Development of a Brief Screener for Crosscutting Patterns of Family Maltreatment and Psychological Health Problems
Abstract
1. Introduction
1.1. Overview
1.2. Identified Classes
1.3. Theoretical Framework
1.4. Implications for Screener Development
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.3.1. FM and PH Problems
2.3.2. Risk and Protective Factors
2.4. Analytic Strategy
2.5. Missing Data
3. Results
3.1. Step 1: Scale-Level Variable Selection
3.2. Step 2: Reducing the Number of Items
4. Discussion
4.1. Limitations
4.2. Implications for Use
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CA | Community Assessment |
| CART | Classification and Regression Tree |
| CES-D | Center for Epidemiological Studies Depression Scale |
| cp | Complexity Parameter |
| CS | Clinically Significant |
| DAF | Department of the Air Force |
| DM | Congressionally Directed Medical Research Program |
| FM | Family Maltreatment |
| IRT | Item Response Theory |
| LCA | Latent Class Analysis |
| NPV | Negative Predictive Value |
| PH | Psychological Health |
| PPV | Positive Predictive Value |
| PTS | Posttraumatic Stress |
| PTSD | Posttraumatic Stress Disorder |
| SM(s) | Service Member(s) |
Appendix A. R Code for Developing a Classification and Regression Tree
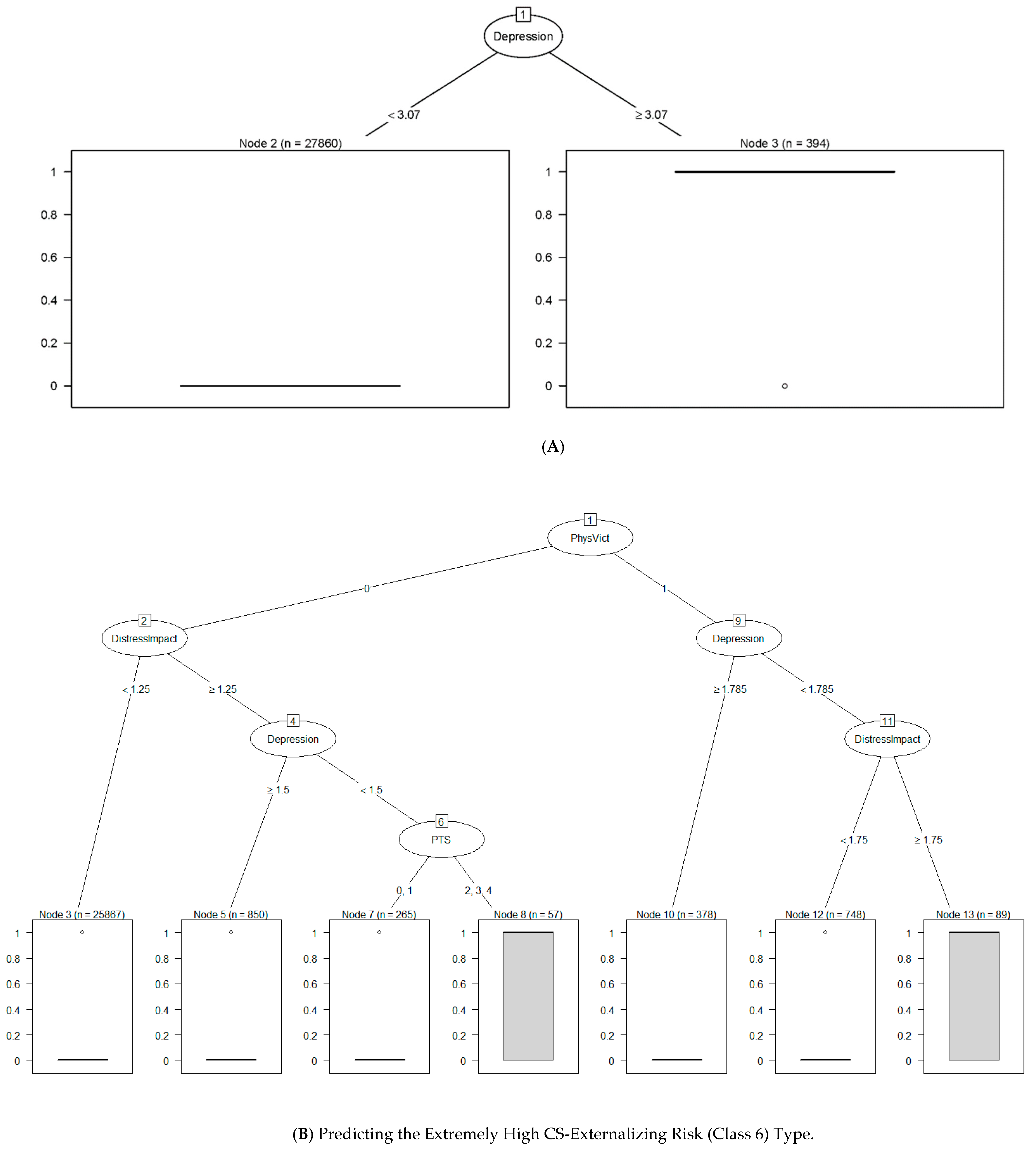
- # Note. PhysVict = partner physical abuse; DistressImpact = impact of stress and depression from partner emotional abuse victimization; PTS = posttraumatic stress disorder symptoms.>library(rpart)>library(partykit)
- # Import working data set>ca2011 = read.csv(“path\\exampledata.csv”, header = TRUE)>head(ca2011)
- # Define categorical variables, otherwise a variable will be treated as continuous>ca2011$PhysVict <- factor(ca2011$ PhysVict, levels = 0:1, labels = c(“0”, “1”))>ca2011$PTS <- factor(ca2011$PTS, levels = 0:4, labels = c(“0”, “1”, “2”, “3”, “4”))
- # Predicting class5 (a model before pruning)>cfit5<-rpart(class5~ PhysVict + PTS + Depression + DistressImpact, data = ca2011, method = ‘class’, na.action = na.rpart, control = rpart.control ( xval = 10, cp = 0, maxsurrogate = 5, minbucket = 0))# Using plot to select the optimal cp value for a final tree model>plotcp(cfit5)>summary(cfit5)>cfit1.re <-prune(cfit5, cp = 0.02)>summary(cfit5.re)# Plot the Resultant Tree>plot(as.party(cfit5.re))# Print out an error matrix>predict1<-predict(cfit5.re, type = “class”, data = ca2011)
Appendix B. Final Set of Screener Items for Predicting Crosscutting FM and PH Problems
| In your life, have you ever had any experience that was so frightening, horrible, or upsetting that, in the past month, you… | Yes (1) | No (0) |
| 🔾 | 🔾 |
| 🔾 | 🔾 |
| 🔾 | 🔾 |
| 🔾 | 🔾 |
| How many days during the past seven days have you… | None (0) | 1–2 days (1) | 3–4 days (1) | 5–7 days (1) |
| 🔾 | 🔾 | 🔾 | 🔾 |
| 🔾 | 🔾 | 🔾 | 🔾 |
| 🔾 | 🔾 | 🔾 | 🔾 |
| 🔾 | 🔾 | 🔾 | 🔾 |
| 🔾 | 🔾 | 🔾 | 🔾 |
| 🔾 | 🔾 | 🔾 | 🔾 |
| 🔾 | 🔾 | 🔾 | 🔾 |
| During the past year, my spouse/significant other… | Yes (1) | No (0) |
| 🔾 | 🔾 |
| 🔾 | 🔾 |
| 🔾 | 🔾 |
| 🔾 | 🔾 |
| 🔾 | 🔾 |
| 🔾 | 🔾 |
| 🔾 | 🔾 |
| Yes (1) | No (0) | |
| 🔾 | 🔾 |
| Almost All (1) | Most (1) | Some (1) | A Little (1) | Almost none or none (0) | |
| 🔾 | 🔾 | 🔾 | 🔾 | 🔾 |
| Yes (1) | No (0) | |
| 🔾 | 🔾 |
| Almost All (1) | Most (1) | Some (1) | A Little (1) | Almost none or none (0) | |
| 🔾 | 🔾 | 🔾 | 🔾 | 🔾 |
| Note. Substitute HWBFGF with husband, wife, boyfriend, or girlfriend as appropriate. | |||||
Appendix C. Scoring Rules for Predicting 6 Crosscutting FM and PH Problem Patterns
- /* Note. PhysVict = partner physical abuse; DistressImpact = impact of stress and depression from partner physical abuse victimization; PTS = posttraumatic stress disorder symptoms. */
- *Step 1: create scale-level variables;PTS = sum(of Item1, Item2, Item3, Item4);Depression = mean(of Item5, Item6, Item7, Item8, Item9, Item10,Item11);If ( Item12 = 1 or Item 13 = 1 or Item14 = 1 or Item15 = 1or Item16 = 1 or Item17 = 1 or Item18 = 1) then PhysVict = 1;else PhysVict = 0;If Item19 = 1 then Distress1 = 0;If Item19 = 0 then Distress1 = 6-Item20;If Item21 = 1 then Distress2 = 0;If Item21 = 0 then Distress2 = 6-Item22;DistressImpact = mean(of Distress1, Distress2);
- *Step 2: applying scoring algorithms;/*A predicted variable with value 1 indicates the presence of a given pattern, or class; otherwise, 0 indicates its absence. */*Class 1;*primary splitting values;If Depression >= 1.38 then Class1_pred = 0;If Depression < 1.38 then Class1_pred = 1;
- *Class 2;If Depression < 1.38 then Class2_pred = 0;If Depression >= 1.38 & Depression >= 1.85 then Class2_pred = 0;If Depression >= 1.38 & Depression < 1.85 then Class2_pred = 1;
- *Class 3;If Depression < 1.85 then Class3_pred = 0;If Depression >= 2.38 then Class3_pred = 0;If Depression >=1.85 & Depression < 2.38 then Class3_pred = 1;*Class 4;If Depression < 2.38 then Class4_pred = 0;If Depression >= 3.07 then Class4_pred = 0;If Depression >=2.38 & Depression < 3.07 then Class4_pred = 1;*Class 5;If Depression < 3.07 then Class5_pred = 0;If Depression >= 3.07 then Class5_pred = 1;*Class 6;If PhysVict = 0 & DistressImpact < 1.25 then Class6_pred = 0;If PhysVict = 0 & DistressImpact >= 1.25 & Depression >=1.5 then Class6_pred = 0;If PhysVict = 0 & DistressImpact >= 1.25 & Depression < 1.5 & (PTS = 0 or PTS = 1) then Class6_pred = 0;If PhysVict = 0 & DistressImpact >= 1.25 & Depression < 1.5 & (PTS = 2 or PTS =3 or PTS =4) then Class6_pred = 1;
- If PhysVict = 1 & Depression >= 1.79 then Class6_pred = 0;If PhysVict = 1 & Depression < 1.79 & DistressImpact < 1.75 then Class6_pred = 0;If PhysVict = 1 & Depression < 1.79 & DistressImpact >= 1.75 then Class6_pred = 1;
References
- Atwoli, L., Stein, D. J., Koenen, K. C., & McLaughlin, K. A. (2015). Epidemiology of posttraumatic stress disorder: Prevalence, correlates and consequences. Current Opinion in Psychiatry, 28(4), 307–311. [Google Scholar] [CrossRef]
- Bowen, G. L., Mancini, J. A., Martin, J. A., Ware, W. B., & Nelson, J. P. (2003). Promoting the adaptation of military families: An empirical test of a community practice model. Family Relations, 52(1), 33–44. [Google Scholar] [CrossRef]
- Breiman, L. (2001). Random forests. Machine Learning, 45, 5–32. [Google Scholar] [CrossRef]
- Breiman, L., Friedman, J., Stone, C. J., & Olshen, R. A. (1984). Classification and regression trees. CRC Press. [Google Scholar] [CrossRef]
- Brener, N. D., Kann, L., McManus, T., Kinchen, S. A., Sundberg, E. C., & Ross, J. G. (2002). Reliability of the 1999 youth risk behavior survey questionnaire. Journal of Adolescent Health, 31(4), 336–342. [Google Scholar] [CrossRef] [PubMed]
- Cai, H., Xie, X.-M., Zhang, Q., Cui, X., Lin, J.-X., Sim, K., Ungvari, G. S., Zhang, L., & Xiang, Y.-T. (2021). Prevalence of suicidality in major depressive disorder: A systematic review and meta-analysis of comparative studies. Frontiers in Psychiatry, 12, 690130. [Google Scholar] [CrossRef]
- Caliber Associates. (2003). 2003 air force community assessment: DAF survey results. Department of the Air Force. [Google Scholar]
- Caspi, A., & Moffitt, T. E. (2018). All for one and one for all: Mental disorders in one dimension. American Journal of Psychiatry, 175(9), 831–844. [Google Scholar] [CrossRef]
- Conger, R. D., Conger, K. J., Elder, G. H., Lorenz, F. O., Simons, R. L., & Whitbeck, L. B. (1993). Family economic stress and adjustment of early adolescent girls. Developmental Psychology, 29(2), 206–219. [Google Scholar] [CrossRef]
- Creech, S. K., & Misca, G. (2017). Parenting with PTSD: A review of research on the influence of PTSD on parent–child functioning in military and veteran families. Frontiers in Psychology, 8, 1101. [Google Scholar] [CrossRef]
- Eshima, N. (2022). An introduction to latent class analysis: Methods and applications. Springer. [Google Scholar] [CrossRef]
- Freisthler, B., & Gruenewald, P. J. (2013). Where the individual meets the ecological: A study of parent drinking patterns, alcohol outlets, and child physical abuse. Alcoholism: Clinical and Experimental Research, 37(6), 993–1000. [Google Scholar] [CrossRef]
- Funk, J. L., & Rogge, R. D. (2007). Testing the ruler with item response theory: Increasing precision of measurement for relationship satisfaction with the Couples Satisfaction Index. Journal of Family Psychology, 21(4), 572–583. [Google Scholar] [CrossRef] [PubMed]
- Goodkind, M., Eickhoff, S. B., Oathes, D. J., Jiang, Y., Chang, A., Jones-Hagata, L. B., Ortega, B. N., Zaiko, Y. V., Roach, E. L., Korgaonkar, M. S., Grieve, S. M., Galatzer-Levy, I., Fox, P. T., & Etkin, A. (2015). Identification of a common neurobiological substrate for mental illness. JAMA Psychiatry, 72(4), 305–315. [Google Scholar] [CrossRef]
- Gottschall, S., Lee, J. E. C., & McCuaig Edge, H. J. (2022). Adverse childhood experiences and mental health in military recruits: Exploring gender as a moderator. Journal of Traumatic Stress, 35(2), 659–670. [Google Scholar] [CrossRef]
- Hastie, T., Tibshirani, R., & Friedman, J. (2009). The elements of statistical learning: Data mining, inference, and prediction (2nd ed.). Springer. [Google Scholar]
- Heyman, R. E., Baucom, K. J. W., Xu, S., Slep, A. M. S., Snarr, J. D., Foran, H. M., Lorber, M. F., Wojda, A. K., & Linkh, D. J. (2021). High sensitivity and specificity screening for clinically significant intimate partner violence. Journal of Family Psychology, 35(1), 80–91. [Google Scholar] [CrossRef]
- Heyman, R. E., Slep, A. M. S., & Nelson, J. P. (2011). Empirically guided community intervention for partner abuse, child maltreatment, suicidality, and substance misuse. In S. M. Wadsworth, & D. Riggs (Eds.), Risk and resilience in US military families (pp. 85–107). Springer. [Google Scholar]
- Heyman, R. E., Snarr, J. D., Slep, A. M. S., Baucom, K. J. W., & Linkh, D. J. (2020). Self-reporting DSM-5/ICD-11 clinically significant intimate partner violence and child abuse: Convergent and response process validity. Journal of Family Psychology, 34(1), 101–111. [Google Scholar] [CrossRef]
- Inungu, J. N., MaloneBeach, L., Sultana, S., & Younis, M. Z. (2024). Trends and factors associated with depression among adults in the United States. European Journal of Environment and Public Health, 8(4), em0166. [Google Scholar] [CrossRef]
- James, G., Witten, D., Hastie, T., & Tibshirani, R. (2021). An introduction to statistical learning: With applications in R (2nd ed.). Springer. [Google Scholar]
- Klinkman, M. S., & Okkes, I. (1998). Mental health problems in primary care: A research agenda. The International Journal of Psychiatry in Medicine, 28(4), 361–374. [Google Scholar] [CrossRef]
- Kohavi, R. (1995, August 20–25). A study of cross-validation and bootstrap for accuracy estimation and model selection. 14th International Joint Conference on Artificial Intelligence (Vol. 2, pp. 1137–1143), Montreal, QC, Canada. Available online: https://www.researchgate.net/profile/Ron-Kohavi/publication/2352264_A_Study_of_Cross-Validation_and_Bootstrap_for_Accuracy_Estimation_and_Model_Selection/links/02e7e51bcc14c5e91c000000/A-Study-of-Cross-Validation-and-Bootstrap-for-Accuracy-Estimation-and-Model-Selection.pdf (accessed on 28 September 2025).
- Korolevskaia, A., & Yampolskaya, S. (2023). The consequences of childhood emotional abuse: A systematic review and content analysis. Families in Society, 104(2), 123–145. [Google Scholar] [CrossRef]
- Kotov, R., Krueger, R. F., Watson, D., Achenbach, T. M., Althoff, R. R., Bagby, R. M., Brown, T. A., Carpenter, W. T., Caspi, A., Clark, L. A., Eaton, N. R., Forbes, M. K., Forbush, K. T., Goldberg, D., Hasin, D., Hyman, S. E., Ivanova, M. Y., Lynam, D. R., Markon, K., … Zimmerman, M. (2017). The hierarchical taxonomy of psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126(4), 454–477. [Google Scholar] [CrossRef]
- Krause, N., & Baker, E. (1992). Financial strain, economic values, and somatic symptoms in later life. Psychology and Aging, 7(1), 4–14. [Google Scholar] [CrossRef]
- Krueger, R. F. (1999). The structure of common mental disorders. Archives of General Psychiatry, 56, 921–926. [Google Scholar] [CrossRef]
- Kuhn, M., & Johnson, K. (2013). Applied predictive modeling. Springer. [Google Scholar]
- Kuntsche, E., Kuntsche, S., Thrul, J., & Gmel, G. (2017). Binge drinking: Health impact, prevalence, correlates and interventions. Psychology & Health, 32(8), 976–1017. [Google Scholar] [CrossRef]
- Lawrence, E., Orengo-Aguayo, R., Langer, A., & Brock, R. L. (2012). The impact and consequences of partner abuse on partners. Partner Abuse, 3(4), 406–428. [Google Scholar] [CrossRef]
- Lorber, M. F., Heyman, R. E., & Slep, A. M. S. (2017). A longitudinal investigation of the psychological health of United States Air Force base communities. Journal of Community Psychology, 45(8), 1033–1049. [Google Scholar] [CrossRef]
- Lorber, M. F., Xu, S., Heyman, R. E., Slep, A. M. S., & Beauchaine, T. P. (2018). Patterns of psychological health problems and family maltreatment among United States Air Force members. Journal of Clinical Psychology, 74(7), 1258–1271. [Google Scholar] [CrossRef]
- MacKillop, J., Agabio, R., Feldstein Ewing, S. W., Heilig, M., Kelly, J. F., Leggio, L., Lingford-Hughes, A., Palmer, A. A., Parry, C. D., Ray, L., & Rehm, J. (2022). Hazardous drinking and alcohol use disorders. Nature Reviews Disease Primers, 8, 80. [Google Scholar] [CrossRef] [PubMed]
- Mathews, B., Pacella, R., Dunne, M. P., Simunovic, M., & Marston, C. (2020). Improving measurement of child abuse and neglect: A systematic review and analysis of national prevalence studies. PLoS ONE, 15(1), e0227884. [Google Scholar] [CrossRef]
- Mirowsky, J., & Ross, C. E. (1992). Age and depression. Journal of Health and Social Behavior, 33(2), 187–205. [Google Scholar] [CrossRef]
- Mitchell, A. J., Yadegarfar, M., Gill, J., & Stubbs, B. (2016). Case finding and screening clinical utility of the Patient Health Questionnaire (PHQ-9 and PHQ-2) for depression in primary care: A diagnostic meta-analysis of 40 studies. BJPsych Open, 2(2), 127–138. [Google Scholar] [CrossRef]
- Moradi, Y., Dowran, B., & Sepandi, M. (2021). The global prevalence of depression, suicide ideation, and attempts in the military forces: A systematic review and meta-analysis of cross-sectional studies. BMC Psychiatry, 21, 510. [Google Scholar] [CrossRef]
- Muthén, L. K., & Muthén, B. O. (2012). Mplus user’s guide (7th ed.). Muthén & Muthén. [Google Scholar]
- National Research Council and Institute of Medicine. (2009). Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities (M. E. O’Connell, T. Boat, & K. E. Warner, Eds.). National Academies Press. Available online: https://www.nap.edu/catalog/12480/preventing-mental-emotional-and-behavioral-disorders-among-young-people (accessed on 28 September 2025).
- Nichols, S. R., Rhoades, K. A., Lorber, M. F., Xu, S., Heyman, R. E., & Slep, A. M. S. (2023). Predictors of crosscutting patterns of psychological health and family maltreatment. Military Medicine, 188(9–10), 3134–3142. [Google Scholar] [CrossRef]
- Princeton Survey Research Associates. (1999). The community indicators survey—National: Topline results. Available online: https://www.icpsr.umich.edu/web/NADAC/studies/35578 (accessed on 28 September 2025).
- Prins, A., Ouimette, P., Kimerling, R., Cameron, R. P., Hugelshofer, D. S., Shaw-Hegwer, J., Thrailkill, A., Gusman, F. D., & Sheikh, J. I. (2003). The Primary Care PTSD Screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatry, 9(1), 9–14. [Google Scholar] [CrossRef]
- Putnick, D. L., & Bornstein, M. H. (2016). Measurement invariance conventions and reporting: The state of the art and future directions for psychological research. Developmental Review, 41, 71–90. [Google Scholar] [CrossRef]
- Rainio, O., & Kannasto, H. (2024). Evaluation metrics and statistical tests for machine learning. Scientific Reports, 14, 1234. [Google Scholar] [CrossRef]
- Research Triangle Institute. (1990). AFRP analysis plan (Vol. 2: Appendices). Research Triangle Institute. [Google Scholar]
- Rumpf, H., Hampke, U., Meyer, C., & John, U. (2002). Screening for alcohol use disorders and at-risk drinking in the general population: Psychometric performance of three questionnaires. Alcohol and Alcoholism, 37(3), 261–268. [Google Scholar] [CrossRef] [PubMed]
- Sadeh, N., Lusk, J., & Marx, B. P. (2017). Military trauma. In S. N. Gold (Ed.), APA handbook of trauma psychology: Foundations in knowledge (pp. 133–144). American Psychological Association. [Google Scholar] [CrossRef]
- Schepis, T. S., McCabe, S. E., & Ford, J. A. (2022). Recent trends in prescription drug misuse in the United States by age, race/ethnicity, and sex. The American Journal on Addictions, 31(5), 396–402. [Google Scholar] [CrossRef]
- Scholz, U., Doña, B. G., Sud, S., & Schwarzer, R. (2002). Is general self-efficacy a universal construct? Psychometric findings from 25 countries. European Journal of Psychological Assessment, 18(3), 242–251. [Google Scholar] [CrossRef]
- Segura, A., Heyman, R. E., & Slep, A. M. S. (2025). Intimate Partner Violence. In N. C. Overall, J. A. Simpson, & J. A. Lavner (Eds.), Research handbook of couple and family relationships (pp. 234–250). Edward Elgar Publishing. [Google Scholar] [CrossRef]
- Simons, R. L., Beaman, J., Conger, R. D., & Chao, W. (1993). Childhood experience, conceptions of parenting, and attitudes of spouse as determinants of parental behavior. Journal of Marriage and the Family, 55(1), 91–106. [Google Scholar] [CrossRef]
- Social Capital Community Benchmark Survey. (2000). Social capital community benchmark survey. Available online: https://ropercenter.cornell.edu/2000-social-capital-community-benchmark-survey (accessed on 28 September 2025).
- Streiner, D. L. (2003). Being inconsistent about consistency: When coefficient alpha does and doesn’t matter. Journal of Personality Assessment, 80(3), 217–222. [Google Scholar] [CrossRef] [PubMed]
- Strenio, J. (2019). Economic Considerations of Intimate Partner Violence. In R. Geffner, J. W. White, L. K. Hamberger, A. Rosenbaum, V. Vaughan-Eden, & V. I. Vieth (Eds.), Handbook of interpersonal violence and abuse across the lifespan. Springer. [Google Scholar] [CrossRef]
- Strobl, C., Malley, J., & Tutz, G. (2009). An introduction to recursive partitioning: Rationale, application, and characteristics of classification and regression trees, bagging, and random forests. Psychological Methods, 14(4), 323–348. [Google Scholar] [CrossRef]
- Taillieu, T. L., Brownridge, D. A., Sareen, J., & Afifi, T. O. (2016). Childhood emotional maltreatment and mental disorders: Results from a nationally representative adult sample from the United States. Child Abuse & Neglect, 59, 1–12. [Google Scholar] [CrossRef]
- Teicher, M. H., Samson, J. A., Anderson, C. M., & Ohashi, K. (2016). The effects of childhood maltreatment on brain structure, function and connectivity. Nature Reviews Neuroscience, 17(10), 652–666. [Google Scholar] [CrossRef]
- Therneau, T., Atkinson, B., & Ripley, B. (2023). rpart: Recursive partitioning and regression trees (R package version 4.1-23) [Computer software]. Comprehensive R Archive Network (CRAN). Available online: https://CRAN.R-project.org/package=rpart (accessed on 28 September 2025).
- Therneau, T. M., & Atkinson, E. J. (2023, December 5). An introduction to recursive partitioning: Using the RPART routines. Mayo Foundation. Available online: https://cran.r-project.org/web/packages/rpart/vignettes/longintro.pdf (accessed on 28 September 2025).
- U.S. Army Community and Support Center. (1989). 1989 Army soldier and family survey: Soldier survey (SCN: ATNC-AO-89-10A). Research Triangle Institute, Caliber Associates, and Human Resources Research Organization. [Google Scholar]
- Varma, S., & Simon, R. (2006). Bias in error estimation when using cross-validation for model selection. BMC Bioinformatics, 7, 91. [Google Scholar] [CrossRef]
- Vinokur, A. D., Price, R. H., & Caplan, R. D. (1996). Hard times and hurtful partners: How financial strain affects depression and relationship satisfaction of unemployed persons and their spouses. Journal of Personality and Social Psychology, 71(1), 166–179. [Google Scholar] [CrossRef] [PubMed]
- Ware, J. E., Jr., Kosinski, M., Dewey, J. E., & Gandek, B. (2001). How to score and interpret single-item health status measures: A manual for users of the SF-8TM health survey. QualityMetric Incorporated. [Google Scholar]
- White, S. J., Sin, J., Sweeney, A., Salisbury, T., Wahlich, C., Montesinos Guevara, C. M., Gillard, S., Brett, E., Allwright, L., Iqbal, N., Khan, A., Perot, C., Marks, J., & Mantovani, N. (2024). Global prevalence and mental health outcomes of intimate partner violence among women: A systematic review and meta-analysis. Trauma, Violence, & Abuse, 25(1), 494–511. [Google Scholar] [CrossRef]
- Williams, G. (2011). Data mining with Rattle and R: The art of excavating data for knowledge discovery. Springer. [Google Scholar]
- Winchester, B. R., Watkins, S. C., Brahm, N. C., Harrison, D. L., & Miller, M. J. (2013). Mental health treatment associated with community-based depression screening: Considerations for planning multidisciplinary collaborative care. Annals of Pharmacotherapy, 47(6), 797–804. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y., Jia, X., Yang, Y., Sun, N., Shi, S., & Wang, W. (2024). Change in the global burden of depression from 1990–2019 and its prediction for 2030. Journal of Psychiatric Research, 178, 16–22. [Google Scholar] [CrossRef] [PubMed]
| Scale | Items | M | SD | Min | Max | α | Scale | Items | M% | SD | Min | Max | α |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Partner emotional abuse a | 13 | 6.60% | – | 0 | 1 | – | Support from significant other | 3 | 5.09% | 0.93 | 1 | 6 | 0.84 |
| Partner physical abuse victimization a | 24 | 1.40% | – | 0 | 1 | – | Workgroup cohesion | 6 | 4.16% | 1.19 | 1 | 6 | 0.87 |
| Partner physical abuse perpetration a | 23 | 0.60% | – | 0 | 1 | – | Work relationship satisfaction | 5 | 4.27% | 0.99 | 1 | 6 | 0.73 |
| Child emotional abuse a | 16 | 3.20% | – | 0 | 1 | – | Community satisfaction | 15 | 4.12% | 0.98 | 1 | 6 | 0.86 |
| Child physical abuse a | 29 | 12.60% | – | 0 | 1 | – | Community unity | 14 | 4.12% | 0.91 | 1 | 6 | 0.95 |
| Hazardous drinking a | 10 | 7.70% | – | 0 | 1 | – | Support from neighbors | 5 | 4.03% | 1.29 | 1 | 6 | 0.87 |
| Prescription drug misuse a | 20 | 4.30% | – | 0 | 1 | – | Support from DAF agencies | 4 | 4.26% | 1.12 | 1 | 6 | 0.96 |
| Suicidal thoughts a | 5 | 2.20% | – | 0 | 1 | – | Social support | 4 | 4.33% | 1.52 | 1 | 6 | 0.95 |
| Suicidal behavior | 5 | 0.10% | – | 0 | 1 | – | Support for youth | 3 | 4.25% | 1.04 | 1 | 6 | 0.76 |
| Depression | 7 | 1.37 | 0.48 | 0 | 4 | 0.86 | Supportive leadership | 9 | 4.05% | 1.02 | 1 | 6 | 0.9 |
| Posttraumatic stress | 4 | 0.36 | 0.92 | 0 | 4 | – | Economic well-being | 2 | 1.59% | 0.81 | 1 | 5 | 0.87 |
| Personal coping | 9 | 4.18 | 0.48 | 1 | 4 | 0.89 | Physical well-being | 6 | 4.19% | 0.71 | 1 | 6.33 | 0.73 |
| Parent–child relationship satisfaction | 3 | 5.12 | 0.74 | 1 | 6 | 0.73 | Religious involvement | 5 | 3.36% | 0.99 | 1 | 5.67 | 0.69 |
| Family coping | 3 | 5.02 | 0.88 | 1 | 6 | 0.89 | Community safety | 4 | 5.15% | 0.79 | 1 | 6 | 0.74 |
| Class | Sensitivity | Specificity | PPV | NPV | Prevalence |
|---|---|---|---|---|---|
| All Scale-Level Predictors | |||||
| 1. Very Low Clinically Significant-Internalizing/Externalizing Risk | 0.996 | 0.978 | 0.989 | 0.992 | 65.6% |
| 2. Low Clinically Significant-Internalizing/Externalizing Risk | 0.981 | 0.996 | 0.983 | 0.996 | 19.4% |
| 3. Moderate Clinically Significant-Internalizing/Externalizing Risk | 0.993 | 0.999 | 0.989 | 0.999 | 9.3% |
| 4. High Clinically Significant-Internalizing/Externalizing Risk | 0.963 | 1.000 | 0.998 | 0.999 | 3.5% |
| 5. Very High Clinically Significant-Internalizing/Externalizing Risk | 1.000 | 0.999 | 0.901 | 1.000 | 1.1% |
| 6. Extremely High Clinically Significant- Externalizing Risk | 0.595 | 0.997 | 0.690 | 0.995 | 1.2% |
| 22-Item Brief Screener | |||||
| 1. Very Low Clinically Significant-Internalizing/Externalizing Risk | 0.999 | 0.978 | 0.987 | 1.000 | |
| 2. Low Clinically Significant-Internalizing/Externalizing Risk | 0.991 | 0.991 | 0.966 | 0.998 | |
| 3. Moderate Clinically Significant-Internalizing/Externalizing Risk | 0.974 | 0.998 | 0.989 | 0.997 | |
| 4. High Clinically Significant-Internalizing/Externalizing Risk | 0.963 | 0.999 | 0.999 | 0.999 | |
| 5. Very High Clinically Significant-Internalizing/Externalizing Risk | 1.000 | 0.998 | 0.901 | 1.000 | |
| 6. Extremely High Clinically Significant- Externalizing Risk | 0.255 | 0.997 | 0.582 | 0.991 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, S.; Lorber, M.F.; Heyman, R.E.; Slep, A.M.S. Development of a Brief Screener for Crosscutting Patterns of Family Maltreatment and Psychological Health Problems. Psychol. Int. 2025, 7, 83. https://doi.org/10.3390/psycholint7040083
Xu S, Lorber MF, Heyman RE, Slep AMS. Development of a Brief Screener for Crosscutting Patterns of Family Maltreatment and Psychological Health Problems. Psychology International. 2025; 7(4):83. https://doi.org/10.3390/psycholint7040083
Chicago/Turabian StyleXu, Shu, Micahel F. Lorber, Richard E. Heyman, and Amy M. Smith Slep. 2025. "Development of a Brief Screener for Crosscutting Patterns of Family Maltreatment and Psychological Health Problems" Psychology International 7, no. 4: 83. https://doi.org/10.3390/psycholint7040083
APA StyleXu, S., Lorber, M. F., Heyman, R. E., & Slep, A. M. S. (2025). Development of a Brief Screener for Crosscutting Patterns of Family Maltreatment and Psychological Health Problems. Psychology International, 7(4), 83. https://doi.org/10.3390/psycholint7040083






