Sustainable Business Models in Hybrids: A Conceptual Framework for Community Pharmacies’ Business Owners
Abstract
1. Introduction
2. Community Pharmacies’ Institutional Context
- Increase in competition on prices of over-the-counter (OTC) drugs;
- Regulations facilitating pharmacy chains and introducing new competitors such as grocery retailers in the OTC drugs market;
- Increase in competitiveness on complementary medicine;
- A shift from the dispensary role of community pharmacists (left to hospital pharmacies) to the management of professional services, introduced by countries’ health policies and related cost-saving measures;
- The advent of information technology that reshaped competitiveness (e-pharmacy; electronic prescribing matched with marketing tools to tailor offerings based on customers’ preferences and reduce the amount of time dedicated to dispensing activities);
- Diversification of big retailers and supermarkets into non-conventional fields.
- The expansion of community pharmacies’ services as an integral part of primary care;
- Improved access to innovative medicines by increasing their supply via community pharmacies;
- Incentivization of the uptake of generic drugs through community pharmacies;
- Involvement of community pharmacies in national health policies to improve vaccination coverage and risk minimization plans for other medicinal therapies.
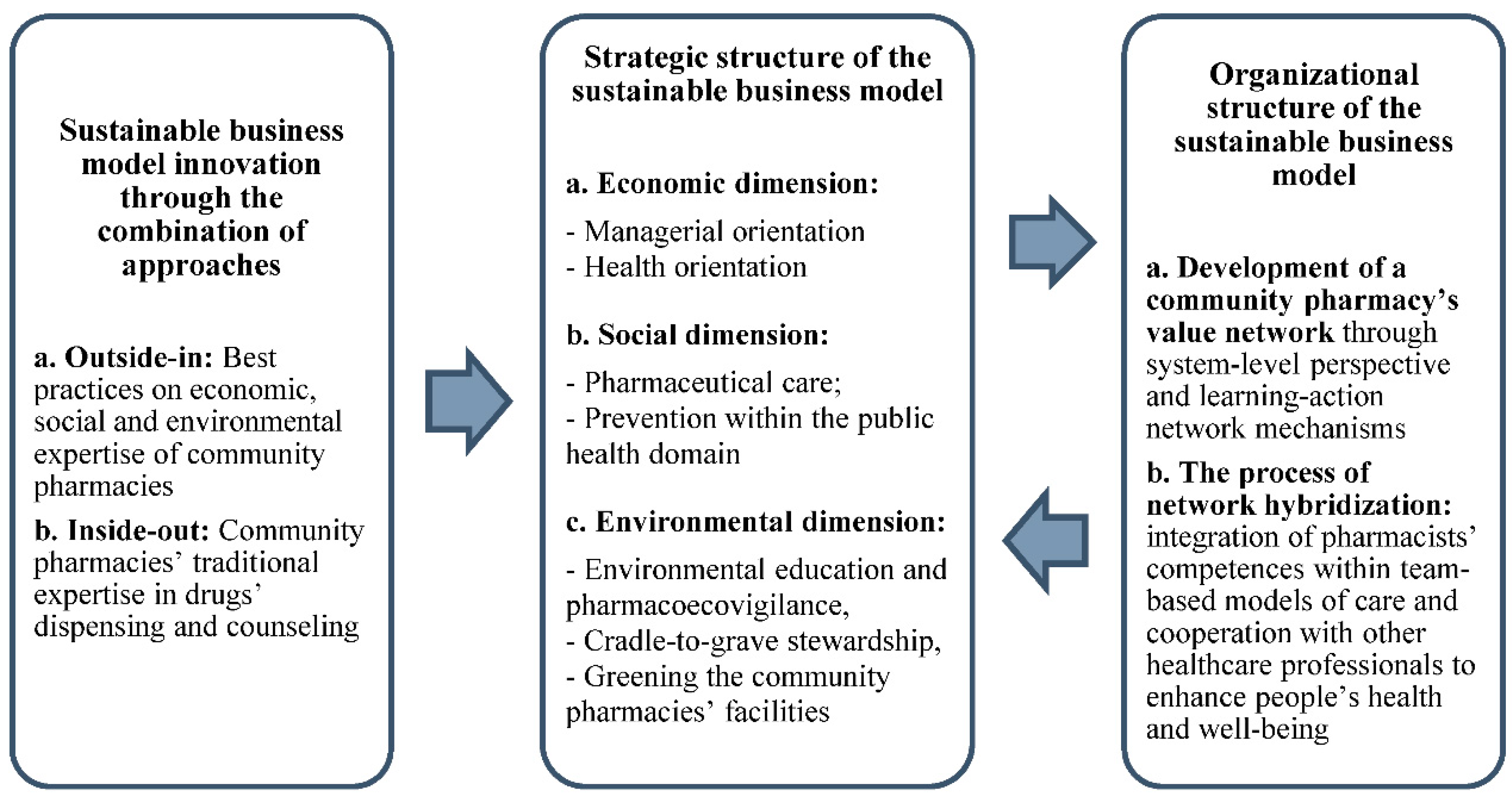
3. Sustainable Business Modelling: Theoretical Background
4. SBM and Community Pharmacies: Strategic Structure
4.1. Economic Dimension
4.1.1. Managerial Orientation
4.1.2. Health Orientation
4.2. Social Dimension
4.2.1. PC
4.2.2. Disease Prevention within the Public Health Domain
4.3. Environmental Dimension
4.3.1. Environmental Education and Ecopharmacovigilance
4.3.2. Cradle-to-Grave Stewardship
4.3.3. Greening Community Pharmacies’ Facilities
5. SBM and Community Pharmacies: Organizational Structure
5.1. The Development of a Community Pharmacy’s Value Network
5.2. The Process of Network Hybridization
6. Community Pharmacies’ SBM in Time of COVID-19
7. Discussion and Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Nunes, F.G.; Anderson, J.E.; Martins, L.M.; Wiig, S. The hybrid identity of micro enterprises: Contrasting the perspectives of community pharmacies’ owners-managers and employees. J. Small Bus. Enterp. Dev. 2017, 24, 34–53. [Google Scholar] [CrossRef]
- Joldersma, C.; Winter, V. Strategic management in hybrid organizations. Public Manag. Rev. 2002, 4, 83–99. [Google Scholar] [CrossRef]
- Dugani, S.; Duke, T.; Kissoon, N. Transforming health through sustainable development. Can. Med. Assoc. J. 2016, 188, E213–E214. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rutter, V.; Chan, A.H.Y.; Tuck, C.; Bader, L.; Bates, I. Weaving the health and pharmaceutical care agenda through the themes of the commonwealth heads of government meeting (CHOGM), London 2018. J. Pharm. Policy Pract. 2018, 11, 1–4. [Google Scholar] [CrossRef]
- Bader, L.; Duggan, C. FIP’s Commitment to Action on the WHO Astana Declaration: Transforming pharmacy for better health for all. Res. Soc. Adm. Pharm. 2020, 16, 724–726. [Google Scholar] [CrossRef]
- Laasch, O. Beyond the purely commercial business model: Organizational value logics and the heterogeneity of sustainability business models. Long Range Plan. 2018, 51, 158–183. [Google Scholar] [CrossRef]
- Institute of Medicine. Green Healthcare Institutions: Health, Environment, and Economics: Workshop Summary; Frumkin, H., Coussens, C., Eds.; National Academies Press: Washington, DC, USA, 2007. [Google Scholar] [CrossRef]
- Elkington, J. Cannibals with Forks: The Triple Bottom Line of 21st Century Business; Capstone: Oxford, UK, 1997. [Google Scholar]
- Breen, L.; Garvey, O.; Mosan, G.; Matthias, O.; Sowter, J. Do we need to be Sustainable? An examination of purpose and intention behind Sustainability practice in Community Pharmacies in the National Health Service (UK). In Proceedings of the British Academy of Management Conference, Warwick, UK, 5–7 September 2017. [Google Scholar]
- Webster, L.; Floyd, M. Green pharmacy practice. In Pharmacy Practice Today for the Pharmacy Technician; Webster, L., Ed.; Mosby: Maryland Heights, MO, USA, 2014; pp. 358–363. [Google Scholar]
- Bocken, N.M.; Short, S.W.; Rana, P.; Evans, S. A literature and practice review to develop sustainable business model archetypes. J. Clean. Prod. 2014, 65, 42–56. [Google Scholar] [CrossRef]
- Joyce, A.; Paquin, R.L. The triple layered business model canvas: A tool to design more sustainable business models. J. Clean. Prod. 2016, 135, 1474–1486. [Google Scholar] [CrossRef]
- Osterwalder, A.; Pigneur, Y. Aligning profit and purpose through business model innovation. In Responsible Management Practices for the 21st Century; Palazzo, G., Wentland, M., Eds.; Pearson Education France: Paris, France, 2011; pp. 61–75. [Google Scholar]
- Porter, M.E.; Kramer, M.R. The big idea: Creating shared value. Harv. Bus. Rev. 2011, 89, 2–17. [Google Scholar]
- Stubbs, W.; Cocklin, C. Conceptualizing a “sustainability business model”. Organ. Environ. 2008, 21, 103–127. [Google Scholar] [CrossRef]
- Abdelkafi, N.; Täuscher, K. Business models for sustainability from a system dynamics perspective. Organ. Environ. 2016, 29, 74–96. [Google Scholar] [CrossRef]
- Evans, S.; Vladimirova, D.; Holgado, M.; Van Fossen, K.; Yang, M.; Silva, E.A.; Barlow, C.Y. Business model innovation for sustainability: Towards a unified perspective for creation of sustainable business models. Bus. Strategy Environ. 2017, 26, 597–608. [Google Scholar] [CrossRef]
- Lüdeke-Freund, F.; Carroux, S.; Joyce, A.; Massa, L.; Breuer, H. The sustainable business model pattern taxonomy—45 patterns to support sustainability-oriented business model innovation. Sustain. Prod. Consum. 2018, 15, 145–162. [Google Scholar] [CrossRef]
- Roome, N.; Louche, C. Journeying toward business models for sustainability: A conceptual model found inside the black box of organisational transformation. Organ. Environ. 2016, 29, 11–35. [Google Scholar] [CrossRef]
- Geissdoerfer, M.; Vladimirova, D.; Evans, S. Sustainable business model innovation: A review. J. Clean. Prod. 2018, 198, 401–416. [Google Scholar] [CrossRef]
- Lüdeke-Freund, F.; Dembek, K. Sustainable business model research and practice: Emerging field or passing fancy? J. Clean. Prod. 2017, 168, 1668–1678. [Google Scholar] [CrossRef]
- Spieth, P.; Schneider, S.; Clauß, T.; Eichenberg, D. Value drivers of social businesses: A business model perspective. Long Range Plan. 2018, 53, 427–444. [Google Scholar] [CrossRef]
- Schaltegger, S.; Hansen, E.G.; Lüdeke-Freund, F. Business models for sustainability: Origins, present research, and future avenues. Organ. Environ. 2016, 29, 3–10. [Google Scholar] [CrossRef]
- Bocken, N.; Short, S.; Rana, P.; Evans, S. A value mapping tool for sustainable business modelling. Corp. Gov. 2013, 13, 482–497. [Google Scholar] [CrossRef]
- Kurunmäki, L. A hybrid profession—The acquisition of management accounting expertise by medical professionals. Account. Organ. Soc. 2004, 29, 327–347. [Google Scholar] [CrossRef]
- Miller, P.; Kurunmäki, L.; O’Leary, T. Accounting, hybrids and the management of risk. Account. Organ. Soc. 2008, 33, 942–967. [Google Scholar] [CrossRef]
- Castaldo, S.; Grosso, M.; Mallarini, E.; Rindone, M. The missing path to gain customers loyalty in pharmacy retail: The role of the store in developing satisfaction and trust. Res. Soc. Adm. Pharm. 2016, 12, 699–712. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, R.A.; Pioch, E.A. Community pharmacies under pressure: Issues of deregulation and competition. Int. J. Retail Distrib. Manag. 2004, 32, 354–357. [Google Scholar] [CrossRef]
- Gavilan, D.; Avello, M.; Abril, C. Shopper marketing: A new challenge for Spanish community pharmacies. Res. Soc. Adm. Pharm. 2014, 10, e125–e136. [Google Scholar] [CrossRef] [PubMed]
- Perepelkin, J.; Di Zhang, D. Brand personality and customer trust in community pharmacies. Int. J. Pharm. Healthc. Mark. 2011, 5, 175–193. [Google Scholar] [CrossRef]
- International Federation of Pharmacists. Advancing the Global Pharmaceutical Workforce towards Achieving Universal Health Coverage and the UN Sustainable Development Goals, 2017. Available online: https://fip.org/files/fip/PharmacyEducation/2017/WHA_2017.pdf (accessed on 25 September 2020).
- Fjeldstad, Ø.D.; Snow, C.C. Business models and organization design. Long Range Plan. 2018, 51, 32–39. [Google Scholar] [CrossRef]
- Baden-Fuller, C.; Haefliger, S. Business models and technological innovation. Long Range Plan. 2013, 46, 419–426. [Google Scholar] [CrossRef]
- Teece, D.J. Business models, business strategy and innovation. Long Range Plan. 2010, 43, 172–194. [Google Scholar] [CrossRef]
- Chesbrough, H. Business model innovation: Opportunities and barriers. Long Range Plan. 2010, 43, 354–363. [Google Scholar] [CrossRef]
- Upward, A.; Jones, P. An ontology for strongly sustainable business models: Defining an enterprise framework compatible with natural and social science. Organ. Environ. 2016, 29, 97–123. [Google Scholar] [CrossRef]
- Pieroni, M.P.; McAloone, T.; Pigosso, D.A. Business model innovation for circular economy and sustainability: A review of approaches. J. Clean. Prod. 2019, 215, 198–216. [Google Scholar] [CrossRef]
- Short, S.W.; Rana, P.; Bocken, N.M.P.; Evans, S. Embedding Sustainability in Business Modelling through Multi-stakeholder Value Innovation. In Advances in Production Management Systems. Competitive Manufacturing for Innovative Products and Services; Emmanouilidis, C., Taisch, M., Kiritsis, D., Eds.; Springer: Berlin, Germany, 2012; pp. 175–183. [Google Scholar]
- Osterwalder, A.; Pigneur, Y. Business Model Generation: A Handbook for Visionaries, Game Changers, and Challengers; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2010. [Google Scholar]
- Mossialos, E.; Courtin, E.; Naci, H.; Benrimoj, S.; Bouvy, M.; Farris, K.; Noyce, P.; Sketris, I. From “retailers” to health care providers: Transforming the role of community pharmacists in chronic disease management. Health Policy 2015, 119, 628–639. [Google Scholar] [CrossRef] [PubMed]
- Al-Arifi, M.N. The managerial role of pharmacist at community pharmacy setting in Saudi Arabia. Pharmacol. Pharm. 2013, 4, 63. [Google Scholar] [CrossRef]
- Pioch, E.A.; Schmidt, R.A. Community pharmacies as good neighbours? A comparative study of Germany and the UK. Int. J. Retail Distrib. Manag. 2004, 32, 532–544. [Google Scholar] [CrossRef]
- Ottewill, R.; Jennings, P.L.; Magirr, P. Management competence development for professional service SMEs: The case of community pharmacy. Educ. Train. 2000, 42, 246–255. [Google Scholar] [CrossRef][Green Version]
- Moullin, J.C.; Sabater-Hernández, D.; Fernandez-Llimos, F.; Benrimoj, S.I. Defining professional pharmacy services in community pharmacy. Res. Soc. Adm. Pharm. 2013, 9, 989–995. [Google Scholar] [CrossRef]
- Woodard, L.J.; Kahaleh, A.A.; Nash, J.D.; Truong, H.; Gogineni, H.; Barbosa-Leiker, C. Healthy People 2020: Assessment of pharmacists’ priorities. Public Health 2018, 155, 69–80. [Google Scholar] [CrossRef]
- Schommer, J.C.; Olson, A.W.; Isetts, B.J. Transforming community-based pharmacy practice through financially sustainable centers for health and personal care. J. Am. Pharm. Assoc. 2018, 59, 306–309. [Google Scholar] [CrossRef]
- Singleton, J.A.; Nissen, L.M. Future-proofing the pharmacy profession in a hypercompetitive market. Res. Soc. Adm. Pharm. 2014, 10, 459–468. [Google Scholar] [CrossRef]
- Wiedenmayer, K.; Summers, R.S.; Mackie, C.A.; Gous, A.G.S.; Everard, M.; Tromp, D. Developing Pharmacy Practice. A Focus on Patient Care; World Health Organization and International Pharmaceutical Federation: Hague, The Netherlands, 2006. [Google Scholar]
- Hepler, C.D.; Strand, L.M. Opportunities and responsibilities in pharmaceutical care. Am. J. Health Syst. Pharm. 1990, 47, 533–543. [Google Scholar] [CrossRef]
- Kehrer, J.P.; Eberhart, G.; Wing, M.; Horon, K. Pharmacy’s role in a modern health continuum. Can. Pharm. J. 2013, 146, 321–324. [Google Scholar] [CrossRef] [PubMed]
- Bernsten, C.; Björkman, I.; Caramona, M.; Crealey, G.; Frøkjær, B.; Grundberger, E.; Gustafsson, T.; Henman, M.; Herborg, H.; Hughes, C.; et al. Improving the well-being of elderly patients via community pharmacy-based provision of pharmaceutical care. Drugs Aging 2001, 18, 63–77. [Google Scholar] [CrossRef] [PubMed]
- Ensing, H.T.; Koster, E.S.; Dubero, D.J.; van Dooren, A.A.; Bouvy, M.L. Collaboration between hospital and community pharmacists to address drug-related problems: The HomeCoMe-program. Res. Soc. Adm. Pharm. 2019, 15, 267–278. [Google Scholar] [CrossRef] [PubMed]
- Cranor, C.W.; Bunting, B.A.; Christensen, D.B. The Asheville Project: Long-term clinical and economic outcomes of a community pharmacy diabetes care program. J. Am. Pharm. Assoc. 2003, 43, 173–184. [Google Scholar] [CrossRef] [PubMed]
- Garrett, D.G.; Bluml, B.M. Patient self-management program for diabetes: First-year clinical, humanistic, and economic outcomes. J. Am. Pharm. Assoc. 2005, 45, 130–137. [Google Scholar] [CrossRef]
- Munroe, W.P.; Kunz, K.; Dalmady-Israel, C.; Potter, L.; Schonfeld, W.H. Economic evaluation of pharmacist involvement in disease management in a community pharmacy setting. Clin. Ther. 1997, 19, 113–123. [Google Scholar] [CrossRef]
- Park, J.J.; Kelly, P.; Carter, B.L.; Burgess, P.P. Comprehensive Pharmaceutical Care in the Chain Setting: Drug therapy monitoring and counseling by pharmacists contributed to improved blood pressure control in study patients. J. Am. Pharm. Assoc. 1996, 36, 443–451. [Google Scholar]
- Wermeille, J.; Bennie, M.; Brown, I.; McKnight, J. Pharmaceutical care model for patients with type 2 diabetes: Integration of the community pharmacist into the diabetes team—A pilot study. Pharm. World Sci. 2004, 26, 18–25. [Google Scholar] [CrossRef]
- Franco-Trigo, L.; Hossain, L.N.; Durks, D.; Fam, D.; Inglis, S.C.; Benrimoj, S.I.; Sabater-Hernández, D. Stakeholder analysis for the development of a community pharmacy service aimed at preventing cardiovascular disease. Res. Soc. Adm. Pharm. 2017, 13, 539–552. [Google Scholar] [CrossRef]
- van Mil, J.F.; Schulz, M. A review of pharmaceutical care in community pharmacy in Europe. Harv. Health Policy Rev. 2006, 7, 155–168. [Google Scholar]
- Peña, C. Spanish pharmacy: Promoting sustainability through corporate social responsibility. Int. Pharm. J. 2011, 27, 1–52. [Google Scholar]
- Vagnoni, E.; Biavati, G.R.; Felisatti, M.; Pomidori, L. Moderating healthcare costs through an assisted physical activity programme. Int. J. Health Plann. Manag. 2018, 33, 1146–1158. [Google Scholar] [CrossRef] [PubMed]
- Root, D.; Varney, J. Pharmacy: A Way Forward for Public Health Opportunities for Action through Pharmacy for Public Health; Public Health England: London, UK, 2017; pp. 1–53. [Google Scholar]
- Anderson, C. Health promotion in community pharmacy: The UK situation. Patient Educ. Couns. 2000, 39, 285–291. [Google Scholar] [CrossRef]
- Nazar, H.; Nazar, Z. Community pharmacy minor ailment services in England: Pharmacy stakeholder perspectives on the factors affecting sustainability. Res. Soc. Adm. Pharm. 2018, 15, 292–302. [Google Scholar] [CrossRef]
- Birkin, F.; Polesie, T.; Lewis, L. A new business model for sustainable development: An exploratory study using the theory of constraints in Nordic organizations. Bus. Strategy Environ. 2009, 18, 277–290. [Google Scholar] [CrossRef]
- Saramunee, K.; Krska, J.; Mackridge, A.; Richards, J.; Suttajit, S.; Phillips-Howard, P. How to enhance public health service utilization in community pharmacy? General public and health providers’ perspectives. Res. Soc. Adm. Pharm. 2014, 10, 272–284. [Google Scholar] [CrossRef]
- Singleton, J. Greening pharmacy—Going green. Aust. J. Pharm. 2013, 94, 64–68. [Google Scholar]
- Campbell, J. Creating an environmentally friendly pharmacy. Pharm. Pract. 2008, March/April, 41–43. [Google Scholar]
- Kreisberg, J. Greener Pharmacy. Integr. Med. 2007, 6, 50–52. [Google Scholar]
- Wick, J.Y. Getting to Green: How’s Pharmacy Doing? Available online: https://www.pharmacytimes.com/publications/issue/2013/November2013/Getting-to-Green-Hows-Pharmacy-Doing (accessed on 25 September 2020).
- Daughton, C.G.; Ruhoy, I.S. Green pharmacy and pharmEcovigilance: Prescribing and the planet. Expert Rev. Clin. Pharmacol. 2011, 4, 211–232. [Google Scholar] [CrossRef]
- Daughton, C.G. Cradle-to-cradle stewardship of drugs for minimizing their environmental disposition while promoting human health. I. Rationale for and avenues toward a green pharmacy. Environ. Health Perspect. 2003, 111, 757. [Google Scholar] [CrossRef] [PubMed]
- Götz, K.; Deffner, J. Options for a more environmentally friendly handling of pharmaceuticals. In Green and Sustainable Pharmacy; Kümmerer, K., Hempel, M., Eds.; Springer: Berlin, Germany, 2010; pp. 149–163. [Google Scholar]
- Velo, G.; Moretti, U. Ecopharmacovigilance for Better Health. Drug Saf. 2010, 33, 963–968. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Breen, L. Greening community pharmaceutical supply chain in UK: A cross boundary approach. Supply Chain Manag. 2012, 17, 40–53. [Google Scholar] [CrossRef]
- Schaper, M. Small firms and environmental management: Predictors of green purchasing in Western Australian pharmacies. Int. Small Bus. J. 2002, 20, 235–251. [Google Scholar] [CrossRef]
- Kümmerer, K. Sustainable from the very beginning: Rational design of molecules by life cycle engineering as an important approach for green pharmacy and green chemistry. Green Chem. 2007, 9, 899–907. [Google Scholar] [CrossRef]
- Kotchen, M.; Kallaos, J.; Wheeler, K.; Wong, C.; Zahller, M. Pharmaceuticals in wastewater: Behavior, preferences, and willingness to pay for a disposal program. J. Environ. Manag. 2009, 90, 1476–1482. [Google Scholar] [CrossRef]
- Thach, A.V.; Brown, C.M.; Pope, N. Consumer perceptions about a community pharmacy-based medication take back program. J. Environ. Manag. 2013, 127, 23–27. [Google Scholar] [CrossRef]
- Mair, J.; Mayer, J.; Lutz, E. Navigating institutional plurality: Organizational governance in hybrid organizations. Organ. Stud. 2015, 36, 713–739. [Google Scholar] [CrossRef]
- Anderson, C.; Bates, I.; Beck, D.; Brock, T.P.; Futter, B.; Mercer, H.; Rouse, M.; Wuliji, T.; Yonemura, A. The WHO UNESCO FIP pharmacy education taskforce. Hum. Resour. Health 2009, 7, 45. [Google Scholar] [CrossRef]
- Allee, V. Value-creating networks: Organizational issues and challenges. Learn. Organ. 2009, 16, 427–442. [Google Scholar] [CrossRef]
- Turner, K.; Weinberger, M.; Renfro, C.; Ferreri, S.; Trygstad, T.; Trogdon, J.; Shea, C.M. The role of network ties to support implementation of a community pharmacy enhanced services network. Res. Soc. Adm. Pharm. 2018, 15, 1118–1125. [Google Scholar] [CrossRef] [PubMed]
- Kozminski, M.; Busby, R.; McGivney, M.S.; Klatt, P.M.; Hackett, S.R.; Merenstein, J.H. Pharmacist integration into the medical home: Qualitative analysis. J. Am. Pharm. Assoc. 2011, 51, 173–183. [Google Scholar] [CrossRef] [PubMed]
- Hakovirta, M.; Denuwara, N. How COVID-19 Redefines the Concept of Sustainability. Sustainability 2020, 12, 3727. [Google Scholar] [CrossRef]
- Nadeem, M.F.; Soumya, S.; Mustafa, M. Is the Paradigm of Community Pharmacy Practice Expected to Shift Due to COVID-19? Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7255229/ (accessed on 25 September 2020).
- Cadogan, C.A.; Hughes, C.M. On the frontline against COVID-19: Community pharmacists’ contribution during a public health crisis. Res. Soc. Adm. Pharm. 2020, in press. [Google Scholar] [CrossRef] [PubMed]
- Bukhari, N.; Huma, R.; Bismah, N.; Zaheer-Ud-Din, B. Pharmacists at the frontline beating the COVID-19 pandemic. J. Pharm. Policy Pract. 2020, 13, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Koster, E.S.; Philbert, D.; Bouvy, M.L. Impact of the COVID-19 epidemic on the provision of pharmaceutical care in community pharmacies. Res. Soc. Adm. Pharm. 2020, in press. [Google Scholar] [CrossRef]
- Nosratabadi, S.; Mosavi, A.; Shamshirband, S.; Zavadskas, E.K.; Rakotonirainy, A.; Chau, K.W. Sustainable business models: A review. Sustainability 2019, 11, 1663. [Google Scholar] [CrossRef]
- Dentchev, N.; Rauter, R.; Jóhannsdóttir, L.; Snihur, Y.; Rosano, M.; Baumgartner, R.; Nyberg, T.; Tang, X.; van Hoof, B.; Jonker, J. Embracing the variety of sustainable business models: A prolific field of research and a future research agenda. J. Clean. Prod. 2018, 194, 695–703. [Google Scholar] [CrossRef]
- Birkin, F.; Cashman, A.; Koh, S.C.L.; Liu, Z. New sustainable business models in China. Bus. Strategy Environ. 2009, 18, 64–77. [Google Scholar] [CrossRef]
- Sobczak, E.; Bartniczak, B.; Raszkowski, A. Aging Society and the Selected Aspects of Environmental Threats: Evidence from Poland. Sustainability 2020, 12, 4648. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cavicchi, C.; Vagnoni, E. Sustainable Business Models in Hybrids: A Conceptual Framework for Community Pharmacies’ Business Owners. Sustainability 2020, 12, 8125. https://doi.org/10.3390/su12198125
Cavicchi C, Vagnoni E. Sustainable Business Models in Hybrids: A Conceptual Framework for Community Pharmacies’ Business Owners. Sustainability. 2020; 12(19):8125. https://doi.org/10.3390/su12198125
Chicago/Turabian StyleCavicchi, Caterina, and Emidia Vagnoni. 2020. "Sustainable Business Models in Hybrids: A Conceptual Framework for Community Pharmacies’ Business Owners" Sustainability 12, no. 19: 8125. https://doi.org/10.3390/su12198125
APA StyleCavicchi, C., & Vagnoni, E. (2020). Sustainable Business Models in Hybrids: A Conceptual Framework for Community Pharmacies’ Business Owners. Sustainability, 12(19), 8125. https://doi.org/10.3390/su12198125





