Examining Self-Weighing Behaviors and Associated Features and Treatment Outcomes in Patients with Binge-Eating Disorder and Obesity with and without Food Addiction
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Measures
2.4. Data Analysis
3. Results
3.1. Aim 1: Examine Changes in Weighing Variables by Food Addiction Status Over Time
3.2. Aim 2: To Examine the Association of Weighing Variables at Post-Treatment with Binge-Eating, Disordered Eating and Weight Outcomes by Food Addiction Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Battle, E.K.; Brownell, K.D. Confronting a rising tide of eating disorders and obesity: Treatment vs. prevention and policy. Addict. Behav. 1996, 21, 755–765. [Google Scholar] [CrossRef]
- Fletcher, P.C.; Kenny, P.J. Food addiction: A valid concept? Neuropsychopharmacology 2018, 43, 2506–2513. [Google Scholar] [CrossRef] [PubMed]
- Gordon, E.L.; Ariel-Donges, A.H.; Bauman, V.; Merlo, L.J. What Is the Evidence for “Food Addiction?” A Systematic Review. Nutrients 2018, 10, 477. [Google Scholar] [CrossRef] [PubMed]
- Gearhardt, A.N.; Davis, C.; Kuschner, R.; Brownell, K.D. The addiction potential of hyperpalatable foods. Curr. Drug Abus. Rev. 2011, 4, 140–145. [Google Scholar] [CrossRef] [PubMed]
- Gearhardt, A.N.; Corbin, W.R.; Brownell, K.D. Preliminary validation of the Yale Food Addiction Scale. Appetite 2009, 52, 430–436. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Boswell, R.G.; White, M.A. The association of “food addiction” with disordered eating and body mass index. Eat. Behav. 2014, 15, 427–433. [Google Scholar] [CrossRef]
- Pedram, P.; Wadden, D.; Amini, P.; Gulliver, W.; Randell, E.; Cahill, F.; Vasdev, S.; Goodridge, A.; Carter, J.C.; Zhai, G.; et al. Food addiction: Its prevalence and significant association with obesity in the general population. PLoS ONE 2013, 8, e74832. [Google Scholar] [CrossRef]
- Schulte, E.M.; Grilo, C.M.; Gearhardt, A.N. Shared and unique mechanisms underlying binge eating disorder and addictive disorders. Clin. Psychol. Rev. 2016, 44, 125–139. [Google Scholar] [CrossRef]
- Taetzsch, A.; Roberts, S.B.; Gilhooly, C.H.; Lichtenstein, A.H.; Krauss, A.J.; Bukhari, A.; Martin, E.; Hatch-McChesney, A.; Das, S.K. Food cravings: Associations with dietary intake and metabolic health. Appetite 2020, 152, 104711. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; White, M.A.; Masheb, R.M.; Morgan, P.T.; Crosby, R.D.; Grilo, C.M. An examination of the food addiction construct in obese patients with binge eating disorder. Int. J. Eat. Disord. 2012, 45, 657–663. [Google Scholar] [CrossRef]
- Frayn, M.; Sears, C.R.; von Ranson, K.M. A sad mood increases attention to unhealthy food images in women with food addiction. Appetite 2016, 100, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Cassin, S.E.; Sijercic, I.; Montemarano, V. Psychosocial interventions for food addiction: A systematic review. Curr. Addict. Rep. 2020, 7, 9–19. [Google Scholar] [CrossRef]
- Burmeister, J.M.; Hinman, N.; Koball, A.; Hoffmann, D.A.; Carels, R.A. Food addiction in adults seeking weight loss treatment. Implications for psychosocial health and weight loss. Appetite 2013, 60, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Grilo, C.M.; Masheb, R.M.; Wilson, G.T.; Gueorguieva, R.; White, M.A. Cognitive-behavioral therapy, behavioral weight loss, and sequential treatment for obese patients with binge-eating disorder: A randomized controlled trial. J. Consult. Clin. Psychol. 2011, 79, 675–685. [Google Scholar] [CrossRef] [PubMed]
- Fielding-Singh, P.; Patel, M.L.; King, A.C.; Gardner, C.D. Baseline Psychosocial and Demographic Factors Associated with Study Attrition and 12-Month Weight Gain in the DIETFITS Trial. Obesity 2019, 27, 1997–2004. [Google Scholar] [CrossRef]
- Lent, M.R.; Eichen, D.M.; Goldbacher, E.; Wadden, T.A.; Foster, G.D. Relationship of food addiction to weight loss and attrition during obesity treatment. Obesity 2014, 22, 52–55. [Google Scholar] [CrossRef]
- Chao, A.M.; Wadden, T.A.; Tronieri, J.S.; Pearl, R.L.; Alamuddin, N.; Bakizada, Z.M.; Pinkasavage, E.; Leonard, S.M.; Alfaris, N.; Berkowitz, R.I. Effects of addictive-like eating behaviors on weight loss with behavioral obesity treatment. J. Behav. Med. 2018. [Google Scholar] [CrossRef]
- Brockmann, A.N.; Eastman, A.; Ross, K.M. Frequency and consistency of self-weighing to promote weight-loss maintenance. Obesity 2020, 28, 1215–1218. [Google Scholar] [CrossRef]
- Butryn, M.L.; Phelan, S.; Hill, J.O.; Wing, R.R. Consistent self-monitoring of weight: A key component of successful weight loss maintenance. Obesity 2007, 15, 3091–3096. [Google Scholar] [CrossRef]
- LaRose, J.G.; Fava, J.L.; Steeves, E.A.; Hecht, J.; Wing, R.R.; Raynor, H.A. Daily self-weighing within a lifestyle intervention: Impact on disordered eating symptoms. Health Psychol. 2014, 33, 297–300. [Google Scholar] [CrossRef]
- Wing, R.R.; Tate, D.F.; Gorin, A.A.; Raynor, H.A.; Fava, J.L.; Machan, J. STOP regain: Are there negative effects of daily weighing? J. Consult. Clin. Psychol. 2007, 75, 652–656. [Google Scholar] [CrossRef] [PubMed]
- Jospe, M.R.; Brown, R.C.; Williams, S.M.; Roy, M.; Meredith-Jones, K.A.; Taylor, R.W. Self-monitoring has no adverse effect on disordered eating in adults seeking treatment for obesity. Obes. Sci. Pr. 2018, 4, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, D.M.; Tate, D.F.; Bennett, G.G.; Ennett, S.; Samuel-Hodge, C.; Ward, D.S. Daily self-weighing and adverse psychological outcomes: A randomized controlled trial. Am. J. Prev. Med. 2014, 46, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Grilo, C.M.; White, M.A.; Masheb, R.M.; Ivezaj, V.; Morgan, P.T.; Gueorguieva, R. Randomized controlled trial testing the effectiveness of adaptive “SMART” stepped-care treatment for adults with binge-eating disorder comorbid with obesity. Am. Psychol. 2020, 75, 204–218. [Google Scholar] [CrossRef]
- Grilo, C.M.; White, M.A.; Ivezaj, V.; Gueorguieva, R. Randomized controlled trial of behavioral weight loss and stepped care for binge-eating disorder: 12-month follow-up. Obesity 2020, in press. [Google Scholar] [CrossRef]
- APA. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- First, M.B.; Spitzer, R.L.; Gibbon, M.; Williams, J.B.W. Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Edition (SCID-I/P, Ver 2.0); United States Department of Veterans Affairs: New York, NY, USA, 1996.
- Fairburn, C.G.; Cooper, Z. The Eating Disorder Examination, 12th ed.; Fairburn, C.G., Wilson, G.T., Eds.; Guilford Press: New York, NY, USA, 1993. [Google Scholar]
- Fairburn, C.G.; Cooper, Z.; O’Connor, M. Eating Disorder Examination (16.0D) in Cognitive Behavior Therapy and Eating Disorders; Fairburn, C.G., Ed.; Guilford Press: New York, NY, USA, 2008. [Google Scholar]
- Grilo, C.M.; Masheb, R.M.; Wilson, G.T. A comparison of different methods for assessing the features of eating disorders in patients with binge eating disorder. J. Consult. Clin. Psychol. 2001, 69, 317–322. [Google Scholar] [CrossRef]
- Grilo, C.M.; Masheb, R.M.; Lozano-Blanco, C.; Barry, D.T. Reliability of the Eating Disorder Examination in patients with binge eating disorder. Int. J. Eat. Disord. 2004, 35, 80–85. [Google Scholar] [CrossRef]
- Berg, K.C.; Peterson, C.B.; Frazier, P.; Crow, S.J. Psychometric evaluation of the eating disorder examination and eating disorder examination-questionnaire: A systematic review of the literature. Int. J. Eat. Disord. 2012, 45, 428–438. [Google Scholar] [CrossRef]
- Ivezaj, V.; White, M.A.; Grilo, C.M. Examining binge-eating disorder and food addiction in adults with overweight and obesity. Obesity (Silver Spring) 2016, 24, 2064–2069. [Google Scholar] [CrossRef]
- Pacanowski, C.R.; Pisetsky, E.M.; Berg, K.C.; Crosby, R.D.; Crow, S.J.; Linde, J.A.; Mitchell, J.E.; Engel, S.G.; Klein, M.H.; Smith, T.L.; et al. Self-weighing behavior in individuals with eating disorders. Int. J. Eat. Disord. 2016, 49, 817–821. [Google Scholar] [CrossRef]
- Rohde, P.; Arigo, D.; Shaw, H.; Stice, E. Relation of self-weighing to future weight gain and onset of disordered eating symptoms. J. Consult. Clin. Psychol. 2018, 86, 677–687. [Google Scholar] [CrossRef]
- Friend, S.; Bauer, K.W.; Madden, T.C.; Neumark-Sztainer, D. Self-weighing among adolescents: Associations with body mass index, body satisfaction, weight control behaviors, and binge eating. J. Acad. Nutr. Diet. 2012, 112, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Neumark-Sztainer, D.; van den Berg, P.; Hannan, P.J.; Story, M. Self-weighing in adolescents: Helpful or harmful? Longitudinal associations with body weight changes and disordered eating. J. Adolesc. Health 2006, 39, 811–818. [Google Scholar] [CrossRef] [PubMed]
- Pacanowski, C.R.; Crosby, R.D.; Grilo, C.M. Self-weighing in individuals with binge-eating disorder. Eat. Disord. 2019, 1, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Grilo, C.M. Psychological and Behavioral Treatments for Binge-Eating Disorder. J. Clin. Psychiatry 2017, 78 (Suppl. 1), 20–24. [Google Scholar] [CrossRef] [PubMed]
- Wilson, G.T.; Grilo, C.M.; Vitousek, K.M. Psychological treatment of eating disorders. Am. Psychol. 2007, 62, 199–216. [Google Scholar] [CrossRef] [PubMed]
- Linardon, J.; Wade, T.D.; de la Piedad Garcia, X.; Brennan, L. The efficacy of cognitive-behavioral therapy for eating disorders: A systematic review and meta-analysis. J. Consult. Clin. Psychol. 2017, 85, 1080–1094. [Google Scholar] [CrossRef] [PubMed]


| Study Variables | EDE Item | Frequency/Rating |
|---|---|---|
| Weighing | “Over the past 4 weeks how often have you weighed yourself?” | Number of times weighed in past 28 days |
| Sensitivity | “Over the past 4 weeks what amount of weight gain, over a period of 1 week, would have definitely upset you?” | 7-point Likert scale based on the number of pounds or kilograms that would generate a marked negative reaction (0 = 7 lbs or 3.5 kg or more to 6 = 1 lb or 0.5 kg). |
| Reaction | “Over the past 4 weeks how would you have felt if you had been asked to weigh yourself once each week for the subsequent 4 weeks … just once a week; no more often and no less often?” | 7-point Likert score ranging from 0 = no reaction to 6 = marked reaction (pronounced reaction which would affect other aspects of the subject’s life). |
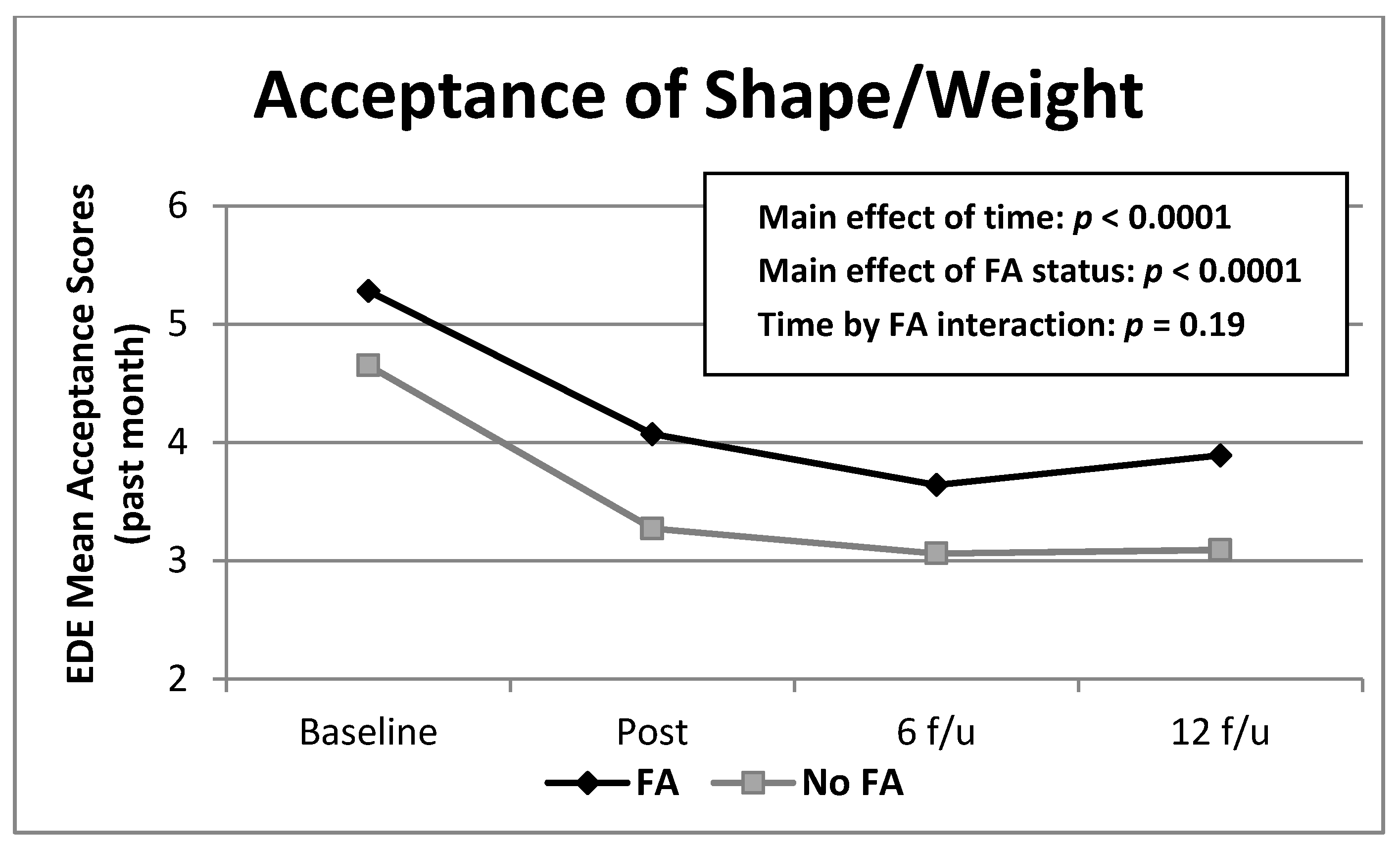
| Acceptance | “Over the past 4 weeks, to what extent have you been able to accept your shape and weight—see them as simply being the way you are?” | 7-point Likert scale ranging from 0 = complete acceptance to 6 = no acceptance. |
| Pre-Treatment | Post-Treatment | 6-Month Follow-Up | 12-Month Follow-Up | ||||||
|---|---|---|---|---|---|---|---|---|---|
| FA (n = 114) | No FA (n = 72) | FA (n = 100) | No FA (n = 66) | FA (n = 114) | No FA (n = 72) | FA (n = 91) | No FA (n = 63) | Sig. | |
| Weighing | 10.63 (15.00) | 8.01 (11.10) | 9.73 (11.98) | 10.18 (17.01) | 10.93 (19.32) | 8.57 (10.35) | 8.66 (10.42) | 9.09 (11.63) | ns |
| Sensitivity | 4.31 (1.73) | 4.40 (1.63) | 4.17 (1.69) | 3.92 (1.45) | 3.45 (1.80) | 3.17 (1.81) | 3.68 (1.89) | 3.19 (1.62) | 0.0001 |
| Reaction | 1.46 (1.88) | 1.01 (1.64) | 1.07 (1.77) | 0.61 (1.39) | 0.59 (1.41) | 0.59 (1.41) | 1.14 (1.81) | 0.72 (1.59) | 0.01 |
| Acceptance | 5.28 (1.20) | 4.65 (1.20) | 4.07 (1.73) | 3.27 (1.64) | 3.64 (1.87) | 3.06 (1.74) | 3.89 (1.85) | 3.09 (1.67) | 0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wiedemann, A.A.; Ivezaj, V.; Gueorguieva, R.; Potenza, M.N.; Grilo, C.M. Examining Self-Weighing Behaviors and Associated Features and Treatment Outcomes in Patients with Binge-Eating Disorder and Obesity with and without Food Addiction. Nutrients 2021, 13, 29. https://doi.org/10.3390/nu13010029
Wiedemann AA, Ivezaj V, Gueorguieva R, Potenza MN, Grilo CM. Examining Self-Weighing Behaviors and Associated Features and Treatment Outcomes in Patients with Binge-Eating Disorder and Obesity with and without Food Addiction. Nutrients. 2021; 13(1):29. https://doi.org/10.3390/nu13010029
Chicago/Turabian StyleWiedemann, Ashley A., Valentina Ivezaj, Ralitza Gueorguieva, Marc N. Potenza, and Carlos M. Grilo. 2021. "Examining Self-Weighing Behaviors and Associated Features and Treatment Outcomes in Patients with Binge-Eating Disorder and Obesity with and without Food Addiction" Nutrients 13, no. 1: 29. https://doi.org/10.3390/nu13010029
APA StyleWiedemann, A. A., Ivezaj, V., Gueorguieva, R., Potenza, M. N., & Grilo, C. M. (2021). Examining Self-Weighing Behaviors and Associated Features and Treatment Outcomes in Patients with Binge-Eating Disorder and Obesity with and without Food Addiction. Nutrients, 13(1), 29. https://doi.org/10.3390/nu13010029






