Implementation of Inhaled Methoxyflurane for the Reduction of Distal Radius Fractures in a Third-Level Hospital: A Descriptive Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Inclusion Criteria
- Patients over 18 years;
- Patients diagnosed with Frykman type I and type II distal radius fractures;
- Patients requiring closed reduction, using inhaled methoxyflurane versus propofol.
2.3. Exclusion Criteria
- Patients with Frykman types III, IV, V, VI, VII, and VIII fractures;
- Open fractures, polytraumatized patients, and patients with previous sedation or using advanced airways.
2.4. Evaluation of Propofol
2.5. Evaluation of Methoxyflurane
2.6. Functionality Evaluation
2.7. Statistical Analysis
3. Results
3.1. Study Population
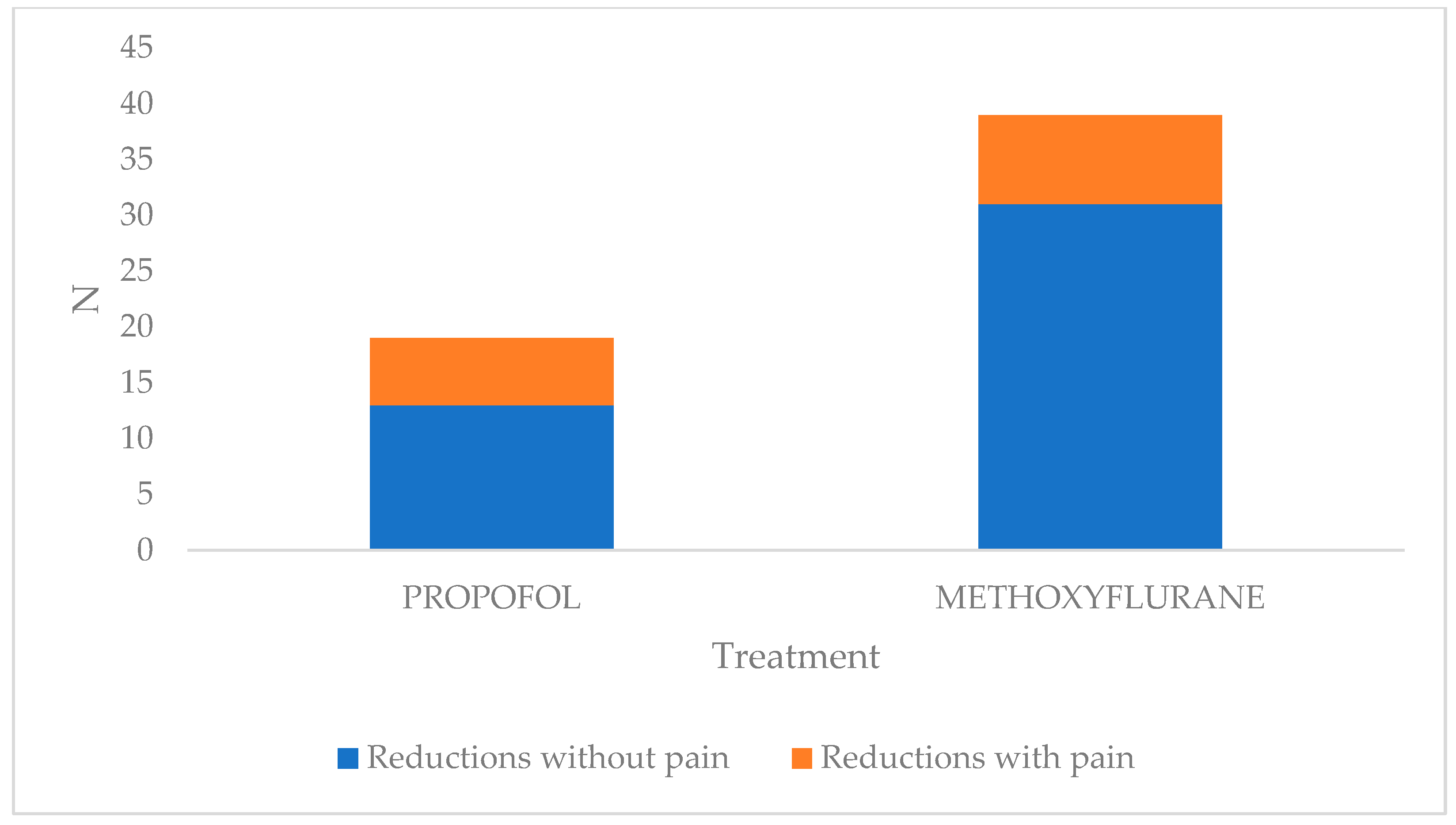
3.2. Evaluation of Methoxyflurane vs. Propofol
3.3. Functionality Evaluation
3.4. Adverse Events
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Porter, K.M.; Dayan, A.D.; Dickerson, S.; Middleton, P.M. The role of inhaled methoxyflurane in acute pain management. Open Access Emerg. Med. 2018, 10, 149–164. [Google Scholar] [CrossRef]
- Blair, H.A.; Frampton, J.E. Methoxyflurane: A review in trauma pain. Clin. Drug Investig. 2016, 36, 1067–1073. [Google Scholar] [CrossRef] [PubMed]
- Cousins, M.J.; Mazze, R.I. Methoxyflurane nephrotoxicity. A study of dose response in man. JAMA 1973, 225, 1611–1616. [Google Scholar] [CrossRef]
- Buntine, P.; Thom, O.; Babl, F.; Bailey, M.; Bernard, S. Prehospital analgesia in adults using inhaled methoxyflurane. Emerg. Med. Australas. 2007, 19, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Oxer, H.F.; Wilkes, G. Methoxyflurane is a safe, easy, effective analgesic for prehospital pain relief. Prehospital Disaster Med. 2007, 22, s77. [Google Scholar]
- Gillis, M.; Keirens, A.; Steinkamm, C.; Verbelen, J.; Muysoms, W.; Reynders, N. The use of methoxyflurane (Penthrox) in the emergency department. Reg. Anesth. Pain Med. 2008, 33, e247. [Google Scholar] [CrossRef]
- Middleton, P.M.; Simpson, P.M.; Sinclair, G.; Dobbins, T.A.; Math, B.; Bendall, J.C. Effectiveness of morphine, fentanyl, and methoxyflurane in the prehospital setting. Prehospital Emerg. Care 2010, 14, 439–447. [Google Scholar] [CrossRef]
- Coffey, F.; Wright, J.; Hartshorn, S.; Hunt, P.; Locker, T.; Mirza, K.; Dissmann, P. STOP!: A randomised, double- blind, placebo-controlled study of the efficacy and safety of methoxyflu-rane for the treatment of acute pain. Emerg. Med. J. 2014, 31, 613–618. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.J.H.; Koh, Z.X.; Zafirah, N.A. Clinical evaluation of Penthrox® (methoxyflurane) and tramadol for the Singapore Emergency Ambulance Service. In Proceedings of the Society for Emergency Medicine in Singapore Annual Scientific Meeting, Singapore, 27–28 February 2016. [Google Scholar]
- Liu, H.; Fu, X.; Ren, Y.F.; Tan, S.Y.; Xiang, S.R.; Zheng, C.; You, F.M.; Shi, W.; Li, L.J. Does Inhaled Methoxyflurane Implement Fast and Efficient Pain Management in Trauma Patients? A Systematic Review and Meta-Analysis. Pain Ther. 2021, 10, 651–674. [Google Scholar] [CrossRef] [PubMed]
- Eager, M.M.; Nolan, G.S.; Tonks, K.; Ramjeeawon, A.; Taylor, N. Inhaled methoxyflurane (Penthrox) for analgesia in trauma: A systematic review protocol. Syst. Rev. 2021, 10, 47. [Google Scholar] [CrossRef] [PubMed]
- Johnston, S.; Wilkes, G.J.; Thompson, J.A. Inhaled methoxyflurane and intranasal fentanyl for prehospital management of visceral pain in an Australian ambulance service. Emerg. Med. J. 2011, 28, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Cortés-Castillo, N.G.; Carrillo-Torres, O.; Camacho-Vacherón, V. The resurgence of methoxyflurane in Mexico. Rev. Mex. Anestesiol. 2023, 46, 32–37. [Google Scholar] [CrossRef]
- Morales Carrasco, Á.; Oña Sánchez, C.; Gavilánez Acosta, M.; López García, M.A. Analgesia multimodal en el manejo del dolor en el área de Emergencia: Artículo de Revisión. Cienc. Ecuad. 2023, 5, 20–31. [Google Scholar]
- Niño-Serna, L.F.; Díaz, H.D.M.; Valenzuela, P.V.; Quintero, J.F. Efectividad y Seguridad Comparativa de Medicamentos Analgésicos Utilizados en el Manejo del Dolor Agudo en Niños: Revisión Sistemática de la Literatura y Metaanálisis en Red. Available online: https://bibliotecadigital.udea.edu.co/handle/10495/20968 (accessed on 20 February 2024).
- Thomason, R.; Light, G.; Holaday, D.A. Methoxyflurane anesthesia: A clinical appraisal. Anesth. Analg. 1962, 41, 225–229. [Google Scholar] [CrossRef] [PubMed]
- Mazze, R.I.; Shue, G.L.; Jackson, S.H. Renal dysfunction associated with methoxyflurane anesthesia. A randomized, prospective clinical evaluation. JAMA 1971, 216, 278–288. [Google Scholar] [CrossRef]
- Ikeda, S. The reincarnation of methoxyflurane. J. Anesth. Hist. 2020, 6, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Fabbri, A.; Ruggiano, G.; Garcia Collado, S.; Ricard-Hibon, A.; Restelli, U.; Sbrana, G.; Marinangeli, F.; Farina, A.; Coffey, F. Role of Inhaled Methoxyflurane in the Management of Acute Trauma Pain. J. Pain Res. 2020, 13, 1547–1555. [Google Scholar] [CrossRef]
- Allison, S.J.; Docherty, P.D.; Pons, D.; Chase, J.G. Exposure to methoxyflurane: Low-dose analgesia and occupational exposure. Australas. J. Paramed. 2020, 17, 1–13. [Google Scholar] [CrossRef]
- Cousins, M.; Mazze, R.; Kosek, J.; Hitt, B.; Love, F.V. The etiology of methoxyflurane nephrotoxicity. J. Pharmacol. Exp. Ther. 1974, 190, 530–541. [Google Scholar] [CrossRef] [PubMed]


| Variable | Percentage | |
|---|---|---|
| Age | 23–35 years | 6% |
| 36–45 years | 44% | |
| 46–58 years | 50% | |
| Sex | Man | 30% |
| Women | 70% | |
| Fracture classification | Frykman I | 28% |
| Frykman II | 72% | |
| Fracture reduction | Si | 76% |
| No | 24% | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Albavera-Gutierrez, R.R.; Paredes-Herrera, F.J.; Gasca-López, G.A.; Waldo-Castañón, Z.; Espinosa-Ramos, M.A.; Valencia-Ledezma, O.E.; Castro-Fuentes, C.A. Implementation of Inhaled Methoxyflurane for the Reduction of Distal Radius Fractures in a Third-Level Hospital: A Descriptive Cohort Study. Emerg. Care Med. 2024, 1, 145-152. https://doi.org/10.3390/ecm1020016
Albavera-Gutierrez RR, Paredes-Herrera FJ, Gasca-López GA, Waldo-Castañón Z, Espinosa-Ramos MA, Valencia-Ledezma OE, Castro-Fuentes CA. Implementation of Inhaled Methoxyflurane for the Reduction of Distal Radius Fractures in a Third-Level Hospital: A Descriptive Cohort Study. Emergency Care and Medicine. 2024; 1(2):145-152. https://doi.org/10.3390/ecm1020016
Chicago/Turabian StyleAlbavera-Gutierrez, Roberto R., Francisco J. Paredes-Herrera, Gilberto A. Gasca-López, Zuri Waldo-Castañón, Manuel A. Espinosa-Ramos, Omar Esteban Valencia-Ledezma, and Carlos Alberto Castro-Fuentes. 2024. "Implementation of Inhaled Methoxyflurane for the Reduction of Distal Radius Fractures in a Third-Level Hospital: A Descriptive Cohort Study" Emergency Care and Medicine 1, no. 2: 145-152. https://doi.org/10.3390/ecm1020016
APA StyleAlbavera-Gutierrez, R. R., Paredes-Herrera, F. J., Gasca-López, G. A., Waldo-Castañón, Z., Espinosa-Ramos, M. A., Valencia-Ledezma, O. E., & Castro-Fuentes, C. A. (2024). Implementation of Inhaled Methoxyflurane for the Reduction of Distal Radius Fractures in a Third-Level Hospital: A Descriptive Cohort Study. Emergency Care and Medicine, 1(2), 145-152. https://doi.org/10.3390/ecm1020016







