Oral Administration of Apigenin Inhibits Metastasis through AKT/P70S6K1/MMP-9 Pathway in Orthotopic Ovarian Tumor Model
Abstract
:1. Introduction
2. Results and Discussion
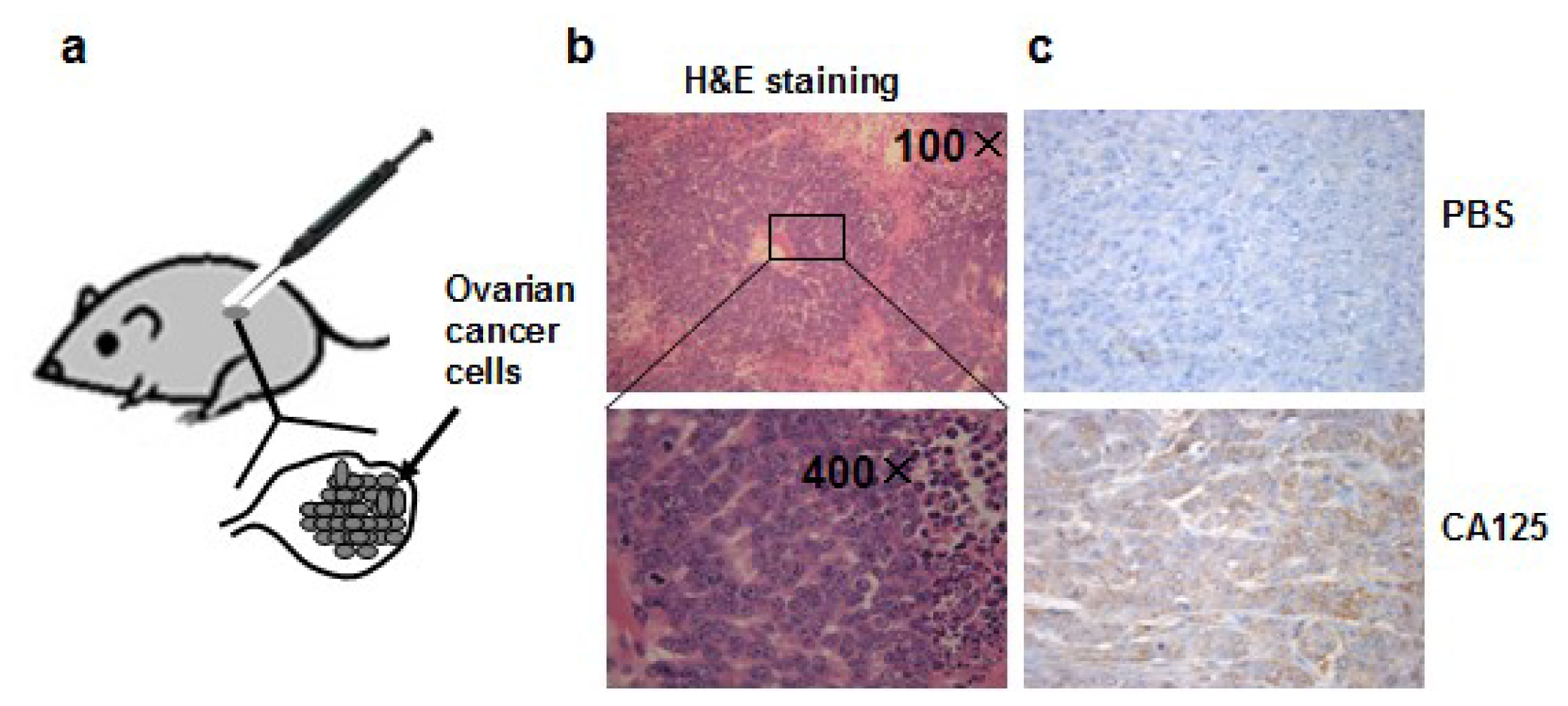
2.1. Establishment of the Orthotopic Ovarian Tumor Model in Nude Mice
2.2. Apigenin Did not Significantly Inhibit Tumor Growth, but Inhibited the Occurrence of Micrometastasis in the Small Intestine and Stomach
2.3. Apigenin Significantly Decreased the Number of Metastasis Cancer Cells Detected in Several Organs
2.4. Apigenin Inhibited OVCAR-3 Cell Migration and Invasion
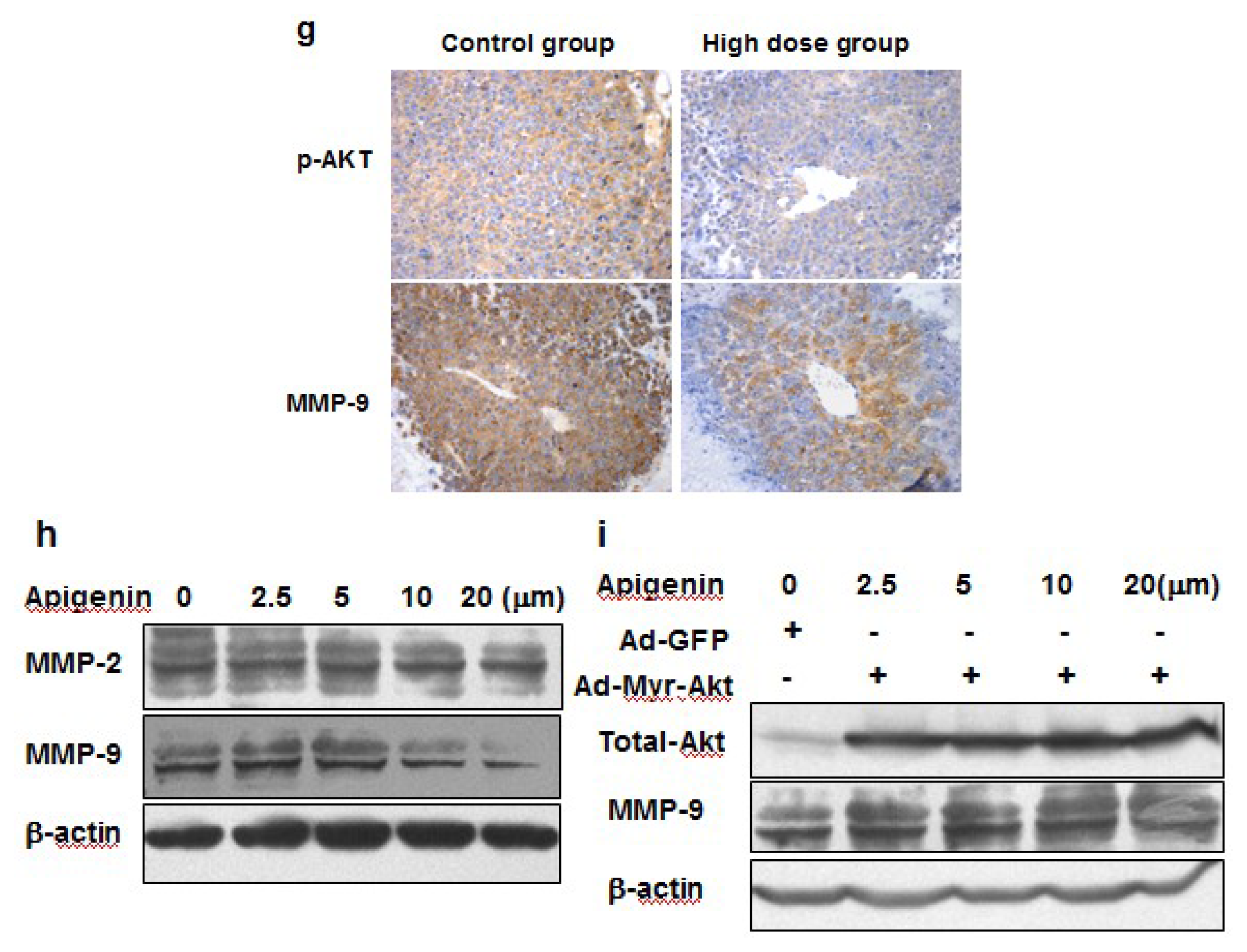
2.5. Apigenin Inhibited MMP-9 Expression through AKT/p70S6K1 Pathway
3. Materials and Methods
3.1. Chemicals and Antibodies
3.2. Animal Model and Treatment
3.3. Micrometastasis Assay Based on Genomic PCR for Alu Sequence
3.4. Immunoblotting
3.5. Immunohistochemistry Analysis
3.6. Cell Culture
3.7. Wound-Healing Assays
3.8. Matrigel Transwell Invasion Assay
3.9. Statistical Analysis
4. Conclusions
Acknowledgment
References
- Perez, R.P.; Godwin, A.K.; Hamilton, T.C.; Ozols, R.F. Ovarian cancer biology. Semin. Oncol 1991, 18, 186–204. [Google Scholar]
- Duthie, G.; Crozier, A. Plant-derived phenolic antioxidants. Curr. Opin. Clin. Nutr. Metab. Care 2000, 3, 447–451. [Google Scholar]
- Fang, J.; Xia, C.; Cao, Z.; Zheng, J.Z.; Reed, E.; Jiang, B.H. Apigenin inhibits VEGF and HIF-1 expression via PI3K/AKT/p70S6K1 and HDM2/p53 pathways. FASEB J 2005, 19, 342–353. [Google Scholar]
- Liu, L.Z.; Fang, J.; Zhou, Q.; Hu, X.; Shi, X.; Jiang, B.H. Apigenin inhibits expression of vascular endothelial growth factor and angiogenesis in human lung cancer cells: Implication of chemoprevention of lung cancer. Mol. Pharmacol 2005, 68, 635–643. [Google Scholar]
- Fang, J.; Zhou, Q.; Liu, L.Z.; Xia, C.; Hu, X.; Shi, X.; Jiang, B.H. Apigenin inhibits tumor angiogenesis through decreasing HIF-1alpha and VEGF expression. Carcinogenesis 2007, 28, 858–864. [Google Scholar]
- Shukla, S.; MacLennan, G.T.; Flask, C.A.; Fu, P.; Mishra, A; Resnick, M.I.; Gupta, S. Blockade of β-catenin signaling by plant flavonoid apigenin suppresses prostate carcinogenesis in TRAMP mice. Cancer Res 2007, 67, 6925–6935. [Google Scholar]
- Yin, F.; Giuliano, A.E.; Law, R.E.; van Herle, A.J. Apigenin inhibits growth and induces G2/M arrest by modulating cyclin-CDK regulators and ERK MAP kinase activation in breast carcinoma cells. Anticancer Res 2001, 21, 413–420. [Google Scholar]
- Lee, W.J.; Chen, W.K.; Wang, C.J.; Lin, W.L.; Tseng, T.H. Apigenin inhibits HGF-promoted invasive growth and metastasis involving blocking PI3K/AKT pathway and β4 integrin function in MDA-MB-231 breast cancer cells. Toxicol. Appl. Pharmacol 2008, 226, 178–191. [Google Scholar]
- Michigami, T.; Watanabe, M.I.; Yamazaki, M.; Ozono, K. Receptor activator of nuclear factor κB ligand (RANKL) is a key molecule of osteoclast formation for bone metastasis in a newly developed model of human neuroblastoma1. Cancer Res 2001, 61, 1637–1644. [Google Scholar]
- Meng, Q.; Xia, C.; Fang, J.; Rojanasakul, Y.; Jiang, B.H. Role of PI3K and AKT specific isoforms in ovarian cancer cell migration, invasion and proliferation through the p70S6K1 pathway. Cell Signal 2006, 18, 2262–2271. [Google Scholar]
- Liu, L.; Fang, J.; Zhou, Q.; Hu, X.; Shi, X.; Jiang, B.H. Apigenin inhibits VEGF expression and angiogenesis in human lung cancer cells: Implication of chemoprevention of lung cancer. Mol. Pharmacol 2005, 68, 635–643. [Google Scholar]
- Franzen, C.A.; Amargo, E.; Todorović, V.; Desai, B.V.; Huda, S.; Mirzoeva, S.; Chiu, K.; Grzybowski, B.A.; Chew, T.L.; Green, K.J.; Pelling, J.C. The chemopreventive bioflavonoid apigenin inhibits prostate cancer cell motility through the focal adhesion kinase/Src signaling mechanism. Cancer Prev. Res. (Phila) 2009, 2, 830–841. [Google Scholar]
- Furmaga, W.B.; Ryan, J.L.; Coleman, W.B.; Cole, S.R.; Tsongalis, G.J. Alu profiling of primary and metastatic nonsmall cell lung cancer. Exp. Mol. Pathol 2003, 74, 224–229. [Google Scholar]
- Khasigov, P.Z.; Podobed, O.V.; Gracheva, T.S.; Salbiev, K.D.; Grachev, S.V.; Berezov, T.T. Role of matrix metalloproteinases and their inhibitors in tumor invasion and metastasis. Biochemistry 2003, 68, 711–717. [Google Scholar]
- Kenny, H.A.; Kaur, S.; Coussens, L.M.; Lengyel, E. The initial steps of ovarian cancer cell metastasis are mediated by MMP-2 cleavage of vitronectin and fibronectin. J. Clin. Invest 2008, 118, 1367–1379. [Google Scholar]
- Nelson, A.R.; Fingleton, B.; Rothenberg, M.L.; Matrisian, L.M. Matrix metalloproteinases: Biologic activity and clinical implications. J. Clin. Oncol 2000, 18, 1135–1149. [Google Scholar]
- Liotta, L.; Abe, S.; Robey, P.; Martin, G. Preferential digestion of basement membrane collagen by an enzyme derived from a metastatic murine tumor. Proc. Natl. Acad. Sci. USA 1979, 76, 2268–2272. [Google Scholar]
- Chantrain, C.F.; Shimada, H.; Jodele, S.; Groshen, S.; Ye, W.; Shalinsky, D.R.; Werb, Z.; Coussens, L.M.; DeClerck, Y.A. Stromal matrix metalloproteinase-9 regulates the vascular architecture in neuroblastoma by promoting pericyte recruitment. Cancer Res 2004, 64, 1675–1686. [Google Scholar]
- Thant, A.A.; Nawa, A.; Kikkawa, F.; Ichigotani, Y.; Zhang, Y.; Sein, T.T.; Amin, A.R.; Hamaguchi, M. Fibronectin activates matrix metalloproteinase-9 secretion via the MEK1-MAPK and the PI3K-AKT pathways in ovarian cancer cells. Clin. Exp. Metastasis 2001, 18, 423–428. [Google Scholar]
- Walker, J.A.; Kilroy, G.E.; Xing, J.; Shewale, J.; Sinha, S.K.; Batzer, M.A. Human DNA quantitation using Alu element-based polymerase chain reaction. Anal. Biochem 2003, 315, 122–128. [Google Scholar]
- Kenny, H.A.; Kaur, S.; Coussens, L.M.; Lengyel, E. The initial steps of ovarian cancer cell metastasis are mediated by MMP-2 cleavage of vitronectin and fibronectin. J. Clin. Investig 2008, 118, 1367–1379. [Google Scholar]





| Group | Lung | Small intestine | Liver | Stomach |
|---|---|---|---|---|
| Control | 4/10 | 7/10 | 7/10 | 6/10 |
| Low dose (75 mg/kg) | 3/10 | 5/10 | 6/10 | 2/10 * |
| High dose (150 mg/kg) | 3/10 | 3/10 * | 5/10 | 3/10 * |
© 2012 by the authors; licensee Molecular Diversity Preservation International, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
He, J.; Xu, Q.; Wang, M.; Li, C.; Qian, X.; Shi, Z.; Liu, L.-Z.; Jiang, B.-H. Oral Administration of Apigenin Inhibits Metastasis through AKT/P70S6K1/MMP-9 Pathway in Orthotopic Ovarian Tumor Model. Int. J. Mol. Sci. 2012, 13, 7271-7282. https://doi.org/10.3390/ijms13067271
He J, Xu Q, Wang M, Li C, Qian X, Shi Z, Liu L-Z, Jiang B-H. Oral Administration of Apigenin Inhibits Metastasis through AKT/P70S6K1/MMP-9 Pathway in Orthotopic Ovarian Tumor Model. International Journal of Molecular Sciences. 2012; 13(6):7271-7282. https://doi.org/10.3390/ijms13067271
Chicago/Turabian StyleHe, Jun, Qing Xu, Min Wang, Chongyong Li, Xu Qian, Zhumei Shi, Ling-Zhi Liu, and Bing-Hua Jiang. 2012. "Oral Administration of Apigenin Inhibits Metastasis through AKT/P70S6K1/MMP-9 Pathway in Orthotopic Ovarian Tumor Model" International Journal of Molecular Sciences 13, no. 6: 7271-7282. https://doi.org/10.3390/ijms13067271
APA StyleHe, J., Xu, Q., Wang, M., Li, C., Qian, X., Shi, Z., Liu, L.-Z., & Jiang, B.-H. (2012). Oral Administration of Apigenin Inhibits Metastasis through AKT/P70S6K1/MMP-9 Pathway in Orthotopic Ovarian Tumor Model. International Journal of Molecular Sciences, 13(6), 7271-7282. https://doi.org/10.3390/ijms13067271




