Distal Femoral Shortening Osteotomy for Severe Knee Flexion Contracture and Crouch Gait in Cerebral Palsy
Abstract
1. Introduction
2. Experimental Section
2.1. Subjects
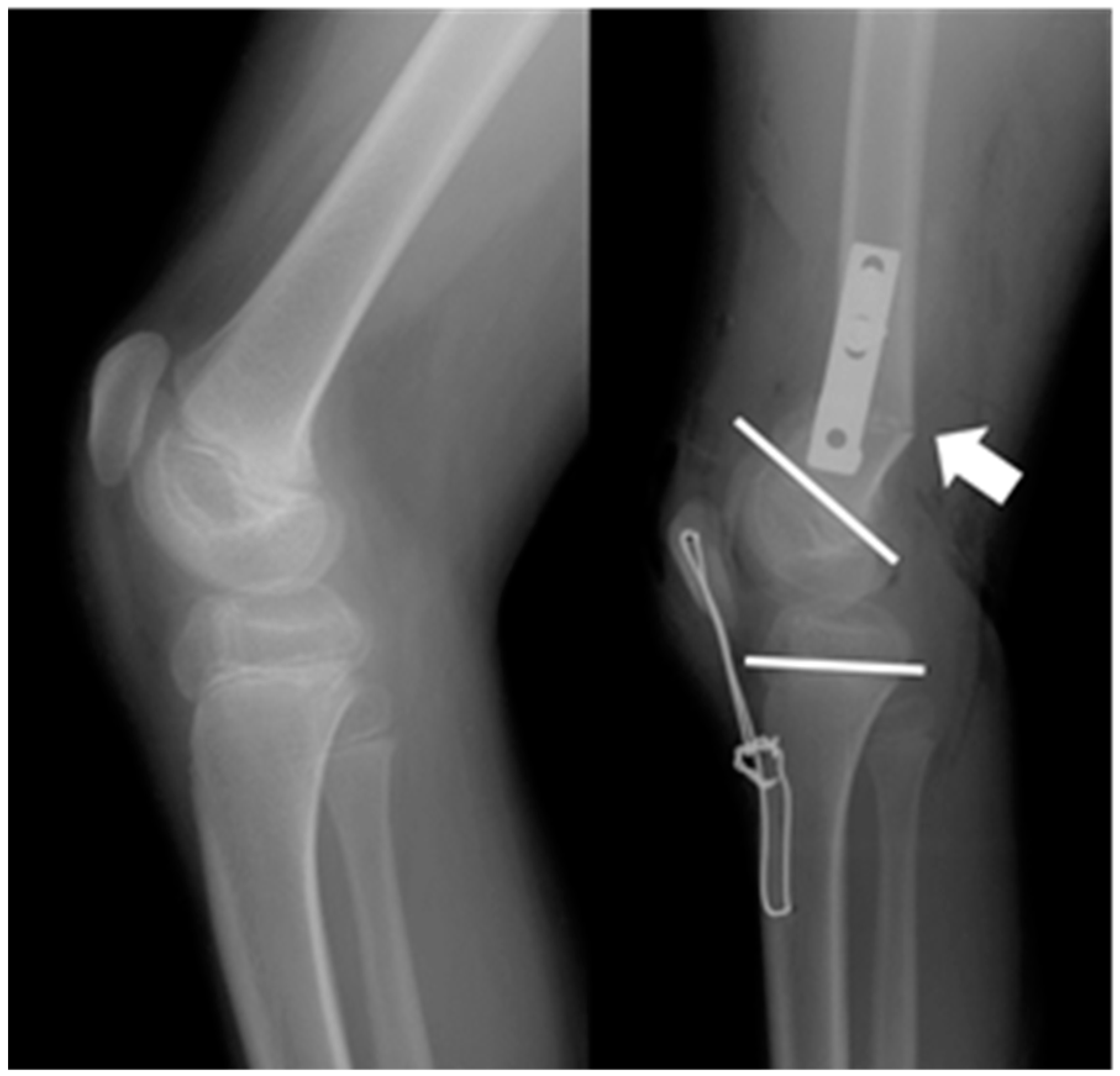
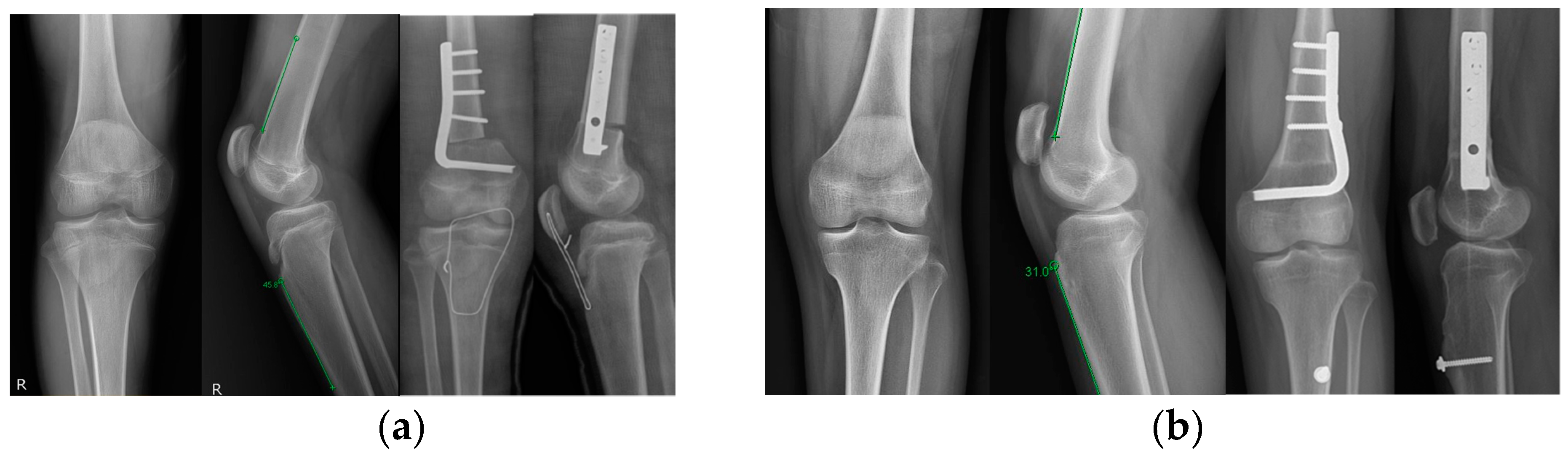
2.2. Surgical Technique
2.3. Clinical, Radiological, and Gait Parameters
2.4. Statistical Analyses
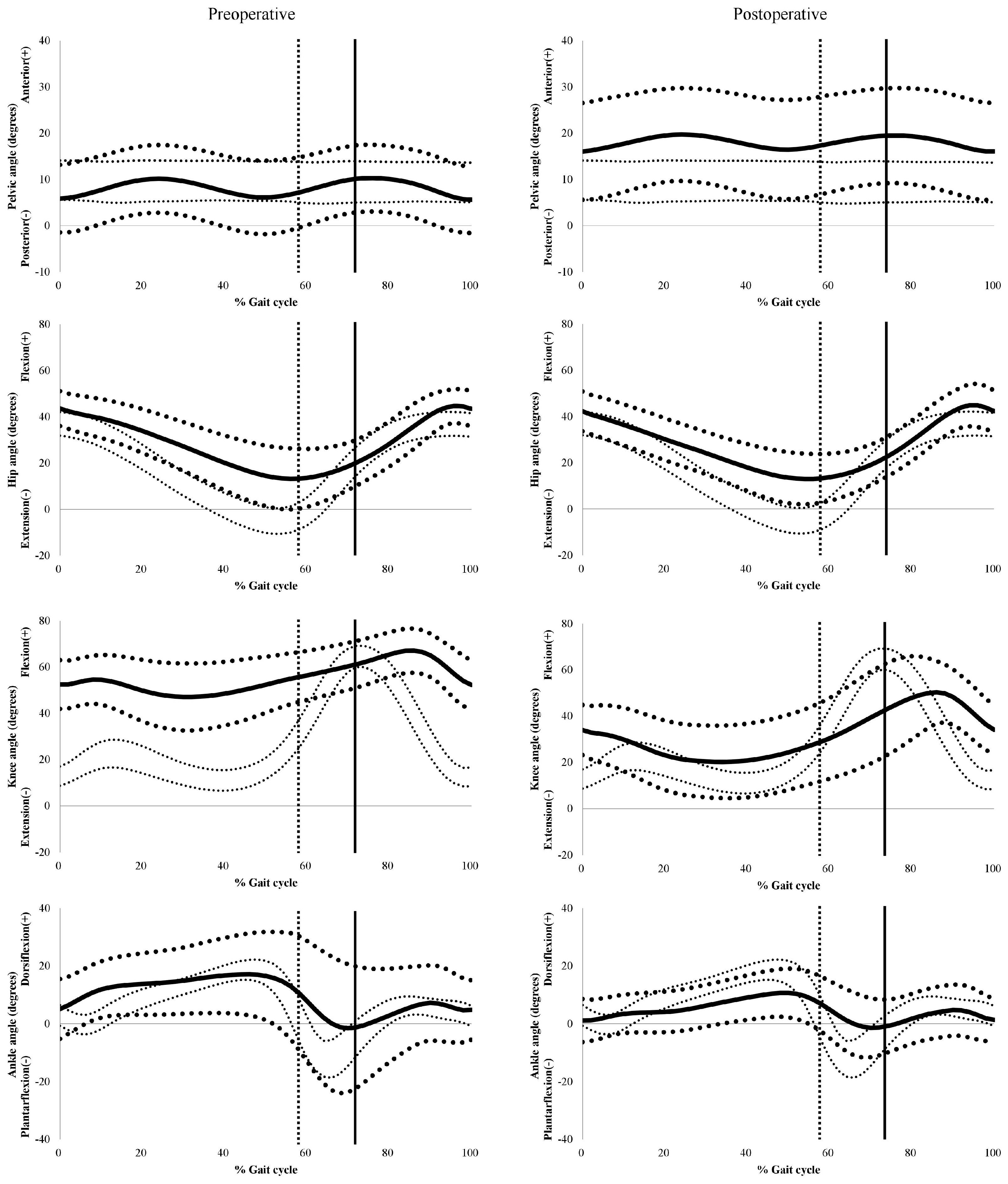
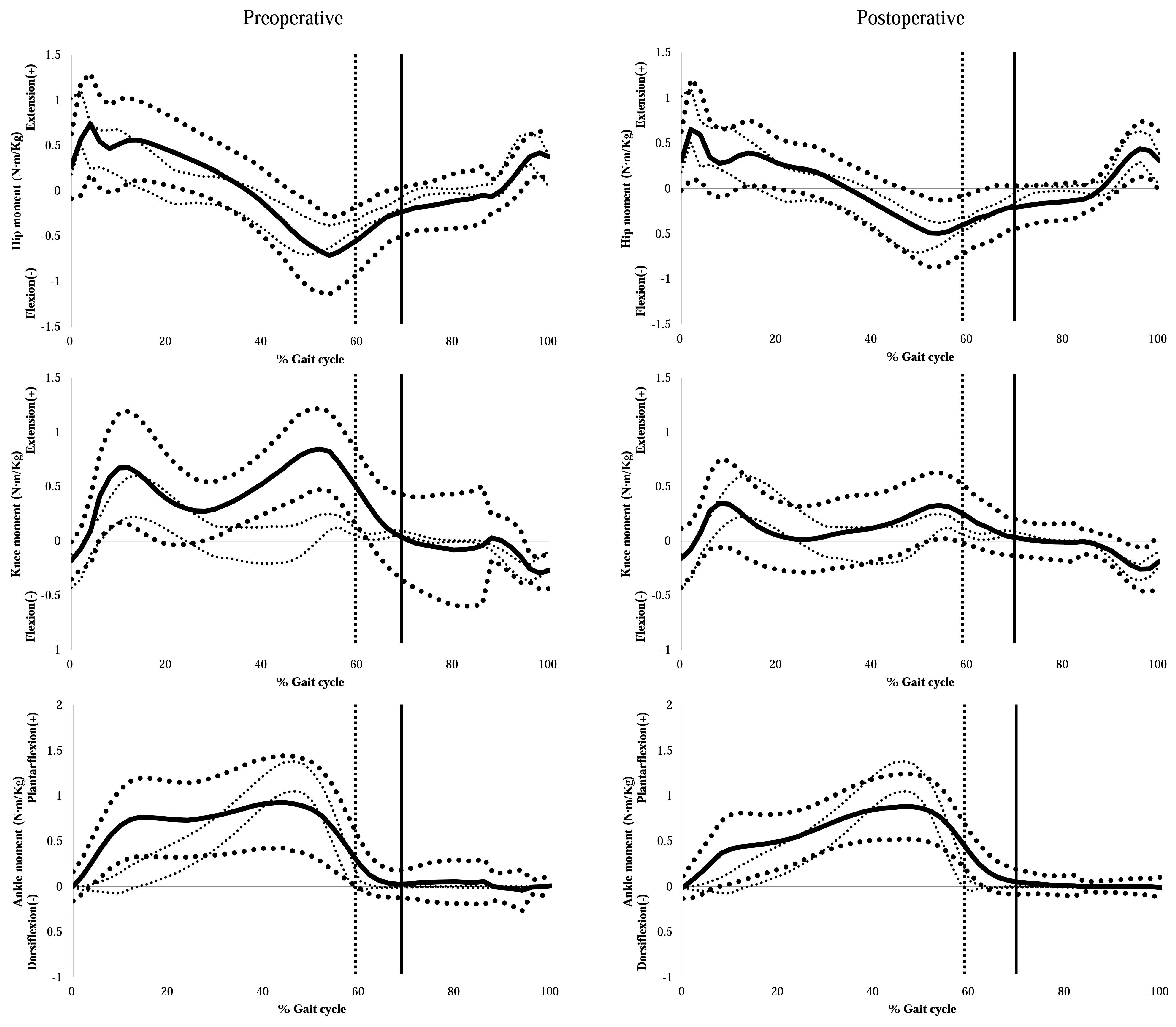
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gage, J.R.; Schwartz, M.H.; Koop, S.E. The Identification and Treatment of Gait Problems in Cerebral Palsy; Mac Keith Press: London, UK, 2014. [Google Scholar]
- Rodda, J.M.; Graham, H.K.; Nattrass, G.R.; Galea, M.P.; Baker, R.; Wolfe, R. Correction of severe crouch gait in patients with spastic diplegia with use of multilevel orthopaedic surgery. J. Bone Jt. Surg. Am. Vol. 2006, 88, 2653–2664. [Google Scholar] [CrossRef] [PubMed]
- Sutherl, D.H.; Davids, J.R. Common Gait Abnormalities of the Knee in Cerebral Palsy. Clin. Orthop. Relat. Res. 1993, 288, 139–147. [Google Scholar] [CrossRef]
- Novacheck, T.F.; Gage, J.R. Orthopedic management of spasticity in cerebral palsy. Child’s Nerv. Syst. 2007, 23, 1015–1031. [Google Scholar] [CrossRef] [PubMed]
- Chang, F.M.; Rhodes, J.T.; Flynn, K.M.; Carollo, J.J. The Role of Gait Analysis in Treating Gait Abnormalities in Cerebral Palsy. Orthop. Clin. N. Am. 2010, 41, 489–506. [Google Scholar] [CrossRef] [PubMed]
- Vuillermin, C.; Rodda, J.; Rutz, E.; Shore, B.J.; Smith, K.; Graham, H.K. Severe crouch gait in spastic diplegia can be prevented: A population-based study. J. Bone Jt. Surg. Br. Vol. 2011, 93, 1670–1675. [Google Scholar] [CrossRef] [PubMed]
- Krughoff, K.; Shapiro, J.A.; Carollo, J.; Seidl, A.; Baldini, T.; Lindeque, B.; Rhodes, J. Biomechanical Assessment of Patellar Advancement Procedures for Patella Alta. Orthopedics 2016, 39, 492–497. [Google Scholar]
- Lenhart, R.L.; Brandon, S.C.; Smith, C.R.; Novacheck, T.F.; Schwartz, M.H.; Thelen, D.G. Influence of patellar position on the knee extensor mechanism in normal and crouched walking. J. Biomech. 2017, 51, 1–7. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Topoleski, T.A.; Kurtz, C.A.; Grogan, D.P. Radiographic Abnormalities and Clinical Symptoms Associated with Patella Alta in Ambulatory Children with Cerebral Palsy. J. Pediatr. Orthop. 2000, 20, 636–639. [Google Scholar] [CrossRef]
- Gordon, A.B.; Baird, G.O.; McMulkin, M.L.; Caskey, P.M.; Ferguson, R.L. Gait Analysis Outcomes of Percutaneous Medial Hamstring Tenotomies in Children with Cerebral Palsy. J. Pediatr. Orthop. 2008, 28, 324–329. [Google Scholar] [CrossRef]
- Park, M.S.; Chung, C.Y.; Lee, S.H.; Choi, I.H.; Cho, T.J.; Yoo, W.J.; Park, B.S.; Lee, K.M. Effects of distal hamstring lengthening on sagittal motion in patients with diplegia: Hamstring length and its clinical use. Gait Posture 2009, 30, 487–491. [Google Scholar] [CrossRef]
- Dreher, T.; Vegvari, D.; Wolf, S.I.; Geisbusch, A.; Gantz, S.; Wenz, W.; Braatz, F. Development of knee function after hamstring lengthening as a part of multilevel surgery in children with spastic diplegia: A long-term outcome study. J. Bone Jt. Surg. Am. Vol. 2012, 94, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Kay, R.M.; Rethlefsen, S.A.; Skaggs, D.; Leet, A. Outcome of Medial Versus Combined Medial and Lateral Hamstring Lengthening Surgery in Cerebral Palsy. J. Pediatr. Orthop. 2002, 22, 169–172. [Google Scholar] [CrossRef] [PubMed]
- Filho, M.C.D.M.; Neves, D.L.; Abreu, F.P.; Juliano, Y.; Guimarães, L. Treatment of fixed knee flexion deformity and crouch gait using distal femur extension osteotomy in cerebral palsy. J. Child. Orthop. 2008, 2, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Stout, J.L.; Gage, J.R.; Schwartz, M.H.; Novacheck, T.F. Distal femoral extension osteotomy and patellar tendon advancement to treat persistent crouch gait in cerebral palsy. J. Bone Jt. Surg. Am. Vol. 2008, 90, 2470–2484. [Google Scholar] [CrossRef] [PubMed]
- Das, S.P.; Pradhan, S.; Ganesh, S.; Sahu, P.K.; Mohanty, R.N.; Das, S.K. Supracondylar femoral extension osteotomy and patellar tendon advancement in the management of persistent crouch gait in cerebral palsy. Indian J. Orthop. 2012, 46, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Klotz, M.C.M.; Hirsch, K.; Heitzmann, D.; Maier, M.W.; Hagmann, S.; Dreher, T. Distal femoral extension and shortening osteotomy as a part of multilevel surgery in children with cerebral palsy. World J. Pediatrics WJP 2017, 13, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Salami, F.; Wagner, J.; Van Drongelen, S.; Klotz, M.C.M.; Dreher, T.; Wolf, S.I.; Niklasch, M. Mid-term development of hamstring tendon length and velocity after distal femoral extension osteotomy in children with bilateral cerebral palsy: A retrospective cohort study. Dev. Med. Child Neurol. 2018, 60, 833–838. [Google Scholar] [CrossRef] [PubMed]
- Filho, M.C.; Blumetti, F.C.; Kawamura, C.M.; Leite, J.B.R.; Lopes, J.A.F.; Fujino, M.H.; Neves, D.L. The increase of anterior pelvic tilt after crouch gait treatment in patients with cerebral palsy. Gait Posture 2018, 63, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Boyer, E.R.; Stout, J.L.; Laine, J.C.; Gutknecht, S.M.; Araujo de Oliveira, L.H.; Munger, M.E.; Schwartz, M.H.; Novacheck, T.F. Long-term outcomes of distal femoral extension osteotomy and patellar tendon advancement in individuals with cerebral palsy. J. Bone Jt. Surg. Am. Vol. 2018, 100, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Novacheck, T.F.; Stout, J.L.; Gage, J.R.; Schwartz, M.H. Distal femoral extension osteotomy and patellar tendon advancement to treat persistent crouch gait in cerebral palsy. Surgical Technique. J. Bone Jt. Surg. Am. Vol. 2009, 91, 271–286. [Google Scholar] [CrossRef] [PubMed]
- Bittmann, M.F.; Lenhart, R.L.; Schwartz, M.H.; Novacheck, T.F.; Hetzel, S.; Thelen, D.G. How does patellar tendon advancement alter the knee extensor mechanism in children treated for crouch gait? Gait Posture 2018, 64, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Inan, M.; Sarikaya, I.A.; Yildirim, E.; Guven, M.F. Neurological complications after supracondylar femoral osteotomy in cerebral palsy. J. Pediatric Orthop. 2015, 35, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Lenhart, R.L.; Smith, C.R.; Schwartz, M.H.; Novacheck, T.F.; Thelen, D.G. The effect of distal femoral extension osteotomy on muscle lengths after surgery. J. Child. Orthop. 2017, 11, 472–478. [Google Scholar] [CrossRef] [PubMed]
- Joseph, B.; Reddy, K.; Varghese, R.A.; Shah, H.; Doddabasappa, S.N. Management of Severe Crouch Gait in Children and Adolescents with Cerebral Palsy. J. Pediatr. Orthop. 2010, 30, 832–839. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, M.H.; Smith, C.F.; Oppenheim, W.L. Supracondylar Femoral Extension Osteotomies in the Treatment of Fixed Flexion Deformity of the Knee. Clin. Orthop. Relat. Res. 1982, 171, 87–93. [Google Scholar] [CrossRef]
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev. Med. Child Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Koshino, T.; Sugimoto, K. New Measurement of Patellar Height in the Knees of Children Using the Epiphyseal Line Midpoint. J. Pediatr. Orthop. B 1989, 9, 216–218. [Google Scholar] [CrossRef]
- Insall, J.; Salvati, E. Patella Position in the Normal Knee Joint 1. Radiology 1971, 101, 101–104. [Google Scholar] [CrossRef] [PubMed]
- Park, C.I.; Park, E.S.; Kim, H.W.; Rha, D.-W. Soft Tissue Surgery for Equinus Deformity in Spastic Hemiplegic Cerebral Palsy: Effects on Kinematic and Kinetic Parameters. Yonsei Med J. 2006, 47, 657–666. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schwartz, M.H.; Rozumalski, A. The gait deviation index: A new comprehensive index of gait pathology. Gait Posture 2008, 28, 351–357. [Google Scholar] [CrossRef] [PubMed]
- Molloy, M.; McDowell, B.; Kerr, C.; Cosgrove, A. Further evidence of validity of the Gait Deviation Index. Gait Posture 2010, 31, 479–482. [Google Scholar] [CrossRef] [PubMed]
- Sossai, R.; Vavken, P.; Brunner, R.; Camathias, C.; Graham, H.K.; Rutz, E. Patellar tendon shortening for flexed knee gait in spastic diplegia. Gait Posture 2015, 41, 658–665. [Google Scholar] [CrossRef] [PubMed]
- Asirvatham, R.; Mukherjee, A.; Agarwal, S.; Rooney, R.J.; Ellis, R.D.; Watts, H.G. Supracondylar femoral extension osteotomy: Its complications. J. Pediatr. Orthop. 1993, 13, 642–645. [Google Scholar] [CrossRef] [PubMed]
- Van Der Krogt, M.M.; Doorenbosch, C.A.; Harlaar, J. The effect of walking speed on hamstrings length and lengthening velocity in children with spastic cerebral palsy. Gait Posture 2009, 29, 640–644. [Google Scholar] [CrossRef] [PubMed]
- Böhm, H.; Hösl, M.; Döderlein, L. Predictors for anterior pelvic tilt following surgical correction of flexed knee gait including patellar tendon shortening in children with cerebral palsy. Gait Posture 2017, 54, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Bialik, G.M.; Pierce, R.; Dorociak, R.; Lee, T.S.; Aiona, M.D.; Sussman, M.D. Iliopsoas Tenotomy at the Lesser Trochanter Versus at the Pelvic Brim in Ambulatory Children with Cerebral Palsy. J. Pediatr. Orthop. 2009, 29, 251–255. [Google Scholar] [CrossRef] [PubMed]
- Zwick, E.B.; Saraph, V.; Zwick, G.; Steinwender, C.; Linhart, W.E.; Steinwender, G. Medial hamstring lengthening in the presence of hip flexor tightness in spastic diplegia. Gait Posture 2002, 16, 288–296. [Google Scholar] [CrossRef]
- Arnold, A.S.; Liu, M.Q.; Schwartz, M.H.; Ounpuu, S.; Delp, S.L. The role of estimating muscle-tendon lengths and velocities of the hamstrings in the evaluation and treatment of crouch gait. Gait Posture 2006, 23, 273–281. [Google Scholar] [CrossRef]
- Healy, M.T.; Schwartz, M.H.; Stout, J.L.; Gage, J.R.; Novacheck, T.F. Is simultaneous hamstring lengthening necessary when performing distal femoral extension osteotomy and patellar tendon advancement? Gait Posture 2011, 33, 1–5. [Google Scholar] [CrossRef]
- Lee, S.Y. Muscle activities of the rectus abdominis and rectus femoris and their ratio during leg raises performed by healthy adults. J. Phys. Ther. Sci. 2015, 27, 549–550. [Google Scholar] [CrossRef][Green Version]
- Wolf, S.I.; Mikut, R.; Kranzl, A.; Dreher, T. Which functional impairments are the main contributors to pelvic anterior tilt during gait in individuals with cerebral palsy? Gait Posture 2014, 39, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Klotz, M.; Krautwurst, B.K.; Hirsch, K.; Niklasch, M.; Maier, M.; Wolf, S.; Dreher, T. Does additional patella tendon shortening influence the effects of multilevel surgery to correct flexed knee gait in cerebral palsy: A randomized controlled trial. Gait Posture 2018, 60, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Hoshino, Y.; Wang, J.H.; Lorenz, S.; Fu, F.H.; Tashman, S. The effect of distal femur bony morphology on in vivo knee translational and rotational kinematics. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 1331–1338. [Google Scholar] [CrossRef] [PubMed]
| Types of Surgery | Previous Surgery | Simultaneous Surgery |
|---|---|---|
| Osseous surgery | ||
| Tibial derotation osteotomy | 2 | 8 |
| Reconstruction of lateral/medial column of the foot | 11 | 11 |
| Soft-tissue release | ||
| Psoas | 8 | 2 |
| Adductor | 10 | 13 |
| Hamstring | 17 | 0 |
| Plantarflexors | 16 | 11 |
| Preoperative | Final Follow-Up | p-Value | |
|---|---|---|---|
| Physical examination | |||
| Knee flexion contracture (°) | 38 ± 6 | 12 ± 7 | <0.001 |
| Popliteal angle (°) | 68 ± 16 | 46 ± 11 | <0.001 |
| Radiographic parameters | |||
| pPDFA (°) | 86.7 ± 3.6 | 88.1 ± 4.8 | 0.014 |
| Koshino index | 1.56 ± 0.17 | 1.24 ± 0.17 | <0.001 |
| Koshino index (z-score) | 2.3 ± 1.8 | −0.7 ± 1.9 | <0.001 |
| Gait parameters | |||
| Walking speed (cm/second) | 54 ± 33 | 48 ± 35 | 0.288 |
| Step length (cm) | 35 ± 14 | 32 ± 15 | 0.232 |
| Cadence (steps/min) | 86 ± 33 | 80 ± 34 | 0.253 |
| Preoperative | Final Follow-Up | p-Value | |
|---|---|---|---|
| Pelvis | |||
| Maximum pelvic tilt (°) | 12.3 ± 7.0 | 21.4 ± 10.0 | <0.001 |
| Average pelvic tilt (°) | 8.2 ± 7.1 | 18.1 ± 10.3 | <0.001 |
| Range of pelvic tilt (°) | 8.6 ± 3.3 | 7.0 ± 2.5 | <0.001 |
| Hip | |||
| Maximum hip extension in stance (°) | 11.1 ± 11.4 | 11.7 ± 10.5 | 0.539 |
| Maximum hip flexion in swing (°) | 46.4 ± 7.7 | 46.1 ± 9.3 | 0.789 |
| Knee | |||
| Maximum knee extension in stance (°) | 44.7 ± 13.3 | 18.3 ± 15.3 | <0.001 |
| Knee flexion at mid-stance (°) | 47.2 ± 14.6 | 20.1 ± 16.2 | <0.001 |
| Maximum knee flexion in swing (°) | 70.1 ± 8.9 | 56.0 ± 11.3 | <0.001 |
| Range of knee flexion (°) | 25.4 ± 9.7 | 37.7 ± 10.9 | <0.001 |
| Knee flexion at initial contact (°) | 52.4 ± 10.7 | 33.4 ± 11.6 | <0.001 |
| Ankle | |||
| Mean dorsiflexion in stance (°) | 12.2 ± 12.8 | 5.6 ± 6.7 | <0.001 |
| Maximum dorsiflexion in stance (°) | 20.7 ± 13.3 | 12.5 ± 7.4 | <0.001 |
| Mid-stance dorsiflexion (°) | 16.1 ± 12.7 | 7.7 ± 7.3 | <0.001 |
| Maximum plantarflexion in swing (°) | −8.7 ± 17.4 | −5.2 ± 9.1 | 0.072 |
| Maximum dorsiflexion in swing (°) | 8.9 ± 12.5 | 6.3 ± 8.5 | 0.035 |
| Group 1 (n = 22) | Group 2 (n = 11) | p-Value | |
|---|---|---|---|
| Pelvis | |||
| Maximum pelvic tilt (°) | 11.6 ± 5.5 | 13.9 ± 9.4 | 0.217 |
| Average pelvic tilt (°) | 7.2 ± 5.7 | 10.4 ± 9.1 | 0.100 |
| Range of pelvic tilt (°) | 8.8 ± 3.0 | 8.0 ± 3.8 | 0.348 |
| Hip | |||
| Maximum hip extension in stance (°) | 9.3 ± 11.6 | 15.1 ± 10.3 | 0.050 |
| Maximum hip flexion in swing (°) | 46.4 ± 6.6 | 46.3 ± 9.8 | 0.955 |
| Knee | |||
| Maximum knee extension in stance (°) | 43.3 ± 13.5 | 47.7 ± 12.5 | 0.208 |
| Knee flexion at mid-stance (°) | 45.8 ± 15.0 | 50.4 ± 13.5 | 0.224 |
| Maximum knee flexion in swing (°) | 70.2 ± 8.8 | 69.7 ± 9.4 | 0.849 |
| Range of knee flexion (°) | 26.9 ± 9.5 | 22.0 ± 9.4 | 0.060 |
| Knee flexion at initial contact (°) | 51.0 ± 10.8 | 55.5 ± 9.9 | 0.109 |
| Ankle | |||
| Mean dorsiflexion in stance (°) | 10.9 ± 12.5 | 15.1 ± 13.3 | 0.223 |
| Maximum dorsiflexion in stance (°) | 19.8 ± 13.5 | 22.8 ± 13.0 | 0.404 |
| Mid-stance dorsiflexion (°) | 15.0 ± 12.4 | 18.4 ± 13.3 | 0.328 |
| Maximum plantarflexion in swing (°) | −10.1 ± 16.5 | −4.5 ± 18.9 | 0.235 |
| Maximum dorsiflexion in swing (°) | 8.2 ± 11.8 | 10.7 ± 14.1 | 0.465 |
| Mean foot progression angle (°) | 1.2 ± 19.11 | 12.9 ± 16.2 | 0.016 |
| Group 1 (n = 22) | Group 2 (n = 11) | p-Value | |
|---|---|---|---|
| Pelvis | |||
| Maximum pelvic tilt (°) | 20.0 ± 9.7 | 24.4 ± 10.3 | 0.255 |
| Average pelvic tilt (°) | 16.5 ± 9.9 | 21.4 ± 10.7 | 0.218 |
| Range of pelvic tilt (°) | 7.4 ± 2.4 | 6.3 ± 2.7 | 0.283 |
| Hip | |||
| Maximum hip extension in stance (°) | 9.5 ± 10.1 | 16.6 ± 9.7 | 0.057 |
| Maximum hip flexion in swing (°) | 45.0 ± 9.9 | 48.6 ± 7.4 | 0.299 |
| Knee | |||
| Maximum knee extension in stance (°) | 19.2 ± 15.9 | 16.1 ± 14.2 | 0.590 |
| Knee flexion at mid-stance (°) | 20.6 ± 16.6 | 19.1 ± 15.6 | 0.800 |
| Maximum knee flexion in swing (°) | 56.2 ± 12.1 | 55.5 ± 9.8 | 0.853 |
| Range of knee flexion (°) | 37.0 ± 10.4 | 39.3 ± 12.0 | 0.543 |
| Knee flexion at initial contact (°) | 32.8 ± 13.0 | 34.6 ± 7.7 | 0.676 |
| Ankle | |||
| Mean dorsiflexion in stance (°) | 5.9 ± 7.0 | 4.9 ± 6.1 | 0.688 |
| Maximum dorsiflexion in stance (°) | 13.1 ± 7.4 | 11.0 ± 7.2 | 0.407 |
| Mid-stance dorsiflexion (°) | 8.0 ± 7.6 | 7.1 ± 7.0 | 0.729 |
| Maximum plantarflexion in swing (°) | -6.2 ± 9.7 | -2.9 ± 7.5 | 0.303 |
| Maximum dorsiflexion in swing (°) | 6.4 ± 9.0 | 6.2 ± 7.6 | 0.940 |
| Mean foot progression angle (°) | 8.7± 10.6 | 8.7 ± 11.2 | 0.994 |
| Preoperative | Final Follow-Up | p-Value | |
|---|---|---|---|
| Hip extension moment (N∙m/Kg) | |||
| Maximum | 1.13 ± 0.46 | 0.91 ± 0.48 | 0.003 |
| Minimum (=maximum flexor moment) | −0.86 ± 0.36 | −0.62 ± 0.31 | <0.001 |
| Average | 0.21 ± 0.16 | 0.12 ± 0.17 | 0.794 |
| Knee extension moment (N∙m/Kg) | |||
| Maximum | 0.99 ± 0.41 | 0.56 ± 0.33 | <0.001 |
| Minimum (=maximum flexor moment) | −0.41 ± 0.49 | −0.37 ± 0.20 | 0.621 |
| Average | 0.28 ± 0.24 | 0.08 ± 0.19 | <0.001 |
| Ankle plantarflexion moment (N∙m/Kg) | |||
| Maximum | 1.15 ± 0.37 | 1.00 ± 0.36 | 0.043 |
| Minimum | −0.12 ± 0.31 | −0.06 ± 0.10 | 0.228 |
| Average | 0.43 ± 0.21 | 0.37 ± 0.15 | 0.151 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, H.; Park, B.K.; Park, K.-B.; Abdel-Baki, S.W.; Rhee, I.; Kim, C.W.; Kim, H.W. Distal Femoral Shortening Osteotomy for Severe Knee Flexion Contracture and Crouch Gait in Cerebral Palsy. J. Clin. Med. 2019, 8, 1354. https://doi.org/10.3390/jcm8091354
Park H, Park BK, Park K-B, Abdel-Baki SW, Rhee I, Kim CW, Kim HW. Distal Femoral Shortening Osteotomy for Severe Knee Flexion Contracture and Crouch Gait in Cerebral Palsy. Journal of Clinical Medicine. 2019; 8(9):1354. https://doi.org/10.3390/jcm8091354
Chicago/Turabian StylePark, Hoon, Byoung Kyu Park, Kun-Bo Park, Sharkawy Wagih Abdel-Baki, Isaac Rhee, Chan Woo Kim, and Hyun Woo Kim. 2019. "Distal Femoral Shortening Osteotomy for Severe Knee Flexion Contracture and Crouch Gait in Cerebral Palsy" Journal of Clinical Medicine 8, no. 9: 1354. https://doi.org/10.3390/jcm8091354
APA StylePark, H., Park, B. K., Park, K.-B., Abdel-Baki, S. W., Rhee, I., Kim, C. W., & Kim, H. W. (2019). Distal Femoral Shortening Osteotomy for Severe Knee Flexion Contracture and Crouch Gait in Cerebral Palsy. Journal of Clinical Medicine, 8(9), 1354. https://doi.org/10.3390/jcm8091354





