic failures over 8 years | 95.6% | 4.34% |
| Anitua E. et al. (2019) [19] Spain | 48 | 14 months | Higher bone loss in short-long splinted group | No prosthetic failures; distal bone loss higher | 100% | 6.25% |
| Maló P et al. (2015) [20] Portugal | 481 | 10 years | 12 biological complications; peri-implantitis | 43 mechanical complications | 96.7% | 21.6% |
| Cesaretti G. (2015) [21] Cuba | 71 | 3 years | No biological complications | No mechanical complications | 100% | 0% |
| Weerapong K. Et al. (2019) [22] Thailand | 46 | 1 year | 2 short implants failed (early failure) | Crown fractures: 3 short, 2 conventional | 91.3% (short), 95.7% (standard) | 10.87% |
| Agliardi et al. (2014) [23]. Italy | 20 | 50 months | No biological complications | None reported | 100% | 0% |
| Amato F. et al. (2024) [24] Italy | 178 | 6 to 10 years (mean 7 years) | 1 implant failure in group 1 | None reported | 99.5% | 0,56% |
| Daher FI et al. (2020) [25] Lebanon | 120 | 12 months | Higher bone loss in second molars; peri-implantitis | Mechanical failures in prosthesis connections | 100% | 15% |
| Esposito et al. (2024) [26] Italy | 72 | 10 years | 5 peri-implantitis cases in occlusion group | Prosthetic fractures and detachment | Non-Occlusion group, 100%. Occlusion group 94.12% | 12.5% |
| Kim YY et al. (2021) [27] South Korea | 102 | 12 months | 2 infections in GBR sites; peri-implantitis (1 case) | Prosthesis fractures (4 in TI, 6 in SI groups) | TI: 96.2%, SI: 86.0% | 11% |
| Reference, Year, Country | Primary Stability Measurement |
|---|---|
| Perelli M. et al. (2020) [18] Italy | Insertion Torque: 47.12 ± 6.37 Ncm (Tapered); 41.60 ± 9.77 Ncm (Straight) |
| Anitua E. et al. (2019) [19] Spain | ISQ values monitored (Osstell Mentor) |
| Maló P et al. (2015) [20] Portugal | Insertion Torque > 30 Ncm required for immediate loading |
| Cesaretti G. (2015) [21] Cuba | Resonance Frequency Analysis (RFA), ISQ values > 70 |
| Weerapong K. Et al. (2019) [22] Thailand | Manual Torque Wrenches, thresholds not reported |
| Agliardi et al. (2014) [23] Italy | Insertion Torque ≥ 35 Ncm (Threshold for stability) |
| Amato F. et al. (2024) [24] Italy | Insertion Torque recorded, values not disclosed |
| Daher FI et al. (2020) [25] Lebanon | ISQ measurements tracked at 3, 6, and 12 months |
| Esposito et al. (2024) [26] Italy | Insertion Torque: range 30–50 Ncm |
| Kim YY et al. (2021) [27] Republic of Korea | No explicit mention of primary stability |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
D’Albis, G.; Forte, M.; Alrashadah, A.O.; Marini, L.; Corsalini, M.; Pilloni, A.; Capodiferro, S. Immediate Loading of Implants-Supported Fixed Partial Prostheses in Posterior Regions: A Systematic Review. Dent. J. 2025, 13, 213. https://doi.org/10.3390/dj13050213
D’Albis G, Forte M, Alrashadah AO, Marini L, Corsalini M, Pilloni A, Capodiferro S. Immediate Loading of Implants-Supported Fixed Partial Prostheses in Posterior Regions: A Systematic Review. Dentistry Journal. 2025; 13(5):213. https://doi.org/10.3390/dj13050213
Chicago/Turabian StyleD’Albis, Giuseppe, Marta Forte, Abdulrahman Omar Alrashadah, Lorenzo Marini, Massimo Corsalini, Andrea Pilloni, and Saverio Capodiferro. 2025. "Immediate Loading of Implants-Supported Fixed Partial Prostheses in Posterior Regions: A Systematic Review" Dentistry Journal 13, no. 5: 213. https://doi.org/10.3390/dj13050213
APA StyleD’Albis, G., Forte, M., Alrashadah, A. O., Marini, L., Corsalini, M., Pilloni, A., & Capodiferro, S. (2025). Immediate Loading of Implants-Supported Fixed Partial Prostheses in Posterior Regions: A Systematic Review. Dentistry Journal, 13(5), 213. https://doi.org/10.3390/dj13050213









