Accuracy of the Provisional Prosthesis Scanning Techniqueversus a Conventional Impression Technique on Completely Edentulous Arches
Abstract
1. Introduction
2. Materials and Methods
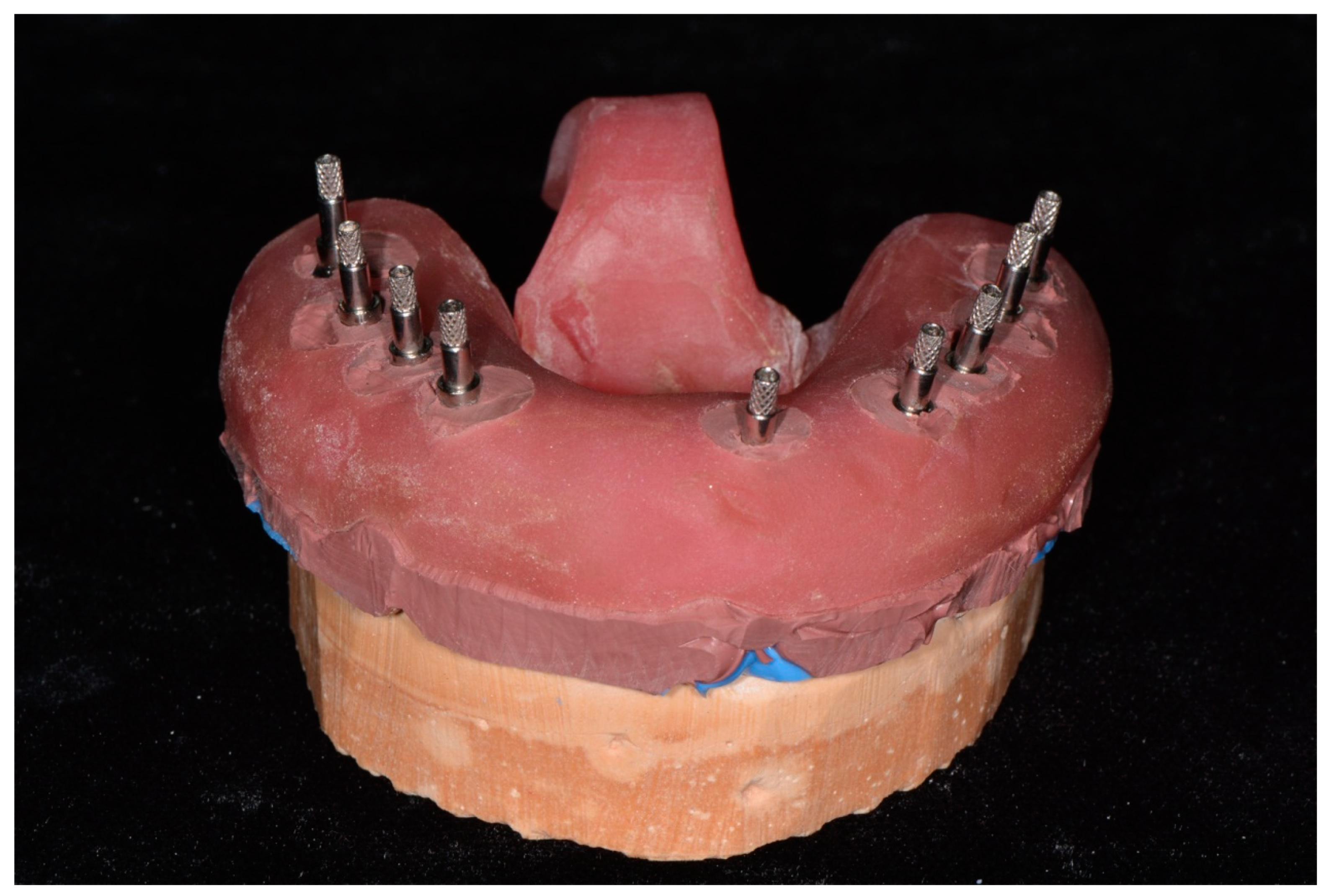
2.1. Conventional Impression Group
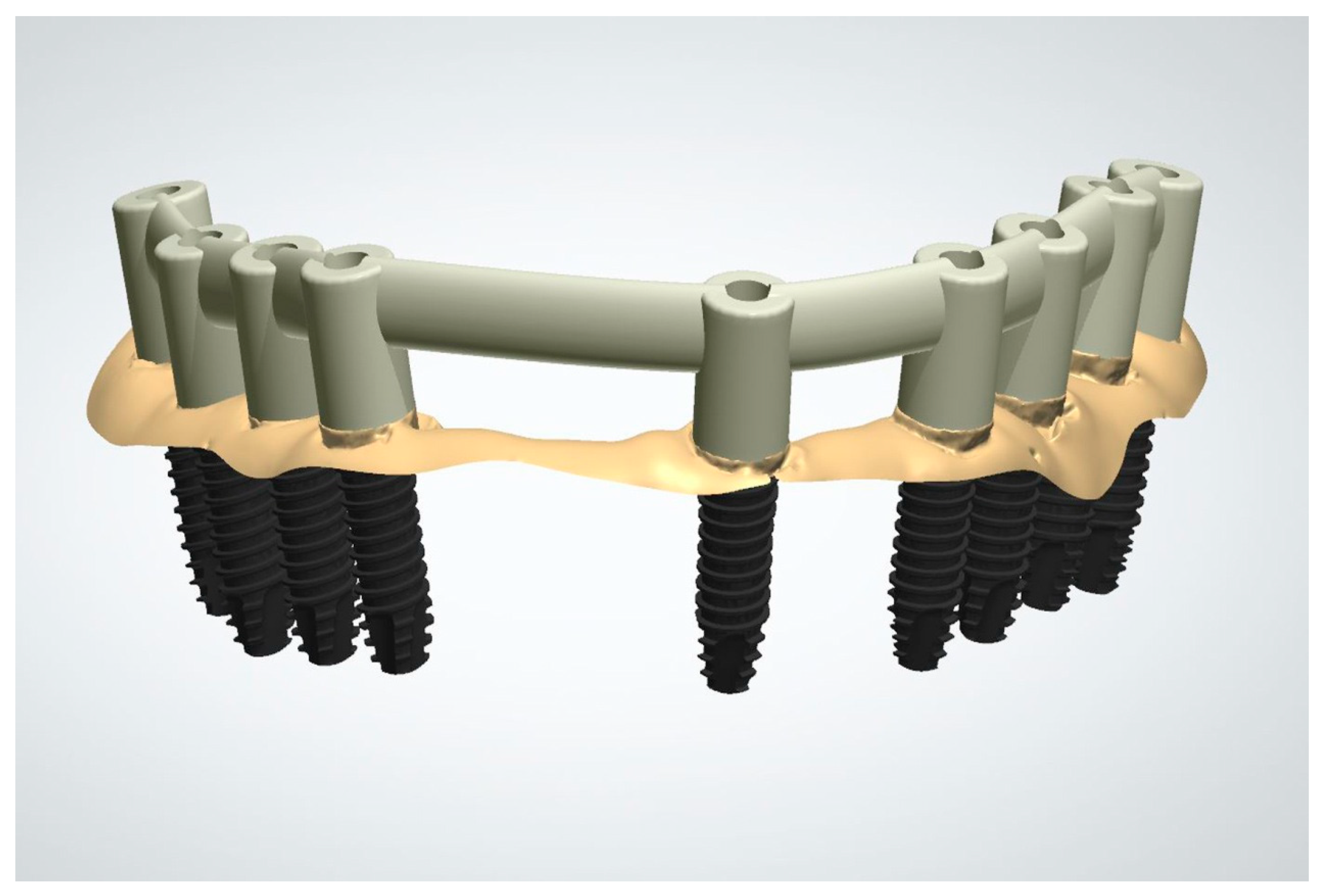
2.2. Provisional Prosthesis Scanning Group
2.3. Examination
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Jemt, T.; Hjalmarsson, L. In vitro measurements of precision of fit of implant-supported frameworks. A comparison between “virtual” and “physical” assessments of fit using two different techniques of measurements. Clin. Implant. Dent. Relat. Res. 2011, 14, e175–e182. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Lal, K. Computer-assisted design/computer-assisted manufacturing zirconia implant fixed complete prostheses: Clinical results and technical complications up to 4 years of function. Clin. Oral Implant. Res. 2012, 24, 659–665. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Chen, C.-J.; Chuang, S.-K.; Weber, H.-P.; Gallucci, G.O. A systematic review of biologic and technical complications with fixed implant rehabilitations for edentulous patients. Int. J. Oral Maxillofac. Implant. 2012, 27, 134–139. [Google Scholar]
- Papaspyridakos, P.; Gallucci, G.O.; Chen, C.J.; Hanssen, S.; Naert, I.; Vandenberghe, B. Digital versus conventional implant impressions for edentulous patients: Accuracy outcomes. Clin. Oral Implant. Res. 2016, 27, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Di Fiore, A.; Monaco, C.; Brunello, G.; Granata, S.; Stellini, E.; Yilmaz, B. Automatic digital design of the occlusal anatomy of monolithic zirconia crowns compared to dental technicians’ DigitalWaxing: A controlled clinical trial. J. Prosthodont. 2021, 30, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, S. The fit of Procera titanium crowns: An in vitro and clinical study. Acta Odontol. Scand. 1993, 51, 129–134. [Google Scholar] [CrossRef]
- Odén, A.; Andersson, M.; Krystek-Ondracek, I.; Magnusson, D. Five-year clinical evaluation of Procera AllCeram crowns. J. Prosthet. Dent. 1998, 80, 450–456. [Google Scholar] [CrossRef]
- Heckmann, S.M.; Karl, M.; Wichmann, M.G.; Winter, W.; Graef, F.; Taylor, T.D. Cement fixation and screw retention: Parameters of passive fit. An in vitro study of three-unit implant-supported fixed partial dentures. Clin. Oral Implant. Res. 2004, 15, 466–473. [Google Scholar] [CrossRef]
- Zhang, R.; Ding, Q.; Sun, Y.; Zhang, L.; Xie, Q. Assessment of CAD-CAM zirconia crowns designed with 2 different methods: A self-controlled clinical trial. J. Prosthet. Dent. 2018, 120, 686–692. [Google Scholar] [CrossRef]
- Di Fiore, A.; Meneghello, R.; Graiff, L.; Savio, G.; Vigolo, P.; Monaco, C.; Stellini, E. Full arch digital scanning systems performances for implant-supported fixed dental prostheses: A comparative study of 8 intraoral scanners. J. Prosthodont. Res. 2019, 63, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Bilmenoglu, C.; Cilingir, A.; Geckili, O.; Bilhan, H.; Bilgin, T. In vitro comparison of trueness of 10 intraoral scanners for implant-supported complete-arch fixed dental prostheses. J. Prosthet. Dent. 2020, 124, 755–760. [Google Scholar] [CrossRef]
- Mangano, F.G.; Admakin, O.; Bonacina, M.; Lerner, H.; Rutkunas, V.; Mangano, C. Trueness of 12 intraoral scanners in the full-arch implant impression: A comparative in vitro study. BMC Oral Health 2020, 20, 1–21. [Google Scholar] [CrossRef]
- Besimo, C.; Jeger, C.; Guggenheim, R. Marginal adaptation of titanium frameworks produced by CAD/CAM techniques. Int. J. Prosthodont. 1998, 10, 154–160. [Google Scholar]
- May, K.B.; Russell, M.M.; Razzoog, M.E.; Lang, B.R. Precision of fit: The ProceraAllCeram crown. J. Prosthet. Dent. 1998, 80, 394–404. [Google Scholar] [CrossRef]
- De Francesco, M.; Stellini, E.; Granata, S.; Mazzoleni, S.; Ludovichetti, F.S.; Monaco, C.; Di Fiore, A. Assessment of fit on ten screw-retained frameworks realized through digital full-arch implant impression. Appl. Sci. 2021, 11, 5617. [Google Scholar] [CrossRef]
- Abduo, J.; Bennani, V.; Waddell, N.; Lyons, K.; Swain, M. Assessing the fit of implant fixed prostheses: A critical review. Int. J. Oral Maxillofac. Implant. 2010, 25, 506–515. [Google Scholar]
- Kan, J.Y.; Rungcharassaeng, K.; Bohsali, K.; Goodacre, C.J.; Lang, B.R. Clinical methods for evaluating implant framework fit. J. Prosthet. Dent. 1999, 81, 7–13. [Google Scholar] [CrossRef]
- Di Fiore, A.; Meneghello, R.; Savio, G.; Sivolella, S.; Katsoulis, J.; Stellini, E. In vitro implant impression accuracy using a new photopolymerizing sdr splinting material. Clin. Implant. Dent. Relat. Res. 2015, 17, e721–e729. [Google Scholar] [CrossRef] [PubMed]
- Jemt, T.; Book, K. Prosthesis misfit and marginal bone loss in edentulous implant patients. Int. J. Oral Maxillofac. Implant. 1996, 11, 142–150. [Google Scholar]
- Eckert, S.E.; Meraw, S.J.; Cal, E.; Ow, R.K. Analysis of incidence and associated factors with fractured implants: A retrospective study. Int. J. Oral Maxillofac. Implant. 2000, 15, 155–163. [Google Scholar]
- Abduo, J.; Judge, R.B. Implications of implant framework misfit: A systematic review of biomechanical sequelae. Int. J. Oral Maxillofac. Implant. 2014, 29, 608–621. [Google Scholar] [CrossRef] [PubMed]
- Alshawaf, B.; Kudara, Y.; Weber, H.P. Management of technical complications during full-mouth implant rehabilitation with hybrid prostheses over a 7-year period. Compend. Contin. Educ. Dent. 2018, 39, 1–4. [Google Scholar]
- Box, V.H.; Sukotjo, C.; Knoernschild, K.L.; Campbell, S.D.; Afshari, F.S. Patient-Reported and Clinical Outcomes of Implant-Supported Fixed Complete Dental Prostheses: A Comparison of Metal-Acrylic, Milled Zirconia, and Retrievable Crown Prostheses. J. Oral Implant. 2018, 44, 51–61. [Google Scholar] [CrossRef]
- Gonzalez, J.; Triplett, R.G. Complications and clinical considerations of the implant-retained zirconia complete-arch prosthesis with various opposing dentitions. Int. J. Oral Maxillofac. Implant. 2017, 32, 864–869. [Google Scholar] [CrossRef]
- Albader, B.; Alhelal, A.; Proussaefs, P.; Garbacea, A.; Kattadiyil, M.; Lozada, J. Digitally Milled Metal Framework for Fixed Complete Denture with Metal Occlusal Surfaces: A Design Concept. Int. J. Periodontics Restor. Dent. 2017, 37, 180–188. [Google Scholar] [CrossRef]
- Jemt, T. Failures and complications in 391 consecutively inserted fixed prostheses supported by Branemark Implants in edentulous jaws: A study of treatment from the time of prosthesis placement to the first annual checkup. Int. J. Oral Maxillofac. Implant. 1991, 6, 89–102. [Google Scholar]
- Malo, P.; Nobre, M.; Guedes, C.; Almeida, R. Outcomes of immediate function implant prosthetic restorations with mechanical complications: A retrospective clinical study with 5 years of follow-up. Eur. J. Prosthodont. Restor. Dent. 2017, 25, 26–34. [Google Scholar]
- Yilmaz, B.; Gilbert, A.B.; Seidt, J.D.; McGlumphy, E.A.; Clelland, N.L. Displacement of implant abutments following initial and repeated torqueing. Int. J. Oral Maxillofac. Implant. 2015, 30, 1011–1018. [Google Scholar] [CrossRef] [PubMed]
- Balshi, T.J. An analysis and management of fractured implants: A clinical report. Int. J. Oral Maxillofac. Implant. 1996, 11, 666. [Google Scholar]
- Amin, S.; Weber, H.P.; Finkelman, M.; El Rafie, K.; Kudara, Y.; Papaspyridakos, P. Digital vs. conventional full-arch implant impressions: A comparative study. Clin. Oral Implant. Res. 2017, 28, 1360–1367. [Google Scholar] [CrossRef] [PubMed]
- Ahlholm, P.; Sipilä, K.; Vallittu, P.; Jakonen, M.; Kotiranta, U. Digital Versus Conventional Impressions in Fixed Prosthodontics: A Review. J. Prosthodont. 2018, 27, 35–41. [Google Scholar] [CrossRef]
- Abdel-Azim, T.; Elathamna, E.; Lin, W.; Zandinejad, A.; Morton, D. The Influence of Digital Fabrication Options on the Accuracy of Dental Implant–Based Single Units and Complete-Arch Frameworks. Int. J. Oral Maxillofac. Implant. 2014, 29, 1281–1288. [Google Scholar] [CrossRef]
- Albdour, E.A.; Shaheen, E.; Vranckx, M.; Mangano, F.G.; Politis, C.; Jacobs, R. A novel in vivo method to evaluate trueness of digital impressions. BMC Oral Health 2018, 18, 117. [Google Scholar] [CrossRef] [PubMed]
- Alikhasi, M.; Siadat, H.; Nasirpour, A.; Hasanzade, M. Three-Dimensional Accuracy of Digital Impression versus Conventional Method: Effect of Implant Angulation and Connection Type. Int. J. Dent. 2018, 2018, 1–9. [Google Scholar] [CrossRef]
- Zimmermann, M.; Koller, C.; Rumetsch, M.; Ender, A.; Mehl, A. Precision of guided scanning procedures for full-arch digital impressions in vivo. J. Orofac. Orthop. 2017, 78, 466–471. [Google Scholar] [CrossRef] [PubMed]
- Jokstad, A.; Shokati, B. New 3D technologies applied to assess the long-term clinical effects of misfit of the full jaw fixed prosthesis on dental Implant. Clin. Oral Implant. Res. 2014, 26, 1129–1134. [Google Scholar] [CrossRef]
- Tiossi, R.; Rodrigues, R.C.S.; Mattos, M.D.G.C.D.; Ribeiro, R.F. Comparative analysis of the fit of 3-unit implant-supported frameworks cast in nickel-chromium and cobalt-chromium alloys and commercially pure titanium after casting, laser welding, and simulated porcelain firings. Int. J. Prosthodont. 2008, 21, 234–244. [Google Scholar]
- Wettstein, F.; Sailer, I.; Roos, M.; Hämmerle, C.H.F. Clinical study of the internal gaps of zirconia and metal frameworks for fixed partial dentures. Eur. J. Oral Sci. 2008, 116, 272–279. [Google Scholar] [CrossRef] [PubMed]
- Papaspyridakos, P.; Chen, C.-J.; Gallucci, G.O.; Doukoudakis, A.; Weber, H.-P.; Chronopoulos, V. Accuracy of Implant Impressions for Partially and Completely Edentulous Patients: A Systematic Review. Int. J. Oral Maxillofac. Implant. 2014, 29, 836–845. [Google Scholar] [CrossRef]
- Joda, T.; Bragger, U. Time-efficiency analysis of the treatment with monolithic implant crowns in a digital workflow: A randomized controlled trial. Clin. Oral Implant. Res. 2016, 27, 1401–1406. [Google Scholar] [CrossRef]
- Joda, T.; Brägger, U. Patient-centered outcomes comparing digital and conventional implant impression procedures: A randomized crossover trial. Clin. Oral Implant. Res. 2016, 27, e185–e189. [Google Scholar] [CrossRef]
- Favero, R.; Volpato, A.; De Francesco, M.; Di Fiore, A.; Guazzo, R.; Favero, L. Accuracy of 3D digital modeling of dental arches. Dent. Press J. Orthod. 2019, 24, 038e1–037e7. [Google Scholar] [CrossRef]
- De Torres, E.M.; Barbosa, G.A.S.; Bernardes, S.R.; De Mattos, M.D.G.C.; Ribeiro, R.F. Correlation between vertical misfits and stresses transmitted to implants from metal frameworks. J. Biomech. 2011, 44, 1735–1739. [Google Scholar] [CrossRef] [PubMed]
- Al-Otaibi, H.N.; Akeel, R.F. The Effects of Two Torque Values on the Screw Preload of Implant-Supported Prostheses with Passive Fit or Misfit. Int. J. Oral Maxillofac. Implant. 2014, 29, 1058–1063. [Google Scholar] [CrossRef][Green Version]
- MassignanBerejuk, H.; Hideo Shimizu, R.; Aparecida de Mattias Sartori, I.; Valgas, L.; Tiossi, R. Vertical microgap and passivity of fit of three-unit implant-supported frameworks fabricated using different techniques. Int. J. Oral Maxillofac. Implant. 2014, 29, 152–159. [Google Scholar]
- Colpani, J.T.; Borba, M.; Della Bona, A. Evaluation of marginal and internal fit of ceramic crown copings. Dent. Mater. 2013, 29, 174–180. [Google Scholar] [CrossRef]
- Oka, Y.; Sasaki, J.-I.; Wakabayashi, K.; Nakano, Y.; Okamura, S.-Y.; Nakamura, T.; Imazato, S.; Yatani, H. Fabrication of a radiopaque fit-testing material to evaluate the three-dimensional accuracy of dental prostheses. Dent. Mater. 2016, 32, 921–928. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, O.; Kuepper, H.; Thompson, G.A.; Cachovan, G.; Hefti, A.F.; Guentsch, A. Effect of CNC-milling on the marginal and internal fit of dental ceramics: A pilot study. Dent. Mater. 2013, 29, 851–858. [Google Scholar] [CrossRef]
- Praça, L.; Pekam, F.C.; Rego, R.O.; Radermacher, K.; Wolfart, S.; Marotti, J. Accuracy of single crowns fabricated from ultrasound digital impressions. Dent. Mater. 2018, 34, e280–e288. [Google Scholar] [CrossRef] [PubMed]
- Zeller, S.; Guichet, D.; Kontogiorgos, E.; Nagy, W.W. Accuracy of three digital workflows for implant abutment and crown fabrication using a digital measuring technique. J. Prosthet. Dent. 2019, 121, 276–284. [Google Scholar] [CrossRef] [PubMed]
- Mai, H.N.; Lee, K.E.; Ha, J.-H.; Lee, D.-H. Effects of image and education on the precision of the measurement method for evaluating prosthesis misfit. J. Prosthet. Dent. 2018, 119, 600–605. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-M.; Hämmerle, C.H.; Benic, G.I. Digital technique for in vivo assessment of internal and marginal fit of fixed dental prostheses. J. Prosthet. Dent. 2017, 118, 452–454. [Google Scholar] [CrossRef] [PubMed]








| CIG Mean ± SM | PPSG Mean ± SM | Mann–Whitney Test | |
|---|---|---|---|
| Marginal fit discrepancy (µm) | 170 ± 50 | 1080 ± 40 | p < 0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, C.; Dusmukhamedov, S.; Fang, Y.-Q.; Jeong, S.-M.; Choi, B.-H. Accuracy of the Provisional Prosthesis Scanning Techniqueversus a Conventional Impression Technique on Completely Edentulous Arches. Appl. Sci. 2021, 11, 7182. https://doi.org/10.3390/app11167182
Lee C, Dusmukhamedov S, Fang Y-Q, Jeong S-M, Choi B-H. Accuracy of the Provisional Prosthesis Scanning Techniqueversus a Conventional Impression Technique on Completely Edentulous Arches. Applied Sciences. 2021; 11(16):7182. https://doi.org/10.3390/app11167182
Chicago/Turabian StyleLee, Chunui, Shavkat Dusmukhamedov, Yi-Qin Fang, Seung-Mi Jeong, and Byung-Ho Choi. 2021. "Accuracy of the Provisional Prosthesis Scanning Techniqueversus a Conventional Impression Technique on Completely Edentulous Arches" Applied Sciences 11, no. 16: 7182. https://doi.org/10.3390/app11167182
APA StyleLee, C., Dusmukhamedov, S., Fang, Y.-Q., Jeong, S.-M., & Choi, B.-H. (2021). Accuracy of the Provisional Prosthesis Scanning Techniqueversus a Conventional Impression Technique on Completely Edentulous Arches. Applied Sciences, 11(16), 7182. https://doi.org/10.3390/app11167182







