Sleep among Youth with Severely Disabling Chronic Pain: Before, during, and after Inpatient Intensive Interdisciplinary Pain Treatment
Abstract
:1. Introduction
1.1. Sleep in Pediatric Chronic Pain
1.2. Interventions for Disabling Pediatric Chronic Pain
1.3. Preliminary Data
1.4. Study Aims and Hypotheses
2. Materials and Methods
2.1. Participants and Recruitment
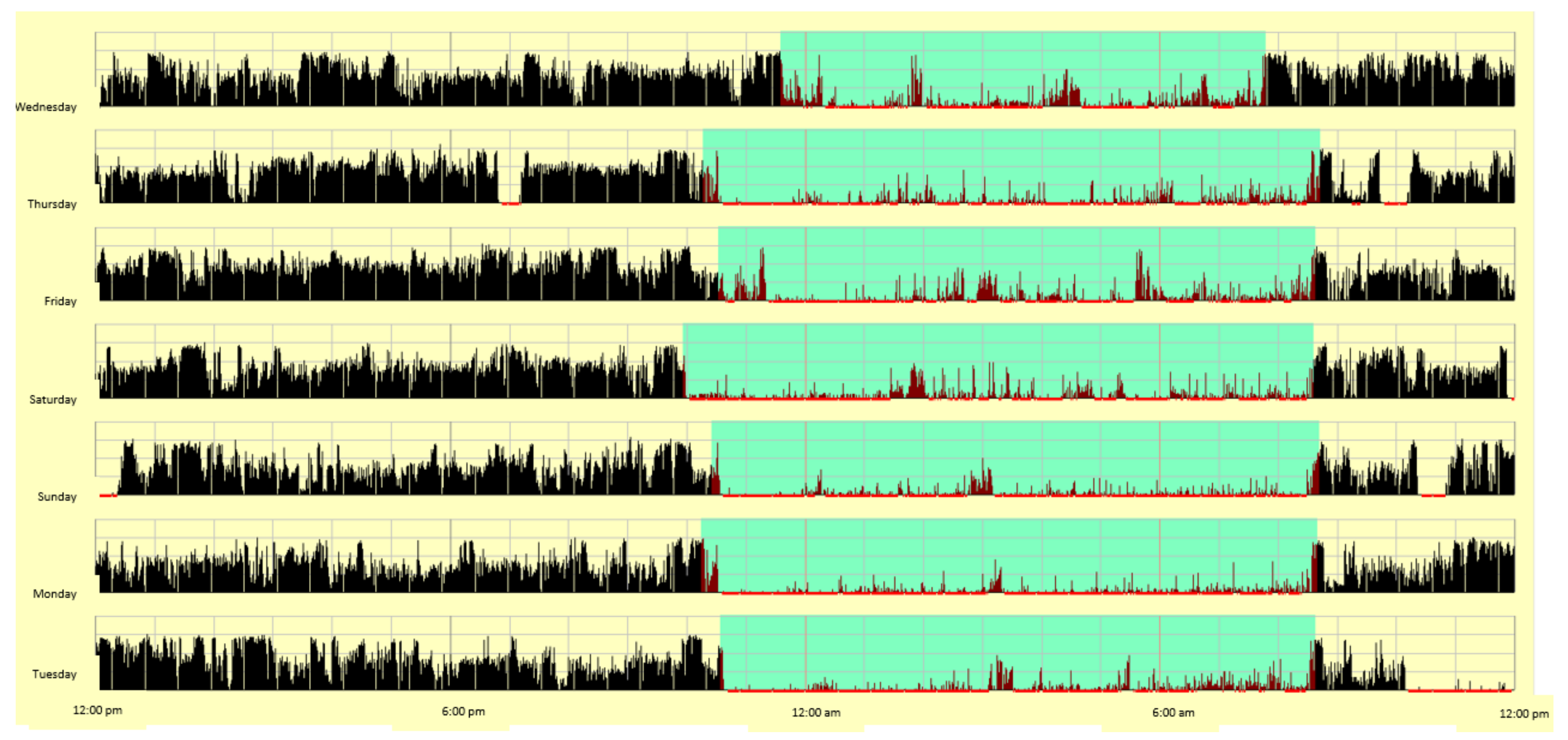
2.2. Procedures
2.3. Inpatient Pain Rehabilitation Setting
2.4. Measures
2.5. Analytic Approach
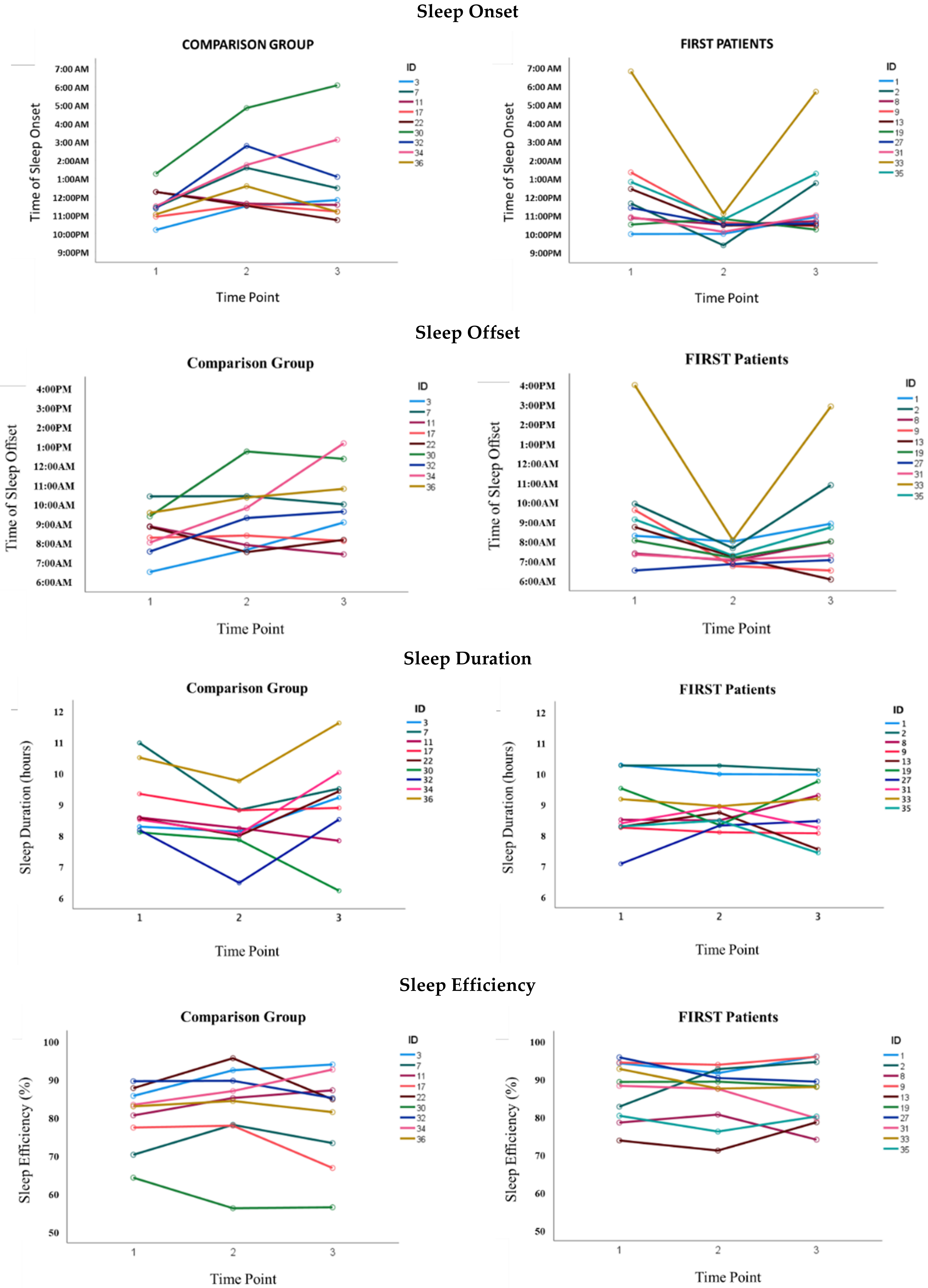
3. Results
4. Discussion
4.1. Overview of Findings
4.2. Possible Drivers of Sleep Pattern Improvements
4.3. Sleep Quality
4.4. Limitations, Strengths, and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lewandowski, A.S.; Palermo, T. Introduction to the special issue: Advances in Behavioral and psychological pain research in children: From prevention through chronic pain management. J. Pediatr. Psychol. 2018, 43, 219–223. [Google Scholar] [CrossRef]
- Huguet, A.; Miró, J. The severity of chronic pediatric pain: An epidemiological study. J. Pain Off. J. Am. Pain Soc. 2008, 9, 226–236. [Google Scholar] [CrossRef] [PubMed]
- Carter, B.D.; Threlkeld, B.M. Psychosocial perspectives in the treatment of pediatric chronic pain. Pediatr. Rheumatol. Online J. 2012, 10, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Logan, D.E.; Simons, L.E.; Stein, M.J.; Chastain, L. School impairment in adolescents with chronic pain. J. Pain 2008, 9, 407–416. [Google Scholar] [CrossRef]
- Hunfeld, J.A.M.; Perquin, C.W.; Bertina, W.; Hazebroek-Kampschreur, A.A.J.M.; van Suijlekom-Smit, L.W.A.; Koes, B.W.; van der Wouden, J.C.; Passchier, J. Stability of pain parameters and pain-related quality of life in adolescents with persistent pain: A three-year follow-up. Clin. J. Pain 2002, 18, 99–106. [Google Scholar] [CrossRef]
- Kashikar-Zuck, S.; Johnston, M.; Ting, T.V.; Graham, B.T.; Lynch-Jordan, A.M.; Verkamp, E.; Passo, M.; Schikler, K.N.; Hashkes, P.J.; Spalding, S.; et al. Relationship between School absenteeism and depressive symptoms among adolescents with Juvenile Fibromyalgia. J. Pediatr. Psychol. 2010, 35, 996–1004. [Google Scholar] [CrossRef]
- Long, A.C.; Palermo, T.M.; Manees, A.M. Brief report: Using actigraphy to compare physical activity levels in adolescents with chronic pain and healthy adolescents. J. Pediatr. Psychol. 2007, 33, 660–665. [Google Scholar] [CrossRef] [Green Version]
- Wilson, A.C.; Palermo, T.M. Physical activity and function in adolescents with chronic pain: A controlled study using actigraphy. J. Pain 2012, 13, 121–130. [Google Scholar] [CrossRef] [Green Version]
- Larsson, B.; Sund, A.M. Emotional/behavioural, social correlates and one-year predictors of frequent pains among early adolescents: Influences of pain characteristics. Eur. J. Pain 2007, 11, 57–65. [Google Scholar] [CrossRef]
- Crowley, S.; Carskadon, M. Modifications to weekend recovery sleep delay circadian phase in older adolescents. Chronobiol. Int. 2010, 27, 1469–1492. [Google Scholar] [CrossRef]
- Monk, T. Enhancing circadian zeitgebers. Sleep 2010, 33, 421–422. [Google Scholar] [CrossRef] [Green Version]
- Beebe, D.W. Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr. Clin. North Am. 2011, 58, 649–665. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palmer, C.A. Tired teens: Sleep disturbances and heightened vulnerability for mental health difficulties. J. Adolesc. Health 2020, 66, 520–521. [Google Scholar] [CrossRef]
- Fobian, A.D.; Elliott, L.; Louie, T. A systematic review of sleep, hypertension, and cardiovascular risk in children and adolescents. Curr. Hypertens. Rep. 2018, 20, 42. [Google Scholar] [CrossRef]
- Morrissey, B.; Taveras, E.; Allender, S.; Strugnell, C. Sleep and obesity among children: A systematic review of multiple sleep dimensions. Pediatr. Obes. 2020, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Samuels, M.; Stebbens, V.; Davies, S.; Picton-Jones, E.; Southall, D. Sleep Related upper airway obstruction and hypoxaemia in sickle cell disease. Arch. Dis. Child. 1992, 67, 925–929. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rogers, V.; Marcus, C.; Jawad, A. Periodic limb movements and disrupted sleep in children with sickle cell disease. Sleep 2011, 34, 899–908. [Google Scholar]
- Bruni, O.; Fabrizi, P.; Ottaviano, S.; Cortesi, F.; Giannotti, F.; Guidetti, V. Prevalence of sleep disorders in childhood and adolescence with headache: A case-control study. Cephalalgia 1997, 17, 492–498. [Google Scholar] [CrossRef]
- Gilman, D.; Palermo, T.; Kabbouche, M.; Hershey, A.; Powers, S. Primary headache and sleep disturbances in adolescents. Headache 2007, 47, 1189–1194. [Google Scholar] [CrossRef]
- Vendrame, M.; Kaleyias, J.; Valencia, I.; Legido, A.; Kothare, S. Polysomnographic findings in children with headaches. Pediatr. Neurol. 2008, 39, 6–11. [Google Scholar] [CrossRef]
- Valrie, C.R.; Bromberg, M.H.; Palermo, T.; Schanberg, L.E. A systematic review of sleep in pediatric pain populations. J. Dev. Behav. Pediatr. 2013, 34, 120–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palermo, T.M.; Wilson, A.C.; Lewandowski, A.S.; Toliver-Sokol, M.; Murray, C.B. Behavioral and psychosocial factors associated with insomnia in adolescents with chronic pain. Pain 2011, 152, 89–94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- LeBourgeois, M.K. The relationship between reported sleep quality and sleep hygiene in Italian and American adolescents. Pediatrics 2005, 115, 257–265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palermo, T.M.; Toliver-Sokol, M.; Fonareva, I.; Koh, J.L. Objective and subjective assessment of sleep in adolescents with chronic pain compared to healthy adolescents. Clin. J. Pain 2007, 23, 812–820. [Google Scholar] [CrossRef] [Green Version]
- Lewandowski, A.S.; Palermo, T.M.; De la Motte, S.; Fu, R. Temporal daily associations between pain and sleep in adolescents with chronic pain versus healthy adolescents. Pain 2010, 151, 220–225. [Google Scholar] [CrossRef] [Green Version]
- Palermo, T.; Kiska, R. Subjective sleep disturbances in adolescents with chronic pain: Relationship to daily functioning and quality of life. J. Pain 2005, 6, 201–207. [Google Scholar] [CrossRef]
- Palermo, T.; Fonareva, I.; Janosy, N. Sleep quality and efficiency in adolescents with chronic pain: Relationship with activity limitations and health-related quality of life. Behav. Sleep. Med. 2008, 6, 234–250. [Google Scholar] [CrossRef] [Green Version]
- Chaput, J.-P.; Dutil, C.; Featherstone, R.; Ross, R.; Giangregorio, L.; Saunders, T.J.; Janssen, I.; Poitras, V.J.; Kho, M.E.; Ross-White, A.; et al. Sleep timing, sleep consistency, and health in adults: A systematic review. Appl. Physiol. Nutr. Metab. 2020, 45, S232–S247. [Google Scholar] [CrossRef]
- McGlinchey, E.L.; Harvey, A.G. Risk behaviors and negative health outcomes for adolescents with late bedtimes. J. Youth Adolesc. 2015, 44, 478–488. [Google Scholar] [CrossRef] [Green Version]
- Asarnow, L.D.; McGlinchey, E.; Harvey, A.G. The effects of bedtime and sleep duration on academic and emotional outcomes in a nationally representative sample of adolescents. J. Adolesc. Health 2014, 54, 350–356. [Google Scholar] [CrossRef] [Green Version]
- Gariépy, G.; Doré, I.; Whitehead, R.D.; Elgar, F.J. More than just sleeping in: A late timing of sleep is associated with health problems and unhealthy behaviours in adolescents. Sleep Med. 2019, 56, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Krietsch, K.N.; Chardon, M.L.; Beebe, D.W.; Janicke, D.M. Sleep and weight-related factors in youth: A systematic review of recent studies. Sleep Med. Rev. 2019, 46, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Bates, J.E.; Viken, R.J.; Alexander, D.B.; Beyers, J.; Stockton, L. Sleep and adjustment in preschool children: Sleep diary reports by mothers relate to behavior reports by teachers. Child Dev. 2002, 73, 62–75. [Google Scholar] [CrossRef] [PubMed]
- Yokomaku, A.; Misao, K.; Omoto, F.; Yamagishi, R.; Tanaka, K.; Takada, K.; Kohyama, J. A Study of the association between sleep habits and problematic behaviors in preschool children. Chronobiol. Int. 2008, 25, 549–564. [Google Scholar] [CrossRef] [PubMed]
- McHale, S.M.; Kim, J.Y.; Kan, M.; Updegraff, K.A. Sleep in Mexican-American adolescents: Social ecological and well-being correlates. J. Youth Adolesc. 2011, 40, 666–679. [Google Scholar] [CrossRef] [Green Version]
- Kuo, S.I.-C.; Updegraff, K.A.; Zeiders, K.H.; McHale, S.M.; Umaña-Taylor, A.J.; De Jesús, S.A.R. Mexican American adolescents’ sleep patterns: Contextual correlates and implications for health and adjustment in young adulthood. J. Youth Adolesc. 2015, 44, 346–361. [Google Scholar] [CrossRef]
- Spruyt, K.; Molfese, D.L.; Gozal, D. Sleep duration, sleep regularity, body weight, and metabolic homeostasis in school-aged children. Pediatrics 2011, 127, e345–e352. [Google Scholar] [CrossRef] [Green Version]
- Kjeldsen, J.S.; Hjorth, M.F.; Andersen, R.; Michaelsen, K.F.; Tetens, I.; Astrup, A.; Chaput, J.-P.; Sjödin, A. Short Sleep duration and large variability in sleep duration are independently associated with dietary risk factors for obesity in danish school children. Int. J. Obes. 2014, 38, 32–39. [Google Scholar] [CrossRef]
- Buckhalt, J.A.; El-Sheikh, M.; Keller, P. Children’s sleep and cognitive functioning: Race and socioeconomic status as moderators of effects. Child Dev. 2007, 78, 213–231. [Google Scholar] [CrossRef]
- Lynch-Jordan, A.M.; Sil, S.; Peugh, J.; Cunningham, N.; Kashikar-Zuck, S.; Goldschneider, K.R. Differential changes in functional disability and pain intensity over the course of psychological treatment for children with chronic pain. Pain 2014, 155, 1955–1961. [Google Scholar] [CrossRef] [Green Version]
- Gatchel, R.J.; Peng, Y.B.; Peters, M.L.; Fuchs, P.N.; Turk, D.C. The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychol. Bull. 2007, 133, 581–624. [Google Scholar] [CrossRef] [PubMed]
- Kashikar-Zuck, S. Treatment of children with unexplained chronic pain. Lancet 2006, 367, 380–382. [Google Scholar] [CrossRef]
- Landry, B.W.; Fischer, P.R.; Driscoll, S.W.; Koch, K.M.; Harbeck-Weber, C.; Mack, K.J.; Wilder, R.T.; Bauer, B.A.; Brandenburg, J.E. Managing chronic pain in children and adolescents: A clinical review. PM&R 2015, 7, S295–S315. [Google Scholar] [CrossRef]
- Simons, L.E.; Logan, D.E.; Chastain, L.; Cerullo, M. Engagement in multidisciplinary interventions for pediatric chronic pain: Parental expectations, barriers, and child outcomes. Clin. J. Pain 2010, 26, 291–299. [Google Scholar] [CrossRef] [PubMed]
- Eccleston, C. Chronic pain in adolescents: Evaluation of a programme of interdisciplinary cognitive behaviour therapy. Arch. Dis. Child. 2003, 88, 881–885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hechler, T.; Dobe, M.; Kosfelder, J.; Damschen, U.; Hübner, B.; Blankenburg, M.; Sauer, C.; Zernikow, B. Effectiveness of a 3-week multimodal inpatient pain treatment for adolescents suffering from chronic pain: Statistical and clinical significance. Clin. J. Pain 2009, 25, 156–166. [Google Scholar] [CrossRef]
- Benore, E.; Webster, E.E.; Wang, L.; Banez, G. Longitudinal analysis of patient-reported outcomes from an interdisciplinary pediatric pain rehabilitation program for children with chronic migraine and headache: Headache. Headache J. Head Face Pain 2018, 58, 1556–1567. [Google Scholar] [CrossRef]
- Hechler, T.; Kanstrup, M.; Holley, A.L.; Simons, L.E.; Wicksell, R.; Hirschfeld, G.; Zernikow, B. Systematic review on intensive interdisciplinary pain treatment of children with chronic pain. Pediatrics 2015, 136, 115–127. [Google Scholar] [CrossRef] [Green Version]
- Williams, S.E.; Homan, K.J.; Crowley, S.L.; Pruitt, D.W.; Collins, A.B.; Deet, E.T.; Samuel, N.D.; John, A.; Banner, K.; Rose, J.B. The impact of spatial distribution of pain on long-term trajectories for chronic pain outcomes after intensive interdisciplinary pain treatment. Clin. J. Pain 2020, 36, 181–188. [Google Scholar] [CrossRef]
- Kemani, M.K.; Kanstrup, M.; Jordan, A.; Caes, L.; Gauntlett-Gilbert, J. Evaluation of an Intensive interdisciplinary pain treatment based on acceptance and commitment therapy for adolescents with chronic pain and their parents: A nonrandomized clinical trial. J. Pediatr. Psychol. 2018, 43, 981–994. [Google Scholar] [CrossRef] [Green Version]
- Logan, D.E.; Sieberg, C.B.; Conroy, C.; Smith, K.; Odell, S.; Sethna, N. Changes in sleep habits in adolescents during intensive interdisciplinary pediatric pain rehabilitation. J. Youth Adolesc. 2015, 44, 543–555. [Google Scholar] [CrossRef] [PubMed]
- Claar, R.L.; Walker, L.S. Functional assessment of pediatric pain patients: Psychometric properties of the functional disability inventory. Pain 2006, 121, 77–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sadeh, A.; Sharkey, K.; Carskadon, M. Activity-based sleep-wake identification: An empirical test of methodological issues. Sleep 1992, 17, 201–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blanca, M.; Alarcon, R.; Arnau, J.; Bono, R.; Bendayan, R. Non-normal data: Is ANOVA still a valid option? Psicothema 2017, 29, 552–557. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Paruthi, S.; Brooks, L.J.; D’Ambrosio, C.; Hall, W.A.; Kotagal, S.; Lloyd, R.M.; Malow, B.A.; Maski, K.; Nichols, C.; Quan, S.F.; et al. Recommended amount of sleep for pediatric populations: A consensus statement of the American academy of sleep medicine. J. Clin. Sleep Med. 2016, 12, 785–786. [Google Scholar] [CrossRef]
- Buxton, O.M.; Chang, A.-M.; Spilsbury, J.C.; Bos, T.; Emsellem, H.; Knutson, K.L. Sleep in the modern family: Protective family routines for child and adolescent sleep. Sleep Health 2015, 1, 15–27. [Google Scholar] [CrossRef] [Green Version]
- Kuula, L.; Pesonen, A.-K.; Merikanto, I.; Gradisar, M.; Lahti, J.; Heinonen, K.; Kajantie, E.; Räikkönen, K. Development of late circadian preference: Sleep timing from childhood to late adolescence. J. Pediatr. 2018, 194, 182–189.e1. [Google Scholar] [CrossRef] [Green Version]
- Bei, B.; Byrne, M.L.; Ivens, C.; Waloszek, J.; Woods, M.J.; Dudgeon, P.; Murray, G.; Nicholas, C.L.; Trinder, J.; Allen, N.B. Pilot Study of a mindfulness-based, multi-component, in-school group sleep intervention in adolescent girls: In-school group sleep intervention. Early Interv. Psychiatry 2013, 7, 213–220. [Google Scholar] [CrossRef]
- He, F.; Bixler, E.O.; Liao, J.; Berg, A.; Imamura Kawasawa, Y.; Fernandez-Mendoza, J.; Vgontzas, A.N.; Liao, D. Habitual sleep variability, mediated by nutrition intake, is associated with abdominal obesity in adolescents. Sleep Med. 2015, 16, 1489–1494. [Google Scholar] [CrossRef] [Green Version]
- Doane, L.D.; Gress-Smith, J.L.; Breitenstein, R.S. Multi-method assessments of sleep over the transition to college and the associations with depression and anxiety symptoms. J. Youth Adolesc. 2015, 44, 389–404. [Google Scholar] [CrossRef]
- Tsai, S.-Y.; Labyak, S.E.; Richardson, L.P.; Lentz, M.J.; Brandt, P.A.; Ward, T.M.; Landis, C.A. Brief report: Actigraphic sleep and daytime naps in adolescent girls with chronic musculoskeletal pain. J. Pediatr. Psychol. 2007, 33, 307–311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meltzer, L.J.; Logan, D.E.; Mindell, J.A. Sleep patterns in female adolescents with chronic musculoskeletal pain. Behav. Sleep. Med. 2005, 3, 193–208. [Google Scholar] [CrossRef] [PubMed]
- Borbély, A.A.; Daan, S.; Wirz-Justice, A.; Deboer, T. The two-process model of sleep regulation: A reappraisal. J. Sleep Res. 2016, 25, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Gavriloff, D.; Sheaves, B.; Juss, A.; Espie, C.A.; Miller, C.B.; Kyle, S.D. Sham sleep feedback delivered via actigraphy biases daytime symptom reports in people with insomnia: Implications for insomnia disorder and wearable devices. J. Sleep Res. 2018, 27, e12726. [Google Scholar] [CrossRef] [PubMed]
- Pyper, E.; Harrington, D.; Manson, H. Do parents’ support behaviours predict whether or not their children get sufficient sleep? A cross-sectional study. BMC Public Health 2017, 17, 432. [Google Scholar] [CrossRef] [Green Version]
- Spielman, A.; Saskin, P.; Thorpy, M. Treatment of chronic insomnia by restriction of time in bed. Sleep 1987, 10, 45–56. [Google Scholar] [CrossRef] [Green Version]
- Armoni Domany, K.; Nahman-Averbuch, H.; King, C.D.; Dye, T.; Xu, Y.; Hossain, M.; Hershey, A.D.; Simakajornboon, N. Clinical presentation, diagnosis and polysomnographic findings in children with migraine referred to sleep clinics. Sleep Med. 2019, 63, 57–63. [Google Scholar] [CrossRef]
- Tayag-Kier, C.E.; Keenan, G.F.; Scalzi, L.V.; Schultz, B.; Elliott, J.; Zhao, R.H.; Arens, R. Sleep and periodic limb movement in sleep in Juvenile Fibromyalgia. Pediatrics 2000, 106, e70. [Google Scholar] [CrossRef] [Green Version]
- Yeung, W.K.; Morgan, K.; Mckenna, F. Comparison of sleep structure and psychometric profiles in patients with fibromyalgia, osteoarthritis and healthy controls. J. Sleep Res. 2018, 27, 292–300. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Chan, N.Y.; Lam, S.P.; Li, S.X.; Liu, Y.; Chan, J.W.Y.; Kong, A.P.S.; Ma, R.C.W.; Chan, K.C.C.; Li, A.M.; et al. Emergence of Sex differences in insomnia symptoms in adolescents: A large-scale school-based study. Sleep 2016, 39, 1563–1570. [Google Scholar] [CrossRef] [Green Version]
- Kashikar-Zuck, S.; Flowers, S.; Strotman, D.; Sil, S.; Ting, T.; Schikler, K. Physical activity monitoring in adolescents with Juvenile Fibromyalgia: Findings from a clinical trial of cognitive–behavioral therapy. Pediatr. Rheumatol. 2013, 65, 398–405. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sousa, I.C.; Souza, J.C.; Louzada, F.M.; Azevedo, C.V.M. Changes in sleep habits and knowledge after an educational sleep program in 12th grade students: Sleep education program for adolescents. Sleep Biol. Rhythms 2013, 11, 144–153. [Google Scholar] [CrossRef] [Green Version]
- De Sousa, I.C.; Araújo, J.F.; de Azevedo, C.V.M. The effect of a sleep hygiene education program on the sleep? Wake cycle of brazilian adolescent students. Sleep Biol. Rhythms 2007, 5, 251–258. [Google Scholar] [CrossRef]

| FIRST Patients | Comparison Group | p | |
|---|---|---|---|
| (N = 10) | (N = 9) | ||
| Age (years, mean ± SD) | 15.39 (2.14) | 16.24 (1.49) | 0.33 |
| Sex (% female) | 8 (80%) | 7 (78%) | 0.91 |
| Race (N, %) | 0.28 | ||
| Caucasian | 10 (100%) | 8 (89%) | |
| Bi-racial | 0 (0%) | 1 (11%) | |
| Primary pain location (N, %) | 0.50 | ||
| Widespread musculoskeletal pain | 6 (60%) | 5 (56%) | |
| Localized musculoskeletal pain | 3 (30%) | 1 (11%) | |
| Abdominal pain | 0 (0%) | 2 (22%) | |
| Headache | 1 (10%) | 1 (11%) | |
| Insurance (N, %) | 0.94 | ||
| Commercial | 9 (90%) | 8 (89%) | |
| Medicaid | 1 (10%) | 1 (11%) | |
| Disability (FDI, mean ± SD) | 0.36 | ||
| Time 1 (baseline) a | 35.10 (7.92) | 30.38 (13.17) | |
| Season recruited (N, %) | 0.86 | ||
| Fall | 1 (10%) | 2 (22%) | |
| Winter | 4 (40%) | 3 (33%) | |
| Spring | 3 (30%) | 3 33%) | |
| Summer | 2 (20%) | 1 (11%) | |
| Visits Completed Pre-COVID-19 shutdown b (N, %) | |||
| Time 1 (baseline) | 10 (100%) | 9 (100%) | - |
| Time 2 (final IIPT week or equiv. time) | 7 (70%) | 5 (56%) | 0.52 |
| Time 3 (follow up) | 7 (70%) | 3 (33%) | 0.11 |
| Structured School Attendance (N, %) c | |||
| Time 1 (baseline) | 30% | 33% | 0.88 |
| Time 2 (final IIPT week or equiv. time) | - | 29% | - |
| Time 3 (follow up) | 73% | 18% | 0.05 |
| Number of days between visits d (mean, min–max) | |||
| Time 1 to Time 2 | 40 (9–65) | 59 (38–76) | 0.04 * |
| Time 2 to Time 3 | 50 (26–80) | 58 (50–80) | 0.29 |
| FIRST Program Length in days (mean, ± SD, min–max) | |||
| 20 (5.28; 11–29) | - | - | |
| Post-Study for Clinical Sleep Follow-Up Referral | |||
| Behavioral Sleep Medicine e | 30% | 22% | 0.52 |
| Sleep Medicine f | 30% | 55% | |
| FIRST Patients | Comparison Group | Mean Difference | p | |||
|---|---|---|---|---|---|---|
| Mean (SD) | Min–Max | Mean (SD) | Min–Max | |||
| Sleep Timing: Onset | ||||||
| Average Timing (Clock Time) | ||||||
| Time 1 | 12:17 a.m. (151) | 9:59 p.m.–6:48 a.m. | 11:35 p.m. (53) | 10:12 p.m.–1:15 a.m. | −45 min | 0.14 |
| Time 2 | 10:26 p.m. (29) | 9:23 p.m.–11:06 p.m. | 1:05 a.m. (110) | 11:30 p.m.–4:50 a.m. | 160 min | 0.004 |
| Time 3 | 11:49 p.m. (139) | 10:14 p.m.–5:42 a.m. | 12:49 a.m. (142) | 10:44 p.m.–6:05 a.m. | 60 min | 0.90 |
| Intra-Individual Variability (min) | ||||||
| Time 1 | 76 (33) | 32–136 | 60 (29) | 23–115 | −16 min | 0.62 |
| Time 2 | 29 (15) | 6–60 | 65 (43) | 24–155 | 35 min | 0.03 |
| Time 3 | 50 (20) | 18–78 | 95 (95) | 14–303 | 45 min | 0.01 |
| Sleep Timing: Offset | ||||||
| Average Timing (Clock Time) | ||||||
| Time 1 | 9:04 a.m. (159) | 6:28 a.m.–3:57 p.m. | 8:34 a.m. (70) | 6:28 a.m.–10:22 a.m. | −30 min | 0.29 |
| Time 2 | 7:16 a.m. (28) | 6:42 a.m.–8:02 a.m. | 9:19 a.m. (102) | 7:30 a.m.–12:42 p.m. | 122 min | 0.01 |
| Time 3 | 8:36 a.m. (156) | 6:01 a.m.–2:52 p.m. | 9:49 a.m. (117) | 7:23 a.m.–1:07 p.m. | 73 min | 0.72 |
| Intra-Individual Variability (min) | ||||||
| Time 1 | 90 (62) | 42–241 | 88 (51) | 27–161 | −2 min | 0.99 |
| Time 2 | 21 (5) | 15–35 | 85 (43) | 8–142 | 64 min | 0.002 |
| Time 3 | 73 (50) | 17–164 | 86 (58) | 22–218 | 13 min | 0.94 |
| Sleep Period (Duration) | ||||||
| Average Period (Mean h:min) | ||||||
| Time 1 | 8:49 (60) | 7:05–10:16 | 9:00 (63) | 8:06–10:57 | 11 min | 0.88 |
| Time 2 | 8:52 (43) | 8:06–10:15 | 8:14 (53) | 6:29–9:45 | −38 min | 0.82 |
| Time 3 | 8:49 (59) | 7:26–10:06 | 9:02 (89) | 6:14–11:36 | 13 min | 0.62 |
| Intra-Individual Variability (min) | ||||||
| Time 1 | 107 (65) | 63–277 | 88 (52) | 26–191 | −19 min | 0.88 |
| Time 2 | 35 (17) | 16–70 | 89 (37) | 34–138 | 54 min | 0.01 |
| Time 3 | 76 (32) | 37–125 | 84 (53) | 32–186 | 8 min | 0.12 |
| Sleep Quality | ||||||
| Average Efficiency (%) | ||||||
| Time 1 | 87% (8) | 74–96% | 80% (8) | 64–90% | −7% | 0.23 |
| Time 2 | 86% (8) | 71–94% | 83% (12) | 56–95% | −3% | 0.48 |
| Time 3 | 86% (8) | 74–96% | 80% (12) | 57–94% | −6% | 0.23 |
| Sleep Onset | Sleep Offset | Duration | Sleep Efficiency | |||||||||||||
| df | F | p | Partial eta2 | df | F | p | Partial eta2 | df | F | p | Partial eta2 | df | F | p | Partial eta2 | |
| Between subjects | ||||||||||||||||
| Group | 1 | 1.80 | 0.20 | 0.10 | 1 | 1.58 | 0.23 | 0.09 | 1 | 0.03 | 0.88 | 0.002 | 1 | 1.81 | 0.20 | 0.1 |
| Within subjects | ||||||||||||||||
| Time | 2 | 0.91 | 0.41 | 0.05 | 2 | 2.28 | 0.12 | 0.12 | 2 | 2.05 | 0.13 | 0.11 | 2 | 0.46 | 0.63 | 0.03 |
| Time x Group | 2 | 8.06 | 0.001 * | 0.32 | 2 | 4.49 | 0.02 * | 0.21 | 2 | 2.68 | 0.08 | 0.14 | 2 | 1.19 | 0.32 | 0.07 |
| Sleep Onset Variability | Sleep Offset Variability | Duration Variability | Sleep Efficiency Variability | |||||||||||||
| df | F | p | Partial eta2 | df | F | p | Partial eta2 | df | F | p | Partial eta2 | df | F | p | Partial eta2 | |
| Between subjects | ||||||||||||||||
| Group | 1 | 1.59 | 0.23 | 0.09 | 1 | 1.87 | 0.19 | 0.1 | 1 | 0.82 | 0.38 | 0.05 | 1 | 4.72 | 0.04 * | 0.217 |
| Within subjects | ||||||||||||||||
| Time | 2 | 3.00 | 0.06 * | 0.15 | 2 | 5.65 | 0.01 * | 0.25 | 2 | 4.14 | 0.03 * | 0.20 | 2 | 0.43 | 0.65 | 0.03 |
| Time x Group | 2 | 4.53 | 0.02 * | 0.21 | 2 | 4.69 | 0.02 * | 0.22 | 2 | 4.53 | 0.02 * | 0.21 | 2 | 2.49 | 0.10 | 0.13 |
| Time 2 (Controlling for Time 1) | Time 3 (Controlling for Time 1) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SS | df | MS | F | p | Partial Eta2 | R2 | SS | df | MS | F | p | Partial Eta2 | R2 | |
| Sleep Onset | ||||||||||||||
| T1 Sleep Onset | 9848 | 1 | 9848 | 1.64 | 0.22 | 0.09 | 171422 | 1 | 171422 | 16.61 | 0.00 * | 0.51 | ||
| Group | 128769 | 1 | 128769 | 21.39 | 0.00 * | 0.57 | 0.57 | 42219 | 1 | 42219 | 4.09 | 0.06 | 0.20 | 0.53 |
| Error | 96321 | 16 | 6020 | 165088 | 16 | 10318 | ||||||||
| Sleep Offset | ||||||||||||||
| T1 Sleep Offset | 11543 | 1 | 11543 | 2.37 | 0.14 | 0.13 | 150445 | 1 | 150445 | 13.52 | 0.00 * | 0.46 | ||
| Group | 76883 | 1 | 76883 | 15.76 | 0.00 * | 0.50 | 0.51 | 42727 | 1 | 42727 | 3.84 | 0.07 | 0.19 | 0.50 |
| Error | 78075 | 16 | 4880 | 178038 | 16 | 11127 | ||||||||
| Sleep Onset Variability | ||||||||||||||
| T1 Sleep Onset Var. | 844 | 1 | 844 | 0.83 | 0.38 | 0.05 | 24672 | 1 | 24672 | 7.83 | 0.01 * | 0.33 | ||
| Group | 6634 | 1 | 6634 | 6.56 | 0.02 | 0.29 | 0.29 | 18757 | 1 | 18757 | 5.95 | 0.03 | 0.27 | 0.41 |
| Error | 16181 | 16 | 1011 | 50403 | 16 | 3150 | ||||||||
| Sleep Offset Variability | ||||||||||||||
| T1 Sleep Offset Var. | 4584 | 1 | 4584 | 6.89 | 0.02 * | 0.30 | 19176 | 1 | 19176 | 10.29 | 0.01 * | 0.39 | ||
| Group | 19412 | 1 | 19412 | 29.16 | 0.00 * | 0.65 | 0.69 | 872 | 1 | 872 | 0.47 | 0.50 | 0.03 | 0.40 |
| Error | 10652 | 16 | 666 | 29816 | 16 | 1863 | ||||||||
| Duration Variability | ||||||||||||||
| T1 Sleep Dur Var. | 2258 | 1 | 2258 | 3.19 | 0.09 | 0.17 | 1015 | 1 | 1015 | 0.53 | 0.48 | |||
| Group | 15118 | 1 | 15118 | 21.38 | 0.00 * | 0.57 | 0.58 | 437 | 1 | 437 | 0.23 | 0.64 | 0.01 | 0.04 |
| Error | 11312 | 16 | 707 | 30763 | 16 | 1923 | ||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krietsch, K.N.; Beebe, D.W.; King, C.; Homan, K.J.; Williams, S.E. Sleep among Youth with Severely Disabling Chronic Pain: Before, during, and after Inpatient Intensive Interdisciplinary Pain Treatment. Children 2021, 8, 42. https://doi.org/10.3390/children8010042
Krietsch KN, Beebe DW, King C, Homan KJ, Williams SE. Sleep among Youth with Severely Disabling Chronic Pain: Before, during, and after Inpatient Intensive Interdisciplinary Pain Treatment. Children. 2021; 8(1):42. https://doi.org/10.3390/children8010042
Chicago/Turabian StyleKrietsch, Kendra N., Dean W. Beebe, Christopher King, Kendra J. Homan, and Sara E. Williams. 2021. "Sleep among Youth with Severely Disabling Chronic Pain: Before, during, and after Inpatient Intensive Interdisciplinary Pain Treatment" Children 8, no. 1: 42. https://doi.org/10.3390/children8010042
APA StyleKrietsch, K. N., Beebe, D. W., King, C., Homan, K. J., & Williams, S. E. (2021). Sleep among Youth with Severely Disabling Chronic Pain: Before, during, and after Inpatient Intensive Interdisciplinary Pain Treatment. Children, 8(1), 42. https://doi.org/10.3390/children8010042





