Mindfulness in Adolescent and Young Adult (AYA) Patients Undergoing Hematopoietic Stem Cell Transplantation (HSCT): A Qualitative Study
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Participants and Recruitment
2.3. Data Collection
2.4. Data Analysis
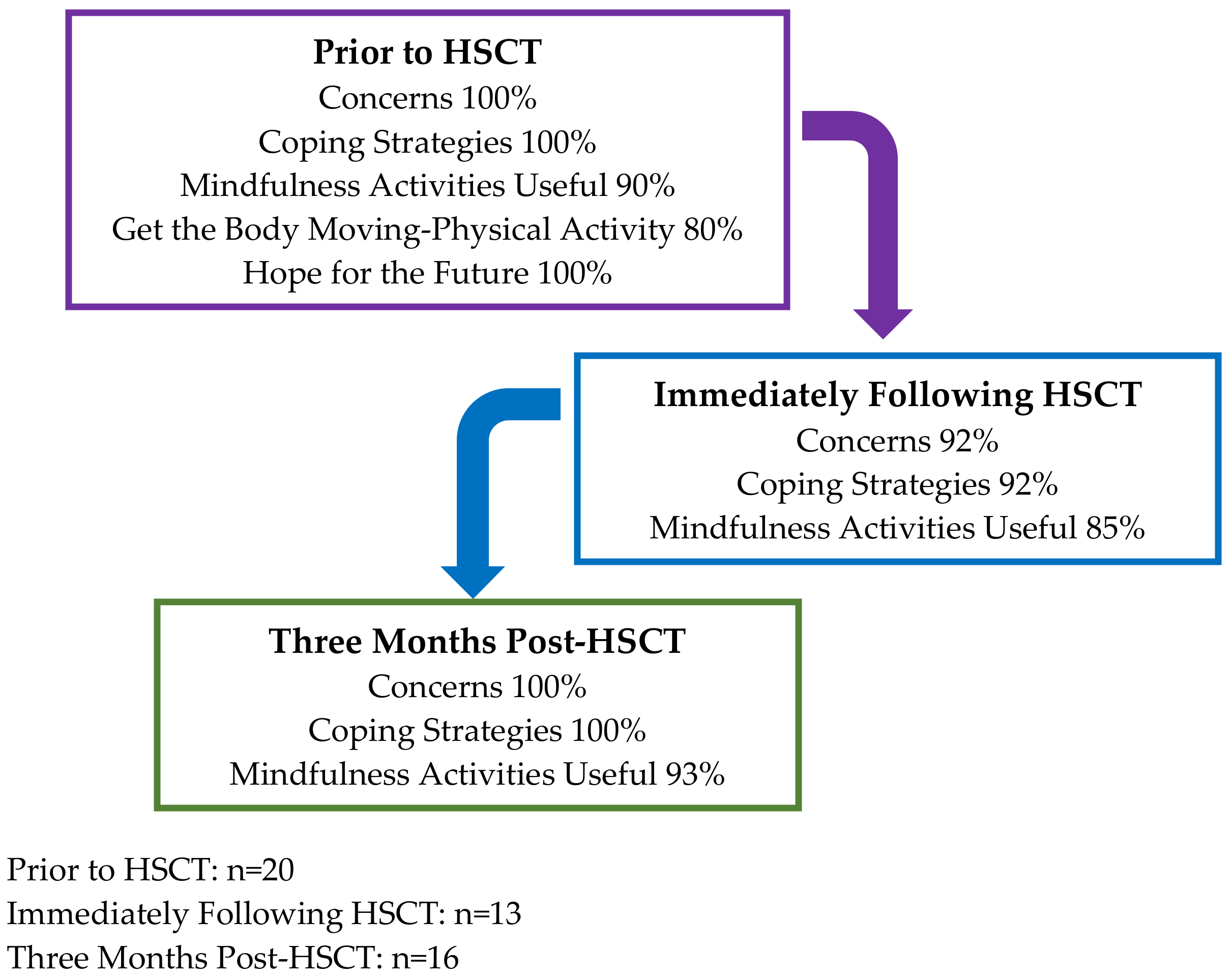
3. Results
3.1. Descriptive Results
3.2. Qualitative Results—Thematic Findings
3.2.1. Timepoint 1: Prior to HSCT
Concerns
Coping Strategies
Mindfulness Activities
Hope for the Future
Getting the Body Moving-Physical Activity
3.2.2. Timepoint 2: Immediately Following HSCT
Concerns
Coping Strategies
Mindfulness Activities
3.2.3. Timepoint 3: Three Months Post HSCT
Concerns
Coping Strategies
Mindfulness Activities
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Cancer Institute. Adolescents and Young Adults with Cancer. Available online: https://www.cancer.gov/types/aya (accessed on 20 April 2022).
- Smith, A.W.; Keegan, T.; Hamilton, A.; Lynch, C.; Wu, X.-C.; Schwartz, S.M.; Kato, I.; Cress, R.; Harlan, L.; AYA HOPE Study Collaborative Group. Understanding care and outcomes in adolescents and young adults with cancer: A review of the AYA HOPE study. Pediatr. Blood Cancer 2018, 66, e27486. [Google Scholar] [CrossRef]
- Mehta, P.A.; Rotz, S.J.; Majhail, N.S. Unique Challenges of Hematopoietic Cell Transplantation in Adolescent and Young Adults with Hematologic Malignancies. Biol. Blood Marrow Transplant. 2018, 24, e11–e19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mathanda, R.R.; Hamilton, B.K.; Rybicki, L.; Advani, A.S.; Colver, A.; Dabney, J.; Ferraro, C.; Hanna, R.; Kalaycio, M.; Lawrence, C.; et al. Quality-of-Life Trajectories in Adolescent and Young Adult versus Older Adult Allogeneic Hematopoietic Cell Transplantation Recipients. Biol. Blood Marrow Transplant. 2020, 26, 1505–1510. [Google Scholar] [CrossRef] [PubMed]
- Saba, N.; Abraham, R.; Keating, A. Overview of autologous stem cell transplantation. Crit. Rev. Oncol. 2000, 36, 27–48. [Google Scholar] [CrossRef]
- Molassiotis, A.; Morris, P. Suicide and suicidal ideation after marrow transplantation. Bone Marrow Transplant. 1997, 19, 87–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolcott, D.L.; Fawzy, F.I.; Wellisch, D.K. Psychiatric aspects of bone marrow transplantation: A review and current issues. Psychiatr. Med. 1986, 4, 299–317. [Google Scholar]
- Belec, R.H. Quality of life: Perceptions of long-term survivors of bone marrow transplantation. Oncol. Nurs. Forum 1992, 19, 31–37. [Google Scholar]
- Jenkins, P.L.; Linington, A.; Whittaker, J.; Path, F. A Retrospective Study of Psychosocial Morbidity in Bone Marrow Transplant Recipients. J. Psychosom. Res. 1991, 32, 65–71. [Google Scholar] [CrossRef]
- Horton-Deutsch, S.; Day, P.O.; Haight, R.; Babin-Nelson, M. Enhancing mental health services to bone marrow transplant recipients through a mindfulness-based therapeutic intervention. Complement. Ther. Clin. Pract. 2007, 13, 110–115. [Google Scholar] [CrossRef]
- Mehta, R.S.; Rezvani, K. Immune reconstitution post allogeneic transplant and the impact of immune recovery on the risk of infection. Virulence 2016, 7, 901–916. [Google Scholar] [CrossRef] [Green Version]
- Creswell, J.D. Mindfulness Interventions. Annu. Rev. Psychol. 2017, 68, 491–516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peterson, L.G.; Pbert, L. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am. J. Psychiatry 1992, 149, 936–943. [Google Scholar] [CrossRef]
- Cladder-Micus, M.B.; Speckens, A.E.; Vrijsen, J.N.; Donders, A.R.T.; Becker, E.S.; Spijker, J. Mindfulness-based cognitive therapy for patients with chronic, treatment-resistant depression: A pragmatic randomized controlled trial. Depress. Anxiety 2018, 35, 914–924. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Knill, K.; Warren, B.; Melnyk, B.; Thrane, S.E. Burnout and Well-Being: Evaluating Perceptions in Bone Marrow Transplantation Nurses Using a Mindfulness Application. Clin. J. Oncol. Nurs. 2021, 25, 547–554. [Google Scholar] [CrossRef] [PubMed]
- Compernolle, M.C.; Sledge, J.A. Effects of a Mindfulness Intervention on Hospitalized Patients With Hematologic Malignancies and Their Caregivers. Oncol. Nurs. Forum 2020, 47, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Donovan, E.; Martin, S.R.; Seidman, L.C.; Zeltzer, L.K.; Cousineau, T.M.; A Payne, L.; Trant, M.; Weiman, M.; Knoll, M.; Federman, N.C. A Mobile-Based Mindfulness and Social Support Program for Adolescents and Young Adults With Sarcoma: Development and Pilot Testing. JMIR mHealth uHealth 2019, 7, e10921. [Google Scholar] [CrossRef]
- Van Der Gucht, K.; Takano, K.; Labarque, V.; Vandenabeele, K.; Nolf, N.; Kuylen, S.; Cosyns, V.; Van Broeck, N.; Kuppens, P.; Raes, F. A Mindfulness-Based Intervention for Adolescents and Young Adults After Cancer Treatment: Effects on Quality of Life, Emotional Distress, and Cognitive Vulnerability. J. Adolesc. Young-Adult Oncol. 2017, 6, 307–317. [Google Scholar] [CrossRef]
- Pathrose, S.P.; Everett, B.; Patterson, P.; Ussher, J.; Salamonson, Y.; McDonald, F.; Biegel, G.; Ramjan, L. Mindfulness-Based Interventions for Young People With Cancer. Cancer Nurs. 2021, 44, 349–360. [Google Scholar] [CrossRef]
- Lewis, A.; Oppenheim, A. Questionnaire Design, Interviewing and Attitude Measurement, London, Pinter. Pp 303. £14.99 paperback, £39.50 hardback. J. Community Appl. Soc. Psychol. 1994, 4, 371–372. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Dedoose Version 9.0.17. A Web Application for Managing, Analyzing, and Presenting Qualitative and Mixed Method Research Data. Available online: www.dedoose.com (accessed on 20 April 2022).
- Vinci, C.; Pidala, J.; Lau, P.; Reblin, M.; Jim, H. A mindfulness-based intervention for caregivers of allogeneic hematopoietic stem cell transplant patients: Pilot results. Psycho-Oncology 2020, 29, 934–937. [Google Scholar] [CrossRef] [PubMed]
- Vinci, C.; Reblin, M.; Jim, H.; Pidala, J.; Bulls, H.; Cutolo, E. Understanding preferences for a mindfulness-based stress management program among caregivers of hematopoietic cell transplant patients. Complement. Ther. Clin. Pract. 2018, 33, 164–169. [Google Scholar] [CrossRef]
- Grossman, P.; Zwahlen, D.; Halter, J.P.; Passweg, J.R.; Steiner, C.; Kiss, A. A mindfulness-based program for improving quality of life among hematopoietic stem cell transplantation survivors: Feasibility and preliminary findings. Support. Care Cancer 2014, 23, 1105–1112. [Google Scholar] [CrossRef] [PubMed]
- Bauer-Wu, S.; Sullivan, A.M.; Rosenbaum, E.; Ott, M.J.; Powell, M.; McLoughlin, M.; Healey, M.W. Facing the Challenges of Hematopoietic Stem Cell Transplantation With Mindfulness Meditation: A Pilot Study. Integr. Cancer Ther. 2008, 7, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Duong, N.; Davis, H.; Robinson, P.D.; Oberoi, S.; Cataudella, D.; Culos-Reed, S.N.; Gibson, F.; Gotte, M.; Hinds, P.; Nijhof, S.L.; et al. Mind and body practices for fatigue reduction in patients with cancer and hematopoietic stem cell transplant recipients: A systematic review and meta-analysis. Crit. Rev. Oncol. Hematol. 2017, 120, 210–216. [Google Scholar] [CrossRef] [PubMed]
| Participant Characteristics | n = 20 (%) |
|---|---|
| Age: mean ± SD [range], years | 29.8 ± 5.6 [23.0–39.0] |
| BMI: mean ± SD [range] | 28.4 ± 6.08 [17.5–45.0] |
| Sex: n (%) female | 9 (45.0) |
| Ethnicity: n (%) non-Hispanic | 15 (75.0) |
| Race: n (%) | |
| White | 15 (75.0) |
| Black | 2 (10.0) |
| Filipino | 1 (5.0) |
| Other | 2 (10.0) |
| Diagnosis: n (%) | |
| a T-NHL | 3 (15.0) |
| b AML | 4 (20.0) |
| Germ cell tumor | 2 (10.0) |
| Hodgkin lymphoma | 6 (30.0) |
| c B-NHL | 1 (5.0) |
| d B-ALL | 4 (20.0) |
| Conditioning chemo: n (%) | |
| Myeloablative | 17 (85.0) |
| Reduced intensity | 3 (15.0) |
| Conditioning: n (%) | |
| BEAM | 7 (35.0) |
| FluBu5300 | 4 (20.0) |
| FluBu3500 | 2 (10.0) |
| FluMel | 1 (5.0) |
| Carbo-VP16 | 2 (10.0) |
| CyTBI | 2 (10.0) |
| FluTBI | 2 (10.0) |
| Transplant number: n (%) | |
| First transplant | 17 (85.0) |
| Second transplant | 3 (15.0) |
| Transplant type: n (%) | |
| Autologous | 9 (45.0) |
| Allogenic | 11 (55.0) |
| Timepoint #1 (Prior to HSCT) | ||
|---|---|---|
| Code | Description | Study ID, Patient’s Sex: Example Quote |
| Theme 1: Concerns | ||
| Treatment anxiety | Nervousness, anxiety, worry, or stress | 0003, Female: But. I’m nervous about the chemo, because they said it was 10 times stronger than my last one. |
| 0002, Male: I’m feeling nervous and scared. But I just want to get it over with. | ||
| Home responsibilities | Worried about home responsibilities including children | 0004, Male: More scared for my son because he’s five and he doesn’t really grasp—that I’m gonna be away from a while… he gets home and he doesn’t see me, and then you know the day keeps on going, he’s not really, he’s not seeing me, he’s just seeing me through FaceTime. |
| 0010, Female: The most I’m worried about is my daughter. I have a one-year-old. So, being away from her for any amount of time is too much for me. But I’ve got to do what I’ve got to do. | ||
| Isolation | Any report of being alone, feeling lonely, or the need to connect with individuals of similar age | 0017, Male: The only thing I’m worried about, like I said, is being bored and away from family and friends that long. |
| Theme 2: Coping Strategies | ||
| Friends/family | Seek social support from friends or family members | 0011, Female: My closest friend I would say just listens to me and I can just go on a tangent and it’s like nothing I say is too scary and she doesn’t get uncomfortable. |
| Activities to stay busy at hospital | Hospital activities | 0003, Female: I got a bunch of stuff to take with me, like movies and coloring books. |
| 0011, Female: In the hospital… we watch a lot of Netflix and just stuff like that. Or I brought my switch and played Animal Crossing. | ||
| Activities to stay busy at home | Home activities | 0011, Female: Yeah, I bake a lot at home. It’s like my core routine hobby. So, I feel like that’s been very therapeutic for me. |
| Social Networking | Interest or disinterest in social networking platforms | 0004, Male: With other people that have been going through the same thing… yeah, I would be interested in it [social networks]. |
| Extra activities | Medications, seeking professional help, etc. | 0002, Male: Just cry it out. |
| 0011, Female: Well, I have Zoloft prescription and that helps a lot I feel like. And I just do things that I know help me. I will read or I write. I journal. I do a lot of that. And maybe like mindfulness stuff. Or if I can’t sleep, I use the calm app. | ||
| 0010, Female: I smoke a lot of weed. | ||
| Theme 3: Hope for the Future | ||
| Positive mindset | Using positive thinking | 0004, Male: And just gotta think of the future… it’s on my heart… My way of positive thinking is just thinking of the goals I want to do… because you know, be able to give other feedback on what worked, what didn’t work. |
| Avoidance of cancer thoughts | Avoid thinking of the treatment, cancer, or diagnosis | 0003: Male: Not sitting at home is the best thing. Because then you think about everything [cancer]. |
| Getting back to “normal” | Discussion of life returning to pre-diagnosis life | 0004, Male: When I get back and just, this is what was placed in my hands to defeat… hopefully I’ll be able to do the things that I’ve been doing. |
| Theme 4: Mindfulness Activities | ||
| Awareness of mindfulness | Discussion of being aware or unaware of the term mindfulness | 0011, Female: I associate it, I guess, mainly with taking time to yourself to reflect and relax or ease your mind. |
| 0018, Male: No, you would have to educate me on it. | ||
| 0014, Male: Kinda perhaps meditation, or just being able to get into your own thoughts… something mindful, you know? | ||
| Tried mindfulness | Discussion of trying or not trying mindfulness activities | 0011, Female: Yeah… I do the Calm app and sometimes I’ll do a little meditation on YouTube or Calm. It’s not every day, but I try to do it when I feel I need it. |
| Interest in mindfulness | Discussion of interest in mindfulness activities | 0004, Male: Yoga. More chemo patients who are, maybe it’s a little slower, it’s a little—trying to do the stance, the praying mantis stance. You know? Stuff like that. |
| Barriers to mindfulness | Potential barriers to mindfulness activities | 0002, Male: Yeah. It’s also the hardest here [hospital], I think. When I’m at home, or somewhere else, I can put this [cancer] away. But when I’m here [hospital], it’s in your face. |
| Theme 5: Getting the Body Moving—Physical Activity | ||
| Motivation for physical activity pre-treatment | Motivation or lack of for physical activity | 0022, Male: I really enjoy walking a lot. And that’s something that I found I like doing. I think it’s a good thing for your body. And I think it just gets you out there moving and everything. |
| 0013, Female: I want to be active… I have a two-year-old. I mean, there’s no getting around being active when there’s a two-year-old running around your house. | ||
| Motivation for physical activity pre-cancer | Activity level prior to cancer diagnosis | 0002, Male: I usually do a lot of physical activities which I’ve had to cut back on. |
| Physical activity barriers | Barriers/challenges for physical activity | 0004, Male: Like just walking to the restroom from the bed, is really challenging. |
| Timepoint #2 (Immediately after HSCT) | ||
| Code | Description | Study ID, Patient’s Sex: Example Quote |
| Theme 1: Concerns | ||
| Procedure anxiety | Description of feeling nervous or anxious before or during procedure | 0016, Female: I was kind of nervous about the new cells not engrafting mostly. I think that’s the only thing I was really worried about |
| 0004, Female: … You never know what’s gonna happen when you have like tubes plugged into you | ||
| 0010, Female: I was a little anxious because I didn’t know how it was going to go. | ||
| Appearance | Discussion of appearance changes from cancer or procedure | 0010, Female: Like today, I was a little upset because, I don’t know if you guys noticed, but I don’t have hair anymore. So, as a female, not having hair is a pretty big deal, it gets to me sometimes |
| 0012, Female: I’ve definitely noticed changes in my physical being, with my skin. On my face, I have got this pigment issue going on. It has become a little more prominent | ||
| Isolation | Feeling or not feeling isolated or bored in the hospital | 0010, Female: Well, I was in isolation so I couldn’t leave my room for three weeks. |
| 0013, Female: I didn’t feel isolated at all. There were cards and things coming to the hospital every day and, again, people reaching out every day | ||
| Unknown future | Fear of the future—recurrence, comorbidities, negative health outcomes, etc. | 0004, Female: you don’t really know how you’re gonna turn out because they talk about graft versus host disease, where can’t walk afterwards |
| 0005, Female: I don’t know what could happen, and if anything happens, I have to get rushed to a hospital | ||
| Theme 2: Coping Strategies | ||
| Positive thinking | Using positive mindset during and after procedure | 0003, Male: I just went in there as positive as I could, hoping for the best |
| Getting back to normal | Discussion of getting through the procedure to get back to normalcy, away from cancer | 0004, Female: I just want to get it done and get back to whatever a normal life is these days |
| 0010, Female: there are a ton of rules, so I need to stay focused and heal to get better and back to normal | ||
| Staying busy | Discussion of staying busy and distracted while in hospital | 0011, Female: I would say just trying to keep as busy as I could in the hospital. My mom and I would section off our time |
| 0015, Male: Watched Netflix, called family members, walked and talked to people, video games, movies, and books | ||
| Family/friends | Any mention of friends and family being a coping/relief during and after transplant | 0005, Female: I had my husband by my side, it was very nice |
| 0010, Female: [Family/friends say] You’re beautiful, don’t worry about it. It’s just hair, it’s gonna grow back, girl. We’re here for you, God got you. They’ve been very supportive, very loving people. And I appreciate it. | ||
| Theme 3: Mindfulness Activities | ||
| Mindfulness in hospital | Discussion of using mindfulness in hospital | 0003, Male: [I] meditated in hospital with my step-mom, first time trying it. Meditated for about 15 min. |
| 0005, Female: I used the calm app to sleep some in the hospital because you’re constantly being woken up. | ||
| 0011, Female: My mom and I did a little mindfulness meditation on the TV screen when we were in the hospital, and I just had a scan the other day, and I listened to a meditation when I was waiting before because I get stressed. | ||
| Useful strategy | Timing of mindfulness to be most useful | 0012, Female: Probably [immediately] after, just because during the transplant, there’s a lot that goes on. And there’s a lot—I mean, when you’re there—I mean, you get—I mean, it’s daily, you get people coming in. |
| 0010, Female: [I] would say it’s very useful because the—well, not me, because you know I’m awesome—but the anxiety that you get going into something that you really don’t know much about, like bone marrow transfusion | ||
| Interest in mindfulness | Interest or disinterest in mindfulness | 0013, Female: I wish you guys were already doing the program because I do think it would’ve been helpful during to do some kind of guided program where somebody was actually kind of talking you through how to stay in the moment, especially leading up to the transplant. |
| 0014, Male: I’d say it’s useful, yeah, just being aware of staying focused on what you can handle at the given time and not, like you said, if it’s good or bad. | ||
| Improve engagement | Discussion of ways to improve engagement and attendance in a mindfulness program | 0012, Female: I guess just stats to see how—just to knowing how it goes better, other people and if there were doctors who had said, “Yeah, this percentage of people are more successful in their healing, than these people who didn’t.” |
| Timepoint #3 (Three Months Post HSCT) | ||
| Code | Description | Study ID, Patient’s Sex: Example Quote |
| Theme 1: Concerns | ||
| Post-hospitalization anxiety | Description of feeling nervous or anxious post procedure | 0005, Male: Honestly, yes. A little uncertainty. I mean, driving on the way here, my neck started hurting a little bit and I started feeling around and I felt like a small lymph node. |
| 0013, Male: Good. I mean, it was getting rough the last couple of weeks before I went home. I think that was the hardest. The two hard periods, I think were days three to 11 when I had mucositis really bad because I couldn’t really talk much, and it was painful and you’re by yourself at the hospital and that was rough. | ||
| Isolation after discharge | Feeling or not feeling isolated or bored after discharge | 0011, Male: It was suffocating almost just because it’s like you can’t go anywhere or do anything. I mean, the pandemic is partially because of that. But yeah, and I just felt uncomfortable walking around, outside the hotel just because I was like people aren’t wearing their masks outside and which, I guess it’s okay. But I didn’t feel safe, just because I’m a newborn basically. So, it was just weird. Weird is the best way to put it. Yeah. |
| 0002, Male: Yeah. So, like, most—cause I stayed at a hotel, and I, kind of, got, not lazy, but, like, I didn’t do much at all. So, I just, like, felt miserable, so I was just, like, stayed miserable. So, I wish I would have, like, kind of, tried to do—be a little more active, I guess. | ||
| Unknown future after discharge | Fear of the future— recurrence, comorbidities, COVID-19 fears, and negative health outcomes after hospitalization | 0019, Male: It was a painful three months of being in the hospital, and then having to stay local for a while. I was always worried about it, but it did its job. |
| 0020, Female: Oh my god, am I going to make it? What happens if I don’t? My son will get cheated out of having his mom. | ||
| Theme 2: Coping Strategies | ||
| Positive thinking after discharge | Using a positive mindset after hospitalization | 0006, Female: Like I said, I always tell myself, “You’re doing good. You got this. Don’t beat yourself up over small things.” |
| 0007, Male: Just trying to stay positive and just trying to look at the end of the tunnel or the end of the road. | ||
| Getting back to normal after discharge | Discussion of getting through the treatment to get back to normalcy, away from cancer post hospitalization | 0005, Male: Pretty good. I’d say the biggest thing is I feel normal now. It’s just we still have to pump the breaks on everything, cause even though I feel good I’m still really not there yet. |
| 0012, Female: Pretty Good. I mean, it does suck that I have to stay isolated from everybody and everything. But it is nice to at least be one step closer to, to getting back into my normal life and being able to actually see people, have friends stop by of course, making sure that they’re yeah, nobody’s sick and they’re sanitizing and whatnot. | ||
| Staying busy after discharge | Using different resources to stay busy, mention of staying busy/distracted when discharged and out of the hospital | 0004, Male: Oh. I just tried to keep busy. |
| 0006, Female: Having my smart phone and having the iPad. I have a Pinterest account. You’re a girl; I’m sure you’re familiar with Pinterest. I sat on Pinterest usually all day long, Facebook. | ||
| 0011, Male: I feel like blocking the day was what my mom and I did. And it was nice to have some sort of routine when we were in the hospital specifically. So, they want you to do so many labs in a day. So, we would break up our walking time. We’d watch Netflix for a little and then we’d go and do two or three laps and then we’d come back and eat lunch and then do this and then, go back out for a couple of labs. | ||
| Support system post HSCT | Any mention of friends and family being a coping/relief during and after transplant and after discharge | 0003, Female: I would say talk with my daughter a lot. |
| 0012, Female: For coping, I mean, really all I did, I had my mom with me, so, we would just talk. She’s always been my support system. | ||
| 0020, Female: A lot of FaceTime. A lot of FaceTime, that helps. I call my son at least two or three times in a day just to talk to him. And my husband stops up on his breaks. So, yeah. Plus, I have my aunt and uncle here, and we’re always joking and talking. And we’re always together. | ||
| Social Networking | Interest or disinterest in social media platforms to form social connections | 0003, Female: I have some on Instagram, and you just write back and forth with them. I think it’s My Cancer Patient or something on there, and a lot of people connect with everybody on there. We’ve done tell your stories and quite a few things and help each other out with all of it. And I’ve met a lot of people on there that actually have the same thing that I did. |
| 0016, Female: Probably just social media and being on my phone. | ||
| Physical activity | Discussion of using physical activity to cope post transplant and after discharge | 0013, Male: I’ve done two scenic rides so far because Sarah, the nurse practitioner said maybe start with just the scenic ride so you can go slow and get your legs underneath you. |
| 0018, Male: Well, my stress reliever has always been the lifting. I have dropped belly fat. I no longer have a dad bod, so I’m trying and that’s always my main thing is, well how do I cope with stress is just weightlifting, working, and just being around friends and family. That’s really all you can do. | ||
| Reflection of Coping Methods | Any mention of changing or not changing coping methods while staying in hospital | 0004, Male: Oh just keep in mind that you gotta stay busy while you’re in there. You got to keep your mind busy while you’re in there. |
| 0006, Female: No. I’m 31 years old. I’m young. I have two kids. So, of course I was stressed not being with them. But there’s nothing you can do. You just gotta go with the flow. I was scared at times, but that’s what Ativan is for. They give it to cancer patients. And if I was full of anxiety that day, I took an Ativan. You have to take advantage of the prescriptions that they provide for you. | ||
| Theme 3: Mindfulness Activities | ||
| Mindfulness after hospitalization | Any discussion of using mindfulness after hospitalization and post treatment | 0006, Female: I’m a high energy person, so I try practicing mindfulness. I did some Zoom calls with a psychologist, and she tried telling me about the breathing exercises. |
| 0015, Male: Meditate. It was pretty good. It’s very relaxing. | ||
| Useful strategy post HSCT | Timing of mindfulness to be most useful | 0003, Female: I just think that I should probably do it again, actually, because it helped me a lot with my stress. But now that I’m with my daughter, I really don’t have any stress. In the hospital, I did, but now that I’m out and it’s over and everything’s alright, now I really—the scary part’s over with basically. |
| 0015, Male: I use it every once in a while, since we’re not going nowhere. | ||
| 0019, Male: For me, I would say after, but I guess it really depends on the person. When I was in the hospital, I wasn’t in the mood to do anything other than lay in my bed, and order food, and just watch TV, and just to bypass all this time. But after being out and being able to sort of get back to my life, I’ve thought about it before, but I haven’t really gotten to it, yet I guess. | ||
| Interest in mindfulness post HSCT | Interest or disinterest in mindfulness post discharge | 0005, Male: I mean, I definitely think that just by—for example, earlier today when I started having that moment where I was kind of spiraling for a little bit, I definitely think that taking a moment to just focus on your breathing or something can really kind of slow that down and maybe help you snap out of it and not start downward spiraling. |
| 0014, Male: Yeah, it might just force me to sit there and really think through something without getting distracted or without moving onto something else before you really give something enough time. | ||
| 0014, Male: Probably less useful now that I’m kind of back on a more normal routine. But it’s tough to say. I’d say if treatment was completely done and everything was just moving forward, then I think I would be fine, but who knows. | ||
| Improve engagement post HSCT | Discussion of ways to improve engagement and attendance in a mindfulness program | 0004, Male: The possibility of time, different times, scheduling. |
| 0002, Male: Well, mostly because I don’t—I don’t live out there. So, it’s, like, two–and–a–half–hour drive. But, you know, when I am there—I don’t know, I just—I’m afraid I’m going to run into a bunch of old people. | ||
| Mindfulness reflection | Any mention of mindfulness being a useful strategy as they reflect on cancer continuum | 0003, Female: Oh, okay. It probably would help me, but I was just so nervous the whole time and it was just a lot to take in. |
| 0012, Female: Yeah. Well, when it comes to meditation and being self-aware of your problems and your emotions, it’s definitely important to first be aware. I’ve usually been the type to figure out ways around depression or anxiety usually just by staying optimistic. I definitely feel like it’d be like having the time to reflect whether it’s during meditation or yoga. Being able to put aside that that time for yourself is very important. I definitely would like to get into yoga. I think that would be healthy. | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Crowder, S.L.; Sauls, R.; Redwine, L.; Nieder, M.; Albanyan, O.; Yasin, H.; Khimani, F.; Stern, M. Mindfulness in Adolescent and Young Adult (AYA) Patients Undergoing Hematopoietic Stem Cell Transplantation (HSCT): A Qualitative Study. Cancers 2022, 14, 2760. https://doi.org/10.3390/cancers14112760
Crowder SL, Sauls R, Redwine L, Nieder M, Albanyan O, Yasin H, Khimani F, Stern M. Mindfulness in Adolescent and Young Adult (AYA) Patients Undergoing Hematopoietic Stem Cell Transplantation (HSCT): A Qualitative Study. Cancers. 2022; 14(11):2760. https://doi.org/10.3390/cancers14112760
Chicago/Turabian StyleCrowder, Sylvia L., Rachel Sauls, Laura Redwine, Michael Nieder, Omar Albanyan, Hassaan Yasin, Farhad Khimani, and Marilyn Stern. 2022. "Mindfulness in Adolescent and Young Adult (AYA) Patients Undergoing Hematopoietic Stem Cell Transplantation (HSCT): A Qualitative Study" Cancers 14, no. 11: 2760. https://doi.org/10.3390/cancers14112760






