1. Introduction
Air pollution, largely driven by industrialization and global warming, has emerged as one of the most critical public health and environmental threats of our time. Beyond its well-documented contribution to climate change, air pollution significantly affects human health, increasing both morbidity and mortality rates [
1,
2,
3]. The respiratory system, being directly exposed to the environment, is particularly vulnerable to ambient pollutants and temperature fluctuations [
4,
5]. To monitor and communicate pollution levels, the Air Quality Index (AQI) plays a crucial role by aggregating concentrations of key pollutants into a simple scale ranging from “Good” to “Extremely poor” [
6]. This tool aids governments in making informed policy decisions to safeguard public health [
7,
8,
9]. To model the complex, short-term impact of environmental exposures on health outcomes, the distributed lag non-linear model (DLNM) framework was applied, which captures both delayed and non-linear exposure-response relationships [
10,
11]. In this study, we apply distributed lag non-linear models (DLNMs) to investigate the effects of the Air Quality Index (AQI) on hospital admissions (HA) and hospital stays (HS), with a particular focus on the potentially distinct and underexplored burden each outcome imposes on the healthcare system and economy.
2. Data and Methodology
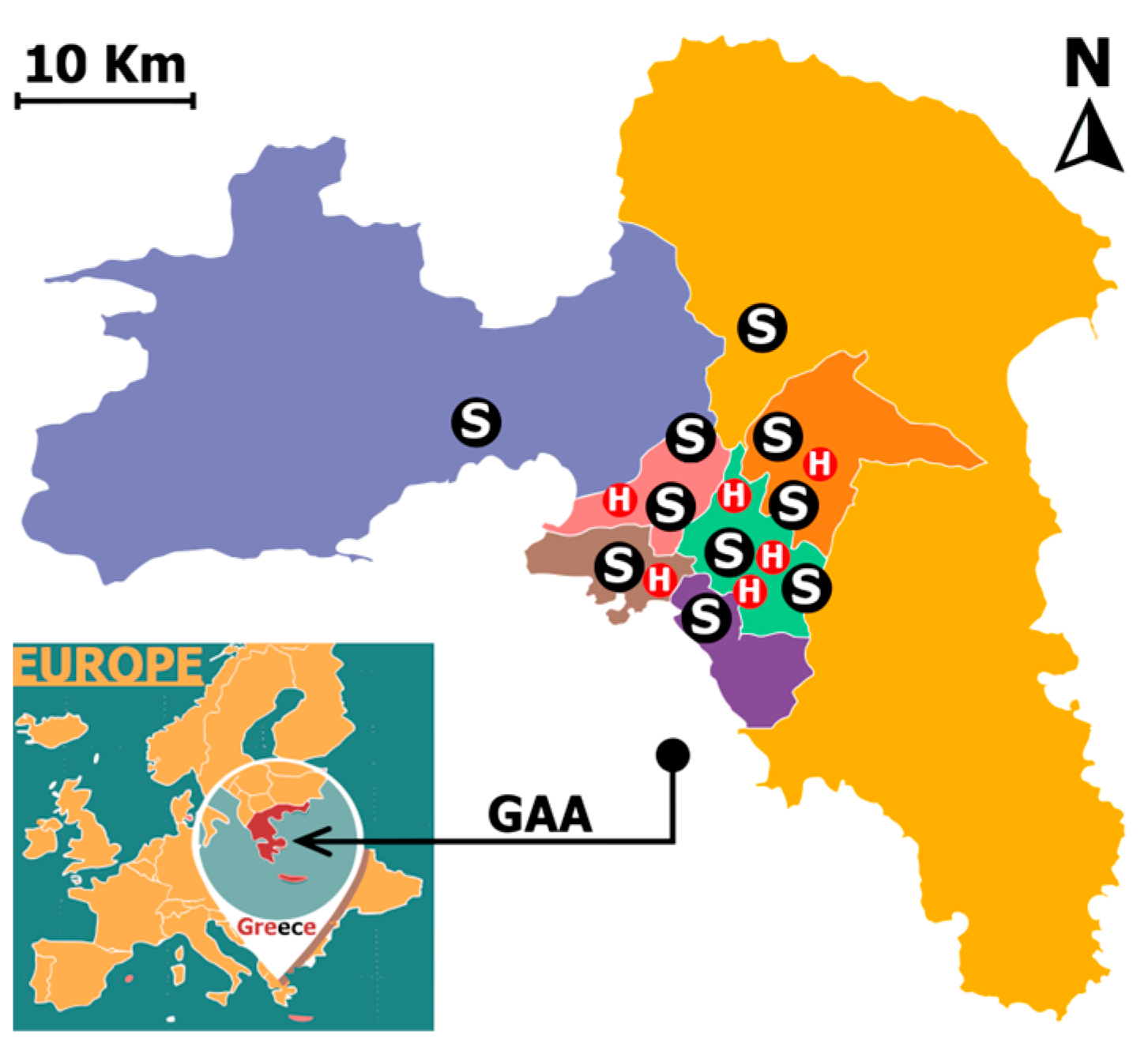
This study analyzes short-term health effects of air pollution in the Greater Athens Area (GAA), Greece, from 2018 to 2022. Hospital data were gathered from six major public hospitals—Evaggelismos, Konstantopoulio, Elpis, Attikon, Tzanio, and Sismanoglio—chosen for their data completeness, specialization in cardiovascular (CVD) and respiratory diseases (RD), and broad geographic coverage (
Figure 1). Two health outcome variables were examined: daily HA, defined as the number of new hospitalizations per day, and daily HS, defined as the total number of hospital bed-days generated by those patients.
Environmental exposure data, including hourly pollutant concentrations (PM2.5, PM10, NO2, O3), were obtained from 10 official monitoring stations operated by the Ministry of Environment and Energy. A single Daily AQI value was computed each day using the European Air Quality Index (EAQI) methodology, reflecting the highest pollutant-based AQI classification for that day.
Two Distributed Lag Non-Linear Models (DLNMs) were developed to assess the association of Daily AQI with: (1) daily HA, and (2) daily HS. Both models included a 10-day lag structure to estimate cumulative relative risks (RR) over this period. Exposure-lag relationships were modeled using cross basis functions, while natural cubic splines controlled for long-term trends and seasonality. Indicator variables for day of the week and year were included as covariates.
To improve model fit and stability, we applied asymmetric kernel smoothing using a wider Epanechnikov window, enhancing the interpretability and precision of cumulative risk estimates. All models were fitted using a Negative Binomial distribution to account for overdispersion in the data. The same base model structure was used for both outcomes—defined by the following equation:
This setup allows for a direct comparison of how daily air quality fluctuations influence both the volume of new hospitalizations and the broader healthcare burden they generate.
3. Discussion and Results
Figure 2 and
Figure 3 display the cumulative RRs of air pollution exposure over a 10-day lag on daily HA and total HS, respectively. Using the Good air quality category as the reference point (RR = 1.00), both models demonstrate a progressive increase in health impacts as air quality deteriorates. However, the magnitude and consistency of the associations are more pronounced in the model examining HS.
For HA, even the Fair air quality category reveals a modest yet statistically significant increase in risk, with a relative risk of 1.04 (95% CI: 1.00–1.07). This risk rises further within the Moderate category, reaching 1.07 (95% CI: 1.00–1.14) and climbing to 1.09 (95% CI: 1.01–1.18). Within the Poor air quality level, the relative risk remains slightly elevated with values like 1.08 (95% CI: 1.01–1.17) and 1.07 (95% CI: 1.00–1.14). In the Very Poor category, relative risks begin to plateau around 1.05 to 1.07, but the confidence intervals begin to include or approach unity, as seen with values such as 1.07 (95% CI: 0.99–1.12), indicating less statistical certainty. At the Extremely Poor level, the RR increases to 1.13 (95% CI: 0.96–1.34), suggesting a potentially important effect, although the association is lesser statistically significant due to the wider interval.
In contrast, the HS model reveals a more robust and consistent trend across all air quality levels. Within the Fair category, the relative risk already reaches 1.08 (95% CI: 1.06–1.12), clearly surpassing the equivalent figure in the admissions model. In the Moderate range, the effect intensifies significantly, with RRs of 1.16 (95% CI: 1.10–1.22) and 1.21 (95% CI: 1.13–1.29). These values highlight a substantial increase in health burden. In the Poor air quality level, the impact remains pronounced with relative risks such as 1.21 (95% CI: 1.13–1.29) and 1.16 (95% CI: 1.09–1.24). Even within the Very Poor category, the model shows persistently elevated risks, including 1.10 (95% CI: 1.04–1.16) and 1.06 (95% CI: 1.00–1.11). Finally, in the Extremely Poor category, the hospital burden peaks at a relative risk of 1.24 (95% CI: 1.07–1.43), providing strong evidence of significantly increased health strain under the worst pollution conditions.
These findings reflect a key distinction between the two outcomes. HA capture the incidence of acute responses requiring urgent care, while HS reflects the accumulation of all hospital stays on a given day, encompassing both the frequency and the duration of illness. The higher RRs observed in the burden model indicate that air pollution not only triggers more admissions, but also prolongs patient stays, suggesting more severe or slower-to-resolve clinical conditions. This results in greater stress on hospital infrastructure and highlights the more complex toll of pollution on public health.
Mechanistically, air pollution has been shown to induce systemic inflammation, oxidative stress, and immune dysfunction [
12,
13]. These effects may prolong recovery periods and exacerbate underlying diseases, particularly among older adults and individuals with chronic comorbidities. Consequently, hospital burden serves as a more sensitive and integrated indicator of overall health strain than admissions alone. This is further evidenced by the higher relative risks across nearly all air quality categories, where differences between the models range from 0.04 to 0.15.
These differences emphasize the broader societal costs of air pollution. While hospital admissions provide a partial measure of acute effects, hospital burden captures the enduring demand on healthcare resources. The greater sensitivity of this metric underlines its importance for surveillance and planning, especially in densely populated urban areas with sustained pollution levels.
4. Conclusions
The analysis confirms a clear and escalating association between worsening air quality and adverse health outcomes, observed both in terms of daily hospital admissions and the broader burden of hospital stays. While both indicators reflect increased risk under higher pollution levels, hospital stays consistently exhibit greater relative risks with stronger statistical confidence. This indicates that hospital burden more accurately captures the full spectrum of air pollution’s health effects, encompassing not only the occurrence of illness but also its severity and duration.
Importantly, this amplified hospital burden translates directly into increased healthcare costs, as longer and more intensive treatments significantly raise financial strain on the system. These findings underscore that the relative risk of hospital stays is not only a sensitive measure of health impact but also a critical economic signal. As such, hospital burden should be prioritized in public health assessments and used to inform policy decisions. Strengthening air quality regulations and reinforcing healthcare infrastructure are essential to mitigate both the clinical and economic toll of air pollution in urban environments.
Author Contributions
Conceptualization, A.K., K.-M.F., K.M., V.D.A. and P.N. methodology, A.K., K.-M.F., K.M., V.D.A. and P.N.; software, A.K.; validation, A.K., K.-M.F., K.M., V.D.A. and P.N.; formal analysis, A.K.; data curation, A.K.; writing—original draft preparation, A.K.; writing—review and editing, A.K., K.-M.F., K.M., V.D.A. and P.N.; visualization, A.K.; supervision, K.M., V.D.A. and P.N.; project administration, A.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to the use of fully anonymized hospital admission data, with no access to personal identifiers or direct involvement of human subjects.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on reasonable request from the corresponding author. Access is restricted due to confidentiality agreements with the data provider, as the data were obtained specifically for a PhD research project.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| GAA | Greater Athens Area |
| RR | Relative Risk |
| HA | Hospital Admissions |
| HS | Hospital Stays |
| RD | Respiratory Diseases |
| CVD | Cardiovascular Diseases |
| DLNM | Distributed Lag Non-linear Model |
References
- Atkinson, R.W.; Kang, S.; Anderson, H.R.; Mills, I.C.; Walton, H.A. Epidemiological time series studies of PM2.5 and daily mortality and hospital admissions: A systematic review and meta-analysis. Thorax 2014, 69, 660–665. [Google Scholar] [CrossRef] [PubMed]
- Manisalidis, I.; Stavropoulou, E.; Stavropoulos, A.; Bezirtzoglou, E. Environmental and Health Impacts of Air Pollution: A Review. Front. Public Health 2020, 8, 14. [Google Scholar] [CrossRef] [PubMed]
- Traini, E.; Huss, A.; Portengen, L.; Rookus, M.; Verschuren, W.M.M.; Vermeulen, R.C.H.; Bellavia, A. A Multipollutant Approach to Estimating Causal Effects of Air Pollution Mixtures on Overall Mortality in a Large, Prospective Cohort. Epidemiology 2022, 33, 514–522. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Etzel, R.A.; Su, H.; Huang, C.; Guo, Y.; Tong, S. Impact of ambient temperature on children’s health: A systematic review. Environ. Res. 2012, 117, 120–131. [Google Scholar] [CrossRef] [PubMed]
- Patz, J.A.; Campbell-Lendrum, D.; Holloway, T.; Foley, J.A. Impact of regional climate change on human health. Nature 2005, 438, 310–317. [Google Scholar] [CrossRef] [PubMed]
- European Environment Agency. European Air Quality Index. European Environment Agency. Available online: https://airindex.eea.europa.eu/AQI/index.html (accessed on 6 September 2025).
- Jiang, X.; Wei, P.; Luo, Y.; Li, Y. Air pollutant concentration prediction based on a CEEMDAN-FE-BiLSTM model. Atmosphere 2021, 12, 1452. [Google Scholar] [CrossRef]
- Wang, J.; Du, P.; Hao, Y.; Ma, X.; Niu, T.; Yang, W. An innovative hybrid model based on outlier detection and correction algorithm and heuristic intelligent optimization algorithm for daily air quality index forecasting. J. Environ. Manag. 2020, 255, 109855. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Wang, J.; Li, R.; Lu, H. Novel analysis–forecast system based on multi-objective optimization for air quality index. J. Clean. Prod. 2019, 208, 1365–1383. [Google Scholar] [CrossRef]
- Schwartz, J. The distributed lag between air pollution and daily deaths. Epidemiology 2000, 11, 320–326. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Leone, M. Attributable risk from distributed lag models. BMC Med. Res. Methodol. 2014, 14, 55. [Google Scholar] [CrossRef] [PubMed]
- Gilmour, P.S.; Rahman, I.; Donaldson, K.; MacNee, W. Histone acetylation regulates epithelial IL-8 release mediated by oxidative stress from environmental particles. Am. J. Physiol. Lung Cell. Mol. Physiol. 2003, 284, L533–L540. [Google Scholar] [CrossRef] [PubMed]
- Tamagawa, E.; Bai, N.; Morimoto, K.; Gray, C.; Mui, T.; Yatera, K.; Zhang, X.; Xing, L.; Li, Y.; Laher, I.; et al. Particulate matter exposure induces persistent lung inflammation and endothelial dysfunction. Am. J. Physiol. Lung Cell. Mol. Physiol. 2008, 295, L79–L85. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).