Impact of Desert Dust Events on the Cardiovascular Disease: A Systematic Review and Meta-Analysis
Abstract
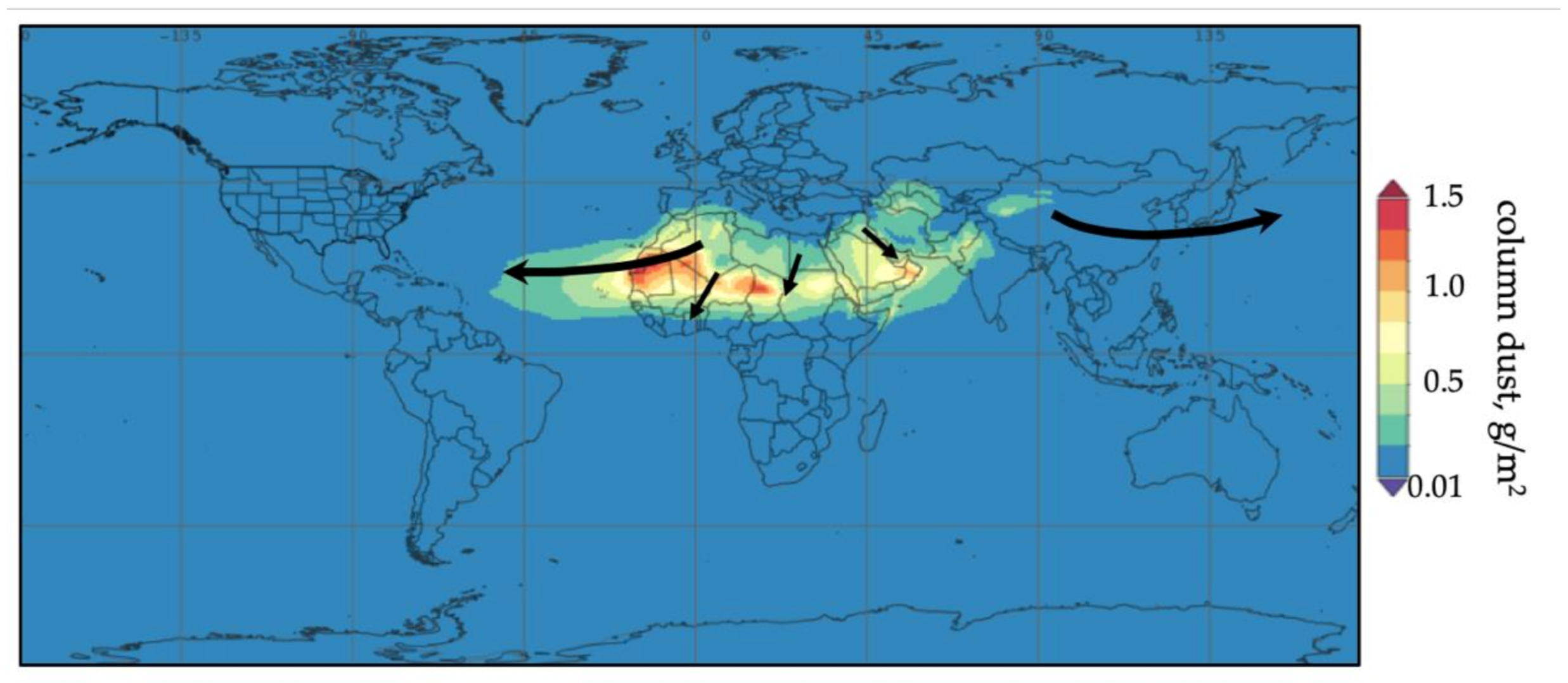
1. Introduction
2. Materials and Methods
2.1. Search Strategy and Selection of Studies
2.2. Definition of Exposure to Desert Dust and Study Selection Criteria
- Comparison of exposure to desert dust versus no such exposure.
- Description of the influence of desert dust (per unit increase) on the incidence of cardiovascular mortality, ACS, or heart failure.
- Identification of the exposure of desert dust in the breathable fraction of the particulate material PM10 [16].
- Human studies.
- Studies with a methodologically adequate design. In other words, studies controlling the main confounding factors (meteorological variables and pollutants in gaseous phase) and comprising time series or adopting a cross-case design [17].
- Studies in Spanish or English.
2.3. Objectives
2.4. Data Extraction and Evaluation of the Quality of the Studies
2.5. Statistical Analysis
3. Results
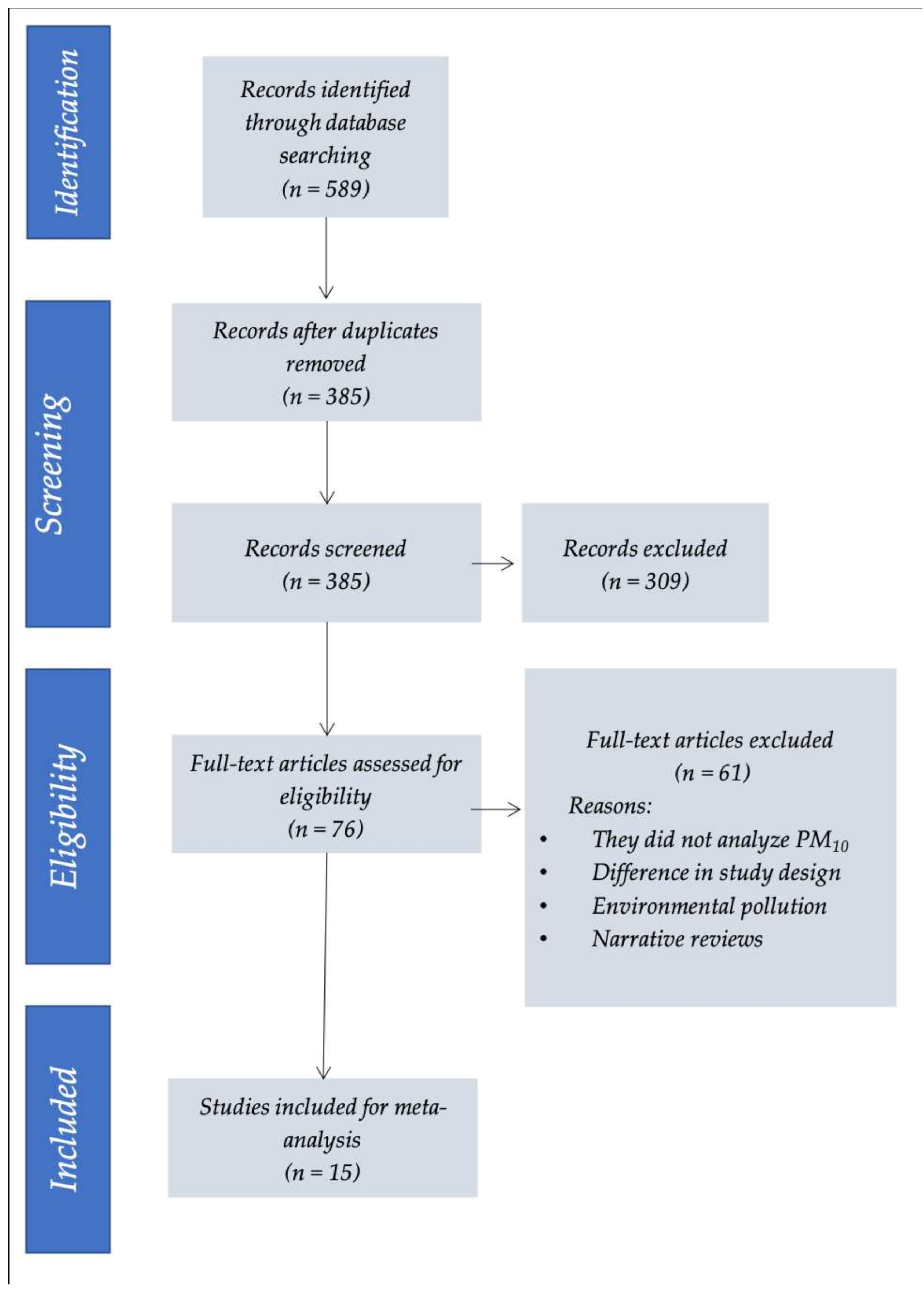
3.1. Systematic Selection of Studies
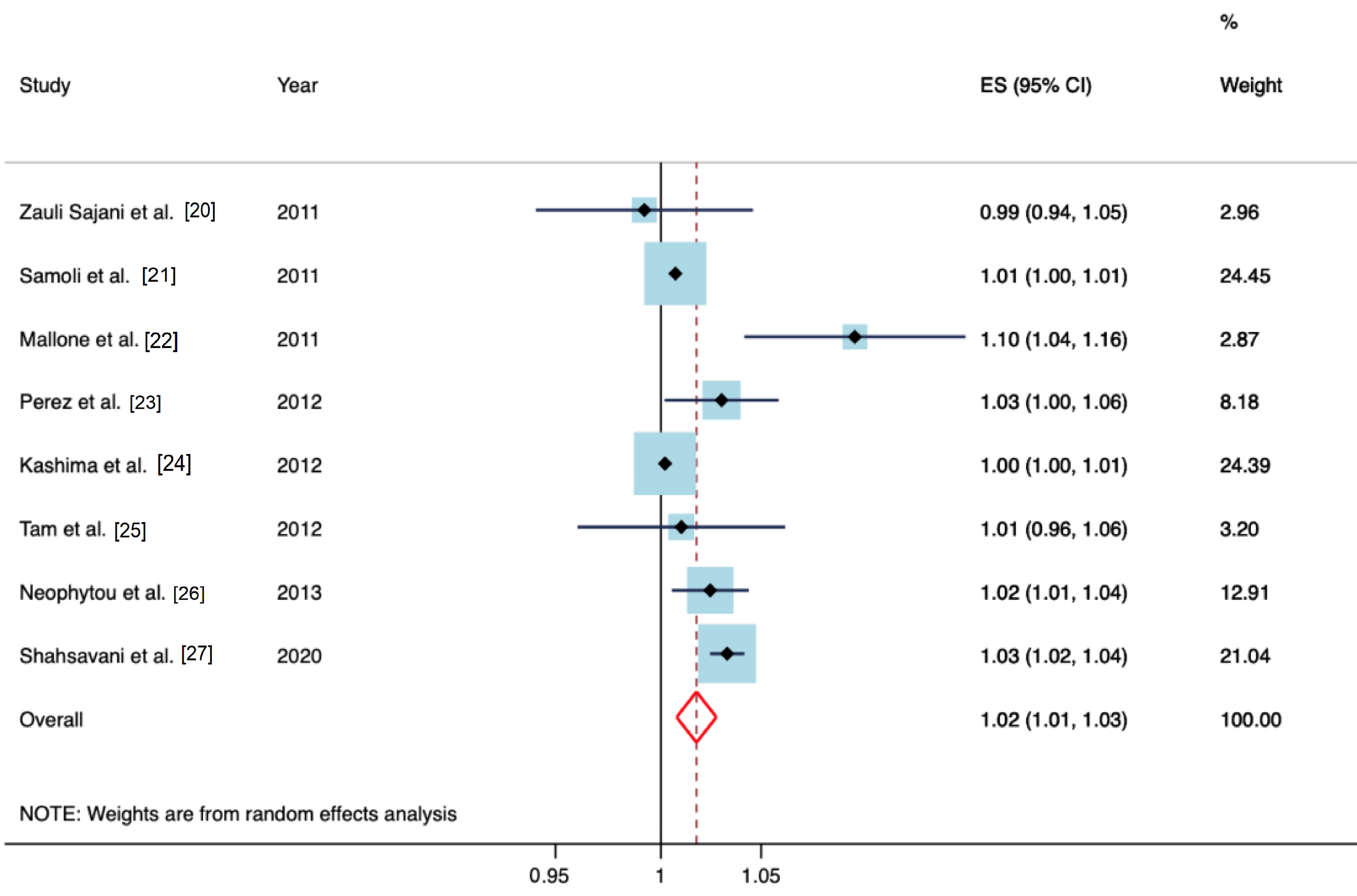
3.2. Cardiovascular Mortality
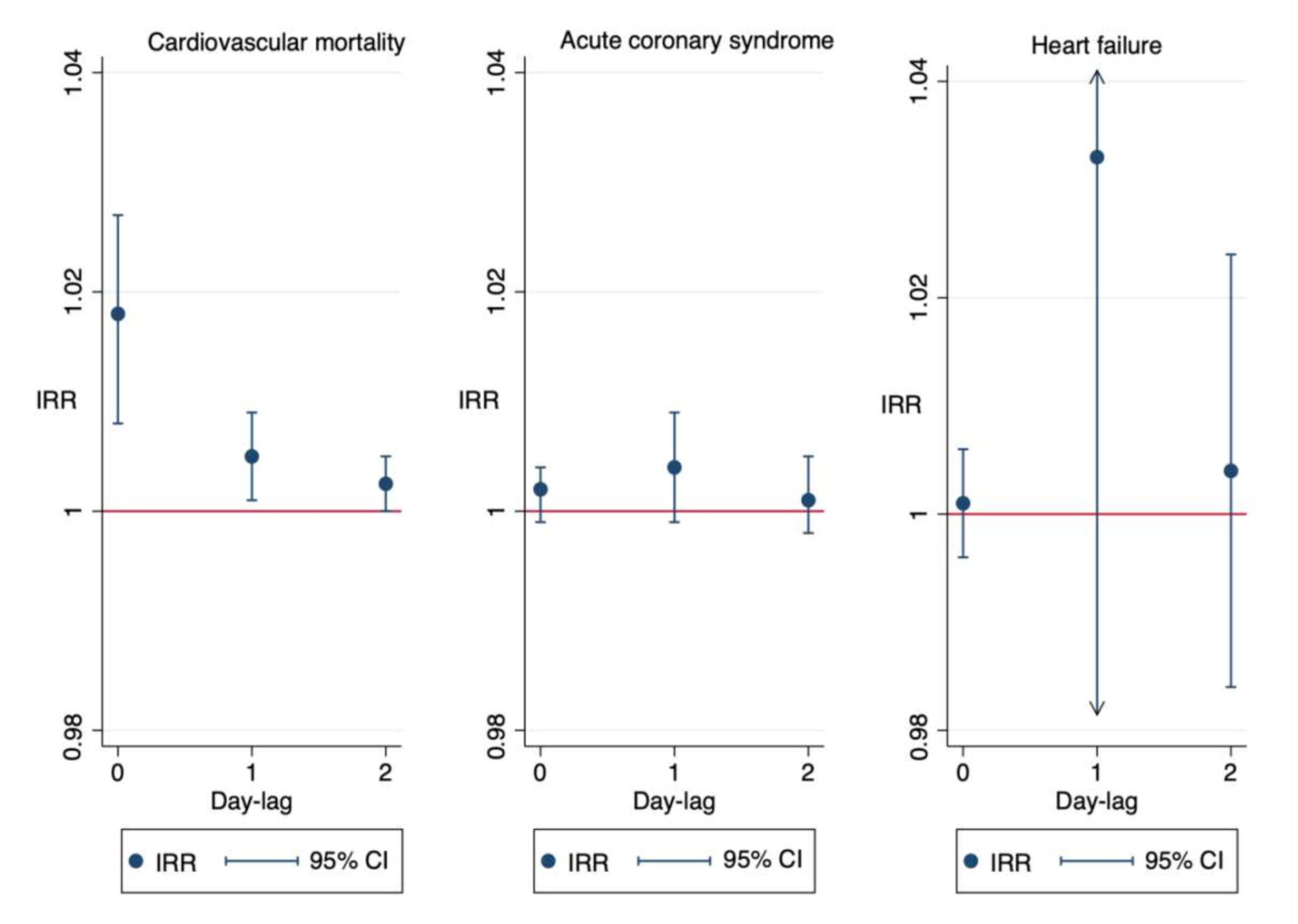
3.3. ACS
3.4. Heart Failure
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ambient Air Pollution: A Global Assessment of Exposure and Burden of Disease. 2016. Available online: https://www.who.int/phe/publications/air-pollution-global-assessment/en/ (accessed on 17 May 2020).
- Landrigan, P.J.; Fuller, R.; Acosta, N.J.R.; Adeyi, O.; Arnold, R.; Basu, N.; Baldé, A.B.; Bertollini, R.; Bose-O’Reilly, S.; Boufford, J.I.; et al. The Lancet Commission on pollution and health. Lancet 2018, 391, 462–512. [Google Scholar] [CrossRef]
- Kotsyfakis, M.; Zarogiannis, S.G.; Patelarou, E. The health impact of Saharan dust exposure. Int. J. Occup. Med. Environ. Health 2019, 32, 749–760. [Google Scholar] [CrossRef]
- Prospero, J.M.; Ginoux, P.; Torres, O.; Nicholson, S.E.; Gill, T.E. Environmental characterization of global sources of atmospheric soil dust identified with the Nimbus 7 Total Ozone Mapping Spectrometer (TOMS) absorbing aerosol product. Rev. Geophys. 2002, 40, 1–31. [Google Scholar] [CrossRef]
- Escudero, M.; Querol, X.; Pey, J.; Alastuey, A.; Pérez, N.; Ferreira, F.; Alonso, S.; Rodríguez, S.; Cuevas, E. A methodology for the quantification of the net African dust load in air quality monitoring networks. Atmos. Environ. 2007, 41, 5516–5524. [Google Scholar] [CrossRef]
- Rodrıguez, S.; Querol, X.; Alastuey, A.; Viana, M.M.; Alarcon, M.; Mantilla, E.; Ruiz, C.R. Comparative PM10–PM2.5 source contribution study at rural, urban and industrial sites during PM episodes in Eastern Spain. Sci. Total Environ. 2004, 328, 95–113. [Google Scholar] [CrossRef]
- Stafoggia, M.; Zauli-Sajani, S.; Pey, J.; Samoli, E.; Alessandrini, E.; Basagaña, X.; Cernigliaro, A.; Chiusolo, M.; Demaria, M.; Díaz, J.; et al. Desert dust outbreaks in southern Europe: Contribution to daily PM₁₀ concentrations and short-term associations with mortality and hospital admissions. Environ. Health Perspect. 2016, 124, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Querol, X.; Tobías, A.; Pérez, N.; Karanasiou, A.; Amato, F.; Stafoggia, M.; García-Pando, C.P.; Ginoux, P.; Forastiere, F.; Gumy, S.; et al. Monitoring the impact of desert dust outbreaks for air quality for health studies. Environ. Int. 2019, 130, 104867. [Google Scholar] [CrossRef]
- Marticorena, B.; Chatenet, B.; Rajot, J.L.; Bergametti, G.; Deroubaix, A.; Vincent, J.; Kouoi, A.; Schmechtig, C.; Coulibaly, M.; Diallo, A.; et al. Mineral dust over west and central Sahel: Seasonal patterns of dry and wet deposition fluxes from a pluriannual sampling (2006–2012). J. Geophys. Res. Atmos. 2017, 122, 1338–1364. [Google Scholar] [CrossRef]
- Karanasiou, A.; Moreno, N.; Moreno, T.; Viana, M.; de Leeuw, F.; Querol, X. Health effects from Sahara dust episodes in Europe: Literature review and research gaps. Environ. Int. 2012, 47, 107–114. [Google Scholar] [CrossRef] [PubMed]
- de Longueville, F.; Ozer, P.; Doumbia, S.; Henry, S. Desert dust impacts on human health: An alarming worldwide reality and a need for studies in West Africa. Int. J. Biometeorol. 2013, 57, 1–19. [Google Scholar] [CrossRef]
- Zhang, X.; Zhao, L.; Tong, D.; Wu, G.; Dan, W.; Teng, B. A systematic review of global desert dust and associated human health effects. Atmosphere 2016, 7, 158. [Google Scholar] [CrossRef]
- Winquist, A.; Klein, M.; Tolbert, P.; Sarnat, S.E. Power estimation using simulations for air pollution time-series studies. Environ. Health 2012, 11, 68. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Rodríguez, A.; Rodríguez, S.; Baez-Ferrer, N.; Avanzas, P.; Abreu-González, P.; Silva, J.; Morís, C.; Hernández-Vaquero, D. Impact of Saharan dust on the incidence of acute coronary syndrome. Rev. Esp. Cardiol. 2020, in press. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- Ambient (Outdoor) Air Pollution. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (accessed on 17 May 2020).
- Lu, Y.; Zeger, S.L. On the equivalence of case-crossover and time series methods in environmental epidemiology. Biostatistics 2007, 8, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomized studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Sajani, S.Z.; Miglio, R.; Bonasoni, P.; Cristofanelli, P.; Marinoni, A.; Sartini, C.; Goldoni, C.A.; De Girolamo, G.; Lauriola, P. Saharan dust and daily mortality in Emilia-Romagna (Italy). Occup. Environ. Med. 2011, 68, 446–451. [Google Scholar] [CrossRef]
- Samoli, E.; Kougea, E.; Kassomenos, P.; Analitis, A.; Katsouyanni, K. Does the presence of desert dust modify the effect of PM10 on mortality in Athens, Greece? Sci. Total Environ. 2011, 409, 2049–2054. [Google Scholar] [CrossRef]
- Mallone, S.; Stafoggia, M.; Faustini, A.; Gobbi, G.P.; Marconi, A.; Forastiere, F. Saharan dust and associations between particulate matter and daily mortality in Rome, Italy. Environ. Health Perspect. 2011, 119, 1409–1414. [Google Scholar] [CrossRef]
- Pérez, L.; Tobías, A.; Pey, J.; Pérez, N.; Alastuey, A.; Sunyer, J.; Querol, X. Effects of local and Saharan particles on cardiovascular disease mortality. Epidemiology 2012, 23, 768–769. [Google Scholar] [CrossRef]
- Kashima, S.; Yorifuji, T.; Tsuda, T.; Eboshida, A. Asian dust and daily all-cause or cause-specific mortality in western Japan. Occup. Environ. Med. 2012, 69, 908–915. [Google Scholar] [CrossRef]
- Tam, W.W.; Wong, T.W.; Wong, A.H. Effect of dust storm events on daily emergency admissions for cardiovascular diseases. Circ. J. 2012, 76, 655–660. [Google Scholar] [CrossRef] [PubMed]
- Neophytou, A.M.; Yiallouros, P.; Coull, B.A.; Kleanthous, S.; Pavlou, P.; Pashiardis, S.; Dockery, D.W.; Koutrakis, P.; Laden, F. Particulate matter concentrations during desert dust outbreaks and daily mortality in Nicosia, Cyprus. J. Expo. Sci. Environ. Epidemiol. 2013, 23, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Shahsavani, A.; Tobías, A.; Querol, X.; Stafoggia, M.; Abdolshahnejad, M.; Mayvaneh, F.; Guo, Y.; Hadei, M.; Hashemi, S.S.; Khosravi, A.; et al. Short-term effects of particulate matter during desert and non-desert dust days on mortality in Iran. Environ. Int. 2020, 134, 105299. [Google Scholar] [CrossRef] [PubMed]
- Vodonos, A.; Friger, M.; Katra, I.; Krasnov, H.; Zahger, D.; Schwartz, J.; Novack, V. Individual Effect Modifiers of Dust Exposure Effect on Cardiovascular Morbidity. PLoS ONE 2015, 10, e0137714. [Google Scholar] [CrossRef] [PubMed]
- Vaduganathan, M.; De Palma, G.; Manerba, A.; Goldoni, M.; Triggiani, M.; Apostoli, P.; Dei Cas, L.; Nodari, S. Risk of Cardiovascular Hospitalizations from Exposure to Coarse Particulate Matter (PM10) Below the European Union Safety Threshold. Am. J. Cardiol. 2016, 117, 1231–1235. [Google Scholar] [CrossRef]
- Al, B.; Bogan, M.; Zengin, S.; Sabak, M.; Kul, S.; Oktay, M.M.; Bayram, H.; Vuruskan, E. Effects of Dust Storms and Climatological Factors on Mortality and Morbidity of Cardiovascular Diseases Admitted to ED. Emerg. Med. Int. 2018, 2018, 3758506. [Google Scholar] [CrossRef]
- Zhang, Q.; Qi, W.; Yao, W.; Wang, M.; Chen, Y.; Zhou, Y. Ambient Particulate Matter (PM(2.5)/PM(10)) Exposure and Emergency Department Visits for Acute Myocardial Infarction in Chaoyang District, Beijing, China During 2014: A Case-Crossover Study. J. Epidemiol. 2016, 26, 538–545. [Google Scholar] [CrossRef]
- Matsukawa, R.; Michikawa, T.; Ueda, K.; Nitta, H.; Kawasaki, T.; Tashiro, H.; Mohri, M.; Yamamoto, Y. Desert dust is a risk factor for the incidence of acute myocardial infarction in Western Japan. Circ. Cardiovasc. Qual. Outcomes 2014, 7, 743–748. [Google Scholar] [CrossRef]
- Yang, C.Y.; Cheng, M.H.; Chen, C.C. Effects of Asian dust storm events on hospital admissions for congestive heart failure in Taipei, Taiwan. J. Toxicol. Environ. Health A 2009, 72, 324–328. [Google Scholar] [CrossRef]
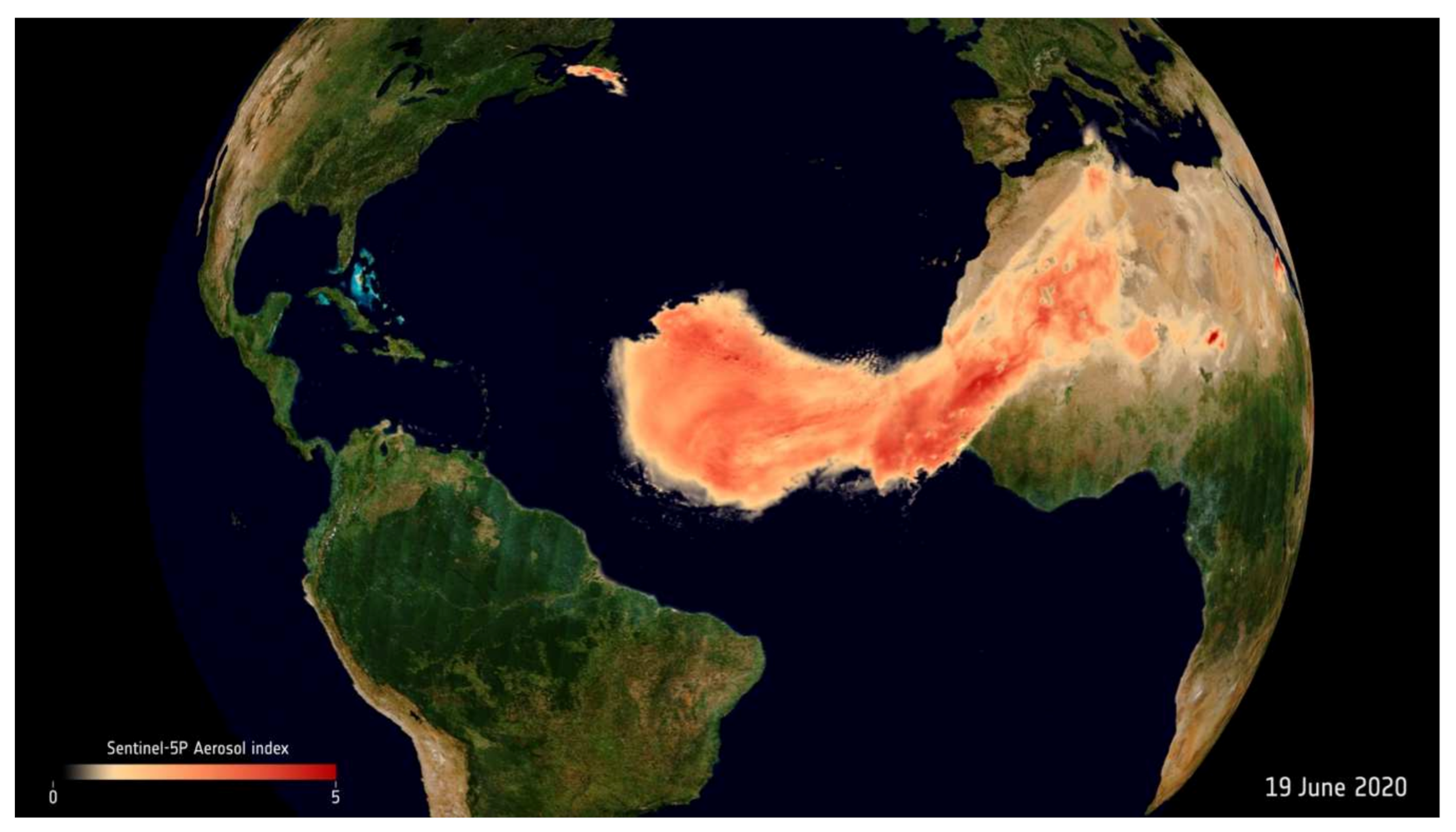
- NASA Earth Observatory, USA. Available online: https://earthobservatory.nasa.gov/images/146913/a-dust-plume-to-remember (accessed on 27 June 2020).
- Rius, J.B.; Ferreira-González, I.; Marsal, J.R.; Barrabés, J.A.; Ribera, A.; Lidón, R.M.; Domingo, E.; Martí, G.; García-Dorado, D. Short-term exposure to air pollutants increases the risk of ST elevation myocardial infarction and of infarct-related ventricular arrhythmias and mortality. Int. J. Cardiol. 2018, 250, 35–42. [Google Scholar]
- Milford, C.; Cuevas, E.; Marrero, C.L.; Bustos, J.J.; Gallo, V.; Rodríguez, S.; Romero-Campos, P.M.; Torres, C. Impacts of desert dust outbreaks on air quality in urban areas. Atmosphere 2020, 11, 23. [Google Scholar] [CrossRef]
- Pandolfi, M.; Tobías, A.; Alastuey, A.; Sunyer, J.; Schwartz, J.; Lorente, J.; Pey, J.; Querol, X. Effect of atmospheric mixing layer depth variations on urban air quality and daily mortality during Saharan dust outbreaks. Sci. Total Environ. 2014, 494–495, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Gao, H.; Wang, K.; Au, W.W.; Zhao, W.; Xia, Z. A Systematic Review and Meta-Analysis of Short-Term Ambient Ozone Exposure and COPD Hospitalizations. Int. J. Environ. Res. Public Health 2020, 17, 2130. [Google Scholar] [CrossRef] [PubMed]
- Navarese, E.P.; Buffon, A.; De Luca, G.; De Servi, S. Regarding “a closer look at meta-analyses of observational data”. J. Vasc. Surg. 2010, 52, 819. [Google Scholar] [CrossRef] [PubMed]
| Authors | Region | Country | Design | CE | PM10 DE | PM10 no-DE | R | Period | Risk of Bias |
|---|---|---|---|---|---|---|---|---|---|
| Zauli, 2011 [20] | Emilia Romagna | Italy | CC | CM | 38 | 42 | 0.9 | 2002–2006 | Low |
| Samoli, 2011 [21] | Athens | Greece | TS | CM | 47 | 39 | 1.2 | 2001–2006 | Low |
| Malone, 2011 [22] | Rome | Italy | CC | CM | 52 | 37 | 1.4 | 2001–2004 | Low |
| Perez, 2012 [23] | Barcelona | Spain | TS | CM | 39 | NS | 2003–2007 | Moderate | |
| Kashima, 2012 [24] | 5 cities | Japan | TS | CM/ACS | 184 | 22 | 8.3 | 2005–2010 | Low |
| Tam, 2012 [25] | Hong Kong | China | CC | CM/ACS/HF | 134 | 50 | 2.7 | 1998–2002 | Low |
| Neophytou, 2013 [26] | Nicosia | Cyprus | TS | CM | 116 | 53 | 2.2 | 2004–2007 | Low |
| Shahsavani, 2020 [27] | Ahvaz | Iran | CC | CM | 266 | 101 | 2.6 | 2015–2017 | Low |
| Shahsavani, 2020 [27] | Tehran | Iran | CC | CM | 192 | 82 | 2.3 | 2015–2017 | Low |
| Dominguez-Rodriguez, 2020 [14] | Tenerife | Spain | CC | ACS | 92 | 16 | 5.6 | 2014–2017 | Low |
| Vodonos, 2015 [28] | Béer-Sheva | Israel | CC | ACS | 2650 | 50 | 53 | 2001–2010 | Low |
| Vaduganathan, 2016 [29] | Brescia | Italy | TS | ACS/HF | NS | NS | 2004–2007 | Moderate | |
| Al, 2018 [30] | Gaziantep | Turkey | TS | ACS/HF | 74 | 72 | 1.0 | 2009–2014 | Low |
| Zhang, 2016 [31] | Beijing | China | CC | ACS | NS | NS | 2014–2014 | Moderate | |
| Matsukawa, 2014 [32] | Fukuoka | Japan | CC | ACS | 55 | 29 | 1.9 | 2003–2010 | Low |
| Yang, 2009 [33] | Taipei | Taiwan | CC | CI | 112 | 55 | 2.0 | 1996–2001 | Low |
| Objective | Incidence Rate Ratio | p-Value | I2 | Egger (p-Value) | Begg (p-Value) |
|---|---|---|---|---|---|
| Cardiovascular mortality | |||||
| Lag 0 | 1.018 (95%CI 1.008–1.027) | <0.001 | 49.54% | 0.14 | 0.71 |
| Lag 1 | 1.005 (95%CI 1.001–1.009) | 0.022 | 34.59% | 0.44 | 1.00 |
| Lag 2 | 1.003 (95%CI 1.000–1.005) | 0.040 | 3.34% | 0.52 | 0.46 |
| Lag 0–1 | 1.015 (95%CI 1.003–1.028) | 0.014 | 0.00% | 0.33 | 0.31 |
| Lag 0–5 | 1.023 (95%CI 0.999–1.047) | 0.053 | 0.00% | 0.88 | 0.73 |
| Acute coronary syndrome | |||||
| Lag 0 | 1.002 (95%CI 0.999–1.004) | 0.144 | 0.00% | 0.11 | 0.67 |
| Lag 1 | 1.004 (95%CI 0.999–1.009) | 0.071 | 13.39% | 0.13 | 0.22 |
| Lag 2 | 1.001 (95%CI 0.998–1.005) | 0.449 | 15.62% | 0.59 | 0.22 |
| Lag 3 | 0.986 (95%CI 0.949–1.028) | 0.507 | 6.24% | 0.14 | 0.60 |
| Lag 4 | 1.025 (95%CI 0.902–1.164) | 0.706 | 43.07% | 0.34 | 0.29 |
| Lag 0–1 | 1.003 (95%CI 1.001–1.006) | 0.006 | 0.00% | 0.46 | 0.73 |
| Heart failure | |||||
| Lag 0 | 1.001 (95%CI 0.996–1.006) | 0.670 | 0.00% | 0.94 | 0.74 |
| Lag 1 | 1.033 (95%CI 0.977–1.091) | 0.253 | 0.00% | 0.06 | 0.29 |
| Lag 2 | 1.004 (95%CI 0.984–1.024) | 0.698 | 0.00% | 0.71 | 0.30 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Domínguez-Rodríguez, A.; Báez-Ferrer, N.; Abreu-González, P.; Rodríguez, S.; Díaz, R.; Avanzas, P.; Hernández-Vaquero, D. Impact of Desert Dust Events on the Cardiovascular Disease: A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 727. https://doi.org/10.3390/jcm10040727
Domínguez-Rodríguez A, Báez-Ferrer N, Abreu-González P, Rodríguez S, Díaz R, Avanzas P, Hernández-Vaquero D. Impact of Desert Dust Events on the Cardiovascular Disease: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2021; 10(4):727. https://doi.org/10.3390/jcm10040727
Chicago/Turabian StyleDomínguez-Rodríguez, Alberto, Néstor Báez-Ferrer, Pedro Abreu-González, Sergio Rodríguez, Rocío Díaz, Pablo Avanzas, and Daniel Hernández-Vaquero. 2021. "Impact of Desert Dust Events on the Cardiovascular Disease: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 10, no. 4: 727. https://doi.org/10.3390/jcm10040727
APA StyleDomínguez-Rodríguez, A., Báez-Ferrer, N., Abreu-González, P., Rodríguez, S., Díaz, R., Avanzas, P., & Hernández-Vaquero, D. (2021). Impact of Desert Dust Events on the Cardiovascular Disease: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 10(4), 727. https://doi.org/10.3390/jcm10040727









