Effectiveness of a Worksite-Based Lifestyle Intervention on Employees’ Obesity Control and Prevention in China: A Group Randomized Experimental Study
Abstract
1. Introduction
2. Methods
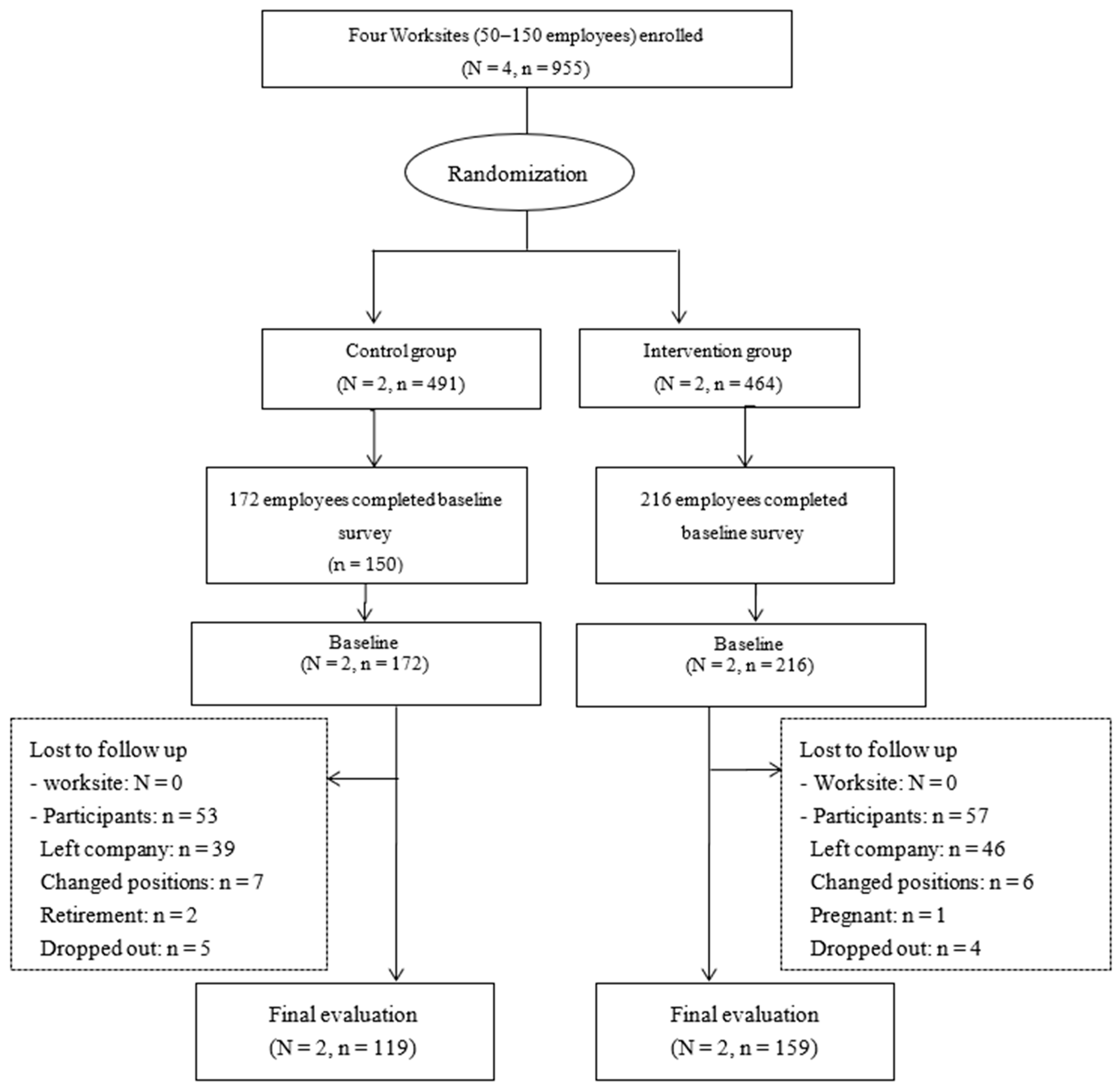
2.1. Study Design and Subjects
2.2. Worksites
2.3. Participants
2.4. Randomization and Blinding
2.5. Measures
2.5.1. Control Worksites
2.5.2. Intervention Worksites
- (1)
- Individual level
- Six lectures on weight management, healthy diets, physical activities and health preservation of traditional Chinese Medicine were given once every two months from January 2018 to November 2018.
- Health information about weight-related lifestyle changes was pushed by the WeChat Subscription—“Official Health Management” 2–3 times weekly, as well as the enquiry of dietary energy and energy consumption of various sports being provided throughout the intervention period. This was also available to all employees in the intervention worksite.
- Several diet and exercise teams were set up voluntarily based on employees’ interests and personal relationships to monitor and improve their daily behaviors by recording the daily diet or exercise and remind each other. Team members were asked to record their daily diet or exercise. In addition, members of the diet teams supervised what each other ate and drank during meals and snacks, and the person with unhealthy food would be reminded by others on the spot. Members of the exercise teams went to exercise regularly at the agreed time and place. For example, the members of the walking team reminded each other after lunch every day and walked together along the set route.
- Walking routes and activities suitable for the workplaces were designed and opened to all employees in each worksite to improve employees’ access to physical activities.
- Automatic ranking of daily steps was provided by the WeChat Subscription of this study and material rewards were provided by the worksites to enhance employees’ enthusiasm to participate in the activities.
- (2)
- Environmental level
- A kick-off event was held at each worksite to introduce the program to the employees.
- Posters about health, diets, and physical activities were displayed on the bulletin board at the worksites.
- Food models and scales were placed at the gate, restroom or conference room.
- Signs encouraging walking were posted beside elevators and stairs at workplaces.
- A fitness area was set up at each worksite for the employees where some sport equipment was provided freely.
- The environment of dining area and snack bar of the worksites was improved. The food calories were displayed in the dining area. The supplies of healthy food were increased including fruit, milk and waters while the supplies of high-calorie food such as instant noodles, french fries and Coca Cola were reduced in the snack bar of worksites. A certain discount was also encouraged to offer to staff on healthy food.
- The “Award for healthy diet showing” and “Exercise challenge” activities were launched for all employees at worksites based on WeChat Subscription to facilitate healthy diet and physical activities maintenance.
- (3)
- Organizational level
- An employee advisory board (EAB), which consisted of four to seven employees from all occupational sectors in the worksite, was established in each worksite and worked closely with research team to design and implement intervention activities [51].
- Positive policies were created in worksites including food subsidy policies for snack bars, financial policies for clubs and groups of dietary and activities and reward policies for “Exercise challenge” and “Show healthy diet and win prizes”.
2.6. Outcomes
- (1)
- Primary outcomes
- (2)
- Secondary outcomes
- Assessment of Dietary Behavior
- Assessment of Physical Activities
2.7. Data Collection
2.8. Statistical Analysis
3. Results
- (1)
- Weight-related indicators
- (2)
- Dietary behaviors
- (3)
- Physical activities
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pan, X.-F.; Wang, L.; Pan, A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021, 9, 373–392. [Google Scholar] [CrossRef]
- Wang, Y.F.; Sun, M.X.; Xue, H.; Zhao, W.H.; Yang, X.G.; Zhu, X.Y.; Zhao, L.; Yang, Y.X. China Blue Paper on Obesity Prevention and Control; Peking University Medical Press: Beijing, China, 2019. [Google Scholar]
- Wang, L. Chinese National Nutrition and Health Survey (2002): Comprehensive Summary; People’s Medical Publishing House: Beijing, China, 2005. (In Chinese) [Google Scholar]
- Chang, J.; Wang, Y.; Liang, X.; Wu, L.; Ding, G. Chinese National Nutrition and Health Survey (2010–2013): Comprehensive Summary; Peking University Medical Press: Beijing, China, 2016. (In Chinese) [Google Scholar]
- GBD 2015 Obesity Collaborators; Afshin, A.; Forouzanfar, M.H.; Reitsma, M.B.; Sur, P.; Estep, K.; Lee, A.; Marczak, L.; Mokdad, A.H.; Moradi-Lakeh, M.; et al. Health effects of overweight and obesity in 195 countries over 25 years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chen, Y.; Liang, X.; Zheng, S.; Wang, Y.; Lu, W. Association of body fat mass and fat distribution with the incidence of hypertension in a population-based chinese cohort: A 22-year follow-up. J. Am. Heart Assoc. 2018, 7, e007153. [Google Scholar] [CrossRef] [PubMed]
- Momin, M.; Fan, F.; Li, J.; Jia, J.; Zhang, L.; Zhang, Y.; Huo, Y. Joint effects of body mass index and waist circumference on the incidence of hypertension in a community-based chinese population. Obes. Facts 2020, 13, 245–255. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.; Wu, Y.; Yang, J.; Li, Y.; Zhang, H.; Zhao, L. Overweight is an independent risk factor for cardiovascular disease in Chinese populations. Obes. Rev. 2002, 3, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Li, J.; Xue, H.; Li, Y.; Huang, J.; Mai, J.; Chen, J.; Cao, J.; Wu, X.; Guo, D.; et al. Type 2 diabetes mellitus incidence in Chinese: Contributions of overweight and obesity. Diabetes Res. Clin. Pract. 2015, 107, 424–432. [Google Scholar] [CrossRef]
- Bragg, F.; Tang, K.; Guo, Y.; Iona, A.; Du, H.; Holmes, M.V.; Bian, Z.; Kartsonaki, C.; Chen, Y.; Yang, L.; et al. Associations of general and central adiposity with incident diabetes in chinese men and women. Diabetes Care 2018, 41, 494–502. [Google Scholar] [CrossRef]
- Mi, B.; Wu, C.; Gao, X.; Wu, W.; Du, J.; Zhao, Y.; Wang, D.; Dang, S.; Yan, H. Long-term BMI change trajectories in Chinese adults and its association with the hazard of type 2 diabetes: Evidence from a 20-year China Health and Nutrition Survey. BMJ Open Diabetes Res. Care 2020, 8, e000879. [Google Scholar] [CrossRef]
- Zhang, X.; Shu, X.-O.; Gao, Y.-T.; Yang, G.; Li, H.; Zheng, W. General and abdominal adiposity and risk of stroke in Chinese women. Stroke 2009, 40, 1098–1104. [Google Scholar] [CrossRef]
- Chen, Z.; Iona, A.; Parish, S.; Chen, Y.; Guo, Y.; Bragg, F.; Yang, L.; Bian, Z.; Holmes, M.V.; Lewington, S.; et al. Adiposity and risk of ischaemic and haemorrhagic stroke in 0·5 million Chinese men and women: A prospective cohort study. Lancet Glob. Health 2018, 6, e630–e640. [Google Scholar] [CrossRef]
- Li, H.; Yang, G.; Xiang, Y.-B.; Gao, J.; Zhang, X.; Zheng, W.; Gao, Y.-T.; Shu, X.-O. Body weight, fat distribution and colorectal cancer risk: A report from cohort studies of 134 255 Chinese men and women. Int. J. Obes. 2013, 37, 783–789. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Andersen, S.W.; Wen, W.; Gao, Y.-T.; Lan, Q.; Rothman, N.; Ji, B.-T.; Yang, G.; Xiang, Y.-B.; Shu, X.-O.; et al. Prospective cohort study of general and central obesity, weight change trajectory and risk of major cancers among Chinese women. Int. J. Cancer 2016, 139, 1461–1470. [Google Scholar] [CrossRef] [PubMed]
- Pang, Y.; Kartsonaki, C.; Guo, Y.; Chen, Y.; Yang, L.; Bian, Z.; Bragg, F.; Millwood, I.Y.; Mao, E.; Li, Y.; et al. Adiposity and risks of colorectal and small intestine cancer in Chinese adults: A prospective study of 0.5 million people. Br. J. Cancer 2018, 119, 248–250. [Google Scholar] [CrossRef] [PubMed]
- Pang, Y.; Holmes, M.V.; Kartsonaki, C.; Guo, Y.; Yang, L.; Bian, Z.; Chen, Y.; Bragg, F.; Iona, A.; Millwood, I.Y.; et al. Young adulthood and adulthood adiposity in relation to incidence of pancreatic cancer: A prospective study of 0.5 million Chinese adults and a meta-analysis. J. Epidemiol. Commun. Health 2017, 71, 1059–1067. [Google Scholar] [CrossRef]
- Peeters, A.; Barendregt, J.J.; Willekens, F.; MacKenbach, J.P.; Mamun, A.; Bonneux, L. Obesity in adulthood and its consequences for life expectancy: A life-table analysis. Ann. Intern. Med. 2003, 138, 24–32. [Google Scholar] [CrossRef]
- Graf, S.C.; Ferrari, N.; Eiser, S. Obesity- status quo and therapeutic approaches. MMW Fortschritte der Medizin 2013, 155, 91–96. [Google Scholar] [CrossRef]
- World Health Organization. Global Health Risk: Mortality and Burden of Disease Attributable to Selected Major Risks; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Cash, S.W.; Beresford, S.A.A.; Henderson, J.A.; McTiernan, A.; Xiao, L.; Wang, C.Y.; Patrick, D.L. Dietary and physical activity behaviours related to obesity-specific quality of life and work productivity: Baseline results from a worksite trial. Br. J. Nutr. 2012, 108, 1134–1142. [Google Scholar] [CrossRef]
- Flegal, K.M.; Kruszon-Moran, D.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Trends in obesity among adults in the United States, 2005 to 2014. JAMA 2016, 315, 2284–2291. [Google Scholar] [CrossRef]
- Harris, J.R.; Hannon, P.A.; Beresford, S.A.; Linnan, L.A.; McLellan, D.L. Health promotion in smaller workplaces in the United States. Annu. Rev. Public Health 2014, 35, 327–342. [Google Scholar] [CrossRef]
- Du, S.F.; Wang, H.; Zhang, B.; Zhai, F.; Popkin, B.M. China in the period of transition from scarcity and extensive undernutrition to emerging nutrition-related non-communicable diseases, 1949–1992. Obes. Rev. 2014, 15, 8–15. [Google Scholar] [CrossRef]
- Gong, P.; Liang, S.; Carlton, E.J.; Jiang, Q.; Wu, J.; Wang, L.; Remais, J.V. Urbanisation and health in China. Lancet 2012, 379, 843–852. [Google Scholar] [CrossRef]
- Zhou, M.; Wang, H.; Zeng, X.; Yin, P.; Zhu, J.; Chen, W.; Li, X.; Wang, L.; Wang, L.; Liu, Y.; et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 394, 1145–1158. [Google Scholar] [CrossRef]
- Popkin, B.M. Synthesis and implications: China’s nutrition transition in the context of changes across other low- and middle-income countries. Obes. Rev. 2014, 15, 60–67. [Google Scholar] [CrossRef]
- Chinese Center for Disease Control and Prevention. CDC Public Health Science Data Center. Available online: http://www.phsciencedata.cn/Share/ky_sjml.jsp?id=940e083e-49d5-443a-bb94-b86d16ce2db0 (accessed on 1 October 2021). (In Chinese).
- Zang, J.; Ng, S.W. Age, period and cohort effects on adult physical activity levels from 1991 to 2011 in China. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 40. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.W.; Popkin, B.M. Time use and physical activity: A shift away from movement across the globe. Obes. Rev. 2012, 13, 659–680. [Google Scholar] [CrossRef]
- Monda, K.L.; Adair, L.S.; Zhai, F.; Popkin, B.M. Longitudinal relationships between occupational and domestic physical activity patterns and body weight in China. Eur. J. Clin. Nutr. 2007, 62, 1318–1325. [Google Scholar] [CrossRef]
- Bell, A.C.; Ge, K.; Popkin, B.M. Weight gain and its predictors in Chinese adults. Int. J. Obes. Relat. Metab. Disord. 2001, 25, 1079–1086. [Google Scholar] [CrossRef]
- Elfhag, K.; Rossner, S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes. Rev. 2005, 6, 67–85. [Google Scholar] [CrossRef]
- Barrington, W.E.; Beresford, S.A.A.; Koepsell, T.D.; Duncan, G.E.; Moudon, A.V. Worksite neighborhood and obesogenic behaviors: Findings among employees in the promoting activity and changes in eating (PACE) trial. Am. J. Prev. Med. 2015, 48, 31–41. [Google Scholar] [CrossRef]
- Engbers, L.; Sattelmair, J. Monitoring and Evaluation of Worksite Health Promotion Progams: Current State of Knowledge and Implications for Practice; World Health Organization (WHO): Geneva, Switzerland, 2008. [Google Scholar]
- Baicker, K.; Cutler, D.; Song, Z. Workplace wellness programs can generate savings. Health Aff. 2010, 29, 304–311. [Google Scholar] [CrossRef]
- Pratt, C.A.; Lemon, S.C.; Fernandez, I.D.; Goetzel, R.; Beresford, S.A.; French, S.A.; Stevens, V.J.; Vogt, T.M.; Webber, L.S. Design characteristics of worksite environmental interventions for obesity prevention*. Obesity 2007, 15, 2171–2180. [Google Scholar] [CrossRef] [PubMed]
- Geaney, F.; Kelly, C.; Greiner, B.; Harrington, J.; Perry, I.; Beirne, P. The effectiveness of workplace dietary modification interventions: A systematic review. Prev. Med. 2013, 57, 438–447. [Google Scholar] [CrossRef] [PubMed]
- Maes, L.; Van Cauwenberghe, E.; Van Lippevelde, W.; Spittaels, H.; De Pauw, E.; Oppert, J.-M.; Van Lenthe, F.J.; Brug, J.; De Bourdeaudhuij, I. Effectiveness of workplace interventions in Europe promoting healthy eating: A systematic review. Eur. J. Public Health 2012, 22, 677–683. [Google Scholar] [CrossRef] [PubMed]
- Mhurchu, C.N.; Aston, L.M.; Jebb, S.A. Effects of worksite health promotion interventions on employee diets: A systematic review. BMC Public Health 2010, 10, 62. [Google Scholar] [CrossRef] [PubMed]
- Plotnikoff, R.C.; Lubans, D.R.; Penfold, C.M.; Courneya, K.S. Testing the utility of three social-cognitive models for predicting objective and self-report physical activity in adults with type 2 diabetes. Br. J. Health Psychol. 2014, 19, 329–346. [Google Scholar] [CrossRef]
- Glanz, K.; Bishop, D.B. The role of behavioral science theory in development and implementation of public health interventions. Annu. Rev. Public Health 2010, 31, 399–418. [Google Scholar] [CrossRef]
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive; Prentice-Hall: Englewoods Cliffs, NJ, USA, 1986. [Google Scholar]
- Jang, Y.; Yoo, H. Self-management programs based on the social cognitive theory for Koreans with chronic disease: A systematic review. Contemp. Nurse 2012, 40, 147–159. [Google Scholar] [CrossRef]
- Hallam, J.S.; Petosa, R. The long-term impact of a four-session work-site intervention on selected social cognitive theory variables linked to adult exercise adherence. Health Educ. Behav. 2004, 31, 88–100. [Google Scholar] [CrossRef]
- Minkler, M.; Wallerstein, N. Community-Based Participatory Research for Health: From Process to Outcomes; John Wiley & Sons: New York, NY, USA, 2011. [Google Scholar]
- Van Olphen, J.; Freudenberg, N.; Galea, S.; Palermo, A.-G.S.; Ritas, C. Advocating Policies to Promote Community Reintegration of Drug Users Leaving Jail; Jossey-Bass: San Francisco, CA, USA, 2003. [Google Scholar]
- Cornwall, A.; Jewkes, R. What is participatory research? Soc. Sci. Med. 1995, 41, 1667–1676. [Google Scholar] [CrossRef]
- Beresford, S.A.A.; Locke, E.; Bishop, S.; West, B.; McGregor, B.A.; Bruemmer, B.; Duncan, G.E.; Thompson, B. Worksite study promoting activity and changes in eating (PACE): Design and baseline results. Obesity 2007, 15, 4S–15S. [Google Scholar] [CrossRef]
- Shrivastava, U.; Fatma, M.; Mohan, S.; Singh, P.; Misra, A. Randomized control trial for reduction of body weight, body fat patterning, and cardiometabolic risk factors in overweight worksite employees in Delhi, India. J. Diabetes Res. 2017, 2017, 7254174. [Google Scholar] [CrossRef] [PubMed]
- Thompson, B.; Hannon, P.A.; Bishop, S.K.; West, B.E.; Peterson, A.K.; Beresford, S.A.A. Factors related to participatory employee advisory boards in small, blue-collar worksites. Am. J. Heal. Promot. 2005, 19, 430–437. [Google Scholar] [CrossRef] [PubMed]
- Mogre, V.; Johnson, N.A.; Tzelepis, F.; Shaw, J.E.; Paul, C. A systematic review of adherence to diabetes self-care behaviours: Evidence from low- and middle-income countries. J. Adv. Nurs. 2019, 75, 3374–3389. [Google Scholar] [CrossRef] [PubMed]
- Barrington, W.E.; Ceballos, R.M.; Bishop, S.K.; McGregor, B.A.; Beresford, S.A. Perceived stress, behavior, and body mass index among adults participating in a worksite obesity prevention program, Seattle, 2005–2007. Prev. Chronic Dis. 2012, 9, E152. [Google Scholar] [CrossRef]
- Zalewska, M.; Maciorkowska, E. Dietary habits and physical activity of 18-year-old adolescents in relation to overweight and obesity. Iran J. Public Health 2019, 48, 864–872. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, M.L.; Otis, M.; Rosal, M.C.; Griecci, C.F.; Lemon, S.C. Reducing sugary drink intake through youth empowerment: Results from a pilot-site randomized study. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 58. [Google Scholar] [CrossRef]
- Liebman, M.; Pelican, S.; Moore, S.A.; Holmes, B.; Wardlaw, M.K.; Melcher, L.M.; Liddil, A.C.; Paul, L.C.; Dunnagan, T.; Haynes, G.W. Dietary intake, eating behavior, and physical activity-related determinants of high body mass index in rural communities in Wyoming, Montana, and Idaho. Int. J. Obes. Relat. Metab. Disord. 2003, 27, 684–692. [Google Scholar] [CrossRef]
- He, K.; Hu, F.B.; Colditz, G.; Manson, J.E.; Willett, W.C.; Liu, S. Changes in intake of fruits and vegetables in relation to risk of obesity and weight gain among middle-aged women. Int. J. Obes. Relat. Metab. Disord. 2004, 28, 1569–1574. [Google Scholar] [CrossRef]
- Jeffery, R.W.; French, S.A. Epidemic obesity in the United States: Are fast foods and television viewing contributing? Am. J. Public Health 1998, 88, 277–280. [Google Scholar] [CrossRef]
- French, S.A.; Harnack, L.; Jeffery, R.W. Fast food restaurant use among women in the Pound of Prevention study: Dietary, behavioral and demographic correlates. Int. J. Obes. Relat. Metab. Disord. 2000, 24, 1353–1359. [Google Scholar] [CrossRef]
- Pereira, M.A.; Kartashov, A.I.; Ebbeling, C.B.; Van Horn, L.; Slattery, M.L.; Jacobs, D.; Ludwig, D. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet 2005, 365, 36–42. [Google Scholar] [CrossRef]
- Wenwen, D. Trend of Eating Out and Its Impact on Nutritional Status of Chinese Adult Residents; Chinese Center for Disease Control and Prevention: Beijing, China, 2014. [Google Scholar]
- Keke, C. Study on the Nutrition of Residents Eating Out and the Relationship between Eating Out and Overweight and Obesity; Chinese Center for Disease Control and Prevention: Beijing, China, 2014. [Google Scholar]
- Berman, E.S. The relationship between eating self-efficacy and eating disorder symptoms in a non-clinical sample. Eat. Behav. 2006, 7, 79–90. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.S.; Volpp, K.G.; Rosin, R.; Bellamy, S.L.; Small, D.S.; Heuer, J.; Sproat, S.; Hyson, C.; Haff, N.; Lee, S.; et al. A randomized, controlled trial of lottery-based financial incentives to increase physical activity among overweight and obese adults. Am. J. Health Prom. 2018, 32, 1568–1575. [Google Scholar] [CrossRef] [PubMed]
- Godin, G.; Shephard, R.J. A simple method to assess exercise behavior in the community. Can. J. Appl. Sport Sci. 1985, 10, 141–146. [Google Scholar] [PubMed]
- Ainsworth, B.E.; Berry, C.B.; Schnyder, V.N.; Vickers, S.R. Leisure-time physical activity and aerobic fitness in African-American young adults. J. Adolesc. Health 1992, 13, 606–611. [Google Scholar] [CrossRef]
- Godin, G.A.; Colantonio, G.M.; Davis, G.M.; Shephard, R.J.; Simard, C. Prediction of leisure time exercise behavior among a group of lower-limb disabled adults. J. Clin. Psychol. 1986, 42, 272–279. [Google Scholar] [CrossRef]
- Godin, G.; Jobin, J.; Desharnais, R.; Cook, J. The impact of physical fitness and health-age appraisal upon exercise intentions and behavior. J. Behav. Med. 1987, 10, 241–250. [Google Scholar] [CrossRef]
- Godin, G. The godin-shephard leisure time physical activity questionnaire. Health Fitness J. Can. 2011, 1, 18–22. [Google Scholar] [CrossRef]
- Almeida, F.A.; You, W.; Harden, S.M.; Blackman, K.C.A.; Davy, B.M.; Glasgow, R.E.; Hill, J.L.; Linnan, L.A.; Wall, S.S.; Yenerall, J.; et al. Effectiveness of a worksite-based weight loss randomized controlled trial: The worksite study. Obesity 2015, 23, 737–745. [Google Scholar] [CrossRef]
- Thorndike, A.N.; Sonnenberg, L.; Healey, E.; Myint-U, K.; Kvedar, J.C.; Regan, S. Prevention of weight gain following a worksite nutrition and exercise program: A randomized controlled trial. Am. J. Prev. Med. 2012, 43, 27–33. [Google Scholar] [CrossRef]
- Lemon, S.C.; Zapka, J.; Li, W.; Estabrook, B.; Rosal, M.; Magner, R.; Andersen, V.; Borg, A.; Hale, J. Step ahead: A worksite obesity prevention trial among hospital employees. Am. J. Prev. Med. 2010, 38, 27–38. [Google Scholar] [CrossRef]
- Hill, J.O.; Wyatt, H.R.; Reed, G.W.; Peters, J.C. Obesity and the environment: Where do we go from here? Science 2003, 299, 853–855. [Google Scholar] [CrossRef] [PubMed]
- Wing, R.R. Behavioral treatment of obesity: Its application to type II diabetes. Diabetes Care 1993, 16, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Lemmens, V.E.P.P.; Oenema, A.; Klepp, K.I.; Henriksen, H.B.; Brug, J. A systematic review of the evidence regarding efficacy of obesity prevention interventions among adults. Obes. Rev. 2008, 9, 446–455. [Google Scholar] [CrossRef] [PubMed]
- Viester, L.; Verhagen, E.A.L.M.; Bongers, P.M.; van der Beek, A.J. Process evaluation of a multifaceted health program aiming to improve physical activity levels and dietary patterns among construction workers. J. Occup. Environ. Med. 2014, 56, 1210–1217. Available online: https://www.jstor.org/stable/48500772 (accessed on 1 October 2021). [CrossRef] [PubMed]
- Hutfless, S.; Maruthur, N.M.; Wilson, R.F.; Gudzune, K.A.; Brown, R.; Lau, B.; Fawole, O.A.; Chaudhry, Z.W.; Anderson, C.A.M.; Segal, J.B. Strategies to Prevent Weight Gain Among Adults; Createspace Independent Pub: Scotts Valley, CA, USA, 2013. [Google Scholar]
- Racette, S.B.; Deusinger, S.S.; Inman, C.L.; Burlis, T.L.; Highstein, G.R.; Buskirk, T.D.; Steger-May, K.; Peterson, L.R. Worksite Opportunities for Wellness (WOW): Effects on cardiovascular disease risk factors after 1 year. Prev. Med. 2009, 49, 108–114. [Google Scholar] [CrossRef]
- Murphy, M.H.; Nevill, A.; Murtagh, E.; Holder, R.L. The effect of walking on fitness, fatness and resting blood pressure: A meta-analysis of randomised, controlled trials. Prev. Med. 2007, 44, 377–385. [Google Scholar] [CrossRef]
- Sarabi, R.E.; Sadoughi, F.; Orak, R.J.; Bahaadinbeigy, K. The effectiveness of mobile phone text messaging in improving medication adherence for patients with chronic diseases: A systematic review. Iran. Red Crescent Med. J. 2016, 18, e25183. [Google Scholar] [CrossRef]
- Lyzwinski, L.N. A systematic review and meta-analysis of mobile devices and weight loss with an intervention content analysis. J. Pers. Med. 2014, 4, 311–385. [Google Scholar] [CrossRef]
- Carter, M.C.; Burley, V.; Nykjaer, C.; Cade, J. Adherence to a smartphone application for weight loss compared to website and paper diary: Pilot randomized controlled trial. J. Med. Internet Res. 2013, 15, e32. [Google Scholar] [CrossRef]
- Tamers, S.L.; Beresford, S.A.; Cheadle, A.D.; Zheng, Y.; Bishop, S.K.; Thompson, B. The association between worksite social support, diet, physical activity and body mass index. Prev. Med. 2011, 53, 53–56. [Google Scholar] [CrossRef] [PubMed]
- Lally, P.; Chipperfield, A.; Wardle, J. Healthy habits: Efficacy of simple advice on weight control based on a habit-formation model. Int. J. Obes. 2007, 32, 700–707. [Google Scholar] [CrossRef] [PubMed]
- A French, S.; Jeffery, R.W.; Story, M.; Breitlow, K.K.; Baxter, J.S.; Hannan, P.; Snyder, M.P. Pricing and promotion effects on low-fat vending snack purchases: The CHIPS Study. Am. J. Public Health 2001, 91, 112–117. [Google Scholar] [CrossRef] [PubMed]
- French, S.A.; Story, M.; Jeffery, R.W. Environmental Influences on eating and physical activity. Annu. Rev. Public Health 2001, 22, 309–335. [Google Scholar] [CrossRef]
- Hill, J.O.; Peters, J.C. Environmental contributions to the obesity epidemic. Science 1998, 280, 1371–1374. [Google Scholar] [CrossRef]
- Cheong, K.C.; Yusoff, A.F.; Ghazali, S.M.; Lim, K.H.; Selvarajah, S.; Haniff, J.; Khor, G.L.; Shahar, S.; Ab Rahman, J.; Zainuddin, A.A.; et al. Optimal BMI cut-off values for predicting diabetes, hypertension and hypercholesterolaemia in a multi-ethnic population. Public Health Nutr. 2013, 16, 453–459. [Google Scholar] [CrossRef]
- Xu, H.; Short, S.E.; Liu, T. Dynamic relations between fast-food restaurant and body weight status: A longitudinal and multilevel analysis of Chinese adults. J. Epidemiol. Commun. Heal. 2012, 67, 271–279. [Google Scholar] [CrossRef]
- Smith-McLallen, A.; Heller, D.; Vernisi, K.; Gulick, D.; Cruz, S.; Snyder, R.L. Comparative effectiveness of two walking interventions on participation, step counts, and health. Am. J. Heal. Promot. 2017, 31, 119–127. [Google Scholar] [CrossRef]
- Perdue, W.C.; Gostin, L.O.; Stone, L.A. Public health and the built environment: Historical, empirical, and theoretical foundations for an expanded role. J. Law Med. Ethics 2003, 31, 557–566. [Google Scholar] [CrossRef]
- Humpel, N.; Humpel, N.; Owen, N.; Leslie, E. Environmental factors associated with adults’ participation in physical activity A review. Am. J. Prev. Med. 2002, 22, 188–199. [Google Scholar] [CrossRef]
- Patel, M.S.; Benjamin, E.; Volpp, K.G.; Fox, C.S.; Small, D.S.; Massaro, J.M.; Lee, J.J.; Hilbert, V.; Valentino, M.; Taylor, D.H.; et al. Effect of a game-based intervention designed to enhance social incentives to increase physical activity among families: The BE FIT randomized clinical trial. JAMA Intern. Med. 2017, 177, 1586–1593. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, E.A.; Haaland, B.A.; Bilger, M.; Sahasranaman, A.; Sloan, R.; Nang, E.E.K.; Evenson, K.R. Effectiveness of activity trackers with and without incentives to increase physical activity (TRIPPA): A randomised controlled trial. Lancet Diabetes Endocrinol. 2016, 4, 983–995. [Google Scholar] [CrossRef]
- Patel, M.S.; Asch, D.; Rosin, R.; Small, D.S.; Bellamy, S.L.; Heuer, J.; Sproat, S.; Hyson, C.; Haff, N.; Lee, S.M.; et al. Framing financial incentives to increase physical activity among overweight and obese adults. Ann. Intern. Med. 2016, 164, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.S.; Benjamin, E.J.; Volpp, K.G.; Fox, C.S.; Small, D.S.; Massaro, J.M.; Lee, J.J.; Hilbert, V.; Valentino, M.; Taylor, D.H. Effect of a social incentive-based gamification intervention using wearable devices and smartphones on physical activity: The BE FIT randomized clinical trial. Circulation 2017, 135, 1. [Google Scholar] [CrossRef]
- Bauman, A.E.; Reis, R.S.; Sallis, J.F.; Wells, J.C.; Loos, R.J.F.; Martin, B.W.; Lancet Physical Activity Series Working Group. Correlates of physical activity: Why are some people physically active and others not? Lancet 2012, 380, 258–271. [Google Scholar] [CrossRef]
- Beresford, S.A.; Thompson, B.; Bishop, S. Long-term fruit and vegetable change in worksites: Seattle 5 a day follow-up. Am. J. Health Behav. 2010, 34, 707–720. [Google Scholar] [CrossRef][Green Version]
| Characteristics | Intervention (N = 216) | Control (N = 172) | p-Value | |
|---|---|---|---|---|
| Age (years) | 30.83 ± 5.57 | 34.61 ± 9.82 | <0.01 ** | |
| Gender | Male | 143 (66.2) | 100 (58.1) | 0.10 |
| Female | 73 (33.8) | 72 (41.9) | ||
| Marital status | Single or divorced | 79 (36.6) | 45 (26.2) | 0.05 |
| Married or cohabiting | 137 (63.4) | 127 (73.8) | ||
| Educational level | Under Junior college | 5 (2.3) | 37 (21.5) | <0.01 ** |
| Junior college | 46 (21.3) | 55 (32.0) | ||
| College or above | 165 (76.4) | 80 (46.5) | ||
| Household incomes per capita (Yuan, USD 1 = 6.7 Yuan) | <24,000 | 29 (13.6) | 21 (12.5) | 0.87 |
| ≥24,000, <56,000 | 49 (22.9) | 42 (25.0) | ||
| ≥56,000 | 136 (63.6) | 105 (62.5) | ||
| Intervention | Control | Adjusted Change between Groups, Mean (95%CI) ☆ | Adjusted p-Value Δ | |||||
|---|---|---|---|---|---|---|---|---|
| Baseline (N = 216) | Follow-Up (N = 159) | p-Value † | Baseline (N = 172) | Follow-Up (N = 119) | p-Value † | |||
| BMI (kg/m2) | 23.21 ± 3.71 | 22.95 ± 3.55 | 0.01 * | 23.39 ± 3.15 | 23.33 ± 3.37 | 0.69 | −0.11 (−0.82, 0.60) | 0.76 |
| WC (cm) | 81.48 ± 11.28 | 80.82 ± 10.18 | 0.11 | 80.81 ± 9.59 | 80.60 ± 9.72 | 0.72 | −0.89 (−2.63, 0.85) | 0.31 |
| HC (cm) | 95.97 ± 6.44 | 95.28 ± 6.64 | 0.03 * | 95.75 ± 6.16 | 95.53 ± 6.09 | 0.65 | −0.11 (−1.34, 1.13) | 0.87 |
| WHR | 0.85 ± 0.08 | 0.85 ± 0.07 | 0.98 | 0.84 ± 0.07 | 0.84 ± 0.06 | 0.88 | −0.01 (−0.02, 0.002) | 0.12 |
| WHtR | 0.49 ± 0.06 | 0.48 ± 0.05 | 0.01 * | 0.49 ± 0.05 | 0.49 ± 0.05 | 0.47 | −0.01 (−0.02, 0.01) | 0.34 |
| Intervention | Control | Adjusted Change between Groups, Mean (95%CI) ☆ | Adjusted p-Value Δ | |||||
|---|---|---|---|---|---|---|---|---|
| Baseline (N = 216) | Follow-Up (N = 159) | p-Value † | Baseline (N = 172) | Follow-Up (N = 119) | p-Value † | |||
| Frequency of fried food per month | 3.46 ± 4.34 | 2.73 ± 3.32 | 0.19 | 3.49 ± 5.58 | 3.24 ± 4.84 | 0.66 | −0.11 (−1.04, 0.83) | 0.82 |
| Servings of fried food per month | 4.91 ± 7.79 | 3.53 ± 5.39 | 0.15 | 3.90 ± 6.60 | 3.79 ± 7.07 | 0.89 | 0.81 (−1.17, 2.79) | 0.42 |
| Frequency of sweetened beverage per month | 4.10 ± 5.37 | 3.13 ± 4.47 | 0.17 | 5.70 ± 11.41 | 4.20 ± 5.75 | 0.13 | −1.81 (−0.52, −3.11) | <0.01 ** |
| Servings of sweetened beverage per month | 4.83 ± 6.69 | 4.04 ± 8.01 | 0.45 | 9.57 ± 35.80 | 4.63 ± 7.15 | 0.08 | −2.44 (−5.68, 0.81) | 0.14 |
| Frequency of sweetened food per month | 4.22 ± 6.02 | 3.29 ± 4.66 | 0.18 | 4.36 ± 7.06 | 3.27 ± 4.42 | 0.09 | 0.14 (−0.89, 1.18) | 0.79 |
| Servings of sweetened food per month | 5.37 ± 10.59 | 3.55 ± 4.81 | 0.11 | 5.78 ± 15.77 | 3.53 ± 4.46 | 0.08 | −0.25 (−2.00, 1.50) | 0.78 |
| Frequency of fruit per month | 18.10 ± 16.12 | 18.47 ± 15.60 | 0.86 | 16.02 ± 14.41 | 15.63 ± 13.41 | 0.79 | 3.68 (1.25, 6.12) | <0.01 ** |
| Servings of fruit per day | 1.05 ± 1.22 | 0.93 ± 0.97 | 0.35 | 0.81 ± 1.03 | 0.77 ± 0.77 | 0.64 | 0.26 (0.44, 0.92) | <0.01 ** |
| Frequency of vegetables per month | 39.03 ± 22.97 | 44.49 ± 26.36 | 0.14 | 34.66 ± 24.92 | 41.25 ± 22.82 | <0.01 ** | 5.66 (1.59, 9.74) | <0.01** |
| Servings of vegetables per day | 1.94 ± 2.01 | 2.15 ± 1.78 | 0.46 | 1.53 ± 1.48 | 1.81 ± 1.51 | 0.06 | 0.53 (0.24, 0.82) | <0.01 ** |
| Servings of vegetables/fruit per day | 2.99 ± 2.72 | 3.10 ± 2.06 | 0.76 | 2.37 ± 1.98 | 2.61 ± 1.81 | 0.20 | 0.79 (0.43, 1.16) | <0.01 ** |
| Frequency of eating out per month | 3.80 ± 4.58 | 3.92 ± 4.19 | 0.85 | 3.50 ± 3.57 | 3.74 ± 4.21 | 0.57 | 0.53 (−0.21, 1.27) | 0.16 |
| Fast-food meals per month | 1.12 ± 1.27 | 2.08 ± 2.89 | <0.01 ** | 1.30 ± 1.69 | 2.09 ± 2.83 | <0.01 ** | 0.05 (−0.43, 0.33) | 0.79 |
| Intervention | Control | Adjusted Change between Groups, Mean/OR (95%CI) ☆ | Adjusted p-Value Δ | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline (N = 216) | Follow-Up (N = 159) | p-Value † | Baseline (N = 172) | Follow-Up (N = 119) | p-Value † | ||||
| Godin index | 22.67 ± 20.04 | 25.77 ± 27.98 | 0.18 | 24.86 ± 29.85 | 23.15 ± 19.48 | 0.88 | 1.04 (−3.59, 5.67) | 0.66 | |
| Walking days per week | 5.16 ± 2.12 | 4.84 ± 2.11 | 0.09 | 5.19 ± 2.30 | 5.21 ± 2.19 | 0.94 | −0.34 (−0.75, 0.07) | 0.10 | |
| Daily steps | 6554.41 ± 3113.82 | 6919.76 ± 4412.09 | 0.36 | 6986.14 ± 2526.67 | 4994.83 ± 2226.66 | <0.01 ** | 863.19 (161.42, 1564.97) | 0.02 * | |
| Exercise to sweating | Yes | 117 (56.0) | 98(63.6) | 0.02 * | 89 (54.3) | 85(71.4) | 0.03 * | 0.68 (0.02, 20.57) | 0.75 |
| No | 92 (44.0) | 56(36.4) | 75 (45.7) | 34(28.6) | |||||
| Exercise self-efficacy | High | 85 (40.5) | 53(34.9) | 0.09 | 71 (42) | 51(55.3) | 0.58 | 1.91 (1.02,3.60) | 0.04 * |
| Low | 125 (59.5) | 99(65.1) | 298(58) | 63(44.7) | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kong, J.; Chen, Y.; Zheng, Y.; Zhu, L.; Chen, B.; Cheng, X.; Song, M.; Patrick, D.L.; Beresford, S.A.A.; Wang, H. Effectiveness of a Worksite-Based Lifestyle Intervention on Employees’ Obesity Control and Prevention in China: A Group Randomized Experimental Study. Int. J. Environ. Res. Public Health 2022, 19, 6738. https://doi.org/10.3390/ijerph19116738
Kong J, Chen Y, Zheng Y, Zhu L, Chen B, Cheng X, Song M, Patrick DL, Beresford SAA, Wang H. Effectiveness of a Worksite-Based Lifestyle Intervention on Employees’ Obesity Control and Prevention in China: A Group Randomized Experimental Study. International Journal of Environmental Research and Public Health. 2022; 19(11):6738. https://doi.org/10.3390/ijerph19116738
Chicago/Turabian StyleKong, Jingxia, Ying Chen, Yingjing Zheng, Lin Zhu, Boyan Chen, Xiao Cheng, Mengna Song, Donald L. Patrick, Shirley A. A. Beresford, and Hongmei Wang. 2022. "Effectiveness of a Worksite-Based Lifestyle Intervention on Employees’ Obesity Control and Prevention in China: A Group Randomized Experimental Study" International Journal of Environmental Research and Public Health 19, no. 11: 6738. https://doi.org/10.3390/ijerph19116738
APA StyleKong, J., Chen, Y., Zheng, Y., Zhu, L., Chen, B., Cheng, X., Song, M., Patrick, D. L., Beresford, S. A. A., & Wang, H. (2022). Effectiveness of a Worksite-Based Lifestyle Intervention on Employees’ Obesity Control and Prevention in China: A Group Randomized Experimental Study. International Journal of Environmental Research and Public Health, 19(11), 6738. https://doi.org/10.3390/ijerph19116738






