Fractional CO2 Laser for Acne Scar Treatment: A Comparative Analysis of Ablative vs. Combined Ablative and Non-Ablative Modalities
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Laser Devices
2.3. Procedures
2.4. Statistical Analysis
3. Results
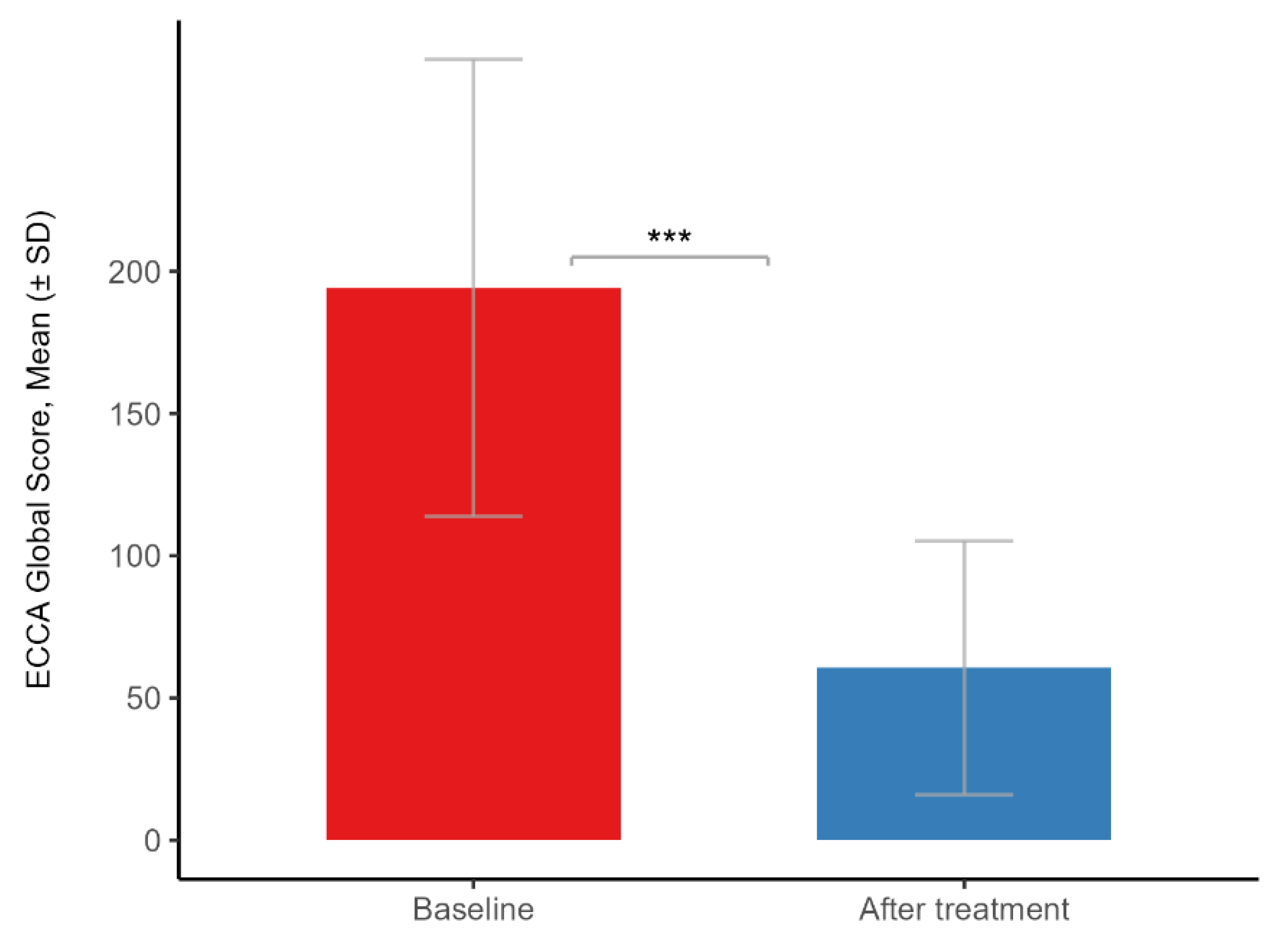
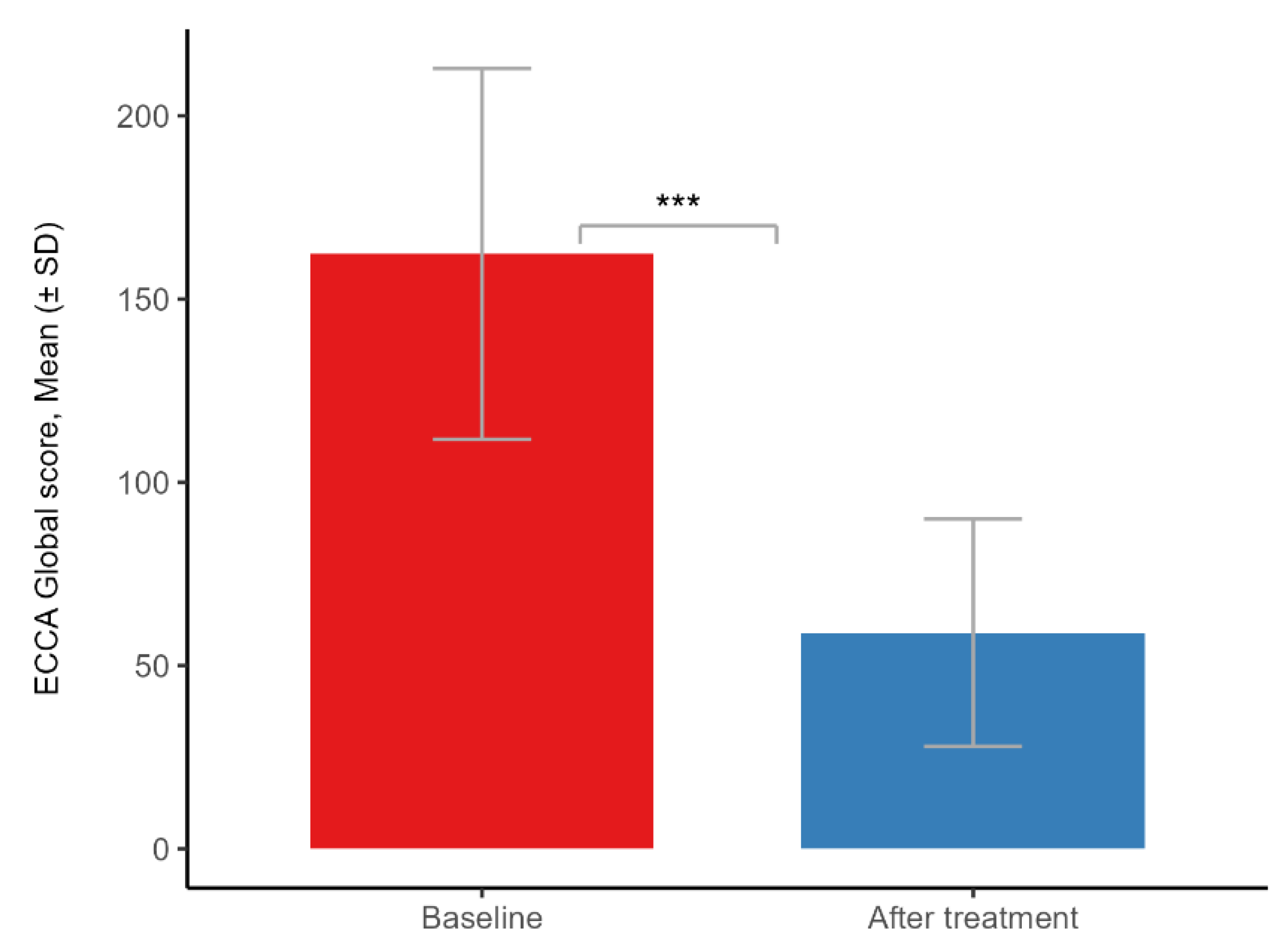
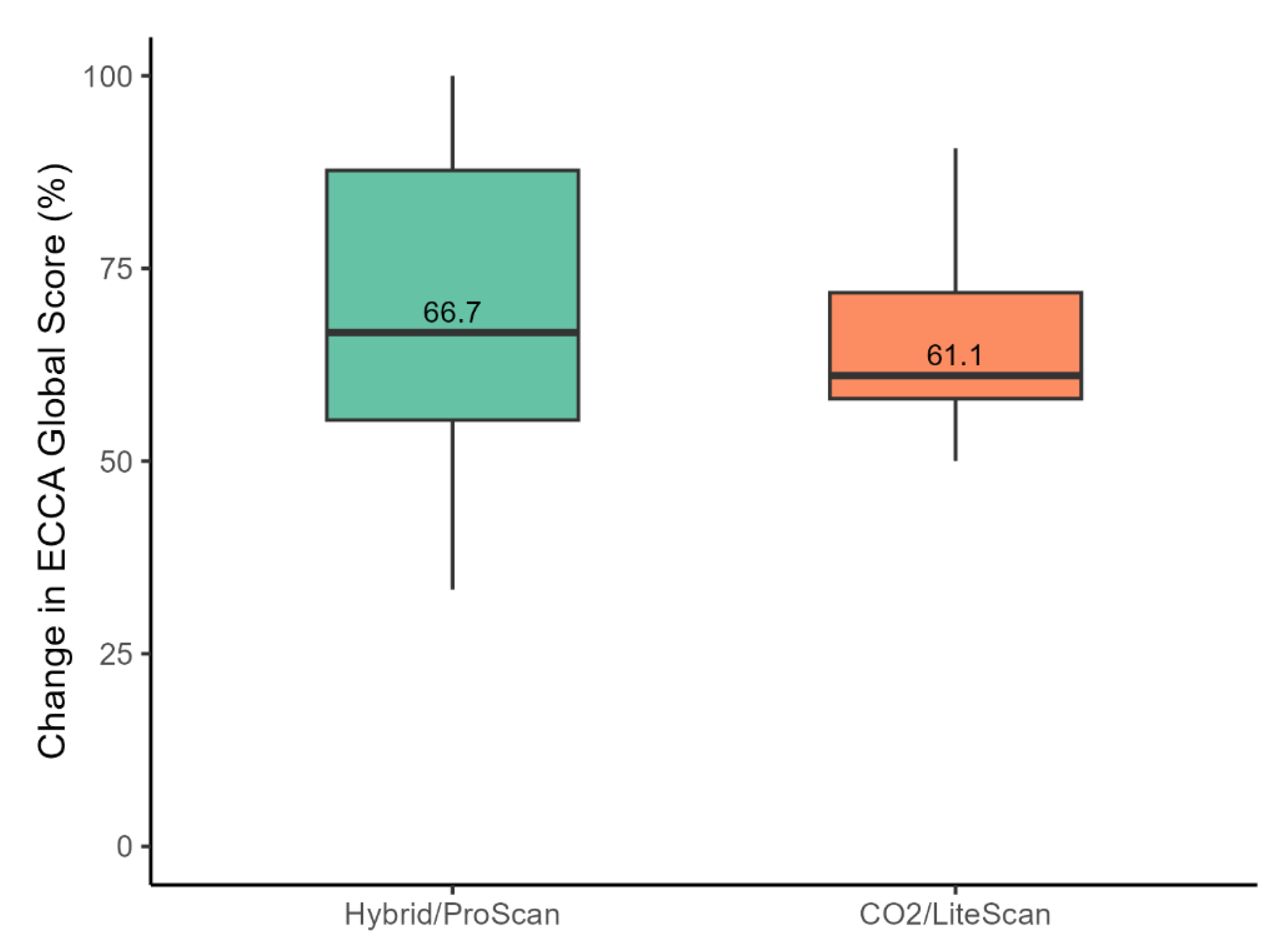
3.1. Clinical Efficacy
3.2. Safety Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ECCA | Echelle d’Evaluation Clinique des Cicatrices D’Acne |
| NAFL | Non-ablative fractional laser |
| AFL | Fractional laser |
| ECM | Extracellular matrix |
| MTZ | Microthermal treatment zone |
| PIH | Post-inflammatory hyperpigmentation |
| TGF-β | Transforming growth factor-β |
| AE | Adverse event |
| CO2 | Carbon dioxide |
| SD | Standard deviation |
References
- Wilcock, J.; Kuznetsov, L.; Ravenscroft, J.; Rafiq, M.I.; Healy, E. New NICE Guidance on Acne Vulgaris: Implications for First-Line Management in Primary Care. Br. J. Gen. Pract. 2021, 71, 568–570. [Google Scholar] [CrossRef] [PubMed]
- Layton, A.M.; Gupta, G.; Seukeran, D.; Maruthappu, T.; Gaillard, S.; Whitehouse, H.; Ali, F.R.; Razzaque, A.; Al-Niaimi, F.; Copperwheat, S. What’s New After NICE Acne Guidelines. Dermatol. Ther. 2024, 14, 2727–2738. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Sinaki, D.G.; Tang, Y.; Chen, Y.; Zhang, Y.; Zhang, Z. Acne-Induced Pathological Scars: Pathophysiology and Current Treatments. Burn. Trauma 2024, 12, tkad060. [Google Scholar] [CrossRef]
- Bhargava, S.; Cunha, P.R.; Lee, J.; Kroumpouzos, G. Acne Scarring Management: Systematic Review and Evaluation of the Evidence. Am. J. Clin. Dermatol. 2018, 19, 459–477. [Google Scholar] [CrossRef]
- Moon, J.; Yoon, J.Y.; Yang, J.H.; Kwon, H.H.; Min, S.; Suh, D.H. Atrophic Acne Scar: A Process from Altered Metabolism of Elastic Fibres and Collagen Fibres Based on Transforming Growth Factor-β1 Signalling. Br. J. Dermatol. 2019, 181, 1226–1237. [Google Scholar] [CrossRef]
- Sadick, N.S.; Cardona, A. Laser Treatment for Facial Acne Scars: A Review. J. Cosmet. Laser Ther. 2018, 20, 424–435. [Google Scholar] [CrossRef]
- Chilicka, K.; Rusztowicz, M.; Szyguła, R.; Nowicka, D. Methods for the Improvement of Acne Scars Used in Dermatology and Cosmetology: A Review. J. Clin. Med. 2022, 11, 2744. [Google Scholar] [CrossRef] [PubMed]
- Karppinen, S.-M.; Heljasvaara, R.; Gullberg, D.; Tasanen, K.; Pihlajaniemi, T. Toward Understanding Scarless Skin Wound Healing and Pathological Scarring. F1000Research 2019, 8, 787. [Google Scholar] [CrossRef]
- Xue, M.; Jackson, C.J. Extracellular Matrix Reorganization During Wound Healing and Its Impact on Abnormal Scarring. Adv. Wound Care 2015, 4, 119–136. [Google Scholar] [CrossRef]
- Fernández-Guarino, M.; Hernández-Bule, M.L.; Bacci, S. Cellular and Molecular Processes in Wound Healing. Biomedicines 2023, 11, 2526. [Google Scholar] [CrossRef]
- Kurokawa, I.; Layton, A.M.; Ogawa, R. Updated Treatment for Acne: Targeted Therapy Based on Pathogenesis. Dermatol. Ther. 2021, 11, 1129–1139. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Xue, Y.; Chen, Y.; Chen, T.; Zhong, J.; Shao, X.; Chen, J. Prevalence and Risk Factors of Acne Scars in Patients with Acne Vulgaris. Ski. Res. Technol. 2023, 29, e13386. [Google Scholar] [CrossRef]
- Xu, Y.; Deng, Y. Ablative Fractional CO2 Laser for Facial Atrophic Acne Scars. Facial Plast. Surg. 2018, 34, 205–219. [Google Scholar] [CrossRef]
- Clark, A.K.; Saric, S.; Sivamani, R.K. Acne Scars: How Do We Grade Them? Am. J. Clin. Dermatol. 2018, 19, 139–144. [Google Scholar] [CrossRef]
- Dreno, B.; Khammari, A.; Orain, N.; Noray, C.; Mérial-Kieny, C.; Méry, S.; Nocera, T. ECCA Grading Scale: An Original Validated Acne Scar Grading Scale for Clinical Practice in Dermatology. Dermatology 2007, 214, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Salameh, F.; Shumaker, P.R.; Goodman, G.J.; Spring, L.K.; Seago, M.; Alam, M.; Al-Niaimi, F.; Cassuto, D.; Chan, H.H.; Dierickx, C.; et al. Energy-Based Devices for the Treatment of Acne Scars: 2022 International Consensus Recommendations. Lasers Surg. Med. 2022, 54, 10–26. [Google Scholar] [CrossRef] [PubMed]
- Chapas, A.M.; Brightman, L.; Sukal, S.; Hale, E.; Daniel, D.; Bernstein, L.J.; Geronemus, R.G. Successful Treatment of Acneiform Scarring with CO 2 Ablative Fractional Resurfacing. Lasers Surg. Med. 2008, 40, 381–386. [Google Scholar] [CrossRef]
- Meghe, S.R.; Khan, A.; Jangid, S.D.; Sarda, B.; Vangala, N.; Saoji, V. Shedding Light on Acne Scars: A Comprehensive Review of CO2 vs. Erbium-Doped Yttrium Aluminium Garnet (Er:YAG) Laser Therapy. Cureus 2024, 16, e57572. [Google Scholar] [CrossRef]
- Kubik, P.; Bighetti, S.; Bettolini, L.; Gruszczyński, W.; Łukasik, B.; Guida, S.; Stabile, G.; Murillo Herrera, E.M.; Carugno, A.; D’Este, E.; et al. Effectiveness and Safety of the Use of 1470 Nm Laser Therapy in Patients Suffering From Acne Scarring of the Facial Skin. Clin. Cosmet. Investig. Dermatol. 2025, 18, 543–551. [Google Scholar] [CrossRef]
- Laubach, H.-J.; Tannous, Z.; Anderson, R.R.; Manstein, D. Skin Responses to Fractional Photothermolysis. Lasers Surg. Med. 2006, 38, 142–149. [Google Scholar] [CrossRef]
- Hantash, B.M.; Mahmood, M.B. Fractional Photothermolysis: A Novel Aesthetic Laser Surgery Modality. Dermatol. Surg. 2007, 33, 525–534. [Google Scholar] [CrossRef]
- Arsiwala, S.Z.; Desai, S.R. Fractional Carbon Dioxide Laser: Optimizing Treatment Outcomes for Pigmented Atrophic Acne Scars in Skin of Color. J. Cutan. Aesthet. Surg. 2019, 12, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Trelles, M.A.; Shohat, M.; Urdiales, F. Safe and Effective One-Session Fractional Skin Resurfacing Using a Carbon Dioxide Laser Device in Super-Pulse Mode: A Clinical and Histologic Study. Aesthetic Plast. Surg. 2011, 35, 31–42. [Google Scholar] [CrossRef] [PubMed]
- Shenhav, L.T.; Shehadeh, W.; Alcotzer, I.; Artzi, O. Hybrid Fractional Laser Facial Resurfacing: A Comparison between a Single Treatment at High Settings versus Multiple Treatments at Low to Moderate Settings. Lasers Surg. Med. 2024, 56, 68–74. [Google Scholar] [CrossRef]
- Fitzpatrick, T.B. The Validity and Practicality of Sun-Reactive Skin Types I through VI. Arch. Dermatol. 1988, 124, 869–871. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.N.; Patel, B.C. Laser Fitzpatrick Skin Type Recommendations. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Lu, K.; Cai, S. Efficacy and Safety Comparison between 1927 Nm Thulium Laser and 2940 Nm Er:YAG Laser in the Treatment of Facial Atrophic Acne Scarring: A Prospective, Simultaneous Spilt-Face Clinical Trial. Lasers Med. Sci. 2022, 37, 2025–2031. [Google Scholar] [CrossRef]
- Asri, E.A.; Widayati, R.I.; Malik, D.A. Effectiveness of Combined 10,600 Nm Fractional CO2 and 1540 Nm Erbium GaAs Laser Therapy on Acne Scar Score Alteration in Patients with Atrophic Acne Scars. Turk. J. Dermatol. 2019, 13, 126. [Google Scholar] [CrossRef]
- Dai, R.; Cao, Y.; Su, Y.; Cai, S. Comparison of 1064-Nm Nd:YAG Picosecond Laser Using Fractional Micro-Lens Array vs. Ablative Fractional 2940-Nm Er:YAG Laser for the Treatment of Atrophic Acne Scar in Asians: A 20-Week Prospective, Randomized, Split-Face, Controlled Pilot Study. Front. Med. 2023, 10, 1248831. [Google Scholar] [CrossRef]
- Ding, Z.; Pan, Z.; Tang, Y.; Wang, S.; Hua, H.; Hou, Z.; Zhou, B. Effectiveness and Safety of the Modified Multiple Mode Procedures versus Traditional Multiple Mode Procedures on Treating Facial Atrophic Acne Scars: A Propensity Score Matching Retrospective Cohort Study. Lasers Med. Sci. 2024, 39, 260. [Google Scholar] [CrossRef]
- Zhang, Z.; Fei, Y.; Chen, X.; Lu, W.; Chen, J. Comparison of a Fractional Microplasma Radio Frequency Technology and Carbon Dioxide Fractional Laser for the Treatment of Atrophic Acne Scars: A Randomized Split-Face Clinical Study. Dermatol. Surg. 2013, 39, 559. [Google Scholar] [CrossRef]
- Yuan, X.-H.; Zhong, S.-X.; Li, S.-S. Comparison Study of Fractional Carbon Dioxide Laser Resurfacing Using Different Fluences and Densities for Acne Scars in Asians: A Randomized Split-Face Trial. Dermatol. Surg. 2014, 40, 545–552. [Google Scholar] [CrossRef] [PubMed]
- Jennings, T.; Duffy, R.; McLarney, M.; Renzi, M.; Heymann, W.R.; Decker, A.; Lawrence, N. Acne Scarring-Pathophysiology, Diagnosis, Prevention and Education: Part I. J. Am. Acad. Dermatol. 2024, 90, 1123–1134. [Google Scholar] [CrossRef]
- Schultz, G.S.; Wysocki, A. Interactions between Extracellular Matrix and Growth Factors in Wound Healing. Wound Repair Regen. 2009, 17, 153–162. [Google Scholar] [CrossRef]
- Mu, Y.-Z.; Jiang, L.; Yang, H. The Efficacy of Fractional Ablative Carbon Dioxide Laser Combined with Other Therapies in Acne Scars. Dermatol. Ther. 2019, 32, e13084. [Google Scholar] [CrossRef]
- Varga, J.; Rosenbloom, J.; Jimenez, S.A. Transforming Growth Factor β (TGFβ) Causes a Persistent Increase in Steady-State Amounts of Type I and Type III Collagen and Fibronectin mRNAs in Normal Human Dermal Fibroblasts. Biochem. J. 1987, 247, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Creely, J.J.; DiMari, S.J.; Howe, A.M.; Haralson, M.A. Effects of Transforming Growth Factor-Beta on Collagen Synthesis by Normal Rat Kidney Epithelial Cells. Am. J. Pathol. 1992, 140, 45–55. [Google Scholar]
- Carniol, P.J.; Hamilton, M.M.; Carniol, E.T. Current Status of Fractional Laser Resurfacing. JAMA Facial Plast. Surg. 2015, 17, 360–366. [Google Scholar] [CrossRef] [PubMed]
- Nowak, K.C.; McCormack, M.; Koch, R.J. The Effect of Superpulsed Carbon Dioxide Laser Energy on Keloid and Normal Dermal Fibroblast Secretion of Growth Factors: A Serum-Free Study. Plast. Reconstr. Surg. 2000, 105, 2039–2048. [Google Scholar] [CrossRef]
- Tretti Clementoni, M.; Galimberti, M.; Tourlaki, A.; Catenacci, M.; Lavagno, R.; Bencini, P.L. Random Fractional Ultrapulsed CO2 Resurfacing of Photodamaged Facial Skin: Long-Term Evaluation. Lasers Med. Sci. 2013, 28, 643–650. [Google Scholar] [CrossRef]
- Clementoni, M.T.; Lavagno, R.; Munavalli, G. A New Multi-Modal Fractional Ablative CO2 Laser for Wrinkle Reduction and Skin Resurfacing. J. Cosmet. Laser Ther. 2012, 14, 244–252. [Google Scholar] [CrossRef]
- Prignano, F.; Campolmi, P.; Bonan, P.; Ricceri, F.; Cannarozzo, G.; Troiano, M.; Lotti, T. Fractional CO2 Laser: A Novel Therapeutic Device upon Photobiomodulation of Tissue Remodeling and Cytokine Pathway of Tissue Repair. Dermatol. Ther. 2009, 22 (Suppl. S1), S8–S15. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Ren, K.; Yin, X.; She, H.; Liu, H.; Zhou, B. Efficacy and Adverse Reactions of Fractional CO2 Laser for Atrophic Acne Scars and Related Clinical Factors: A Retrospective Study on 121 Patients. J. Cosmet. Dermatol. 2022, 21, 1989–1997. [Google Scholar] [CrossRef] [PubMed]
- Chan, N.P.Y.; Ho, S.G.Y.; Yeung, C.K.; Shek, S.Y.N.; Chan, H.H. Fractional Ablative Carbon Dioxide Laser Resurfacing for Skin Rejuvenation and Acne Scars in Asians. Lasers Surg. Med. 2010, 42, 615–623. [Google Scholar] [CrossRef]
- Majid, I.; Imran, S. Fractional CO2 Laser Resurfacing as Monotherapy in the Treatment of Atrophic Facial Acne Scars. J. Cutan. Aesthetic Surg. 2014, 7, 87–92. [Google Scholar] [CrossRef]
- Qian, H.; Lu, Z.; Ding, H.; Yan, S.; Xiang, L.; Gold, M.H. Treatment of Acne Scarring with Fractional CO 2 Laser. J. Cosmet. Laser Ther. 2012, 87, 162–165. [Google Scholar] [CrossRef]
- Reinholz, M.; Schwaiger, H.; Heppt, M.; Poetschke, J.; Tietze, J.; Epple, A.; Ruzicka, T.; Kaudewitz, P.; Gauglitz, G. Comparison of Two Kinds of Lasers in the Treatment of Acne Scars. Facial Plast Surg. 2015, 31, 523–531. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Xu, F.; Lin, H.; Ma, Y.; Hu, Y.; Meng, Q.; Lin, P.; Zhang, Y. Efficacy of Fractional CO2 Laser Therapy Combined with Hyaluronic Acid Dressing for Treating Facial Atrophic Acne Scars: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Lasers Med. Sci. 2023, 38, 214. [Google Scholar] [CrossRef]
- Galal, O.; Tawfik, A.A.; Abdalla, N.; Soliman, M. Fractional CO2 Laser versus Combined Platelet-rich Plasma and Fractional CO2 Laser in Treatment of Acne Scars: Image Analysis System Evaluation. J. Cosmet. Dermatol. 2019, 18, 1665–1671. [Google Scholar] [CrossRef]
- Belletti, S.; Pennati, B.M.; Madeddu, F. A Sequential CO2 and 1540 Nm Laser for the Treatment of Neck Skin Laxity. Ski. Res. Technol. 2023, 29, e13469. [Google Scholar] [CrossRef]
- Mezzana, P.; Valeriani, M.; Valeriani, R. Combined Fractional Resurfacing (10600 Nm/1540 Nm): Tridimensional Imaging Evaluation of a New Device for Skin Rejuvenation. J. Cosmet. Laser Ther. 2016, 18, 397–402. [Google Scholar] [CrossRef]
- Fiorentini, F.; Fusco, I. Synergistic Sequential Emission of Fractional 1540 Nm and 10 600 Lasers for Abdominal Postsurgical Scar Management: A Clinical Case Report. Am. J. Case Rep. 2022, 24, e938607-1. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Cho, K.-H. Clinical Trial of Dual Treatment with an Ablative Fractional Laser and a Nonablative Laser for the Treatment of Acne Scars in Asian Patients. Dermatol. Surg. 2009, 35, 1089. [Google Scholar] [CrossRef] [PubMed]
- Belletti, S.; Madeddu, F.; Amoruso, G.F.; Provenzano, E.; Nisticò, S.P.; Fusco, I.; Bennardo, L. An Innovative Dual-Wavelength Laser Technique for Atrophic Acne Scar Management: A Pilot Study. Medicina 2023, 59, 2012. [Google Scholar] [CrossRef] [PubMed]
- García, P.N.; Andrino, R.L. Resurfacing of Atrophic Facial Acne Scars with a Multimodality CO2 and 1570 Nm Laser System. J. Cosmet. Dermatol. 2024, 23, 13–18. [Google Scholar] [CrossRef]


| Characteristic | Alma Hybrid/ProScan | Alma Pixel CO2/LiteScan |
|---|---|---|
| Patients | 45 | 43 |
| Age (years) 1 | 31.11 (7.95) | 30.19 (7.45) |
| Treatment sessions 1 | 4.16 (1.36) | 4.23 (1.39) |
| Gender 2 | ||
| F | 33 (73.3) | 19 (44.2) |
| M | 12 (26.7) | 24 (55.8) |
| Body area 2 | ||
| Back | 1 (2.2) | 3 (7.0) |
| Chest | 1 (2.2) | 2 (4.7) |
| Face | 43 (95.6) | 38 (88.4) |
| Skin types 2,3 | ||
| Type II | 26 (57.8) | 4 (9.3) |
| Type III | 16 (35.6) | 30 (69.8) |
| Type IV | 3 (6.7) | 7 (16.3) |
| Type V | 0 | 2 (4.7) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Avdulaj, A.; Menashe, S.; Govrin-Yehudain, Y.; Hadad, E.; Moscovici, S.; Dor, O.; Heller, L. Fractional CO2 Laser for Acne Scar Treatment: A Comparative Analysis of Ablative vs. Combined Ablative and Non-Ablative Modalities. J. Aesthetic Med. 2025, 1, 2. https://doi.org/10.3390/jaestheticmed1010002
Avdulaj A, Menashe S, Govrin-Yehudain Y, Hadad E, Moscovici S, Dor O, Heller L. Fractional CO2 Laser for Acne Scar Treatment: A Comparative Analysis of Ablative vs. Combined Ablative and Non-Ablative Modalities. Journal of Aesthetic Medicine. 2025; 1(1):2. https://doi.org/10.3390/jaestheticmed1010002
Chicago/Turabian StyleAvdulaj, Arminda, Shaked Menashe, Yoad Govrin-Yehudain, Eran Hadad, Sharon Moscovici, Omer Dor, and Lior Heller. 2025. "Fractional CO2 Laser for Acne Scar Treatment: A Comparative Analysis of Ablative vs. Combined Ablative and Non-Ablative Modalities" Journal of Aesthetic Medicine 1, no. 1: 2. https://doi.org/10.3390/jaestheticmed1010002
APA StyleAvdulaj, A., Menashe, S., Govrin-Yehudain, Y., Hadad, E., Moscovici, S., Dor, O., & Heller, L. (2025). Fractional CO2 Laser for Acne Scar Treatment: A Comparative Analysis of Ablative vs. Combined Ablative and Non-Ablative Modalities. Journal of Aesthetic Medicine, 1(1), 2. https://doi.org/10.3390/jaestheticmed1010002






