Abstract
Study Design: Very few studies exist regarding the fracture pattern variability of the zygomaticoorbital (ZMO) complex. The retrospective evaluation of a large series of surgically treated unilateral ZMO fractures would in certain circumstances help intraoperative predictability and define sensitive indicators for open reduction and internal fixation. Objective: The aim of this study was to investigate the different fracture patterns after ZMO complex injury regarding the 5 anatomic sutures of the zygoma as well as the concomitance of the paranasal buttress and maxillary sinus wall fracture. Methods: The medical records of all patients with unilateral ZMO fractures who underwent surgical intervention in a single trauma center department between April 2015 and June 2020 were retrospectively reviewed. Demographic and anamnesis data, radiologic findings, and surgical reports were evaluated. According to the preoperative radiologic evaluation, ZMO fractures were classified as unisutural, bisutural, trisutural, tetrasutural, and complete based on the number of zygomatic sutures. The prevalence of various fracture patterns was analyzed. The impact of patient’s age and trauma etiology on the fracture pattern was evaluated using descriptive statistical analysis. Results: The study included 492 patients with unilateral ZMO fractures, with a mean age of 49.93 years (SD = 20.66) and a male:female ratio of 2.23:1. The most affected age group was 19–44 years (41.67%) and tripping falls were the most common etiology (27.24%). Trisutural (57.32%) and unisutural fractures (23.17%) were the most common, followed by tetrasutural (8.94%), bisutural (8.54%), and complete fractures (2.03%). A trisutural fracture involving the zygomaticomaxillary suture, the infraorbital rim, and the zygomaticosphenoidal suture was the most common fracture pattern (52.03%). Most fractures were observed in the zygomaticosphenoidal suture (86.99%), followed by the infraorbital rim (74.59%) and the zygomaticomaxillary suture (68.29%). Fractures of the maxillary sinus wall and the paranasal buttress co-existed in 9.55% and 31.30% of all cases, respectively. No correlation was detected between age and fracture pattern (P = .4111). Tripping falls and bicycle accidents significantly influenced the fracture pattern (P < .0001). Conclusions: According to the results, knowledge of the fracture pattern variability of the ZMO complex could in certain circumstances designate CT or CBCT as mandatory before operating on ZMO fractures. Consequently, unnecessary incisions could be avoided. The high concomitance of paranasal buttress fracture also suggests its intraoperative surgical exploration. Further studies should correlate the clinical findings with indication for surgery and postoperative outcome for the different fracture patterns described.
Introduction
Fractures of the zygoma are among the most common fractures evaluated at level I trauma centers with varying causes and severity [1,2,3]. Zygomaticoorbital (ZMO) fractures have diverse patterns, and a standardized classification has not been established. The classical fracture patterns described by Le Fort in 1901 are rare today and common fracture line combinations may guide the diagnostic process [4].
A ZMO fracture occurs with single fracture lines passing through one or several of the abovementioned anatomic sutures. A complete “en bloc” fracture of the zygoma requires discontinuance of all 5 anatomic sutures, which is uncommon in clinical practice. It is important to understand that every ZMO fracture includes an orbital fracture in at least 70% of the cases since the zygoma forms the lateral part of the inferior orbital wall [5,6,7,8,9].
Several fracture classifications have been proposed in the international literature trying to improve clinical relevance and interpersonal communication [10]. The AO Foundation has established a 3-level classification system based on CT-confirmed fracture lines. This system describes the exact fracture location within defined regions in the central and lateral midface with reference to classic Le Fort fractures and their analogs [4,11]. However, since ZMO fractures do not always occur across the buttress-related sutures and are frequently diagnosed in combination with classic Le Fort fractures, a lack of research exists regarding the concomitance of paranasal buttress fracture as Le Fort I fracture component along with zygoma fractures. This knowledge would help improve accuracy in diagnosis and treatment especially when 3D imaging is not available.
This study aimed to evaluate the different fracture patterns after ZMO injury regarding the 5 anatomic sutures of the zygoma as well as the concomitance of the paranasal buttress and maxillary sinus wall fracture.
Material and Methods
Patient Collection
For this retrospective cohort study, medical records of all patients with midface trauma who were referred to a single trauma centre between April 2015 and June 2020 were reviewed using the hospital electronic database. Ethical approval for this study was obtained from the ethics committee of the chamber of physicians in Rhineland-Palatine, Mainz, Germany (approval number: 2018-13524). This study was performed in accordance with the Declaration of Helsinki 1964 and its later amendments [12]. Patients of any age range who underwent surgery to repair a unilateral ZMO fracture after clinical and radio-graphic diagnosis at this hospital were eligible for inclusion.
Exclusion criteria were (1) patients with ZMO fractures who were treated conservatively, (2) patients with bilateral midface fractures, (3) patients with isolated fractures of the orbital medial wall, maxillary sinus wall, nasal skeleton, or nasoethmoidal complex, and (4) patients with incomplete medical charts.
A board certified oral and maxillofacial surgeon indicated surgical treatment according to following clinical and radiological features: extensive fracture dislocation, diplopia, enopthalmos, cosmetic deformity with depression of the malar eminence, facial widening, malocclusion, reduced mouth opening, and neurosensory disturbances of the infraorbital nerve. The benefit of surgical treatment was also evaluated considering the patient’s age and general medical condition.
Data Collection
The study variables were obtained by reviewing patients’ charts, demographic and anamnesis data, radiologic findings, and surgical reports. Patients were anonymized prior to data analysis. The following preoperative and postoperative variables were analyzed:
Demographics
- Patients’ age and gender
Using the World Health Organization classification (2010), patients were divided into 5 age groups: children (≤12 years), adolescents (13–18 years), young adults (19–44 years), middle-aged (45–60 years), and elderly (>60 years).
Injury details
- Etiology of trauma
Injury causes were classified into 13 types: tripping fall, interpersonal violence, bicycle accident, work accident, syncope-related fall, road traffic accident, sport injury, stair fall, alcohol-related fall, epilepsy-related fall, suicide-related fall, animal-related accident, and other.
- Fracture laterality (right/left side)
- Fracture location according to the anatomic sutures of the zygoma
- Radiologic involvement of maxillary sinus wall and paranasal buttress fractures.
Patterns of ZMO Fractures Regarding the Anatomic Sutures of the Zygoma
Zygomaticoorbital fracture was diagnosed in all patients on the same day of initial assessment by a cone beam computer tomography and/or conventional CT scan if brain injury was suspected. Accompanying injuries associated with maxillofacial trauma such as traumatic brain and orthopedic injury or facial soft tissue alterations were documented but not analyzed in this study.
Zygomaticoorbital fractures were divided into the following patterns:
- Unisutural fracture (isolated fracture of a single anatomic suture of the zygoma):
- -
- Zygomaticomaxillary suture (ZM)
- -
- Infraorbital rim (IOR)
- -
- Zygomaticofrontal suture (ZF)
- -
- Zygomaticosphenoidal suture (ZS)—the anterolateral orbital floor
- -
- Zygomaticotemporal suture (ZT)
- Bisutural fracture with the following fracture line combinations:
- -
- ZM suture + IOR
- -
- ZM suture + ZS suture
- -
- IOR + ZF suture
- -
- IOR + ZS suture
- -
- ZF suture + ZS suture
- Trisutural fracture with the following fracture line combinations:
- -
- ZM suture + IOR + ZS suture
- -
- ZM suture + ZF suture + ZS suture
- -
- ZM suture + IOR + ZT
- -
- IOR + ZF suture + ZS suture
- -
- IOR + ZF suture + ZT
- -
- IOR + ZS suture + ZT
- Tetrasutural fracture with the following fracture line combinations:
- -
- ZM suture + IOR + ZF suture + ZS suture
- -
- ZM suture + IOR + ZS suture + ZT
- -
- IOR + ZF suture + ZS suture + ZT
- Complete ZMO fracture involving all 5 anatomic sutures of the zygoma:
- -
- ZM suture + IOR + ZF suture + ZS suture + ZT
Different fracture patterns are demonstrated in Figure 1, Figure 2, Figure 3, Figure 4, Figure 5 and Figure 6.
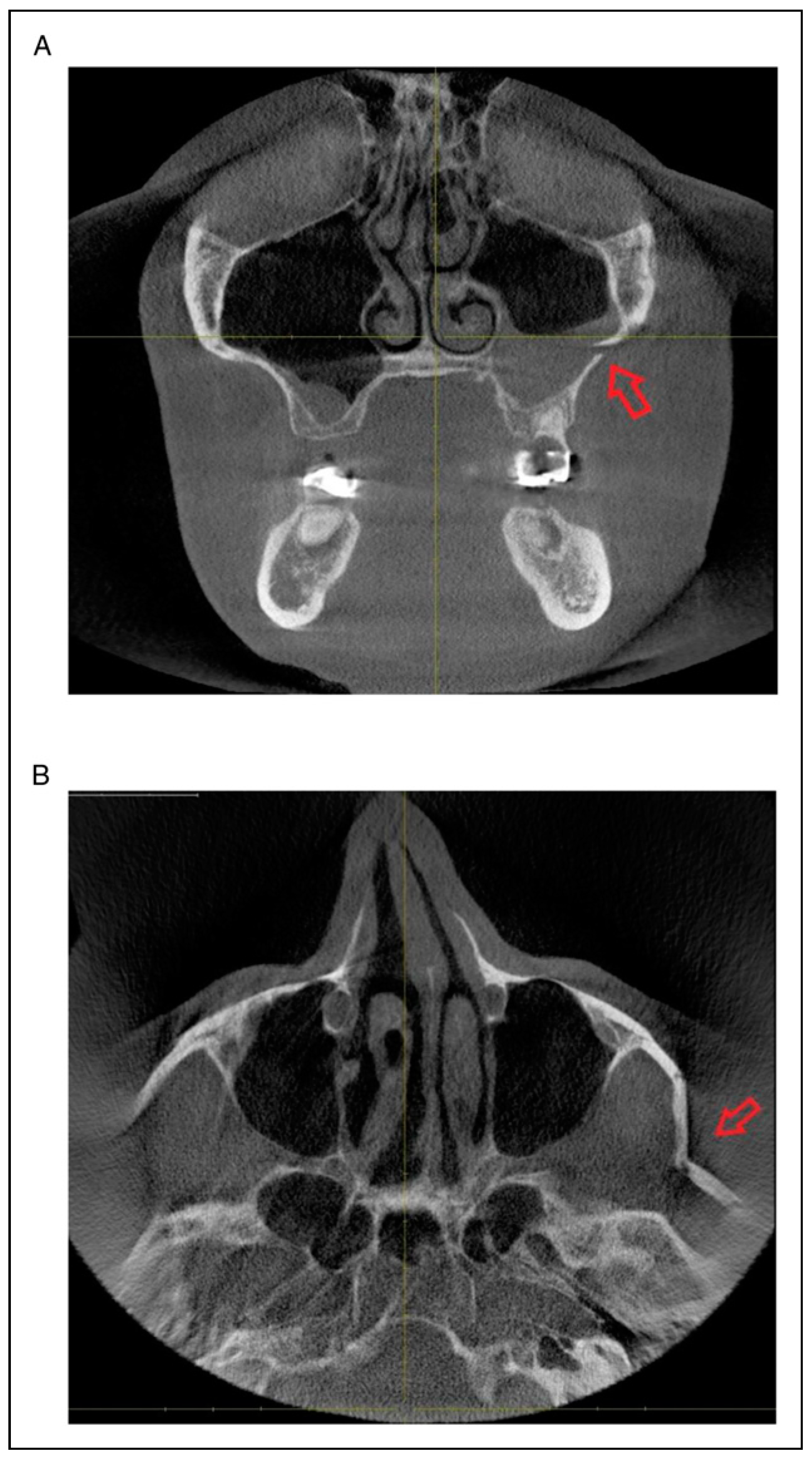
Figure 1.
(A) Unisutural ZMO complex fracture regarding the left zygomaticomaxillary suture, (B) Unisutural ZMO complex fracture regarding the left zygomatic arch (zygomaticotemporal suture).
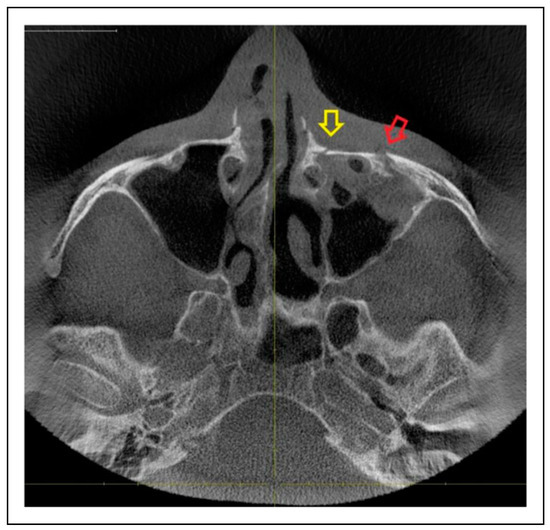
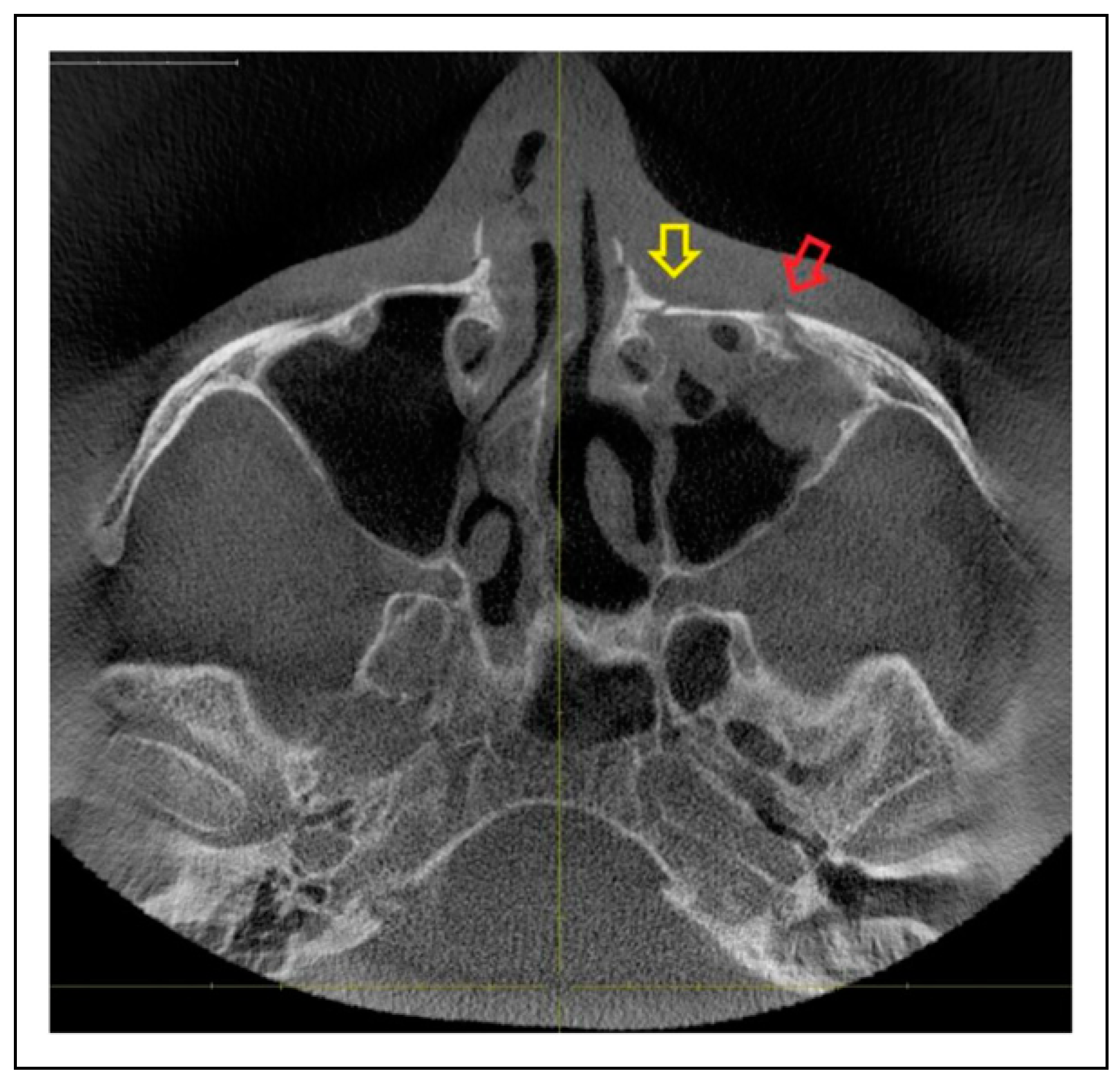
Figure 2.
Bisutural ZMO complex fracture regarding the left infraorbital rim (red arrow) and paranasal buttress (yellow arrow).
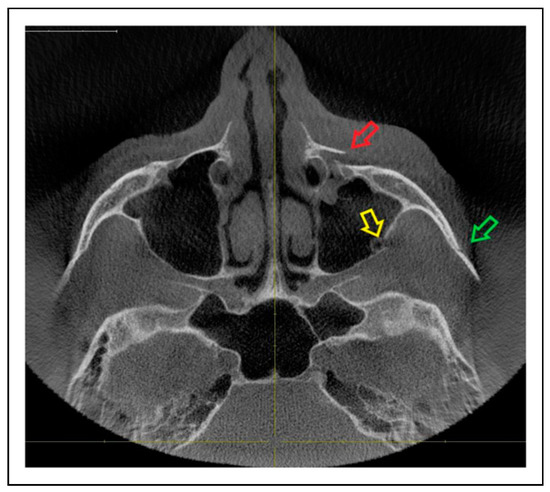
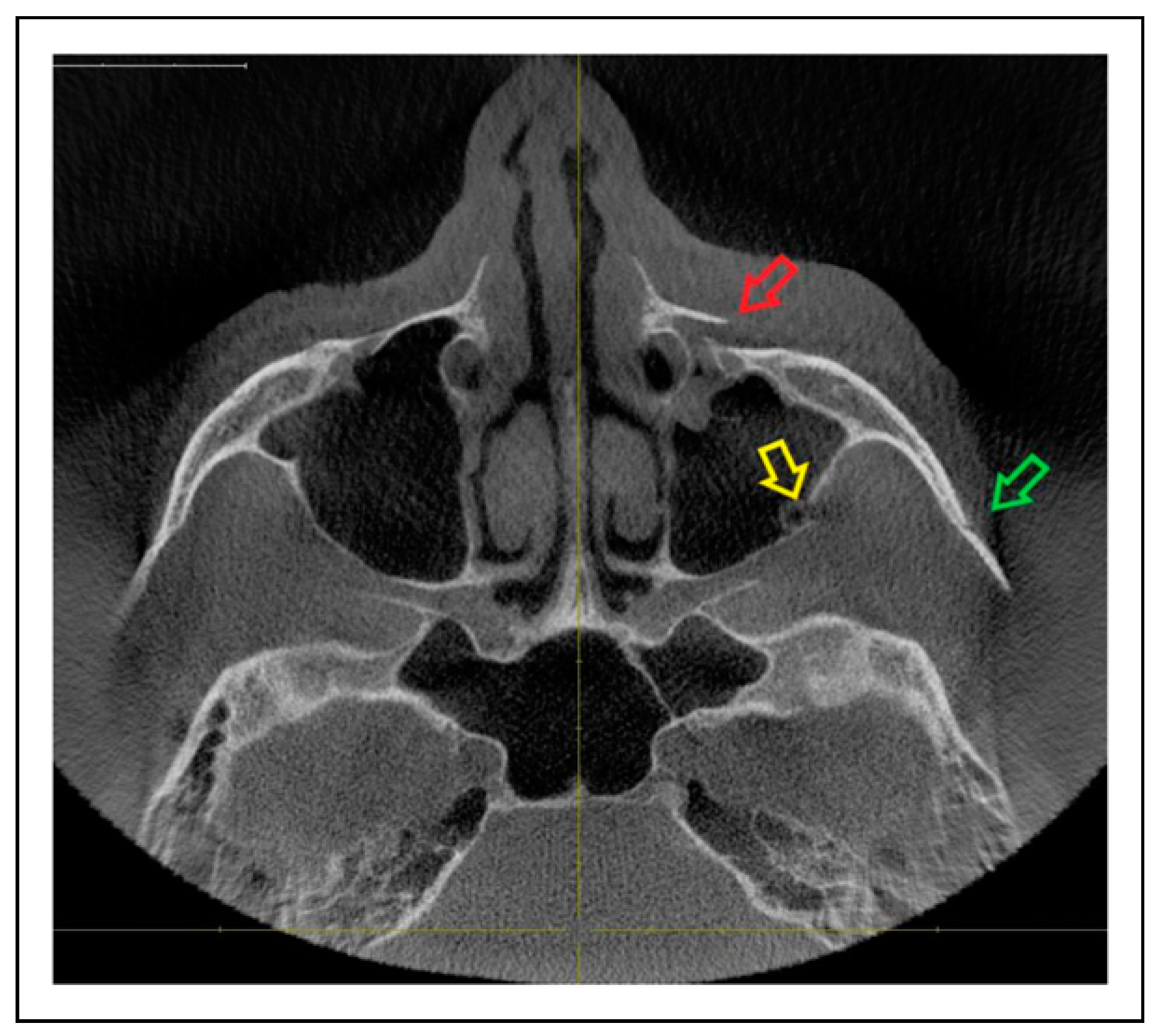
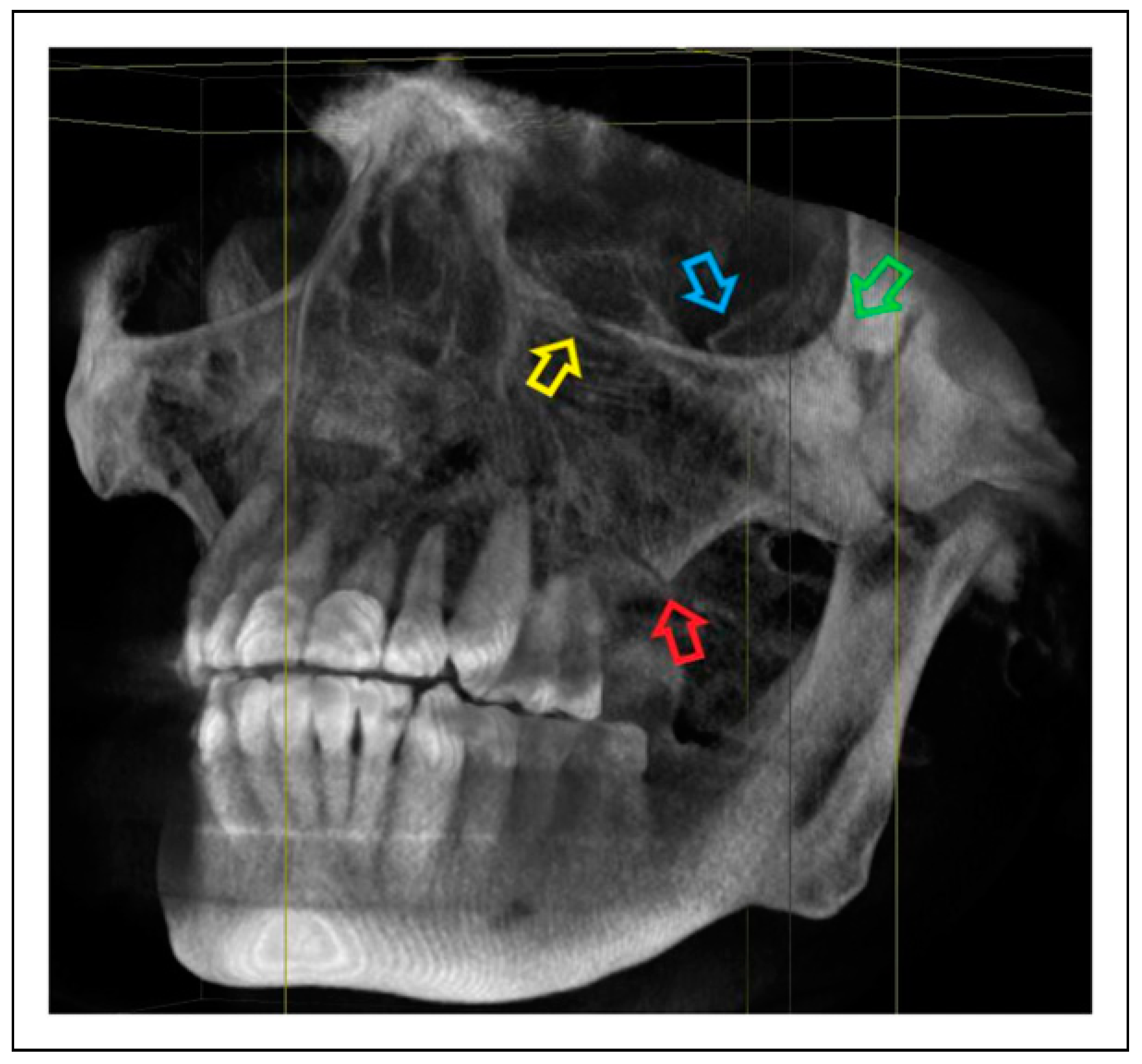
Figure 3.
Trisutural ZMO complex fracture regarding the left infraorbital rim (red arrow), zygomaticosphenoidal suture (yellow arrow) and zygomaticotemporal suture arch (green arrow).
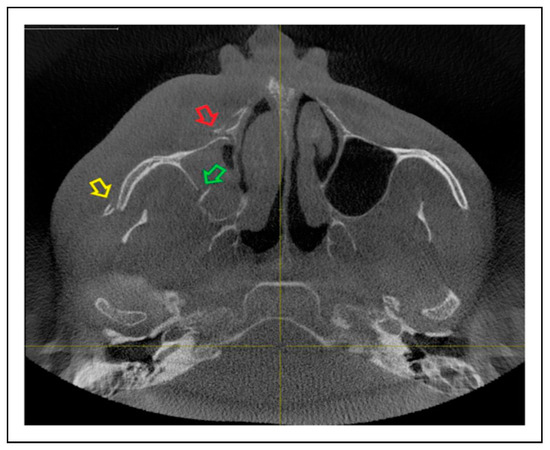
Figure 4.
Trisutural ZMO complex fracture regarding the right paranasal buttress (red arrow), zygomaticosphenoidal suture (green arrow) and zygomaticotemporal suture (yellow arrow).
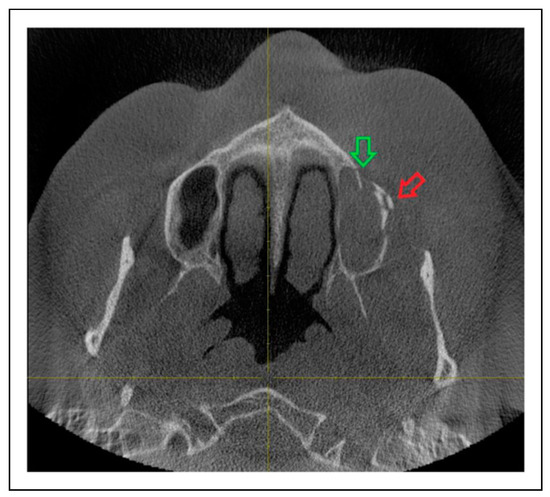
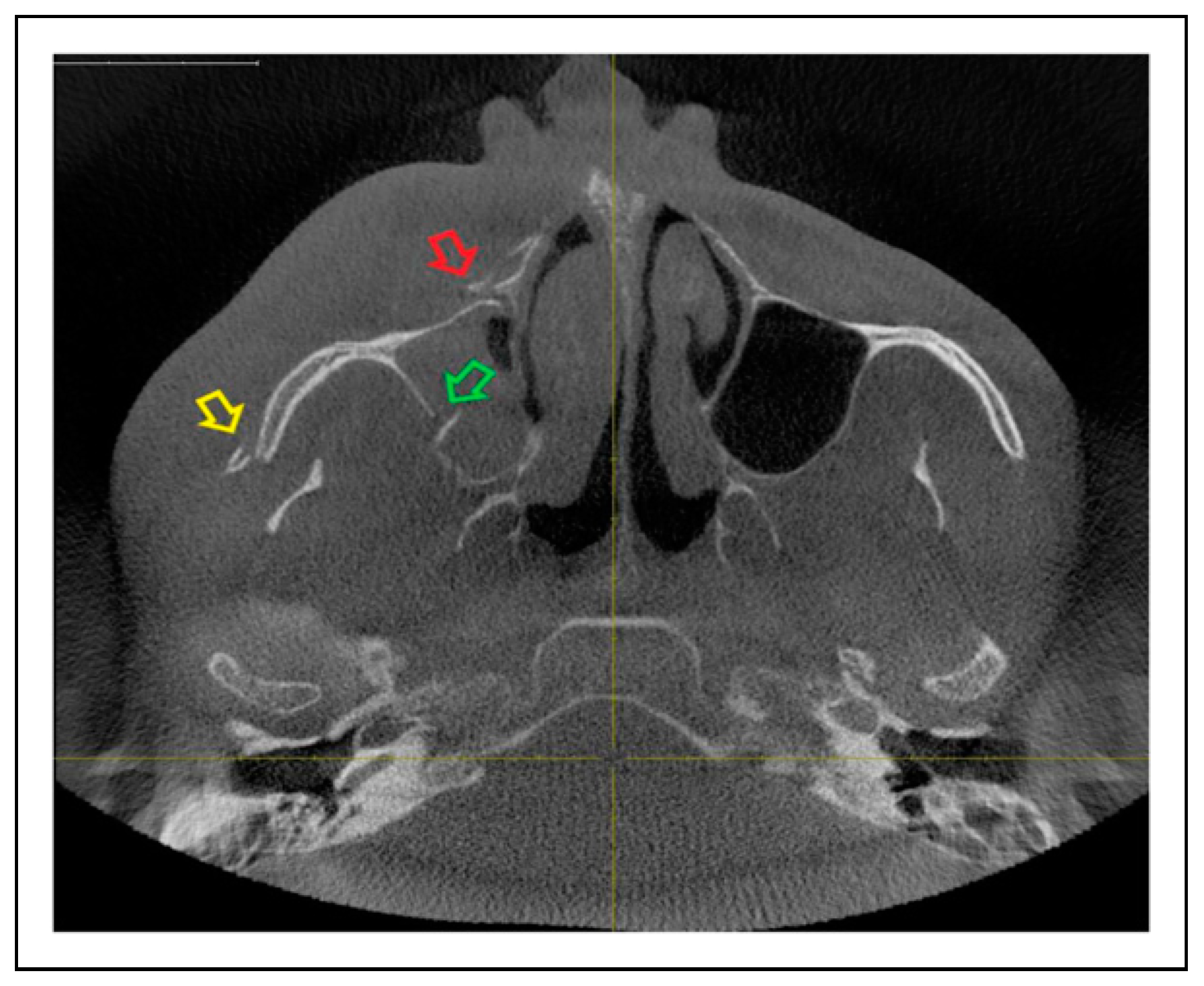
Figure 5.
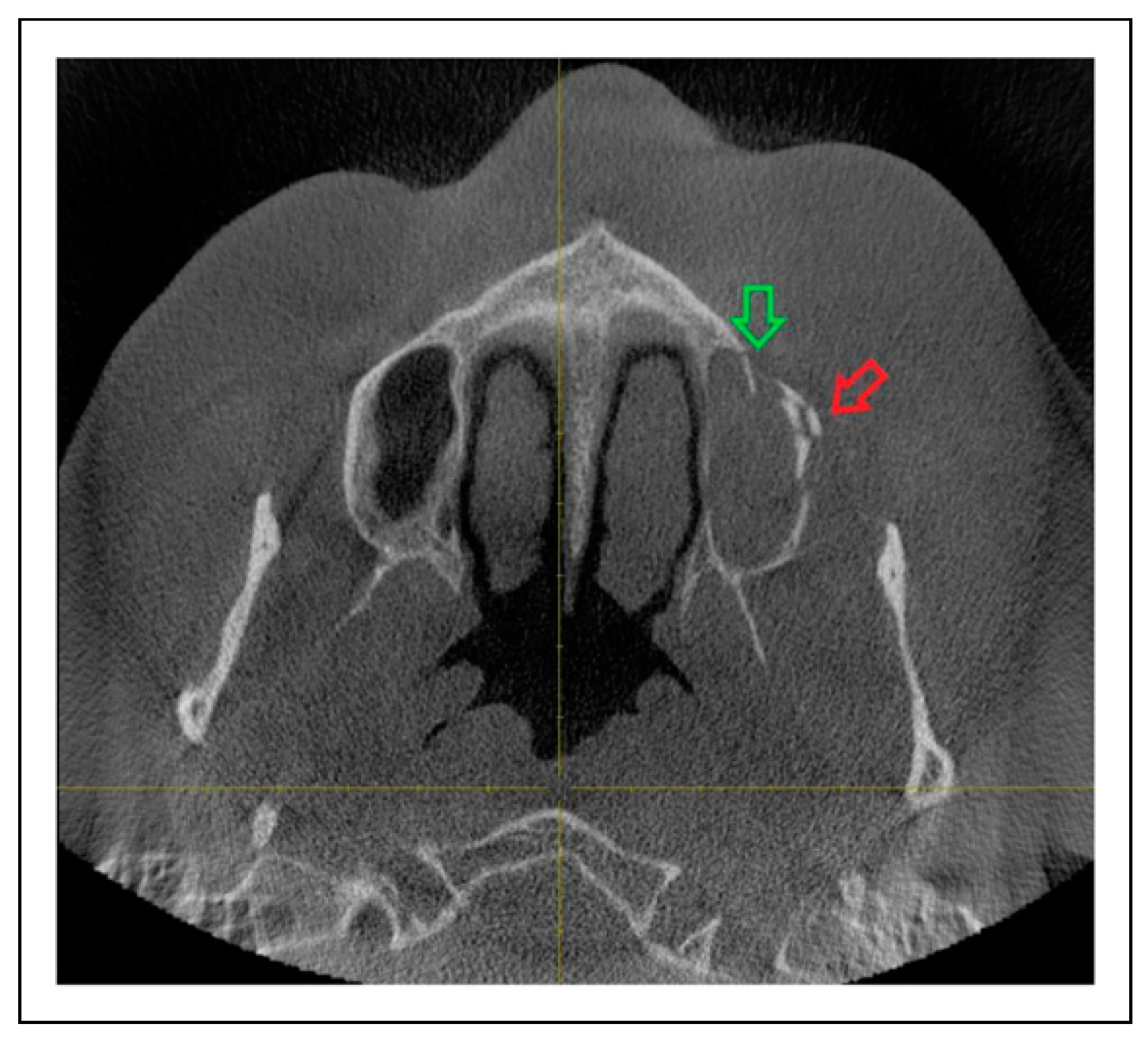
Bisutural ZMO complex fracture regarding the left zygomaticomaxillary suture (red arrow) and maxillary sinus wall (green arrow).
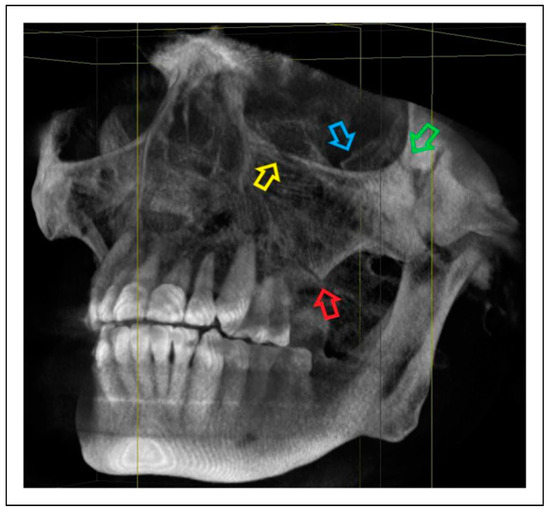
Figure 6.
Tetrasutural ZMO complex fracture regarding the left zygomaticomaxillary suture (red arrow), infraorbital rim (yellow arrow), zygomaticofrontal suture (green arrow) and zygomaticosphenoidal suture (blue arrow).
Surgical Treatment
Zygomaticoorbital fractures were surgically treated under general anesthesia with oral or nasotracheal intubation. Surgeries were performed by different surgeons with different levels of surgical experience. Fracture reduction and osteosynthesis were performed following a top-down outside-in sequence in most cases. The infraorbital rim and orbita floor fractures were approached via various surgical incisions. Allogenic polydioxanone membranes (PDSTMPlate, ETHICON®, Johnson & Johnson International, Norderstedt, Germany) or titanium mesh implants (Orbita Mesh, KLS Martin Group, Tuttlingen, Germany) were used to stabilize and reconstruct the orbita floor depending on the fracture displacement grade. Fractured buttresses were approached for reduction and osteosynthesis as previously described [7].
Statistical Analysis
Data were centralized in electronic format using Microsoft Excel software and analyzed descriptively with a two decimal percentage accuracy. Statistical processing was performed using the SAS®, Release 9.4 (SAS Institute Inc., Cary NC, USA). Metric data were expressed as mean and standard deviation, while nominal data were expressed as frequency and percentage. The frequencies of a nominal variable among the categories of another nominal variable were compared using chi-square tests. Binomial tests were performed to evaluate the null hypothesis when two categories were equally likely to occur. To evaluate correlations between the different age groups and fracture patterns, Spearman’s correlation coefficient and Kruskal–Wallis tests were performed. Fisher’s exact tests, Kruskal–Wallis tests and trend-tests were used to detect associations between fracture etiology and fracture patterns. A P value <.05 was considered statistically significant.
Results
Demographic Distribution
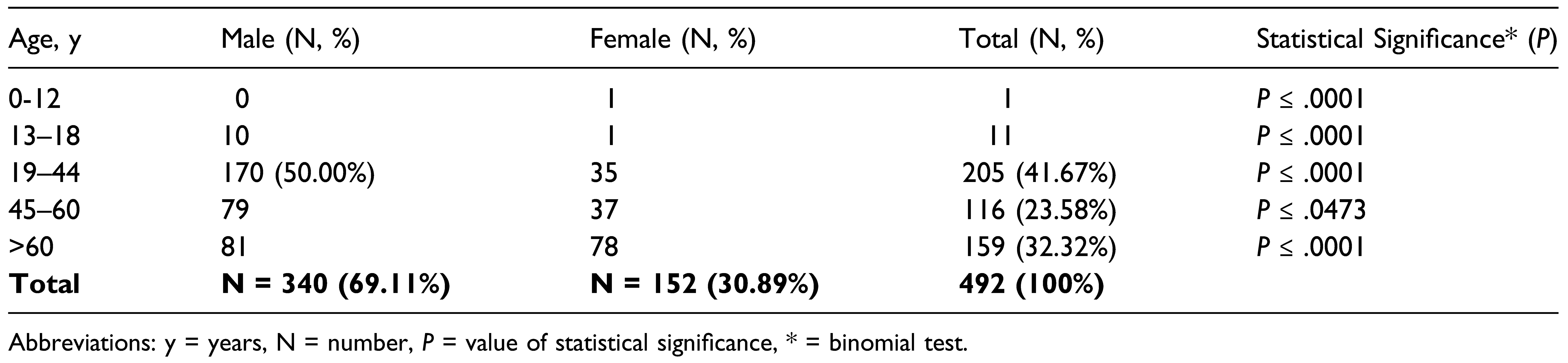
This retrospective study included 492 patients with unilateral ZMO fractures. There were significantly more males (n = 340; 69.11%) than females (n = 152; 30.89%) (P ≤ .0001; male to female ratio = 2.23:1). Patient age at the time of injury ranged from 8 to 96 years, with a mean age of 49.93 years (SD = 20.66). The ZMO was fractured on the left side in 261 patients (53.05%) and on the right side in 231 (46.95%) patients.
Zygomaticoorbital fractures were most frequent in the 19–44-year age group (n = 205; 41.67%), followed by the >60-year age group (n = 159; 32.32%), and 45-60-year age group (n = 116; 23.58%). Fracture prevalence was lowest in the 12 ≤ years old group (P < .0001). Significantly more males than females were affected in all age groups, except ≤12 years. Most female patients were 19-44 years old (23.03%), 45–60 years old (24.34%), or >60 years old (51.32%). The null hypothesis that fracture prevalence was equal among age groups was rejected, since significant differences were detected between the groups. Table 1 shows the age and gender distribution in this cohort.

Table 1.
Demographic Distribution of Unilateral Zygomaticoorbital Complex Fractures Regarding Patient’s Age and Gender (N = 492).
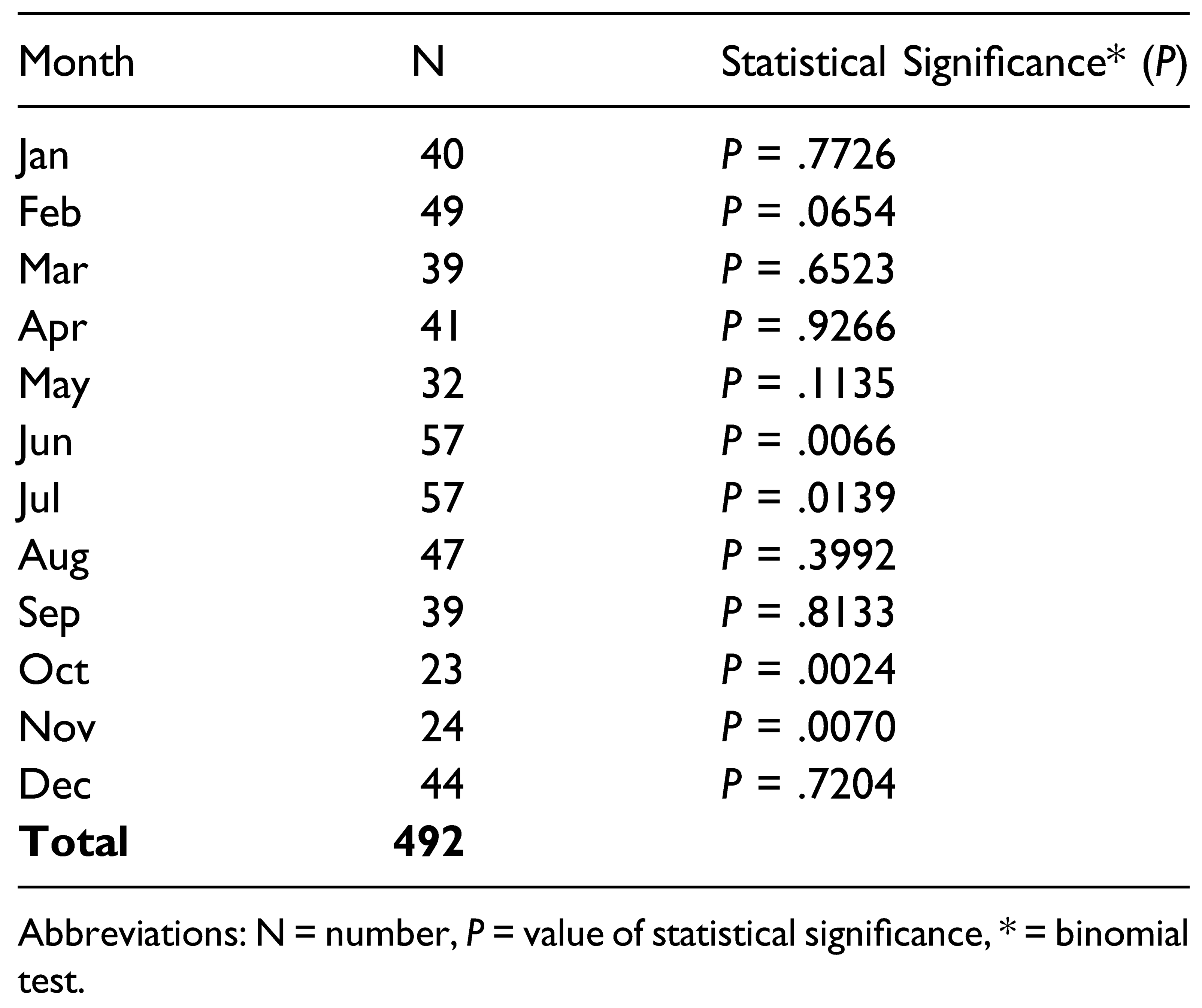
Table 2 presents the monthly prevalence of ZMO fractures. Binomial tests revealed a significantly higher fracture prevalence in June (P = .0066) and July (P = .0139) and a significantly lower prevalence in October (P = .0024) and November (P = .0070).

Table 2.
Monthly Prevalence of Unilateral Zygomaticoorbital Complex Fractures (N = 492).
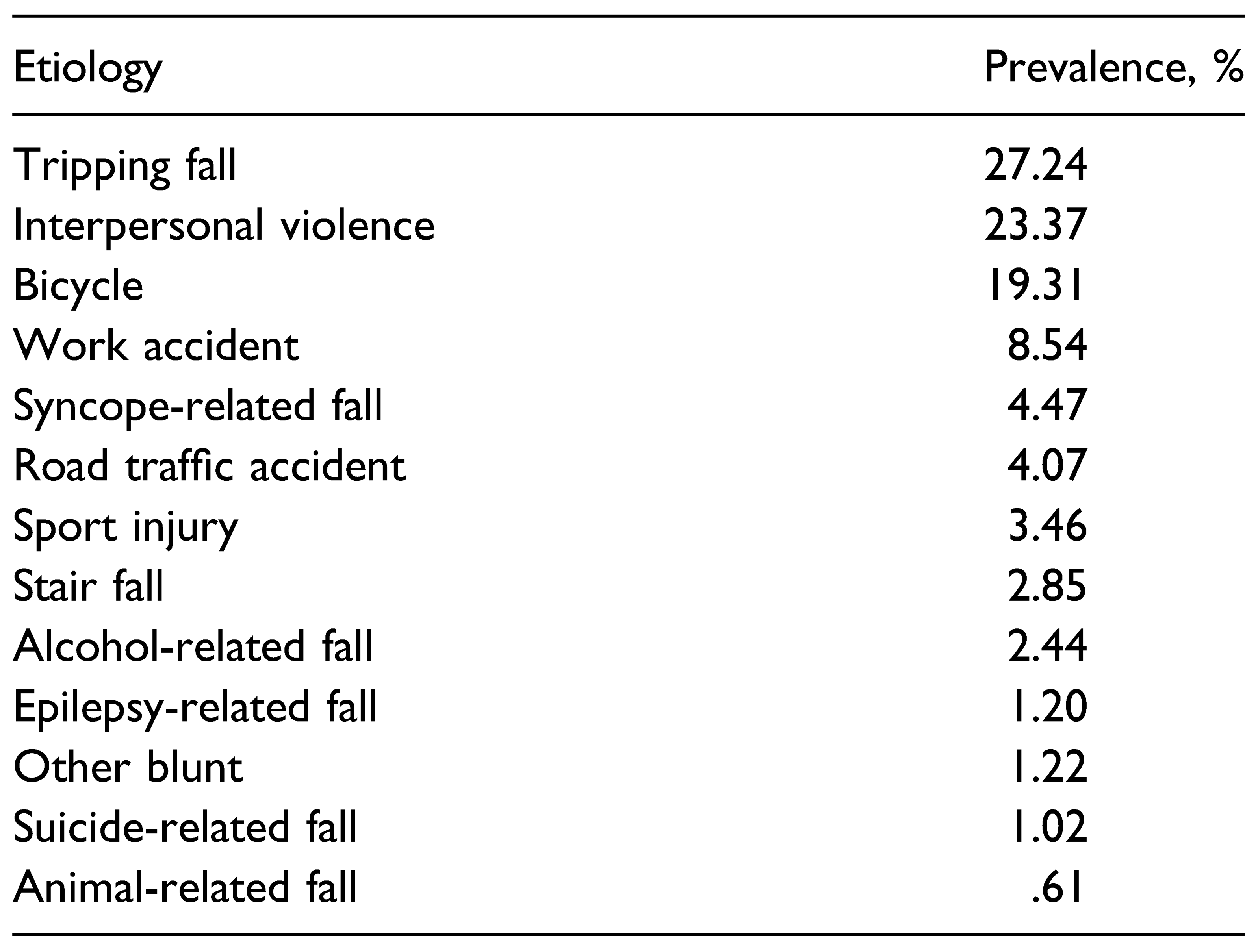
Trauma Etiology
Tripping fall was the most common cause of ZMO fractures (n = 134; 27.24%) followed by interpersonal violence (n = 115; 23.37%) and bicycle accidents (n = 95) (Table 3). Trauma etiology also contributed to the fracture prevalence according to binomial tests (P=<.0001), except for work accidents (P = .4822).

Table 3.
Distribution of Etiology of Zygomaticoorbital Complex Trauma in Our Collective (%).
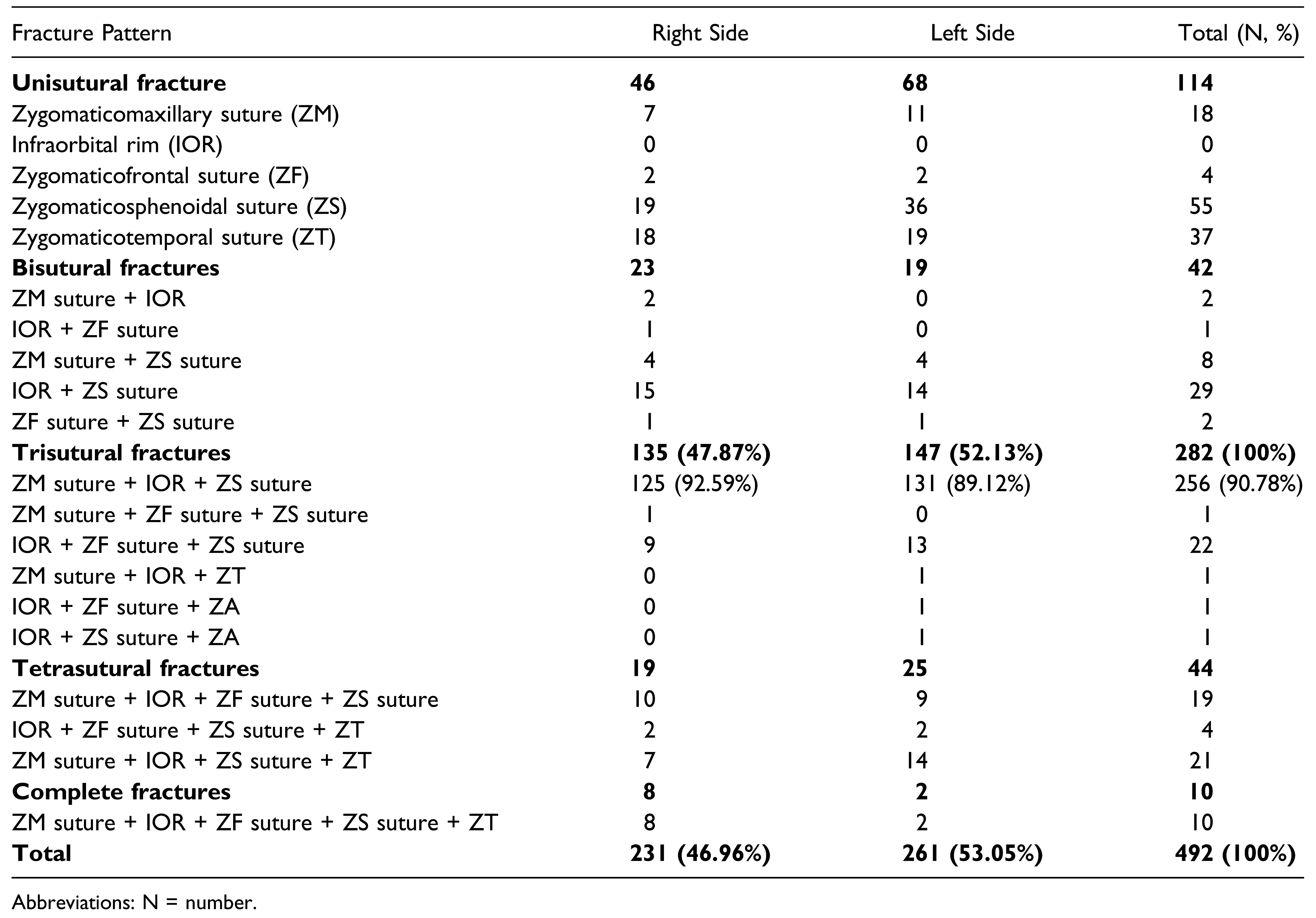
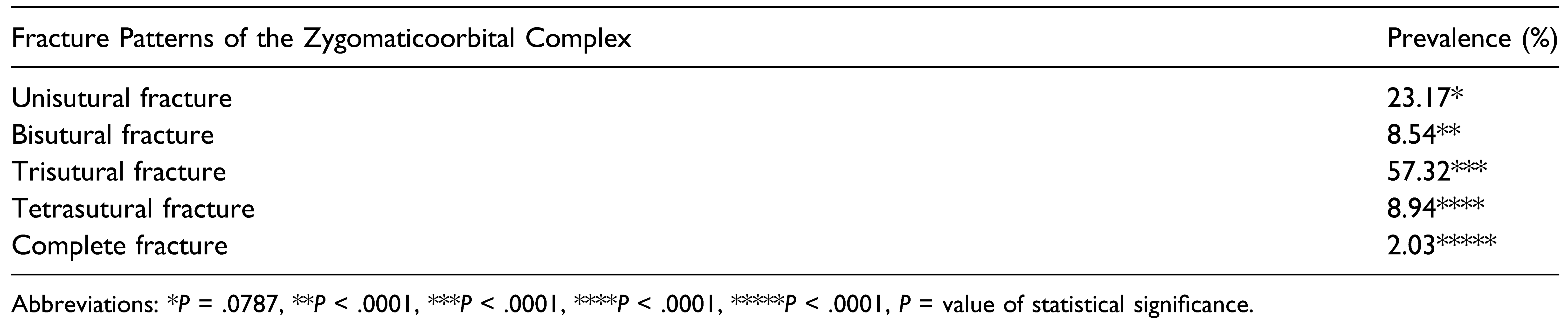
Patterns of ZMO Fractures Regarding the Anatomic Sutures of the Zygoma
Zygomaticoorbital fracture patterns revealed in preoperative radiographic diagnosis are presented in Table 4. Of the 492 surgically treated ZMO fractures, 282 were trisutural fractures (57.32%), 114 were unisutural fractures (23.17%), 44 were tetrasutural fractures, 42 were bisutural fractures, and 10 were complete fractures. The fracture prevalence did not increase with increasing numbers of fractured sutures. The performed binomial tests showed a significant difference between the prevalences of each fracture pattern (Table 5).

Table 4.
Prevalence of Different Fracture Patterns Regarding the Anatomic Sutures of the Zygoma and Side of Trauma (N = 492).

Table 5.
Prevalence of Different Fracture Patterns of the Zygomaticoorbital Complex Regarding the Number of Fractured Anatomic Sutures of the Zygoma (%).
Of the unisutural fractures, 48.25% were fractures of the zygomaticosphenoidal suture (anterolateral orbita floor) and 32.46% were isolated fractures of the ZMO suture. No isolated fracture of the infraorbital rim was reported. Most of bisutural fractures were fractures of the infraorbital rim and zygomaticosphenoidal suture (69.05%). Among trisutural fractures, 90.78% % (n = 256/282) involved the infraorbital rim and the zygomaticosphenoidal suture. Significant differences in suture combinations for unisutural (P ≤.0001), bisutural (P ≤.0001), trisutural (P ≤.0001), and tetrasutural (P = .0028) fractures were observed. The suture combinations in complete ZMO fractures could not be analyzed because all zygoma sutures were fractured.
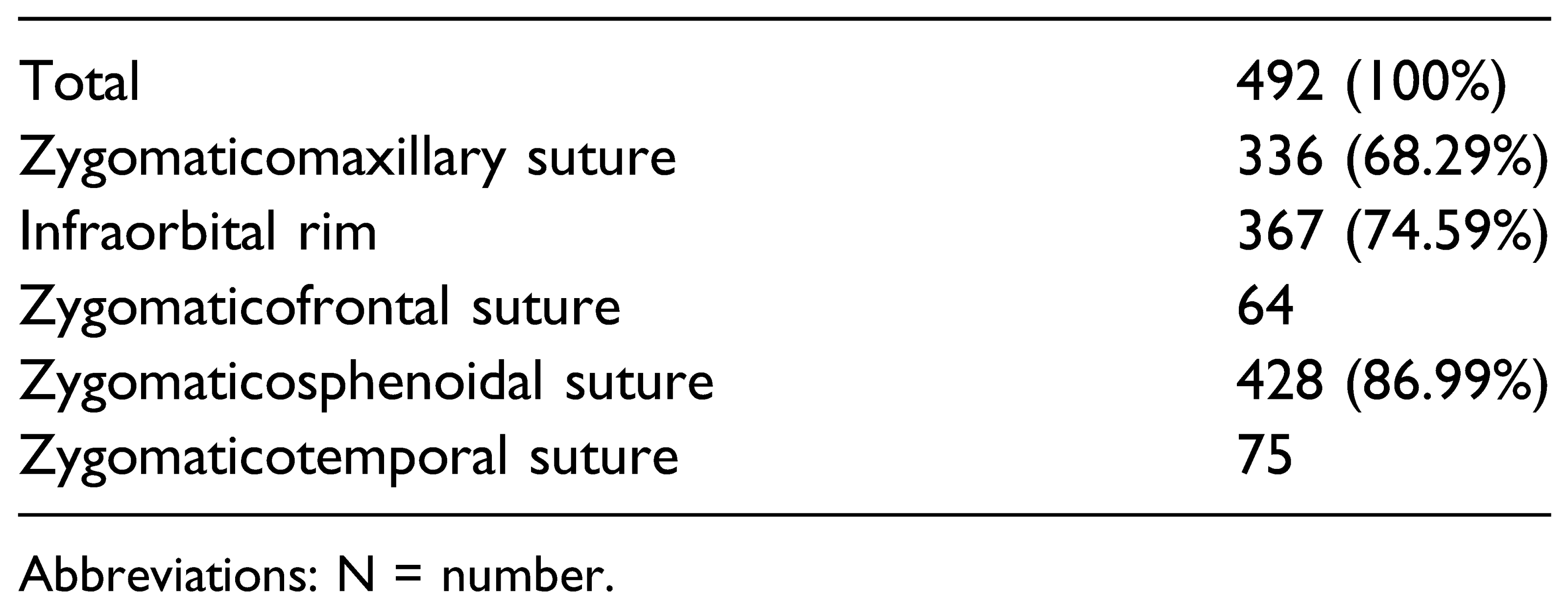
Table 6 lists the fracture prevalence of all zygoma sutures. Fractures in the zygomaticosphenoidal suture were most prevalent (n = 428; 86.99%), followed by the infraorbital rim (n = 367; 74.59%) and the zygomaticomaxillary suture (n = 336; 68.29%). The zygomaticotemporal suture was fractured in 75 and the zygomaticofrontal suture in 64 out of 492 cases respectively.

Table 6.
Absolute and Relative Fracture Prevalence Regarding the Anatomic Sutures of the Zygoma Individually (N = 492, 100%).
No significant differences were detected in fracture laterality between patients (P = .1762) or suture level (P = .2170).
Table 7 presents the effect of age on fracture patterns. No correlation between age and fracture pattern was detected (P = .4111). The effect of trauma etiology on the fracture pattern was also examined, resulting that fractures caused by tripping falls, bicycle accidents and road traffic accidents had awe significantly more severe pattern (P ≤ .0001, P ≤ .0001, and P = .0022, respectively) (Table 8).

Table 7.
Prevalence of Different Fracture Patterns Regarding Patient’s Age (N = 492).

Table 8.
Prevalence of Different Fracture Patterns Regarding Trauma Etiology (N = 492).
Fracture Prevalence of Maxillary Sinus Wall and Paranasal Buttress as Concomitance to the ZMO
Maxillary sinus wall fractures were the most frequent component of complete ZMO fractures (n = 4/10), followed by bisutural (n = 12/42) and tetrasutural fractures (n = 8/44). In total, they were detected in 47 out of 492 ZMO fractures. Fractures of the paranasal buttress was diagnosed in 6 out of 10 complete ZMO fractures, in 20 out of 44 tetrasutural fractures, and in 104 out of 282 (36.88%) trisutural fractures. In total, paranasal buttress fractures were detected in 31.30% (n = 154/492) of all ZMO fractures (Table 9).

Table 9.
Concomitance of Maxillary Sinus Wall and Paranasal Buttress Fractures in Relation to the Different Fracture Patterns of the Zygomaticoorbital Complex (%).
Discussion
This study aimed to find which zygoma sutures are more frequently fractured and in which possible combination as well the concomitance of paranasal buttress and maxillary sinus wall fractures on a large series of surgically treated unilateral ZMO fractures. The ZMO as a pentapod structure consisting of 5 anatomic sutures was evaluated, with the infraorbital rim and the zygomaticosphenoidal suture of the orbital floor as individual zygoma junctions.
The cohort was predominantly male and a decreased male-female ratio with age was observed, in agreement with previous reports [13,14,15,16]. Zygomaticoorbital fractures were found to be most common in the 19–44-year age group, followed by the >60-year age group, in accordance with previous findings [13,14]. Regarding the etiology of lateral midface injury, the study findings are consistent with the recent European multicenter EURMAT study, which showed that most ZMO fractures are caused by falls [17].
A comparison of the present study findings of ZMO fracture patterns with those of other authors was not possible because there are no studies of a similar design.
The study results confirm that most zygoma fractures include the orbital floor, justifying the use of the term “ZMO complex” [18,19]. Based on these findings, high attention is paid at the zygomaticomaxillary suture, the infraorbital rim, and the zygomaticosphenoidal suture as component of the orbital floor considering them as key anatomic landmarks during preoperative diagnosis. Accordingly, open reduction and osteosynthesis is performed primarily at these anatomic points of the zygoma. Additionally, based on the high prevalence of orbital floor fractures and secondly of fractures of the paranasal buttress, a more critical evaluation of the orbital region preoperatively and the surgical exploration of the orbita floor and the paranasal buttress as standard approach is strongly recommended, except when intraoperative 3D imaging is available.
The importance of the infraorbital rim, as was the second most prevalent fracture in this cohort, is highlighted as anatomic landmark when evaluating patients with suspected ZMO fractures [20]. The present study demonstrates that fractures of the zygomaticomaxillary suture were detected primarily as a component of trisutural fractures, but also in bisutural and tetrasutural fractures. The fact that this articulating buttress was often combined with fractures of the infraorbital rim demonstrates its importance as a key stabilization factor for the zygoma. Single linear fractures of the zygomaticomaxillary suture occured rarely in this patient collective and are probably caused by low energy trauma. These fractures are usually minimal dislocated and can be treated conservatively if no functional alterations exist. Fractures of the zygomaticotemporal suture and zygomaticofrontal suture were significantly less prevalent than other anatomic sutures of the zygoma in this cohort. This could be because the convex geometry of the zygomatic arch and its junction with both temporal and zygomatic bones absorb more force thereby reducing fracture frequency and fragment displacement [21]. The zygomaticofrontal suture is anatomically not prominent compared with other zygoma buttresses and is therefore less exposed to trauma [22,23]. Considering the study results, the zygomaticotemporal and zygomaticofrontal suture are postulated as less sensitive indicators for open reduction and internal fixation.
The involvement of the paranasal buttress and maxillary sinus wall in ZMO fractures was also investigated. These structures were mainly involved in complex ZMO fractures. Importantly, the prevalence of paranasal buttress fractures increased with the number of zygoma sutures. This could be explained by trauma severity, since the paranasal buttress maintains the facial dimensions and skeleton stability [20,24].
The more severe the trauma, the more zygoma articulating junctions are dislocated and the more fractures are detected. On the other hand, the prevalence of maxillary sinus wall fractures was not related to the number of fractured sutures in this study. They were mainly detected in bisutural and complete ZMO fractures, probably because the maxillary sinus wall is located between vertical and horizontal facial buttresses, which could prevent primary fracture [25,26]. However, these reflections need to be validated by further studies, correlating the trauma mechanism and midface bone characteristics. Additionally, further studies should investigate the correlation of these concomitant fractures with clinical parameters such as dental occlusion disturbance and facial deformity that could indicate reduction and osteosynthesis.
Osteosynthesis at non-fractured zygoma sutures should not be performed and applying minimum osteosynthesis material is recommended, especially when the ZMO complex can be reliable assessed intraoperatively due to 3D imaging. The osteosynthesis concept of ZMO fractures in regards to plate number and location has been debated since decades. In the present clinic, osteosynthesis was performed in the minimal manner that could provide sufficient skeletal stability and satisfied function and esthetics. According to the authors’ surgical experience, the treatment of ZMO fractures should be individualized, and most can be treated without three- or four-point exposure considering the clinical parameters of the patient preoperatively. The need of one- or more-point fixation should be based on skeleton stability and facial esthetics [27,28,29]. Isolated fractures of the maxillary sinus wall and paranasal buttress are usually non-dislocated and could be treated conservatively [2]. When they co-exist with ZMO fractures, open reduction and internal fixation could be indicated for example in cases of dental occlusion disturbance or facial deformity. The authors do not believe that osteosynthesis of an isolated monosutural or non-dislocated bisutural ZMO fracture, as defined in this study, increases bone stability. The ZMO complex is usually intact after injury in these cases, and functional stability is guaranteed without surgery. However, surgery is occasionally performed to improve the esthetical outcome. The individual osteosynthesis protocol, the surgical outcome and postoperative complications of this collective were not evaluated. However, it would be of great interest to investigate if the different fracture patterns, that were classificated in this study, have a significant impact on the surgical protocol and postoperative outcome. The proposed classification of the current work based on the radiologically detected number of fractured zygoma sutures is not as helpful in daily clinical management, as CT diagnosis is becoming the standard of care and the fracture pattern can be visualized directly in 3D imaging. Another approach for classification based on clinical aspects would facilitate the treatment concept in units with less resource. In that case, the individual clinical presentations need to be correlated with the surgical indication for each different pattern of ZMO fractures to standardize fracture management.
The current study has limitations. The retrospective nature of the research could lead to bias. Through this retrospective review, only prevalences and correlations could be described. However, this limitation is clearly outweighed by the large number of patients with ZMO fractures in the present cohort, thanks to the retrospective design. Due to the retrospective design and the limitations of the hospital information system, the data collection was unfortunately limited to the surgical cases. Consequently, only patients who underwent surgical intervention were included, which may affect the severity analysis. In order to propose every possible fracture variation, both the surgical and the conservatively treated cases need to be further investigated. Additionally, considering that in other geographic regions the fracture patterns and their frequency could vary due to different mechanisms of injury, the generalizability of the study findings is quite limited. Further multicenter studies including international trauma centers would assess the general effectiveness of the present work. Furthermore, bilateral ZMO fractures or fractures with concomitance of the medial orbital wall and nasoethmoidal complex were not included, that could limit the generalizability of the study findings. Another limitation is that preoperative patient’s clinical symptoms were not reported, thus, a correlation of clinical features with indications for surgery and postoperative outcome could not be derived from the results. However, postoperative radiographs verified the accuracy of fracture reduction in all included patients. The investigation of reconstruction accuracy and postoperative function according to the preoperative patient’s symptoms should be aim of future studies.
Conclusion
Trisutural fractures involving the zygomaticomaxillary suture, the infraorbital rim, and the zygomaticosphenoidal suture were the most common fracture pattern. The high concomitance of paranasal buttress fracture suggests its intraoperative surgical exploration. Knowledge of the fracture pattern variability of the ZMO complex could in certain circumstances designate CT or CBCT as mandatory before operating on ZMO fractures. Consequently, unnecessary incisions could be avoided. Further studies should correlate the clinical findings with indication for surgery and postoperative outcome for the different fracture patterns described.
Ethical Statement
This research was conducted in full accordance with the ethical standards of the institutional research committee as well as with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this noninterventional observational retrospective study, patient data were referenced to with the understanding and written consent of the patient, and all data were also anonymized and de-identified prior to analysis. In case of non-adults, the written consent was given by one of the parents. Full compliance with data protection and safeguarding of data was ensured and no information which could identify the patients was collected. Reporting was based on the recommendations of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) initiative [30].
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to thank Bacon Editing® for language editing of this manuscript.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
The responsibility of the study physician remains in full force and is not affected by this decision. This decision is subject to the following conditions. The Ethics Committee must be informed immediately of serious incidents (relating to study protocols and protocol violations) without delay. The Ethics Committee also asks to be made aware of the study results. Aspects of research projects relating to data protection law are generally only reviewed cursorily by the Ethics Committee. This vote/assessment therefore does not replace consultation with the responsible company or official data protection officer. In accordance with § 9 of the Rules of Procedure of the Ethics Committee, the matter was decided within one meeting.
References
- Alharbi, F.A.; Makrami, A.M.; Ali, F.M.; Maghdi, A.A. Patterns and etiology of maxillofacial fractures: A 5-year retrospective study. J Contemp Dent Pract. 2020, 21, 445–452. [Google Scholar] [PubMed]
- Gadkari, N.; Bawane, S.; Chopra, R.; Bhate, K.; Kulkarni, D. Comparative evaluation of 2-point vs 3-point fixation in the treatment of zygomaticomaxillary complex fractures—A systematic review. J Cranio-Maxillo-Fac Surg. 2019, 47, 1542–1550. [Google Scholar] [CrossRef]
- Rothweiler, R.; Bayer, J.; Zwingmann, J.; et al. Outcome and complications after treatment of facial fractures at different times in polytrauma patients. J Cranio-Maxillo-Fac Surg. 2018, 46, 283–287. [Google Scholar] [CrossRef]
- Kunz, C.; Audigé, L.; Cornelius, C.P.; et al. The comprehensive AOCMF classification system: Midface fractures—level 2 tutorial. Craniomaxillofac Trauma Reconstr. 2014, 7, S059–S067. [Google Scholar] [CrossRef] [PubMed]
- Haworth, S.; Bates, A.; Beech, A.; Knepil, G. A clinical decision rule to predict zygomatico-maxillary fractures. J Cranio-Maxillo-Fac Surg. 2017, 45, 1333–1337. [Google Scholar] [CrossRef] [PubMed]
- van Hout, W.M.M.T.; Van Cann, E.M.; Koole, R.; Rosenberg, A.J.W.P. Surgical treatment of unilateral zygomaticomaxillary complex fractures: A 7-year observational study assessing treatment outcome in 153 cases. J Cranio-Maxillo-Fac Surg. 2016, 44, 1859–1865. [Google Scholar] [CrossRef]
- Bartoli, D.; Fadda, M.T.; Battisti, A.; et al. Retrospective analysis of 301 patients with orbital floor fracture. J Cranio-Maxillo-Fac Surg. 2015, 43, 244–247. [Google Scholar] [CrossRef]
- Ellis, E. , 3rd.; Perez, D. An algorithm for the treatment of isolated zygomatico-orbital fractures. J Oral Maxillofac Surg. 2014, 72, 1975–1983. [Google Scholar] [CrossRef]
- Raschke, G.F.; Rieger, U.M.; Bader, R.D.; et al. The zygomaticomaxillary complex fracture-an anthropometric appraisal of surgical outcomes. J Cranio-Maxillo-Fac Surg. 2013, 41, 331–337. [Google Scholar] [CrossRef]
- Audigé, L.; Cornelius, C.P.; Di Ieva, A.; Prein, J.; CMF Classification Group 6. The first AO classification system for fractures of the craniomaxillofacial skeleton: Rationale, methodological background, developmental process, and objectives. Craniomaxillofac Trauma Reconstr. 2014, 7, S006–S014. [Google Scholar]
- Cornelius, C.P.; Audigé, L.; Kunz, C.; et al. The comprehensive AOCMF classification system: midface fractures—level 3 tutorial. Craniomaxillofac Trauma Reconstr. 2014, 7, S068–S091. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association Declaration of Helsinki. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Organ. 2001, 79, 373–374. [Google Scholar]
- Brucoli, M.; Boffano, P.; Broccardo, E.; et al. The “European zygomatic fracture” research project: The epidemiological results from a multicenter European collaboration. J Cranio-Maxillo-Fac Surg. 2019, 47, 616–621. [Google Scholar] [CrossRef] [PubMed]
- Blumer, M.; Kumalic, S.; Gander, T.; et al. Retrospective analysis of 471 surgically treated zygomaticomaxillary complex fractures. J Cranio-Maxillo-Fac Surg. 2018, 46, 269–273. [Google Scholar] [CrossRef]
- Mijiti, A.; Ling, W.; Tuerdi, M.; et al. Epidemiological analysis of maxillofacial fractures treated at a university hospital, Xinjiang, China: A 5-year retrospective study. J Cranio-Maxillo-Fac Surg. 2014, 42, 227–233. [Google Scholar] [CrossRef]
- Salentijn, E.G.; Boverhoff, J.; Heymans, M.W.; van den Bergh, B.; Forouzanfar, T. The clinical and radiographical characteristics of zygomatic complex fractures: A comparison between the surgically and non-surgically treated patients. J Cranio-Maxillo-Fac Surg. 2014, 42, 492–497. [Google Scholar] [CrossRef]
- Boffano, P.; Roccia, F.; Zavattero, E.; et al. Assault-related maxillofacial injuries: The results from the European Maxillofacial Trauma (EURMAT) multicenter and prospective collaboration. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015, 119, 385–391. [Google Scholar] [CrossRef]
- Jin, K.S.; Lee, H.; Sohn, J.B.; et al. Fracture patterns and causes in the craniofacial region: an 8-year review of 2076 patients. Maxillofac Plast Reconstr Surg. 2018, 40, 29. [Google Scholar] [CrossRef]
- Sharma, R.; Muralidharan, C.G.; Roy, I.D.; Jain, N.K.; Patrikar, S. Radiological evaluation of sphenozygomatic suture fixation for restoration of orbital volume: A retrospective study. J Cranio-Maxillo-Fac Surg. 2016, 44, 1903–1908. [Google Scholar] [CrossRef]
- Ho, J.P.T.F.; Schreurs, R.; Aydi, S.; et al. Natural variation of the zygomaticomaxillary complex symmetry in normal individuals. J Cranio-Maxillo-Fac Surg. 2017, 45, 1927–1933. [Google Scholar] [CrossRef]
- Buller, J.; Zirk, E.; Kreppel, M.; et al. Radiomorphometric analysis of isolated zygomatic arch fractures: A comparison of classifications and reduction outcomes. J Cranio-Maxillo-Fac Surg. 2018, 46, 1252–1257. [Google Scholar] [CrossRef] [PubMed]
- Nasr, W.F.; ElSheikh, E.; El-Anwar, M.W.; Sweed, A.H.; Bessar, A.; Ezzeldin, N. Two- versus three-point internal fixation of displaced zygomaticomaxillary complex fractures. Cranio-maxillofac Trauma Reconstr. 2018, 11, 256–264. [Google Scholar] [CrossRef]
- Wilde, F.; Schramm, A. Intraoperative imaging in orbital and midface reconstruction. Facial Plast Surg. 2014, 30, 545–553. [Google Scholar] [PubMed]
- Jazayeri, H.E.; Khavanin, N.; Yu, J.W.; et al. Fixation points in the treatment of traumatic zygomaticomaxillary complex fractures: A systematic review and meta-analysis. J Oral Maxillofac Surg. 2019, 77, 2064–2073. [Google Scholar] [CrossRef] [PubMed]
- Ali-Alsuliman, D.; Ibrahim, E.H.; Braimah, R.O. Patterns of zygomatic complex bone fracture in Saudi Arabia. J Emerg Trauma Shock. 2018, 11, 170–174. [Google Scholar]
- Lee, C.W.; Foo, Q.C.; Wong, L.V.; Leung, Y.Y. An overview of maxillofacial trauma in Oral and Maxillofacial Tertiary Trauma Centre, Queen Elizabeth Hospital, Kota Kinabalu, Sabah. Craniomaxillofac Trauma Reconstr. 2017, 10, 16–21. [Google Scholar] [CrossRef]
- Starch-Jensen, T.; Linnebjerg, L.B.; Jensen, J.D. Treatment of zygomatic complex fractures with surgical or nonsurgical intervention: A retrospective study. Open Dent J. 2018, 12, 377–387. [Google Scholar] [CrossRef]
- Strong, E.B.; Gary, C. Management of zygomaticomaxillary complex fractures. Facial Plast Surg Clin North Am. 2017, 25, 547–562. [Google Scholar] [CrossRef]
- Farber, S.J.; Nguyen, D.C.; Skolnick, G.B.; Woo, A.S.; Patel, K.B. Current management of zygomaticomaxillary complex fractures: A multidisciplinary survey and literature review. Craniomaxillofac Trauma Reconstr. 2016, 9, 313–322. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; et al. Strengthening the reporting of observational studies in epidemiology (STROBE): Explanation and elaboration. Int J Surg 2014, 12, 1500–1524. [Google Scholar] [CrossRef]
© 2023 by the author. The Author(s) 2023.