Comparing Healthcare Facilities to Demographic Standards in the Pakistani Rural Environment
Abstract
1. Introduction
- i.
- how to compute public sector basic health institutions’ demand per population standards?
- ii.
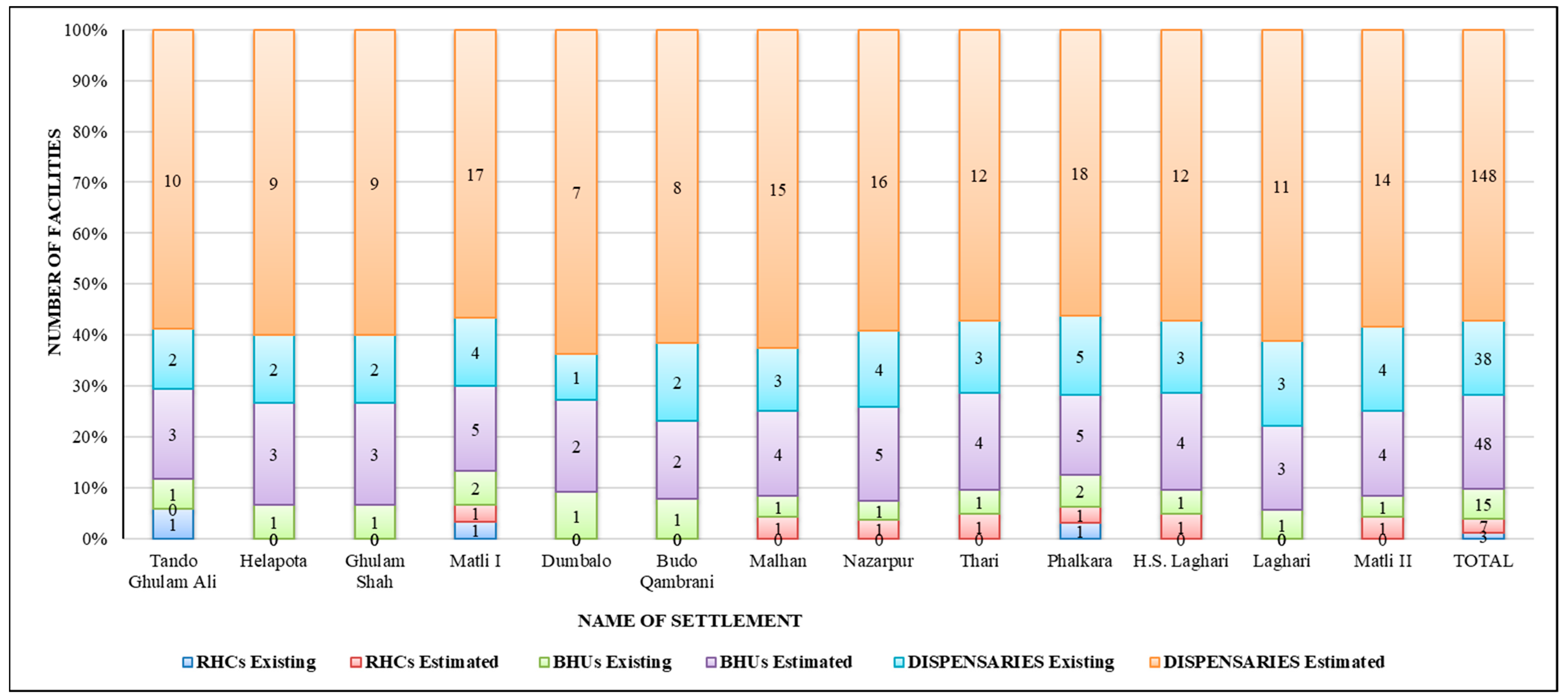
- what are the current and projected requirements of health institutions, i.e., hospitals, basic health units (BHUs), rural health centers (RHCs), and dispensaries, per demographic standards in the Badin sub-region?
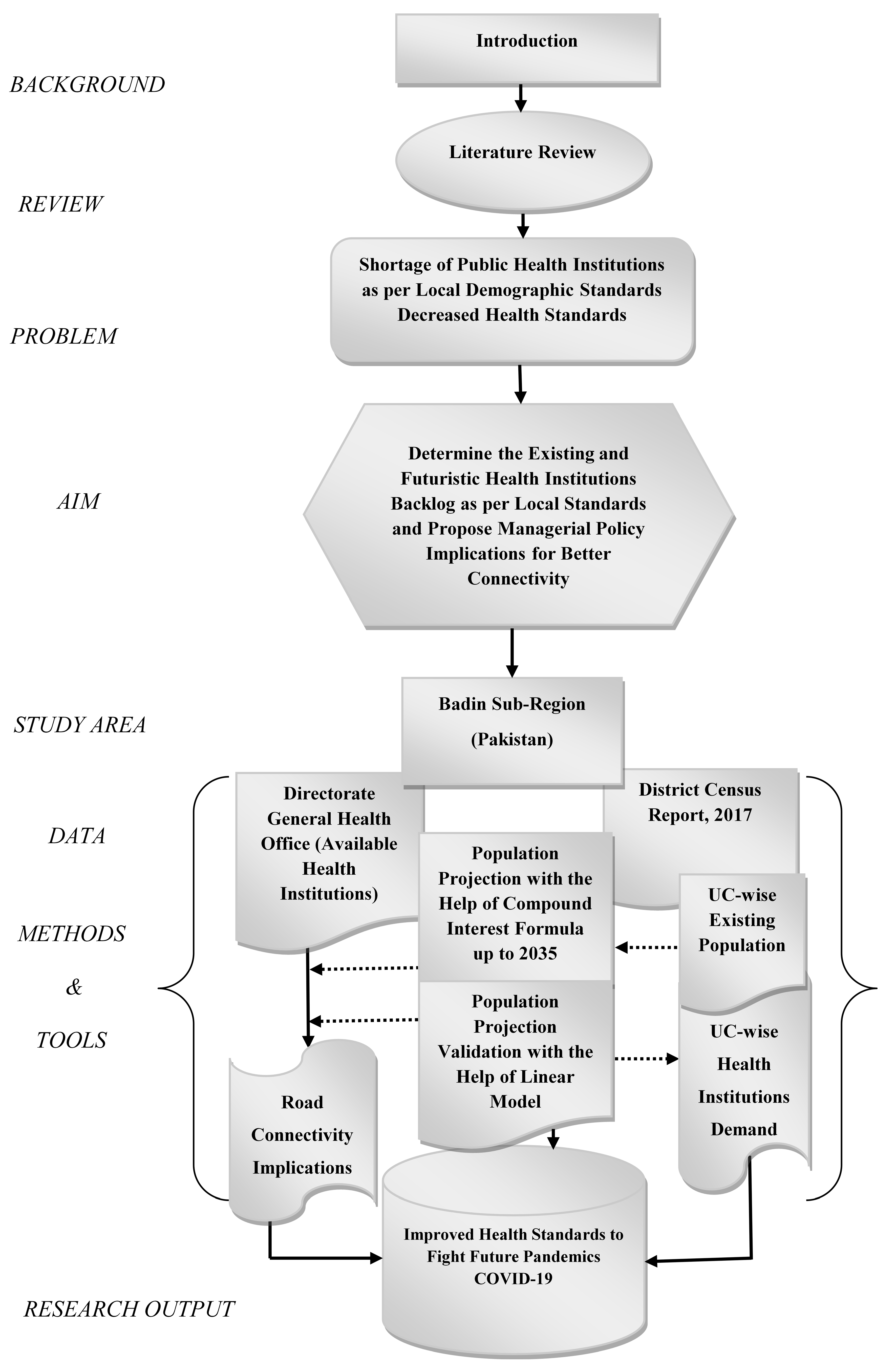
2. Methodology
Study Area
- i.
- The available number of health facilities was collected from the concerned authorities during the phase of data collection;
- ii.
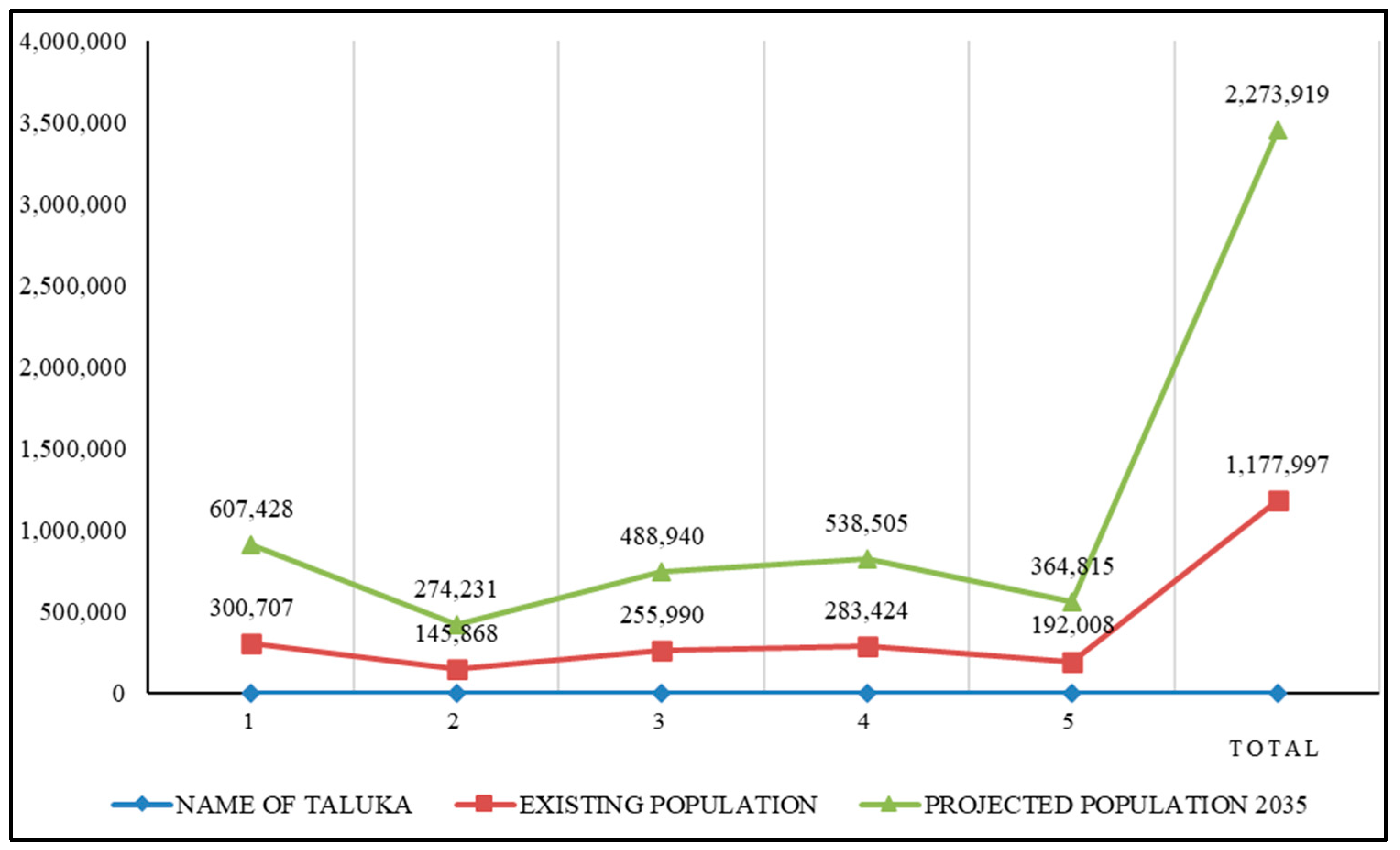
- The population was projected for all UCs with the help of equations 1 and 2 (the compound interest formula) up to the year 2035;
- iii.
- The health standards were collected from the National Reference Manual (NRM) for the availability of health services;
3. Results and Discussions
Proposed Road Connectivity
4. Research Limitations
- i.
- The demographic features of the study area, i.e., Badin, Pakistan were procured from the census report. Meanwhile, the quantity of available public health institutions was retrieved with the help of a questionnaire from the office of Director-General Health, Sindh;
- ii.
- Only a statistical test, i.e., the linear model, was used to validate the population-projection exercise. This is the only parameter in the study that required a statistical test. No further statistical tests were performed;
- iii.
- This study did not measure the travel accessibility of the residents while commuting to reach health institutes. This research work will be conducted in the future;
- iv.
- Only existing and futuristic shortages of health institutions were computed per local demographic standards. For better connectivity, road patterns were proposed to connect local inhabitants with health institutions;
- v.
- The population of Pakistan is increasing at a growth rate of 2.0. Hence, the demand for health institutions keeps mounting at a greater pace. The output of this study is helpful for planning until the year 2035. After that period, population projection should be carried out again to determine the demand for health services per the local population standards.
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mansour, S. Spatial analysis of public health facilities in Riyadh Governorate, Saudi Arabia: A GIS-based study to assess geographic variations of service provision and accessibility. Geo-Spat. Inf. Sci. 2016, 19, 26–38. [Google Scholar] [CrossRef]
- McGrail, M.R.; Humphreys, J.S. Measuring spatial accessibility to primary health care services: Utilising dynamic catchment sizes. Appl. Geogr. 2014, 54, 182–188. [Google Scholar] [CrossRef]
- Cheng, G.; Zeng, X.; Duan, L.; Lu, X.; Sun, H.; Jiang, T.; Li, Y. Spatial difference analysis for accessibility to high level hospitals based on travel time in Shenzhen, China. Habitat Int. 2016, 53, 485–494. [Google Scholar] [CrossRef]
- Nadeem, M.; Aziz, A.; Al-Rashid, M.A.; Tesoriere, G.; Asim, M.; Campisi, T. Scaling the Potential of Compact City Development: The Case of Lahore, Pakistan. Sustainability 2021, 13, 5257. [Google Scholar] [CrossRef]
- Qureshi, S.; Memon, I.A.; Talpur, M.A.H. Association between Objectively Measured Neighbourhood Built Environment and Walkability. Mehran Univ. Res. J. Eng. Technol. 2022, 41, 157–168. [Google Scholar] [CrossRef]
- Choudhry, M.T.; Elhorst, J.P. Demographic transition and economic growth in China, India and Pakistan. Econ. Syst. 2010, 34, 218–236. [Google Scholar] [CrossRef]
- Khahro, S.H.; Talpur, M.A.H.; Bhellar, M.G.; Das, G.; Shaikh, H.; Sultan, B. GIS-Based Sustainable Accessibility Mapping of Urban Parks: Evidence from the Second Largest Settlement of Sindh, Pakistan. Sustainability 2023, 15, 6228. [Google Scholar] [CrossRef]
- Talpur, M.A.H.; Khahro, S.H.; Ali, T.H.; Waseem, H.B.; Napiah, M. Computing travel impendences using trip generation regression model: A phenomenon of travel decision-making process of rural households. Environ. Dev. Sustain. 2022, 25, 5973–5996. [Google Scholar] [CrossRef]
- Han, W. Health care system reforms in developing countries. J. Public Health Res. 2012, 1, 199–207. [Google Scholar] [CrossRef]
- Sharma, A.; Prinja, S.; Aggarwal, A.K. Measurement of health system performance at district level: A study protocol. J. Public Health Res. 2017, 6, 917. [Google Scholar] [CrossRef]
- Talpur, M.A.H.; Napiah, M.; Chandio, I.A.; Memon, I.A. Analyzing Public Sector Education Facilities: A Step Further Towards Accessible Basic Education Institutions in Destitute Subregions. Int. Educ. Stud. 2014, 7, 110–119. [Google Scholar] [CrossRef]
- Leisinger, K.M.; Garabedian, L.F.; Wagner, A.K. Improving Access to Medicines in Low and Middle Income Countries: Corporate Responsibilities in Context. South. Med. Rev. 2012, 5, 3–8. [Google Scholar] [PubMed]
- Smailes, P.J.; Argent, N.; Griffin, T.L.C. Rural population density: Its impact on social and demographic aspects of rural communities. J. Rural Stud. 2002, 18, 385–404. [Google Scholar] [CrossRef]
- Bhellar, M.G.; Talpur, M.A.H.; Khahro, S.H.; Ali, T.H.; Javed, Y. Visualizing Travel Accessibility in a Congested City Center: A GIS-Based Isochrone Model and Trip Rate Analysis Considering Sustainable Transportation Solutions. Sustainability 2023, 15, 16499. [Google Scholar] [CrossRef]
- Terluin, I.J. Differences in economic development in rural regions of advanced countries: An overview and critical analysis of theories. J. Rural Stud. 2003, 19, 327–344. [Google Scholar] [CrossRef]
- Firdaus, G.; Ahmad, A. Impact analysis of urbanization on rural livelihood—An empirical study of an urban centre of Delhi, India. Int. J. Urban Sci. 2011, 15, 147–160. [Google Scholar] [CrossRef]
- Arif, G.M.; Hamid, S. Urbanization, City Growth and Quality of Life in Pakistan. Eur. J. Soc. Sci. 2009, 10, 196–215. [Google Scholar]
- Li, L.-H. Balancing Rural and Urban Development: Applying Coordinated Urban–Rural Development (CURD) Strategy to Achieve Sustainable Urbanisation in China. Sustainability 2017, 9, 1948. [Google Scholar] [CrossRef]
- Karamat, J.; Shurong, T.; Ahmad, N.; Afridi, S.; Khan, S.; Khan, N. Developing Sustainable Healthcare Systems in Developing Countries: Examining the Role of Barriers, Enablers and Drivers on Knowledge Management Adoption. Sustainability 2019, 11, 954. [Google Scholar] [CrossRef]
- Talpur, M.A.H.; Napiah, M.; Chandio, I.A.; Qureshi, T.A.; Khahro, S.H. Development of a Regional Transport Policy Support System for Rural Planning Agencies in Developing World. Procedia Eng. 2014, 77, 2–10. [Google Scholar] [CrossRef]
- Zaidi, S.A. The urban bias in health facilities in Pakistan. Soc. Sci. Med. 1985, 20, 473–482. [Google Scholar] [CrossRef]
- Hussain, A.; Asif, M.; Jameel, A.; Hwang, J. Measuring OPD Patient Satisfaction with Different Service Delivery Aspects at Public Hospitals in Pakistan. Int. J. Environ. Res. Public Health 2019, 16, 2340. [Google Scholar] [CrossRef] [PubMed]
- Islam, A. Health Sector Reform in Pakistan: Future Directions. J. Pak. Med. Assoc. 2002, 52, 174–182. [Google Scholar] [PubMed]
- Nishtar, S. The Gateway Paper Health Systems in Pakistan—A Way Forward; Pakistan’s Health Policy Forum and Heartfile: Islamabad, Pakistan, 2006. [Google Scholar]
- Akram, M.; Khan, F.J. Health Care Services and Government Spending in Pakistan; Pakistan Institute of Development Economics (PIDE): Islamabad, Pakistan, 2007. [Google Scholar]
- Bocarejo, S.J.P.; Oviedo, H.D.R. Transport accessibility and social inequities: A tool for identification of mobility needs and evaluation of transport investments. J. Transp. Geogr. 2012, 24, 142–154. [Google Scholar] [CrossRef]
- Talpur, M.A.H.; Memon, F.A.; Khahro, S.H. Public Sector Education Institution’s Analysis: A Way Forward to Curtail Rural-Regional Education Accessibility Problems. Mehran Univ. Res. J. Eng. Technol. 2014, 33, 492–500. [Google Scholar]
- Fiorini, G.; Rigamonti, A.E.; Galanopoulos, C.; Adamoli, M.; Ciriaco, E.; Franchi, M.; Genovese, E.; Corrao, G.; Cella, S.G. Undocumented migrants during the COVID-19 pandemic: Social conditions, clinical features and pharmacological treatment. J. Public Health Res. 2020, 9, 496–500. [Google Scholar] [CrossRef] [PubMed]
- Wang, R. Measuring the Effect of Government Response on COVID-19 Pandemic: Empirical Evidence from Japan. COVID 2021, 1, 276–287. [Google Scholar] [CrossRef]
- Zhou, Z.; Xu, Z.; Liu, A.; Zhou, S.; Mu, L.; Zhang, X. Mapping the Accessibility of Medical Facilities of Wuhan during the COVID-19 Pandemic. ISPRS Int. J. Geo-Inf. 2021, 10, 318. [Google Scholar] [CrossRef]
- Sohil, F.; Sohail, M.U.; Shabbir, J. COVID-19 in Pakistan: Challenges and priorities. Cogent Med. 2021, 8, 1966179. [Google Scholar] [CrossRef]
- Campisi, T.; Basbas, S.; Skoufas, A.; Akgün, N.; Ticali, D.; Tesoriere, G. The Impact of COVID-19 Pandemic on the Resilience of Sustainable Mobility in Sicily. Sustainability 2020, 12, 8829. [Google Scholar] [CrossRef]
- Talpur, M.A.H.; Napiah, M.; Chandio, I.A.; Khahro, S.H. Transportation Planning Survey Methodologies for the Proposed Study of Physical and Socio-economic Development of Deprived Rural Regions: A Review. Mod. Appl. Sci. 2012, 06, 1–16. [Google Scholar] [CrossRef]
- Talpur, M.A.H.; Chandio, I.A.; Memon, I.A.; Qureshi, T.A. Computer-based Database System: Rapid Response for Rural Planning Agencies to Devise Transport Policies. Indian J. Sci. Technol. 2014, 7, 1603–1612. [Google Scholar] [CrossRef]
- Talpur, M.A.H.; Madzlan, N.; Irfan, A.; Chandio, I.A.; Hussain, S. Time-Space Geography: A Creditable Transport Accessibility Measure for Rural Dwellers. Appl. Mech. Mater. 2014, 567, 763–768. [Google Scholar] [CrossRef]
- Highlights of the Pakistan Economic Survey 2011-12; Economic Adviser’s Wing, Finance Division, Government of Pakistan: Islamabad, Pakistan, 2012.
- Bagahl, G.U.; Khaskhelly, N.; Shaikh, D.E.K.Z.; Sheikh, M.A. Empirical Analytical Study on Socio-Economic Factor of Early Marriages: A Case Study of Badin District, Sindh, Pakistan. Gov. Res. J. Political Sci. 2016, 5, 101–116. [Google Scholar]
- Pakistan, H.R. Humanitarian Response Pakistan. 2011. Available online: http://pakresponse.info/MapDataCenter.aspx (accessed on 12 February 2024).
- Bureau of Statistics, Government of Pakistan, District Vision Badin (A Framework for Sustainable Development). Int. Union Conserv. Nat. Nat. Resour. 2006, 134.
- Badin, Bureau of Statistics; Government of Pakistan: Islamabad, Pakistan, 1998.
- Rees, P.; Clark, S.; Wohland, P.; Kalamandeen, M. Evaluation of Sub-National Population Projections: A Case Study for London and the Thames Valley. Appl. Spat. Anal. Policy 2019, 12, 797–829. [Google Scholar] [CrossRef]
- Khahro, S.H.; Matori, A.N.; Chandio, I.A.; Talpur, M.A.H. Data Preparation for GIS based Land Suitability Modelling: A Stepped Approach. E3S Web Conf. 2019, 101, 02001. [Google Scholar] [CrossRef]
- NRM. National Reference Manual Ministry of Housing, Works, Environmental and Urban Affairs Division; Government of Pakistan: Islamabad, Pakistan, 1986. [Google Scholar]
- Noh, J.-W.; Kim, Y.-m.; Akram, N.; Yoo, K.-B.; Cheon, J.; Lee, L.J.; Kwon, Y.D.; Stekelenburg, J. Impact of Socio-Economic Factors and Health Information Sources on Place of Birth in Sindh Province, Pakistan: A Secondary Analysis of Cross-Sectional Survey Data. Int. J. Environ. Res. Public Health 2019, 16, 932. [Google Scholar] [CrossRef]











| S. NO. | Type | Function | Facilities | Demographic Standards |
|---|---|---|---|---|
| 1 | Dispensary | First aid | Dispenser | Per 3000 Population |
| 2 | BHU | Provide Medicines and Training | 1 Doctor 2- 3 Paramedics | 5000–10,000 Population |
| 3 | RHC | Provide Medicines and Training | 3 Doctors 25 Beds | 50,000 Population |
| 4 | Taluka Hospital | 3 Basic Specialties/Dentistry | 60 Beds | One/Taluka Town |
| 5 | District Hospital | All Medical Facilities 6–10 specialties | 100–250 Beds | One/District Head Quarter Town |
| Linear Model | R | R2 | R2 Change | F-Change | Sig. F-Change |
| 0.996 a | 0.991 | 0.991 | 334.231 | 0.000 |
| Model | Unstandardized Coefficients | Standardized Coefficients | t | Sig. | |
|---|---|---|---|---|---|
| B | Std. Error | Beta | |||
| (Constant) | −29,998.396 | 27,312.072 | -- | −1.098 | 0.352 |
| Current Population | 2.058 | 0.113 | 0.996 | 18.282 | 0.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Talpur, M.A.H. Comparing Healthcare Facilities to Demographic Standards in the Pakistani Rural Environment. Hospitals 2024, 1, 114-130. https://doi.org/10.3390/hospitals1010010
Talpur MAH. Comparing Healthcare Facilities to Demographic Standards in the Pakistani Rural Environment. Hospitals. 2024; 1(1):114-130. https://doi.org/10.3390/hospitals1010010
Chicago/Turabian StyleTalpur, Mir Aftab Hussain. 2024. "Comparing Healthcare Facilities to Demographic Standards in the Pakistani Rural Environment" Hospitals 1, no. 1: 114-130. https://doi.org/10.3390/hospitals1010010
APA StyleTalpur, M. A. H. (2024). Comparing Healthcare Facilities to Demographic Standards in the Pakistani Rural Environment. Hospitals, 1(1), 114-130. https://doi.org/10.3390/hospitals1010010


_Basu.png)




