Are There Any Cognitive and Behavioral Changes Potentially Related to Quarantine Due to the COVID-19 Pandemic in People with Mild Cognitive Impairment and AD Dementia? A Longitudinal Study
Abstract
:1. Introduction
Aim of the Study
2. Methods
2.1. Participants
2.2. Procedure
2.3. Ethics
2.4. Data Analysis
3. Results
3.1. Descriptive Statistics
3.2. The Effects of Diagnostic Group and ‘Deterioration Difference’ on Cognition, Everyday Functioning, Affect and Behavior
3.2.1. General Cognitive Status (MMSE, MoCA)
3.2.2. Activities of Daily Living—Everyday Functioning (FUCAS)
3.2.3. Mood and Behavioral Tests (SAST and NPI)
3.2.4. Tests Measuring Short-Term Memory and Visual Perception (RAVLT, 1st Trial; RCFT, Copy Trial)
3.2.5. Test Measuring Verbal Learning (RAVLT, 5th Trial)
3.2.6. Tests Measuring Visual and Verbal Long-Term Memory (RAVLT, Delayed Recall; RCFT, Delayed Recall)
3.2.7. Tests Measuring Verbal Fluency and Executive Function
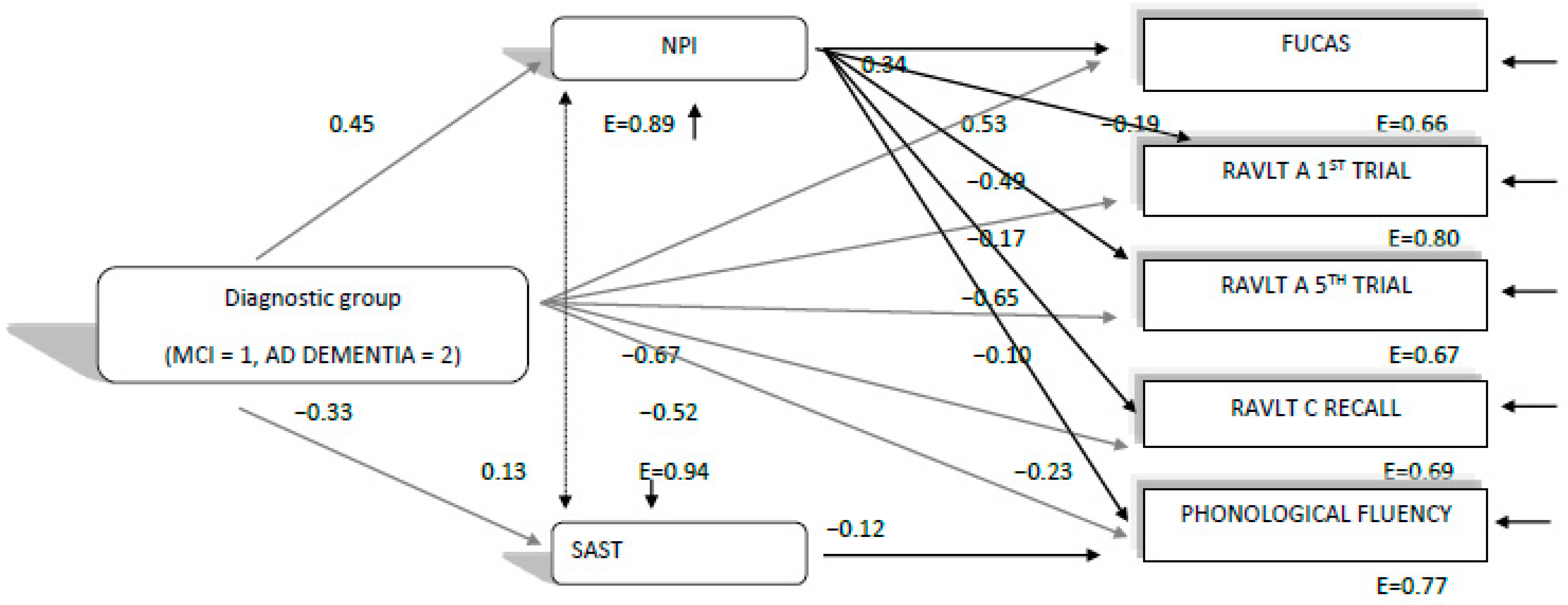
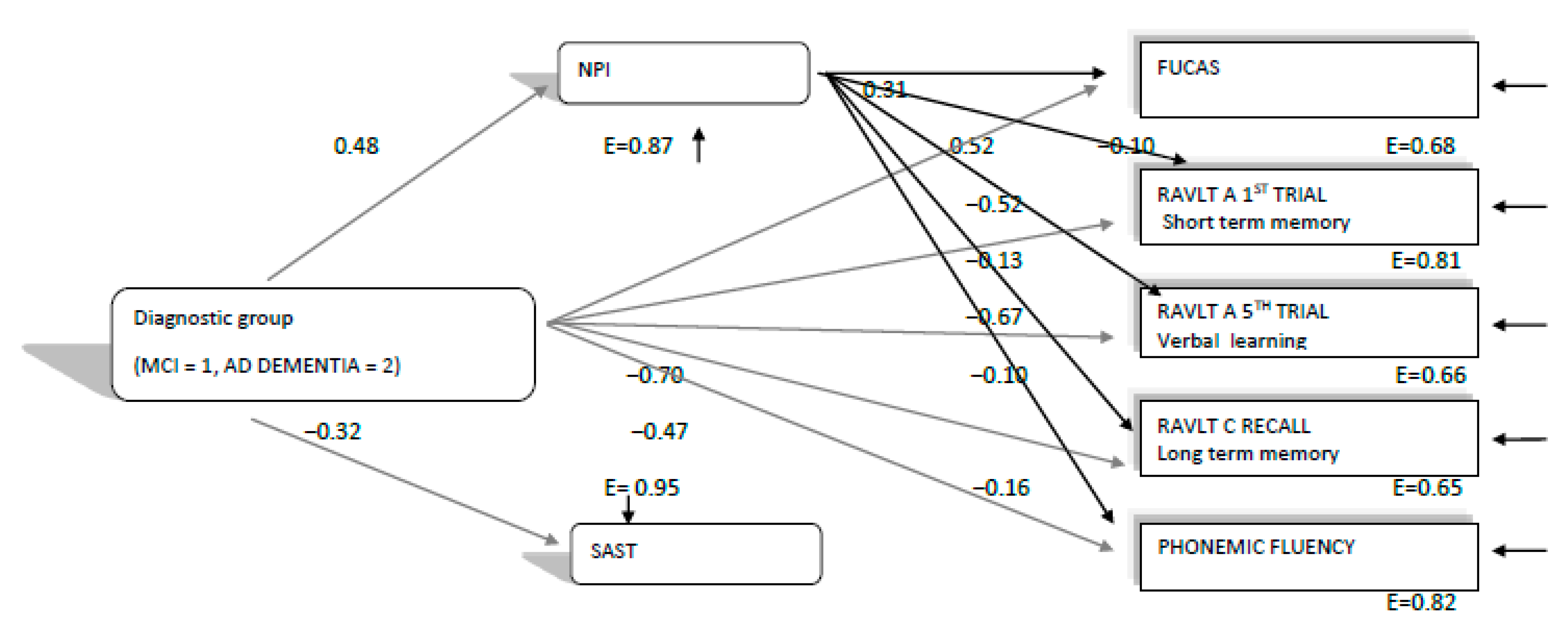
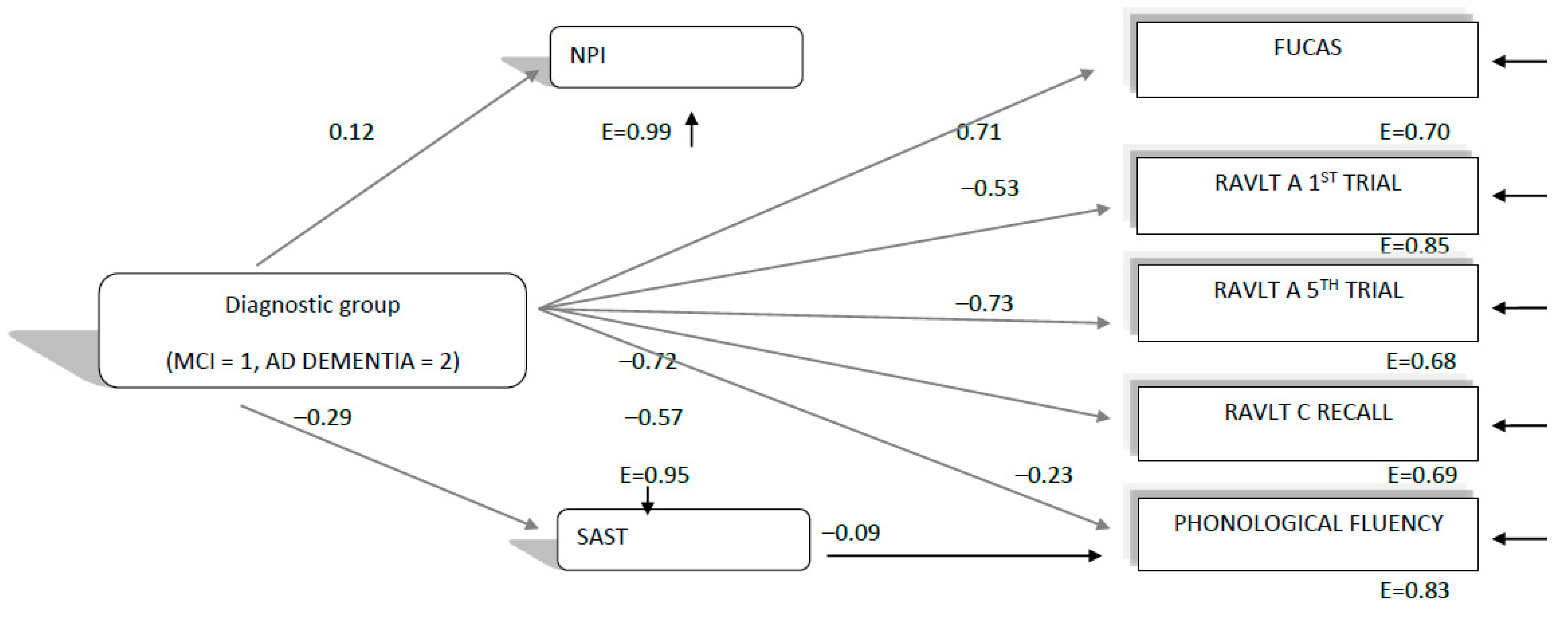
3.3. The Directed Relationships between Diagnostic Group, Mood, Behavioral, Cognitive and Everyday Functioning Performance in 2020 (during the Lockdowns), 2019 and 2018 Neuropsychological Assessments
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef]
- Bianchetti, A.; Rozzini, R.; Guerini, F.; Boffelli, S.; Ranieri, P.; Minelli, G.; Bianchetti, L.; Trabucchi, M. Clinical Presentation of COVID-1919 in Dementia Patients. J. Nutr. Health Aging 2020, 24, 560–562. [Google Scholar] [CrossRef]
- Hawryluck, L.; Gold, W.L.; Robinson, S.; Pogorski, S.; Galea, S.; Styra, R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004, 10, 1206–1212. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Henry, B.M.; Bovo, C.; Sanchis-Gomar, F. Health risks and potential remedies during prolonged lockdowns for coronavirus disease 2019 (COVID-19). Diagnosis 2020, 7, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Fofana, N.K.; Latif, F.; Sarfraz, S.; Bashir, M.F.; Komal, B. Fear and agony of the pandemia leading to stress and mental illness: An emerging crisis in the novel coronavirus (COVID-19) outbreak. Psychiatry Res. 2020, 291, 113230. [Google Scholar] [CrossRef] [PubMed]
- Brown, E.E.; Kumar, S.; Rajji, T.K.; Pollock, B.G.; Mulsant, B.H. Anticipating and Mitigating the Impact of the COVID-19 Pandemia on Alzheimer’s Disease and Related Dementias. Am. J. Geriatr. Psychiatry 2020, 28, 712–721. [Google Scholar] [CrossRef] [PubMed]
- Cagnin, A.; Di Lorenzo, R.; Marra, C.; Bonanni, L.; Cupidi, C.; Laganà, V.; Rubino, E.; Vacca, A.; Provero, P.; Isella, V.; et al. Behavioral and psychological effects of coronavirus disease-19 quarantine in patients with dementia. Front. Psychiatry 2020, 11, 916. [Google Scholar] [CrossRef]
- Velayudhan, L.; Aarsland, D.; Ballard, C. Mental health of people living with dementia in care homes during COVID-19 pandemia. Int. Psychogeriatr. 2020, 32, 1253–1254. [Google Scholar] [CrossRef]
- Leigh-Hunt, N.; Bagguley, D.; Bash, K.; Turner, V.; Turnbull, S.; Valtorta, N.; Caan, W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 2017, 152, 157–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santini, Z.I.; Jose, P.E.; Cornwell, E.Y.; Koyanagi, A.; Nielsen, L.; Hinrichsen, C.; Meilstrup, C.; Madsen, K.R.; Koushede, V. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Health 2020, 5, 62–70. [Google Scholar] [CrossRef] [Green Version]
- Song, H.; Sieurin, J.; Wirdefeldt, K.; Pedersen, N.; Almqvist, C.; Larsson, H.; Valdimarsdóttir, U.A.; Fang, F. Association of Stress-Related Disorders with Subsequent Neurodegenerative Diseases. JAMA Neurol. 2020, 77, 700–709. [Google Scholar] [CrossRef] [PubMed]
- Boutoleau-Bretonnière, C.; Pouclet-Courtemanche, H.; Gillet, A.; Bernard, A.; Deruet, A.L.; Gouraud, I.; Mazoue, A.; Lamy, E.; Rocher, L.; Kapogiannis, D.; et al. The effects of confinement on neuropsychiatric symptoms in Alzheimer’s disease during the COVID-19 crisis. J. Alzheimer’s Dis. 2020, 76, 41–47. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Benaque, A.; Gurruchaga, M.J.; Abdelnour, C.; Hernández, I.; Cañabate, P.; Alegret, M.; Rodríguez, I.; Rosende-Roca, M.; Tartari, J.P.; Esteban, E.; et al. Dementia care in times of COVID-19: Experience at Fundació ACE in Barcelona, Spain. J. Alzheimer’s Dis. 2020, 76, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Ousset, P.J.; Vellas, B. Viewpoint: Impact of the Covid-19 outbreak on the clinical and research activities of memory clinics: An Alzheimer’s disease center facing the Covid-19 crisis. J. Prev. Alzheimers Dis. 2020, 7, 197–198. [Google Scholar] [PubMed]
- Reisberg, B.; Ferris, S.H.; de Leon, M.J.; Crook, T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am. J. Psychiatry 1982, 139, 1136–1139. [Google Scholar]
- Fountoulakis, K.N.; Tsolaki, M.; Chantzi, H.; Kazis, A. Mini mental state examination (MMSE): A validation study in Greece. Am. J. Alzheimer’s Dis. Other Dement.® 2000, 15, 342–345. [Google Scholar] [CrossRef]
- Poptsi, E.; Moraitou, D.; Eleftheriou, M.; Kounti-Zafeiropoulou, F.; Papasozomenou, C.; Agogiatou, C.; Bakoglidou, E.; Batsila, G.; Liapi, D.; Markou, N.; et al. Normative data for the Montreal cognitive assessment in Greek older adults with subjective cognitive decline, mild cognitive impairment and dementia. J. Geriatr. Psychiatry Neurol. 2019, 32, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Messinis, L.; Tsakona, I.; Malefaki, S.; Papathanasopoulos, P. Normative data and discriminant validity of Rey’s Verbal Learning Test for the Greek adult population. Arch. Clin. Neuropsychol. 2007, 22, 739–752. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kosmidis, M.H.; Vlahou, C.H.; Panagiotaki, P.; Kiosseoglou, G. The verbal fluency task in the Greek population: Normative data, and clustering and switching strategies. J. Int. Neuropsychol. Soc. JINS 2004, 10, 164. [Google Scholar] [CrossRef]
- Tsatali, M.; Emmanouel, A.; Gialaouzidis, M.; Avdikou, K.; Stefanatos, C.; Diamantidou, A.; Kouroundi, E.; Messini, C.; Tsolaki, M. Rey Complex Figure Test (RCFT): Norms for the Greek older adult population. Appl. Neuropsychol. Adult 2020, 1–9. [Google Scholar] [CrossRef]
- Tsatali, M.; Poptsi, E.; Moraitou, D.; Agogiatou, C.; Bakoglidou, E.; Gialaouzidis, M.; Papasozomenou, C.; Soumpourou, A.; Tsolaki, M. Discriminant Validity of the WAIS-R Digit Symbol Substitution Test in Subjective Cognitive Decline, Mild Cognitive Impairment (Amnestic Subtype) and Alzheimer’s Disease Dementia (ADD) in Greece. Brain Sci. 2021, 11, 881. [Google Scholar] [CrossRef] [PubMed]
- Kounti, F.; Tsolaki, M.; Kiosseoglou, G. Functional cognitive assessment scale (FUCAS): A new scale to assess executive cognitive function in daily life activities in patients with dementia and mild cognitive impairment. Hum. Psychopharmacol. Clin. Exp. 2006, 21, 305–311. [Google Scholar] [CrossRef]
- Sinoff, G.; Ore, L.; Zlotogorsky, D.; Tamir, A. Short anxiety screening test—A brief instrument for detecting anxiety in the elderly. Int. J. Geriatr. Psychiatry 1999, 14, 1062–1071. [Google Scholar] [CrossRef]
- Grammatikopoulos, I.A.; Sinoff, G.; Alegakis, A.; Kounalakis, D.; Antonopoulou, M.; Lionis, C. The short anxiety screening test in Greek: Translation and validation. Ann. Gen. Psychiatry 2010, 9, 1. [Google Scholar] [CrossRef] [Green Version]
- Politis, A.M.; Mayer, L.S.; Passa, M.; Maillis, A.; Lyketsos, C.G. Validity and reliability of the newly translated Hellenic Neuropsychiatric Inventory (H-NPI) applied to Greek outpatients with Alzheimer’s disease: A study of disturbing behaviors among referrals to a memory clinic. Int. J. Geriatr. Psychiatry 2004, 19, 203–208. [Google Scholar] [CrossRef]
- Bendler, P.M. EQS 6 Structural Equation Program Manual; Multivariate Software: Encino, CA, USA, 2005. [Google Scholar]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research; Guilford Press: New York, NY, USA, 2006. [Google Scholar]
- Alonso-Lana, S.; Marquié, M.; Ruiz, A.; Boada, M. Cognitive and neuropsychiatric manifestations of COVID-19 and effects on elderly individuals with dementia. Front. Aging Neurosci. 2020, 12, 588872. [Google Scholar] [CrossRef]
- van Maurik, I.S.; Bakker, E.D.; Buuse, S.V.D.; Gillissen, F.; van De Beek, M.; Lemstra, E.; Mank, A.; Bosch, K.A.V.D.; van Leeuwenstijn, M.; Bouwman, F.H.; et al. Psychosocial effects of corona measures on patients with dementia, mild cognitive impairment and subjective cognitive decline. Front. Psychiatry 2020, 11, 585686. [Google Scholar] [CrossRef] [PubMed]
- Barguilla, A.; Fernández-Lebrero, A.; Estragués-Gázquez, I.; García-Escobar, G.; Navalpotro-Gómez, I.; Manero, R.M.; Puente-Periz, V.; Roquer, J.; Puig-Pijoan, A. Effects of COVID-19 Pandemia Confinement in Patients with Cognitive Impairment. Front. Neurol. 2020, 11, 589901. [Google Scholar] [CrossRef]
- Tsapanou, A.; Papatriantafyllou, J.D.; Yiannopoulou, K.; Sali, D.; Kalligerou, F.; Ntanasi, E.; Zoi, P.; Margioti, E.; Kamtsadeli, V.; Hatzopoulou, M.; et al. The impact of COVID-19 pandemia on people with mild cognitive impairment/dementia and on their caregivers. Int. J. Geriatr. Psychiatry 2020, 36, 583–587. [Google Scholar] [CrossRef]
- Lara, B.B.; Carnes, A.; Dakterzada, F.; Benitez, I.; Piñol-Ripoll, G. Neuropsychiatric symptoms and quality of life in Spanish Alzheimer’s disease patients during COVID-19 lockdown. Eur. J. Neurol. 2020, 27, 1744–1747. [Google Scholar] [CrossRef]
- Canevelli, M.; Valletta, M.; Blasi, M.T.; Remoli, G.; Sarti, G.; Nuti, F.; Sciancalepore, F.; Ruberti, E.; Cesari, M.; Bruno, G. Facing dementia during the COVID-19 outbreak. J. Am. Geriatr. Soc. 2020, 68, 1673–1676. [Google Scholar] [CrossRef]
- Shankar, A.; Hamer, M.; McMunn, A.; Steptoe, A. Social isolation and loneliness: Relationships with cognitive function during 4 years of follow-up in the English Longitudinal Study of Ageing. Psychosom. Med. 2013, 75, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Wing, Y.K.; Leung, C.M. Mental health impact of severe acute respiratory syndrome: A prospective study. Hong Kong Med. J. 2012, 18, 24–27. [Google Scholar]
- Holwerda, T.; Deeg, D.; Beekman, A.; van Tilburg, T.; Stek, M.; Jonker, C.; Schoevers, R. Feelings of loneliness, but not social isolation, predict dementia onset: Results from the Amsterdam study of the Elderly (AMSTEL). J. Neurol. Neurosurg. Psychiatry 2014, 85, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Courtin, E.; Knapp, M. Social isolation, loneliness and health in old age: A scoping review. Health Soc. Care Community 2017, 25, 799–812. [Google Scholar] [CrossRef]
- Poptsi, E.; Tsatali, M.; Agogiatou, C.; Bakoglidou, E.; Batsila, G.; Dellaporta, D.; Kounti-Zafeiropoulou, F.; Liapi, D.; Lysitsas, K.; Markou, N.; et al. Longitudinal Cognitive and Physical Training Effectiveness in MCI, Based on the Experience of the Alzheimer’s Hellas Day Care Centre. J. Geriatr. Psychiatry Neurol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Goodman-Casanova, J.M.; Dura-Perez, E.; Guzman-Parra, J.; Cuesta-Vargas, A.; Mayoral-Cleries, F. Telehealth home support during COVID-19 confinement for community-dwelling older adults with mild cognitive impairment or mild dementia: Survey study. J. Med. Internet Res. 2020, 22, e19434. [Google Scholar] [CrossRef]
| Demographics | MCI (n = 296) | ADD (n = 111) |
|---|---|---|
| Gender | ||
| Men | 99 | 47 |
| Women | 197 | 64 |
| Age (years) | 71.60 (7.7) | 77.32 (6.6) |
| Education (years) | 12.38 (3.9) | 9.28 (4.8) |
| Mean (SD) | |||||
|---|---|---|---|---|---|
| Neuropsychological Tests/ Psychometric Tools | Group | 2018 | 2019 | 2020 | p |
| MMSE | MCI | 27.77 (2.1) | 27.73 (1.9) | 27.74 (1.9) | <0.001 |
| ADD | 21.59 (3.8) | 20.53 (4.9) | 19.05 (5.6) | ||
| MoCA | MCI | 23.69 (3.4) | 23.77 (3.0) | 23.74 (3.3) | 0.550 |
| ADD | |||||
| FUCAS | MCI | 43.77 (1.6) | 43.95 (1.7) | 43.75 (1.8) | <0.001 |
| ADD | 54.20 (8.6) | 55.86 (10) | 60.37 (15) | ||
| NPI | MCI | 3.37 (5.9) | 1.75 (7.8) | 2.33 (4) | 0.001 |
| ADD | 7.27 (7.8) | 7.81 (7.7) | 8.78 (8.9) | ||
| SAST | MCI | 18.27 (5.1) | 17.66 (4.7) | 16.95 (4.7) | <0.001 |
| ADD | 14.82 (4.5) | 14.40 (3.8) | 13.69 (3.3) | ||
| RAVLT1 | MCI | 6.19 (2.5) | 6.27 (2.3) | 5.18 (1.6) | <0.001 |
| Short term memory | ADD | 2.89 (1.6) | 2.96 (1.6) | 2.65 (1.5) | |
| RAVLT 5 | MCI | 11.44 (2.4) | 11.64 (2.5) | 10.54 (2.5) | <0.001 |
| Verbal learning | ADD | 5.59 (2.2) | 5.49 (2.6) | 4.67 (2.5) | |
| RAVLT | MCI | 9.58 (3.3) | 9.63 (3.3) | 7.71 (3.3) | <0.001 |
| Delayed Recall | ADD | 2.24 (2.3) | 2.07 (2,1) | 1.22 (1.9) | |
| RCFT | MCI | 28.79 (4.6) | 29.01 (4.7) | 30.81 (3.7) | 0.031 |
| Copy | ADD | 19.78 (4.6) | 19.51 (7.9) | 20.51 (10) | |
| RCFT | MCI | 15.28 (6.1) | 15.67 (6.2) | 17.69 (6.9) | 0.081 |
| Delayed Recall | ADD | 4.6 (4) | 4.3 (3.8) | 4.08 (4.3) | |
| Phonemic fluency | MCI | 11.33 (3.6) | 11.48 (3.6) | 11.54 (3.6) | 0.011 |
| ADD | 6.34 (3) | 6.35 (3.2) | 5.89 (3.4) | ||
| DSST | MCI | 34.06 (12.31) | 34.94 (12.13) | 34.05 (12.19) | <0.001 |
| ADD | - | ||||
| Deterioration Rate (D) | Group | Group by D Interaction | |||||||
|---|---|---|---|---|---|---|---|---|---|
| F | p | η2 | F | p | η2 | F | p | η2 | |
| MMSE | 2.06 | 0.152 | 0.007 | 81.5 | <0.001 * | 0.2 | 2.38 | 0.008 | 0.12 |
| MoCA | 0.851 | 0.357 | 0.003 | ------ | ------ | ||||
| FUCAS | 15.77 | <0.001 * | 0.049 | 103.38 | <0.001 * | 0.251 | 24.59 | <0.001 * | 0.317 |
| NPI | 2.67 | 0.103 | 0.009 | 3.7 | 0.055 | 0.012 | 0.76 | 0.383 | 0.003 |
| SAST | 1.16 | 0.281 | 0.004 | 1.15 | 0.136 | 0.001 | 1.35 | 0.245 | 0.004 |
| RAVLT | 23.2 | <0.001 * | 0.007 | 7.14 | 0.127 | 0.008 | 7 | 0.009 | 0.023 |
| First trial | |||||||||
| RCFT | 3.42 | 0.065 | 0.011 | 7.61 | 0.006 | 0.025 | 0.04 | 0.833 | 0.001 |
| Copy | |||||||||
| RAVLT | 24.8 | <0.001 * | 0.077 | 0.9 | 0.342 | 0.003 | 3.7 | 0.055 | 0.01 |
| 5th trial | |||||||||
| RAVLT | 29.8 | <0.001 * | 0.009 | 3.56 | 0.06 | 0.01 | 10.1 | 0.002 * | 0.03 |
| Delayed | |||||||||
| RCFT | 0.44 | 0.5 | 0.001 | 22.45 | <0.001 * | 0.07 | 0.19 | 0.658 | 0.001 |
| Delayed | |||||||||
| Verbal | 8.29 | 0.004 * | 0.02 | 12.37 | 0.001 * | 0.04 | 2.02 | 0.155 | 0.007 |
| Fluency | |||||||||
| DSST | 20.87 | <0.001 * | 0.09 | ------ | ------ | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsatali, M.; Moraitou, D.; Poptsi, E.; Sia, E.; Agogiatou, C.; Gialaouzidis, M.; Tabakis, I.-M.; Avdikou, K.; Bakoglidou, E.; Batsila, G.; et al. Are There Any Cognitive and Behavioral Changes Potentially Related to Quarantine Due to the COVID-19 Pandemic in People with Mild Cognitive Impairment and AD Dementia? A Longitudinal Study. Brain Sci. 2021, 11, 1165. https://doi.org/10.3390/brainsci11091165
Tsatali M, Moraitou D, Poptsi E, Sia E, Agogiatou C, Gialaouzidis M, Tabakis I-M, Avdikou K, Bakoglidou E, Batsila G, et al. Are There Any Cognitive and Behavioral Changes Potentially Related to Quarantine Due to the COVID-19 Pandemic in People with Mild Cognitive Impairment and AD Dementia? A Longitudinal Study. Brain Sciences. 2021; 11(9):1165. https://doi.org/10.3390/brainsci11091165
Chicago/Turabian StyleTsatali, Marianna, Despina Moraitou, Eleni Poptsi, Eleni Sia, Christina Agogiatou, Moses Gialaouzidis, Irene-Maria Tabakis, Konstantina Avdikou, Evaggelia Bakoglidou, Georgia Batsila, and et al. 2021. "Are There Any Cognitive and Behavioral Changes Potentially Related to Quarantine Due to the COVID-19 Pandemic in People with Mild Cognitive Impairment and AD Dementia? A Longitudinal Study" Brain Sciences 11, no. 9: 1165. https://doi.org/10.3390/brainsci11091165
APA StyleTsatali, M., Moraitou, D., Poptsi, E., Sia, E., Agogiatou, C., Gialaouzidis, M., Tabakis, I.-M., Avdikou, K., Bakoglidou, E., Batsila, G., Bekiaridis-Moschou, D., Chatziroumpi, O., Diamantidou, A., Gavra, A., Kouroundi, E., Liapi, D., Markou, N., Ouzouni, F., Papasozomenou, C., ... Tsolaki, M. (2021). Are There Any Cognitive and Behavioral Changes Potentially Related to Quarantine Due to the COVID-19 Pandemic in People with Mild Cognitive Impairment and AD Dementia? A Longitudinal Study. Brain Sciences, 11(9), 1165. https://doi.org/10.3390/brainsci11091165







