Etiology, Pathogenesis, Diagnosis, and Practical Implications of Hepatocellular Neoplasms
Abstract
:Simple Summary
Abstract
1. Introduction
2. Etiology and Pathogenesis of Hepatocellular Adenomas
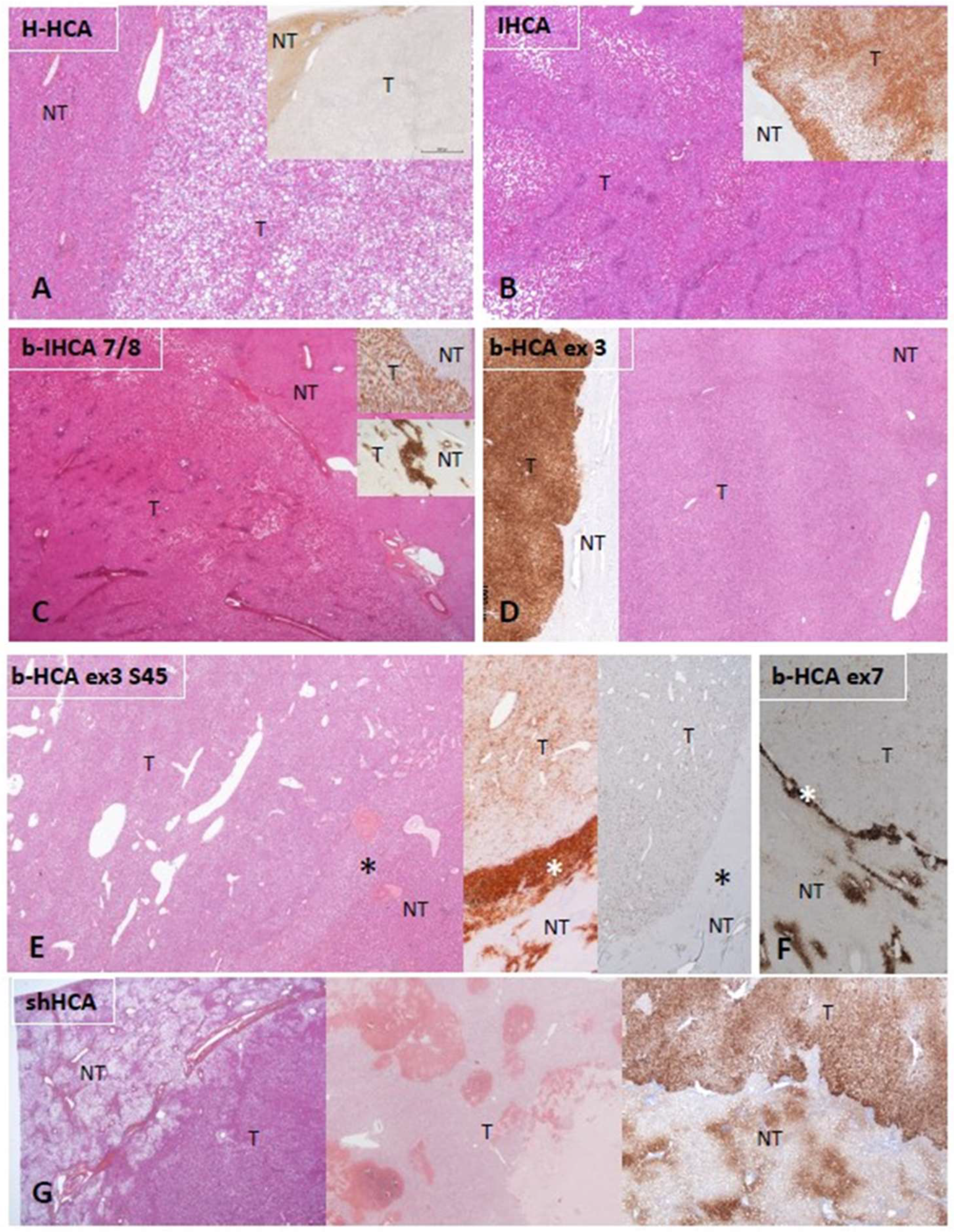
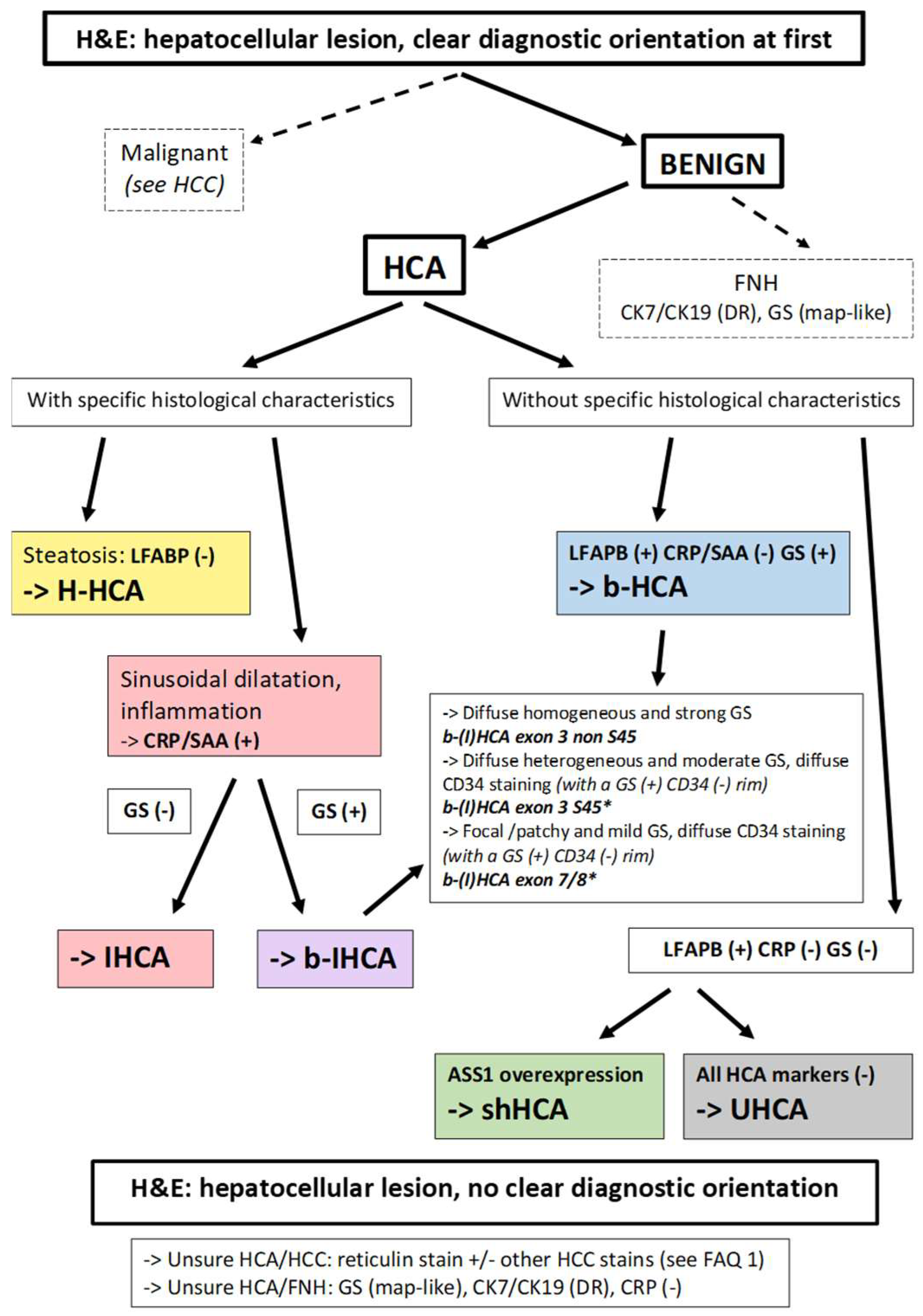
3. Diagnosis and Subtyping of Hepatocellular Adenomas
4. Etiology and Pathogenesis of Hepatocellular Carcinoma
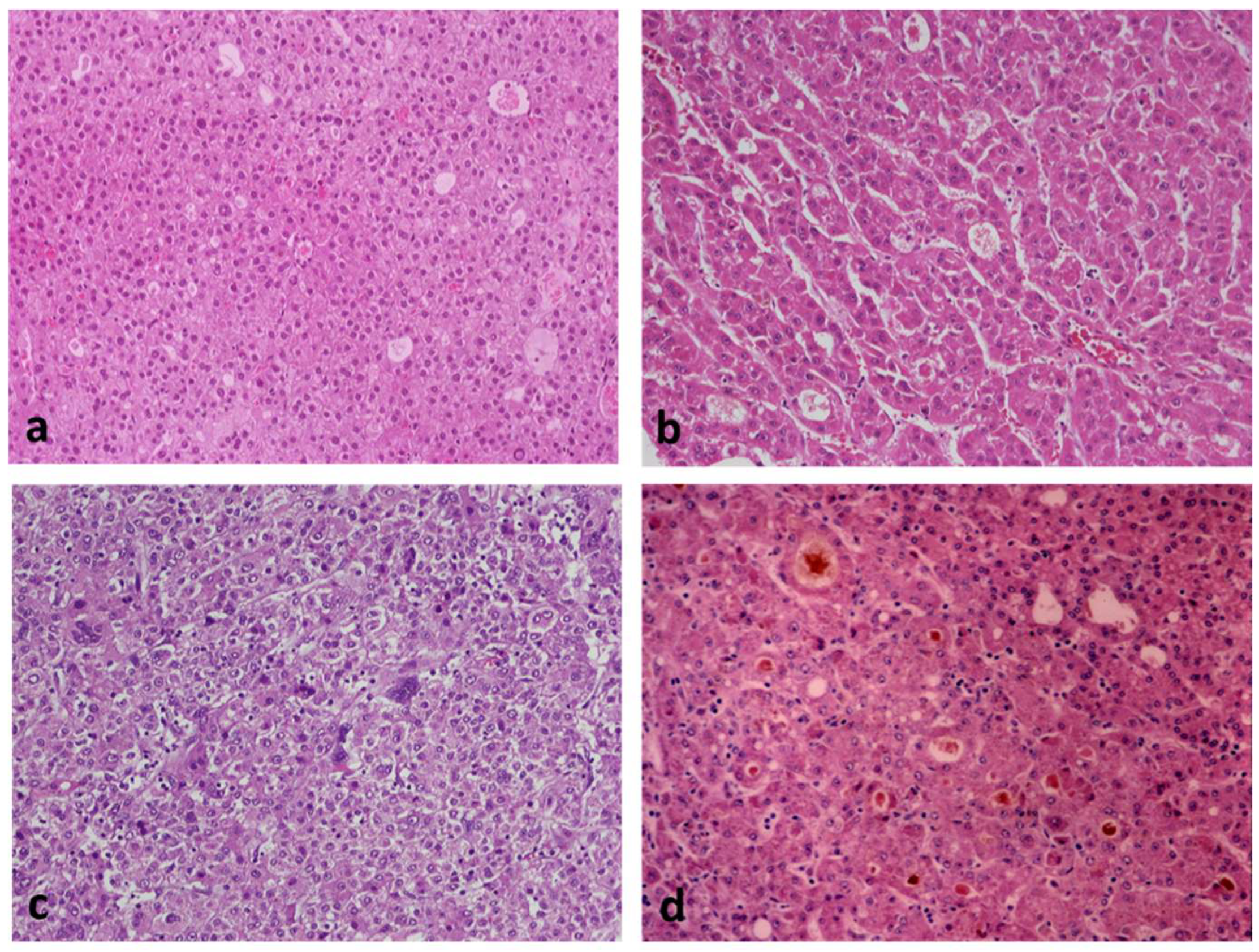
5. Diagnosis of Hepatocellular Carcinoma
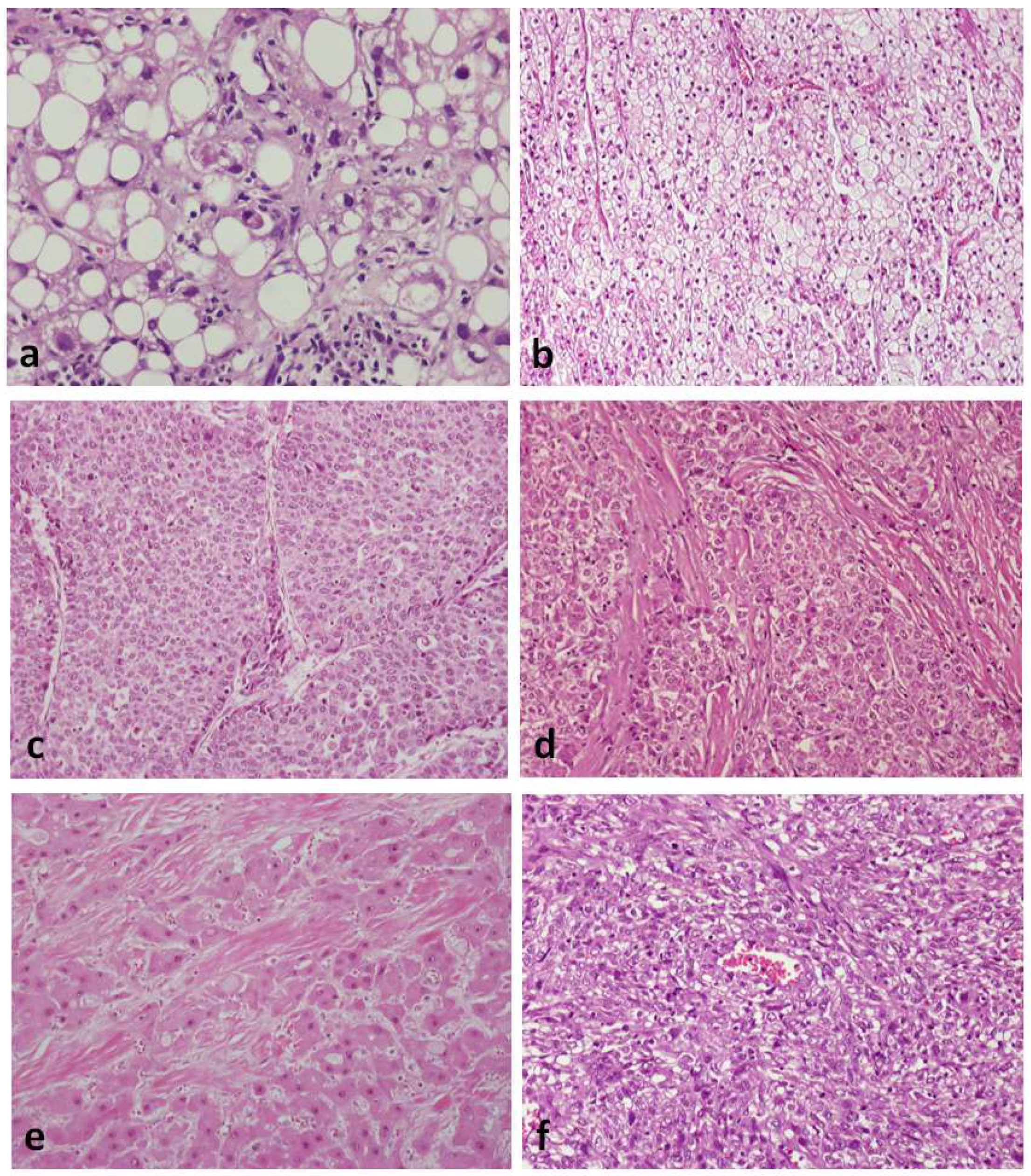
HCC Subtypes
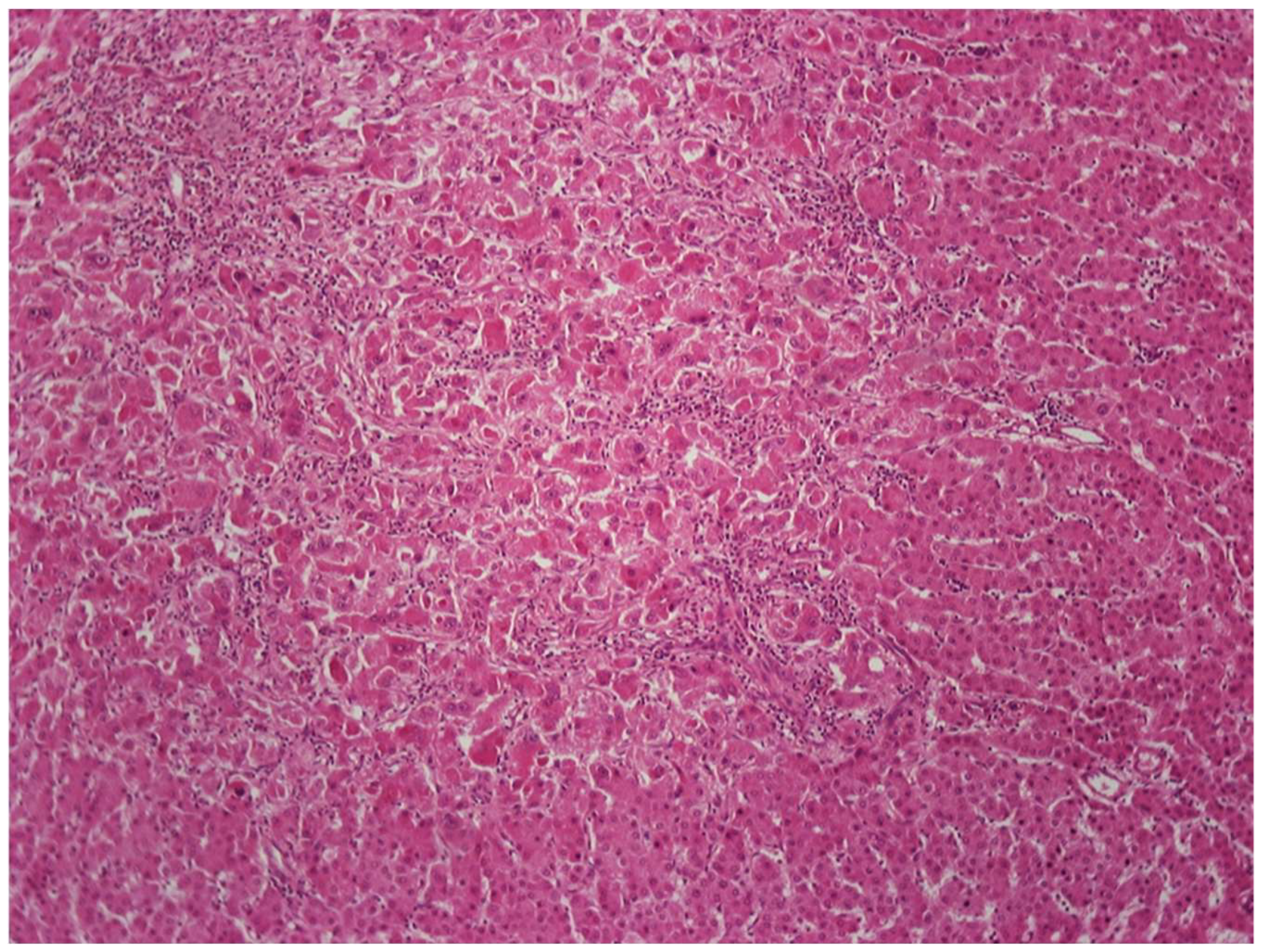
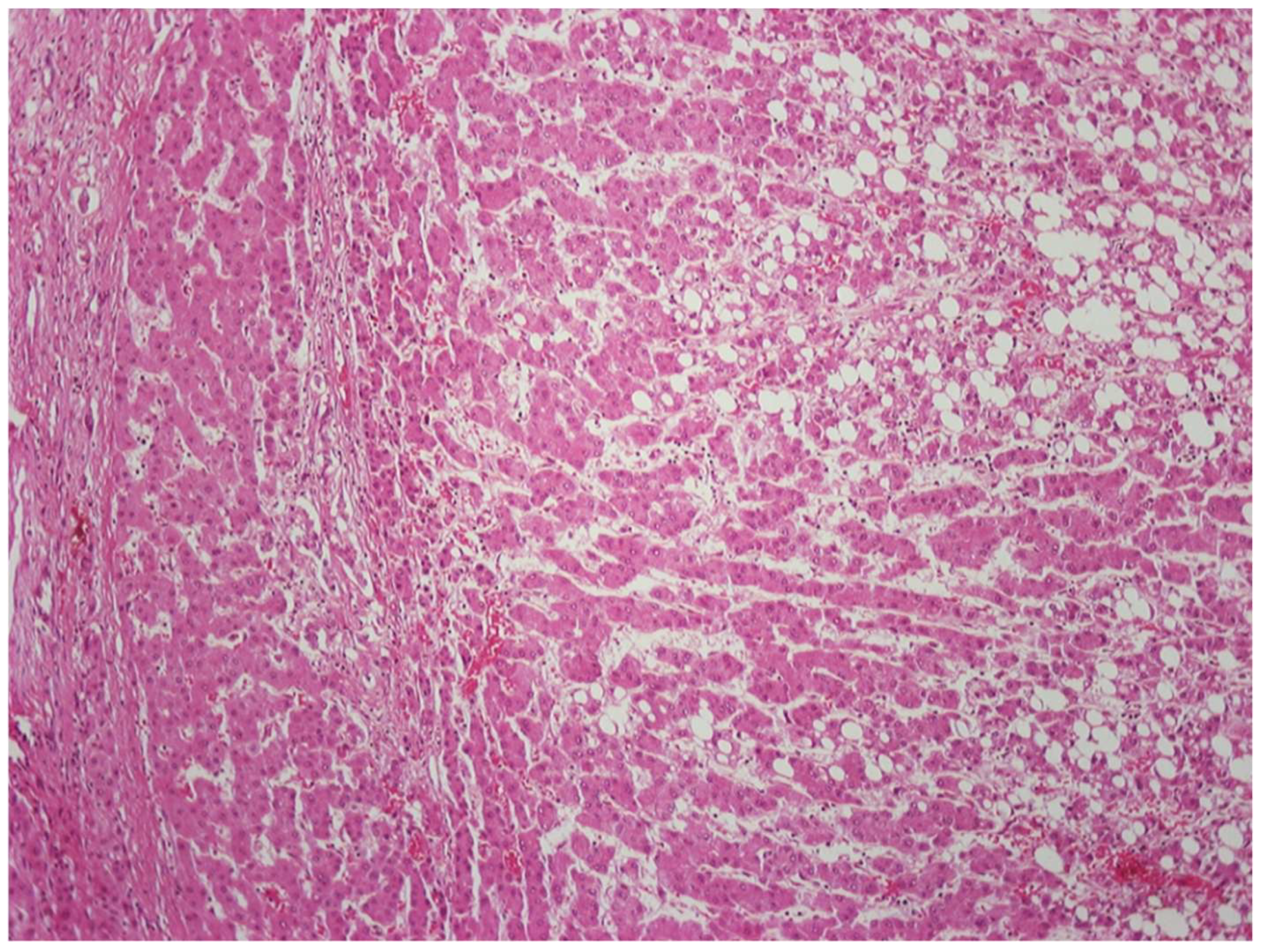
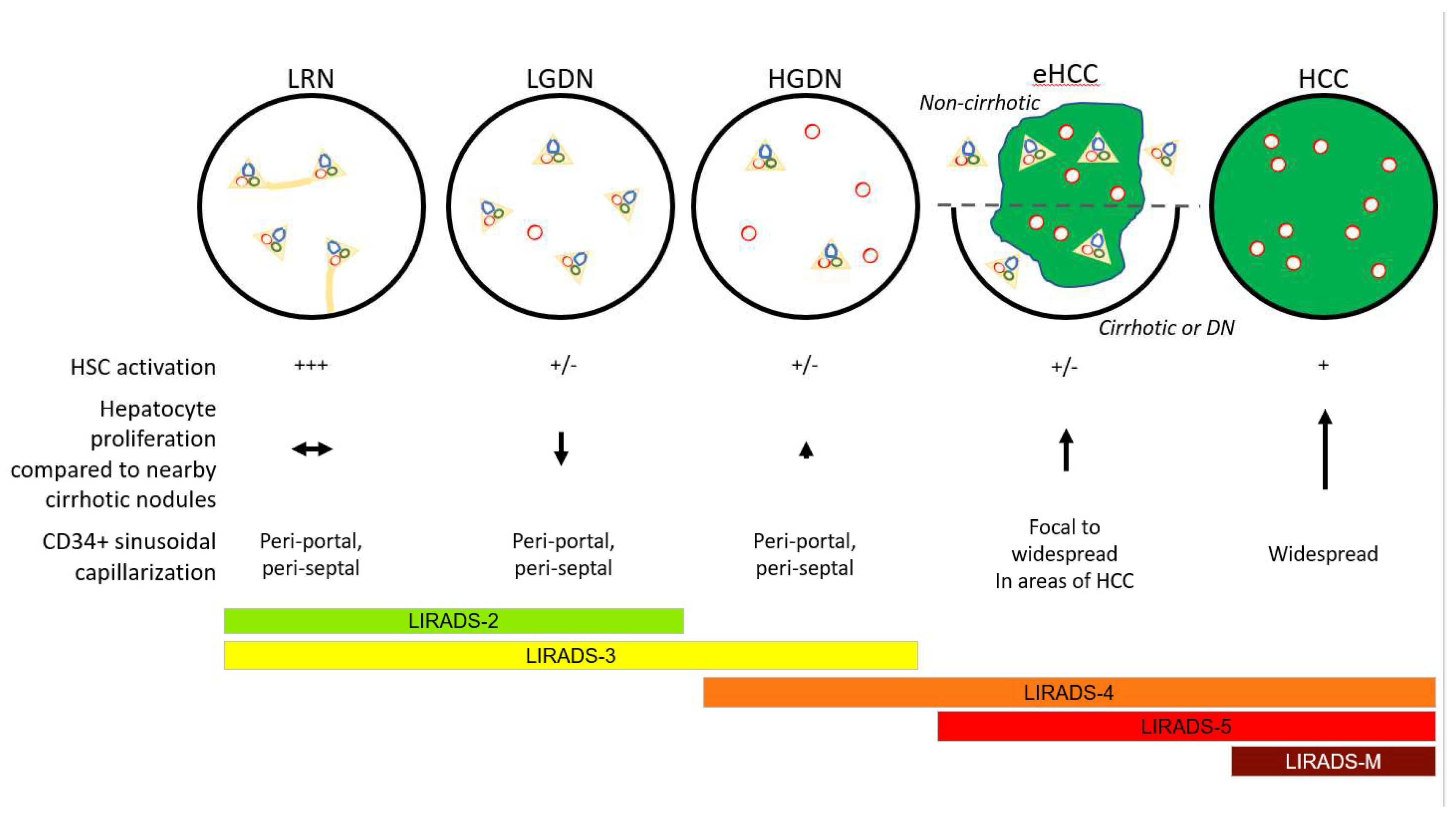
6. Precancerous Lesions in Hepatocarcinogenesis
- (i)
- dysplastic foci (DFs), which are incidentally detected on microscopic examination and measure less than 1 mm in diameter;
- (ii)
- dysplastic nodules (DNs), which are larger than dysplastic foci, occasionally measuring over 1 cm in diameter, and may be detected on imaging studies and gross examination
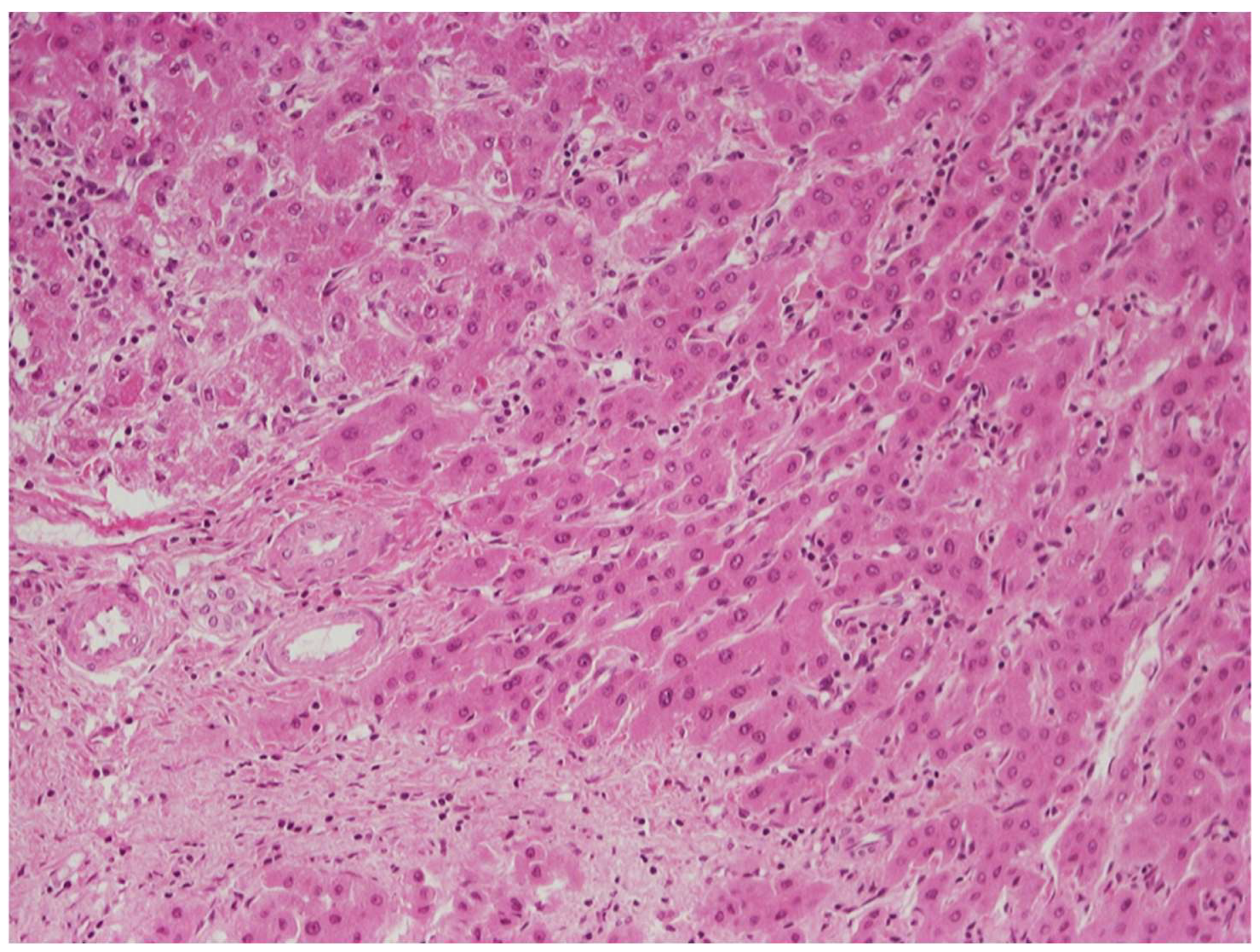
6.1. Low-Grade vs. High-Grade Dysplastic Nodules
6.2. Low-Grade Dysplastic Nodules vs. Large Regenerative Nodules
6.3. High-Grade Dysplastic Nodules vs. Hepatocellular Carcinoma
7. Frequently Asked Questions
- FAQ14.1. Tissue Diagnosis of cHCC–CCA
- FAQ14.2. Pathology–Radiology Collaboration for cHCC–CCA
- FAQ14.3. Molecular Pathology and Treatment Implications of the Diagnosis of cHCC–CCA
- LIRADS-1: The pathologist may advise the clinical team that, while this lesion is probably just a regenerative nodule, the possibility that it is a DN, possibly even an HGDN, is not excluded. Repeat screening at a shorter time interval may be warranted. If the lesion disappears, it was probably large regenerative nodule that underwent involution or further scarring that eliminated its distinctive appearance on imaging. If it does indeed disappear, return to normal surveillance screening is reasonable.
- LIRADS-2 or -3: These lesions are more likely to be DNs, either LGDN or HGDN. Repeat imaging should be performed more frequently. If the nodule disappears, it was probably regenerative. If it persists, then it may be LGDN or HGDN and the patient is considered at higher risk for HCC and should return more frequently for imaging. If the lesion progresses upward in LIRADS score, it is probably a DN giving rise to an HCC. Continued imaging or ablation may be considered depending on the clinical circumstances.
- LIRADS-4: These lesions are probably an HGDN, possibly with an emerging focus of HCC, or possibly a small HCC. Continued imaging or ablation may be considered depending on clinical circumstances.
- LIRADS-5: This feature is diagnostic for HCC. While a biopsy is not necessary for diagnosis, oncologists are increasingly requesting a pre-ablation biopsy for molecular studies to inform future treatments if the lesion is resistant to ablation or if there is post-treatment (i.e., ablation, resection, or transplant) recurrence.
- LIRADS-M: These are lesions without typical imaging features of HCC, but highly suspicious for malignancy. The pathologists may aver that the lesion could be metastatic (M), but they could also be iCCA or cHCC–CCA. Such lesions probably require biopsy for diagnosis.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bioulac-Sage, P.; Gouw, A.S.; Balabaud, C.; Sempoux, C. Hepatocellular adenoma: What we know, what we do not know, and why it matters. Histopathology 2022, 80, 878–897. [Google Scholar] [CrossRef] [PubMed]
- Sempoux, C.; Gouw, A.S.; Dunet, V.; Paradis, V.; Balabaud, C.; Bioulac-Sage, P. Predictive Patterns of Glutamine Synthetase Immunohistochemical Staining in CTNNB1-mutated Hepatocellular Adenomas. Am. J. Surg. Pathol. 2021, 45, 477–487. [Google Scholar] [CrossRef] [PubMed]
- Henriet, E.; Hammoud, A.A.; Dupuy, J.-W.; Dartigues, B.; Ezzoukry, Z.; Dugot-Senant, N.; Leste-Lasserre, T.; Pallares-Lupon, N.; Nikolski, M.; Le Bail, B.; et al. Argininosuccinate synthase 1 (ASS1): A marker of unclassified hepatocellular adenoma and high bleeding risk. Hepatology 2017, 66, 2016–2028. [Google Scholar] [CrossRef] [Green Version]
- Sala, M.; Gonzales, D.; Leste-Lasserre, T.; Dugot-Senant, N.; Paradis, V.; Di Tommaso, S.; Dupuy, J.; Pitard, V.; Dourthe, C.; Sciarra, A.; et al. ASS1 Overexpression: A Hallmark of Sonic Hedgehog Hepatocellular Adenomas; Recommendations for Clinical Practice. Hepatol. Commun. 2020, 4, 809–824. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Disease Liver Cancer Collaboration. The Burden of Primary Liver Cancer and Underlying Etiologies From 1990 to 2015 at the Global, Regional, and National Level: Results from the Global Burden of Disease Study 2015. JAMA Oncol. 2017, 3, 1683–1691. [Google Scholar] [CrossRef]
- Ioannou, G.N. Epidemiology and risk-stratification of NAFLD-associated HCC. J. Hepatol. 2021, 75, 1476–1484. [Google Scholar] [CrossRef] [PubMed]
- Paterlini-Bréchot, P.; Saigo, K.; Murakami, Y.; Chami, M.; Gozuacik, D.; Mugnier, C.; Lagorce, D.; Bréchot, C. Hepatitis B virus-related insertional mutagenesis occurs frequently in human liver cancers and recurrently targets human telomerase gene. Oncogene 2003, 22, 3911–3916. [Google Scholar] [CrossRef]
- Murakami, Y.; Saigo, K.; Takashima, H.; Minami, M.; Okanoue, T.; Bréchot, C.; Brechot, P.P. Large scaled analysis of hepatitis B virus (HBV) DNA integration in HBV related hepatocellular carcinomas. Gut 2005, 54, 1162–1168. [Google Scholar] [CrossRef]
- Sung, W.-K.; Zheng, H.; Li, S.; Chen, R.; Liu, X.; Li, Y.; Lee, N.P.; Lee, W.H.; Ariyaratne, P.N.; Tennakoon, C.; et al. Genome-wide survey of recurrent HBV integration in hepatocellular carcinoma. Nat. Genet. 2012, 44, 765–769. [Google Scholar] [CrossRef]
- Goh, J.; Callagy, G.; McEntee, G.; O’Keane, J.C.; Bomford, A.; Crowe, J. Hepatocellular carcinoma arising in the absence of cirrhosis in genetic haemochromatosis: Three case reports and review of literature. Eur. J. Gastroenterol. Hepatol. 1999, 11, 915–919. [Google Scholar] [CrossRef] [PubMed]
- Honeyman, J.N.; Simon, E.P.; Robine, N.; Chiaroni-Clarke, R.; Darcy, D.G.; Lim, I.I.P.; Gleason, C.E.; Murphy, J.M.; Rosenberg, B.R.; Teegan, L.; et al. Detection of a Recurrent DNAJB1-PRKACA Chimeric Transcript in Fibrolamellar Hepatocellular Carcinoma. Science 2014, 343, 1010–1014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thorgeirsson, S.S.; Grisham, J.W. Molecular pathogenesis of human hepatocellular carcinoma. Nat. Genet. 2002, 31, 339–346. [Google Scholar] [CrossRef]
- Hatziapostolou, M.; Polytarchou, C.; Aggelidou, E.; Drakaki, A.; Poultsides, G.A.; Jaeger, S.A.; Ogata, H.; Karin, M.; Struhl, K.; Hadzopoulou-Cladaras, M.; et al. An HNF4α-miRNA inflammatory feedback circuit regulates hepatocellular oncogenesis. Cell 2011, 147, 1233–1247. [Google Scholar] [CrossRef] [Green Version]
- Brody, R.I.; Theise, N.D. An inflammatory proposal for hepatocarcinogenesis. Hepatology 2012, 56, 382–384. [Google Scholar] [CrossRef]
- Hytiroglou, P.; Bioulac-Sage, P. Molecular Pathogenesis and Diagnostics of Hepatocellular Tumors. In Odze and Goldblum Surgical Pathology of the GI Tract, Liver, Biliary Tract, and Pancreas, 4th ed.; Odze, R.D., Goldblum, J.R., Eds.; Elsevier: Philadelphia, PA, USA, 2023; pp. 1369–1383. [Google Scholar]
- Gerbes, A.; Zoulim, F.; Tilg, H.; Dufour, J.-F.; Bruix, J.; Paradis, V.; Salem, R.; Peck-Radosavljevic, M.; Galle, P.R.; Greten, T.F.; et al. Gut roundtable meeting paper: Selected recent advances in hepatocellular carcinoma. Gut 2018, 67, 380–388. [Google Scholar] [CrossRef]
- Nault, J.C.; Mallet, M.; Pilati, C.; Calderaro, J.; Bioulac-Sage, P.; Laurent, C.; Laurent, A.; Cherqui, D.; Balabaud, C.; Zucman-Rossi, J. High frequency of telomerase reverse-transcriptase promoter somatic mutations in hepatocellular carcinoma and preneoplastic lesions. Nat. Commun. 2013, 4, 2218. [Google Scholar] [CrossRef] [Green Version]
- Nault, J.-C.; Ningarhari, M.; Rebouissou, S.; Zucman-Rossi, J. The role of telomeres and telomerase in cirrhosis and liver cancer. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 544–558. [Google Scholar] [CrossRef] [PubMed]
- Nault, J.C.; Calderaro, J.; Di Tommaso, L.; Balabaud, C.; Zafrani, E.S.; Bioulac-Sage, P.; Roncalli, M.; Zucman-Rossi, J. Telomerase reverse transcriptase promoter mutation is an early somatic genetic alteration in the transformation of premalignant nodules in hepatocellular carcinoma on cirrhosis. Hepatology 2014, 60, 1983–1992. [Google Scholar] [CrossRef] [PubMed]
- The Cancer Genome Atlas Research Network. Comprehensive and integrative genomic characterization of hepatocellular carcinoma. Cell 2017, 169, 1327–1341. [Google Scholar] [CrossRef] [Green Version]
- Dhanasekaran, R.; Nault, J.-C.; Roberts, L.R.; Zucman-Rossi, J. Genomic Medicine and Implications for Hepatocellular Carcinoma Prevention and Therapy. Gastroenterology 2019, 156, 492–509. [Google Scholar] [CrossRef]
- Nault, J.; Martin, Y.; Caruso, S.; Hirsch, T.; Bayard, Q.; Calderaro, J.; Charpy, C.; Copie-Bergman, C.; Ziol, M.; Bioulac-Sage, P.; et al. Clinical Impact of Genomic Diversity From Early to Advanced Hepatocellular Carcinoma. Hepatology 2020, 71, 164–182. [Google Scholar] [CrossRef]
- Totoki, Y.; Tatsuno, K.; Covington, K.R.; Ueda, H.; Creighton, C.J.; Kato, M.; Tsuji, S.; Donehower, L.A.; Slagle, B.L.; Nakamura, H.; et al. Trans-ancestry mutational landscape of hepatocellular carcinoma genomes. Nat. Genet. 2014, 46, 1267–1273. [Google Scholar] [CrossRef] [PubMed]
- Schulze, K.; Imbeaud, S.; Letouzé, E.; Alexandrov, L.B.; Calderaro, J.; Rebouissou, S.; Couchy, G.; Meiller, C.; Shinde, J.; Soysouvanh, F.; et al. Exome sequencing of hepatocellular carcinomas identifies new mutational signatures and potential therapeutic targets. Nat. Genet. 2015, 47, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Villanueva, A. Hepatocellular carcinoma. N. Engl. J. Med. 2019, 380, 1450–1462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boyault, S.; Rickman, D.S.; Bioulac-Sage, P.; De Reyniès, A.; Balabaud, C.; Rebouissou, S.; Jeannot, E.; Hérault, A.; Saric, J.; Belghiti, J.; et al. Transcriptome classification of HCC is related to gene alterations and to new therapeutic targets. Hepatology 2007, 45, 42–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoshida, Y.; Nijman, S.M.B.; Kobayashi, M.; Chan, J.A.; Brunet, J.-P.; Chiang, D.Y.; Villanueva, A.; Newell, P.; Ikeda, K.; Hashimoto, M.; et al. Integrative Transcriptome Analysis Reveals Common Molecular Subclasses of Human Hepatocellular Carcinoma. Cancer Res. 2009, 69, 7385–7392. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nault, J.; De Reyniès, A.; Villanueva, A.; Calderaro, J.; Rebouissou, S.; Couchy, G.; Decaens, T.; Franco, D.; Imbeaud, S.; Rousseau, F.; et al. A Hepatocellular Carcinoma 5-Gene Score Associated With Survival of Patients After Liver Resection. Gastroenterology 2013, 145, 176–187. [Google Scholar] [CrossRef]
- Calderaro, J.; Couchy, G.; Imbeaud, S.; Amaddeo, G.; Letouzé, E.; Blanc, J.-F.; Laurent, C.; Hajji, Y.; Azoulay, D.; Bioulac-Sage, P.; et al. Histological subtypes of hepatocellular carcinoma are related to gene mutations and molecular tumour classification. J. Hepatol. 2017, 67, 727–738. [Google Scholar] [CrossRef] [PubMed]
- Torbenson, M.S.; Ng, I.O.L.; Park, Y.N.; Roncalli, M.; Sakamoto, M. Hepatocellular carcinoma. In Digestive System Tumours, 5th ed.; WHO Classification of Tumours Editorial Board; WHO Classification of Tumours Series; International Agency for Research on Cancer: Lyon, France, 2019; Volume 1, pp. 229–239. [Google Scholar]
- International Consensus Group for Hepatocellular Neoplasia. Pathologic diagnosis of early hepatocellular carcinoma: A report of the International Consensus Group for Hepatocellular Neoplasia. Hepatology 2009, 49, 658–664. [Google Scholar] [CrossRef] [Green Version]
- Kojiro, M. Pathology of Hepatocellular Carcinoma; Blackwell: Malden, MA, USA, 2006. [Google Scholar]
- Salomao, M.; Woojin, M.Y.; Brown, R.S., Jr.; Emond, J.C.; Lefkowitch, J.H. Steatohepatitic hepatocellular carcinoma (SH-HCC): A distinctive histological variant of HCC in hepatitis C virus-related cirrhosis with associated NAFLD/NASH. Am. J. Surg. Pathol. 2010, 34, 1630–1636. [Google Scholar] [CrossRef]
- Yeh, M.M.; Liu, Y.; Torbenson, M. Steatohepatitic variant of hepatocellular carcinoma in the absence of metabolic syndrome or background steatosis: A clinical, pathological, and genetic study. Hum. Pathol. 2015, 46, 1769–1775. [Google Scholar] [CrossRef]
- Li, T.; Fan, J.; Qin, L.-X.; Zhou, J.; Sun, H.-C.; Qiu, S.-J.; Ye, Q.-H.; Wang, L.; Tang, Z.-Y. Risk Factors, Prognosis, and Management of Early and Late Intrahepatic Recurrence After Resection of Primary Clear Cell Carcinoma of the Liver. Ann. Surg. Oncol. 2011, 18, 1955–1963. [Google Scholar] [CrossRef]
- Torbenson, M.S. Hepatocellular carcinoma: Making sense of morphological heterogeneity, growth patterns, and subtypes. Hum. Pathol. 2021, 112, 86–101. [Google Scholar] [CrossRef]
- Wood, L.D.; Heaphy, C.M.; Daniel, H.D.-J.; Naini, B.V.; Lassman, C.R.; Arroyo, M.R.; Kamel, I.R.; Cosgrove, D.P.; Boitnott, J.K.; Meeker, A.K.; et al. Chromophobe hepatocellular carcinoma with abrupt anaplasia: A proposal for a new subtype of hepatocellular carcinoma with unique morphological and molecular features. Mod. Pathol. 2013, 26, 1586–1593. [Google Scholar] [CrossRef]
- Torbenson, M.S. Morphologic Subtypes of Hepatocellular Carcinoma. Gastroenterol. Clin. N. Am. 2017, 46, 365–391. [Google Scholar] [CrossRef] [PubMed]
- Maeda, T.; Adachi, E.; Kajiyama, K.; Takenaka, K.; Sugimachi, K.; Tsuneyoshi, M. Spindle cell hepatocellular carcinoma: A clinicopathologic and immunohistochemical analysis of 15 cases. Cancer 1996, 77, 51–57. [Google Scholar] [CrossRef]
- Kojiro, M.; Sugihara, S.; Kakizoe, S.; Nakashima, O.; Kiyomatsu, K. Hepatocellular carcinoma with sarcomatous change: A special reference to the relationship with anticancer therapy. Cancer Chemother. Pharmacol. 1989, 23, S4–S8. [Google Scholar] [CrossRef]
- International Working Party. Terminology of nodular hepatocellular lesions. Hepatology 1995, 22, 983–993. [Google Scholar] [CrossRef]
- Watanabe, S.; Okita, K.; Harada, T.; Kodama, T.; Numa, Y.; Takemoto, T.; Takahashi, T. Morphologic studies of the liver cell dysplasia. Cancer 1983, 51, 2197–2205. [Google Scholar] [CrossRef]
- Deugnier, Y.M.; Charalambous, P.; Le Quilleuc, D.; Turlin, B.; Searle, J.; Brissot, P.; Powell, L.W.; Halliday, J.W. Preneoplastic significance of hepatic iron-free foci in genetic hemochromatosis: A study of 185 patients. Hepatology 1993, 18, 1363–1369. [Google Scholar]
- Hytiroglou, P.; Park, Y.N.; Krinsky, G.; Theise, N.D. Hepatic Precancerous Lesions and Small Hepatocellular Carcinoma. Gastroenterol. Clin. N. Am. 2007, 36, 867–887. [Google Scholar] [CrossRef]
- Park, Y.N.; Kojiro, M.; Di Tommaso, L.; Dhillon, A.P.; Kondo, F.; Nakano, M.; Sakamoto, M.; Theise, N.D.; Roncalli, M. Ductular reaction is helpful in defining early stromal invasion, small hepatocellular carcinomas, and dysplastic nodules. Cancer 2007, 109, 915–923. [Google Scholar] [CrossRef]
- Hytiroglou, P.; Theise, N.D. The differential diagnosis of liver nodules. Sem. Diag. Pathol. 1998, 15, 285–299. [Google Scholar]
- Theise, N.D.; Marcelin, K.; Goldfischer, M.; Hytiroglou, P.; Ferrell, L.; Thung, S.N. Low proliferative activity in macroregenerative nodules: Evidence for an alternate hypothesis concerning human hepatocarcinogenesis. Liver 1996, 16, 134–139. [Google Scholar] [CrossRef]
- Park, Y.N.; Yang, C.-P.; Cubukcu, O.; Thung, S.N.; Theise, N.D. Hepatic stellate cell activation in dysplastic nodules: Evidence for an alternate hypothesis concerning human hepatocarcinogenesis. Liver Int. 2008, 17, 271–274. [Google Scholar] [CrossRef] [PubMed]
- Hytiroglou, P.; Theise, N.D.; Schwartz, M.; Mor, E.; Miller, C.; Thung, S.N. Macroregenerative nodules in a series of adult cirrhotic liver explants: Issues of classification and nomenclature. Hepatology 1995, 21, 703–708. [Google Scholar] [PubMed]
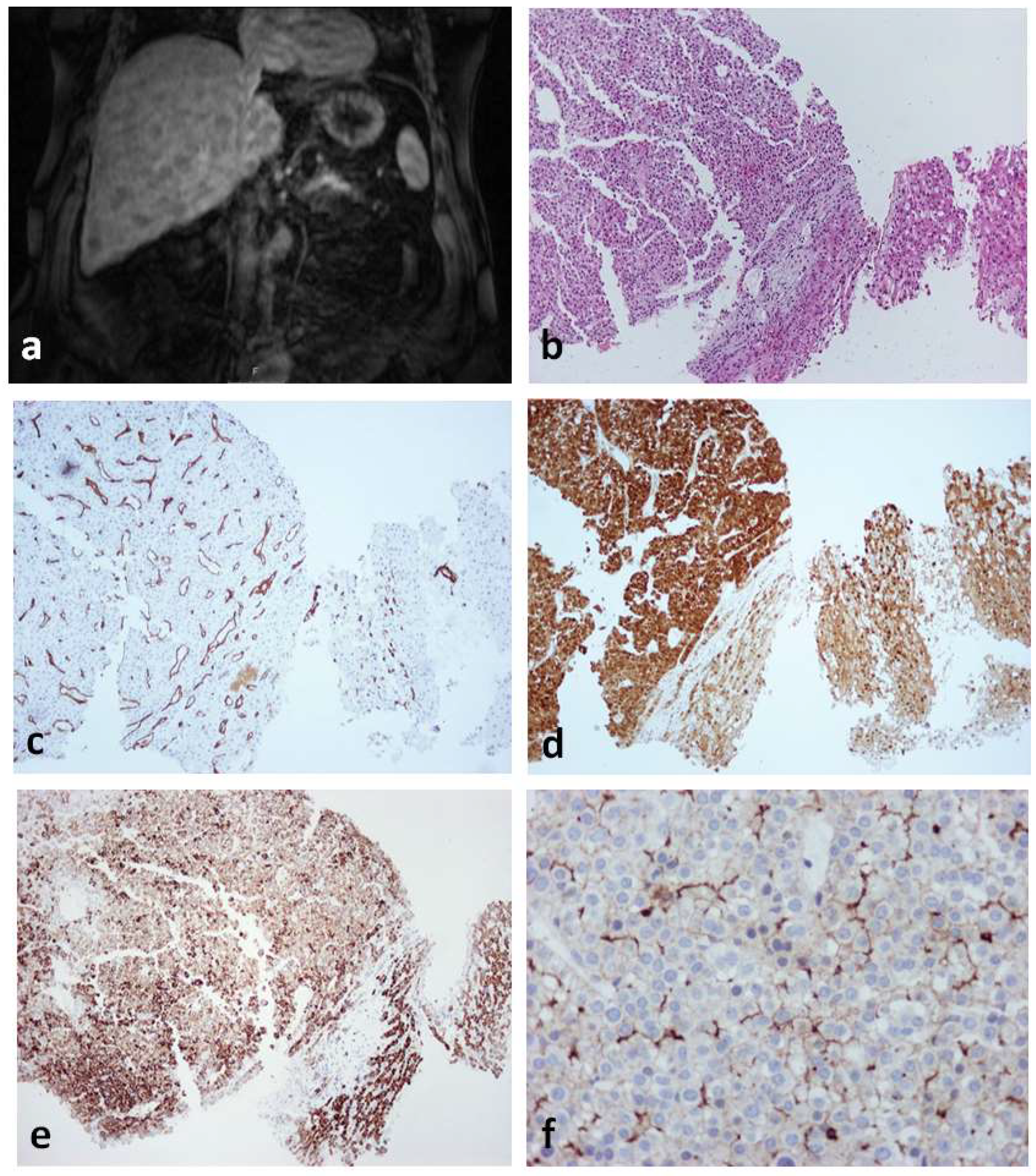
- Park, Y.N.; Yang, C.-P.; Fernandez, G.J.; Cubukcu, O.; Thung, S.N.; Theise, N.D. Neoangiogenesis and Sinusoidal “Capillarization” in Dysplastic Nodules of the Liver. Am. J. Surg. Pathol. 1998, 22, 656–662. [Google Scholar] [CrossRef] [PubMed]
- Theise, N.D.; Park, Y.N.; Thung, S.N. “Vascular profiles” of regenerative and dysplastic nodules. Hepatology 2000, 31, 1380–1381. [Google Scholar] [CrossRef] [PubMed]
- Di Tommaso, L.; Franchi, G.; Park, Y.N.; Fiamengo, B.; Destro, A.; Morenghi, E.; Montorsi, M.; Torzilli, G.; Tommasini, M.; Terracciano, L.; et al. Diagnostic value of HSP70, glypican 3, and glutamine synthetase in hepatocellular nodules in cirrhosis. Hepatology 2007, 45, 725–734. [Google Scholar]
- Di Tommaso, L.; Destro, A.; Seok, J.Y.; Balladore, E.; Terracciano, L.; Sangiovanni, A.; Iavarone, M.; Colombo, M.G.; Jang, J.J.; Yu, E.; et al. The application of markers (HSP70 GPC3 and GS) in liver biopsies is useful for detection of hepatocellular carcinoma. J. Hepatol. 2009, 50, 746–754. [Google Scholar]
- Hytiroglou, P. Well-differentiated hepatocellular nodule: Making a diagnosis on biopsy and resection specimens of patients with advanced stage chronic liver disease. Semin. Diagn. Pathol. 2017, 34, 138–145. [Google Scholar] [CrossRef]
- Bioulac-Sage, P.; Kakar, S.; Nault, J.C. Hepatocellular adenoma. In Digestive System Tumours, 5th ed.; WHO Classification of Tumours Editorial Board; WHO Classification of Tumours Series; International Agency for Research on Cancer: Lyon, France, 2019; Volume 1, pp. 224–228. [Google Scholar]
- Joseph, N.M.; Blank, A.; Shain, A.H.; Gill, R.M.; Umetsu, S.E.; Shafizadeh, N.; Torbenson, M.S.; Kakar, S. Hepatocellular neoplasms with loss of liver fatty acid binding protein: Clinicopathologic features and molecular profiling. Hum. Pathol. 2022, 122, 60–71. [Google Scholar] [CrossRef]
- Julien, C.; Le Bail, B.; Chiche, L.; Balabaud, C.; Bioulac-Sage, P. Malignant transformation of hepatocellular adenoma. JHEP Rep. 2022, 4, 100430. [Google Scholar] [CrossRef] [PubMed]
- Calderaro, J.; Nault, J.C.; Balabaud, C.; Couchy, G.; Saint-Paul, M.-C.; Azoulay, D.; Mehdaoui, D.; Luciani, A.; Zafrani, E.S.; Bioulac-Sage, P.; et al. Inflammatory hepatocellular adenomas developed in the setting of chronic liver disease and cirrhosis. Mod. Pathol. 2016, 29, 43–50. [Google Scholar] [CrossRef] [Green Version]
- Sasaki, M.; Yoneda, N.; Sawai, Y.; Imai, Y.; Kondo, F.; Fukusato, T.; Yoshikawa, S.; Kobayashi, S.; Sato, Y.; Matsui, O.; et al. Clinicopathological characteristics of serum amyloid A-positive hepatocellular neoplasms/nodules arising in alcoholic cirrhosis. Histopathology 2015, 66, 836–845. [Google Scholar] [CrossRef] [PubMed]
- Rebouissou, S.; Franconi, A.; Calderaro, J.; Letouzé, E.; Imbeaud, S.; Pilati, C.; Nault, J.-C.; Couchy, G.; Laurent, A.; Balabaud, C.; et al. Genotype-phenotype correlation of CTNNB1 mutations reveals different β-catenin activity associated with liver tumor progression. Hepatology 2016, 64, 2047–2061. [Google Scholar] [CrossRef] [Green Version]
- European Association for the Study of the Liver (EASL). EASL Clinical Practice Guidelines on the Management of Benign Liver Tumours. Available online: https://www.journal-of-hepatology.eu/article/S0168-8278(16)30101-5/pdf (accessed on 31 January 2022).
- Julien, C.; Le-Bail, B.; Touhami, K.O.; Frulio, N.; Blanc, J.; Adam, J.; Laurent, C.; Balabaud, C.; Bioulac-Sage, P.; Chiche, L. Hepatocellular adenoma risk factors of hemorrhage: Size is not the only concern! Single center retrospective experience of 261 patients. Ann. Surg. 2021, 274, 843–850. [Google Scholar] [CrossRef]
- Klompenhouwer, A.J.; Rosmalen, B.V.; Haring, M.P.D.; Thomeer, M.G.J.; Doukas, M.; Verheij, J.; Meijer, V.E.; Gulik, T.M.; Takkenberg, R.B.; Kazemier, G.; et al. A multicentre retrospective analysis on growth of residual hepatocellular adenoma after resection. Liver Int. 2020, 40, 2272–2278. [Google Scholar] [CrossRef]
- Putra, J.; Ferrell, L.D.; Gouw, A.S.H.; Paradis, V.; Rishi, A.; Sempoux, C.; Balabaud, C.; Thung, S.N.; Bioulac-Sage, P. Malignant transformation of liver fatty acid binding protein-deficient hepatocellular adenomas: Histopathologic spectrum of a rare phenomenon. Mod. Pathol. 2020, 33, 665–675. [Google Scholar] [CrossRef] [PubMed]
- Haring, M.P.D.; Cuperus, F.J.C.; Duiker, E.W.; de Haas, R.J.; de Meijer, V.E. Scoping review of clinical practice guidelines on the management of benign liver tumors. BMJ Open Gastroenterol. 2021, 8, e000592. [Google Scholar]
- Lang, H.; Sotiropoulos, G.C.; Brokalaki, E.I.; Schmitz, K.J.; Bertona, C.; Meyer, G.; Frilling, A.; Paul, A.; Malagó, M.; Broelsch, C.E. Survival and Recurrence Rates after Resection for Hepatocellular Carcinoma in Noncirrhotic Livers. J. Am. Coll. Surg. 2007, 205, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Rui, J.-A.; Wang, S.-B.; Chen, S.-G.; Qu, Q.; Chi, T.-Y.; Wei, X.; Han, K.; Zhang, N.; Zhao, H.-T. Outcomes and prognostic factors of cirrhotic patients with hepatocellular carcinoma after radical major hepatectomy. World J. Surg. 2007, 31, 1782–1787. [Google Scholar] [CrossRef] [PubMed]
- Jonas, S.; Bechstein, W.O.; Steinmüller, T.; Herrmann, M.; Radke, C.; Berg, T.; Settmacher, U.; Neuhaus, P. Vascular invasion and histopathologic grading determine outcome after liver transplantation for hepatocellular carcinoma in cirrhosis. Hepatology 2001, 33, 1080–1086. [Google Scholar] [CrossRef] [PubMed]
- Colecchia, A.; Scaioli, E.; Montrone, L.; Vestito, A.; Di Biase, A.R.; Pieri, M.; D’Errico-Grigioni, A.; Bacchi-Reggiani, M.L.; Ravaioli, M.; Grazi, G.L.; et al. Pre-operative liver biopsy in cirrhotic patients with early hepatocellular carcinoma represents a safe and accurate diagnostic tool for tumour grading assessment. J. Hepatol. 2011, 54, 300–305. [Google Scholar] [CrossRef]
- Ferrell, L.D.; Kakar, S.; Terraciano, M.; Wee, A. Tumours and Tumour-like lesions of the liver. In MacSween’s Pathology of the Liver, 7th ed.; Burt, A.D., Ferrell, L.D., Huebscher, S.G., Eds.; Elsevier: Phladelphia, PA, USA, 2018; pp. 780–879. [Google Scholar]
- Lagana, S.; Hsiao, S.; Bao, F.; Sepulveda, A.; Moreira, R.; Lefkowitch, J.; Remotti, H. HepPar-1 and Arginase-1 Immunohistochemistry in Adenocarcinoma of the Small Intestine and Ampullary Region. Arch. Pathol. Lab. Med. 2015, 139, 791–795. [Google Scholar] [CrossRef] [Green Version]
- Saxena, R.; Albores-Saavedra, J.; Bioulac-Sage, P.; Hytiroglou, P.; Sakamoto, M.; Theise, N.D.; Sui, W.M.S. Diagnostic algorithms for tumours of the liver. In WHO Classification of Tumours of the Digestive System, 4th ed.; Bosman, F.T., Carneiro, F., Hruban, R.H., Theise, N.D., Eds.; IARC: Lyon, France, 2010. [Google Scholar]
- Kim, H.; Choi, G.H.; Na, D.C.; Ahn, E.Y.; Kim, G.I.; Lee, J.E.; Cho, J.Y.; Yoo, J.E.; Choi, J.S.; Park, Y.N. Human hepatocellular carcinomas with “Stemness”-related marker expression: Keratin 19 expression and a poor prognosis. Hepatology 2011, 54, 1707–1717. [Google Scholar] [CrossRef]
- Tsuchiya, K.; Komuta, M.; Yasui, Y.; Tamaki, N.; Hosokawa, T.; Ueda, K.; Kuzuya, T.; Itakura, J.; Nakanishi, H.; Takahashi, Y.; et al. Expression of Keratin 19 Is Related to High Recurrence of Hepatocellular Carcinoma after Radiofrequency Ablation. Oncology 2011, 80, 278–288. [Google Scholar] [CrossRef]
- Rhee, H.; Nahm, J.H.; Kim, H.; Choi, G.H.; Yoo, J.E.; Lee, H.S.; Koh, M.J.; Park, Y.N. Poor outcome of hepatocellular carcinoma with stemness marker under hypoxia: Resistance to transarterial chemoembolization. Mod. Pathol. 2016, 29, 1038–1049. [Google Scholar] [CrossRef]
- Llovet, J.M.; Pinyol, R.; Kelley, R.K.; El-Khoueiry, A.; Reeves, H.L.; Wang, X.W.; Gores, G.J.; Villanueva, A. Molecular pathogenesis and systemic therapies for hepatocellular carcinoma. Nat. Cancer 2022, 3, 386–401. [Google Scholar] [CrossRef] [PubMed]
- Brunt, E.; Aishima, S.; Clavien, P.-A.; Fowler, K.; Goodman, Z.; Gores, G.; Gouw, A.; Kagen, A.; Klimstra, D.; Komuta, M.; et al. cHCC-CCA: Consensus terminology for primary liver carcinomas with both hepatocytic and cholangiocytic differentation. Hepatology 2018, 68, 113–126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Vito, C.; Sarker, D.; Ross, P.; Heaton, N.; Quaglia, A. Histological heterogeneity in primary and metastatic classic combined hepatocellular-cholangiocarcinoma: A case series. Virchows Arch. 2017, 471, 619–629. [Google Scholar] [CrossRef]
- Zen, C.; Zen, Y.; Mitry, R.R.; Corbeil, D.; Karbanova, J.; O’Grady, J.; Karani, J.; Kane, P.; Heaton, N.; Portmann, B.C.; et al. Mixed phenotype hepatocellular carcinoma after transarterial chemoembolization and liver transplantation. Liver Transplant. 2011, 17, 943–954. [Google Scholar] [CrossRef]
- Lai, J.-P.; Conley, A.; Knudsen, B.S.; Guindi, M. Hypoxia after transarterial chemoembolization may trigger a progenitor cell phenotype in hepatocellular carcinoma. Histopathology 2015, 67, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Theise, N.D.; Nakashima, O.; Park, Y.N.; Nakanuma, Y. Combined hepatocellular-cholangiocarcinoma. In WHO Classification of Tumours of the Digestive System, 4th ed.; Bosman, F.T., Carneiro, F., Hruban, R.H., Theise, N.D., Eds.; IARC: Lyon, France, 2010. [Google Scholar]
- Sempoux, C.; Kakar, S.; Kondo, F. Combined hepatocellular-cholangiocarcinoma and undifferentiated primary liver carcinoma. In Digestive System Tumours, 5th ed.; WHO Classification of Tumours Editorial Board; WHO Classification of Tumours Series; International Agency for Research on Cancer: Lyon, France, 2019; Volume 1, pp. 260–262. [Google Scholar]
- Kim, M.; Hwang, S.; Ahn, C.-S.; Kim, K.-H.; Moon, D.-B.; Song, G.-W.; Jung, D.-H.; Hong, S.-M. Post-resection prognosis of combined hepatocellular carcinoma-cholangiocarcinoma cannot be predicted by the 2019 World Health Organization classification. Asian J. Surg. 2021, 44, 1389–1395. [Google Scholar] [CrossRef]
- Gigante, E.; Ronot, M.; Bertin, C.; Ciolina, M.; Bouattour, M.; Dondero, F.; Cauchy, F.; Soubrane, O.; Vilgrain, V.; Paradis, V. Combining imaging and tumour biopsy improves the diagnosis of combined hepatocellular-cholangiocarcinoma. Liver Int. 2019, 39, 2386–2396. [Google Scholar] [CrossRef] [PubMed]
- Jeon, S.K.; Joo, I.; Lee, D.H.; Lee, S.M.; Kang, H.-J.; Lee, K.-B.; Lee, J.M. Combined hepatocellular cholangiocarcinoma: LI-RADS v2017 categorisation for differential diagnosis and prognostication on gadoxetic acid-enhanced MR imaging. Eur. Radiol. 2019, 29, 373–382. [Google Scholar] [CrossRef]
- Zou, X.; Luo, Y.; Morelli, J.N.; Hu, X.; Shen, Y.; Hu, D. Differentiation of hepatocellular carcinoma from intrahepatic cholangiocarcinoma and combined hepatocellular-cholangiocarcinoma in high-risk patients matched to MR field strength: Diagnostic performance of LI-RADS version 2018. Abdom. Radiol. 2021, 46, 3168–3178. [Google Scholar] [CrossRef]
- Beaufrère, A.; Calderaro, J.; Paradis, V. Combined hepatocellular-cholangiocarcinoma: An update. J. Hepatol. 2021, 74, 1212–1224. [Google Scholar] [CrossRef] [PubMed]
- Yen, C.-C.; Yen, C.-J.; Shan, Y.-S.; Lin, Y.J.; Liu, I.-T.; Huang, H.-Y.; Yeh, M.M.; Chan, S.-H.; Tsai, H.-W. Comparing the clinicopathological characteristics of combined hepatocellular-cholangiocarcinoma with those of other primary liver cancers by use of the updated World Health Organization classification. Histopathology 2021, 79, 556–572. [Google Scholar] [CrossRef]
- Dageforde, L.A.; Vachharajani, N.; Tabrizian, P.; Agopian, V.; Halazun, K.; Maynard, E.; Croome, K.; Nagorney, D.; Hong, J.C.; Lee, D.; et al. Multi-Center Analysis of Liver Transplantation for Combined Hepatocellular Carcinoma-Cholangiocarcinoma Liver Tumors. J. Am. Coll. Surg. 2021, 232, 361–371. [Google Scholar] [CrossRef]
- Rizell, M.; Åberg, F.; Perman, M.; Ny, L.; Stén, L.; Hashimi, F.; Svanvik, J.; Lindnér, P. Checkpoint Inhibition Causing Complete Remission of Metastatic Combined Hepatocellular-Cholangiocarcinoma after Hepatic Resection. Case Rep. Oncol. 2020, 13, 478–484. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, C.T.; Caruso, S.; Maille, P.; Beaufrère, A.; Augustin, J.; Favre, L.; Pujals, A.; Boulagnon-Rombi, C.; Rhaiem, R.; Amaddeo, G.; et al. Immune Profiling of Combined Hepatocellular- Cholangiocarcinoma Reveals Distinct Subtypes and Activation of Gene Signatures Predictive of Response to Immunotherapy. Clin. Cancer Res. 2022, 28, 540–551. [Google Scholar] [CrossRef]
- Yagi, N.; Suzuki, T.; Mizuno, S.; Kojima, M.; Kudo, M.; Sugimoto, M.; Kobayashi, S.; Gotohda, N.; Ishii, G.; Nakatsura, T. Component with abundant immune-related cells in combined hepatocellular cholangiocarcinoma identified by cluster analysis. Cancer Sci. 2022, 113, 1564–1574. [Google Scholar] [CrossRef]
- Murugesan, K.; Sharaf, R.; Montesion, M.; Moore, J.A.; Pao, J.; Pavlick, D.C.; Frampton, G.M.; Upadhyay, V.A.; Alexander, B.M.; Miller, V.A.; et al. Genomic Profiling of Combined Hepatocellular Cholangiocarcinoma Reveals Genomics Similar to Either Hepatocellular Carcinoma or Cholangiocarcinoma. JCO Precis. Oncol. 2021, 5, 1285–1296. [Google Scholar] [CrossRef]
- Fowler, K.J.; Burgoyne, A.; Fraum, T.J.; Hosseini, M.; Ichikawa, S.; Kim, S.; Kitao, A.; Lee, J.M.; Paradis, V.; Taouli, B.; et al. Pathologic, Molecular, and Prognostic Radiologic Features of Hepatocellular Carcinoma. RadioGraphics 2021, 41, 1611–1631. [Google Scholar] [CrossRef]
- Fung, A.; Shambhogue, K.; Tafel, M.; Theise, N.D. Imaging of hepatocarcinogenesis with clinical and pathological correlation. Magn. Reson. Imaging Clin. N. Am. 2021, 29, 359–374. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Q.; Klein, C.; Caruso, S.; Maille, P.; Laleh, N.G.; Sommacale, D.; Laurent, A.; Amaddeo, G.; Gentien, D.; Rapinat, A.; et al. Artificial intelligence predicts immune and inflammatory gene signatures directly from hepatocellular carcinoma histology. J. Hepatol. 2022, 77, 116–127. [Google Scholar] [CrossRef] [PubMed]
| Hepatocellular Adenoma | Hepatocellular Carcinoma | |
|---|---|---|
| Etiology and Pathogenesis | ||
| Chronic liver disease | Usually absent | Usually present |
| Molecular changes | Four specific morpho-molecular | Large variety of mutations |
| subtypes, including the following: | affecting a number of signal | |
| transduction pathways; | |
| most frequent mutations | |
| Involve TERT promoter | |
| ||
| Tumor architecture | ||
| Thickness of cell plates | 1–2 cells | Variable |
| Pseudoglandular structures | Absent or few | Absent or present |
| Reticulin fibers | Preserved or focally disorganized | Decreased, disorganized |
| Invasive growth in stroma or vessels | Absent | Present |
| Cytologic features | ||
| Small cell size | Uncommon | Sometimes present |
| Nuclear hyperchromasia | Uncommon | Commonly present |
| Nuclear contour irregularities | Uncommon | Commonly present |
| Nuclear pleomorphism | Uncommon | Commonly present |
| Nuclear–cytoplasmic ratio | Usually normal | Often increased |
| Cytoplasmic basophilia | Usually absent | Commonly present |
| Mitotic figures | Absent or rare | Often present |
| Nonlesional hepatic parenchyma | ||
| Evidence of cirrhosis | Absent (rarely present in IHCA) | Present or absent |
| Positive immunohistochemical staining | ||
| Alpha-fetoprotein | Absent | Present or absent |
| Glypican-3 | Absent | Present or absent |
| Subtype | Characteristic Histologic Findings | Characteristic Molecular Findings |
|---|---|---|
| Steatohepatitic | Features simulating steatohepatitis (macrovesicular steatosis, inflammation, ballooned cells, Mallory–Denk bodies, and pericellular fibrosis) | IL6/JAK/STAT pathway activation |
| Clear cell | Glycogen accumulation in tumor cells | None to date |
| Macrotrabecular massive | Thick trabeculae (>6 cells thick) | TP53 mutations, FGF19 amplifications |
| Scirrhous | Diffuse fibrosis | TSC1/TSC2 mutations |
| Chromophobe | Light staining cytoplasm, mostly bland nuclei, occasional large atypical nuclei; cystic spaces with serum-like material | Alternative lengthening of telomeres |
| Fibrolamellar | Large polygonal cells with abundant eosinophilic cytoplasm, large nuclei and prominent nucleoli; pale bodies; lamellar fibrosis; immunopositivity for cytokeratin 7 and CD68 | DNAJB1–PRKACA gene fusion |
| Neutrophil-rich | Abundant intratumoral neutrophils | G-CSF production by neoplastic cells |
| Lymphocyte-rich | Abundant intratumoral lymphocytes | None to date |
| Sarcomatoid | Spindle cell morphology | None to date |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hytiroglou, P.; Bioulac-Sage, P.; Theise, N.D.; Sempoux, C. Etiology, Pathogenesis, Diagnosis, and Practical Implications of Hepatocellular Neoplasms. Cancers 2022, 14, 3670. https://doi.org/10.3390/cancers14153670
Hytiroglou P, Bioulac-Sage P, Theise ND, Sempoux C. Etiology, Pathogenesis, Diagnosis, and Practical Implications of Hepatocellular Neoplasms. Cancers. 2022; 14(15):3670. https://doi.org/10.3390/cancers14153670
Chicago/Turabian StyleHytiroglou, Prodromos, Paulette Bioulac-Sage, Neil D. Theise, and Christine Sempoux. 2022. "Etiology, Pathogenesis, Diagnosis, and Practical Implications of Hepatocellular Neoplasms" Cancers 14, no. 15: 3670. https://doi.org/10.3390/cancers14153670






