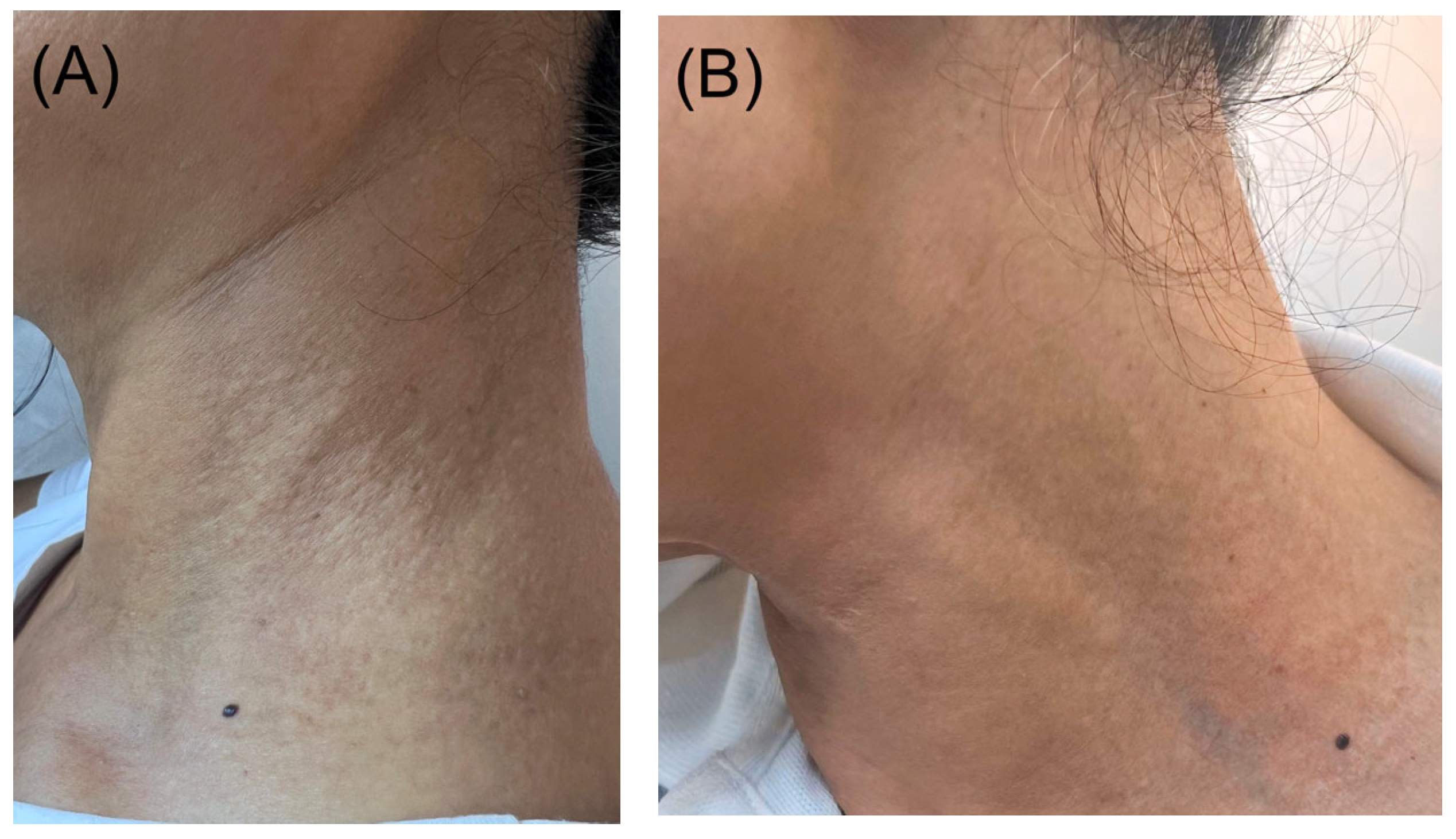
Skin-Colored Papules on the Neck of a Postmenopausal Woman: A Diagnostic Challenge
Abstract
1. Case Presentation
2. What Is the Diagnosis?
- A.
- Pseudoxanthoma elasticum;
- B.
- Pseudoxanthoma elasticum-like papillary dermal elastolysis;
- C.
- White fibrous papulosis;
- D.
- Papillary dermal elastosis;
- E.
- Mid-dermal elastolysis.
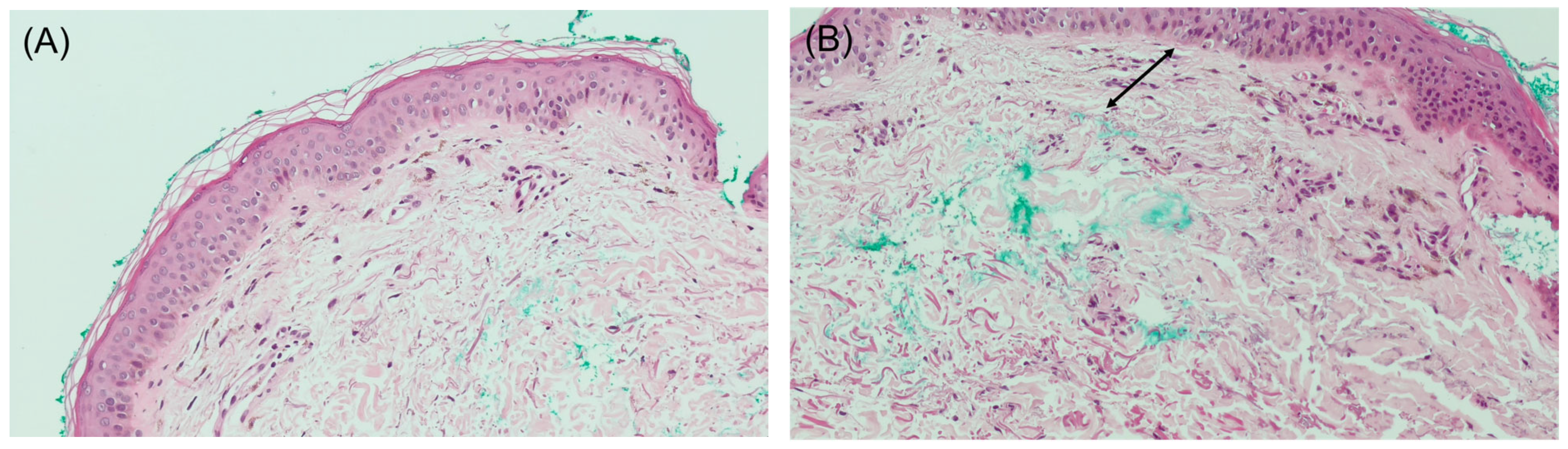
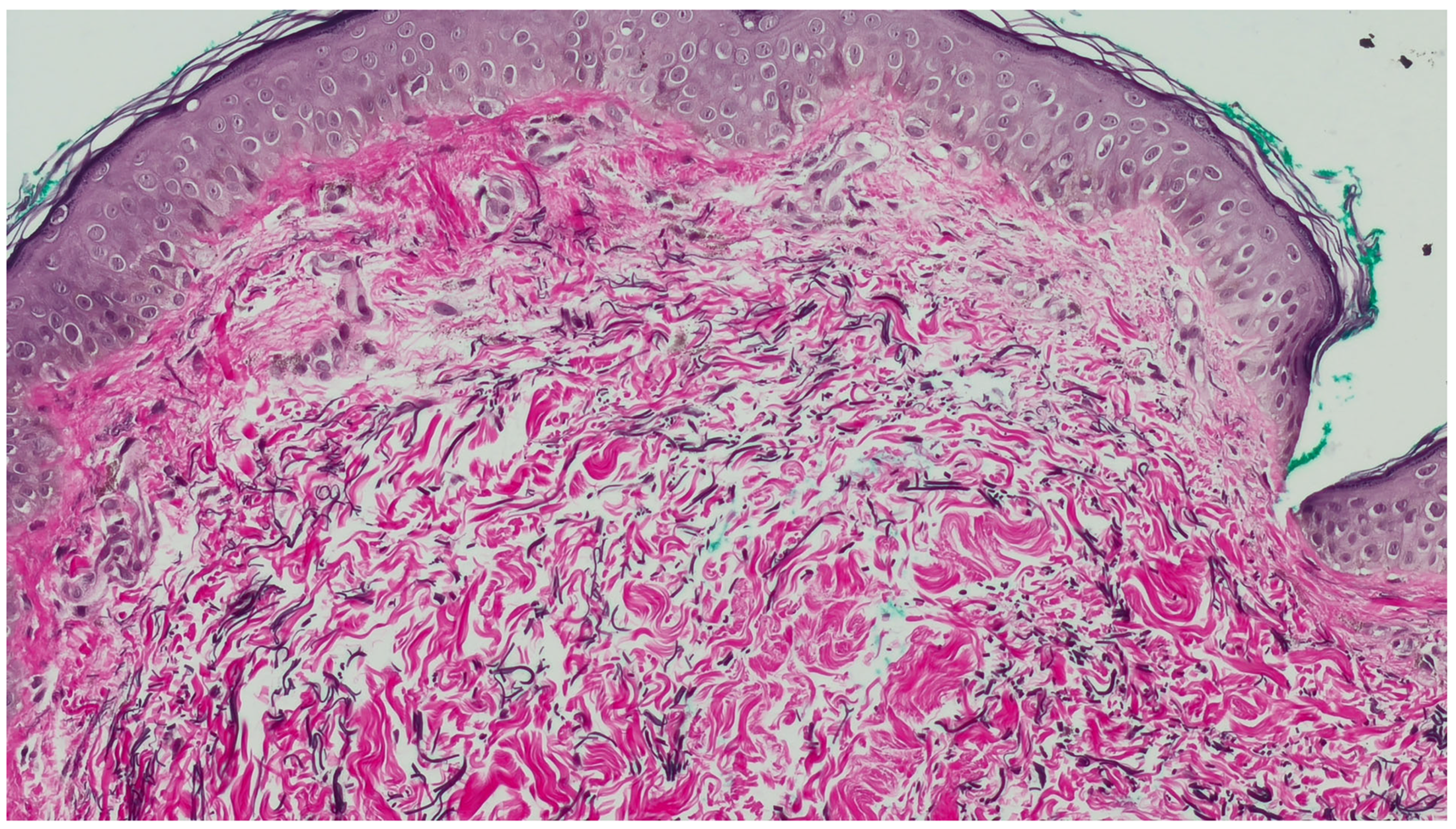
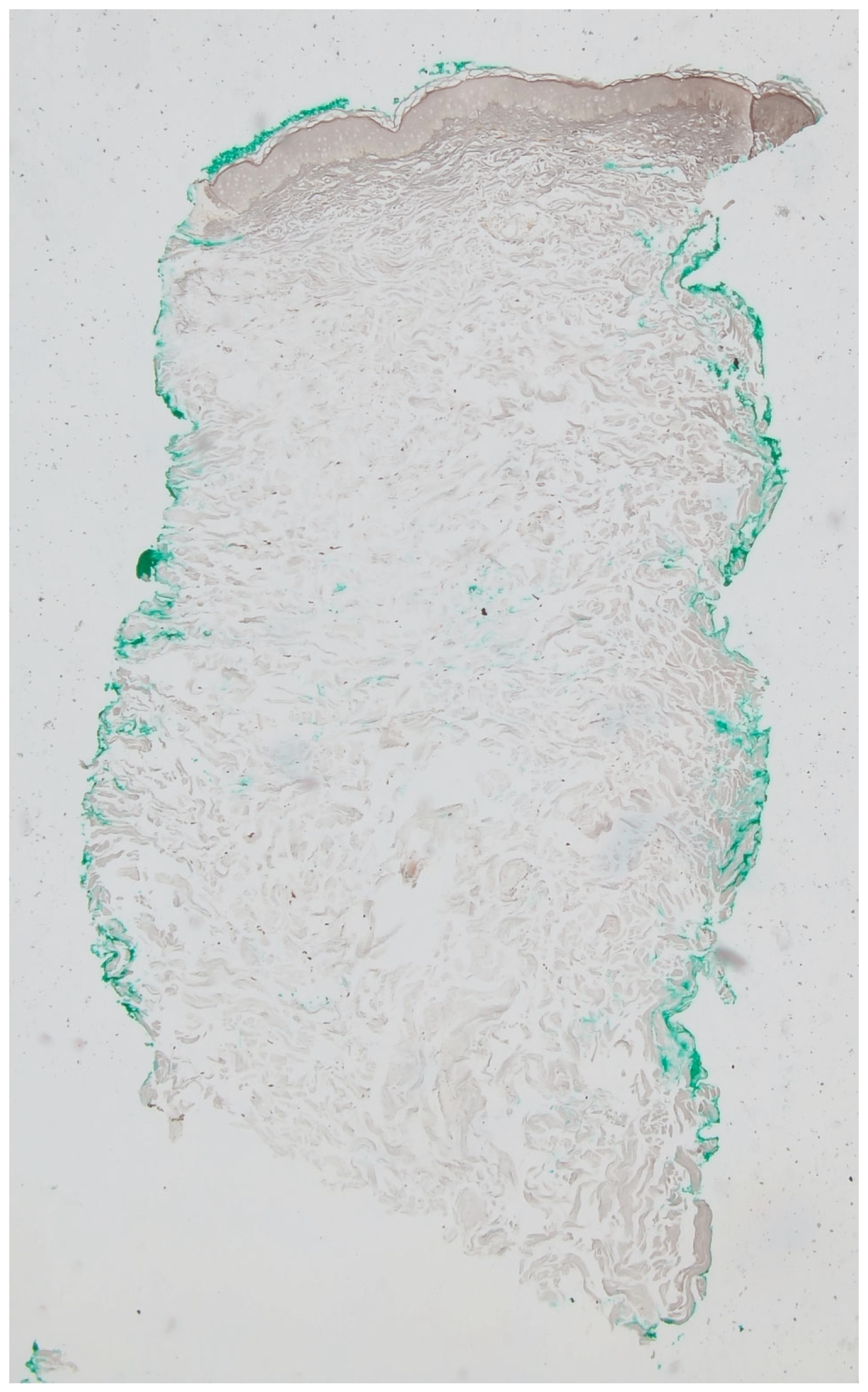
3. Diagnosis
Pseudoxanthoma Elasticum-like Papillary Dermal Elastolysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pranteda, G.; Muscianese, M.; Marmo, G.; Fidanza, L.; Pranteda, G.; Tamburi, F.; Bottoni, U.; Nisticò, S. Role of steroid therapy in pseudoxanthoma elasticum-like papillary dermal elastolysis. Int. J. Immunopathol. Pharmacol. 2013, 26, 1013–1018. [Google Scholar] [CrossRef] [PubMed]
- Rongioletti, F.; Rebora, A. Pseudoxanthoma elasticum-like papillary dermal elastolysis. J. Am. Acad. Dermatol. 1992, 26, 648–650. [Google Scholar] [CrossRef] [PubMed]
- Byun, J.Y.; Do, M.O.; Kim, S.H.; Choi, H.Y.; Myung, K.B.; Choi, Y.W. Pseudoxanthoma elasticum-like papillary dermal elastolysis developed in early middle age. J. Dermatol. 2007, 34, 709–711. [Google Scholar] [CrossRef] [PubMed]
- Rongioletti, F.; Izakovic, J.; Romanelli, P.; Lanuti, E.; Miteva, M. Pseudoxanthoma elasticum-like papillary dermal elastolysis: A large case series with clinicopathological correlation. J. Am. Acad. Dermatol. 2012, 67, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Orlandi, A.; Bianchi, L.; Nini, G.; Spagnoli, L.G. Familial occurrence of pseudoxanthoma-elasticum-like papillary dermal elastolysis. J. Eur. Acad. Dermatol. Venereol. 1998, 10, 175–178. [Google Scholar] [PubMed]
- Lewis, K.G.; Bercovitch, L.; Dill, S.W.; Robinson-Bostom, L. Acquired disorders of elastic tissue, part II: Decreased elastic tissue. J. Am. Acad. Dermatol. 2004, 51, 165–185. [Google Scholar] [CrossRef] [PubMed]
- Rongioletti, F.; Rebora, A. Fibroelastolytic patterns of intrinsic skin aging: Pseudoxanthoma-elasticum-like papillary dermal elastolysis and white fibrous papulosis of the neck. Dermatology 1995, 191, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Bhawan, J.; Andersen, W.; Lee, J.; Labadie, R.; Solares, G. Photoaging versus intrinsic aging: A morphologic assessment of facial skin. J. Cutan. Pathol. 1995, 22, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Fabre, V.C.; Lear, S.; Reichlin, M.; Hodge, S.J.; Callen, J.P. Twenty percent of biopsy specimens from sun-exposed skin of normal young adults demonstrate positive immunofluorescence. Arch. Dermatol. 1991, 127, 1006–1011. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, H.; Kimura, S.; Harada, T.; Nishikawa, T. White fibrous papulosis of the neck: A new clinicopathologic entity? J. Am. Acad. Dermatol. 1989, 20, 1073–1077. [Google Scholar] [CrossRef] [PubMed]
- Gencoglan, G.; Ceylan, C.; Kazandi, A.C. White fibrous papulosis of the neck. Cutan. Ocul. Toxicol. 2011, 30, 69–71. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.R.; Lewis, K.; Lewis, M.; Robinson-Bostom, L. Papillary dermal elastosis: A unique elastic tissue disorder or an unusual manifestation of pseudoxanthoma elasticum-like papillary dermal elastolysis? J. Cutan. Pathol. 2009, 36, 1010–1013. [Google Scholar] [CrossRef] [PubMed]
- Gambichler, T. Mid-dermal elastolysis revisited. Arch. Dermatol. Res. 2010, 302, 85–93. [Google Scholar] [CrossRef]
- Foering, K.; Torbeck, R.L.; Frank, M.P.; Saedi, N. Treatment of pseudoxanthoma elasticum-like papillary dermal elastolysis with nonablative fractional resurfacing laser resulting in clinical and histologic improvement in elastin and collagen. J. Cosmet. Laser Ther. 2018, 20, 382–384. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the European Society of Dermatopathology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
El Jalkh, J.; Obeid, P.M.; Guermazi, D.; Soubra, A.; Saliba, E. Skin-Colored Papules on the Neck of a Postmenopausal Woman: A Diagnostic Challenge. Dermatopathology 2025, 12, 15. https://doi.org/10.3390/dermatopathology12020015
El Jalkh J, Obeid PM, Guermazi D, Soubra A, Saliba E. Skin-Colored Papules on the Neck of a Postmenopausal Woman: A Diagnostic Challenge. Dermatopathology. 2025; 12(2):15. https://doi.org/10.3390/dermatopathology12020015
Chicago/Turabian StyleEl Jalkh, Jason, Pia Maria Obeid, Dorra Guermazi, Aya Soubra, and Elie Saliba. 2025. "Skin-Colored Papules on the Neck of a Postmenopausal Woman: A Diagnostic Challenge" Dermatopathology 12, no. 2: 15. https://doi.org/10.3390/dermatopathology12020015
APA StyleEl Jalkh, J., Obeid, P. M., Guermazi, D., Soubra, A., & Saliba, E. (2025). Skin-Colored Papules on the Neck of a Postmenopausal Woman: A Diagnostic Challenge. Dermatopathology, 12(2), 15. https://doi.org/10.3390/dermatopathology12020015





