Health Outcomes and Resource Consumption Analysis of Radioembolization with Y90 Glass Microspheres (TARE-Y90) Versus Transarterial Chemoembolization with Irinotecan (DEBIRI) in Patients with Liver Metastases from Colorectal Cancer in Spain
Abstract
:1. Introduction
2. Materials and Methods
3. Study Design
4. Variables
5. Health Resource Consumption Analysis
- (1)
- Pre-procedural resource consumption (which accounts for the preparation of the patient before the intervention);
- (2)
- Treatment resource consumption (which includes the treatment itself, surgery room time, staff involved and specific material used in the procedure, including prophylactic drugs administered to the patient);
- (3)
- Post-procedure resource consumption (ICU stay and hospitalization length of stay).
6. Statistical Analysis
7. Results
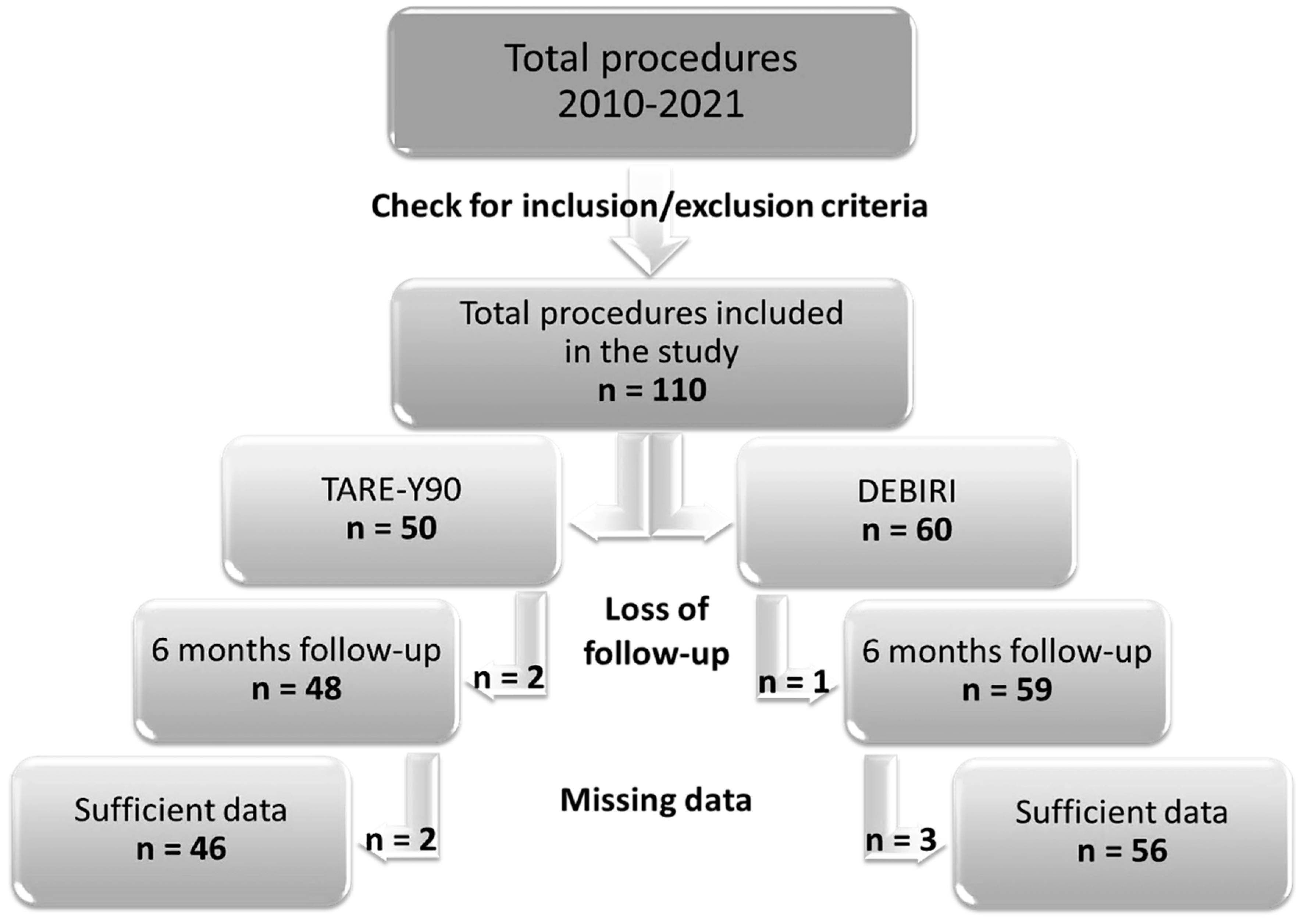
7.1. Retrospective Data Search: Subject Inclusion and Exclusion
7.2. Response to Treatment
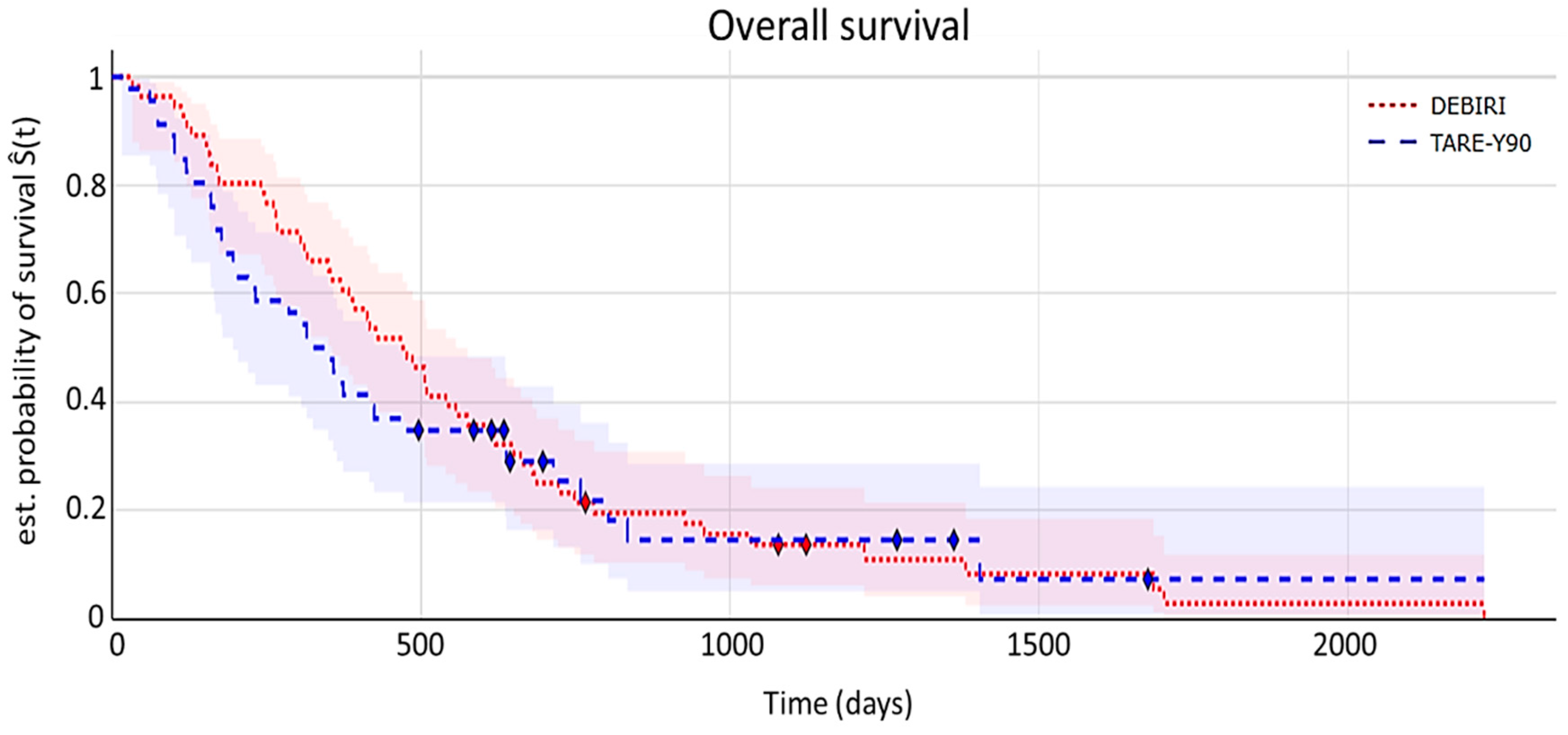
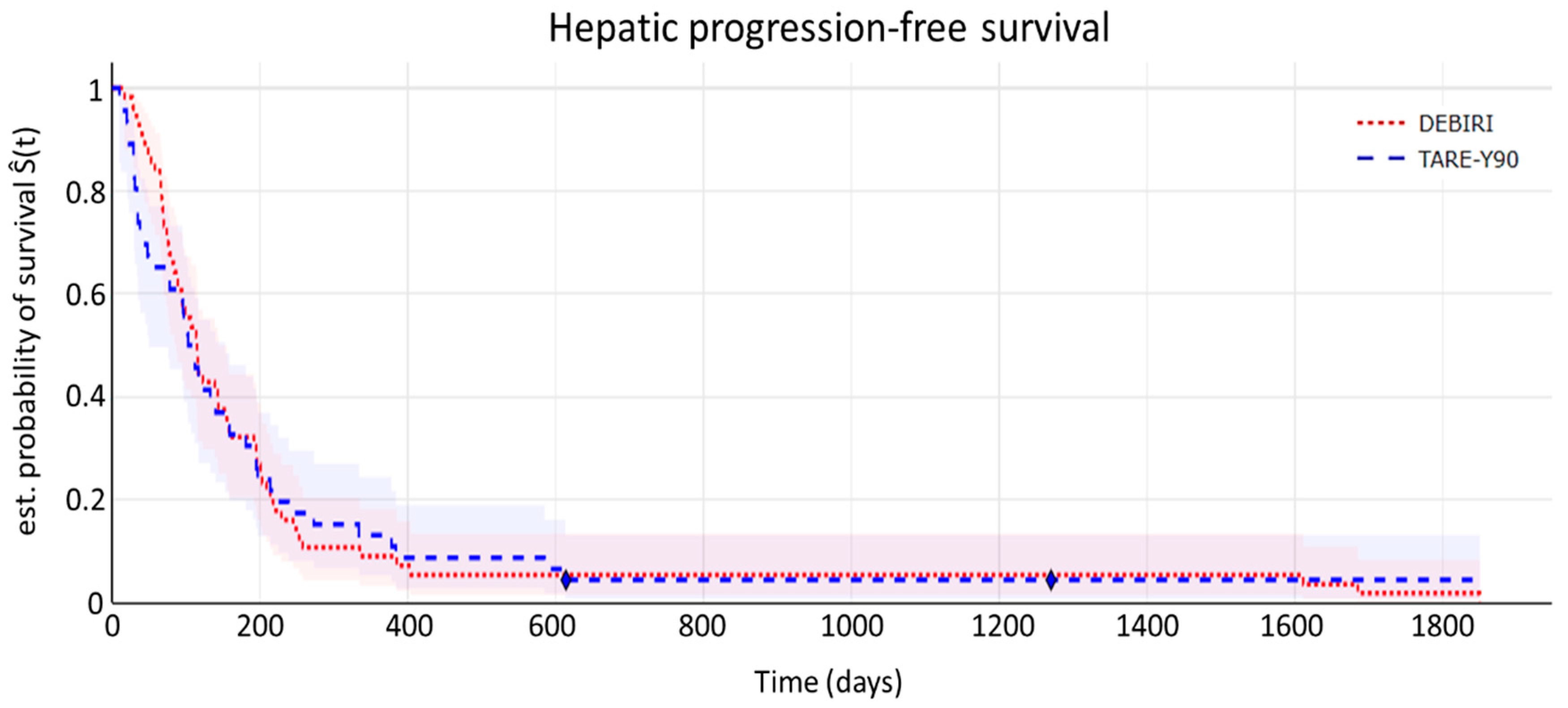
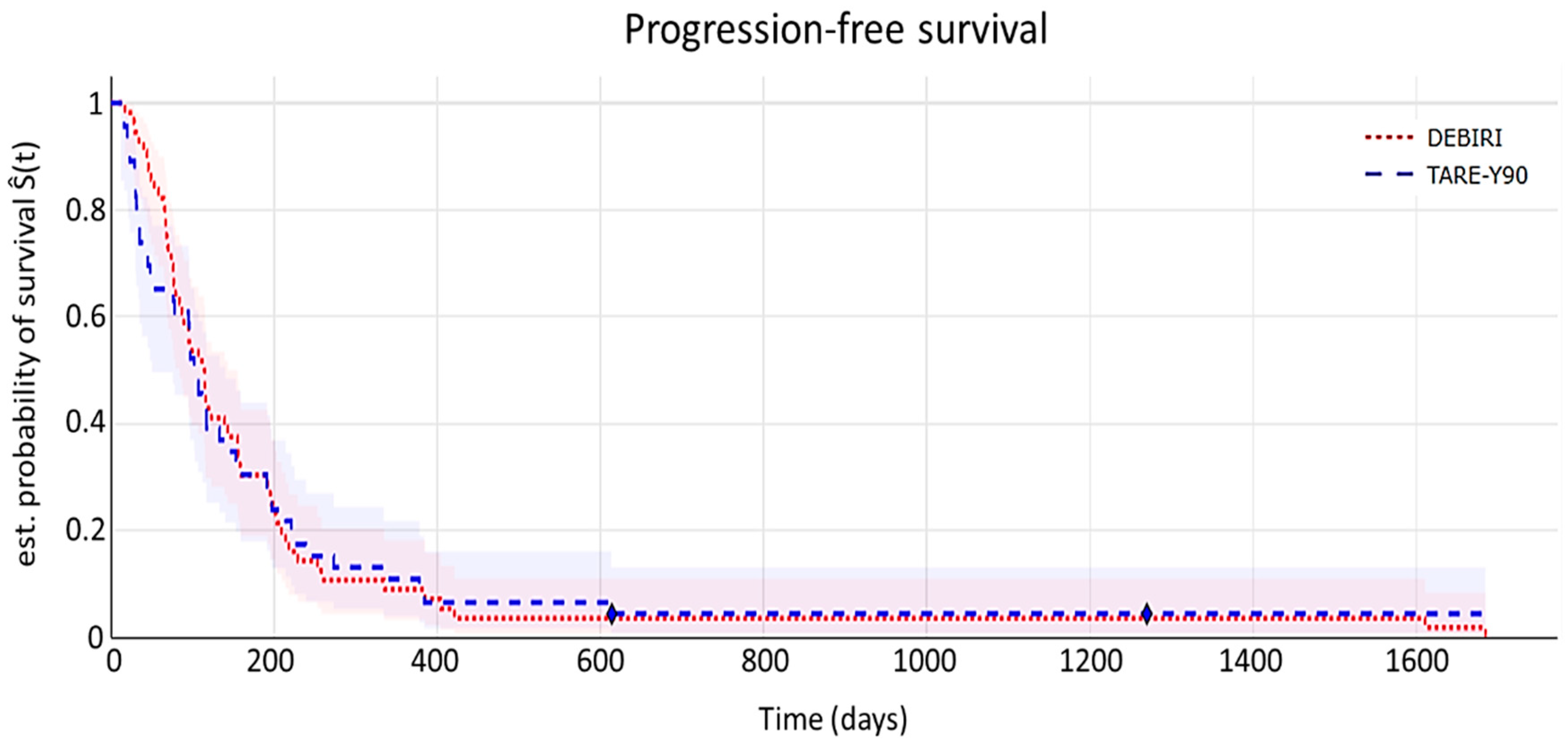
7.3. Time-to-Event Analyses
- (a)
- Overall survival (OS)
- (b)
- Hepatic progression-free survival (hPFS)
- (c)
- Progression-free survival (PFS)
7.4. Health Resource Consumption Analysis
8. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACs | Autonomous Communities |
| CEA | Carcinoembryonic antigen |
| CGP | Clinical Good Practice |
| CR | Complete response |
| DEBIRI | Transarterial chemoembolization (TACE) with irinotecan-preloaded particles |
| DL | Dyslipidemia |
| DM | Diabetes mellitus |
| DP | Disease progression |
| ECOG-PS | Eastern Cooperative Oncology Group Performance Status |
| eCRF | Electronic case report form |
| HBP | High blood pressure |
| HBV | Hepatitis B Virus |
| HCV | Hepatitis C Virus |
| HIV | Human Immunodeficiency Virus |
| hPFS | Hepatic progression-free survival |
| mCRC | Metastatic colorectal cancer |
| MSI | Microsatellite instability |
| NOR | No overall response |
| LM | Liver metastasis |
| OR | Overall response |
| OS | Overall survival |
| PFS | Progression-free survival |
| PR | Partial response |
| PPP | Purchasing power parity |
| PT | Primary tumor |
| QoL | Quality of life |
| QALY | Quality of life-adjusted life year |
| RECIST | Response Evaluation Criteria in Solid Tumors |
| SD | Stable disease |
| TACE | Transarterial chemoembolization |
| TARE | Transarterial radioembolization |
| TARE-Y90 | Transarterial radioembolization with Y90 glass microspheres |
| Y90 | Yttrium-90 radioactive |
References
- Cancer Research 2019. Cancer Research UK. Bowel Cancer Statistics. 2020. Available online: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/bowel-cancer#heading-Zero (accessed on 1 September 2020).
- IACR 2020. Cancer Today: International Association of Cancer Registries. Estimated Number of Deaths in 2020, Worldwide, Both Sexes, All Ages. 2021. Available online: https://gco.iarc.fr/today/online-analysis-table?v=2020&mode=cancer&mode_population=continents&population=900&populations=908&key=asr&sex=0&cancer=39&type=1&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=17&group_cancer=1&include_nmsc=1&include_nmsc_other=1#collapse-others (accessed on 18 March 2021).
- ACS 2020. American Cancer Society. 2020. Available online: https://www.cancer.org/cancer/colon-rectal-cancer/about/key-statistics.html#:~:text=In%20the%20United%20States%2C%20colorectal,about%2053%2C200%20deaths%20during%202020 (accessed on 16 March 2025).
- Safiri, S.; Sepanlou, S.G.; Ikuta, K.S.; Bisignano, C.; Salimzadeh, H.; Delavari, A. The global, regional, and national burden of colorectal cancer and its attributable risk factors in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2019, 4, 913–933. [Google Scholar]
- Ponz de Leon, M.; Benatti, P.; Borghi, F.; Pedroni, M.; Scarselli, A.; Di Gregorio, C.; Losi, L.; Viel, A.; Genuardi, M.; Abbati, G.; et al. Aetiology of colorectal cancer and relevance of monogenic inheritance. Gut 2004, 53, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Macrae, F. Colorectal Cancer: Epidemiology, Risk Factors, and Protective Factors. Macrae. 2022. Available online: https://www.uptodate.com/contents/colorectal-cancer-epidemiology-risk-factors-and-protective-factors (accessed on 16 March 2025).
- Lykoudis, P.M.; O’Reilly, D.; Nastos, K.; Fusai, G. Systematic review of surgical management of synchronous colorectal liver metastases. Br. J. Surg. 2014, 101, 605–612. [Google Scholar] [PubMed]
- Manfredi, S.; Lepage, C.; Hatem, C.; Coatmeur, O.; Faivre, J.; Bouvier, A.-M. Epidemiology and management of liver metastases from colorectal cancer. Ann. Surg. 2006, 244, 254–259. [Google Scholar] [CrossRef]
- Levy, J.; Zuckerman, J.; Garfinkle, R.; Acuna, S.A.; Touchette, J.; Vanounou, T.; Pelletier, J.S. Intra-arterial therapies for unresectable and chemorefractory colorectal cancer liver metastases: A systematic review and meta-analysis. HPB 2018, 20, 905–915. [Google Scholar]
- Wang, J.; Li, S.; Liu, Y.; Zhang, C.; Li, H.; Lai, B. Metastatic patterns and survival outcomes in patients with stage IV colon cancer: A population-based analysis. Cancer Med. 2020, 9, 361–373. [Google Scholar]
- Riihimäki, M.; Hemminki, A.; Sundquist, J.; Hemminki, K. Patterns of metastasis in colon and rectal cancer. Sci. Rep. 2016, 6, 29765. [Google Scholar] [CrossRef]
- Helling, T.S.; Martin, M. Cause of death from liver metastases in colorectal cancer. Ann. Surg. Oncol. 2014, 21, 501–506. [Google Scholar] [CrossRef]
- Gómez-España, M.A.; Gallego, J.; González-Flores, E.; Maurel, J.; Páez, D.; Sastre, J.; Aparicio, J.; Benavides, M.; Feliu, J.; Vera, R. SEOM clinical guidelines for diagnosis and treatment of metastatic colorectal cancer (2018). Clin. Transl. Oncol. 2019, 21, 46–54. [Google Scholar]
- Rodríguez-Fraile, M.; Iñarrairaegui, M. Radioembolización de tumores hepáticos con (90)Y-microesferas [Radioembolization with (90)Y-microspheres for liver tumors]. Rev. Esp. Med. Nucl. Imagen Mol. 2015, 34, 244–257. [Google Scholar]
- Salem, R.; Lewandowski, R.J.; Mulcahy, M.F.; Riaz, A.; Ryu, R.K.; Ibrahim, S.; Atassi, B.; Baker, T.; Gates, V.; Miller, F.H.; et al. Radioembolization for hepatocellular carcinoma using Yttrium-90 microspheres: A comprehensive report of long-term outcomes. Gastroenterology 2010, 138, 52–64. [Google Scholar] [CrossRef]
- Mulcahy, M.F.; Mahvash, A.; Pracht, M.; Montazeri, A.H.; Bandula, S.; Martin, R.C.G., 2nd; Salem, R.; Herrmann, K.; Brown, E.; Zuckerman, D.; et al. Radioembolization with Chemotherapy for Colorectal Liver Metastases: A Randomized, Open-Label, International, Multicenter, Phase III Trial. J. Clin. Oncol. 2021, 39, 3897–3907. [Google Scholar] [PubMed]
- Fiorentini, G.; Aliberti, C.; Benea, G.; Massimo, T.; Graziano, F.; Mambrini, A.; Guadagni, S. Hepatic arterial chemoembolization adopting DC Bead drug eluting bead loaded with irinotecan versus systemic therapy for colorectal cancer: A randomized study of efficacy and quality of life. AGH 2012, 6, 1448–1459. [Google Scholar] [CrossRef]
- Vera, R.; Gonzalez-Flores, E.; Rubio, C.; Urbano, J.; Valero Camps, M.; Ciampi-Dopazo, J.J.; Orcajo Rincón, J.; Morillo Macías, V.; Gomez Braco, M.A.; Suarez-Artacho, A. Multidisciplinary management of liver metastases in patients with colorectal cancer: A consensus of SEOM, AEC, SEOR, SERVEI, and SEMNIM. Clin. Transl. Oncol. 2020, 22, 647–662. [Google Scholar] [CrossRef]
- Kao, Y.H.; Tan, E.H.; Ng, C.E.; Goh, S.W. Clinical implications of the body surface area method versus partition model dosimetry for yttrium-90 radioembolization using resin microspheres: A technical review. Ann. Nucl. Med. 2011, 25, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Mikell, J.K.; Mahvash, A.; Siman, W.; Baladandayuthapani, V.; Mourtada, F.; Kappadath, S.C. Selective internal radiation therapy with yttrium-90 glass microspheres: Biases and uncertainties in absorbed dose calculations between clinical dosimetry models. Int. J. Radiat. Oncol. Biol. Phys. 2016, 96, 888–896. [Google Scholar]
- Morán, V.; Prieto, E.; Sancho, L.; Rodríguez-Fraile, M.; Soria, L.; Zubiria, A.; Martí-Climent, J.M. Impact of the dosimetry approach onthe resulting 90Y radioembolization planned absorbed doses based on99mTc-MAA SPECT-CT: ¿is there agreement between dosimetry methods? EJNMMI Phys. 2020, 7, 1–22. [Google Scholar]
- Knight, G.M.; Gordon, A.C.; Gates, V.; Talwar, A.; Riaz, A.; Salem, R.; Lewandowski, R. Evolution of Personalized Dosimetry for Radioembolization of Hepatocellular Carcinoma. J. Vasc. Interv. Radiol. 2023, 34, 1214–1225. [Google Scholar] [PubMed]
- Bester, L.; Wasan, H.; Sangro, B.; Kennedy, A.; Pennington, B.; Sennfält, K. Selective internal Radiotherapy (SIRT) using Resin Yttrium-90 Microspheres for Chemotherapy-Refractory metastatic colorectal Cancer: A UK cost-effectiveness analysis. Value Health 2013, 16, A413. [Google Scholar] [CrossRef]
- Cosimelli, M.; Golfieri, R.; Pennington, B.; Sennfält, K. Selective internal Radiotherapy (SIRT) using Resin Yttrium-90 Microspheres for Chemotherapy-Refractory metastatic colorectal Cancer: An italian cost-effectiveness analysis. Value Health 2013, 16, A409. [Google Scholar] [CrossRef]
- Pennington, B.; Akehurst, R.; Wasan, H.; Sangro, B.; Kennedy, A.S.; Sennfält, K.; Bester, L. Cost-effectiveness of selective internal radiation therapy using yttrium-90 resin microspheres in treating patients with inoperable colorectal liver metastases in the UK. J. Med. Econ. 2015, 18, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Brennan, V.K.; Colaone, F.; Shergill, S.; Pollock, R.F. A cost-utility analysis of SIR-Spheres Y-90 resin microspheres versus best supportive care in the treatment of unresectable metastatic colorectal cancer refractory to chemotherapy in the UK. J. Med. Econ. 2020, 23, 1588–1597. [Google Scholar] [CrossRef] [PubMed]
- Loveman, E.; Jones, J.; Clegg, A.J.; Picot, J.; Colquitt, J.L.; Mendes, D.; Breen, D.J.; Moore, E.; George, S.; Poston, G.; et al. The clinical effectiveness and cost-effectiveness of ablative therapies in the management of liver metastases: Systematic review and economic evaluation. Health Technol. Assess. 2014, 18, 1–284. [Google Scholar] [CrossRef]
- Fusco, F.; Wolstenholme, J.; Gray, A.; Chau, I.; Dunham, L.; Love, S.; Roberts, A.; Moschandreas, J.; Virdee, P.; Lewington, V.; et al. Selective internal Radiotherapy (SIRT) in metastatic colorectal Cancer patients with liver metastases: Preliminary primary Care Resource Use and Utility results from the Foxfire Randomised Controlled Trial. Value Health 2017, 20, A445–A446. [Google Scholar] [CrossRef]
- Dhir, M.; Zenati, M.S.; Jones, H.L.; Bartlett, D.L.; Choudry, M.H.A.; Pingpank, J.F.; Holtzman, M.P.; Bahary, N.; Hogg, M.E.; Zeh, H.J., 3rd; et al. Effectiveness of hepatic artery infusion (HAI) Versus Selective Internal Radiation Therapy (Y90) for pretreated isolated unresectable colorectal liver metastases (IU-CRCLM). Ann. Surg. Oncol. 2018, 25, 550–557. [Google Scholar] [CrossRef] [PubMed]
- Bester, L.; Meteling, B.; Pocock, N.; Pavlakis, N.; Chua, T.C.; Saxena, A.; Morris, D.L. Radioembolization versus standard care of hepatic metastases: Comparative retrospective cohort study of survival outcomes and adverse events in salvage patients. J. Vasc. Interv. Radiol. JVIR 2012, 23, 96–105. [Google Scholar] [CrossRef]
- Gray, B.; Van Hazel, G.; Hope, M.; Burton, M.; Moroz, P.; Anderson, J.; Gebski, V. Randomised trial of SIR-Spheres plus chemotherapy vs. chemotherapy alone for treating patients with liver metastases from primary large bowel cancer. Ann. Oncol. Off J. Eur. Soc. Med. Oncol. 2001, 12, 1711–1720. [Google Scholar] [CrossRef]
- Karanicolas, P.; Beecroft, J.; Cosby, R.; David, E.; Kalyvas, M.; Kennedy, E.; Sapisochin, G.; Wong, R.; Zbuk, K. Regional Therapies for Colorectal Liver Metastases: Systematic review and clinical practice Guideline. Clin. Color. Cancer 2021, 20, 20–28. [Google Scholar] [CrossRef]
- Salem, R.; Lewandowski, R.J.; Gates, V.L.; Nutting, C.W.; Murthy, R.; Rose, S.C.; Soulen, M.C.; Geschwind, J.F.; Kulik, L.; Kim, Y.H.; et al. Research Reporting Standards for Radioembolization of hepatic malignancies. J. Vasc. Interv. Radiol. 2011, 22, 265–278. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Colorectal cancer with unilobar or bilobar metastatic liver disease (stage IV), unresectable and with disease progression in the liver after several lines of chemotherapy (at least one). | Background of hepatic encephalopathy. |
| Clinically stable or resected primary tumor. | Pulmonary insufficiency or clinically evident chronic obstructive pulmonary disease. |
| Tumor replacement below 50% of the total volume of the liver. | Cirrhosis and portal hypertension. |
| Patients treated with TARE-Y90 (TheraSphere® Y-90 Glass Microspheres- Boston Scientific, Malborough, MA, USA). | History of severe allergy or intolerance to contrast agents, narcotics, sedatives or atropine that cannot be treated medically. |
| Patients treated with DEBIRI (DC Beads M1 70–150 µ- Boston Scientific, Malborough, MA, USA). | Contraindications to angiography or selective visceral catheterization such as bleeding or coagulopathy not controllable with common hemostatic agents (e.g., device closure). |
| Life expectancy greater than 6 months at the start of locoregional therapy (minimum post-procedure follow-up time: 6 months or until death). | Intervention or compromise of the Ampulla of Vater. |
| ECOG 0–1 until the first treatment under scope. | Clinically obvious ascites (traces of ascites on imaging are acceptable). |
| Creatinine serum < 2.0 mg/dL. | Hepatic toxicity due to previous cancer therapy that has not been resolved before the start of study treatment, if the researcher determines that the continuing complication will compromise the patient’s safe treatment. |
| Serum bilirubin up to 1.2× upper limit. | Significant life-threatening extra-hepatic disease, including patients who are on dialysis, have unresolved diarrhea or have severe unresolved infections, including patients known to be HIV-positive or to have acute HBV or HCV. |
| Albumin > 3.0 g/dL. | Confirmed extra-hepatic metastases. Limited and indeterminate extra-hepatic lesions are allowed in the lung and/or lymph nodes (up to 5 lesions in the lung, with each individual lesion < 1 cm; any number of lymph nodes with each individual node < 1.5 cm). |
| Neutrophil count > 1200/mm3 (1.2 × 109/L) | Previous treatment with liver radiotherapy. |
| Previous intra-arterial therapy directed at the liver, including transarterial chemoembolization (TACE) using irinotecan-loaded beads or TARE-Y90 therapy. | |
| Treatment with biological agents within 28 days of receiving TARE-Y90 therapy. |
|
|
|
|
| TARE-Y90 (N = 46) | DEBIRI (N = 56) | p | ||
|---|---|---|---|---|
| Age (years) | 62 ± 10 (34–77) | 62 ± 9 (45–79) | 0.89 (a) | |
| Sex | Men | 67% (31) | 70% (39) | 0.83 (c) |
| Women | 33% (15) | 30% (17) | ||
| ECOG | PS 0 | 72% (33) | 66% (38) | 0.56 (c) |
| PS 1 | 26% (12) | 25% (14) | ||
| PS 2 | 2% (1) | 7% (4) | ||
| HTA | 46% (21) | 41% (23) | 0.69 (c) | |
| DM | 13% (6) | 16% (9) | 0.78 (c) | |
| DL | 22% (10) | 30% (17) | 0.37 (c) | |
| PT localization | DX | 28% (13) | 23% (13) | 0.81 (c) |
| SX | 72% (33) | 75% (42) | ||
| DX; SX | 0% (0) | 2% (1) | ||
| PT vascular invasion | 50% (23) | 28% (16) | 0.30 (c) | |
| RAS mutation | 28% (13) | 27% (15) | 1.00 (c) | |
| BRAf | 2% (1) | 4% (2) | 1.00 (c) | |
| LM at PT diagnosis | 72% (33) | 70% (39) | 0.83 (c) | |
| Other Metastasis during the treatment | Lymph node | 12% (6) | 12% (7) | 1.00 (c) |
| Lung | 11% (5) | 12% (7) | ||
| Other location | 5% (2) | 4% (2) | ||
| No | 72% (33) | 72% (40) | ||
| Ascites | 4% (2) | 0% (0) | 0.20 (c) | |
| Peritoneal carcinomatosis | 7% (3) | 2% (1) | 0.32 (c) | |
| Imaging test mode | CT | 80% (37) | 84% (47) | 0.78 (c) |
| PET-CT | 9% (4) | 5% (3) | ||
| RM | 7% (3) | 9% (5) | ||
| Echography | 4% (2) | 2% (1) | ||
| N° LM | 4 ± 2 | 4 ± 4 | 0.61 (b) | |
| Size of target lesion | 45.7 ± 33.8 | 53.1 ± 35.1 | 0.30 (a) | |
| PET-CT pre-treatment | 61% (28) | 39% (22) | 0.05 (c) * | |
| LM localization | LHD | 50% (23) | 34% (19) | 0.14 (c) |
| LHI | 2% (1) | 9% (5) | ||
| Bilobar extension | 48% (22) | 56% (32) | ||
| Tumor burden | <25% | 58% (27) | 68% (38) | 0.58 (c) |
| from 25 to 50% | 33% (15) | 23% (13) | ||
| >50% | 9% (4) | 9% (5) | ||
| Pre-treatment CEA value (ng/mL) | 286 ± 958 | 179 ± 557 | 0.61 (a) | |
| Previous treatment for PT | Primary tumor surgery | 78% (36) | 96% (54) | 0.006 (c) ** |
| Systemic therapy | 96% (44) | 100% (56) | 0.20 (c) | |
| Surgery and/or systemic therapy | 100% (46) | 100% (56) | 1.00 (c) | |
| N° lines of systemic therapy | 1.9 ± 0.7 | 2.1 ± 1.4 | 0.57 (a) | |
| Type of first-line therapy | FOLFOX | 65% (30) | 66% (37) | 0.92 (c) |
| FOLFIRI | 15% (7) | 18% (10) | ||
| FOLFOX; FOLFIRI | 20% (9) | 16% (9) | ||
| Type of previous treatment for LM | Surgery | 30% (14) | 50% (28) | 0.07 (c) |
| TACE | 2% (1) | 9% (5) | 1.00 (c) | |
| Ablation | 20% (9) | 21% (12) | 1.00 (c) | |
| TARE-Y90 (n = 46) | DEBIRI (n = 56) | p | |
|---|---|---|---|
| CR | 4% (1) | 12% (9) | 0.06 |
| PR | 20% (9) | 20% (10) | |
| SD | 30% (15) | 20% (10) | |
| PD | 46% (21) | 48% (27) |
| TARE-Y90 (n = 46) | DEBIRI (n = 56) | p | |
|---|---|---|---|
| OR | 24% (10) | 52% (19) | 0.19 |
| NOR | 18% (36) | 48% (37) |
| Device/Procedure/Health Provider/Time | Units per TARE-Y90 Procedure | Units per DEBIRI Procedure |
|---|---|---|
| Selective angiographic catheter | 1 | 0 |
| Simmons catheter | 1 | 0 |
| Guide | 1 | 0 |
| Introducer | 1 | 0 |
| Vascular puncture needle | 1 | 0 |
| Micro catheter | 1 | 0 |
| Vascular closure device | 1 | 0 |
| Coils | 1 | 0 |
| 99Tc-MAA | 1 | 0 |
| Pre-treatment assessment with MAA | 1 | 0 |
| Dosimetry of patients treated with radioactive isotopes | 1 | 0 |
| Physician/specialist | 3 | 0 |
| Specialist technician | 1 | 0 |
| Nurse | 2 | 0 |
| Hospitalization (days) | 1 | 0 |
| Device/Drug/Health Provider/Time | Units per TARE-Y90 Procedure | Units per DEBIRI Procedure |
|---|---|---|
| Selective angiographic catheter | 1 | 1 |
| Simmons catheter | 1 | 1 |
| Guide | 1 | 1 |
| Introducer | 1 | 1 |
| Vascular puncture needle | 1 | 1 |
| Micro catheter | 1 | 1 |
| Vascular closure device | 1 | 1 |
| 90Y particles | 1 | 0 |
| DEBIRI particles | 0 | 2 |
| Irinotecan | 0 | 2 |
| - Gastroduodenal ulcer prophylaxis | 1 | 1 |
| - Anti-nausea prophylaxis | 0 | 1 |
| - Postembolization syndrome prophylaxis | 1 | 1 |
| - Intravenous corticosteroid before treatment | 1 | 1 |
| - Cefuroxime | 1 | 1 |
| Physician/specialist | 3 | 1 |
| Specialist technician | 1 | 1 |
| Nurse | 2 | 2 |
| Procedure/Hospitalization | Units per TARE-Y90 Procedure | Units per DEBIRI Procedure |
|---|---|---|
| Whole-body positron tomography (PET-CT) | 1 | 0 |
| Dosimetry of patients treated with radioactive isotopes | 1 | 0 |
| Stay in intensive care unit (hours) | 0 | 2.20 |
| Hospitalization (days) | 1 | 2.56 |
| Concept | TARE-Y90 | DEBIRI |
|---|---|---|
| Average treatments per patient | 1.33 | 3.16 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciampi-Dopazo, J.J.; Ruiz Villaverde, G.; Espejo, J.J.; García Marcos, R.; Pérez Enguix, D.; Pisoni, S.; Martínez-Rodrigo, J.J.; Navarro Vergara, P.; Pardo Moreno, P.; Rodríguez-Fernández, A. Health Outcomes and Resource Consumption Analysis of Radioembolization with Y90 Glass Microspheres (TARE-Y90) Versus Transarterial Chemoembolization with Irinotecan (DEBIRI) in Patients with Liver Metastases from Colorectal Cancer in Spain. Diagnostics 2025, 15, 796. https://doi.org/10.3390/diagnostics15070796
Ciampi-Dopazo JJ, Ruiz Villaverde G, Espejo JJ, García Marcos R, Pérez Enguix D, Pisoni S, Martínez-Rodrigo JJ, Navarro Vergara P, Pardo Moreno P, Rodríguez-Fernández A. Health Outcomes and Resource Consumption Analysis of Radioembolization with Y90 Glass Microspheres (TARE-Y90) Versus Transarterial Chemoembolization with Irinotecan (DEBIRI) in Patients with Liver Metastases from Colorectal Cancer in Spain. Diagnostics. 2025; 15(7):796. https://doi.org/10.3390/diagnostics15070796
Chicago/Turabian StyleCiampi-Dopazo, Juan José, Gonzalo Ruiz Villaverde, Juan José Espejo, Raúl García Marcos, Daniel Pérez Enguix, Serena Pisoni, José J. Martínez-Rodrigo, Pablo Navarro Vergara, Pedro Pardo Moreno, and Antonio Rodríguez-Fernández. 2025. "Health Outcomes and Resource Consumption Analysis of Radioembolization with Y90 Glass Microspheres (TARE-Y90) Versus Transarterial Chemoembolization with Irinotecan (DEBIRI) in Patients with Liver Metastases from Colorectal Cancer in Spain" Diagnostics 15, no. 7: 796. https://doi.org/10.3390/diagnostics15070796
APA StyleCiampi-Dopazo, J. J., Ruiz Villaverde, G., Espejo, J. J., García Marcos, R., Pérez Enguix, D., Pisoni, S., Martínez-Rodrigo, J. J., Navarro Vergara, P., Pardo Moreno, P., & Rodríguez-Fernández, A. (2025). Health Outcomes and Resource Consumption Analysis of Radioembolization with Y90 Glass Microspheres (TARE-Y90) Versus Transarterial Chemoembolization with Irinotecan (DEBIRI) in Patients with Liver Metastases from Colorectal Cancer in Spain. Diagnostics, 15(7), 796. https://doi.org/10.3390/diagnostics15070796










