Psychometric Properties of the Albanian Version of the Nursing Self-Efficacy Scale
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Instrument
2.3. Setting and Sample
2.4. Ethical Statement
2.5. Translation Process and Content Validity
2.6. Data Analysis
3. Results
3.1. Face and Content Validity
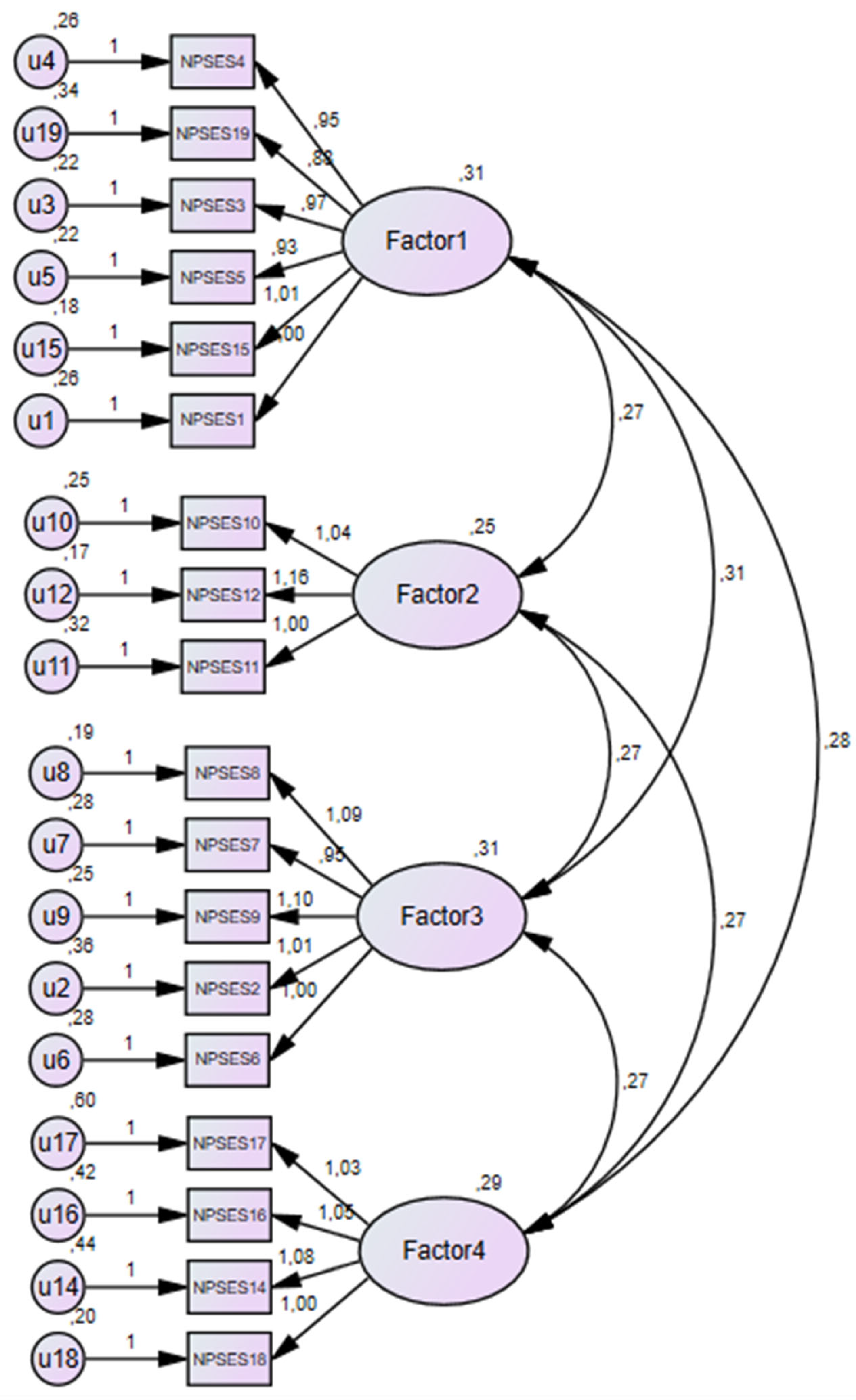
3.2. Construct Validity
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kingma, M. Nurses on the Move: Migration and the Global Health Care Economy; Cornell University Press: New York, NJ, USA, 2018. [Google Scholar]
- Farokhzadian, J.; Dehghan Nayeri, N.; Borhani, F. The long way ahead to achieve an effective patient safety culture: Challenges perceived by nurses. BMC Health Serv. Res. 2018, 18, 654. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. The explanatory and predictive scope of self-efficacy theory. J. Soc. Clin. Psychol. 1986, 4, 359–373. [Google Scholar] [CrossRef]
- Bandura, A. Toward a psychology of human agency. Perspect. Psychol. Sci. 2006, 1, 164–180. [Google Scholar] [CrossRef] [PubMed]
- Gori, A.; Topino, E.; Brugnera, A.; Compare, A. Assessment of professional self-efficacy in psychological interventions and psychotherapy sessions: Development of the Therapist Self-Efficacy Scale (T-SES) and its application for eTherapy. J. Clin. Psychol. 2022, 78, 2122–2144. [Google Scholar] [CrossRef] [PubMed]
- Usher, E.L.; Li, C.R.; Butz, A.R.; Rojas, J.P. Perseverant grit and self-efficacy: Are both essential for children’s academic success? J. Educ. Psychol. 2019, 111, 877. [Google Scholar] [CrossRef]
- Bhatti, M.A.; Hussain, M.S.; Al Doghan, M.A. The role of personal and job resources in boosting nurses’ work engagement and performance. Glob. Bus. Organ. Excell. 2018, 37, 32–40. [Google Scholar] [CrossRef]
- Sharour, L.A.; Salameh, A.B.; Suleiman, K.; Subih, M.; Mahmoud, A.H.; Al Dameery, K.; Al Omari, O. Nurses’ self-efficacy, confidence and interaction with patients with COVID-19: A cross-sectional study. Disaster Med. Public Health Prep. 2022, 16, 1393–1397. [Google Scholar] [CrossRef]
- Li, J.; Li, X.; Gu, L.; Zhang, R.; Zhao, R.; Cai, Q.; Lu, Y.; Wang, H.; Meng, Q.; Wei, H. Effects of simulation-based deliberate practice on nursing students’ communication, empathy, and self-efficacy. J. Nurs. Educ. 2019, 58, 681–689. [Google Scholar] [CrossRef]
- Dehghani, F.; Barkhordari-Sharifabad, M.; Sedaghati-Kasbakhi, M.; Fallahzadeh, H. Effect of palliative care training on perceived self-efficacy of the nurses. BMC Palliat. Care 2020, 19, 63. [Google Scholar] [CrossRef]
- Dellafiore, F.; Rosa, D.; Udugampolage, N.S.; Villa, G.; Albanesi, B. Professional values and nursing self-efficacy in the Italian context: Correlational descriptive study. Scand. J. Caring Sci. 2022, 36, 142–149. [Google Scholar] [CrossRef]
- Lugo, R.G.; Hjelmeland, I.; Hansen, M.T.; Haug, E.; Sütterlin, S.; Grønlien, H.K. Impact of initial emotional states and self-efficacy changes on nursing students’ practical skills performance in simulation-based education. Nurs. Rep. 2021, 11, 267–278. [Google Scholar] [CrossRef] [PubMed]
- Hines, S.; Ramsbotham, J.; Coyer, F. A theory-based research literacy intervention for nurses: A pilot study. Nurs. Forum 2022, 1–7. [Google Scholar] [CrossRef]
- Yoo, S.Y.; Cho, H. Exploring the influences of nurses’ partnership with parents, attitude to families’ importance in nursing care, and professional self-efficacy on quality of pediatric nursing care: A path model. Int. J. Environ. Res. Public Health 2020, 17, 5452. [Google Scholar] [CrossRef]
- Carvalho, M.; Gaspar, F.; Potra, T.; Lucas, P. Translation, adaptation, and validation of the self-efficacy scale for clinical nurse leaders for the Portuguese culture. Int. J. Environ. Res. Public Health 2022, 19, 8590. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.Y.; Hwang, G.J.; Gau, M.L. Promoting students’ learning achievement and self-efficacy: A mobile chatbot approach for nursing training. Br. J. Educ. Technol. 2022, 53, 171–188. [Google Scholar]
- Boswell, C.; Ashcraft, A.; Long, J.; Cannon, S.; DiVito-Thomas, P.; Delaney, T. Self-efficacy: Changing the tide of evidence-based practice. Worldviews Evid. Based Nurs. 2020, 17, 129–135. [Google Scholar] [CrossRef]
- Zwart, D.P.; Noroozi, O.; Van Luit, J.E.; Goei, S.L.; Nieuwenhuis, A. Effects of digital learning materials on nursing students’ mathematics learning, self-efficacy, and task value in vocational education. Nurse Educ. Pract. 2020, 44, 102755. [Google Scholar] [CrossRef]
- Shorey, S.; Lopez, V. Self-efficacy in a nursing context. In Health Promotion in Health Care—Vital Theories and Research; Springer: Cham, Switzerland, 2021; pp. 145–158. [Google Scholar]
- Brenner, R.; Witzig-Brändli, V.; Vetsch, J.; Kohler, M. Nursing interventions focusing on self-efficacy for patients with multiple sclerosis in rehabilitation: A systematic review. Int. J. MS Care 2022, 24, 189–198. [Google Scholar] [CrossRef]
- Brando-Garrido, C.; Montes-Hidalgo, J.; Limonero, J.T.; Gómez-Romero, M.J.; Tomás-Sábado, J. Relationship of academic procrastination with perceived competence, coping, self-esteem and self-efficacy in nursing students. Enferm. Clín. Engl. Ed. 2020, 30, 398–403. [Google Scholar] [CrossRef]
- Tohmola, A.; Saarnio, R.; Mikkonen, K.; Kyngäs, H.; Elo, S. Competencies relevant for gerontological nursing: Focus-group interviews with professionals in the nursing of older people. Nord. J. Nurs. Res. 2022, 42, 123–132. [Google Scholar] [CrossRef]
- Puschmann, A.K.; Drießlein, D.; Beck, H.; Arampatzis, A.; Catalá, M.M.; Schiltenwolf, M.; Mayer, F.; Wippert, P.M. Stress and self-efficacy as long-term predictors for chronic low back pain: A prospective longitudinal study. J. Pain Res. 2020, 13, 613. [Google Scholar] [CrossRef] [PubMed]
- Caruso, R.; Pittella, F.; Zaghini, F.; Fida, R.; Sili, A. Development and validation of the Nursing Profession Self-Efficacy Scale. Int. Nurs. Rev. 2016, 63, 455–464. [Google Scholar] [CrossRef] [PubMed]
- Kyriazos, T.A. Applied psychometrics: Sample size and sample power considerations in factor analysis (EFA, CFA) and SEM in general. Psychology 2018, 9, 2207. [Google Scholar] [CrossRef]
- Serdar, C.C.; Cihan, M.; Yücel, D.; Serdar, M.A. Sample size, power and effect size revisited: Simplified and practical approaches in pre-clinical, clinical and laboratory studies. Biochem. Med. 2021, 31, 27–53. [Google Scholar] [CrossRef]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the Process of Cross-Cultural Adaptation of Self-Report Measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef] [PubMed]
- Polit, D.F.; Beck, C.T. The content validity index: Are you sure you know what’s being reported? Critique and recommendations. Res. Nurs. Health 2006, 29, 489–497. [Google Scholar] [CrossRef]
- Lawshe, C.H. A quantitative approach to content validity. Pers. Psychol. 1975, 28, 563–575. [Google Scholar] [CrossRef]
- Polit, D.F.; Beck, C.T. Essentials of Nursing Research: Appraising Evidence for Nursing Practice, 8th ed.; Wolters Kluwer Health/Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2014. [Google Scholar]
- Brett, W.; Onsman, A.; Brown, T. Exploratory factor analysis: A five-step guide for novices. Australas. J. Paramed. 2010, 8, 225–236. [Google Scholar]
- Garnier-Villarreal, M.; Jorgensen, T.D. Adapting fit indices for Bayesian structural equation modeling: Comparison to maximum likelihood. Psychol. Methods 2020, 25, 46. [Google Scholar] [CrossRef]
- Ximénez, C.; Maydeu-Olivares, A.; Shi, D.; Revuelta, J. Assessing cut-off values of SEM fit indices: Advantages of the unbiased SRMR index and its cut-off criterion based on communality. Struct. Equ. Model. 2022, 29, 368–380. [Google Scholar] [CrossRef]
- Yaşlioğlu, M.; Yaşlioğlu, D.T. How and when to use which fit indices? A practical and critical review of the methodology. Istanb. Manag. J. 2020, 88, 1–20. [Google Scholar] [CrossRef]
- Kang, H. Discussions on the suitable interpretation of model fit indices and the strategies to fit model in structural equation modeling. J. Korean Data Anal. Soc. 2013, 15, 653–668. [Google Scholar]
- Wang, J.; Wang, X. Structural Equation Modeling: Applications Using Mplus; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Parady, G.; Ory, D.; Walker, J. The overreliance on statistical goodness-of-fit and under-reliance on model validation in discrete choice models: A review of validation practices in the transportation academic literature. J. Choice Model. 2021, 38, 100257. [Google Scholar] [CrossRef]
- Watkins, M.W. Exploratory factor analysis: A guide to best practice. J. Black Psychol. 2018, 44, 219–246. [Google Scholar] [CrossRef]
- Bandalos, D.L.; Finney, S.J. Factor analysis: Exploratory and confirmatory. In The Reviewer’s Guide to Quantitative Methods in the Social Sciences; Routledge: London, UK, 2018; pp. 98–122. [Google Scholar]
- Ximénez, C.; Revuelta, J.; Castañeda, R. What are the consequences of ignoring cross-loadings in bifactor models? A simulation study assessing parameter recovery and sensitivity of goodness-of-fit indices. Front. Psychol. 2022, 13, 923877. [Google Scholar] [CrossRef]
- Browne, C.; Wall, P.; Batt, S.; Bennett, R. Understanding perceptions of nursing professional identity in students entering an Australian undergraduate nursing degree. Nurs. Educ. Pract. 2018, 32, 90–96. [Google Scholar] [CrossRef]
- Santhanam, S.P.; Parveen, S.; Santhanam, S.P.; Parveen, S. Serving culturally and linguistically diverse clients: A review of changing trends in speech-language pathologists’ self-efficacy and implications for stakeholders. Clin. Arch. Commun. Disord. 2018, 3, 165–177. [Google Scholar]
- Adamovic, M.; Gahan, P.; Olsen, J.; Gulyas, A.; Shallcross, D.; Mendoza, A. Exploring the adoption of virtual work: The role of virtual work self-efficacy and virtual work climate. Int. J. Hum. Resour. Manag. 2022, 33, 3492–3525. [Google Scholar] [CrossRef]
- Labrague, L.J.; Al Sabei, S.; Al Rawajfah, O.; AbuAlRub, R.; Burney, I. Authentic leadership and nurses’ motivation to engage in leadership roles: The mediating effects of nurse work environment and leadership self-efficacy. J. Nurs. Manag. 2021, 29, 2444–2452. [Google Scholar] [CrossRef]
- Oh, J.; Cho, H.; Kim, Y.Y.; Yoo, S.Y. Validation of the Korean version of the nursing profession self-efficacy scale: A methodological study. Int. J. Environ. Res. Public Health 2021, 18, 1080. [Google Scholar] [CrossRef]
- Koota, E.; Kääriäinen, M.; Lääperi, M.; Melender, H.L. Emergency nurses’ Evidence-Based Practice attitudes, self-efficacy, knowledge, skills and behaviors before an educational intervention–Baseline of a Randomized Controlled Trial. Collegian 2020, 27, 361–369. [Google Scholar] [CrossRef]
| N | % | |
|---|---|---|
| Gender | ||
| F | 361 | 85.3 |
| M | 62 | 14.7 |
| Age Classes | ||
| 20–30 | 161 | 38.1 |
| 31–41 | 133 | 31.4 |
| 41–52 | 82 | 19.4 |
| 53–63 | 47 | 11.1 |
| Work Place | ||
| Private | 13 | 3.1 |
| Public | 410 | 96.9 |
| Work Unit | ||
| Critical Area | 49 | 11.6 |
| Medical Area | 276 | 65.2 |
| Pediatric Area | 27 | 6.4 |
| Undeclared | 71 | 16.8 |
| Years Profession | ||
| 0–11 | 266 | 62.9 |
| 12–23 | 102 | 24.1 |
| 24–35 | 48 | 11.3 |
| 36–47 | 7 | 1.7 |
| Years Ward Unit | ||
| 0–9 | 288 | 68.1 |
| 10–19 | 80 | 18.9 |
| 20–29 | 40 | 9.5 |
| 30–39 | 15 | 3.5 |
| Job Satisfaction | ||
| Nothing | 8 | 1.9 |
| Little | 21 | 5.0 |
| Fair | 180 | 42.6 |
| More | 214 | 50.6 |
| I-CVIs | Interpretation | S-CVI | |
|---|---|---|---|
| NPSES 1 | 0.82 | Pertinent | 0.87 |
| NPSES 2 | 0.82 | Pertinent | |
| NPSES 3 | 0.80 | Pertinent | |
| NPSES 4 | 0.96 | Pertinent | |
| NPSES 5 | 0.85 | Pertinent | |
| NPSES 6 | 0.80 | Pertinent | |
| NPSES 7 | 0.94 | Pertinent | |
| NPSES 8 | 0.86 | Pertinent | |
| NPSES 9 | 0.90 | Pertinent | |
| NPSES 10 | 0.80 | Pertinent | |
| NPSES 11 | 0.83 | Pertinent | |
| NPSES 12 | 1 | Pertinent | |
| NPSES 13 | 0.80 | Pertinent | |
| NPSES 14 | 1 | Pertinent | |
| NPSES 15 | 0.94 | Pertinent | |
| NPSES 16 | 0.84 | Pertinent | |
| NPSES 17 | 0.88 | Pertinent | |
| NPSES 18 | 0.85 | Pertinent | |
| NPSES 19 | 0.85 | Pertinent |
| New Item Scale A-NPSES | Old Item Scale NPSES | F1 | F2 | F3 | F4 | Communalities | |
|---|---|---|---|---|---|---|---|
| Factor 1 Nursing Care Procedure Situation | NPSES1 | NPSES4 | 0.713 | 0.164 | 0.371 | 0.130 | 0.628 |
| NPSES2 | NPSES19 | 0.649 | 0.009 | −0.075 | 0.384 | 0.629 | |
| NPSES3 | NPSES3 | 0.642 | 0.374 | 0.321 | 0.068 | 0.660 | |
| NPSES4 | NPSES5 | 0.629 | 0.223 | 0.450 | 0.033 | 0.689 | |
| NPSES5 | NPSES15 | 0.607 | 0.605 | 0.030 | 0.114 | 0.649 | |
| NPSES6 | NPSES1 | 0.606 | 0.078 | 0.456 | 0.216 | 0.510 | |
| Factor 2 Nursing Research Situation | NPSES7 | NPSES10 | 0.108 | 0.786 | 0.162 | 0.150 | 0.503 |
| NPSES8 | NPSES12 | 0.307 | 0.755 | 0.235 | 0.000 | 0.679 | |
| NPSES9 | NPSES11 | 0.090 | 0.696 | 0.282 | 0.397 | 0.558 | |
| Factor 3 Nursing Ethics Situation | NPSES10 | NPSES8 | 0.115 | 0.273 | 0.760 | 0.120 | 0.679 |
| NPSES11 | NPSES7 | 0.240 | 0.153 | 0.607 | 0.229 | 0.730 | |
| NPSES12 | NPSES9 | 0.134 | 0.464 | 0.570 | −0.023 | 0.720 | |
| NPSES13 | NPSES2 | 0.321 | −0.009 | 0.566 | 0.453 | 0.572 | |
| NPSES14 | NPSES6 | 0.271 | 0.238 | 0.481 | 0.385 | 0.748 | |
| Factor 4 Nursing Practice Situation | NPSES15 | NPSES17 | 0.105 | −0.014 | 0.118 | 0.774 | 0.704 |
| NPSES16 | NPSES16 | 0.281 | 0.292 | 0.161 | 0.716 | 0.623 | |
| NPSES17 | NPSES14 | 0.010 | 0.476 | 0.188 | 0.556 | 0.479 | |
| NPSES18 | NPSES18 | 0.453 | 0.174 | 0.180 | 0.459 | 0.575 |
| Mean | SD | Corrected Item-Total Correlation | Cronbach’s Alpha If Item Deleted | Cronbach’s Alpha Factor | Total Cronbach’s Alpha | ||
|---|---|---|---|---|---|---|---|
| Factor 1 Nursing Care Procedure Situation | NPSES1 | 4.4929 | 0.64269 | 0.652 | 0.905 | 0.763 | 0.911 |
| NPSES2 | 4.4408 | 0.74963 | 0.431 | 0.911 | |||
| NPSES3 | 4.5261 | 0.61955 | 0.670 | 0.905 | |||
| NPSES4 | 4.5877 | 0.59812 | 0.631 | 0.906 | |||
| NPSES5 | 4.6066 | 0.59502 | 0.639 | 0.905 | |||
| NPSES6 | 4.5403 | 0.67756 | 0.636 | 0.905 | |||
| Factor 2 Nursing Research Situation | NPSES7 | 4.4028 | 0.73276 | 0.540 | 0.908 | 0.810 | |
| NPSES8 | 4.5024 | 0.69264 | 0.598 | 0.906 | |||
| NPSES9 | 4.2796 | 0.77614 | 0.673 | 0.904 | |||
| Factor 3 Nursing Ethics Situation | NPSES10 | 4.5308 | 0.64936 | 0.584 | 0.906 | 0.772 | |
| NPSES11 | 4.3318 | 0.71307 | 0.555 | 0.907 | |||
| NPSES12 | 4.4929 | 0.69261 | 0.525 | 0.908 | |||
| NPSES13 | 4.4123 | 0.75318 | 0.607 | 0.906 | |||
| NPSES14 | 4.3033 | 0.72568 | 0.621 | 0.905 | |||
| Factor 4 Nursing Practice Situation | NPSES15 | 4.1469 | 0.93209 | 0.403 | 0.913 | 0.788 | |
| NPSES16 | 4.3412 | 0.83218 | 0.657 | 0.904 | |||
| NPSES17 | 4.2322 | 0.92998 | 0.531 | 0.909 | |||
| NPSES18 | 4.5355 | 0.62672 | 0.577 | 0.907 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duka, B.; Stievano, A.; Caruso, R.; Prendi, E.; Spada, F.; Rocco, G.; Notarnicola, I. Psychometric Properties of the Albanian Version of the Nursing Self-Efficacy Scale. Healthcare 2022, 10, 2232. https://doi.org/10.3390/healthcare10112232
Duka B, Stievano A, Caruso R, Prendi E, Spada F, Rocco G, Notarnicola I. Psychometric Properties of the Albanian Version of the Nursing Self-Efficacy Scale. Healthcare. 2022; 10(11):2232. https://doi.org/10.3390/healthcare10112232
Chicago/Turabian StyleDuka, Blerina, Alessandro Stievano, Rosario Caruso, Emanuela Prendi, Florian Spada, Gennaro Rocco, and Ippolito Notarnicola. 2022. "Psychometric Properties of the Albanian Version of the Nursing Self-Efficacy Scale" Healthcare 10, no. 11: 2232. https://doi.org/10.3390/healthcare10112232
APA StyleDuka, B., Stievano, A., Caruso, R., Prendi, E., Spada, F., Rocco, G., & Notarnicola, I. (2022). Psychometric Properties of the Albanian Version of the Nursing Self-Efficacy Scale. Healthcare, 10(11), 2232. https://doi.org/10.3390/healthcare10112232









