The Experience of the Upu Smurd Floreasca Team during the Earthquakes in Turkey, February 2023
Abstract
1. Introduction
2. Materials and Methods
- The call for assistance—mobilization
- Take off from Baza 90 towards Adana commercial airport: 06/02/2023 16:45.
- Touchdown in Adana: 06/02/2023 20:35.
- Leaving the airport and heading towards the AFAD regional base camp: 06/02/2023 22:30.
- Leaving the AFAD regional base camp and heading towards the allocated operations base camp: 07/02/2023 05:30.
- Arrival at the allocated operations base camp: 07/02/2023 07:29.
- Start of the first save mission: 07/02/2023 11:40.
- First victim extracted: 07/02/2023 18:29.
- Last extracted victim: 09/02/2023 00:57.
- b.
- Operations
- c.
- Scene management and extrication
- d.
- Second evaluation after extrication
3. Results
- I.
- Victim A—female, 23 years old
- (a)
- Time and date of first contact: 07/02/2023 at 10:30 (+30 h and 12 min from T0).
- (b)
- Time of the first visual contact: 11:30.
- (c)
- Time of the first medical aid provided: 13:00.
- (d)
- Time of extraction: 18:00 (+38 h from T0 and +8 h from the initial contact).
- (e)
- Initial diagnosis: Polytrauma by head trauma, thoracic trauma with right hemithorax subcutaneous emphysema, pelvic trauma, trauma of all four limbs, hypothermia, and hypovolemic shock.
- (f)
- Initial vital signs: GCS 13 (M5V4E4), vital signs impossible to assess, patient is hypothermic and in shock.
- (g)
- Treatment/procedures: Initially covered with a heat blanket, oxygen therapy, analgesia by opioid administration (fentanyl), intravenous hydration after peripheral venous access, cervical immobilization, and immobilization of the right leg and right arm.
- (h)
- Vital signs at the moment of the transport: GCS 14, core body temperature 35.6C, PA (arterial pressure) 106/58 mmHg, heart frequency 95 bpm, SpO2 94%.
- II.
- Victim B—male, 35 years old
- (a)
- Time and date of first contact: 07/02/2023 at 10:30 (+30 h and 12 min from T0).
- (b)
- Time of the first visual contact: 13:30.
- (c)
- Time of the first medical aid provided: 14:30.
- (d)
- Time of extraction: 19:00 (+39 h from T0 and +9 h from the initial contact).
- (e)
- Initial diagnosis: Polytrauma by head trauma, ocular trauma, thoraco-abdominal trauma, left arm and leg trauma, hypothermia, and hypovolemic shock.
- (f)
- Initial vital signs: GCS 14, initial vital signs not evaluable (limited access to the victim).
- (g)
- Treatment/procedures: Initially covered with a heat blanket, oxygen therapy, analgesia by opioid administration (fentanyl), intravenous hydration after peripheral venous access, cervical immobilization, and administration of heated crystalloid solutions (NaCl 0.9%).
- (h)
- Vital signs at the moment of the transport: GCS 15, core body temperature 35.8C, PA 119/81 mmHg, heart frequency 82 bpm, SpO2 96%.
- III.
- Victim C—male, 32 years old
- (a)
- Time and date of first contact: 07/02/2023 at 23:00 (+46 h from T0).
- (b)
- Time of the first visual contact: 23:30.
- (c)
- Time of the first medical aid provided: 08/02/2023 at 00:30.
- (d)
- Time of extraction: 08/02/2023 at 06:30 (+54 h from T0).
- (e)
- Initial diagnosis: Polytrauma with thoraco-abdominal contusion, complex left pelvic fracture by crushing complicated with compartment syndrome and gangrene.
- (f)
- Initial vital signs: GCS 14, hypothermic (34C), in hypovolemic shock with PAs <90 mmHg.
- (g)
- Treatment/procedures: The victim is stuck under the debris, especially the lower left extremity. The initial medical assessment considered the left lower extremity unrecoverable and wanted to proceed with an amputation in the field to reduce the risk of complications and to significantly reduce the extraction time. This request was rejected by the local health authorities. The medical team proceeded to place a gurney of the left lower extremity, analgesia by administration of opioids-numerous fentanyl boluses, peripheral venous access and intravenous hydration with warm crystalloid solutions.
- (h)
- Vital signs at the moment of the transport: core body temperature 35.7C, PA 140/84 mmHg, heart frequency 90/min, SpO2 94% with 6 L of O2 administered by facial mask. The patient is deceased 24 h later at the hospital.
- IV.
- Victim D—male, 16 years old
- (a)
- Time and date of first contact: 07/02/2023 at 23:00 (+46h from T0).
- (b)
- Time of the first visual contact: 08/02/2023 at 11:00 (+58h from T0).
- (c)
- Time of the first medical aid provided: 08/02/2023 at 12:00 (+59h from T0).
- (d)
- Time of extraction: 09/02/2023 at 00:52 (+72h from T0).
- (e)
- Initial diagnosis: Polytrauma due to thoraco-abdominal contusion, complex left pelvic fracture due to crushing, and trauma of the right arm.
- (f)
- Initial vital signs: GCS 14, thready pulse, PAs <90 mmHg.
- (g)
- Treatment/procedures: Very difficult access of the patient for the medical team. Due to an aftershock of the earthquake, the initial access had to be changed as the first one became impassable. Initially covered with a heat blanket, oxygen therapy, analgesia by administration of opioids (numerous Fentanyl boluses), intravenous hydration after peripheral venous access, cervical immobilization, and administration of heated crystalloid solutions (NaCl 0.9% 4 L).
- (h)
- Vital signs at the moment of the transport: PA 128/70 mmHg, SpO2 = 96% with 6 L of O2 administered by facial mask, core body temperature 35.7 C. The patient was admitted fully conscious to the ICU unit.
- V.
- Victim E—male, 35 years old
- (a)
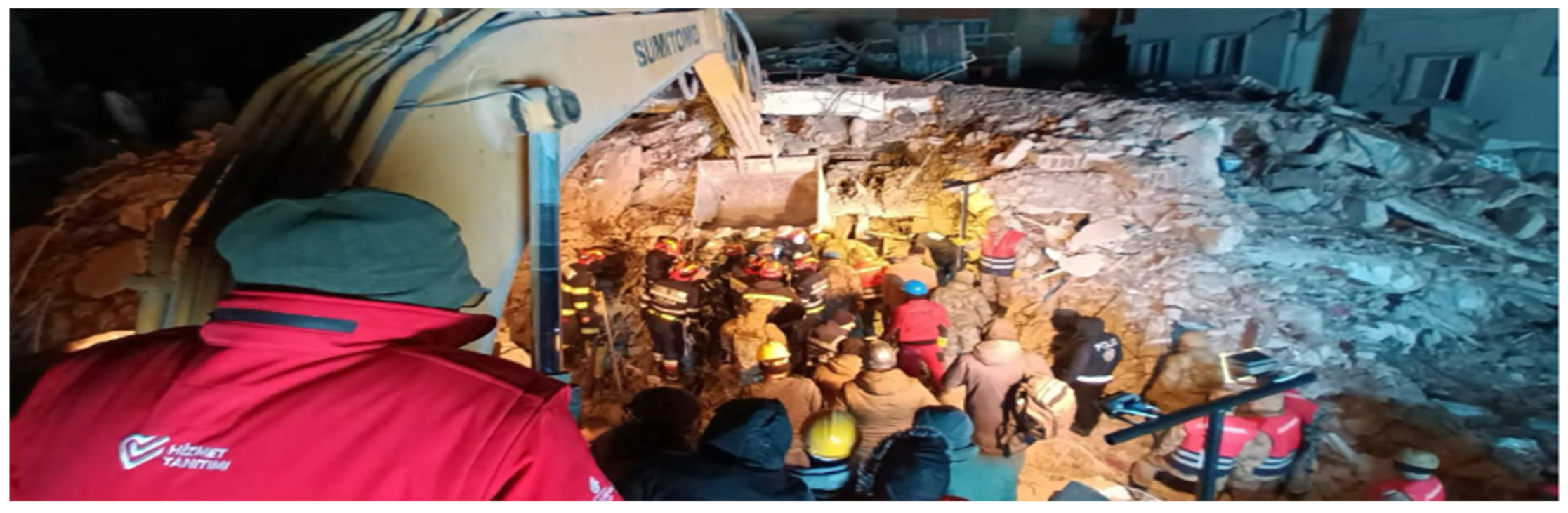
- Time and date of first contact: 11/02/2023 at 20:30 (+136 h from T0) (Figure 1).
- (b)
- Time of the first visual contact: 11/02/2023 at 21:15.
- (c)
- Time of the first medical aid provided: 12/02/2023 at 03:10 (+143 h from T0) (Figure 2).
- (d)
- Time of extraction: 12/02/2023 at 08:30 (+148 h from T0).
- (e)
- Initial diagnosis: Polytrauma with minor head trauma, crush trauma of the lower right extremity, and lower left leg luxation.
- (f)
- Initial vital signs: GCS 14, thready pulse with a heart frequency of 60 bpm, hypothermic 34.6 C, PA not obtainable.
- (g)
- Treatment/procedures: Intravenous hydration after peripheral venous access, cervical immobilization, administration of heated crystalloid solutions (NaCl 0.9% 4 L), oxygen by facial mask up to 6 L per minute, analgesia by administration of opioids before and during the extraction and the mobilization of the trapped lower extremities by fentanyl boluses initially then tramadol.
- (h)
- Vital signs at the moment of the transport: core body temperature 35.2 C, PA 117/54 mmHg, heart frequency of 95/min, SpO2 97% with 6 L of O2 administered by facial mask.

4. Discussion
4.1. Logistical Problems Encountered
- During the mission, medical staff had accommodation in a tent that also served as a warehouse for medical supplies, with heating provided by gas-powered heaters (as the temperatures in Turkey reach freezing during the night). Depending on the direction and intensity of the wind, the smoke emitted by these heaters can enter the living spaces and could have posed serious issues (CO intoxication, asthma attacks, etc.).
- Basic hygiene was very limited during the first hours, i.e., there was no real bathroom on site, and no running hot water.
- Another issue was the lack of adequate equipment provided to the medical team. Considering the level of dust and cadaveric decomposition, adequate protective masks should have been mandatory; also, since the temperatures were very low at that time in Turkey, basic first intervention suits are not suitable for the working conditions, and led to an increase in the fatigue of the medical team.
- No internet access in the first 72 h.
4.2. Post-Mission Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ministry of Interior. Disaster and Emergency Management Presidency. Available online: https://en.afad.gov.tr/about-us (accessed on 15 March 2024).
- 2023 Turkey-Syria Earthquake Data in Context—APM Research Lab. Available online: https://www.apmresearchlab.org/2023-earthquake-turkey-data-in-context (accessed on 15 March 2024).
- USAR Directory. Available online: http://unocha.org (accessed on 20 May 2024).
- INSARAG AAR Türkiye Syria Comprehensive Report—INSARAG. Available online: https://www.insarag.org/wp-content/uploads/2024/04/INSARAG_AAR_Turkiye_Syria.pdf (accessed on 2 April 2024).
- Earthquake: EU Mobilizes More Than 1180 Rescuers to Türkiye via Civil Protection Mechanism—European Commission. Available online: https://civil-protection-humanitarian-aid.ec.europa.eu/news-stories/news/earthquake-eu-mobilises-more-1180-rescuers-turkiye-civil-protection-mechanism-2023-02-07_en (accessed on 23 May 2024).
- Medical Technical Reference Library—INSARAG. Available online: https://www.insarag.org/uncategorized/medical-technical-reference-library/ (accessed on 2 April 2024).
- Slater, M.S.; Mullins, R.J. Rhabdomyolysis and myoglobinuric renal failure in trauma and surgical patients: A review. J. Am. Coll. Surg. 1998, 186, 693–716. [Google Scholar] [CrossRef] [PubMed]
- Bywaters, E.G.; Beall, D. Crush injuries with impairment of renal function. 1941. J. Am. Soc. Nephrol. 1998, 9, 322–332. [Google Scholar] [CrossRef]
- Crush Syndrome-Prolonged Field Care. Joint Trauma System Clinical Practice Guideline. Available online: https://jts.amedd.army.mil/assets/docs/cpgs/Crush_Syndrome_PFC_28_Dec_2016_ID58.pdf (accessed on 21 February 2023).
- Macintyre, A.G.; Barbera, J.A.; Smith, E.R. Surviving collapsedstructure entrapment after earthquakes: A ‘time-to-rescue’ analysis. Prehosp. Disaster Med. 2006, 21, 4–17. [Google Scholar] [CrossRef]
- Better, O.S. History of the crush syndrome: From the earthquakes of Messina, Sicily 1909 to Spitak, Armenia 1988. Am. J. Nephrol. 1997, 17, 392–394. [Google Scholar] [CrossRef]
- Sever, M.S.; Vanholder, R. RDRTF of ISN Work Group on Recommendations for the Management of Crush Victims in Mass Disasters. Recommendation for the management of crush victims in mass disasters. Nephrol. Dial. Transplant. 2012, 27 (Suppl. S1), i4–i67. [Google Scholar] [CrossRef] [PubMed]
- International Search and Rescue Advisory Group. The Medical Management of the Entrapped Person with Crush Syndrome. Available online: https://www.insarag.org/wp-content/uploads/2018/12/ATTACHMENT_C_The_Medical_Management_of_the_Entrapped_Patient_with_Crush_Syndrome_10_2019_-_Final.pdf (accessed on 17 February 2023).
- Reis, N.D.; Michaelson, M. Crush injury to the lower limbs. Treatment of the local injury. J. Bone Joint Surg. Am. 1986, 68, 414–418. [Google Scholar] [CrossRef]
- Better, O.S. The crush syndrome revisited (1940–1990). Nephron 1990, 55, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Long, B.; Liang, S.Y.; Gottlieb, M. Crush injury and syndrome: A review for emergency clinicians. Am. J. Emerg. Med. 2023, 69, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Sever, M.S.; Vanholder, R. Management of crush victims in mass disasters: Highlights from recently published recommendations. Clin. J. Am. Soc. Nephrol. 2013, 8, 328–335. [Google Scholar] [CrossRef]
- Gibney, R.T.; Sever, M.S.; Vanholder, R.C. Disaster nephrology: Crush injury and beyond. Kidney Int. 2014, 85, 1049–1057. [Google Scholar] [CrossRef]
- Cetinalp, N.E.; Alnageeb, A.; Aliyev, A.; Azizli, G.; Ozsoy, K.M.; Oktay, K.; Erman, T. Analysis of Neurosurgical Injuries and the Lessons Learned after the Catastrophic Double Earthquakes in Turkey. Turk. Neurosurg. 2024, 34, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Hekimoglu, Y.; Melez, İ.E.; Canturk, G.; Erkol, Z.; Canturk, N.; Dizdar, M.G.; Melez, D.O.; Guler, O.N. Evaluation of the deaths secondary to entrapment under the debris in the Van earthquake. Egypt. J. Forensic Sci. 2013, 3, 44–47. [Google Scholar] [CrossRef]
- Gu, J.W.; Zhou, H.T.; Yang, T.; Cheng, J.M.; Qu, Y.; Li, C.Y.; Li, Q.J.; Lü, J.Y.; Cheng, S.L.; Liu, J.J.; et al. Ultimate treatment for a patient with severe traumatic brain injury without intake for 192 hours after Wenchuan massive earthquake. Chin. Med. J. 2009, 122, 113–116. [Google Scholar] [PubMed]
- Joseph, B.; Pandit, V.; Aziz, H.; Kulvatunyou, N.; Zangbar, B.; Green, D.J.; Haider, A.; Tang, A.; O’Keeffe, T.; Gries, L.; et al. Mild traumatic brain injury defined by Glasgow Coma Scale: Is it really mild? Brain Inj. 2015, 29, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Cakir, I.M.; Sengul, I.; Bekci, T.; Tonkaz, G.; Eryuruk, U.; Onder, R.O.; Aksoy, I.; Bayar, A.E.; Tonkaz, M.; Aslan, S.; et al. A needful, unique, and in-place evaluation of the injuries in earthquake victims with computed tomography, in catastrophic disasters! The 2023 Turkey-Syria earthquakes: Part I. Rev. da Assoc. Médica Bras. 2023, 69, e20230399. [Google Scholar] [CrossRef]
- Peiris, D. A historical perspective on crush syndrome: The clinical application of its pathogenesis, established by the study of wartime crush injuries. J. Clin. Pathol. 2017, 70, 277–281. [Google Scholar] [CrossRef]
- Ashkenazi, I.; Isakovich, B.; Kluger, Y.; Alfici, R.; Kessel, B.; Better, O.S. Prehospital management of earthquake casualties buried under rubble. Prehosp. Disaster Med. 2005, 20, 122–133. [Google Scholar] [CrossRef]
- Santangelo, M.L.; Usberti, M.; Di Salvo, E.; Belli, G.; Romano, G.; Sassoli, C.; Zotti, G. A study of the pathology of the crush syndrome. Surg. Gynecol. Obstet. 1982, 154, 372–374. [Google Scholar]
- Noji, E.K. Acute renal failure in natural disasters. Ren. Fail. 1992, 14, 245–249. [Google Scholar] [CrossRef]
- Bartal, C.; Zeller, L.; Miskin, I.; Sebbag, G.; Karp, E.; Grossman, A.; Engel, A.; Carter, D.; Kreiss, Y. Crush syndrome: Saving more lives in disasters: Lessons learned from the earlyresponse phase in Haiti. Arch. Intern. Med. 2011, 171, 694–696. [Google Scholar] [CrossRef]
- Onan, E.; Torun, D.; Kozanoğlu, R.; Miçözkadıoğlu, H.; Beyaz, S.; Özgözen, L.; Turgut, N.; Demiroğlu, Y.Z.; Karagün, Ö.; Ergenoğlu, P.; et al. Mortality factors in crush syndrome. Ulus Travma Acil Cerrahi Derg. 2024, 30, 174–184. [Google Scholar] [CrossRef] [PubMed]
| Time Period under Ruble (TPR) (hours) | Extrication Duration (hours) | Initial Systolic Arterial Pression (mmHg) | Initial GCS (Glasgow Coma Scale) | Hypothermia (Yes/No) | Crush Syndrome Suspected (Yes/No) | Neurological Injury Suspected (Yes/No) | GCS after Extrication | Arterial Pressure after Extrication and IV NaCl Resuscitation (Systolic/Diastolic, mmHg) | |
|---|---|---|---|---|---|---|---|---|---|
| Victim A | 38 | 8 | N/A | 13 | Yes | Yes | Yes | 14 | 106/58 |
| Victim B | 39 | 9 | N/A | 14 | Yes | Yes | Yes | 15 | 119/81 |
| Victim C | 54 | 8 | <90 mmHg | 14 | Yes | Yes | Yes | 15 | 140/84 |
| Victim D | 72 | 14 | <90 mmHg | 14 | Yes | Yes | No | 15 | 128/70 |
| Victim E | 148 | 12 | N/A | 14 | Yes | Yes | Yes | 14 | 117/54 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oprita, B.; Oprita, R.; Berea, T.-N.; Olaru, I.; Draghici, M.A. The Experience of the Upu Smurd Floreasca Team during the Earthquakes in Turkey, February 2023. Emerg. Care Med. 2024, 1, 341-349. https://doi.org/10.3390/ecm1040034
Oprita B, Oprita R, Berea T-N, Olaru I, Draghici MA. The Experience of the Upu Smurd Floreasca Team during the Earthquakes in Turkey, February 2023. Emergency Care and Medicine. 2024; 1(4):341-349. https://doi.org/10.3390/ecm1040034
Chicago/Turabian StyleOprita, Bogdan, Ruxandra Oprita, Teodor-Nicolae Berea, Ionut Olaru, and Marian Alexandru Draghici. 2024. "The Experience of the Upu Smurd Floreasca Team during the Earthquakes in Turkey, February 2023" Emergency Care and Medicine 1, no. 4: 341-349. https://doi.org/10.3390/ecm1040034
APA StyleOprita, B., Oprita, R., Berea, T.-N., Olaru, I., & Draghici, M. A. (2024). The Experience of the Upu Smurd Floreasca Team during the Earthquakes in Turkey, February 2023. Emergency Care and Medicine, 1(4), 341-349. https://doi.org/10.3390/ecm1040034





