Predictors of Delirium with Agitation After Aortic Valve Replacement and Its Long-Term Consequences: An Observational File Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Preoperative and Operative Variables
3.2. Early Postoperative Adverse Events and Need for Resources
3.3. Independent Predictors of POD
3.4. Long-Term Effects of Postoperative Delirium
4. Discussion
4.1. Observed Rates of POD and Detection Methods
4.2. Predictors of POD
4.3. Long-Term Effects of POD
4.4. Treatment of POD
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Deblier, I.; Dossche, K.; Vanermen, A.; Mistiaen, W. Operation in the gray zone: Is SAVR still useful in patients aged between 75 and 80 years? Future Cardiol. 2024, 20, 849–858. [Google Scholar] [CrossRef]
- Mistiaen, W.; Deblier, I.; Dossche, K.; Vanermen, A. Clinical Outcomes after Surgical Aortic Valve Replacement in 681 Octogenarians: A Single-Center Real-World Experience Comparing the Old Patients with the Very Old Patients. Geriatrics 2024, 9, 44. [Google Scholar] [CrossRef]
- Wueest, A.S.; Berres, M.; Bettex, D.A.; Steiner, L.A.; Monsch, A.U.; Goettel, N. Independent External Validation of a Preoperative Prediction Model for Delirium After Cardiac Surgery: A Prospective Observational Cohort Study. J. Cardiothorac. Vasc. Anesth. 2023, 37, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Hoogma, D.F.; Milisen, K.; Rex, S.; Al Tmimi, L. Postoperative delirium: Identifying the patient at risk and altering the course: A narrative review. Eur. J. Anaesthesiol. Intensive Care 2023, 2, e0022. [Google Scholar] [CrossRef]
- Mossie, A.; Regasa, T.; Neme, D.; Awoke, Z.; Zemedkun, A.; Hailu, S. Evidence-Based Guideline on Management of Postoperative Delirium in Older People for Low Resource Setting: Systematic Review Article. Int. J. Gen. Med. 2022, 15, 4053–4065. [Google Scholar] [CrossRef]
- Jansen Klomp, W.W.; Nierich, A.P.; Peelen, L.M.; Brandon Bravo Bruinsma, G.J.; Dambrink, J.E.; Moons, K.G.M.; van’t Hof, A.W.J. Survival and quality of life after surgical aortic valve replacement in octogenarians. J. Cardiothorac. Surg. 2016, 11, 38. [Google Scholar] [CrossRef]
- Koster, S.; Hensens, A.G.; Schuurmans, M.J.; van der Palen, J. Consequences of delirium after cardiac operations. Ann. Thorac. Surg. 2012, 93, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Deblier, I.; Dossche, K.; Vanermen, A.; Mistiaen, W. The Outcomes for Different Biological Heart Valve Prostheses in Surgical Aortic Valve Replacement before and after the Introduction of Transcatheter Aortic Valve Implantation. Prosthesis 2024, 6, 708–725. [Google Scholar] [CrossRef]
- Böning, A.; Lutter, G.; Mrowczynski, W.; Attmann, T.; Bödeker, R.; Scheibelhut, C.; Cremer, J. Octogenarians undergoing combined aortic valve replacement and myocardial revascularization: Perioperative mortality and medium-term survival. Thorac. Cardiovasc. Surg. 2010, 58, 159–163. [Google Scholar] [CrossRef]
- Dell’Amore, A.; Aquino, T.M.; Pagliaro, M.; Lamarra, M.; Zussa, C. Aortic valve replacement with and without combined coronary bypass grafts in very elderly patients: Early and long-term results. Eur. J. Cardiothorac. Surg. 2012, 41, 491–498. [Google Scholar] [CrossRef][Green Version]
- Habib, A.M.; Hussain, A.; Jarvis, M.; Cowen, M.E.; Chaudhry, M.A.; Loubani, M.; Cale, A.; Ngaage, D.L. Changing clinical profiles and in-hospital outcomes of octogenarians undergoing cardiac surgery over 18 years: A single-centre experience. Interact. Cardiovasc. Thorac. Surg. 2019, 28, 602–606. [Google Scholar] [CrossRef]
- Oettinger, V.; Kaier, K.; von Zur Mühlen, C.; Zehender, M.; Bode, C.; Beyersdorf, F.; Stachon, P.; Bothe, W. Impact of Procedure Volume on the Outcomes of Surgical Aortic Valve Replacement. Thorac. Cardiovasc. Surg. 2024, 72, 173–180. [Google Scholar] [CrossRef]
- Tang, A.; Eitan, T.; Dewan, K.C.; Zhou, G.; Rosinski, B.F.; Koroukian, S.M.; Svensson, L.G.; Gillinov, A.M.; Soltesz, E.G. National outcomes for dementia patients undergoing cardiac surgery in a pre-structural era. J. Cardiothorac. Surg. 2024, 19, 628. [Google Scholar] [CrossRef]
- Eide, L.S.; Ranhoff, A.H.; Fridlund, B.; Haaverstad, R.; Hufthammer, K.O.; Kuiper, K.K.; Nordrehaug, J.E.; Norekvål, T.M.; CARDELIR Investigators. CARDELIR Investigators. Comparison of frequency, risk factors, and time course of postoperative delirium in octogenarians after transcatheter aortic valve implantation versus surgical aortic valve replacement. Am. J. Cardiol. 2015, 115, 802–809. [Google Scholar] [CrossRef] [PubMed]
- Lingehall, H.C.; Smulter, N.S.; Lindahl, E.; Lindkvist, M.; Engström, K.G.; Gustafson, Y.G.; Olofsson, B. Preoperative Cognitive Performance and Postoperative Delirium Are Independently Associated with Future Dementia in Older People Who Have Undergone Cardiac Surgery: A Longitudinal Cohort Study. Crit. Care Med. 2017, 45, 1295–1303. [Google Scholar] [CrossRef] [PubMed]
- Teller, J.; Gabriel, M.M.; Schimmelpfennig, S.D.; Laser, H.; Lichtinghagen, R.; Schäfer, A.; Fegbeutel, C.; Weissenborn, K.; Jung, C.; Hinken, L.; et al. Stroke, Seizures, Hallucinations and Postoperative Delirium as Neurological Complications after Cardiac Surgery and Percutaneous Valve Replacement. J. Cardiovasc. Dev. Dis. 2022, 9, 365. [Google Scholar] [CrossRef] [PubMed]
- Werner, A.; Conrads, H.; Rosenberger, J.; Creutzenberg, M.; Graf, B.; Foltan, M.; Blecha, S.; Stadlbauer, A.; Floerchinger, B.; Tafelmeier, M.; et al. Effects of Implementing an Enhanced Recovery After Cardiac Surgery Protocol with On-Table Extubation on Patient Outcome and Satisfaction-A Before-After Study. J. Clin. Med. 2025, 14, 352. [Google Scholar] [CrossRef]
- Crocker, E.; Beggs, T.; Hassan, A.; Denault, A.; Lamarche, Y.; Bagshaw, S.; Elmi-Sarabi, M.; Hiebert, B.; Macdonald, K.; Giles-Smith, L.; et al. Long-term effects of postoperative delirium in patients undergoing cardiac operation: A systematic review. Ann. Thorac. Surg. 2016, 102, 1391–1399. [Google Scholar] [CrossRef]
- Körber, M.I.; Schäfer, M.; Vimalathasan, R.; Mauri, V.; Iliadis, C.; Metze, C.; Freyhaus, H.T.; Rudolph, V.; Baldus, S.; Pfister, R. Periinterventional inflammation and blood transfusions predict postprocedural delirium after percutaneous repair of mitral and tricuspid valves. Clin. Res. Cardiol. 2021, 110, 1921–1929. [Google Scholar] [CrossRef]
- Shahabi Raberi, V.; Solati Kooshk Qazi, M.; Zolfi Gol, A.; GhorbaniNia, R.; Kahourian, O.; Faramarz Zadeh, R. Postoperative Delirium and Dementia in Patients Undergoing Cardiac Surgery: A Review of Randomized Controlled Trials. Galen Med. J. 2023, 12, e3045. [Google Scholar] [CrossRef]
- Eggebrecht, H.; Bestehorn, K.; Rassaf, T.; Bestehorn, M.; Voigtländer, T.; Fleck, E.; Schächinger, V.; Schmermund, A.; Mehta, R.H. In-hospital outcomes after transcatheter or surgical aortic valve replacement in younger patients less than 75 years old: A propensity-matched comparison. EuroIntervention 2018, 14, 50–57. [Google Scholar] [CrossRef]
- Taghiyev, Z.T.; Bechtel, M.; Schlömicher, M.; Useini, D.; Taghi, H.N.; Moustafine, V.; Strauch, J.T. Early-Term Results of Rapid-Deployment Aortic Valve Replacement versus Standard Bioprosthesis Implantation Combined with Coronary Artery Bypass Grafting. Thorac. Cardiovasc. Surg. 2023, 71, 519–527. [Google Scholar] [CrossRef]
- Instenes, I.; Fridlund, B.; Amofah, H.A.; Ranhoff, A.H.; Eide, L.S.; Norekvål, T.M. ‘I hope you get normal again’: An explorative study on how delirious octogenarian patients experience their interactions with healthcare professionals and relatives after aortic valve therapy. Eur. J. Cardiovasc. Nurs. 2019, 18, 224–233. [Google Scholar] [CrossRef]
- Browndyke, J.N.; Tomalin, L.E.; Erus, G.; Overbey, J.R.; Kuceyeski, A.; Moskowitz, A.J.; Bagiella, E.; Iribarne, A.; Acker, M.; Mack, M.; et al. Cardiothoracic Surgical Trials Network (CTSN) Investigators. Infarct-related structural disconnection and delirium in surgical aortic valve replacement patients. Ann. Clin. Transl. Neurol. 2024, 11, 263–277. [Google Scholar] [CrossRef]
- Méndez-Martínez, C.; Casado-Verdejo, I.; Fernández-Fernández, J.A.; Sánchez-Valdeón, L.; Bello-Corral, L.; Méndez-Martínez, S.; Sandoval-Diez, A.; Gómez-Salgado, J.; García-Suárez, M.; Fernández-García, D. Projection ofvisual material on postoperative delirium in patients undergoing cardiac surgery: A double blind randomized clinical trial. Medicine 2024, 103, e39470. [Google Scholar] [CrossRef]
- Messé, S.R.; Overbey, J.R.; Thourani, V.H.; Moskowitz, A.J.; Gelijns, A.C.; Groh, M.A.; Mack, M.J.; Ailawadi, G.; Furie, K.L.; Southerland, A.M.; et al. Cardiothoracic Surgical Trials Network (CTSN) Investigators. The impact of perioperative stroke and delirium on outcomes after surgical aortic valve replacement. J. Thorac. Cardiovasc. Surg. 2024, 167, 624–633.e4. [Google Scholar] [CrossRef]
- Amofah, H.A.; Broström, A.; Fridlund, B.; Bjorvatn, B.; Haaverstad, R.; Hufthammer, K.O.; Kuiper, K.K.; Ranhoff, A.H.; Norekvål, T.M.; On Behalf of the CARDELIR Investigators. Sleep in octogenarians during the postoperative phase after transcatheter or surgical aortic valve replacement. Eur. J. Cardiovasc. Nurs. 2016, 15, 168–177. [Google Scholar] [CrossRef] [PubMed]
- Lopez, M.G.; Hughes, C.G.; DeMatteo, A.; O’Neal, J.B.; McNeil, J.B.; Shotwell, M.S.; Morse, J.; Petracek, M.R.; Shah, A.S.; Brown, N.J.; et al. Intraoperative Oxidative Damage and Delirium after Cardiac Surgery. Anesthesiology 2020, 132, 551–561. [Google Scholar] [CrossRef]
- Rudolph, J.L.; Jones, R.N.; Levkoff, S.E.; Rockett, C.; Inouye, S.K.; Sellke, F.W.; Khuri, S.F.; Lipsitz, L.A.; Ramlawi, B.; Levitsky, S.; et al. Derivation and validation of a preoperative prediction rule for delirium after cardiac surgery. Circulation 2009, 119, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Fong, T.G.; Davis, D.; Growdon, M.E.; Albuquerque, A.; Inouye, S.K. The interface of delirium and dementia in older persons. Lancet 2015, 14, 823–832. [Google Scholar] [CrossRef] [PubMed]
- Au, E.; Thangathurai, G.; Saripella, A.; Yan, E.; Englesakis, M.; Nagappa, M.; Chung, F. Postoperative Outcomes in Elderly Patients Undergoing Cardiac Surgery with Preoperative Cognitive Impairment: A Systematic Review and Meta-Analysis. Anesth. Analg. 2023, 136, 1016–1028. [Google Scholar] [CrossRef] [PubMed]
- Ko, C.C.; Hung, K.C.; Chang, Y.P.; Liu, C.C.; Cheng, W.J.; Wu, J.Y.; Li, Y.-Y.; Lin, T.-C.; Sun, C.-K. Association of general anesthesia exposure with risk of postoperative delirium in patients receiving transcatheter aortic valve replacement: A meta-analysis and systematic review. Sci. Rep. 2023, 13, 16241. [Google Scholar] [CrossRef]
- Stavridis, D.; Runkel, A.; Starvridou, A.; Fischer, J.; Fazzini, L.; Kirov, H.; Wacker, M.; Wippermann, J.; Doenst, T.; Caldonazo, T. Postoperative delirium in patients undergoing TAVI versus SAVR—A systematic review and meta-analysis. Int. J. Cardiol. Heart Vasc. 2024, 55, 101544. [Google Scholar] [CrossRef]
- Sadlonova, M.; Vogelgsang, J.; Lange, C.; Günther, I.; Wiesent, A.; Eberhard, C.; Ehrentraut, J.; Kirsch, M.; Hansen, N.; Esselmann, H.; et al. Identification of risk factors for delirium, cognitive decline, and dementia after cardiac surgery (FINDERI-find delirium risk factors): A study protocol of a prospective observational study. BMC Cardiovasc. Disord. 2022, 22, 299. [Google Scholar] [CrossRef]
- Deblier, I.; Dossche, K.; Vanermen, A.; Mistiaen, W. Dementia Development during Long-Term Follow-Up after Surgical Aortic Valve Replacement with a Biological Prosthesis in a Geriatric Population. J. Cardiovasc. Dev. Dis. 2024, 11, 136. [Google Scholar] [CrossRef]
- DiMeglio, M.; Furey, W.; Hajj, J.; Lindekens, J.; Patel, S.; Acker, M.; Bavaria, J.; Szeto, W.Y.; Atluri, P.; Haber, M.; et al. Observational study of long-term persistent elevation of neurodegeneration markers after cardiac surgery. Sci. Rep. 2019, 9, 7177. [Google Scholar] [CrossRef]
- Medeiros, R.; Baglietto-Vargas, D.; LaFerla, F.M. The role of tau in Alzheimer’s disease and related disorders. CNS Neurosci. Ther. 2011, 17, 514–524. [Google Scholar] [CrossRef]
- Amofah, H.A.; Broström, A.; Instenes, I.; Fridlund, B.; Haaverstad, R.; Kuiper, K.; Ranhoff, A.H.; Norekvål, T.M. CARDELIR Investigators. Octogenarian patients’ sleep and delirium experiences in hospital and four years after aortic valve replacement: A qualitative interview study. BMJ Open 2021, 11, e039959. [Google Scholar] [CrossRef] [PubMed]
- Hoogma, D.F.; Venmans, E.; Al Tmimi, L.; Tournoy, J.; Verbrugghe, P.; Jacobs, S.; Fieuws, S.; Milisen, K.; Adriaenssens, T.; Dubois, C.; et al. Postoperative delirium and quality of life after transcatheter and surgical aortic valve replacement: A prospective observational study. J. Thorac. Cardiovasc. Surg. 2023, 166, 156–166.e6. [Google Scholar] [CrossRef] [PubMed]
- Ozga, D.; Krupa, S.; Witt, P.; Mędrzycka-Dąbrowska, W. Nursing Interventions to Prevent Delirium in Critically Ill Patients in the Intensive Care Unit during the COVID19 Pandemic-Narrative Overview. Healthcare 2020, 8, 578. [Google Scholar] [CrossRef]
- Lange, S.; Mȩdrzycka-Dabrowska, W.; Friganović, A.; Religa, D.; Krupa, S. Family experiences and attitudes toward care of ICU patients with delirium: A scoping review. Front. Public Health 2022, 10, 1060518. [Google Scholar] [CrossRef] [PubMed]
- Krewulak, K.D.; Hiploylee, C.; Ely, E.W.; Stelfox, H.T.; Inouye, S.K.; Fiest, K.M. Adaptation and Validation of a Chart-Based Delirium Detection Tool for the ICU (CHART-DEL-ICU). J. Am. Geriatr. Soc. 2021, 69, 1027–1034. [Google Scholar] [CrossRef] [PubMed]
| Factor | Absent (%) | Present (%) | OR (CI) | p |
|---|---|---|---|---|
| Preoperative | ||||
| Age > 80 | 94/1036 (9.1) | 89/491 (18.1) | 2.22 (1.62–3.03) | <0.001 |
| Male gender | 51/610 (8.4) | 132/917 (14.4) | 1.84 (1.31–2.59) | <0.001 |
| Peripheral art disease | 119/1139 (10.4) | 64/387 (16.5) | 1.70 (1.22–2.36) | 0.001 |
| Myocardial infarction | 145/1277 (11.4) | 38/247 (15.4) | 1.42 (0.96–2.09) | 0.002 |
| Atrial fibrillation | 120/1124 (10.7) | 63/402 (15.7) | 1.55 (1.12–2.16) | 0.008 |
| TIA | 167/1443 (11.6) | 16/77 (20.8) | 2.00 (1.13–3.56) | 0.016 |
| Era after 2008 | 22/282 (7.8) | 161/1245 (12.9) | 1.76 (1.10–2.80) | 0.017 |
| LVEF < 50% | 87/786 (11.1) | 37/217 (17.1) | 1.65 (1.09–2.51) | 0.018 |
| Non-elective SAVR | 138/1248 (11.0) | 45/279 (16.1) | 1.55 (1.07–2.23) | 0.018 |
| eGFR < 60 mL/min | 101/940 (10.7) | 66/437 (15.1) | 1.48 (1.06–2.06) | 0.021 |
| Smoking | 133/1210 (11.0) | 47/298 (15.8) | 1.52 (1.06–2.17) | 0.023 |
| FEV1 < 80% | 120/1088 (11.0) | 62/406 (15.3) | 1.45 (1.05–2.02) | 0.026 |
| CVA | 153/1350 (11.3) | 30/176 (17.0) | 1.61 (1.05–2.47) | 0.028 |
| Congestive HF | 123/1127 (10.9) | 60/398 (15.1) | 1.45 (1.04–2.02) | 0.028 |
| NYHA class IV | 87/715 (12.2) | 33/205 (16.1) | 1.58 (1.02–2.43) | 0.038 |
| Coronary art disease | 57/577 (9.9) | 126/950 (13.2) | 1.40 (1.00–1.94) | 0.048 |
| LV hypertrophy | 11/159 (6.9) | 153/1255 (12.2) | 1.87 (0.99–3.53) | 0.050 |
| Carotid art surgery | 169/1453 (11.6) | 14/73 (19.2) | 1.80 (0.99–3.30) | 0.053 |
| Diabetes mellitus | 128/1148 (11.1) | 55/379 (14.5) | 1.35 (0.96–1.90) | 0.081 |
| Prior PPM implant | 170/1456 (11.7) | 13/71 (18.3) | 1.70 (0.91–3.16) | 0.093 |
| Emergent SAVR | 165/1420 (11.6) | 18/106 (17.0) | 1.56 (0.91–2.65) | 0.101 |
| Ventricular arrhythmia | 153/1331 (11.5) | 30/194 (15.5) | 1.41 (0.92–2.15) | 0.112 |
| Prior PCI | 151/1310 (11.5) | 32/217 (14.7) | 1.33 (0.88–2.00) | 0.176 |
| Prior CABG | 172/1396 (12.3) | 11/131 (8.4) | 0.65 (0.34–1.22) | 0.186 |
| Carotid art disease | 143/1238 (11.6) | 40/289 (13.8) | 1.23 (0.84–1.79) | 0.280 |
| Arterial hypertension | 42/388 (10.8) | 141/1135 (12.4) | 1.17 (0.81–1.68) | 0.403 |
| Hyperlipidemia | 72/576 (12.5) | 106/930 (11.4) | 0.90 (0.65–1.24) | 0.520 |
| Malignancy | 148/1261 (11.7) | 34/260 (13.1) | 1.13 (0.76–1.69) | 0.544 |
| Pulmonary art hypert | 125/1088 (11.5) | 47/373 (12.6) | 1.11 (0.78–1.59) | 0.565 |
| Prior SAVR | 179/1490 (12.0) | 4/37 (10.8) | 0.89 (0.31–2.54) | 0.824 |
| Conduction defect | 122/1022 (11.9) | 61/503 (12.1) | 1.02 (0.73–1.41) | 0.915 |
| Obesity | 131/1101 (11.9) | 48/406 (11.8) | 0.99 (0.70–1.41) | 0.968 |
| Operative | ||||
| CPB time > 120 min | 68/744 (9.1) | 97/637 (15.2) | 1.86 (1.28–2.48) | <0.001 |
| ACC > 60 min | 41/477 (8.6) | 106/770 (13.8) | 1.70 (1.16–2.48) | 0.006 |
| Partial sternotomy | 177/1409 (12.6) | 6/116 (5.2) | 0.38 (0.16–0.88) | 0.019 |
| Concomitant CABG | 60/618 (9.7) | 123/909 (13.5) | 1.46 (1.05–2.02) | 0.024 |
| Ascending aorta | 161/1392 (11.5) | 22/133 (16.5) | 1.52 (0.93–2.46) | 0.092 |
| Incomplete revasc | 159/1363 (11.7) | 22/155 (14.2) | 1.25 (0.77–2.03) | 0.357 |
| Mitral valve repair | 171/1444 (11.8) | 12/83 (14.5) | 1.26 (0.67–2.37) | 0.476 |
| Small valve | 178/1499 (11.9) | 4/25 (16.0) | 1.41 (0.48–4.17) | 0.528 |
| Concomintant CEA | 179/1494 (12.0) | 4/33 (12.1) | 1.01 (0.35–2.92) | 0.980 |
| Factor | Absent (%) | Present (%) | OR (CI) | p |
|---|---|---|---|---|
| Lab values | ||||
| pO2 < 80 mm Hg | 64/756 (8.5) | 117/736 (15.9) | 2.04 (1.48–2.82) | <0.001 |
| Glycemia > 160 mg% | 66/716 (9.2) | 112/776 (14.4) | 1.66 (1.20–2.29) | 0.002 |
| Low thrombocytes (HIT) | 144/1311 (11.0) | 39/214 (18.2) | 1.81 (1.23–2.66) | 0.003 |
| Hematocrit < 25% | 73/711 (10.3) | 107/790 (13.5) | 1.37 (1.00–1.88) | 0.051 |
| Need for resources | ||||
| Stay in ICU > 1 day | 64/1040 (6.2) | 123/487 (25.3) | 4.97 (3.59–6.89) | <0.001 |
| Need for RRT | 154/1437 (10.7) | 29/85 (34.1) | 4.31 (2.67–6.96) | <0.001 |
| Need for revision | 164/1472 (11.1) | 19/55 (34.5) | 4.21 (2.36–7.51) | <0.001 |
| LOS postoperative > 8 d | 73/990 (7.4) | 108/521 (20.7) | 3.28 (2.39–4.52) | <0.001 |
| Low TC | 143/1323 (10.8) | 38/179 (21.2) | 2.22 (1.59–3.31) | <0.001 |
| Need for >4 Units PC | 112/1189 (9.4) | 69/315 (21.9) | 2.70 (1.94–3.75) | <0.001 |
| Need for TC concentrate | 143/1323 (10.8) | 38/179 (21.2) | 2.22 (1.49–3.31) | <0.001 |
| Need for plasma | 107/1074 (10.0) | 74/428 (17.3) | 1.98 (1.37–2.60) | <0.001 |
| Ventilation < 8 h | 87/920 (9.5) | 91/578 (15.7) | 1.79 (1.31–2.45) | <0.001 |
| Need for PPM implant | 172/1480 (11.6) | 11/47 (23.4) | 2.32 (1.16–4.65) | 0.014 |
| Adverse events | ||||
| Pulmonary | 107/1261 (8.5) | 76/266 (28.6) | 4.31 (3.10–6.01) | <0.001 |
| Congestive heart failure | 140/1388 (10.1) | 43/138 (31.2) | 4.03 (2.70–6.02) | <0.001 |
| Bleeding | 150/1256 (11.9) | 33/121 (27.3) | 3.14 (2.03–4.85) | <0.001 |
| Acute renal injury | 96/1031 (9.3) | 87/309 (28.2) | 3.02 (2.20–4.15) | <0.001 |
| Ventricular arrhythmia | 167/1466 (11.4) | 16/61 (26.2) | 2.77 (1.53–5.00) | <0.001 |
| Atrial fibrillation | 92/925 (9.9) | 91/602 (15.1) | 1.61 (1.18–2.20) | 0.002 |
| Myocardial infarction | 177/1333 (13.3) | 6/17 (35.3) | 4.11 (1.50–11.25) | 0.003 |
| Conduction defect | 132/1218 (12.2) | 51/309 (16.5) | 1.62 (1.15–2.31) | 0.006 |
| Thromboembolism | 172/1297 (13.3) | 11/58 (19.0) | 1.76 (0.90–3.47) | 0.095 |
| Endocarditis | 182/1524 (11.9) | 1/3 (3.33) | 3.69 (0.33–40.86) | 0.254 |
| Predictor | OR | (95% CI) | p |
|---|---|---|---|
| Need for revision | 5.35 | 2.89–9.91 | <0.001 |
| Age above 80 years | 2.42 | 1.74–3.37 | <0.001 |
| Male gender | 1.68 | 1.17–2.40 | 0.005 |
| Peripheral artery disease | 1.61 | 1.14–2.28 | 0.007 |
| Smoking | 1.64 | 1.11–2.42 | 0.013 |
| Non-elective SAVR | 1.60 | 1.09–2.35 | 0.017 |
| Atrial fibrillation | 1.46 | 1.03–2.07 | 0.033 |
| TIA | 1.94 | 1.05–3.59 | 0.035 |
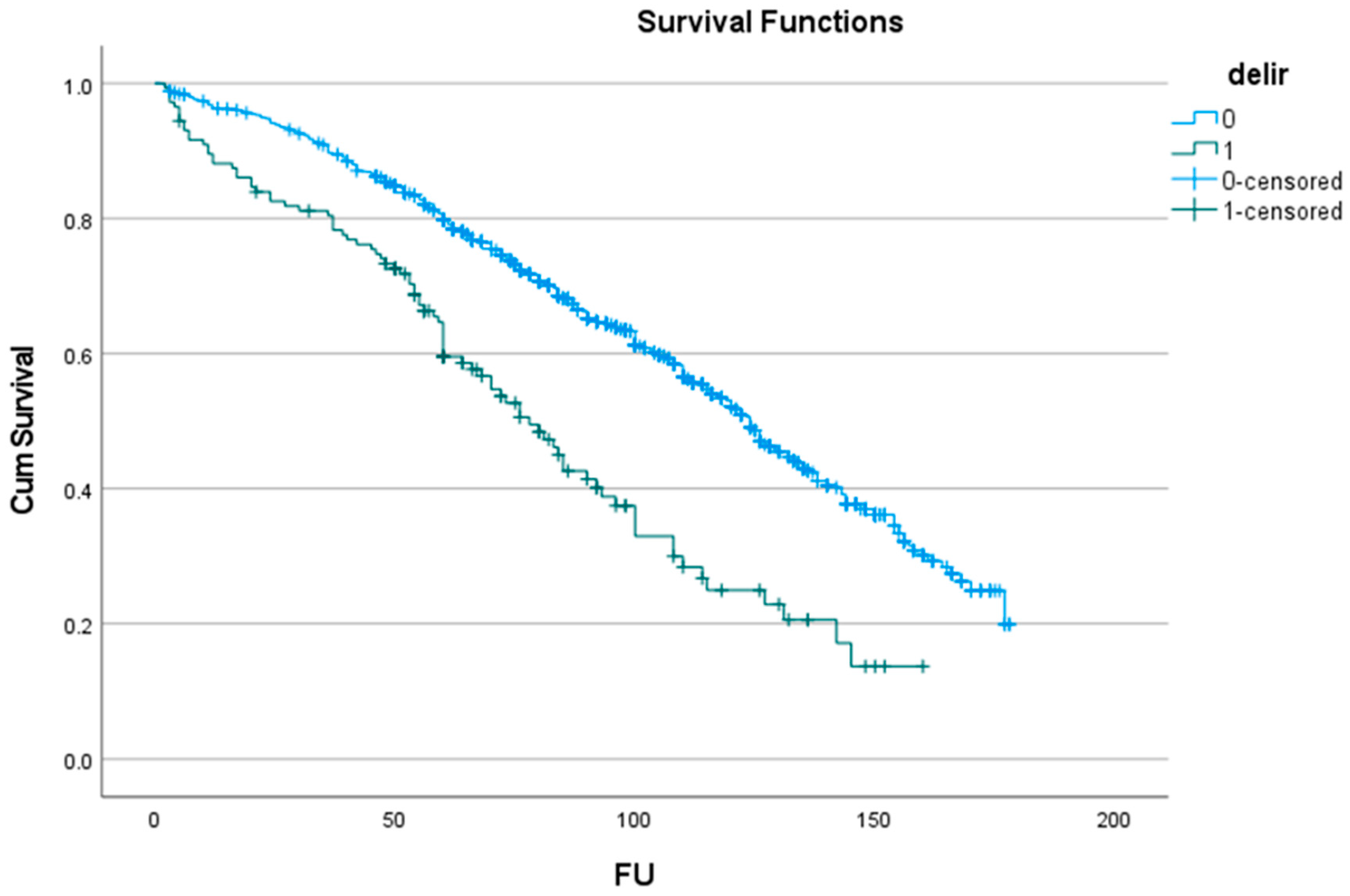
| No Delirium | (at Risk) | Delirium | (at Risk) | |
|---|---|---|---|---|
| 1 y | 96.3 ± 0.5% | (1165) | 89.5 ± 2.6% | (128) |
| 2 y | 94.1 ± 0.7% | (1141) | 82.5 ± 3.2% | (118) |
| 5 y | 79.8 ± 1.2% | (889) | 59.5 ± 4.3% | (75) |
| 10 y | 52.2 ± 1.8% | (258) | 24.9 ± 4.9% | (13) |
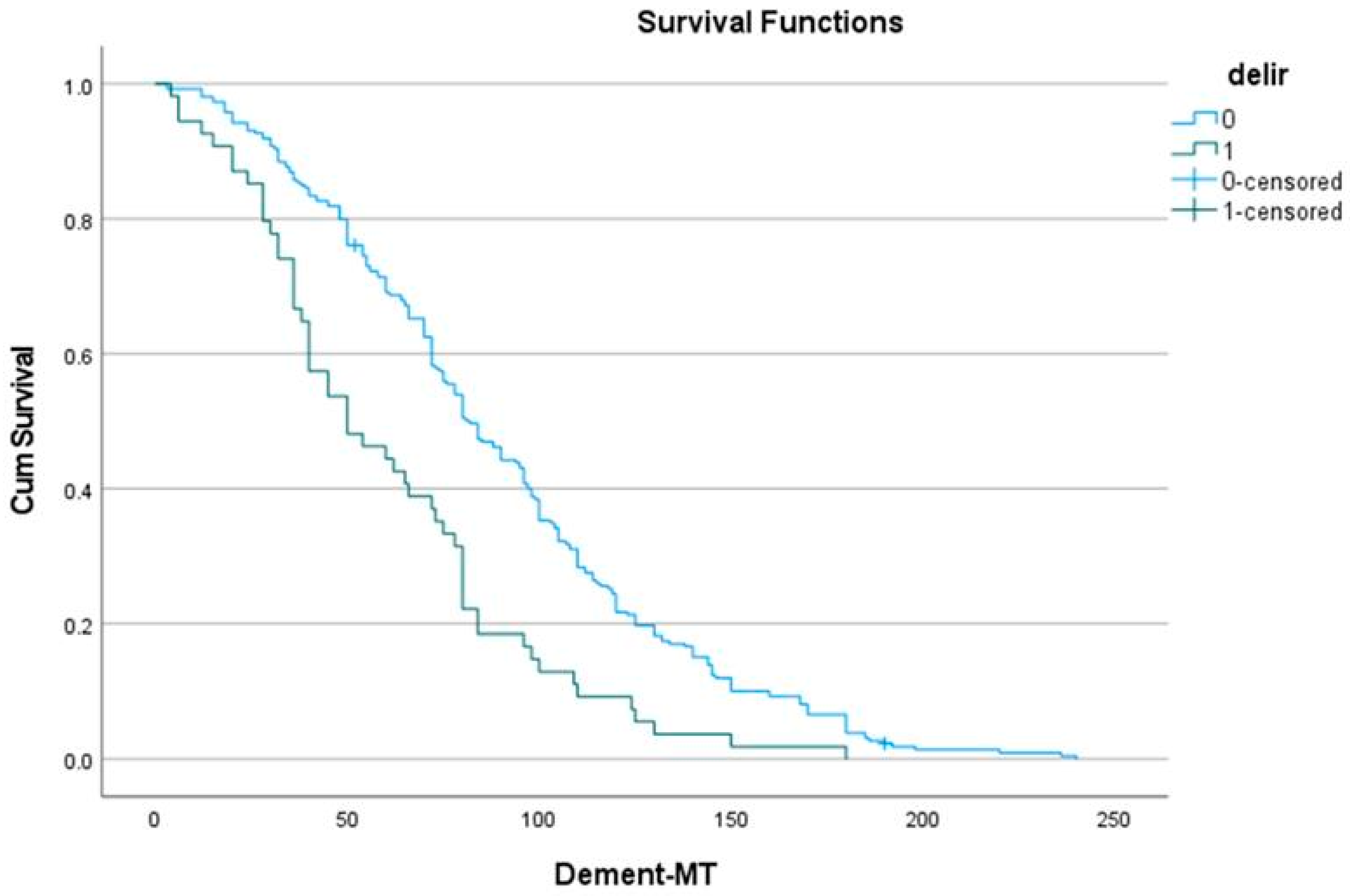
| No Delirium | (at Risk) | Delirium | (at Risk) | |
|---|---|---|---|---|
| 1 y | 98.1 ± 0.9 | (170) | 77.8 ± 5.7 | (40) |
| 2 y | 93.1 ± 1.6 | (158) | 85.2 ± 4.8 | (36) |
| 5 y | 69.1 ± 2.9 | (107) | 44.4 ± 6.8 | (17) |
| 10 y | 21.7 ± 6.3 | (18) | 7.4 ± 3.6 | (2) |
| Predictor | Hazard Ratio | 95% CI | p |
|---|---|---|---|
| Age over 80 years | 2.65 | 2.25–3.11 | <0.001 |
| Atrial fibrillation | 1.55 | 1.30–1.84 | <0.001 |
| Chronic pulmonary disease | 1.48 | 1.25–1.75 | <0.001 |
| Diabetes mellitus | 1.39 | 1.11–1.58 | <0.001 |
| Prior malignancy | 1.39 | 1.15–1.68 | <0.001 |
| Acute myocardial infarction | 1.33 | 1.08–1.65 | 0.007 |
| Atrioventricular block grade 1–2 | 1.41 | 1.07–1.85 | 0.015 |
| Postoperative delirium | 1.33 | 1.05–1.68 | 0.018 |
| CPB time > 120 min | 1.21 | 1.03–1.41 | 0.018 |
| Peripheral artery disease | 1.21 | 1.02–1.43 | 0.033 |
| Acute kidney injury | 1.22 | 1.01–1.47 | 0.039 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deblier, I.; Dossche, K.; Vanermen, A.; Mistiaen, W. Predictors of Delirium with Agitation After Aortic Valve Replacement and Its Long-Term Consequences: An Observational File Study. J. Dement. Alzheimer's Dis. 2025, 2, 45. https://doi.org/10.3390/jdad2040045
Deblier I, Dossche K, Vanermen A, Mistiaen W. Predictors of Delirium with Agitation After Aortic Valve Replacement and Its Long-Term Consequences: An Observational File Study. Journal of Dementia and Alzheimer's Disease. 2025; 2(4):45. https://doi.org/10.3390/jdad2040045
Chicago/Turabian StyleDeblier, Ivo, Karl Dossche, Anthony Vanermen, and Wilhelm Mistiaen. 2025. "Predictors of Delirium with Agitation After Aortic Valve Replacement and Its Long-Term Consequences: An Observational File Study" Journal of Dementia and Alzheimer's Disease 2, no. 4: 45. https://doi.org/10.3390/jdad2040045
APA StyleDeblier, I., Dossche, K., Vanermen, A., & Mistiaen, W. (2025). Predictors of Delirium with Agitation After Aortic Valve Replacement and Its Long-Term Consequences: An Observational File Study. Journal of Dementia and Alzheimer's Disease, 2(4), 45. https://doi.org/10.3390/jdad2040045







