1. Introduction
Dengue (pronounced “DEN-gi”) is one of the most rapidly spreading febrile illnesses caused by a Flavivirus, transmitted by mosquito vectors. This disease is prevalent in more than 120 countries worldwide. Its geographical distribution shows that the virus affects populations in the Americas, Southeast Asia (SEA), and the Western Pacific regions, with Asia accounting for 70% of the global disease burden [
1]. Approximately 400 million infections occur annually, with 100 million presenting clinical symptoms. Dengue is considered a growing threat to global health security due to its epidemic potential, especially in urban and tropical settings [
2]. The World Health Organization (WHO) has long recognized dengue as a significant public health concern due to its outbreak potential, along with its rapid geographic expansion and pressure on healthcare systems [
3].
Dengue was first identified in Bangladesh during a 1964 outbreak in Dhaka, recorded as “Dacca fever” [
4]. Although sporadic cases and limited outbreaks occurred between 1964 and 1999, they were not systematically documented [
1]. The disease became a major public health concern in 2000, with 5551 reported cases and 93 deaths, prompting the establishment of a Centre for Disease Control under the Directorate General of Health Services (DGHS). Since then, dengue has caused recurring large-scale outbreaks, most notably over 430,000 cases in 2019, followed by fluctuating annual trends, including 28,429 confirmed cases in 2021 [
5,
6,
7].
The CDC unit of the DGHS warned of a major outbreak in March 2019. As suspected, a nationwide outbreak began in April 2019 and has continued since. Dhaka city, the greater Dhaka district, and parts of the Chattogram Division were identified as infection hotspots [
8]. In 2019, dengue cases nearly doubled compared to the cumulative total of the previous 19 years [
9]. Unfortunately, the virus also spread into rural areas, primarily due to travelers [
10].
Following the historic outbreak in 2019, with over 430,000 reported cases, dengue incidence temporarily declined in 2020 (59,675 cases) and 2021 (28,429 cases), likely due to COVID-19 restrictions and reduced surveillance [
11,
12]. However, the disease rebounded sharply in 2022 and culminated in the deadliest outbreak in 2023, with over 300,000 cases and more than 1600 deaths, highlighting the growing threat of dengue amid rapid urbanization and climate variability [
13,
14].
DVI remains a significant public health challenge in Bangladesh, with frequent outbreaks placing a heavy burden on healthcare systems. Understanding the epidemiological aspects of dengue, including the demographic risk factors, seroprevalence, and clinical–immunological characteristics, is essential for improving disease management and control strategies. Comprehensive serological, clinical, and demographic data can help policymakers and public health officials effectively evaluate, control, and prevent future outbreaks [
15].
Dhaka, a megacity of over 19 million residents, has thousands of construction sites with pits that collect stagnant water during the monsoon season, creating ideal breeding grounds for mosquitoes. Additionally, limited public awareness, ineffective insecticides, and the absence of specific treatment and preventive measures contribute to the underestimated threats posed by ongoing and future outbreaks [
10]. Local spatial variations in rainfall, temperature, humidity, urbanization, and the quality of vector control services influence dengue risk in urban areas [
1]. Travel has also been identified as a factor contributing to the spread of viruses into rural regions [
10].
Numerous studies have identified potential risk factors for dengue transmission, including inadequate mosquito control practices, exposure to mosquito breeding sites (e.g., flowerpots and water containers), housing conditions, human mobility, and sociodemographic variables, such as age, sex, and occupation [
16,
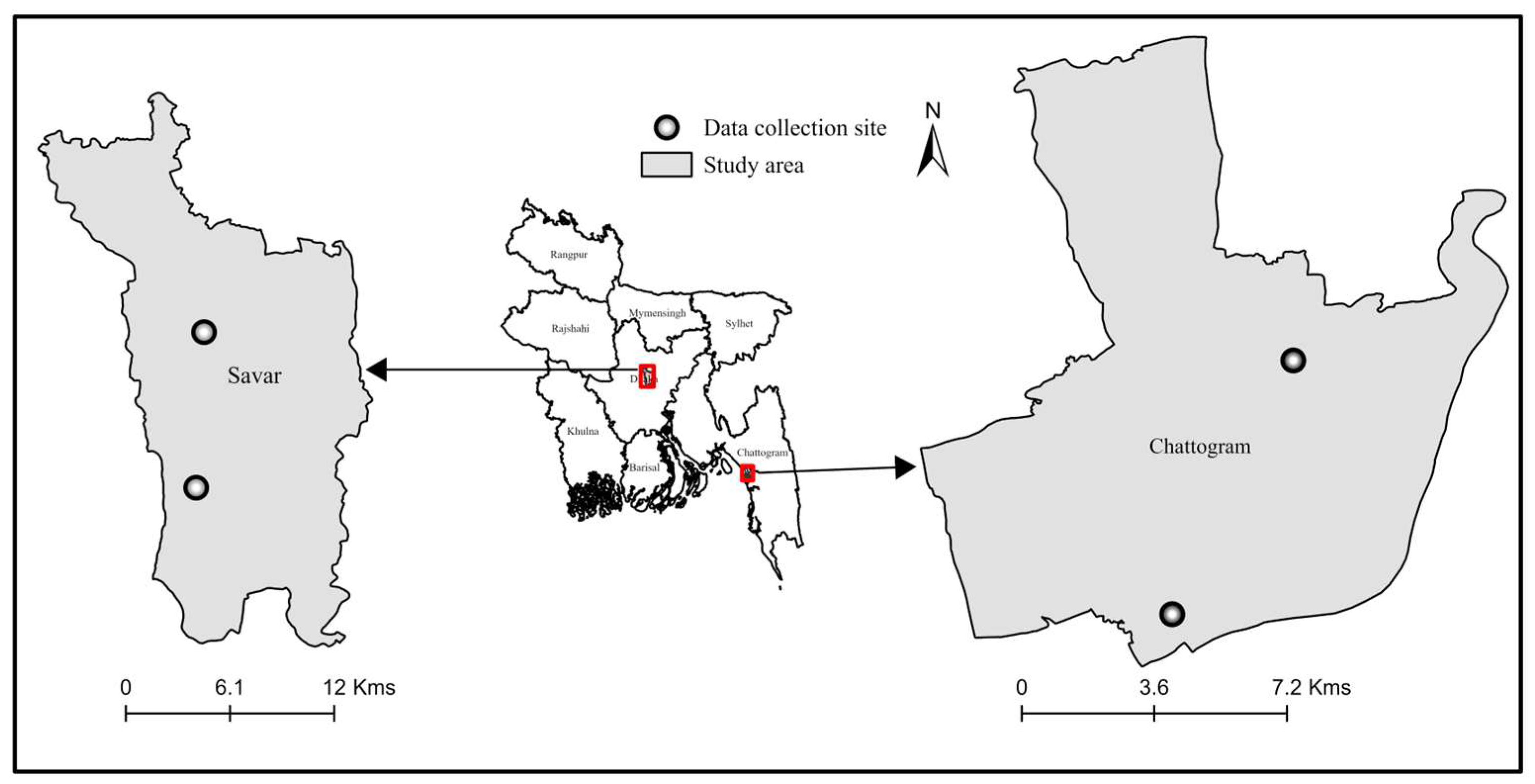
17]. However, given the limitations of hospital-based data, our study focused on a set of modifiable behavioral and environmental factors that could be extracted from patient records and that have been implicated in previous outbreaks in Bangladesh. In this study, we identified the area-specific risk factors associated with DVI among hospitalized patients in two urban centers of Bangladesh—Savar (Dhaka) and Chattogram—during the major outbreak of 2019. This study is going to inform targeted and locally appropriate dengue control strategies to minimize the knowledge gaps related to dengue burden, vulnerable populations, and health outcomes. These findings are essential for strengthening surveillance and guiding targeted intervention strategies in Bangladesh.
3. Results
3.1. Descriptive Analysis
Overall, 55.88% (475) of the total admissions (n = 850) tested positive for dengue, with 73.33% (330) of the cases from Savar and 36.25% (145) from Chattogram. Among the total, 51.17% (435 patients) were serologically positive for dengue-specific antigens and antibodies. Of these, 303 (67.33%) were from Savar and 132 (33%) were from Chattogram, based on the dengue NS1 antigen test.
Additionally, 5.17% (44 patients) tested positive for anti-dengue IgM and IgG antibodies. The proportion of IgM-positive patients was 6.2% (28/450) in Savar and 4% (16/400) in Chattogram. For IgG-positive cases, the overall proportion was 5.4% (46 patients), with 5.7% (26/450) from Savar and 5% (20/400) from Chattogram.
3.2. Number of Admissions
The number of admissions, number of dengue-positive cases, percentages of positive cases, and 95% confidence intervals for the proportions of positive cases under each category of each variable are presented separately for each area in
Table 1. Additionally, the table includes
p-values from chi-square tests assessing the independence of dengue-positive status from each factor.
In the Savar area, 450 admissions were recorded, while Chattogram reported 400 admissions. In both areas, a higher number of admissions occurred in private hospitals compared to government hospitals, with private hospital admissions accounting for 53% in Savar and 52% in Chattogram.
Regarding the month-wise distribution of admissions, both areas show similar patterns (
Figure S1). Very few admissions occurred between January and March. The first peak in admissions was observed in May, with 12% and 11% of the total monthly admissions in Savar and Chattogram, respectively. The second and most significant peak occurred in August, accounting for the highest number of admissions, 51% in Savar and 54% in Chattogram, which is more than four times the figures observed in May. As expected, the highest admissions were recorded during the rainy season in both areas, accounting for 72% in Savar and 75% in Chattogram (
Figure S2). The pre-monsoon season also showed a notable proportion of admissions, with 22% in Savar and 18% in Chattogram, while the winter season had the lowest admissions, approximately 6% in each area.
Urban areas in Savar and Chattogram had higher numbers of admissions than peri-urban areas. The ratio of urban-to-peri-urban admissions was roughly 56:44 in both regions (
Figure S3). Interestingly, male admissions were significantly higher than female admissions, more than double in both areas, with male patients comprising approximately 70% of admissions (
Figure S4).
Among the admitted patients, the majority reported no prior contact with known dengue patients (
Figure S5). In both Savar and Chattogram, approximately 95% of patients had not come into contact with someone diagnosed with dengue. Additionally, more than half of the admitted patients, 58% in Savar and 55% in Chattogram, did not use mosquito nets as a protective measure (
Figure S6). However, a large majority reported using mosquito repellents on the skin (92% in Savar and 93% in Chattogram) (
Figure S7), and a similarly high percentage reported using repellents inside the home (84% in Savar and 83% in Chattogram) (
Figure S8). These high usage rates indicate widespread use of repellents in both areas. Furthermore, about two-thirds (69%) of the admissions confirmed the absence of flowerpots inside their homes (
Figure S9).
3.3. Percentage of Positive Cases
In both Savar and Chattogram, the highest percentages of positive cases are reported by government hospitals, where a smaller number of admissions could be observed. The ratios of these percentages of positive cases between government and private hospitals are 79:68 and 41:32 in Savar and Chattogram, respectively.
The highest percentage, 100%, of positive cases was reported in October (five out of five), and it is followed by the next highest percentage, 92%, in September, and 90% in April in the Savar area. In June–August, the percentage remains in the range of 74–82%. The highest percentages (almost the same) of positive cases in Chattogram were reported in June and October, around 60%. Except for these two months, the percentages of positive cases in other months of this area are 7–45%, below 50%.
Similar to the number of admissions, the highest percentages of positive cases are in the rainy season of each area. Pre-monsoon seasons in both areas report the second-largest positive cases as a percentage. The percentages of positive cases in the rainy, pre-monsoon, and winter seasons are 83:56:22 and 39:29:22, respectively, in Savar and Chattogram. The percentages of positive cases are almost equal (72% and 74%) across peri-urban and urban areas in Savar. In Chattogram, the corresponding percentages are 31% and 40%, which are much smaller than in the Savar area. The gender-wise ratio (male–female) in percentages of positive cases is 73:72 in Savar. However, this ratio for Chattogram is much smaller, and it is 35:40.
In both areas, higher percentages of positive cases are shown by admissions with no previous contact with dengue patients, and this percentage is reasonably higher compared to the percentage of positive cases among persons who had contact with patients. These ratios are 76:21 and 38:9 in Savar and Chattogram, respectively.
Slight changes can be seen in the percentages of positive cases of people who used and did not use mosquito nets in both areas. They are 70:76 and 40:33, respectively. This ratio in Chattogram is considerably lower than in Savar. There was no considerable difference in the percentages of positive cases between those who used repellents in-house and those who did not. The ratio is 72:79 in Savar, while 34:48 is the ratio in Chattogram. According to the usage of repellents on the skin, we cannot observe a reasonable difference in percentages of positive cases under each level of usage in each area. They are, respectively, 73:73 and 36:39 for Savar and Chattogram (used–not used). Depending on the status of the availability of flower plots inside the house, no reasonable difference (73:74) can be observed in the percentages of positive cases for each level in Savar. However, in Chattogram, a slight change is visible (33:42).
Very interestingly, Savar has shown a higher percentage of positive cases out of admission (within a category), and most of these percentages are higher than 50%, which is confirmed by 95% confidence intervals. However, the corresponding percentages in Chattogram are below 50%, except in two situations (59% and 60%).
3.4. Results of Chi-Square Analysis
In Savar, dengue status (positive/negative) showed a significant association with hospital type, season, and prior contact with dengue patients. The findings indicate a strong dependence on seasonal variation and patient exposure (p < 0.001), highlighting their critical role in dengue transmission dynamics in this area.
In Chattogram, dengue status was significantly associated (p < 0.05) with prior contacts with dengue patients and in-house use of mosquito repellents, while the landscape was marginally significant.
3.5. Results of Logistic Regression Analysis
According to the logistic regression results, the dengue status in the Savar area is significantly influenced by patient contact, use of mosquito nets, and season. The significant constant term (intercept) suggests that additional, unaccounted factors might also influence dengue status in this area. No contact with dengue patients was associated with a 2.9-fold increase in the log odds of being dengue-positive (odds of being positive increased by 1888.56%) compared to those who had contact with infected individuals, which contradicts the general consensus on dengue transmission.
The use of mosquito nets was associated with a 59% reduction in the odds of testing positive for dengue compared to those who did not use mosquito nets. The use of mosquito nets was associated with a negative impact on the log of odds of dengue positivity, with individuals who used mosquito nets being 0.52 times less likely to be affected by dengue (odds of being positive decreased by 40.54%) compared to those who did not use nets. When comparing the seasonal effects, the rainy season had a positive impact (1.7 times) on the log of odds of being a positive dengue case (odds of being positive increased by 447.39%). The winter season showed a negative impact (−1.4 times) (odds of being positive decreased by 76.31%), compared to the pre-monsoon season as the baseline.
According to the logistic regression results (
Table 2), in Chattogram, the factors of contact with patients and use of repellents in the house are identified as significant at the 5% significance level. However, the effect of repellent use in houses has marginal significance. No contact with patients was associated with a 1.7-fold increase in the likelihood of being dengue-positive compared to those who had direct contact with infected individuals, aligning with expectations of vector-borne transmission. Using repellents in the house was associated with a negative impact on being affected by dengue, as those who used repellents were 0.55 times less likely to test positive for dengue compared to those who did not use repellents in the house.
4. Discussion
This study highlights the importance of shaping dengue control strategies to local areas, as the risk factors influencing dengue status were found to vary across study areas. These findings imply that the same strategies may be less effective. Instead, area-specific risk factors based on preventive measures could enhance the effectiveness of measures. Such an approach may improve early detection, resource allocation, and overall outbreak management.
This study revealed that, in 2019, the number of positive dengue cases in Dhaka was significantly higher than in Chattogram—almost twice the number of cases in Chattogram. Between 2012 and 2019, Dhaka, Bangladesh’s capital and most populous city, with nearly 16 million residents [
20,
21], reported the largest number of dengue cases. A 2014 study found that nearly 80% of the population in both Dhaka and Chattogram were seropositive for dengue [
22]. In 2022, Dhaka again showed the highest incidence of dengue in the country, with 63.07% of patients reported in Dhaka compared to only 14.42% in Chattogram [
23]. The mortality rate was also higher in Dhaka, with 63.34% of deaths occurring there, compared to 24.16% in Chattogram [
23]. Additionally, a study confirmed that, out of 59,196 dengue cases reported from January to December 2022, 70% of the patients and 61% of fatalities were from Dhaka, while Chattogram reported 14% of patients and 23.64% of deaths [
24].
Urbanization is a major driver of mosquito-borne disease transmission, as it creates breeding grounds for mosquitoes, facilitates vector–human interactions, and contributes to outbreaks. Dhaka, the capital and most populous city in Bangladesh [
20,
21], has a significantly higher population density [
23] compared to Chattogram. The differences in dengue case numbers between these two cities may be attributed to variations in population size, climatic conditions, and geographical features.
There is a noticeable trend in both Savar and Chattogram, where people tend to seek admission to private hospitals rather than government hospitals. A previous study found that 78% of hospitalized patients during the 2000–2017 dengue outbreaks sought services from private hospitals, where the mortality rate was four times lower than in public hospitals [
25]. The World Bank also reported that nearly 70% of patients in Bangladesh seek medical services in the private healthcare sector [
26]. This preference may stem from the perception that private hospitals offer better facilities and care than government hospitals, or it could be due to limited access to government facilities. Other than facilities, private hospitals may also provide faster service, more flexible visiting hours, and shorter waiting times, which could contribute to the public’s preference. Socioeconomic status and insurance coverage may also influence the patients’ ability to access private care. Additionally, social factors, such as family status, may influence this decision. However, several initiatives have been introduced to address this imbalance, including healthcare management training, the expansion of rapid diagnostic tests (e.g., NS1-based kits), the allocation of more beds for dengue patients in district-level public hospitals, and the updating of clinical management guidelines [
27]. In terms of diagnostic practices in hospitals, NS1 antigen tests are typically used during the early febrile phase (day 1–5), while IgM and IgG antibody tests are more commonly applied from day 5 onward [
28]. In Bangladesh, most hospitals—especially government ones—rely on NS1 and IgM tests for dengue diagnosis, with IgG testing used less frequently due to limited resources [
29]. Private hospitals may offer a broader range of diagnostics due to better laboratory infrastructure.
In 2019, a higher number of dengue cases were reported between April and September, with a peak in August, a pattern observed in both cities. Previous studies also noted that most cases occurred in August that year [
30]. Another study reported that over 90% of dengue fever cases were concentrated in August and September. Some researchers have suggested that the period from August to October is particularly vulnerable to dengue outbreaks in Bangladesh [
23], while others observed that dengue incidence rises sharply in early July and decreases by December [
23].
The distribution of dengue cases across months is closely tied to the climatic conditions of different seasons. This study’s results further confirm that dengue status is seasonal, specifically in Savar. Dengue spread has been associated with rainfall [
31]. Most cases in Bangladesh are reported during the monsoon (June–September) and post-monsoon (October–November) seasons, with a peak incidence in September [
30]. Heavy rainfall, flooding, waterlogging, and unpredictable seasonal changes have created ideal conditions for dengue outbreaks in Khulna [
32]. Climate change has exacerbated heavy rainfall and prolonged rainy seasons in Bangladesh, creating favorable conditions for Aedes mosquito proliferation and subsequent dengue outbreaks [
31]. A significant link between increased rainfall and longer dengue seasons in Bangladesh may help explain the irregular yearly patterns of dengue cases [
33].
An analysis of reported cases shows that more males are affected by dengue compared to females, a trend observed in several studies. Male predominance has been noted in all dengue outbreaks in Bangladesh [
30]. One study confirmed that the proportion of male patients was twice that of females across all outbreaks [
30]. Similar findings have been reported in studies from Bangladesh, where male children are also more likely to contract dengue, as well as in most studies from India [
34]. These results stand in contrast to some findings from South America, where the gender distribution may differ.
This could be because males are more exposed to the contaminated environment than females. Another reason could be cultural aspects, such as dress codes, where females in some cultures cover the body entirely [
30]. Another contributing factor may be cultural norms around clothing. In Bangladesh, it is common for women to wear modest clothing, including full-sleeve garments and long dresses, which may reduce skin exposure and lower the risk of mosquito bites. This dress code, aligned with cultural and religious practices, may serve as a passive protective factor against Aedes bites. A study has pointed out that wearing long sleeves and pants could be preventive while participating in outdoor activities [
33]. Perhaps, females may be reluctant to be admitted to hospitals, and most studies are based on hospital records, so there could be a bias in the data.
Among the reported admissions, the proportion of individuals with a history of previous contact with dengue patients is relatively low. However, a logistic regression analysis identified this as a key factor influencing dengue status. A national seroprevalence study conducted between 2014 and 2015 found that 24% of patients (
n = 5866) reported a previous history of dengue, with over 80% of participants in two major cities (Dhaka and Chattogram) being seropositive [
22]. The spread of the virus may also be linked to travel patterns, particularly from Dhaka to other regions. Previous studies have shown that large-scale movement during religious festivals, such as Eid, when up to 10–12 million people leave Dhaka city, has coincided with major outbreaks of dengue, chikungunya, and COVID-19 [
35]. However, the impact of contact with dengue patients may vary depending on factors such as the time elapsed from exposure, the health status of the individual, and the virulence of the circulating dengue strain.
The use of mosquito nets appears to influence the dengue status in Savar, although no similar effect was observed in Chattogram. This suggests that mosquito net usage may offer some level of protection against dengue. However, there is limited supporting evidence in the literature for this specific finding. Some studies suggest that using mosquito nets while sleeping can help protect against mosquito bites [
33]. It is important to note that Aedes mosquitoes are day-biting, and the protective benefit of nets is likely limited to daytime naps or morning rest. If nets are used only during nighttime sleep, the effectiveness may be reduced. Therefore, assessing the time and context of mosquito net usage is essential for understanding its actual impact.
The variations observed across areas could be attributed to differences in practices and behaviors in each region. For instance, this study shows that, in Chattogram, the use of repellents within the house is associated with a reduction in dengue cases, although this result is marginally significant. However, the use of repellents on the skin may not be as effective when repellents are used inside the house, suggesting that these impacts could be confounded by other factors.
The presence or absence of flower plots inside houses does not have a significant impact, according to the data in this study, despite being a common belief. Other potential Aedes breeding sites, such as uncovered water containers in kitchens and bathrooms, buckets, and rooftop tanks, may have a greater role in mosquito proliferation. These were not directly assessed in this study but represent key targets for future research.
Despite being heavily affected by dengue, Dhaka city lacks a coordinated vector control policy [
30]. The development and implementation of effective policies are crucial for controlling disease. Long-term dengue prevention requires the government to implement urbanization strategies aimed at reducing dengue incidence. While most residents are aware of dengue, they lack knowledge about mosquito breeding sites and biting habits [
30]. Awareness can be increased through electronic media, print media, and social networks.
The Bangladeshi government controls Culex mosquitoes by applying Temephos larvicide in drains and using fogging to target adult mosquitoes during the vector season [
23]. Similarly, targeted insecticide spraying on Aedes breeding sites, chlorination, and the use of larvicides for outdoor water storage are effective control measures. However, effective Aedes control requires an integrated vector management approach. This includes not only chemical methods but also environmental management, such as cleaning water containers, sealing tanks, and community-based source reduction activities. Indoor mosquito protection can be achieved using pesticide sprays, mosquito coils, or by installing window and door screens to prevent their entry [
33]. In addition, wearing long sleeves and pants during outdoor activities is a preventive measure. For indoor protection, pesticide sprays or mosquito coils are commonly used [
33].
Insufficient resources and workforce within the city corporation, along with limited community engagement, hinder effective prevention efforts (vector control policy). In both Savar and Chattogram, the local authorities periodically initiate public awareness campaigns and water-drainage drives, especially during peak dengue season. However, sustained household-level practices, such as the weekly cleaning of rooftop tanks, draining flowerpots, and covering water barrels, remain inconsistent. Therefore, it is crucial to involve citizens through programs that encourage regular draining and cleaning of household water storage containers. Such community-driven initiatives can significantly contribute to reducing mosquito breeding sites and improving overall prevention efforts.
This study has some limitations, such as we could not verify the specific type of diagnostic test used for all patients or the timing of sample collection, and only hospitalized patients were included, which may introduce selection bias and limit generalizability to community-level infections. Additionally, as antibody responses, such as IgG, can persist for months or years after infection, relying on serological tests alone may lead to a misclassification of recent infections.