Biomechanical and Biological Multidisciplinary Strategies in the Orthodontic Treatment of Patients with Periodontal Diseases: A Review of the Literature
Abstract
1. Introduction
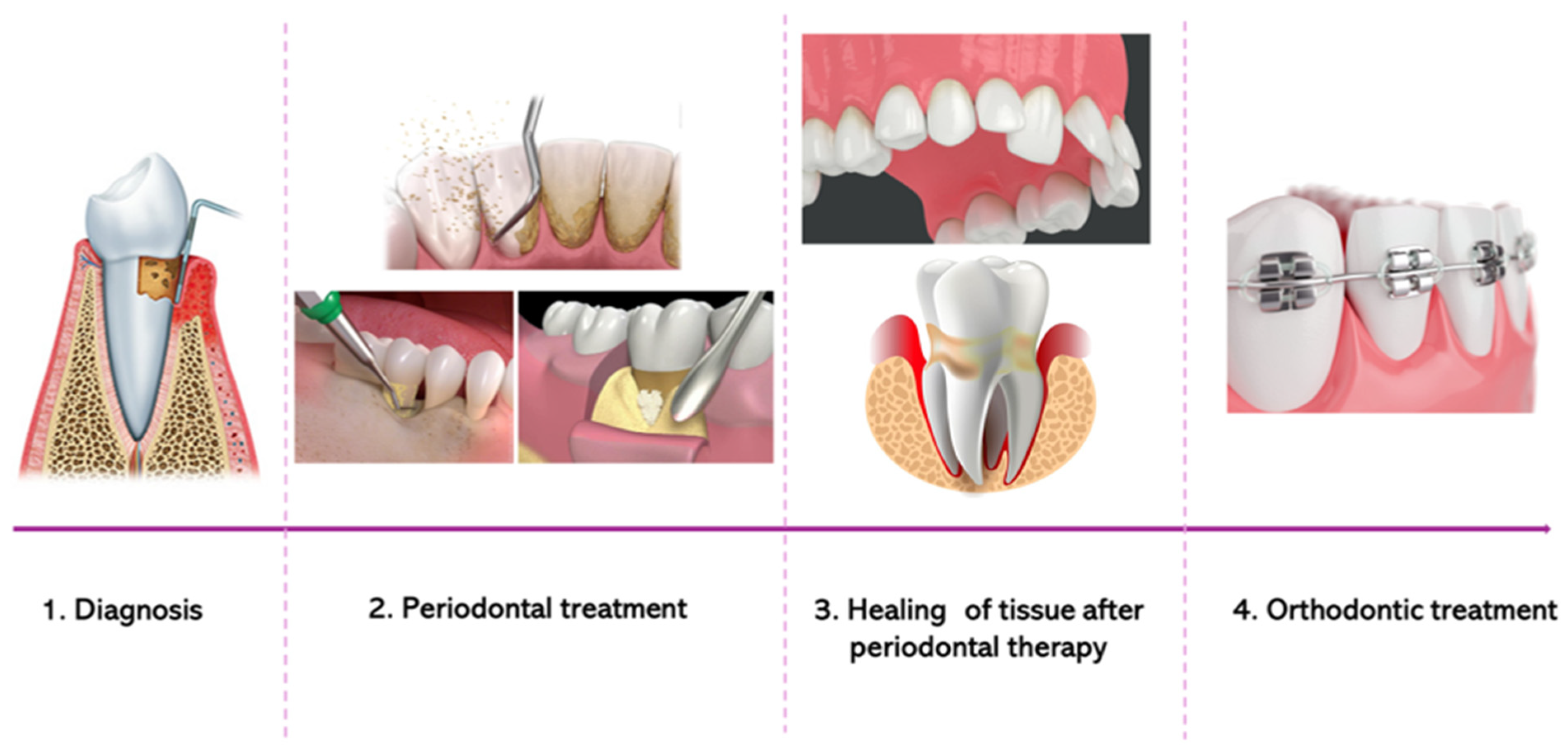
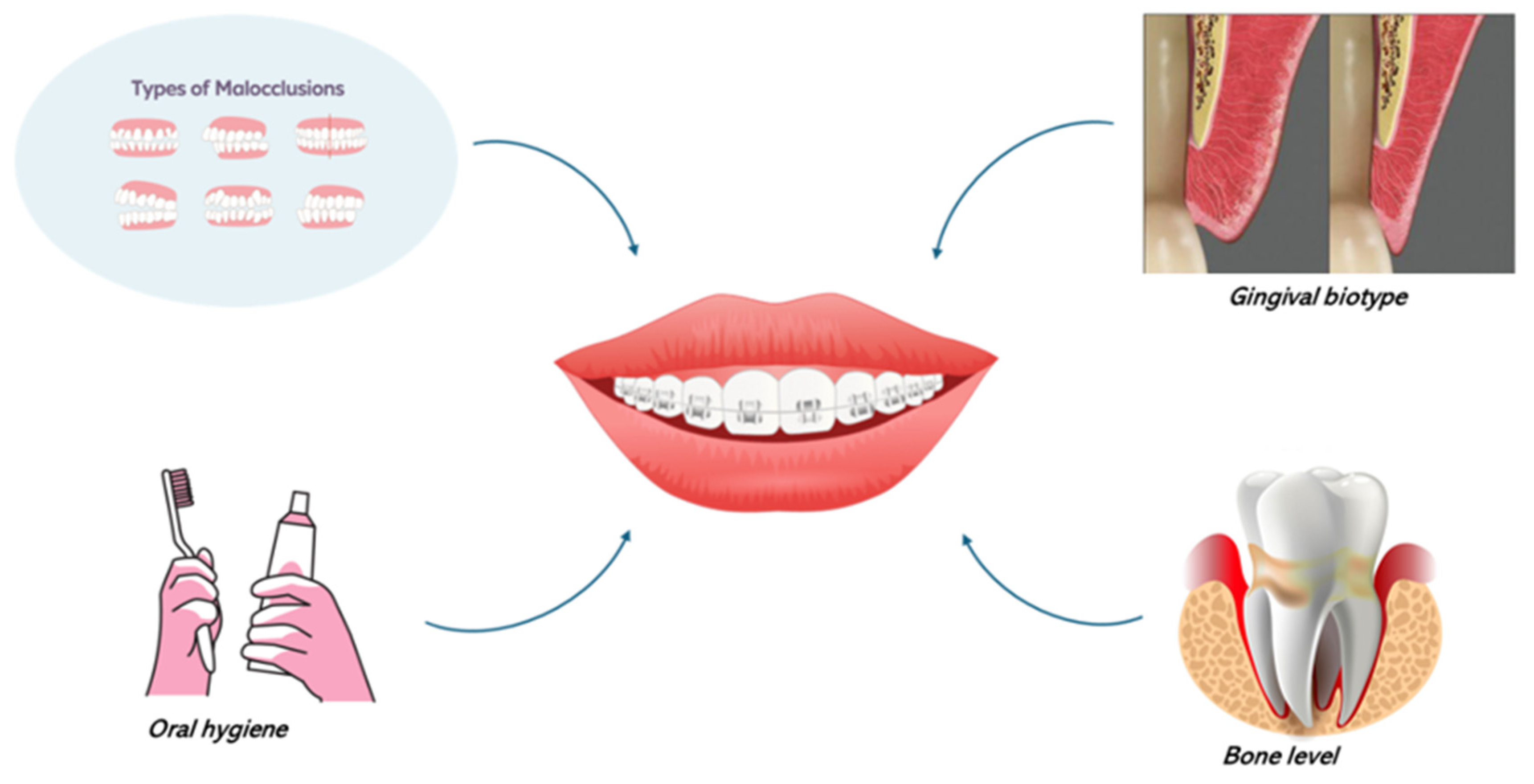
2. The Interplay Between Orthodontic Therapy and Periodontal Health
2.1. Orthodontic Mechanics and Periodontal Tissues
2.2. Iatrogenic Effects: Root Resorption and Gingival Recession
3. Interdisciplinary Collaboration: Orthodontist–Periodontist Partnerships
3.1. Communication and Treatment Coordination
3.2. Periodontal Considerations in Treatment Planning
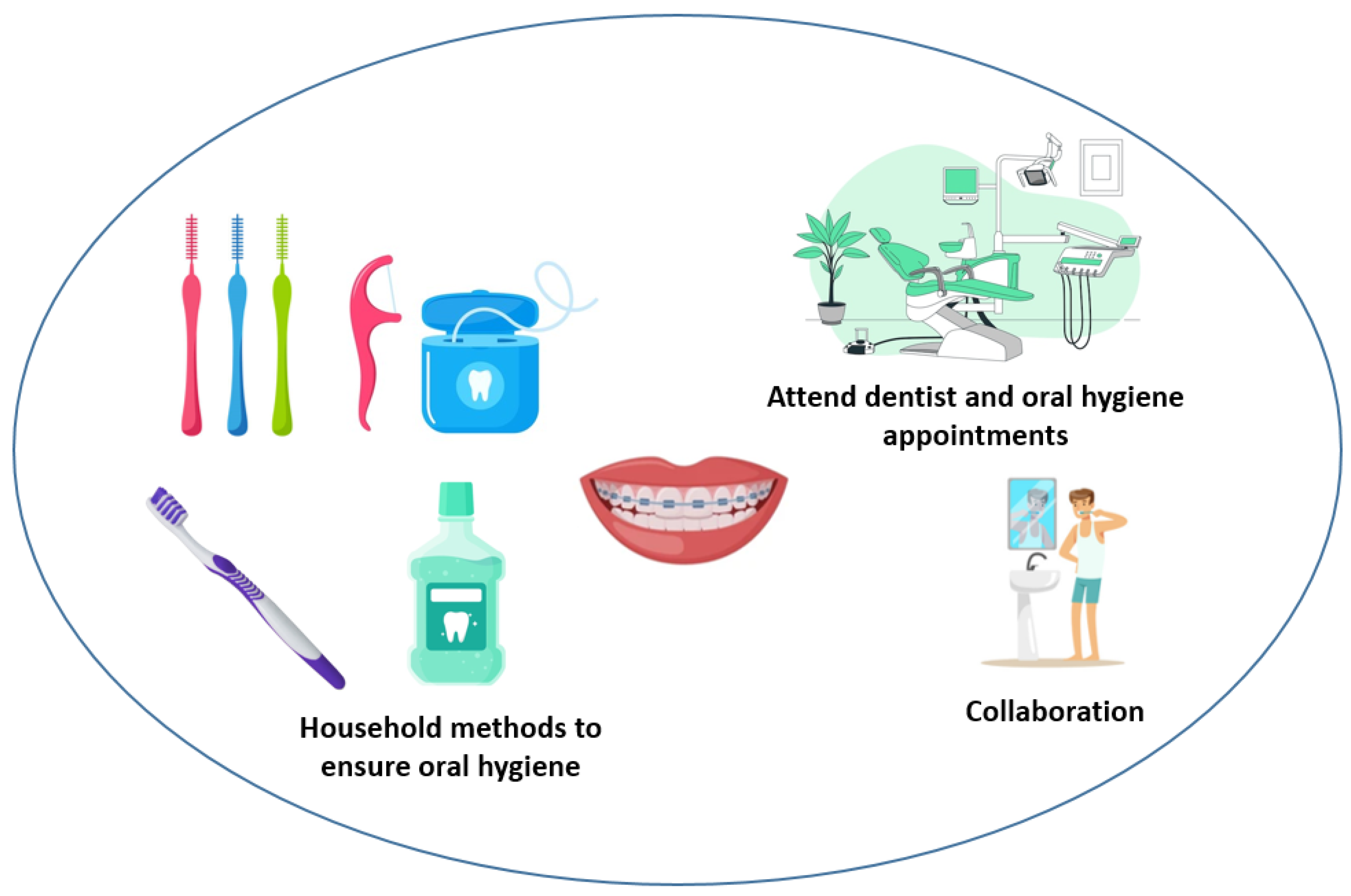
4. Patient Education and Oral Hygiene Instruction
5. Adjunctive Periodontal Therapy in Orthodontic Patients
5.1. Selective Alveolar Decortication
5.2. Periodontal Regenerative Procedure
6. Limitations and Future Directions
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sanz, M.; Van Winkelhoff, A.J.; Working Group 1 of Seventh European Workshop on Periodontology. Periodontal infections: Understanding the complexity–consensus of the Seventh European Workshop on Periodontology. J. Clin. Periodontol. 2011, 38, 3–6. [Google Scholar] [CrossRef]
- Kassebaum, N.; Bernabé, E.; Dahiya, M.; Bhandari, B.; Murray, C.; Marcenes, W. Global burden of severe periodontitis in 1990-2010: A systematic review and meta-regression. J. Dent. Res. 2014, 93, 1045–1053. [Google Scholar] [CrossRef]
- Kassebaum, N.J.; Smith, A.G.; Bernabé, E.; Fleming, T.D.; Reynolds, A.E.; Vos, T.; Murray, C.; Marcenes, W.; GBD 2015 Oral Health Collaborators. Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 countries, 1990–2015: A systematic analysis for the global burden of diseases, injuries, and risk factors. J. Dent. Res. 2017, 96, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Sanz, M.; Herrera, D.; Kebschull, M.; Chapple, I.; Jepsen, S.; Berglundh, T.; Sculean, A.; Tonetti, M.S.; Participants, E.W.; Consultants, M.; et al. Treatment of stage I–III periodontitis—The EFP S3 level clinical practice guideline. J. Clin. Periodontol. 2020, 47, 4–60. [Google Scholar] [CrossRef] [PubMed]
- Darveau, R.P.; Tanner, A.; Page, R.C. The microbial challenge in periodontitis. Periodontology 2000 1997, 14, 12–32. [Google Scholar] [CrossRef] [PubMed]
- Cardaropoli, D.; Gaveglio, L.; Abou-Arraj, R.V. Orthodontic movement and periodontal bone defects: Rationale, timing, and clinical implications. Semin. Orthod. 2014, 20, 177–187. [Google Scholar] [CrossRef]
- Wagenberg, B.D.; Eskow, R.N.; Langer, B. Orthodontic procedures that improve the periodontal prognosis. J. Am. Dent. Assoc. 1980, 100, 370–373. [Google Scholar] [CrossRef] [PubMed]
- Polizzi, A.; Alibrandi, A.; Lo Giudice, A.; Distefano, A.; Orlando, L.; Analazi, A.M.; Pizzo, G.; Volti, G.L.; Isola, G. Impact of periodontal microRNAs associated with alveolar bone remodeling during orthodontic tooth movement: A randomized clinical trial. J. Transl. Med. 2024, 22, 1155. [Google Scholar] [CrossRef]
- Proffit, W.; Fields, H., Jr. Contemporary Orthodontics; Mosby–Year Book: St. Louis, MO, USA, 1993. [Google Scholar]
- Graber, T. Biomechanical principles and reactions. In Orthodontics: Current Principles and Techniques; Elsevier: Amsterdam, The Netherlands, 1985; pp. 101–192. [Google Scholar]
- Williams, S.; Melsen, B.; Agerbaek, N.; Asboe, V. The orthodontic treatment of malocclusion in patients with previous periodontal disease. Br. J. Orthod. 1982, 9, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Tanne, K.; Nagataki, T.; Inoue, Y.; Sakuda, M.; Burstone, C.J. Patterns of initial tooth displacements associated with various root lengths and alveolar bone heights. Am. J. Orthod. Dentofac. Orthop. 1991, 100, 66–71. [Google Scholar] [CrossRef]
- Burstone, C.J.; Pryputniewicz, R.J. Holographic determination of centers of rotation produced by orthodontic forces. Am. J. Orthod. 1980, 77, 396–409. [Google Scholar] [CrossRef]
- Choi, S.-H.; Kim, Y.-H.; Lee, K.-J.; Hwang, C.-J. Effect of labiolingual inclination of a maxillary central incisor and surrounding alveolar bone loss on periodontal stress: A finite element analysis. Korean J. Orthod. 2016, 46, 155–162. [Google Scholar] [CrossRef]
- Geramy, A. Alveolar bone resorption and the center of resistance modification (3-D analysis by means of the finite element method). Am. J. Orthod. Dentofac. Orthop. 2000, 117, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Matarese, G.; Cordasco, G.; Perillo, L.; Ramaglia, L. Mechanobiology of the tooth movement during the orthodontic treatment: A literature review. Minerva Stomatol. 2016, 65, 299–327. [Google Scholar]
- Melsen, B. Limitations in adult orthodontics. Curr. Controv. Orthod. 1991, 2, 147–180. [Google Scholar]
- Janson, M. Pergunte a um expert. Marcos Janson responde. Rev. Clin. Ortod. Dent. Press 2005, 4, 7–21. [Google Scholar]
- Shen, X.; Shi, J.; Xu, L.; Jiao, J.; Lu, R.; Meng, H. Clinical evaluation of periodontal-orthodontic treatment in patients with aggressive periodontitis and malocclusion. Beijing Da Xue Xue Bao. Yi Xue Ban = J. Peking University. Health Sci. 2017, 49, 60–66. [Google Scholar]
- Malmgren, O.; Levander, E. Minimizing Orthodontically Induced Root Resorption: Guidelines Based on a Review of Clinical Studies. World J. Orthod. 2003, 4, 19–30. [Google Scholar]
- Matarese, G.; Isola, G.; Alibrandi, A.; Lo Gullo, A.; Bagnato, G.; Cordasco, G.; Perillo, L. Occlusal and MRI characterizations in systemic sclerosis patients: A prospective study from Southern Italian cohort. Jt. Bone Spine 2016, 83, 57–62. [Google Scholar] [CrossRef]
- Agarwal, S.; Gupta, S.; Chugh, V.K.; Jain, E.; Valiathan, A.; Nanda, R. Interdisciplinary treatment of a periodontally compromised adult patient with multiple missing posterior teeth. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 238–248. [Google Scholar] [CrossRef]
- Couto, G.M.D.; Soares, C.E.S.; Queiroz, A.P.G.; Rodrigues, V.B.; Barbosa, O.L.C. Tratamento ortodôntico em paciente com periodonto reduzido dez anos de acompanhamento. Ortodontia 2016, 49, 376–386. [Google Scholar]
- Pearson, L.E. Vertical control in fully-banded orthodontic treatment. Angle Orthod. 1986, 56, 205–224. [Google Scholar] [PubMed]
- Thilander, B. Infrabony pockets and reducedalveolar bone height in relation to orthodontic therapy. Semin. Orthod. 1996, 2, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Behr, M.; Proff, P.; Leitzmann, M.; Pretzel, M.; Handel, G.; Schmalz, G.; Driemel, O.; Reichert, T.E.; Koller, M. Survey of congenitally missing teeth in orthodontic patients in Eastern Bavaria. Eur. J. Orthod. 2011, 33, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Cardaropoli, D.; Re, S.; Corrente, G.; Abundo, R. Intrusion of migrated incisors with infrabony defects in adult periodontal patients. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 671–675. [Google Scholar] [CrossRef] [PubMed]
- Zasčiurinskienė, E.; Basevičienė, N.; Lindsten, R.; Slotte, C.; Jansson, H.; Bjerklin, K. Orthodontic treatment simultaneous to or after periodontal cause-related treatment in periodontitis susceptible patients. Part I: Clinical outcome. A randomized clinical trial. J. Clin. Periodontol. 2018, 45, 213–224. [Google Scholar] [CrossRef] [PubMed]
- Ericsson, I.; Tehlander, B.; Lindhe, J.; Okamoto, H. The effect of orthodontic tilting movements on the periodontal tissues of infected and non-infected dentitions in dogs. J. Clin. Periodontol. 1977, 4, 278–293. [Google Scholar] [CrossRef] [PubMed]
- Melsen, B.; Agerbaek, N.; Markenstam, G. Intrusion of incisors in adult patients with marginal bone loss. Am. J. Orthod. Dentofac. Orthop. 1989, 96, 232–241. [Google Scholar] [CrossRef]
- Smith, R.K.; Roberts, W.E. Cell kinetics of the initial response to orthodontically induced osteogenesis in rat molar periodontal ligament. Calcif. Tissue Int. 1980, 30, 51–56. [Google Scholar] [CrossRef]
- Roberts, W.E.; Goodwin Jr, W.C.; Heiner, S.R. Cellular response to orthodontic force. Dent. Clin. N. Am. 1981, 25, 3–17. [Google Scholar] [CrossRef] [PubMed]
- EugeneRoberts, W.; Chase, D.C. Kinetics of cell proliferation and migration associated with orthodontically-induced osteogenesis. J. Dent. Res. 1981, 60, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Corrente, G.; Abundo, R.; Re, S.; Cardaropoli, D.; Cardaropoli, G. Orthodontic movement into infrabony defects in patients with advanced periodontal disease: A clinical and radiological study. J. Periodontol. 2003, 74, 1104–1109. [Google Scholar] [CrossRef] [PubMed]
- Lindhe, J.; Svanberg, G. Influence of trauma from occlusion on progression of experimental periodontitis in the beagle dog. J. Clin. Periodontol. 1974, 1, 3–14. [Google Scholar] [CrossRef]
- Ericsson, I.; Lindhe, J. Effect of longstanding jiggling on experimental marginal periodontitis in the beagle dog. J. Clin. Periodontol. 1982, 9, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Cardaropoli, D.; Gaveglio, L. The influence of orthodontic movement on periodontal tissues level. Semin. Orthod. 2007, 13, 234–245. [Google Scholar] [CrossRef]
- Brezniak, N.; Wasserstein, A. Orthodontically induced inflammatory root resorption. Part I: The basic science aspects. Angle Orthod. 2002, 72, 175–179. [Google Scholar] [PubMed]
- Mosby, E. Mosby’s Dental Dictionary; Elsevier Health Sciences: Amsterdam, The Netherlands, 2007. [Google Scholar]
- Harris, E.F.; Robinson, Q.C.; Woods, M.A. An analysis of causes of apical root resorption in patients not treated orthodontically. Quintessence Int. 1993, 24, 417–428. [Google Scholar] [PubMed]
- Baumrind, S.; Korn, E.L.; Boyd, R.L. Apical root resorption in orthodontically treated adults. Am. J. Orthod. Dentofac. Orthop. 1996, 110, 311–320. [Google Scholar] [CrossRef] [PubMed]
- Sameshima, G.T.; Sinclair, P.M. Predicting and preventing root resorption: Part I. Diagnostic factors. Am. J. Orthod. Dentofac. Orthop. 2001, 119, 505–510. [Google Scholar] [CrossRef]
- Segal, G.; Schiffman, P.; Tuncay, O. Meta analysis of the treatment-related factors of external apical root resorption. Orthod. Craniofacial Res. 2004, 7, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Fox, N. Longer orthodontic treatment may result in greater external apical root resorption. Evid.-Based Dent. 2005, 6, 21. [Google Scholar] [CrossRef] [PubMed]
- Alfuriji, S.; Alhazmi, N.; Alhamlan, N.; Al-Ehaideb, A.; Alruwaithi, M.; Alkatheeri, N.; Geevarghese, A. The effect of orthodontic therapy on periodontal health: A review of the literature. Int. J. Dent. 2014, 2014, 585048. [Google Scholar] [CrossRef] [PubMed]
- Jepsen, S.; Caton, J.G.; Albandar, J.M.; Bissada, N.F.; Bouchard, P.; Cortellini, P.; Demirel, K.; de Sanctis, M.; Ercoli, C.; Fan, J. Periodontal manifestations of systemic diseases and developmental and acquired conditions: Consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45, S219–S229. [Google Scholar] [CrossRef] [PubMed]
- Tonetti, M.S.; Jepsen, S.; Bouchard, P.; Cairo, F.; Eickholz, P.; Graziani, F.; Herrera, D.; Jepsen, S.; Jung, R.; Machtei, E. Clinical efficacy of periodontal plastic surgery procedures: Consensus report of Group 2 of the 10th European Workshop on Periodontology. J. Clin. Periodontol. 2014, 41, S36–S43. [Google Scholar] [CrossRef]
- Renkema, A.M.; Fudalej, P.S.; Renkema, A.A.; Abbas, F.; Bronkhorst, E.; Katsaros, C. Gingival labial recessions in orthodontically treated and untreated individuals: A case–control study. J. Clin. Periodontol. 2013, 40, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Kassab, M.M.; Cohen, R.E. The etiology and prevalence of gingival recession. J. Am. Dent. Assoc. 2003, 134, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Maroso, F.B.; Gaio, E.J.; Rösing, C.K.; Fernandes, M.I. Correlation between gingival thickness and gingival recession in humans. Acta Odontol. Latinoam. 2015, 28, 162–166. [Google Scholar]
- Cannavale, R.; Matarese, G.; Isola, G.; Grassia, V.; Perillo, L. Early treatment of an ectopic premolar to prevent molar-premolar transposition. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 559–569. [Google Scholar] [CrossRef]
- Nibali, L.; Sun, C.; Akcalı, A.; Meng, X.; Tu, Y.K.; Donos, N. A retrospective study on periodontal disease progression in private practice. J. Clin. Periodontol. 2017, 44, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Kloukos, D.; Eliades, T.; Sculean, A.; Katsaros, C. Indication and timing of soft tissue augmentation at maxillary and mandibular incisors in orthodontic patients. A systematic review. Eur. J. Orthod. 2014, 36, 442–449. [Google Scholar] [CrossRef]
- Thilander, B. The role of the orthodontist in the multidisciplinary approach to periodontal therapy. Int. Dent. J. 1986, 36, 12–17. [Google Scholar]
- Re, S.; Corrente, G.; Abundo, R.; Cardaropoli, D. Orthodontic treatment in periodontally compromised patients: 12-year report. Int. J. Periodontics Restor. Dent. 2000, 20, 31–39. [Google Scholar]
- Boyd, R.; Leggott, P.; Quinn, R.; Eakle, W.; Chambers, D. Periodontal implications of orthodontic treatment in adults with reduced or normal periodontal tissues versus those of adolescents. Am. J. Orthod. Dentofac. Orthop. 1989, 96, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Herrera, D.; Sanz, M.; Kebschull, M.; Jepsen, S.; Sculean, A.; Berglundh, T.; Papapanou, P.N.; Chapple, I.; Tonetti, M.S.; Participants, E.W.; et al. Treatment of stage IV periodontitis: The EFP S3 level clinical practice guideline. J. Clin. Periodontol. 2022, 49, 4–71. [Google Scholar] [CrossRef] [PubMed]
- Pini Prato, G.P.; Chambrone, L. Orthodontic treatment in periodontal patients: The use of periodontal gold standards to overcome the “grey zone”. J. Periodontol. 2020, 91, 437–441. [Google Scholar] [CrossRef]
- Levin, L.; Einy, S.; Zigdon, H.; Aizenbud, D.; Machtei, E.E. Guidelines for periodontal care and follow-up during orthodontic treatment in adolescents and young adults. J. Appl. Oral Sci. 2012, 20, 399–403. [Google Scholar] [CrossRef] [PubMed]
- Musilli, M.; Lee, S.; Farella, M.; Paolantoni, G. The Orthodontic-Periodontal Risk Assessment (OPRA) in developing Periodontal Disease. Ann. Di Stomatol. 2020, 11, 16–27. [Google Scholar] [CrossRef]
- Martin, C.; Celis, B.; Ambrosio, N.; Bollain, J.; Antonoglou, G.N.; Figuero, E. Effect of orthodontic therapy in periodontitis and non-periodontitis patients: A systematic review with meta-analysis. J. Clin. Periodontol. 2022, 49, 72–101. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, S.N.; Antonoglou, G.N.; Michelogiannakis, D.; Kakali, L.; Eliades, T.; Madianos, P. Effect of periodontal–orthodontic treatment of teeth with pathological tooth flaring, drifting, and elongation in patients with severe periodontitis: A systematic review with meta-analysis. J. Clin. Periodontol. 2022, 49, 102–120. [Google Scholar] [CrossRef]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Periodontal health during clear aligners treatment: A systematic review. Eur. J. Orthod. 2014, 37, 539–543. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, C.C.O.; Fagundes, N.C.F.; da Costa, G.C.; Normando, D. Clear aligner treatment among patients with compromised periodontal tissue. Semin. Orthod. 2024, 30, 141–145. [Google Scholar] [CrossRef]
- Arn, M.-L.; Dritsas, K.; Pandis, N.; Kloukos, D. The effects of fixed orthodontic retainers on periodontal health: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 156–164.e17. [Google Scholar] [CrossRef] [PubMed]
- Jiang, C.; Fan, C.; Yu, X.; Xu, T.; Cai, J.; Fan, X.; Zhang, J. Comparison of the efficacy of different periodic periodontal scaling protocols for oral hygiene in adolescents with fixed orthodontic appliances: A prospective cohort study. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 435–442. [Google Scholar] [CrossRef] [PubMed]
- Han, J.; Dong, J.; Zhao, H.; Ma, Y.; Yang, S.; Ma, Y. Efficacy of periodontal tissue regeneration combined with orthodontic therapy on periodontitis and its influences on inflammatory factors in patients. J. Biomater. Tissue Eng. 2020, 10, 737–742. [Google Scholar] [CrossRef]
- Geisinger, M.L.; Abou-Arraj, R.V.; Souccar, N.M.; Holmes, C.M.; Geurs, N.C. Decision making in the treatment of patients with malocclusion and chronic periodontitis: Scientific evidence and clinical experience. Semin. Orthod. 2014, 20, 170–176. [Google Scholar] [CrossRef]
- Sadowsky, C.; BeGole, E.A. Long-term effects of orthodontic treatment on periodontal health. Am. J. Orthod. 1981, 80, 156–172. [Google Scholar] [CrossRef] [PubMed]
- Årtun, J.; Urbye, K.S. The effect of orthodontic treatment on periodontal bone support in patients with advanced loss of marginal periodontium. Am. J. Orthod. Dentofac. Orthop. 1988, 93, 143–148. [Google Scholar] [CrossRef]
- Michalowicz, B.S.; Wolff, L.F.; Klump, D.; Hinrichs, J.E.; Aeppli, D.M.; Bouchard Jr, T.J.; Pihlstrom, B.L. Periodontal bacteria in adult twins. J. Periodontol. 1999, 70, 263–273. [Google Scholar] [CrossRef] [PubMed]
- Rasperini, G.; Acunzo, R.; Cannalire, P.; Farronato, G. Influence of Periodontal Biotype on Root Surface Exposure During Orthodontic Treatment: A Preliminary Study. Int. J. Periodontics Restor. Dent. 2015, 35, 655–675. [Google Scholar] [CrossRef]
- Marini, I.; Bortolotti, F.; Parenti, S.I.; Gatto, M.R.; Bonetti, G.A. Combined effects of repeated oral hygiene motivation and type of toothbrush on orthodontic patients: A blind randomized clinical trial. Angle Orthod. 2014, 84, 896–901. [Google Scholar] [CrossRef]
- Jackson, C.L.; Orthod, C. Comparison between electric toothbrushing and manual toothbrushing, with and without oral irrigation, for oral hygiene of orthodontic patients. Am. J. Orthod. Dentofac. Orthop. 1991, 99, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Kurem, I.; Topsakal, U.; Ozturk, T. Evaluation of Multidisciplinary Treatment Relationship between Orthodontics and Periodontology Departments by Examining Inter-Departmental Consultation Notes. Niger. J. Clin. Pract. 2021, 24, 1234–1239. [Google Scholar] [CrossRef] [PubMed]
- Shirozaki, M.U.; da Silva, R.A.B.; Romano, F.L.; da Silva, L.A.B.; De Rossi, A.; Lucisano, M.P.; Messora, M.R.; Feres, M.; Novaes Júnior, A.B. Clinical, microbiological, and immunological evaluation of patients in corrective orthodontic treatment. Prog. Orthod. 2020, 21, 1–8. [Google Scholar] [CrossRef]
- Meyer-Marcotty, P.; Klenke, D.; Knocks, L.; Santander, P.; Hrasky, V.; Quast, A. The adult orthodontic patient over 40 years of age: Association between periodontal bone loss, incisor irregularity, and increased orthodontic treatment need. Clin. Oral Investig. 2021, 25, 6357–6364. [Google Scholar] [CrossRef] [PubMed]
- Meikle, M.C. The tissue, cellular, and molecular regulation of orthodontic tooth movement: 100 years after Carl Sandstedt. Eur. J. Orthod. 2006, 28, 221–240. [Google Scholar] [CrossRef] [PubMed]
- Ong, M.M.; Wang, H.-L. Periodontic and orthodontic treatment in adults. Am. J. Orthod. Dentofac. Orthop. 2002, 122, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Wilcko, W.M.; Wilcko, M.T.; Bouquot, J.; Ferguson, D.J. Rapid orthodontics with alveolar reshaping: Two case reports of decrowding. Int. J. Periodontics Restor. Dent. 2001, 21, 9–20. [Google Scholar]
- Köle, H. Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg. Oral Med. Oral Pathol. 1959, 12, 515–529. [Google Scholar] [CrossRef] [PubMed]
- Amit, G.; Kalra, J.; Pankaj, B.; Suchinder, S.; Parul, B. Periodontally accelerated osteogenic orthodontics (PAOO)—A review. J. Clin. Exp. Dent. 2012, 4, e292. [Google Scholar] [CrossRef]
- AlGhamdi, A.S.T. Corticotomy facilitated orthodontics: Review of a technique. Saudi Dent. J. 2010, 22, 1–5. [Google Scholar] [CrossRef]
- Han, Y.; Miao, L.; Liu, J.; Xu, X.; Yue, Z.; Xu, M.; Shu, C.; Xu, L.; Hou, J. Periodontal soft tissue increase induced by periodontally accelerated osteogenic orthodontics surgery. BMC Oral Health 2022, 22, 506. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, D.D.; Oliveira, B.F.d.; Soares, R.V. Alveolar corticotomies in orthodontics: Indications and effects on tooth movement. Dent. Press J. Orthod. 2010, 15, 144–157. [Google Scholar] [CrossRef]
- Kurohama, T.; Hotokezaka, H.; Hashimoto, M.; Tajima, T.; Arita, K.; Kondo, T.; Ino, A.; Yoshida, N. Increasing the amount of corticotomy does not affect orthodontic tooth movement or root resorption, but accelerates alveolar bone resorption in rats. Eur. J. Orthod. 2017, 39, 277–286. [Google Scholar] [CrossRef] [PubMed]
- Aboul, S.M.B.E.-D.; El-Beialy, A.R.; El-Sayed, K.M.F.; Selim, E.M.N.; El-Mangoury, N.H.; Mostafa, Y.A. Miniscrew implant-supported maxillary canine retraction with and without corticotomy-facilitated orthodontics. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 252–259. [Google Scholar] [CrossRef]
- Kloukos, D.; Roccuzzo, A.; Stähli, A.; Sculean, A.; Katsaros, C.; Salvi, G.E. Effect of combined periodontal and orthodontic treatment of tilted molars and of teeth with intra-bony and furcation defects in stage-IV periodontitis patients: A systematic review. J. Clin. Periodontol. 2022, 49, 121–148. [Google Scholar] [CrossRef]
- Jepsen, K.; Tietmann, C.; Kutschera, E.; Wüllenweber, P.; Jäger, A.; Cardaropoli, D.; Gaveglio, L.; Sanz Sanchez, I.; Martin, C.; Fimmers, R. The effect of timing of orthodontic therapy on the outcomes of regenerative periodontal surgery in patients with stage IV periodontitis: A multicenter randomized trial. J. Clin. Periodontol. 2021, 48, 1282–1292. [Google Scholar] [CrossRef]
- Tietmann, C.; Bröseler, F.; Axelrad, T.; Jepsen, K.; Jepsen, S. Regenerative periodontal surgery and orthodontic tooth movement in stage IV periodontitis: A retrospective practice-based cohort study. J. Clin. Periodontol. 2021, 48, 668–678. [Google Scholar] [CrossRef] [PubMed]
- Nanda, R. Biomechanics and Esthetic Strategies in Clinical Orthodontics; Elsevier Health Sciences: Amsterdam, The Netherlands, 2005. [Google Scholar]
- Krishnan, V.; Kuijpers-Jagtman, A.M.; Davidovitch, Z.E. Controversies and Research Directions in Tooth-movement Research. In Biological Mechanisms of Tooth Movement, 3rd ed.; Wiley: Hoboken, NJ, USA, 2021; pp. 327–342. [Google Scholar] [CrossRef]
- Takahashi, A.; Nagata, M.; Gupta, A.; Matsushita, Y.; Yamaguchi, T.; Mizuhashi, K.; Maki, K.; Ruellas, A.C.; Cevidanes, L.S.; Kronenberg, H.M. Autocrine regulation of mesenchymal progenitor cell fates orchestrates tooth eruption. Proc. Natl. Acad. Sci. USA 2019, 116, 575–580. [Google Scholar] [CrossRef]
- Li, X.-x.; Wang, M.-t.; Wu, Z.-f.; Sun, Q.; Ono, N.; Nagata, M.; Zang, X.-l.; Ono, W. Etiological Mechanisms and Genetic/Biological Modulation Related to PTH1R in Primary Failure of Tooth Eruption. Calcif. Tissue Int. 2024, 115, 101–116. [Google Scholar] [CrossRef] [PubMed]
- Hajishengallis, G. Immunomicrobial pathogenesis of periodontitis: Keystones, pathobionts, and host response. Trends Immunol. 2014, 35, 3–11. [Google Scholar] [CrossRef] [PubMed]

| Adjunctive Periodontal Therapy in Orthodontics | ||
|---|---|---|
| Goals | ||
| Corticotomy | Accelerate orthodontic movement in the area in which was a corticotomy procedure was performed. | [77] |
| Regenerative | Regenerate soft and hard periodontal tissue to allow for the closure of the periodontal pocket and reduction in bone defects. Better anchorage during the orthodontic movement is another benefit obtained from this surgical procedure. | [58,59,83,84,85] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Viglianisi, G.; Polizzi, A.; Lombardi, T.; Amato, M.; Grippaudo, C.; Isola, G. Biomechanical and Biological Multidisciplinary Strategies in the Orthodontic Treatment of Patients with Periodontal Diseases: A Review of the Literature. Bioengineering 2025, 12, 49. https://doi.org/10.3390/bioengineering12010049
Viglianisi G, Polizzi A, Lombardi T, Amato M, Grippaudo C, Isola G. Biomechanical and Biological Multidisciplinary Strategies in the Orthodontic Treatment of Patients with Periodontal Diseases: A Review of the Literature. Bioengineering. 2025; 12(1):49. https://doi.org/10.3390/bioengineering12010049
Chicago/Turabian StyleViglianisi, Gaia, Alessandro Polizzi, Teresa Lombardi, Mariacristina Amato, Cristina Grippaudo, and Gaetano Isola. 2025. "Biomechanical and Biological Multidisciplinary Strategies in the Orthodontic Treatment of Patients with Periodontal Diseases: A Review of the Literature" Bioengineering 12, no. 1: 49. https://doi.org/10.3390/bioengineering12010049
APA StyleViglianisi, G., Polizzi, A., Lombardi, T., Amato, M., Grippaudo, C., & Isola, G. (2025). Biomechanical and Biological Multidisciplinary Strategies in the Orthodontic Treatment of Patients with Periodontal Diseases: A Review of the Literature. Bioengineering, 12(1), 49. https://doi.org/10.3390/bioengineering12010049











