Chronic Primary Tinnitus: A Management Dilemma
Abstract
1. Introduction
Clinical Evaluation
2. Materials and Methods
2.1. Design
2.2. Inclusion and Exclusion Criteria
3. Results
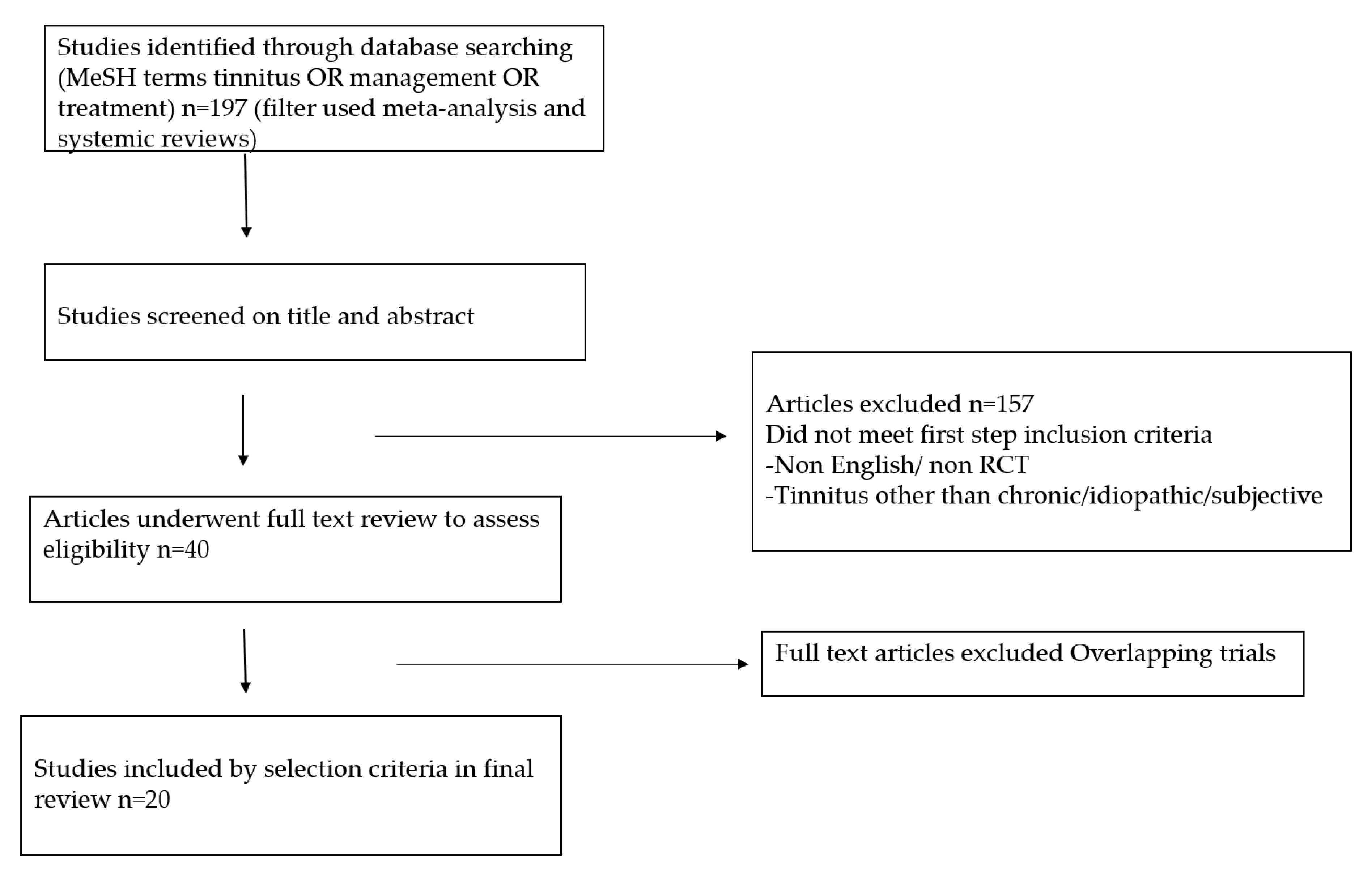
3.1. Identification and Selection of Reviews
3.2. Treatment
3.2.1. Sound Therapy
3.2.2. Cochlear Implant (CI)
3.2.3. Tinnitus Retraining Therapy (TRT)
3.2.4. Transcranial Magnetic Stimulation (TMS)
3.2.5. Cognitive Behavioral Therapy (CBT)
3.2.6. Anticonvulsants
- Increasing the inhibitory neurotransmitter GABA
- Decreasing the excitatory glutamate transmission
- Blocking the sodium channels
3.2.7. Antidepressant and Anxiolytic
3.2.8. Gingko Biloba
3.2.9. Zinc Supplementation
3.2.10. Betahistine
3.2.11. Hyperbaric Oxygen Therapy (HBOT)
3.2.12. Educational Counseling
3.2.13. Acupuncture
3.2.14. Future Therapies
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jastrebof, P.J.; Hazell, J.W.P. Tinnitus Retraining Therapy: Implementing the Neurophysiological Model; Cambridge University Press: New York, NY, USA, 2004. [Google Scholar]
- Jastreboff, P.J.; Brennan, J.F.; Coleman, J.K.; Sasaki, C.T. Phantom auditory sensation in rats: An animal model for tinnitus. Behav. Neurosci. 1988, 102, 811–822. [Google Scholar] [CrossRef]
- Dauman, R.; Tyler, R.S. Some Considerations on the Classification of Tinnitus. In Proceedings of the 4th International Tinnitus Seminar, Bordeaux, France; Kugler publications: Amsterdam, NY, USA, 1991; pp. 225–229. [Google Scholar]
- Gallus, S.; Lugo, A.; Garavello, W.; Bosetti, C.; Santoro, E.; Colombo, P.; Perin, P.; la Vecchia, C.; Langguth, B. Prevalence and determinants of tinnitus in the Italian adult population. Neuroepidemiology 2015, 45, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Hall, D.A.; Láinez, M.J.A.; Sanchez, C.W.N.G.; Egler, M.; Tennigkeit, F.; Koch, M.; Langguth, B. Treatment options for subjective tinnitus: Self reports from a sample of general practitioners and ENT physicians within Europe and the USA. BMC Health Serv. Res. 2011, 11, 302. [Google Scholar] [CrossRef] [PubMed]
- Fowler, E. Head noises in normal and in disordered ears: Significance, measurement, differentiation and treatment. Arch. Otolaryngol. 1944, 39, 498–503. [Google Scholar] [CrossRef]
- Sanchez, T.G.; Ferrari, G.M.S. The control of tinnitus through hearing aids: Suggestions for optimal use. Pró-Fono Rev. Atualização Científica 2002, 14, 111–118. [Google Scholar]
- Baguley, D.; McFerran, D.; Hall, D. Tinnitus. Lancet 2013, 382, 1600–1607. [Google Scholar] [CrossRef]
- Schaette, R.; McAlpine, D. Tinnitus with a normal audiogram: Physiological evidence for hidden hearing loss and computational model. J. Neurosci. 2011, 31, 13452–13457. [Google Scholar] [CrossRef]
- Kujawa, S.G.; Liberman, M.C. Adding insult to injury: Cochlear nerve degeneration after “temporary” noise-induced hearing loss. J. Neurosci. 2009, 29, 14077–14085. [Google Scholar] [CrossRef]
- Henry, J.A.; Dennis, K.C.; Schechter, M.A. General review of tinnitus: Prevalence, mechanisms, effects, and management. J. Speech Lang. Hear. Res. 2005, 48, 1204–1235. [Google Scholar] [CrossRef]
- Claussen, C.F. Rakel & Bope: Conn’s Current Therapy, 60th ed.; Elsevier Inc.: Philadelphia, PA, USA, 2008. [Google Scholar]
- Qiu, C.; Salvi, R.; Ding, D.; Burkard, R. Inner hair cell loss leads to enhanced response amplitudes in auditory cortex of unanesthetized chinchillas: Evidence for increased system gain. Hear Res. 2000, 139, 153–171. [Google Scholar] [CrossRef]
- Cueva, R.A. Auditory brainstem response versus magnetic resonance imaging for the evaluation of asymmetric sensorineural hearing loss. Laryngoscope 2004, 114, 1686–1692. [Google Scholar] [CrossRef] [PubMed]
- Fortnum, H.; O’Neill, C.; Taylor, R.; Lenthall, R.; Nikolopoulos, T.; Lightfoot, G.; O’Donoghue, G.; Mason, S.; Baguley, D.; Jones, H.; et al. The role of magnetic resonance imaging in the identification of suspected acoustic neuroma: A systematic review of clinical and cost effectiveness and natural history. Health Technol. Assess. 2009, 13, 18. [Google Scholar] [CrossRef] [PubMed]
- Milloy, V.; Fournier, P.; Benoit, D.; Noreña, A.; Koravand, A. Auditory Brainstem Responses in Tinnitus: A Review of Who, How, and What? Front. Aging Neurosci. 2017, 9, 237. [Google Scholar] [CrossRef] [PubMed]
- Henry, J.A. “Measurement” of Tinnitus. Otol. Neurotol. 2016, 37, e276–e285. [Google Scholar] [CrossRef] [PubMed]
- Newman, C.W.; Jacobson, G.P.; Spitzer, J.B. Development of the Tinnitus Handicap Inventory. Arch Otolaryngol. Head Neck Surg. 1996, 122, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Henry, J.A.; Griest, S.; Thielman, E.; McMillan, G.; Kaelin, C.; Kathleen; Carlson, F. Tinnitus Functional Index: Development, validation, outcomes research, and clinical application. Hear. Res. 2016, 334, 58–64. [Google Scholar] [CrossRef]
- Carmen, R.; Uram, S. Hearing loss and anxiety in adults. Hear. J. 2002, 55, 48–50. [Google Scholar] [CrossRef]
- Surr, R.K.; Montgomery, A.A.; Mueller, H.G. Effect of amplification on tinnitus among new hearing aid users. Ear Hear. 1985, 6, 71–75. [Google Scholar] [CrossRef]
- Sereda, M.; Xia, J.; El Refaie, A.; Hall, D.A.; Hoare, D.J. Sound therapy (using amplification devices and/or sound generators) for tinnitus in adults. Cochrane Database Syst. Rev. 2018, 12. [Google Scholar] [CrossRef]
- Hobson, J.; Chisholm, E.; El Refaie, A. Sound therapy (masking) in the management of tinnitus in adults. Cochrane Database Syst. Rev. 2012, 11. [Google Scholar] [CrossRef]
- Hoare, D.J.; Edmondson-Jones, M.; Sereda, M.; Akeroyd, M.A.; Hall, D. Amplification with hearing aids for patients with tinnitus and co-existing hearing loss. Cochrane Database Syst. Rev. 2014, 1. [Google Scholar] [CrossRef] [PubMed]
- Baguley, D.M.; Atlas, M.D. Cochlear implants and tinnitus. Prog. Brain Res. 2007, 166, 347–355. [Google Scholar] [PubMed]
- Levy, D.A.; Lee, J.A.; Nguyen, S.A.; McRackan, T.R.; Meyer, T.A.; Lambert, P.R. Cochlear Implantation for Treatment of Tinnitus in Single-sided Deafness: A Systematic Review and Meta-analysis. Otol. Neurotol. 2020, 41, e1004–e1012. [Google Scholar] [CrossRef] [PubMed]
- Phillips, J.S.; McFerran, D.J. Tinnitus Retraining Therapy (TRT) for tinnitus. Cochrane Database Syst. Rev. 2010, 3. [Google Scholar] [CrossRef]
- Barker, A.T.; Jalinous, R.; Freeston, I.L. Non-invasive magnetic stimulation of human motor cortex. Lancet 1985, 1, 1106–1107. [Google Scholar] [CrossRef]
- Meng, Z.; Liu, S.; Zheng, Y.; Phillips, J.S. Repetitive transcranial magnetic stimulation for tinnitus. Cochrane Database Syst. Rev. 2011, 10. [Google Scholar] [CrossRef]
- Chen, J.-J.; Zeng, B.-S.; Wu, C.-N.; Stubbs, B.; Carvalho, A.F.; Brunoni, A.R.; Su, K.-P.; Tu, Y.-K.; Wu, Y.-C.; Chen, T.-Y.; et al. Association of Central Noninvasive Brain Stimulation Interventions With Efficacy and Safety in Tinnitus Management: A Meta-analysis. AMA Otolaryngol. Neck Surg. 2020, 146, 801–809. [Google Scholar] [CrossRef]
- Fuller, T.; Cima, R.; Langguth, B.; Mazurek, B.; Vlaeyen, J.W.; Hoare, D.J. Cognitive behavioural therapy fortinnitus. Cochrane DatabaseSyst. Rev. 2020, 1. [Google Scholar] [CrossRef]
- Landry, E.C.; Sandoval, X.C.R.; Simeone, C.N.; Tidball, G.; Lea, J.; Westerberg, B.D. Systematic Review and Network Meta-analysis of Cognitive and/or Behavioral Therapies (CBT) for Tinnitus. Otol. Neurotol. 2019, 41, 153–166. [Google Scholar] [CrossRef]
- Martinez-Devesa, P.; Perera, R.; Theodoulou, M.; Waddell, A. Cognitive behavioural therapy for tinnitus. Cochrane Database Syst. Rev. 2010, 9. [Google Scholar] [CrossRef]
- Hesser, H.; Weise, C.; Westin, V.Z.; Andersson, G. A systematic review and meta-analysis of randomized controlled trials of cognitive-behavioral therapy for tinnitus distress. Clin. Psychol. Rev. 2011, 31, 545–553. [Google Scholar] [CrossRef]
- Hoekstra, C.E.L.; Rynja, S.P.; van Zanten, G.A.; Rovers, M.M. Anticonvulsants for tinnitus. Cochrane Database Syst. Rev. 2010, 7. [Google Scholar] [CrossRef]
- McFerran, D.J.; Baguley, D. The efficacy of treatments for depression used in the management of tinnitus. Audiol. Med. 2008, 6, 40–47. [Google Scholar] [CrossRef]
- Baldo, P.; Doree, C.; Molin, P.; McFerran, D.J.; Cecco, S. Antidepressants for patients with tinnitus. Cochrane Database Syst. Rev. 2012, 9. [Google Scholar] [CrossRef]
- Tunkel, D.E.; Bauer, C.A.; Sun, G.H.; Rosenfeld, R.M. Clinical practice guideline: Tinnitus. Otolaryngol. Head Neck Surg. 2014, 151 (Suppl. 2), S1–S40. [Google Scholar] [CrossRef]
- Költringer, P.; Eber, O.; Klima, G.; Rothlauer, W.; Wakonig, P.; Langsteger, W.; Lind, P. Microcirculation in parenteral Ginkgo biloba extract therapy [Die Mikrozirkulation unter parenteraler Ginkgo–biloba–Extrakt–Therapie]. Wien. Klin. Wochenschr. 1989, 101, 198–200. [Google Scholar]
- Braquet, P.; Hosford, D. Ethnopharmacology and the development of natural PAF antagonists as therapeutic agents. J. Ethnopharmacol. 1991, 32, 135–139. [Google Scholar] [CrossRef]
- De Feudis, F.V. Ginkgo biloba Extract (EGb 761): Pharmacological Activities and Clinical Applications. Editions Scientifiques; Elsevier: Paris, France, 1991; pp. 68–73. [Google Scholar]
- Ernst, E.; Stevinson, C. Ginkgo biloba for tinnitus: A review. Clin. Otolaryngol. 1999, 24, 164–167. [Google Scholar] [CrossRef]
- Hilton, M.P.; Zimmermann, E.F.; Hunt, W.T. Ginkgo biloba for tinnitus. Cochrane Database Syst. Rev. 2013, 3. [Google Scholar] [CrossRef]
- Drescher, M.J.; Drescher, D.G. Glutamate, of the endogenous primary a-amino acids, is specifically released from hair cells by elevated extracellular potassium. J. Neurochem. 1992, 59, 93–98. [Google Scholar] [CrossRef]
- Person, O.C.; Puga, M.E.S.; da Silva, E.M.K.; Torloni, M.R. Zinc supplementation for tinnitus. Cochrane Database Syst. Rev. 2016, 11. [Google Scholar] [CrossRef] [PubMed]
- Martinez, D.M. The eBect of Serc (betahistine hydrochloride) on the circulation of the inner ear in experimental animals. Acta Oto-laryngologica. Supplementum 1972, 305, 29–47. [Google Scholar]
- Wegner, I.; Hall, D.A.; Smit, A.L.; McFerran, D.; Stegeman, I. Betahistine for tinnitus. Cochrane Database Syst. Rev. 2018, 12. [Google Scholar] [CrossRef] [PubMed]
- Bennett, M.H.; Kertesz, T.; Perleth, M.; Yeung, P.; Lehm, J.P. Hyperbaric oxygen for idiopathic sudden sensorineural hearing loss and tinnitus. Cochrane Database Syst. Rev. 2012, 10. [Google Scholar] [CrossRef] [PubMed]
- Xiang, T.; Zhong, J.; Lu, T.; Pu, J.M.; Liu, L.; Xiao, Y.; Lai, D. Effect of educational counseling alone on people with tinnitus: Meta-analysis of randomized controlled trials. Patient Educ. Couns. 2020, 103, 44–54. [Google Scholar] [CrossRef] [PubMed]
- Huang, K.; Liang, S.; Chen, L.; Grellet, A. Acupuncture for tinnitus: A systematic review and meta-analysis of randomized controlled trials. Acupunct. Med. 2020, 10. [Google Scholar] [CrossRef]
- Duckert, L.G.; Rees, T.S. Placebo Effect in Tinnitus Management. Otolaryngol. Head Neck Surg. 1984, 92, 697–699. [Google Scholar] [CrossRef]
- Ryals, B.M.; Dent, M.L.; Dooling, R.J. Return of function after hair cell regeneration. Hear. Res. 2013, 297, 113–120. [Google Scholar] [CrossRef]
- Zhao, Z.; Krishnaney, A.; Teng, Q.; Yang, J.; Garrity-Moses, M.; Liu, J.K.; Venkiteswaran, K.; Subramanian, T.; Davis, M.; Boulis, N. Anatomically discrete functional effects of adenoviral clostridial light chain gene-based synaptic inhibition in the midbrain. Gene Ther. 2000, 13, 942–952. [Google Scholar] [CrossRef]
- Elgoyhen, A.B.; Vetter, D.E.; Katz, E.; Rothlin, C.V.; Heinemann, S.F.; Boulter, J. alpha10: A determinant of nicotinic cholinergic receptor function in mammalian vestibular and cochlear mechanosensory hair cells. Proc. Natl. Acad. Sci. USA 2001, 98, 3501–3506. [Google Scholar] [CrossRef]
- Plazas, P.V.; Savino, J.; Kracun, S.; Gomez-Casati, M.E.; Katz, E.; Parsons, C.G.; Millar, N.S.; Elgoyhen, A.B. Inhibition of the alpha9alpha10 nicotinic cholinergic receptor by neramexane, an open channel blocker of N-methyl-D-aspartate receptors. Eur. J. Pharmacol. 2007, 566, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Shemirani, N.; Tang, D.; Friedland, D. Acute Auditory and Vestibular Symptoms Associated With Heat and Transdermal Lidocaine. Clin. J. Pain 2010, 26, 58–59. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Ding, D.L.; Wang, P.; Sun, J.; Jin, X.; Salvi, R.J. Substance P inhibits potassium and calcium currents in inner ear spiral ganglion neurons. Brain Res. 2004, 1012, 82–92. [Google Scholar] [CrossRef] [PubMed]
| s.n | Study | No of RCT/ Pt | Intervention | Comparator | Outcome (95% CI) | Level of Evidence |
|---|---|---|---|---|---|---|
| 1. | Fuller et al. | 28/2733 | CBT | No intervention (10 RCT/ 537) | SMD 0.56 lower (0.83 lower to 0.30) | low |
| Audiological care (3 RCT/ 430) | MD 5.65 lower (9.79 lower to 1.5 lower) | moderate | ||||
| TRT (1 RCT/42) | MD 15.79 lower (27.91 lower to 3.67) | low | ||||
| Active control (12 RCT/966) | SMD 0.30 lower (0.55 lower to. 0.05) | low | ||||
| 2. | Martinez et al. | 8/468 | CBT | no intervention(6RCT/354) | SMD 0.24 (−0.02 to 0.051) | - |
| Yoga/education (4/164) | SMD 0.1 (−0.22 to 0.42) | - | ||||
| 3. | Landry et al. | 11/1111 | CBT | no intervention (11RCT/1111) | SMD 1.46 (0.67 to 2.24) | low |
| 4. | Hesser et al. | 15/1091 | CBT | no intervention (14RCT) | SMD 0.70 (0.56 to 0.84 | low |
| Education /TRT/yoga (5RCT) | SMD 0.44 (0.16 to 0.72) | low | ||||
| 5. | Baldo et al. | 6/610 | TCA | different trials could not be combined | ||
| 6. | Bennett et al. | 2/83 | HBOT | sham / pharmacological therapy | RR 0.68 (0.32 to 1.42) | moderate |
| 7. | Hilton et al. | 4/1543 | ginkgobiloba | placebo, different trials could not be combined | low | |
| 8. | Hoare et al. | 1/91 | hearing aids | sound generators | MD −0.90 (−7.92 to 6.12) | moderate |
| 9. | Hobson et al. | 6/533 | sound therapy | different trials could not be combined | ||
| 10. | Hoekstra et al. | 7/453 | Gabapentin | Placebo | SMD 0.07 (−0.26 to 0.40) | low |
| 11. | Huang et al. | 8/504 | acupuncture | sham acupuncture | MD −2.18 (−4.89 to 0.53) | low |
| Drug therapy | MD −1.33 (−2.01 to −0.65) | low | ||||
| 12. | Levy et al. | 17/247 | CI | Pt prior to intervention | VAS MD −4.6 (−6 to −3.3) | low |
| THI MD −35.4 (−55.8 to −15) | ||||||
| 13. | Meng et al. | 5/233 | r TMS | sham r TMS | RR 12 (1.76 to 81.74) | moderate |
| 14. | Dong et al. | 10/567 | r TMS | sham r TMS | VAS SMD −0.28 (−0.59 to 0.02) | moderate |
| THI SMD −0.04 (−0.23 to 0.16) | ||||||
| 15. | Chen et al. | 32/1458 | central NIBS | Sham control | SMD −1.89 (−3 to −0.78) | moderate |
| 16. | Person et al. | 3/209 | zinc | different trials could not be combined | very low | |
| 17. | Philips et al. | 1/123 | TRT | tinnitus masking | low | |
| 18. | Sereda et al. | 8/590 | sound therapy | different trials could not be combined | low | |
| 19. | Xiang et al. | 9/582 | educational counseling | other psychological and combination therapy | MD 3.59 (−0.56 to 7.74) | moderate |
| 20. | Wegner et al. | 5/303 | Betahistine | Placebo | MD −0.16 (−1.01 to 0.70 | very low |
| Review | Primary Outcome | Review Author Conclusion | Overview Author Conclusion |
|---|---|---|---|
| Fuller et al. | THI score | CBT may be effective in reducing the negative impact on quality of life | CBT is a cost effective measure, helpful in alleviating tinnitus associated negative impact on patient’s life, though it may not reduce the tinnitus volume. |
| Martin et al. | Tinnitus loudness (VAS) | CBT is unlikely to be effective in improving subjective tinnitus loudness but effective for improving quality of life | |
| Landry et al. | QOL | CBT had larger effect sizes on tinnitus-related QOL | |
| Hesser et al. | QOL | CBT is an effective treatment in reducing annoyance and distress associated with tinnitus | |
| Baldo et al. | Tinnitus severity and disability | No evidence that TCA are effective in management of tinnitus | Further trials with uniform robust methodology are required to compare the results and derive any conclusions |
| Bennet et al. | Relief of tinnitus | No suggestion that HBOT improves chronic tinnitus | Only two trials report outcome for chronic tinnitus (demand a cautious interpretation owing to low no of patients) |
| Hilton et al. | Tinnitus loudness (VAS), Tinnitus associated QOL | Not demonstrated to be effective for primary tinnitus | Further high quality trials with uniform methodology are required |
| Hoare et al. | Tinnitus severity | No evidence to support or refute the use of hearing aids | The benefit of sound therapy alone in the treatment of tinnitus is unproven. Use of hearing aid improves the hearing handicap and quality of life. Further trials are required to support the efficacy of hearing aids in tinnitus handicap. |
| Hobson et al. | Tinnitus loudness, QOL | No evidence that a significant change in loudness of tinnitus can be achieved by sound generator as solo intervention | Further trials with uniform methodology are required for analysis |
| Hoekstra et al. | Tinnitus specific health related QOL | Do not show a beneficial effect on tinnitus (significant risk of bias) | Further methodological trials of high quality are required |
| Huang et al. | Tinnitus loudness (VAS) | Did not have significant impact on tinnitus loudness but did improve tinnitus specific health related QOL | Further high quality studies are required to confirm the efficacy of acupuncture |
| Levy et al. | Tinnitus specific health related QOL, Tinnitus loudness (VAS) | Significant reduction in THI and VAS score | Cochlear implant is an effective treatment strategy in patients with severe to profound hearing loss. Further trials of high quality are needed to support their use for tinnitus. |
| Person et al. | Tinnitus severity and disability (THI) | No evidence that the use of oral zinc improve tinnitus | Further trials with uniform methodology are warranted to analyse the results |
| Philips et al. | Tinnitus severity and disability (THI) | TRT is much more effective than tinnitus masking | Single low quality RCT. Further high quality studies with robust methodology are required using protocols as proposed by Jastreboff 1999 |
| Dang et al. | Tinnitus severity and disability (THI), tinnitus loudness | rTMS not effective in treating chronic tinnitus | Further studies with uniform protocols are needed to explore the potential benefits of r TMS in chronic tinnitus |
| Chen et al. | Tinnitus severity | Central noninvasive brain stimulation is associated with improvement in tinnitus severity | |
| Meng et al. | Tinnitus severity and disability (THI) | Limited support for the efficacy of rTMS in treating patients with tinnitus | |
| Xiang et al. | Tinnitus severity | Educational counseling alone is helpful in improving tinnitus and has same effect as other psychological and combined treatment | It is a cost effective measure useful in decreasing tinnitus-related negative impact on the patient’s life. |
| Wegner et al. | Tinnitus loudness | Absence of any evidence suggestive of beneficial effect of betahistine on tinnitus | High quality trials are required to derive any conclusion |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soni, A.; Dubey, A. Chronic Primary Tinnitus: A Management Dilemma. Audiol. Res. 2020, 10, 55-66. https://doi.org/10.3390/audiolres10020010
Soni A, Dubey A. Chronic Primary Tinnitus: A Management Dilemma. Audiology Research. 2020; 10(2):55-66. https://doi.org/10.3390/audiolres10020010
Chicago/Turabian StyleSoni, Annanya, and Abhishek Dubey. 2020. "Chronic Primary Tinnitus: A Management Dilemma" Audiology Research 10, no. 2: 55-66. https://doi.org/10.3390/audiolres10020010
APA StyleSoni, A., & Dubey, A. (2020). Chronic Primary Tinnitus: A Management Dilemma. Audiology Research, 10(2), 55-66. https://doi.org/10.3390/audiolres10020010




