Pressure-Relief Effect of Post-Op Shoes Depends on Correct Usage While Walking
Abstract
1. Introduction
2. Methodology
2.1. Study Population
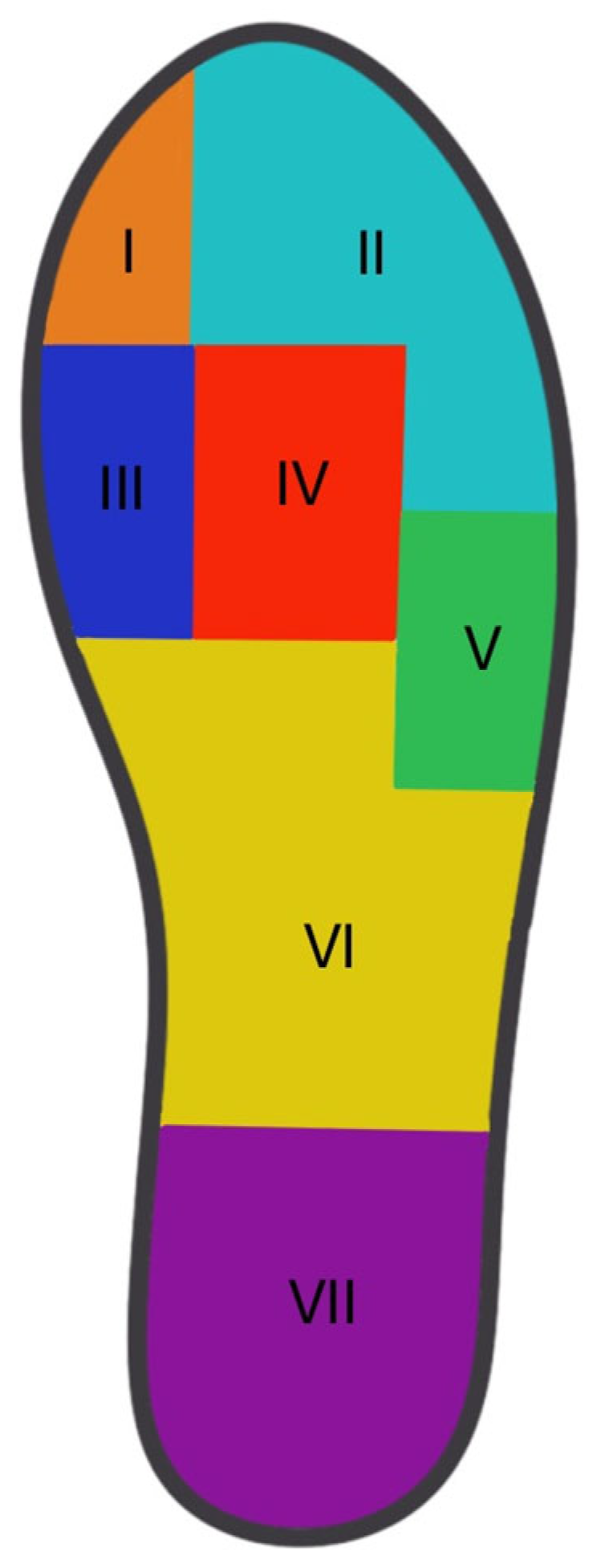
2.2. Measurement of Plantar Pressure Parameters
2.3. Testing Protocol
2.4. Barefoot Plantar Pressure Measurement (I)
2.5. POS Plantar Pressure Measurement (II)
2.6. Footwear
2.7. Data Analysis
2.8. Statistics
3. Results
3.1. Hallux
3.2. Lesser Toes
3.3. MTH1
3.4. MTH23
3.5. MTH45
3.6. Midfoot and Heel
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chen, J.; Devine, A.; Dick, I.M.; Dhaliwal, S.S.; Prince, R.L. Prevalence of lower extremity pain and its association with functionality and quality of life in elderly women in Australia. J. Rheumatol. 2003, 30, 2689–2693. [Google Scholar] [PubMed]
- Shirzad, K.; Kiesau, C.D.; DeOrio, J.K.; Parekh, S.G. Lesser toe deformities. J. Am. Acad. Orthop. Surg. 2011, 19, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.W.; Cheung, J.C.; Zhao, J.G.; Ni, M.; Yang, Z.Y. Forefoot Function after Hallux Valgus Surgery: A Systematic Review and Meta-Analysis on Plantar Load Measurement. J. Clin. Med. 2023, 12, 1384. [Google Scholar] [CrossRef]
- Cai, Y.; Song, Y.; He, M.; He, W.; Zhong, X.; Wen, H.; Wei, Q. Global prevalence and incidence of hallux valgus: A systematic review and meta-analysis. J. Foot. Ankle Res. 2023, 16, 63. [Google Scholar] [CrossRef]
- Simonsen, E.B.; Svendsen, M.B.; Nørreslet, A.; Baldvinsson, H.K.; Heilskov-Hansen, T.; Larsen, P.K.; Alkjær, T.; Henriksen, M. Walking on high heels changes muscle activity and the dynamics of human walking significantly. J. Appl. Biomech. 2012, 28, 20–28. [Google Scholar] [CrossRef]
- Roddy, E. Epidemiology and impact of hallux valgus: More than just bunions. J. Foot Ankle Res. 2011, 4, 1. [Google Scholar] [CrossRef]
- Roan, L.Y.; Tanaka, Y.; Taniguchi, A.; Tomiwa, K.; Kumai, T.; Cheng, Y.M. Why do lesser toes deviate laterally in hallux valgus? A radiographic study. Foot Ankle Int. 2015, 36, 664–672. [Google Scholar] [CrossRef]
- Schrier, J.C.; Verheyen, C.C.; Louwerens, J.W. Definitions of hammer toe and claw toe: An evaluation of the literature. J. Am Podiatr. Med. Assoc. 2009, 99, 194–197. [Google Scholar] [CrossRef]
- Zelen, C.M.; Young, N.J. Digital arthrodesis. Clin. Podiatr. Med. Surg. 2013, 30, 271–282. [Google Scholar] [CrossRef]
- Saro, C.; Bengtsson, A.S.; Lindgren, U.; Adami, J.; Blomqvist, P.; Felländer-Tsai, L. Surgical treatment of hallux valgus and forefoot deformities in Sweden: A population-based study. Foot Ankle Int. 2008, 29, 298–304. [Google Scholar] [CrossRef]
- Menz, H.B.; Gilheany, M.F.; Landorf, K.B. Foot and ankle surgery in Australia: A descriptive analysis of the Medicare Benefits Schedule database, 1997–2006. J. Foot Ankle Res. 2008, 1, 10. [Google Scholar] [CrossRef] [PubMed]
- Zirngibl, B.; Grifka, J.; Baier, C.; Götz, J. Hallux valgus: Etiology, diagnosis, and therapeutic principles. Orthopade 2017, 46, 283–296. [Google Scholar] [CrossRef] [PubMed]
- Burchard, R.; Massa, R.; Soost, C.; Richter, W.; Dietrich, G.; Ohrndorf, A.; Christ, H.-J.; Fritzen, C.-P.; Graw, J.A.; Schmitt, J. Biomechanics of common fixation devices for first tarsometatarsal joint fusion-a comparative study with synthetic bones. J. Orthop. Surg. Res. 2018, 13, 176. [Google Scholar] [CrossRef] [PubMed]
- Goransson, M.; Constant, D. Hammertoe. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Döhner, C.; Beyerle, H.; Graw, J.A.; Soost, C.; Burchard, R. Biomechanical comparison of different implants for PIP arthrodesis. Foot Ankle. Surg. 2023, 29, 518–524. [Google Scholar] [CrossRef]
- Hester, W.A., 3rd; Pedowitz, D.I. Postoperative Considerations in the Management of Hallux Valgus. Foot Ankle Clin. 2020, 25, 141–150. [Google Scholar] [CrossRef]
- Martone, J.; Poel, L.V.; Levy, N. Complications of arthrodesis and nonunion. Clin. Podiatr. Med. Surg. 2012, 29, 11–18. [Google Scholar] [CrossRef]
- Grosen, S.L.; Hansen, A.M. Sensor-floors: Changing Work and Values in Care for Frail Older Persons. Sci. Technol. Hum. Values. 2021, 46, 254–274. [Google Scholar] [CrossRef]
- Bränzel, A.; Holz, C.; Hoffmann, D.; Schmidt, D.; Knaust, M.; Lühne, P.; Meusel, R.; Richter, S.; Info, P.B. GravitySpace: Tracking users and their poses in a smart room using a pressure-sensing floor. In Proceedings of the Sigchi Conference on Human Factors in Computing Systems, Paris, France, 27 April 2013; Association for Computing Machinery. pp. 725–734. [Google Scholar]
- Lopez, A.; Bakaes, Y.; Porter, G.; Shi, G.; Myers, P.; Jackson, J.B., 3rd; Gonzalez, T.; Haupt, E.T. The Effect of First Metatarsal Shortening and Sagittal Displacement on Forefoot Pressure in Minimally Invasive Hallux Valgus Correction. Foot Ankle. Spec. 2024, 26, 19386400241261129. [Google Scholar] [CrossRef]
- Nouman, M.; Apiputhanayut, R.; Narungsri, T.; Tipchatyotin, S.; Dissaneewate, T. Comparative Analysis of Three Types of Therapeutic Offloading Diabetic Shoes With Custom Made Insole on Plantar Pressure Distribution in Severe Diabetic Charcot Foot. Can. Prosthet. Orthot. J. 2024, 7, 41780. [Google Scholar] [CrossRef]
- Schuh, R.; Trnka, H.J.; Sabo, A.; Reichel, M.; Kristen, K.H. Biomechanics of postoperative shoes: Plantar pressure distribution, wearing characteristics and design criteria: A preliminary study. Arch. Orthop. Trauma. Surg. 2011, 131, 197–203. [Google Scholar] [CrossRef]
- Fuchs, M.; Hermans, M.M.N.; Kars, H.J.J.; Hendriks, J.G.E.; van der Steen, M.C. Plantar pressure distribution and wearing characteristics of three forefoot offloading shoes in healthy adult subjects. Foot 2020, 45, 101744. [Google Scholar] [CrossRef] [PubMed]
- Navarro-Cano, E.; Guevara-Noriega, K.A.; Lucar-Lopez, G.; Reina, F.; Carrera, A. A comparison of two designs of postoperative shoe for hallux valgus surgery: A biomechanical study in a cadaveric model. Foot Ankle. Surg. 2021, 27, 82–86. [Google Scholar] [CrossRef] [PubMed]
- Carl, H.D.; Pfander, D.; Swoboda, B. Assessment of plantar pressure in forefoot relief shoes of different designs. Foot Ankle. Int. 2006, 27, 117–120. [Google Scholar] [CrossRef]
- Lorei, T.; Klärner, H.; Rosenbaum, D. Influence of postoperative shoes on plantar pressure patterns. Z. Orthop. Ihre. Grenzgeb. 2006, 144, 153–157. [Google Scholar] [CrossRef]
- Sarmah, S.S.; Hossain, F.S.; Mishra, V. Effectiveness of the reverse camber shoe in postoperative hallux valgus surgery. Foot Ankle. Spec. 2012, 5, 245–248. [Google Scholar] [CrossRef]
- Patel, S.; Garg, P.; Fazal, M.A.; Shahid, M.S.; Park, D.H.; Ray, P.S. A Comparison of Two Designs of Postoperative Shoe on Function, Satisfaction, and Back Pain After Hallux Valgus Surgery. Foot Ankle. Spec. 2019, 12, 228–232. [Google Scholar] [CrossRef]
- Eidmann, A.; Vinke, W.; Jakuscheit, A.; Rudert, M.; Stratos, I. The influence of partial weight bearing on plantar peak forces using three different types of postoperative shoes. Foot Ankle. Surg. 2022, 28, 1384–1388. [Google Scholar] [CrossRef]
- Pataky, T.C.; Bosch, K.; Mu, T.; Keijsers, N.L.; Segers, V.; Rosenbaum, D.; Goulermas, J.Y. An anatomically unbiased foot template for inter-subject plantar pressure evaluation. Gait. Posture. 2011, 33, 418–422. [Google Scholar] [CrossRef]
- Reints, R.; Hijmans, J.M.; Burgerhof, J.G.M.; Postema, K.; Verkerke, G.J. Effects of flexible and rigid rocker profiles on in-shoe pressure. Gait. Posture. 2017, 58, 287–293. [Google Scholar] [CrossRef]
- Chapman, J.D.; Preece, S.; Braunstein, B.; Höhne, A.; Nester, C.J.; Brueggemann, P.; Hutchins, S. Effect of rocker shoe design features on forefoot plantar pressures in people with and without diabetes. Clin. Biomech. 2013, 28, 679–685. [Google Scholar] [CrossRef]
- Preece, S.J.; Chapman, J.D.; Braunstein, B.; Brüggemann, G.P.; Nester, C.J. Optimisation of rocker sole footwear for prevention of first plantar ulcer: Comparison of group-optimised and individually-selected footwear designs. J. Foot Ankle. Res. 2017, 10, 27. [Google Scholar] [CrossRef] [PubMed]
- Dearden, P.M.C.; Ray, R.I.; Robinson, P.W.; Varrall, C.R.; Goff, T.J.; Fogarty, K.A. Clinical and Radiological Outcomes of Forefoot Offloading Versus Rigid Flat Shoes in Patients Undergoing Surgery of the First Ray. Foot Ankle. Int. 2019, 40, 1189–1194. [Google Scholar] [CrossRef] [PubMed]
- Brown, H.E.; Mueller, M.J. A “step-to” gait decreases pressures on the forefoot. J. Orthop. Sports Phys. Ther. 1998, 28, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Drerup, B.; Szczepaniak, A.; Wetz, H.H. Plantar pressure reduction in step-to gait: A biomechanical investigation and clinical feasibility study. Clin. Biomech. 2008, 23, 1073–1079. [Google Scholar] [CrossRef]
- van Schie, C.; Ulbrecht, J.S.; Becker, M.B.; Cavanagh, P.R. Design criteria for rigid rocker shoes. Foot Ankle. Int. 2000, 21, 833–844. [Google Scholar] [CrossRef]
- Lee, P.Y.; Landorf, K.B.; Bonanno, D.R.; Menz, H.B. Comparison of the pressure-relieving properties of various types of forefoot pads in older people with forefoot pain. J. Foot Ankle Res. 2014, 7, 18. [Google Scholar] [CrossRef]
- Zulkifli, S.S.; Loh, W.P. A state-of-the-art review of foot pressure. Foot Ankle Surg. 2020, 26, 25–32. [Google Scholar] [CrossRef]
- Segal, A.; Rohr, E.; Orendurff, M.; Shofer, J.; O’Brien, M.; Sangeorzan, B. The effect of walking speed on peak plantar pressure. Foot Ankle Int. 2004, 25, 926–933. [Google Scholar] [CrossRef]


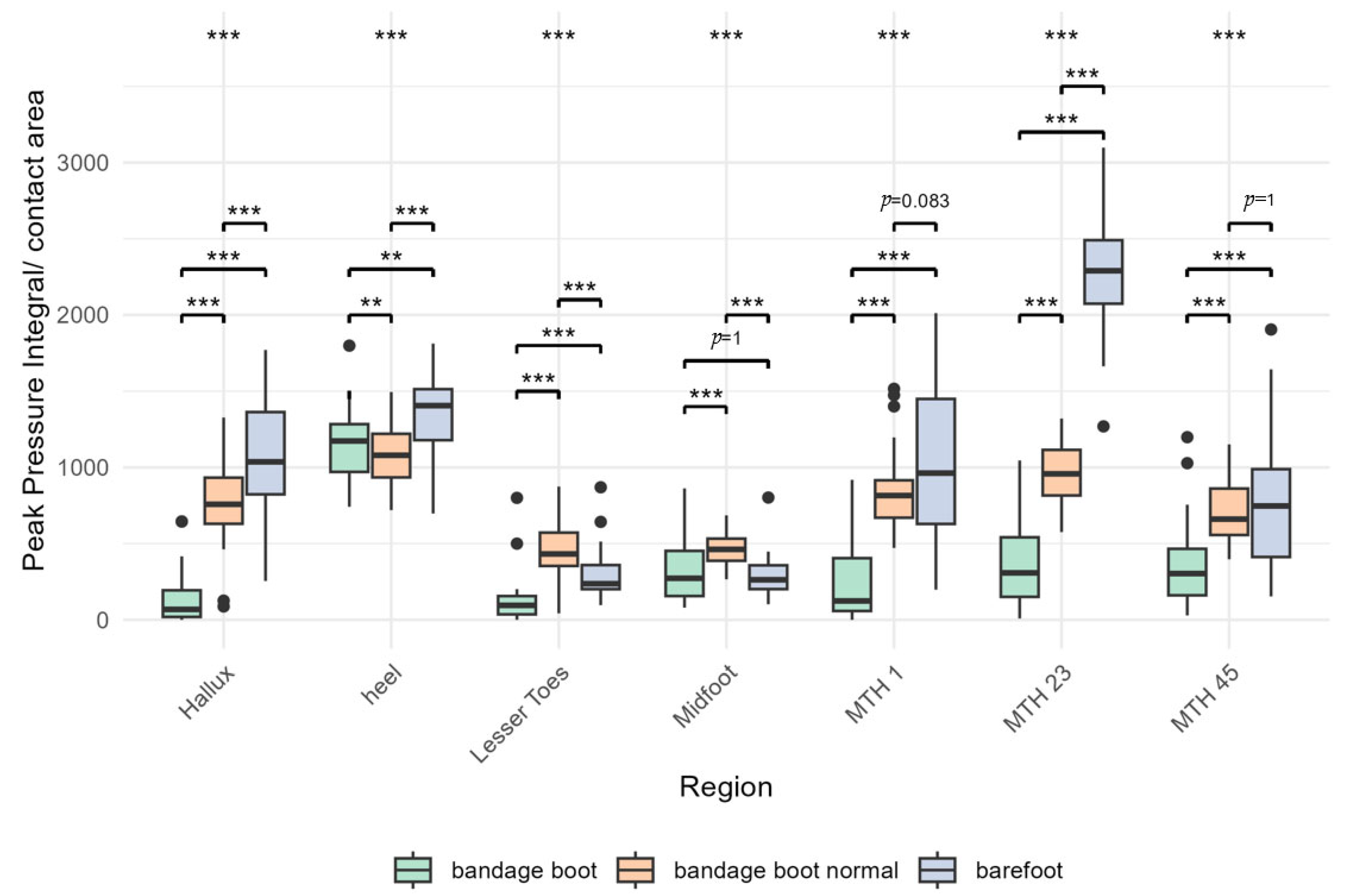
| Region | Gait Model | Mean | SD | ATS | p |
|---|---|---|---|---|---|
Hallux | POS Heel POS Normal Barefoot | 141.0 771.1 1071.7 | 176.4 297.0 380.7 | 114.5 | p < 0.001 |
Heel | POS Heel POS Normal Barefoot | 1154.8 1073.5 1353.3 | 231.6 199.5 252.0 | 15.84 | p < 0.001 |
| Lesser Toes | POS Heel POS Normal Barefoot | 128.2 467.4 298.9 | 162.5 188.8 166.0 | 41.0 | p < 0.001 |
Midfoot | POS Heel POS Normal Barefoot | 316.0 468.46 289.35 | 188.1 111.5 133.9 | 14.2 | p < 0.001 |
MTH1 | POS Heel POS Normal Barefoot | 258.3 843.5 1050.2 | 286.6 267.5 513.6 | 24.6 | p < 0.001 |
MTH23 | POS Heel POS Normal Barefoot | 377.6 963.1 2268.7 | 293.4 194.0 369.3 | 246.1 | p < 0.001 |
MTH45 | POS Heel POS Normal Barefoot | 360.9 711.4 751.2 | 282.7 200.7 441.9 | 15.7 | p < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Döhner, C.; Soost, C.; Steinhöfer, S.; Graw, J.A.; Bliemel, C.; Barsumyan, A.; Burchard, R. Pressure-Relief Effect of Post-Op Shoes Depends on Correct Usage While Walking. Bioengineering 2025, 12, 489. https://doi.org/10.3390/bioengineering12050489
Döhner C, Soost C, Steinhöfer S, Graw JA, Bliemel C, Barsumyan A, Burchard R. Pressure-Relief Effect of Post-Op Shoes Depends on Correct Usage While Walking. Bioengineering. 2025; 12(5):489. https://doi.org/10.3390/bioengineering12050489
Chicago/Turabian StyleDöhner, Claudia, Christian Soost, Sam Steinhöfer, Jan A. Graw, Christopher Bliemel, Artur Barsumyan, and Rene Burchard. 2025. "Pressure-Relief Effect of Post-Op Shoes Depends on Correct Usage While Walking" Bioengineering 12, no. 5: 489. https://doi.org/10.3390/bioengineering12050489
APA StyleDöhner, C., Soost, C., Steinhöfer, S., Graw, J. A., Bliemel, C., Barsumyan, A., & Burchard, R. (2025). Pressure-Relief Effect of Post-Op Shoes Depends on Correct Usage While Walking. Bioengineering, 12(5), 489. https://doi.org/10.3390/bioengineering12050489






