Ventilation and Infection Control in Healthcare Facilities: A Post-COVID-19 Literature Synthesis
Abstract
1. Introduction
Problem Statement
- Has the COVID-19 pandemic improved our knowledge base specific to healthcare settings, and what are the new or novel findings?
- How often do we see recommendations not supported by evidence in the scholarly works published after the COVID-19 pandemic?
- To what extent has the existing knowledge and experience available in the literature shaped the written recommendations and policies during the pandemic?
2. Background
2.1. Routes of Disease Transmission
2.2. Role of HVAC Systems
2.3. IAQ Strategies and Safety Measures
2.4. Takeaway from the Literature
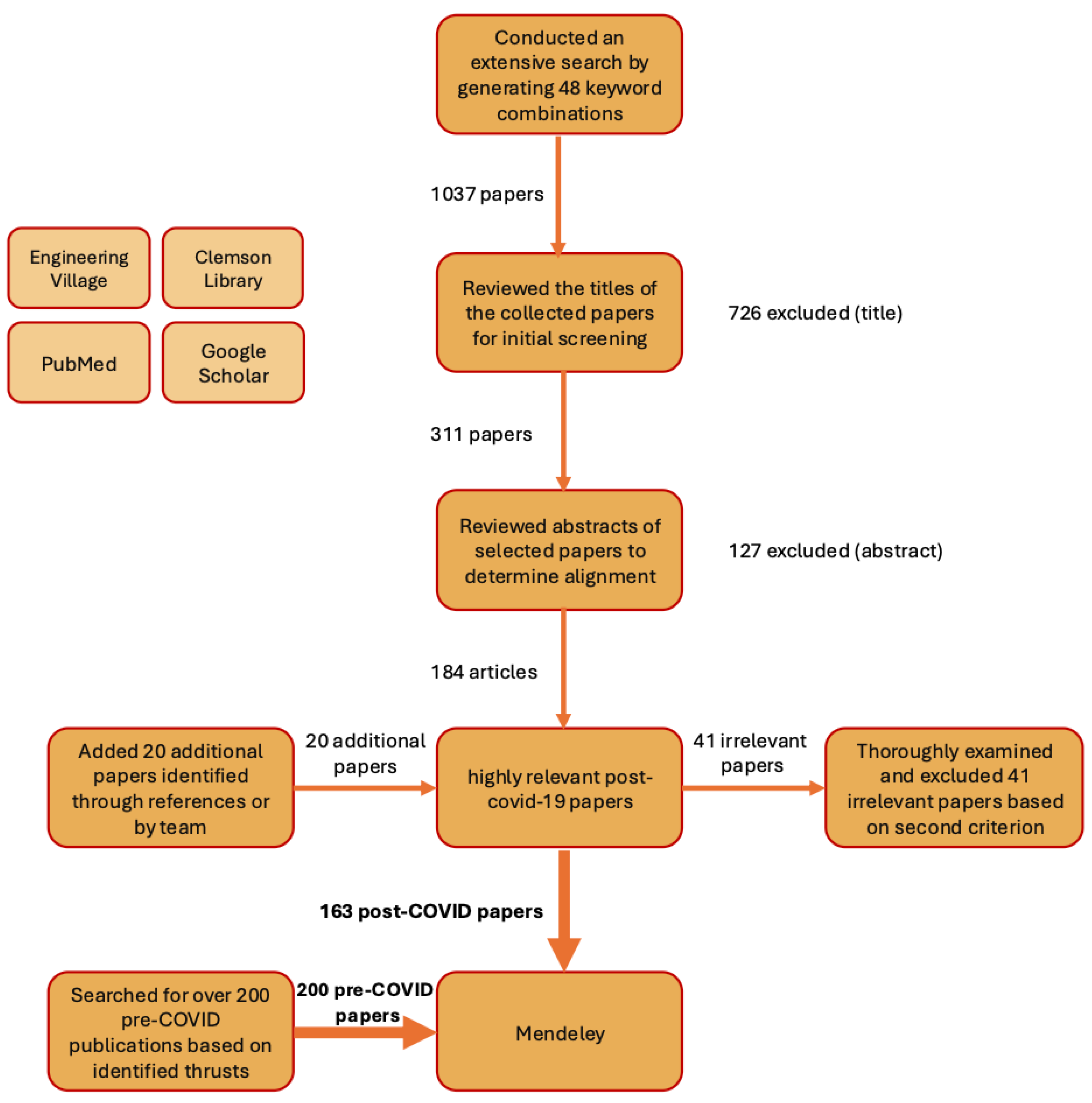
3. Methodology
3.1. Literature Search Strategy
3.2. Inclusion and Exclusion Criteria
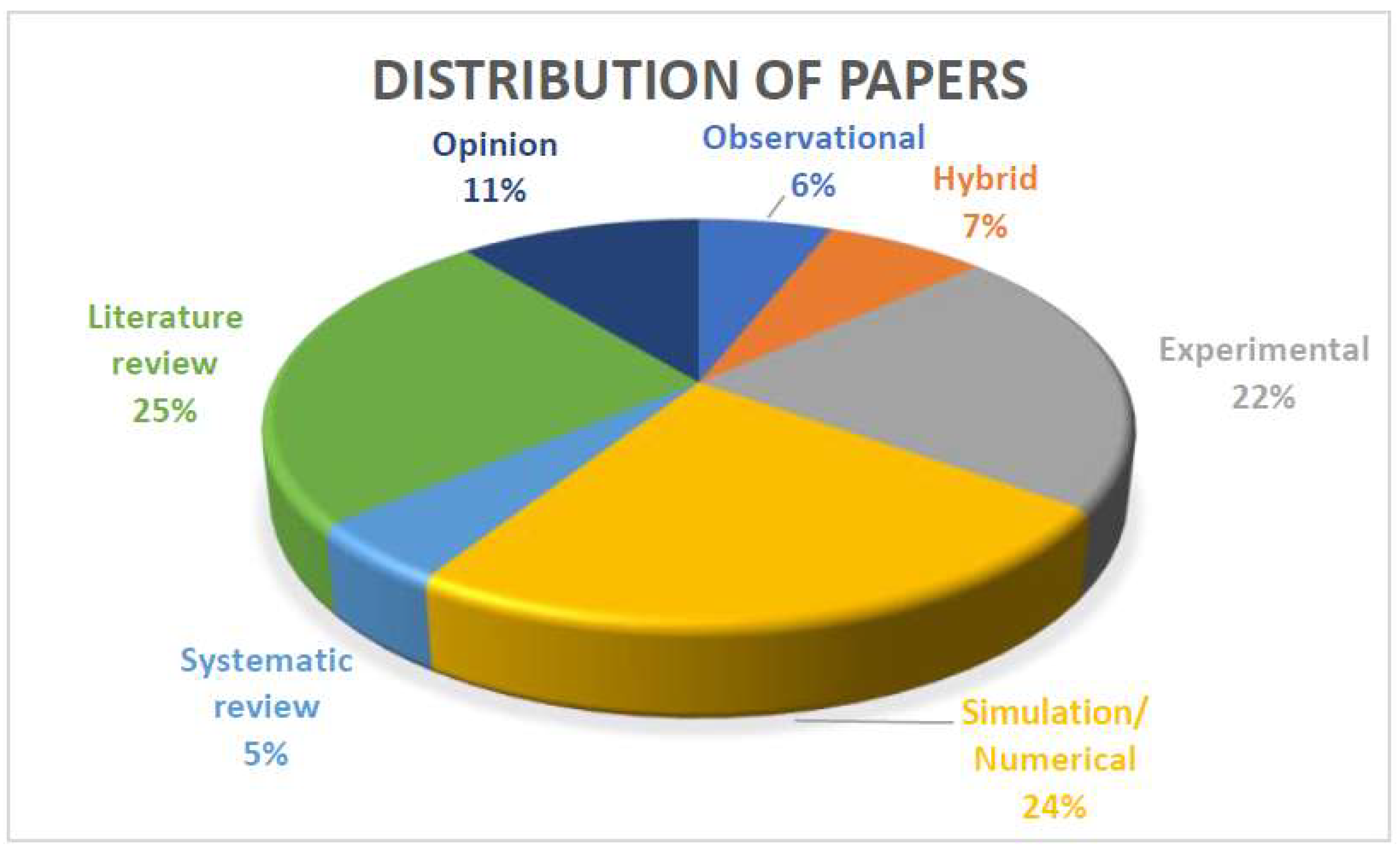
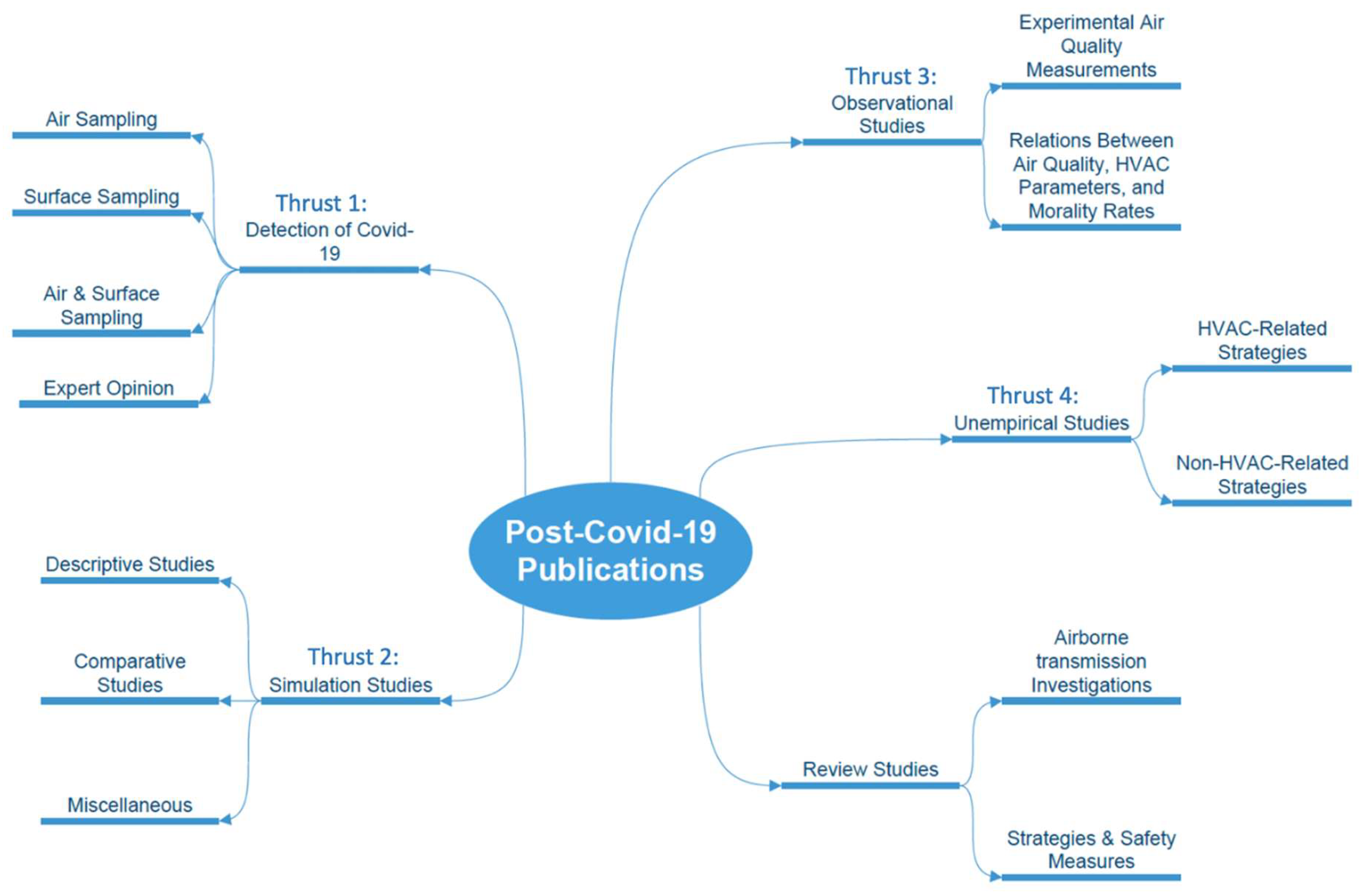
4. Results
4.1. Thrust 1: Detection
4.1.1. Air Sampling
4.1.2. Surface Sampling
4.1.3. Air & Surface Sampling
4.2. Thrust 2: Simulation Studies
4.2.1. Descriptive Studies
4.2.2. Comparative Studies
4.3. Thrust 3: Observational Studies
4.4. Thrust 4: Unempirical Studies
4.4.1. HVAC-Related Strategies
4.4.2. Non-HVAC-Related Strategies
4.4.3. Design-Related Strategies
5. Discussion
6. Conclusions
6.1. COVID-19’s Impact on Indoor Air Quality Knowledge in Healthcare
6.2. Unsubstantiated Recommendations in Post-COVID Scholarly Works
6.3. How Existing Knowledge and Experience Impact Recommendations
6.4. Path Forward
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Use of Artificial Intelligence
Conflicts of Interest
Abbreviations
| ACH | Air changes per hour |
| ACHe | Equivalent air changes per hour |
| AGP | Aerosol-generating procedure |
| AIIR | Airborne infection isolation room |
| CFD | Computational fluid dynamics |
| CO2 | Carbon dioxide |
| DMEM | Dulbecco’s Modified Eagle Medium |
| ER | Emergency room |
| HEPA | High efficiency particulate air |
| HVAC | Heating, ventilation, and air conditioning |
| IAQ | Indoor air quality |
| ICU | Intensive care unit |
| IoT | Internet of things |
| LEV | Local exhaust ventilation |
| MERV | Minimum efficiency reporting value |
| ML | Machine learning |
| N95 | N95 filtering facepiece respirator |
| OPC | Overall particle counter |
| OR | Operating room |
| PM10 | Particulate matter ≤ 10 μm |
| PM2.5 | Particulate matter ≤ 2.5 μm |
| PPE | Personal protective equipment |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| RH | Relative humidity |
| RNA | Ribonucleic acid |
| RT-PCR | Reverse transcription polymerase chain reaction |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus 2 |
| TMT | Total maximum time |
| ULPA | Ultra-low penetration air |
| UVGI | Ultraviolet germicidal irradiation |
References
- Rahimi, N.R.; Fouladi-Fard, R.; Aali, R.; Shahryari, A.; Rezaali, M.; Ghafouri, Y.; Ghalhari, M.R.; Asadi-Ghalhari, M.; Farzinnia, B.; Gea, O.C.; et al. Bidirectional association between COVID-19 and the environment: A systematic review. Environ. Res. 2021, 194, 110692. [Google Scholar] [CrossRef]
- Noorimotlagh, Z.; Jaafarzadeh, N.; Martínez, S.S.; Mirzaee, S.A. A systematic review of possible airborne transmission of the COVID-19 virus (SARS-CoV-2) in the indoor air environment. Environ. Res. 2021, 193, 110612. [Google Scholar] [CrossRef]
- Aghalari, Z.; Dahms, H.-U.; Sosa-Hernandez, J.E.; Oyervides-Muñoz, M.A.; Parra-Saldívar, R. Evaluation of SARS-CoV-2 transmission through indoor air in hospitals and prevention methods: A systematic review. Environ. Res. 2021, 195, 110841. [Google Scholar] [CrossRef]
- Rahmani, A.R.; Leili, M.; Azarian, G.; Poormohammadi, A. Sampling and detection of corona viruses in air: A mini review. Sci. Total Environ. 2020, 740, 140207. [Google Scholar] [CrossRef]
- Jayaweera, M.; Perera, H.; Gunawardana, B.; Manatunge, J. Transmission of COVID-19 virus by droplets and aerosols: A critical review on the unresolved dichotomy. Environ. Res. 2020, 188, 109819. [Google Scholar] [CrossRef]
- Fadaei, A. Ventilation Systems and COVID-19 Spread: Evidence from a Systematic Review Study. Eur. J. Sustain. Dev. Res. 2021, 5, em0157. [Google Scholar] [CrossRef]
- Fadaei, A. Influence of Ventilation in Healthcare Facilities Prevention of Infection COVID-19: Systematic Review Study. Eur. J. Sustain. Dev. Res. 2021, 5, em0170. [Google Scholar] [CrossRef]
- Chirico, F.; Sacco, A.; Bragazzi, N.L.; Magnavita, N. Can Air-Conditioning Systems Contribute to the Spread of SARS/MERS/COVID-19 Infection? Insights from a Rapid Review of the Literature. Int. J. Environ. Res. Public Health 2020, 17, 6052. [Google Scholar] [CrossRef]
- Hirota, K. Air contamination with SARS-CoV-2 in the operating room. J. Anesth. 2021, 35, 333–336. [Google Scholar] [CrossRef]
- Correia, G.; Rodrigues, L.; da Silva, M.G.; Gonçalves, T. Airborne route and bad use of ventilation systems as non-negligible factors in SARS-CoV-2 transmission. Med. Hypotheses 2020, 141, 109781. [Google Scholar] [CrossRef]
- Nair, A.N.; Anand, P.; George, A.; Mondal, N. A review of strategies and their effectiveness in reducing indoor airborne transmission and improving indoor air quality. Environ. Res. 2022, 213, 113579. [Google Scholar] [CrossRef]
- Güven, Y.; Sepet, E.; Sezgin, B.I.; Çelik, E.G. The Importance and Improvement of Indoor Air Quality in Dental Clinics within the context of COVID-19. EC Dent. Sci. 2021, 20, 32–50. [Google Scholar]
- Ahlawat, A.; Wiedensohler, A.; Mishra, S.K. An overview on the role of relative humidity in airborne transmission of SARS-CoV-2 in indoor environments. Aerosol Air Qual. Res. 2020, 20, 1856–1861. [Google Scholar] [CrossRef]
- Maulani, C.; Masulili, S.L.C.; Auerkari, E.I. COVID-19 transmission and dental treatment: A narrative review. In AIP Conference Proceedings; American Institute of Physics Inc.: College Park, ML, USA, 2021. [Google Scholar] [CrossRef]
- Engelman, D.T.; Lother, S.; George, I.; Funk, D.J.; Ailawadi, G.; Atluri, P.; Grant, M.C.; Haft, J.W.; Hassan, A.; Legare, J.-F.; et al. Adult Cardiac Surgery and the COVID-19 Pandemic: Aggressive Infection Mitigation Strategies Are Necessary in the Operating Room and Surgical Recovery. Ann. Thorac. Surg. 2020, 110, 707–711. [Google Scholar] [CrossRef]
- Theodorou, C.; Simpson, G.; Walsh, C. Theatre ventilation. R. Coll. Surg. Engl. 2021, 103, 151–154. [Google Scholar] [CrossRef]
- Dunne, C. The place of the literature review in grounded theory research. Int. J. Soc. Res. Methodol. 2011, 14, 111–124. [Google Scholar] [CrossRef]
- Ram, K.; Thakur, R.C.; Singh, D.K.; Kawamura, K.; Shimouchi, A.; Sekine, Y.; Nishimura, H.; Singh, S.K.; Pavuluri, C.M.; Singh, R.; et al. Why airborne transmission hasn’t been conclusive in case of COVID-19? An atmospheric science perspective. Sci. Total Environ. 2021, 773, 145525. [Google Scholar] [CrossRef]
- Faridi, S.; Niazi, S.; Sadeghi, K.; Naddafi, K.; Yavarian, J.; Shamsipour, M.; Jandaghi, N.Z.S.; Sadeghniiat, K.; Nabizadeh, R.; Yunesian, M.; et al. A field indoor air measurement of SARS-CoV-2 in the patient rooms of the largest hospital in Iran. Sci. Total Environ. 2020, 725, 138401. [Google Scholar] [CrossRef]
- Kenarkoohi, A.; Noorimotlagh, Z.; Falahi, S.; Amarloei, A.; Mirzaee, S.A.; Pakzad, I.; Bastani, E. Hospital indoor air quality monitoring for the detection of SARS-CoV-2 (COVID-19) virus. Sci. Total Environ. 2020, 748, 141324. [Google Scholar] [CrossRef]
- Masoumbeigi, H.; Ghanizadeh, G.; Arfaei, R.Y.; Heydari, S.; Goodarzi, H.; Sari, R.D.; Tat, M. Investigation of hospital indoor air quality for the presence of SARS-CoV-2. J. Environ. Health Sci. Eng. 2020, 18, 1259–1263. [Google Scholar] [CrossRef]
- Vosoughi, M.; Karami, C.; Dargahi, A.; Jeddi, F.; Jalali, K.M.; Hadisi, A.; Haghighi, S.B.; Dogahe, H.P.; Noorimotlagh, Z.; Mirzaee, S.A. Investigation of SARS-CoV-2 in hospital indoor air of COVID-19 patients’ ward with impinger method. Environ. Sci. Pollut. Res. 2021, 28, 50480–50488. [Google Scholar] [CrossRef]
- Grimalt, J.O.; Vílchez, H.; Fraile-Ribot, P.A.; Marco, E.; Campins, A.; Orfila, J.; van Drooge, B.L.; Fanjul, F. Spread of SARS-CoV-2 in hospital areas. Environ. Res. 2021, 204, 112074. [Google Scholar] [CrossRef]
- Nissen, K.; Krambrich, J.; Akaberi, D.; Hoffman, T.; Ling, J.; Lundkvist, Å.; Svensson, L.; Salaneck, E. Long-distance airborne dispersal of SARS-CoV-2 in COVID-19 wards. Sci. Rep. 2020, 10, 19589. [Google Scholar] [CrossRef]
- Ding, Z.; Qian, H.; Xu, B.; Huang, Y.; Miao, T.; Yen, H.-L.; Xiao, S.; Cui, L.; Wu, X.; Shao, W.; et al. Toilets dominate environmental detection of severe acute respiratory syndrome coronavirus 2 in a hospital. Sci. Total Environ. 2020, 753, 141710. [Google Scholar] [CrossRef]
- Jiang, Y.; Wang, H.; Chen, Y.; He, J.; Chen, L.; Liu, Y.; Hu, X.; Li, A.; Liu, S.; Zhang, P.; et al. Clinical Data on Hospital Environmental Hygiene Monitoring and Medical Staff Protection during the Coronavirus Disease 2019 Outbreak. medRxiv 2020. [Google Scholar] [CrossRef]
- Alkalamouni, H.; Hitti, E.; Zaraket, H. Adopting fresh air ventilation may reduce the risk of airborne transmission of SARS-CoV-2 in COVID-19 unit. J. Infect. 2021, 83, e4–e5. [Google Scholar] [CrossRef]
- Mouchtouri, V.A.; Koureas, M.; Kyritsi, M.; Vontas, A.; Kourentis, L.; Sapounas, S.; Rigakos, G.; Petinaki, E.; Tsiodras, S.; Hadjichristodoulou, C. Environmental contamination of SARS-CoV-2 on surfaces, air-conditioner and ventilation systems. Int. J. Hyg. Environ. Health 2020, 230, 113599. [Google Scholar] [CrossRef]
- Razzini, K.; Castrica, M.; Menchetti, L.; Maggi, L.; Negroni, L.; Orfeo, N.V.; Pizzoccheri, A.; Stocco, M.; Muttini, S.; Balzaretti, C.M. SARS-CoV-2 RNA detection in the air and on surfaces in the COVID-19 ward of a hospital in Milan, Italy. Sci. Total Environ. 2020, 742, 140540. [Google Scholar] [CrossRef]
- Alrebi, O.F.; Obeidat, B.; Abdallah, I.A.; Darwish, E.F.; Amhamed, A. Airflow dynamics in an emergency department: A CFD simulation study to analyse COVID-19 dispersion. Alex. Eng. J. 2021, 61, 3435–3445. [Google Scholar] [CrossRef]
- Anuraghava, C.; Abhiram, K.; Reddy, V.N.S.; Rajan, H. CFD modelling of airborne virus diffusion characteristics in a negative pressure room with mixed mode ventilation. Int. J. Simul. Multidiscip. Des. Optim. 2021, 12, 1. [Google Scholar] [CrossRef]
- Zhou, Y.; Ji, S. Experimental and numerical study on the transport of droplet aerosols generated by occupants in a fever clinic. Build. Environ. 2021, 187, 107402. [Google Scholar] [CrossRef]
- Anghel, L.; Popovici, C.-G.; Stătescu, C.; Sascău, R.; Verdeș, M.; Ciocan, V.; Șerban, I.-L.; Mărănducă, M.A.; Hudișteanu, S.-V.; Țurcanu, F.-E. Impact of HVAC-systems on the dispersion of infectious aerosols in a cardiac intensive care unit. Int. J. Environ. Res. Public Health 2020, 17, 6582. [Google Scholar] [CrossRef]
- Beaussier, M.; Vanoli, E.; Zadegan, F.; Peray, H.; Bezian, E.; Jilesen, J.; Gandveau, G.; Gayraud, J.-M. Aerodynamic analysis of hospital ventilation according to seasonal variations. A simulation approach to prevent airborne viral transmission pathway during COVID-19 pandemic. Environ. Int. 2022, 158, 106872. [Google Scholar] [CrossRef]
- Satheesan, M.K.; Mui, K.W.; Wong, L.T. A numerical study of ventilation strategies for infection risk mitigation in general inpatient wards. Build. Simul. 2020, 13, 887–896. [Google Scholar] [CrossRef]
- Wang, J.-X.; Cao, X.; Chen, Y.-P. An air distribution optimization of hospital wards for minimizing cross-infection. J. Clean. Prod. 2021, 279, 123431. [Google Scholar] [CrossRef]
- Ghorui, S. CFD Study of Ventilation in a Room Maintained Under Negative-Pressure to Prevent Airborne Contamination; FOSSEE IIT Bombay: Mumbai, Maharashtra, India, 2020. [Google Scholar]
- Feng, Y.; Zhao, J.; Spinolo, M.; Lane, K.; Leung, D.; Marshall, D.; Mlinaric, P. Assessing the filtration effectiveness of a portable ultraviolet air cleaner on airborne SARS-CoV-2 laden droplets in a patient room: A numerical study. Aerosol Air Qual. Res. 2021, 21, 200608. [Google Scholar] [CrossRef]
- Pease, L.F.; Wang, N.; Salsbury, T.I.; Underhill, R.M.; Flaherty, J.E.; Vlachokostas, A.; Kulkarni, G.; James, D.P. Investigation of potential aerosol transmission and infectivity of SARS-CoV-2 through central ventilation systems. Build. Environ. 2021, 197, 107633. [Google Scholar] [CrossRef]
- Wang, F.; Chaerasari, C.; Rakshit, D.; Permana, I.; Kusnandar. Performance Improvement of a Negative-Pressurized Isolation Room for Infection Control. Healthcare 2021, 9, 1081. [Google Scholar] [CrossRef]
- Borro, L.; Mazzei, L.; Raponi, M.; Piscitelli, P.; Miani, A.; Secinaro, A. The role of air conditioning in the diffusion of SARS-CoV-2 in indoor environments: A first computational fluid dynamic model, based on investigations performed at the Vatican State Children’s hospital. Environ. Res. 2021, 193, 110343. [Google Scholar] [CrossRef]
- Park, J.; Lee, K.S.; Park, H. Optimized mechanism for fast removal of infectious pathogen-laden aerosols in the negative-pressure unit. J. Hazard. Mater. 2022, 435, 128978. [Google Scholar] [CrossRef]
- King, K.G.; Delclos, G.L.; Brown, E.L.; Emery, S.T.; Yamal, J.M.; Emery, R.J. An assessment of outpatient clinic room ventilation systems and possible relationship to disease transmission. Am. J. Infect. Control 2021, 49, 808–812. [Google Scholar] [CrossRef]
- ANSI/ASHRAE/ASHE Standard 170-2017; Ventilation of Health Care Facilities. ASHRAE: Atlanta, GA, USA, 2017.
- Tsui, B.C.; Pan, S. Are aerosol-generating procedures safer in an airborne infection isolation room or operating room? Br. J. Anaesth. 2020, 125, e485–e487. [Google Scholar] [CrossRef]
- Nimra, A.; Ali, Z.; Nasir, Z.A.; Tyrrel, S.; Sidra, S. Characterization of Indoor Air Quality in Relation to Ventilation Practices in Hospitals of Lahore, Pakistan. Sains Malays. 2021, 50, 1609–1620. [Google Scholar] [CrossRef]
- Tang, J.W.; Marr, L.C.; Li, Y.; Dancer, S.J. COVID-19 has redefined airborne transmission. BMJ 2021, 373, n913. [Google Scholar] [CrossRef]
- Morawska, L.; Tang, J.W.; Bahnfleth, W.; Bluyssen, P.M.; Boerstra, A.; Buonanno, G.; Cao, J.; Dancer, S.; Floto, A.; Franchimon, F.; et al. How can airborne transmission of COVID-19 indoors be minimised? Environ. Int. 2020, 142, 105832. [Google Scholar] [CrossRef]
- Tian, Y.; Gong, Y.; Liu, P.; Wang, S.; Xu, X.; Wang, X.; Huang, Y. Infection Prevention Strategy in Operating Room during Coronavirus Disease 2019 (COVID-19) Outbreak. Chin. Med. Sci. J. 2020, 35, 114–120. [Google Scholar] [CrossRef]
- Al-Benna, S. Negative pressure rooms and COVID-19. J. Perioper. Pract. 2021, 31, 18–23. [Google Scholar] [CrossRef]
- Rezaei, N.; Jafari, M.; Nazari, A.; Salehi, S.; Talati, F.; Torab, R.; Nejad-Rahim, R. A novel methodology and new concept of SARS-CoV-2 elimination in heating and ventilating air conditioning systems using waste heat recovery. AIP Adv. 2020, 10, 085308. [Google Scholar] [CrossRef]
- Bhagat, R.K.; Linden, P.F. Displacement ventilation: A viable ventilation strategy for makeshift hospitals and public buildings to contain COVID-19 and other airborne diseases: Ventilation strategy for COVID-19. R. Soc. Open Sci. 2020, 7, 200680. [Google Scholar] [CrossRef]
- Allen, J.G.; Ibrahim, A.M. Indoor Air Changes and Potential Implications for SARS-CoV-2 Transmission. JAMA 2021, 325, 2112–2113. [Google Scholar] [CrossRef]
- Chen, C.; Zhao, B. Makeshift hospitals for COVID-19 patients: Where health-care workers and patients need sufficient ventilation for more protection. J. Hosp. Infect. 2020, 105, 98–99. [Google Scholar] [CrossRef] [PubMed]
- Lynch, R.M.; Goring, R. Practical Steps to Improve Air Flow in Long-Term Care Resident Rooms to Reduce COVID-19 Infection Risk. J. Am. Med. Dir. Assoc. 2020, 21, 893–894. [Google Scholar] [CrossRef] [PubMed]
- Elias, B.; Bar-Yam, Y. Could Air Filtration Reduce COVID-19 Severity and Spread? New England Complex Systems Institute: Cambridge, MA, USA, 2020; Volume 9, pp. 1–4. [Google Scholar]
- Nwanaji-Enwerem, J.C.; Allen, J.G.; Beamer, P.I. Another invisible enemy indoors: COVID-19, human health, the home, and United States indoor air policy. J. Expo. Sci. Environ. Epidemiol. 2020, 30, 773–775. [Google Scholar] [CrossRef]
- Morawska, L.; Allen, J.; Bahnfleth, W.; Bluyssen, P.M.; Boerstra, A.; Buonanno, G.; Cao, J.; Dancer, S.J.; Floto, A.; Franchimon, F.; et al. A paradigm shift to combat indoor respiratory infection. Science 2021, 372, 689–691. [Google Scholar] [CrossRef]
- Santos, A.F.; Gaspar, P.D.; Hamandosh, A.; de Aguiar, E.B.; Filho, A.C.G.; de Souza, H.J.L. Best Practices on HVAC Design to Minimize the Risk of COVID-19 Infection within Indoor Environments. Braz. Arch. Biol. Technol. 2020, 63, e20200335. [Google Scholar] [CrossRef]
- Ahlawat, A.; Mishra, S.K.; Birks, J.W.; Costabile, F.; Wiedensohler, A. Preventing airborne transmission of SARS-CoV-2 in hospitals and nursing homes. Int. J. Environ. Res. Public Health 2020, 17, 8553. [Google Scholar] [CrossRef]
- Choi, H.; Chatterjee, P.; Lichtfouse, E.; Martel, J.A.; Hwang, M.; Jinadatha, C.; Sharma, V.K. Classical and alternative disinfection strategies to control the COVID-19 virus in healthcare facilities: A review. Environ. Chem. Lett. 2021, 19, 1945–1951. [Google Scholar] [CrossRef]
- Ho, Y.-H.; Li, P.-E.; Chen, L.-J.; Liu, Y.-L. Indoor air quality monitoring system for proactive control of respiratory infectious diseases: Poster abstract. In Proceedings of the SenSys 2020—2020 18th ACM Conference on Embedded Networked Sensor Systems, Virtual, 16 November 2020; Association for Computing Machinery, Inc.: New York, NY, USA, 2020; pp. 693–694. [Google Scholar] [CrossRef]
- Saini, J.; Dutta, M.; Marques, G. Indoor Air Quality Monitoring Systems and COVID-19. In Emerging Technologies During the Era of COVID-19 Pandemic; Studies in Systems, Decision and Control; Springer Science and Business Media Deutschland GmbH: Berlin/Heidelberg, Germany, 2021; Volume 348, pp. 133–147. [Google Scholar] [CrossRef]
- Capolongo, S.; Gola, M.; Brambilla, A.; Morganti, A.; Mosca, E.I.; Barach, P. COVID-19 and healthcare facilities: A decalogue of design strategies for resilient hospitals. Acta Bio-Medica Atenei Parm. 2020, 91, 50–60. [Google Scholar] [CrossRef]
- Makram, A.; El-Ashmawy, R.A. Future Hospital Building Design Strategies Post COVID-19 Pandemic. Int. J. Sustain. Dev. Plan. 2022, 17, 1169–1179. [Google Scholar] [CrossRef]
- Zhang, Y.; Han, O.; Li, A.; Hou, L.; Olofsson, T.; Zhang, L.; Lei, W. Adaptive wall-based attachment ventilation: A comparative study on its effectiveness in airborne infection isolation rooms with negative pressure. Engineering 2022, 8, 130–137. [Google Scholar] [CrossRef]
- Nielsen, P.V.; Li, Y.; Buus, M.; Winther, F.V. Risk of cross-infection in a hospital ward with downward ventilation. Build. Environ. 2010, 45, 2008–2014. [Google Scholar] [CrossRef]
- Qian, H.; Li, Y.; Nielsen, P.V.; Hyldgaard, C.E. Dispersion of exhalation pollutants in a two-bed hospital ward with a downward ventilation system. Build. Environ. 2008, 43, 344–354. [Google Scholar] [CrossRef]
- Nielsen, P.V.; Li, Y.; Buus, M.; Winther, F.V.; Qian, H. Cross infection in a hospital ward and deposition of particles exhaled from a source manikin. In Proceedings of the Fifth International Workshop on Energy and Environment of Residential Buildings and the Third International Conference on Built Environment and Public Health, Guilin, China, 29–31 May 2009. [Google Scholar]
- Qian, H.; Zheng, X. Ventilation control for airborne transmission of human exhaled bio-aerosols in buildings. J. Thorac. Dis. 2018, 10, S2295–S2304. [Google Scholar] [CrossRef] [PubMed]
- Kao, P.; Yang, R. Virus diffusion in isolation rooms. J. Hosp. Infect. 2006, 62, 338–345. [Google Scholar] [CrossRef]
- Reddy, S.C.; Valderrama, A.L.; Kuhar, D.T. Improving the Use of Personal Protective Equipment: Applying Lessons Learned. Clin. Infect. Dis. 2019, 69, S165–S170. [Google Scholar] [CrossRef]
- John, A.; Tomas, M.E.; Cadnum, J.L.; Mana, T.S.; Jencson, A.; Shaikh, A.; Zabarsky, T.F.; Wilson, B.M.; Donskey, C.J. Are health care personnel trained in correct use of personal protective equipment? Am. J. Infect. Control 2016, 44, 840–842. [Google Scholar] [CrossRef]
- Reid, S.M.; Farion, K.J.; Suh, K.N.; Audcent, T.; Barrowman, N.J.; Plint, A.C. Use of personal protective equipment in Canadian pediatric emergency departments. Can. J. Emerg. Med. 2011, 13, 71–78. [Google Scholar] [CrossRef][Green Version]
- Sargent, E.V.; Gallo, F. Use of Personal Protective Equipment for Respiratory Protection. ILAR J. 2003, 44, 52–56. [Google Scholar] [CrossRef]
- Fischer, W.A.; Weber, D.J.; Wohl, D.A. Personal Protective Equipment: Protecting Health Care Providers in an Ebola Outbreak. Clin. Ther. 2015, 37, 2402–2410. [Google Scholar] [CrossRef]
- Morawska, L.; Cao, J. Airborne transmission of SARS-CoV-2: The world should face the reality. Environ. Int. 2020, 139, 105730. [Google Scholar] [CrossRef]
- Houghton, C.; Meskell, P.; Delaney, H.; Smalle, M.; Glenton, C.; Booth, A.; Chan, X.H.S.; Devane, D.; Biesty, L.M. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: A rapid qualitative evidence synthesis. Cochrane Database Syst. Rev. 2020, 2020, CD013582. [Google Scholar] [CrossRef] [PubMed]
- Harper, S.A.; Fukuda, K.; Uyeki, T.M.; Cox, N.J.; Bridges, C.B. Prevention and Control of Influenza: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. 2005, 54, 1–41. [Google Scholar] [PubMed]
- Arnold, F.W.; LaJoie, A.S.; Brock, G.N.; Peyrani, P.; Rello, J.; Menéndez, R.; Lopardo, G.; Torres, A.; Rossi, P.; Ramirez, J.A.; et al. Improving Outcomes in Elderly Patients With Community-Acquired Pneumonia by Adhering to National Guidelines Community-Acquired Pneumonia Organization International Cohort Study Results. Arch. Intern. Med. 2009, 169, 1515–1524. [Google Scholar] [CrossRef] [PubMed]
- McIntosh, K.A.; Maxwell, D.J.; Pulver, L.K.; Horn, F.; Robertson, M.B.; Kaye, K.I.; Peterson, G.M.; Dollman, W.B.; Wai, A.; Tett, S.E. A quality improvement initiative to improve adherence to national guidelines for empiric management of community-acquired pneumonia in emergency departments. Int. J. Qual. Health Care 2011, 23, 142–150. [Google Scholar] [CrossRef]
- Durando, P.; Bassetti, M.; Orengo, G.; Crimi, P.; Battistini, A.; Bellina, D.; Talamini, A.; Tiberio, G.; Alicino, C.; Iudici, R.; et al. Adherence to international and national recommendations for the prevention of surgical site infections in Italy: Results from an observational prospective study in elective surgery. Am. J. Infect. Control 2012, 40, 969–972. [Google Scholar] [CrossRef]
- Landers, T.; Abusalem, S.; Coty, M.-B.; Bingham, J. Patient-centered hand hygiene: The next step in infection prevention. Am. J. Infect. Control 2012, 40, S11–S17. [Google Scholar] [CrossRef]
- Nancy, B. The Evolution Handwashing to Hand Hygiene Guidance. Crit. Care Nurs. Q. 2004, 27, 295–307. [Google Scholar]
- Bloomfield, S.F.; Aiello, A.E.; Cookson, B.; O’BOyle, C.; Larson, E.L. The effectiveness of hand hygiene procedures in reducing the risks of infections in home and community settings including handwashing and alcohol-based hand sanitizers. Am. J. Infect. Control 2007, 35, S27–S64. [Google Scholar] [CrossRef]
- Jumaa, P. Hand hygiene: Simple and complex. Int. J. Infect. Dis. 2005, 9, 3–14. [Google Scholar] [CrossRef]
- Allegranzi, B.; Pittet, D. Role of hand hygiene in healthcare-associated infection prevention. J. Hosp. Infect. 2009, 73, 305–315. [Google Scholar] [CrossRef]
- Boyce, J.M. Modern technologies for improving cleaning and disinfection of environmental surfaces in hospitals. Antimicrob. Resist. Infect. Control 2016, 5, 10. [Google Scholar] [CrossRef]
- Dancer, S. The role of environmental cleaning in the control of hospital-acquired infection. J. Hosp. Infect. 2009, 73, 378–385. [Google Scholar] [CrossRef]
- Escombe, A.R.; Oeser, C.C.; Gilman, R.H.; Navincopa, M.; Ticona, E.; Pan, W.; Martínez, C.; Chacaltana, J.; Rodríguez, R.; Moore, D.A.J.; et al. Natural ventilation for the prevention of airborne contagion. PLoS Med. 2007, 4, e68. [Google Scholar] [CrossRef]
- Mehta, Y.; Gupta, A.; Todi, S.; Myatra, S.; Samaddar, D.P.; Patil, V.; Bhattacharya, P.K.; Ramasubban, S. Guidelines for prevention of hospital acquired infections. Indian J. Crit. Care Med. 2014, 18, 149–163. [Google Scholar] [CrossRef]
- Guo, Y.; Qian, H.; Sun, Z.; Cao, J.; Liu, F.; Luo, X.; Ling, R.; Weschler, L.B.; Mo, J.; Zhang, Y. Assessing and controlling infection risk with Wells-Riley model and spatial flow impact factor (SFIF). Sustain. Cities Soc. 2021, 67, 102719. [Google Scholar] [CrossRef]
- Yu, I.T.; Li, Y.; Wong, T.W.; Tam, W.; Chan, A.T.; Lee, J.H.; Leung, D.Y.; Ho, T. Evidence of Airborne Transmission of the Severe Acute Respiratory Syndrome Virus. N. Engl. J. Med. 2004, 350, 1731–1739. [Google Scholar] [CrossRef] [PubMed]
- Ha, L.D.; Bloom, S.A.; Hien, N.Q.; Maloney, S.A.; Mai, L.Q.; Leitmeyer, K.C.; Anh, B.H.; Reynolds, M.G.; Montgomery, J.M.; Comer, J.A.; et al. Lack of SARS Transmission among Public Hospital Workers, Vietnam. Emerg. Infect. Dis. 2004, 10, 265–268. [Google Scholar] [CrossRef] [PubMed]
- Mao, J.; Gao, N. The airborne transmission of infection between flats in high-rise residential buildings: A review. Build. Environ. 2015, 94, 516–531. [Google Scholar] [CrossRef] [PubMed]
- Brankston, G.; Gitterman, L.; Hirji, Z.; Lemieux, C.; Gardam, M. Transmission of influenza A in human beings. Lancet Infect. Dis. 2007, 7, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Seto, W. Airborne transmission and precautions: Facts and myths. J. Hosp. Infect. 2015, 89, 225–228. [Google Scholar] [CrossRef]
- Zhou, L.; Yao, M.; Zhang, X.; Hu, B.; Li, X.; Chen, H.; Zhang, L.; Liu, Y.; Du, M.; Sun, B.; et al. Breath-, air- and surface-borne SARS-CoV-2 in hospitals. J. Aerosol. Sci. 2020, 152, 105693. [Google Scholar] [CrossRef]
- Daisey, J.M.; Angell, W.J.; Apte, M.G. Indoor air quality, ventilation and health symptoms in schools: An analysis of existing information. Indoor Air 2003, 13, 53–64. [Google Scholar] [CrossRef]
- Goyal, R.; Khare, M. Indoor Air Quality: Current Status, Missing Links and Future Road Map for India. J. Civ. Environ. Eng. 2012, 2, 2–4. [Google Scholar] [CrossRef]
- Kennedy, M.; Lee, S.J.; Epstein, M. Modeling aerosol transmission of SARS-CoV-2 in multi-room facility. J. Loss Prev. Process Ind. 2021, 69, 104336. [Google Scholar] [CrossRef]
- Miller-Leiden, S.; Lohascio, C.; Nazaroff, W.W.; Macher, J. Effectiveness of In-Room Air Filtration and Dilution Ventilation for Tuberculosis Infection Control. J. Air Waste Manag. Assoc. 1996, 46, 869–882. [Google Scholar] [CrossRef]
- Adal, K.A.; Anglim, A.M.; Palumbo, C.L.; Titus, M.G.; Coyner, B.J.; Farr, B.M. The Use of High-Efficiency Particulate Air-Filter Respirators to Protect Hospital Workers from Tuberculosis--A Cost-Effectiveness Analysis. N. Engl. J. Med. 1994, 331, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Salam, Z.-H.A.; Karlin, R.B.; Ling, M.L.; Yang, K.S. The impact of portable high-efficiency particulate air filters on the incidence of invasive aspergillosis in a large acute tertiary-care hospital. Am. J. Infect. Control 2010, 38, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Aliabadi, A.A.; Rogak, S.N.; Bartlett, K.H.; Green, S.I. Preventing Airborne Disease Transmission: Review of Methods for Ventilation Design in Health Care Facilities. Adv. Prev. Med. 2011, 2011, 124064. [Google Scholar] [CrossRef] [PubMed]
- Azimi, P.; Stephens, B. HVAC filtration for controlling infectious airborne disease transmission in indoor environments: Predicting risk reductions and operational costs. Build. Environ. 2013, 70, 150–160. [Google Scholar] [CrossRef]
- Jefferson, T.; Foxlee, R.; Del Mar, C.; Dooley, L.; Ferroni, E.; Hewak, B.; Prabhala, A.; Nair, S.; Rivetti, A. Physical interventions to interrupt or reduce the spread of respiratory viruses: Systematic review. BMJ 2008, 336, 77–80. [Google Scholar] [CrossRef]
- Lee, K.; Shukla, V.; Clark, M.; Mierzwinski-Urban, M.; Pessoa-Silva, C.; Conly, J. Physical Interventions to Interrupt or Reduce the Spread of Respiratory Viruses—Resource Use Implications: A Systematic Review. CADTH Technol. Overv. 2011, 2, e2302. [Google Scholar]
- Larson, E.; Kretzer, E. Compliance with handwashing and barrier precautions. J. Hosp. Infect. 1995, 30, 88–106. [Google Scholar] [CrossRef] [PubMed]
- Garbey, M.; Joerger, G.; Furr, S. A systems approach to assess transport and diffusion of hazardous airborne particles in a large surgical suite: Potential impacts on viral airborne transmission. Int. J. Environ. Res. Public Health 2020, 17, 5404. [Google Scholar] [CrossRef]
- Tang, J.W.; Nicolle, A.; Pantelic, J.; Klettner, C.A.; Su, R.; Kalliomaki, P.; Saarinen, P.; Koskela, H.; Reijula, K.; Mustakallio, P.; et al. Different Types of Door-Opening Motions as Contributing Factors to Containment Failures in Hospital Isolation Rooms. PLoS ONE 2013, 8, e66663. [Google Scholar] [CrossRef]
- Kalliomäki, P.; Saarinen, P.; Tang, J.W.; Koskela, H. Airflow patterns through single hinged and sliding doors in hospital isolation rooms—Effect of ventilation, flow differential and passage. Build. Environ. 2016, 107, 154–168. [Google Scholar] [CrossRef]
- Sadrizadeh, S.; Pantelic, J.; Sherman, M.; Clark, J.; Abouali, O. Airborne particle dispersion to an operating room environment during sliding and hinged door opening. J. Infect. Public Health 2018, 11, 631–635. [Google Scholar] [CrossRef]
- Cheong, K.; Chong, K. Development and application of an indoor air quality audit to an air-conditioned building in Singapore. Build. Environ. 2001, 36, 181–188. [Google Scholar] [CrossRef]
- Sun, S.; Zheng, X.; Villalba-Díez, J.; Ordieres-Meré, J. Indoor air-quality data-monitoring system: Long-term monitoring benefits. Sensors 2019, 19, 4157. [Google Scholar] [CrossRef]
- Kim, J.-Y.; Chu, C.-H.; Shin, S.-M. ISSAQ: An integrated sensing systems for real-time indoor air quality monitoring. IEEE Sens. J. 2014, 14, 4230–4244. [Google Scholar] [CrossRef]
- Yang, C.-T.; Liao, C.-J.; Liu, J.-C.; Den, W.; Chou, Y.-C.; Tsai, J.-J. Construction and application of an intelligent air quality monitoring system for healthcare environment. J. Med. Syst. 2014, 38, 15. [Google Scholar] [CrossRef]
- Asthana, P.; Mishra, S. IoT Enabled Real Time Bolt based Indoor Air Quality Monitoring System. In Proceedings of the 2018 International Conference on Computational and Characterization Techniques in Engineering & Sciences (CCTES) Integral University, Lucknow, India, 14–15 September 2018. [Google Scholar]
- Memarzadeh, F.; Olmsted, R.N.; Bartley, J.M. Applications of ultraviolet germicidal irradiation disinfection in health care facilities: Effective adjunct, but not stand-alone technology. Am. J. Infect. Control 2010, 38, S13–S24. [Google Scholar] [CrossRef]
- Ethington, T.; Newsome, S.; Waugh, J.; Lee, L.D. Cleaning the air with ultraviolet germicidal irradiation lessened contact infections in a long-term acute care hospital. Am. J. Infect. Control 2018, 46, 482–486. [Google Scholar] [CrossRef] [PubMed]
- Reed, N.G. The History of Ultraviolet Germicidal Irradiation for Air Disinfection. Public Health Rep. 2010, 125, 15–27. [Google Scholar] [CrossRef] [PubMed]
- Green, C.F.; Scarpino, P.V. The use of ultraviolet germicidal irradiation (UVGI) in disinfection of airborne bacteria. Environ. Eng. Policy 2001, 3, 101–107. [Google Scholar] [CrossRef]
- Kujundzic, E.; Matalkah, F.; Howard, C.J.; Hernandez, M.; Miller, S.L. UV air cleaners and upper-room air ultraviolet germicidal irradiation for controlling airborne bacteria and fungal spores. J. Occup. Environ. Hyg. 2006, 3, 536–546. [Google Scholar] [CrossRef]
- Hsiao, T.-C.; Chuang, H.-C.; Griffith, S.M.; Chen, S.-J.; Young, L.-H. COVID-19: An aerosol’s point of view from expiration to transmission to viral-mechanism. Aerosol Air Qual. Res. 2020, 20, 905–910. [Google Scholar] [CrossRef]
- Li, Y.; Leung, G.M.; Tang, J.W.; Yang, X.; Chao, C.Y.H.; Lin, J.Z.; Lu, J.W.; Nielsen, P.V.; Niu, J.; Qian, H.; et al. Role of ventilation in airborne transmission of infectious agents in the built environment? A multidisciplinary systematic review. Indoor Air 2007, 17, 2–18. [Google Scholar] [CrossRef]
- Tang, J.; Li, Y.; Eames, I.; Chan, P.; Ridgway, G. Factors involved in the aerosol transmission of infection and control of ventilation in healthcare premises. J. Hosp. Infect. 2006, 64, 100–114. [Google Scholar] [CrossRef]
- Luongo, J.C.; Fennelly, K.P.; Keen, J.A.; Zhai, Z.J.; Jones, B.W.; Miller, S.L. Role of mechanical ventilation in the airborne transmission of infectious agents in buildings. Indoor Air 2016, 26, 666–678. [Google Scholar] [CrossRef]
- Knibbs, L.D.; Morawska, L.; Bell, S.C.; Grzybowski, P. Room ventilation and the risk of airborne infection transmission in 3 health care settings within a large teaching hospital. Am. J. Infect. Control 2011, 39, 866–872. [Google Scholar] [CrossRef]
- Vonci, N.; De Marco, M.F.; Grasso, A.; Spataro, G.; Cevenini, G.; Messina, G. Association between air changes and airborne microbial contamination in operating rooms. J. Infect. Public Health 2019, 12, 827–830. [Google Scholar] [CrossRef]
- Nielsen, P.V. Control of airborne infectious diseases in ventilated spaces. J. R. Soc. Interface 2009, 6, S747–S755. [Google Scholar] [CrossRef]
- Sundell, J.; Levin, H.; Nazaroff, W.W.; Cain, W.S.; Fisk, W.J.; Grimsrud, D.T.; Gyntelberg, F.; Li, Y.; Persily, A.K.; Pickering, A.C.; et al. Ventilation rates and health: Multidisciplinary review of the scientific literature. Indoor Air 2011, 21, 191–204. [Google Scholar] [CrossRef]
- Cooke, M.W.; Higgins, J.; Kidd, P. Use of emergency observation and assessment wards: A systematic literature review. Emerg. Med. J. 2003, 20, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, J.; Chartier, Y.; Pessoa-Silva, C.L.; Jensen, P.; Li, Y.; Seto, W.-H. Natural Ventilation for Infection Control in Healthcare Settings; WHO Publication: Geneva, Switzerland, 2009. [Google Scholar]
- Qian, H.; Li, Y.; Seto, W.; Ching, P.; Ching, W.; Sun, H. Natural ventilation for reducing airborne infection in hospitals. Build. Environ. 2010, 45, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Hobday, R.; Dancer, S. Roles of sunlight and natural ventilation for controlling infection: Historical and current perspectives. J. Hosp. Infect. 2013, 84, 271–282. [Google Scholar] [CrossRef] [PubMed]
- Escombe, A.R.; Ticona, E.; Chávez-Pérez, V.; Espinoza, M.; Moore, D.A.J. Improving natural ventilation in hospital waiting and consulting rooms to reduce nosocomial tuberculosis transmission risk in a low resource setting. BMC Infect. Dis. 2019, 19, 88. [Google Scholar] [CrossRef]
- Chaivisit, P.; Fontana, A.; Galindo, S.; Strub, C.; Choosong, T.; Kantachote, D.; Suksaroj, T.T. Airborne bacteria and fungi distribution characteristics in natural ventilation system of a university hospital in Thailand. EnvironmentAsia 2018, 11, 53–66. [Google Scholar] [CrossRef]
- Haas, C.N.; Rycroft, T.; Bibby, K.; Casson, L. Risks from Ebolavirus Discharge from Hospitals to Sewer Workers. Water Environ. Res. 2017, 89, 357–368. [Google Scholar] [CrossRef]
- Teixeira, J.V.; Miranda, S.; Monteiro, R.A.R.; Lopes, F.V.S.; Madureira, J.; Silva, G.V.; Pestana, N.; Pinto, E.; Vilar, V.J.P.; Boaventura, R.A.R. Assessment of indoor airborne contamination in a wastewater treatment plant. Environ. Monit. Assess. 2013, 185, 59–72. [Google Scholar] [CrossRef]
- Goldmann, D.A. Transmission of viral respiratory infections in the home. Pediatr. Infect. Dis. J. 2000, 19, S97–S102. [Google Scholar] [CrossRef] [PubMed]
- Beggs, C.B. The Airborne Transmission of Infection in Hospital Buildings: Fact or Fiction? Indoor Built Environ. 2003, 12, 9–18. [Google Scholar] [CrossRef]
- Seto, W.; Conly, J.; Silva, C.P.; Malik, M.; Eremin, S. Infection prevention and control measures for acute respiratory infections in healthcare settings: An update. East. Mediterr. Health J. 2013, 19, S39–S47. [Google Scholar] [CrossRef]
- Wei, J.; Li, Y. Airborne spread of infectious agents in the indoor environment. Am. J. Infect. Control 2016, 44, S102–S108. [Google Scholar] [CrossRef]
- Fernstrom, A.; Goldblatt, M. Aerobiology and Its Role in the Transmission of Infectious Diseases. J. Pathog. 2013, 2013, 493960. [Google Scholar] [CrossRef]
- Lai, A.C.K.; Poon, C.K.M.; Cheung, A.C.T. Effectiveness of facemasks to reduce exposure hazards for airborne infections among general populations. J. R. Soc. Interface 2012, 9, 938–948. [Google Scholar] [CrossRef]
- Johnson, D.F.; Druce, J.D.; Birch, C.; Grayson, M.L. A quantitative assessment of the efficacy of surgical and N95 masks to filter influenza virus in patients with acute influenza infection. Clin. Infect. Dis. 2009, 49, 275–277. [Google Scholar] [CrossRef]
- Bischoff, W.E.; Reid, T.; Russell, G.B.; Peters, T.R. Transocular entry of seasonal influenza-attenuated virus aerosols and the efficacy of N95 respirators, surgical masks, and eye protection in humans. J. Infect. Dis. 2011, 204, 193–199. [Google Scholar] [CrossRef]
- Bin-Reza, F.; Chavarrias, V.L.; Nicoll, A.; Chamberland, M.E. The use of masks and respirators to prevent transmission of influenza: A systematic review of the scientific evidence. Influ. Other Respir. Viruses 2012, 6, 257–267. [Google Scholar] [CrossRef]
- Smith, J.D.; MacDougall, C.C.; Johnstone, J.; Copes, R.A.; Schwartz, B.; Garber, G.E. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: A systematic review and meta-analysis. Can. Med. Assoc. J. 2016, 188, 567–574. [Google Scholar] [CrossRef]
- Offeddu, V.; Yung, C.F.; Low, M.S.F.; Tam, C.C. Effectiveness of Masks and Respirators Against Respiratory Infections in Healthcare Workers: A Systematic Review and Meta-Analysis. Clin. Infect. Dis. 2017, 65, 1934–1942. [Google Scholar] [CrossRef]
- Pryor, F.; Messmer, P.R. The Effect of Traffic Patterns in the OR on Surgical Site Infections. AORN J. 1998, 68, 649–660. [Google Scholar] [CrossRef]
- Andersson, A.E.; Bergh, I.; Karlsson, J.; Eriksson, B.I.; Nilsson, K. Traffic flow in the operating room: An explorative and descriptive study on air quality during orthopedic trauma implant surgery. Am. J. Infect. Control 2012, 40, 750–755. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.B.; Raphael, I.J.; Maltenfort, M.G.; Honsawek, S.; Dolan, K.; Younkins, E.A. The effect of laminar air flow and door openings on operating room contamination. J. Arthroplast. 2013, 28, 1482–1485. [Google Scholar] [CrossRef] [PubMed]
- Taaffe, K.; Lee, B.; Ferrand, Y.; Fredendall, L.; San, D.; Salgado, C.; Shvorin, D.; Khoshkenar, A.; Reeves, S.; the Realizing Improved Patient Care through Human-Centered Design in the Operating Room (RIPCHDOR) Study Group. The Influence of Traffic, Area Location, and Other Factors on Operating Room Microbial Load. Infect. Control Hosp. Epidemiol. 2018, 39, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Anderson, D.J.; Kaye, K.S.; Classen, D.; Arias, K.M.; Podgorny, K.; Burstin, H.; Calfee, D.P.; Coffin, S.E.; Dubberke, E.R.; Fraser, V.; et al. Strategies to Prevent Surgical Site Infections in Acute Care Hospitals. Infect. Control. Hosp. Epidemiol. 2008, 29, S51–S61. [Google Scholar] [CrossRef]
- Sun, C.; Zhai, Z. The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustain. Cities Soc. 2020, 62, 102390. [Google Scholar] [CrossRef]
- Hall, C.B.; Douglas, R.G., Jr. Modes of transmission of respiratory syncytial virus. J. Pediatr. 1981, 99, 100–103. [Google Scholar] [CrossRef]
- Kelso, J.K.; Milne, G.J.; Kelly, H. Simulation suggests that rapid activation of social distancing can arrest epidemic development due to a novel strain of influenza. BMC Public Health 2009, 9, 117. [Google Scholar] [CrossRef]
- Halder, N.; Kelso, J.K.; Milne, G.J. Analysis of the effectiveness of interventions used during the 2009 A/H1N1 influenza pandemic. BMC Public Health 2010, 10, 168. [Google Scholar] [CrossRef]
- Ahmed, F.; Zviedrite, N.; Uzicanin, A. Effectiveness of workplace social distancing measures in reducing influenza transmission: A systematic review. BMC Public Health 2018, 18, 518. [Google Scholar] [CrossRef]
- Naskar, I.; Pal, A.K. Automatic Indoor Air Quality Control of COVID-19 Patient Facilities Using Type-2 Fuzzy Controller. J. Phys. Conf. Ser. 2021, 1937, 012035. [Google Scholar] [CrossRef]
- Kumar, V.; Kumar, S.; Kansal, H. Fuzzy logic controller based operating room air condition control system. Int. J. Innov. Res. Electr. Electron. Instrum. Control Eng. 2014, 2, 510–514. [Google Scholar]
- Pradityo, F.; Surantha, N. Indoor Air Quality Monitoring and Controlling System based on IoT and Fuzzy Logic. In Proceedings of the 2019 7th International Conference on Information and Communication Technology (ICoICT), Kuala Lumpur, Malaysia, 24–26 July 2019; IEEE: New York, NY, USA, 2019; pp. 1–6. [Google Scholar] [CrossRef]
- Li, W.; Koo, C.; Cha, S.H.; Hong, T.; Oh, J. A novel real-time method for HVAC system operation to improve indoor environmental quality in meeting rooms. Build. Environ. 2018, 144, 365–385. [Google Scholar] [CrossRef]
- Ahamed, N.U.; Bin Taha, Z.; Khairuddin, I.B.M.; Rabbi, M.F.; Rahaman, S.A.M.M.; Sundaraj, K. Fuzzy logic controller design for intelligent air-conditioning system. In Proceedings of the 2016 2nd International Conference on Control Science and Systems Engineering (ICCSSE), Singapore, 27–29 July 2016; IEEE: New York, NY, USA, 2016; pp. 232–236. [Google Scholar] [CrossRef]
- Yu, T.-C.; Lin, C.-C. An Intelligent Wireless Sensing and Control System to Improve Indoor Air Quality: Monitoring, Prediction, and Preaction. Int. J. Distrib. Sens. Netw. 2015, 11, 140978. [Google Scholar] [CrossRef]
- Chow, T.; Yang, X. Ventilation performance in operating theatres against airborne infection: Review of research activities and practical guidance. J. Hosp. Infect. 2004, 56, 85–92. [Google Scholar] [CrossRef]
- Romano, F.; Marocco, L.; Gustén, J.; Joppolo, C.M. Numerical and experimental analysis of airborne particles control in an operating theater. Build. Environ. 2015, 89, 369–379. [Google Scholar] [CrossRef]
- Haque, S.E.; Rahman, M. Association between temperature, humidity, and COVID-19 outbreaks in Bangladesh. Environ. Sci. Policy 2020, 114, 253–255. [Google Scholar] [CrossRef]
- Chan, K.H.; Peiris, J.S.M.; Lam, S.Y.; Poon, L.L.M.; Yuen, K.-Y.; Seto, W.H. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv. Virol. 2011, 2011, 734690. [Google Scholar] [CrossRef]
- Songer, J.R. Influence of Relative Humidity on the Survival of Some Airborne Viruses. Appl. Microbiol. 1967, 15, 35–42. [Google Scholar] [CrossRef]
- Casanova, L.M.; Jeon, S.; Rutala, W.A.; Weber, D.J.; Sobsey, M.D. Effects of Air Temperature and Relative Humidity on Coronavirus Survival on Surfaces. Appl. Environ. Microbiol. 2010, 76, 2712–2717. [Google Scholar] [CrossRef] [PubMed]
- Pica, N.; Bouvier, N.M. Environmental factors affecting the transmission of respiratory viruses. Curr. Opin. Virol. 2012, 2, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Crijns, F.; Keinänen-Toivola, M.; Dunne, C. Antimicrobial coating innovations to prevent healthcare-associated infection. J. Hosp. Infect. 2017, 95, 243–244. [Google Scholar] [CrossRef] [PubMed]
- Rock, C.; Small, B.A.; Thom, K.A.; CDC Prevention Epicenters Program. Innovative Methods of Hospital Disinfection in Prevention of Healthcare-Associated Infections. Curr. Treat. Options Infect. Dis. 2018, 10, 65–77. [Google Scholar] [CrossRef]
- Fleming, M.; Patrick, A.; Gryskevicz, M.; Masroor, N.; Hassmer, L.; Shimp, K.; Cooper, K.; Doll, M.; Stevens, M.; Bearman, G. Deployment of a touchless ultraviolet light robot for terminal room disinfection: The importance of audit and feedback. Am. J. Infect. Control 2018, 46, 241–243. [Google Scholar] [CrossRef]
- Doll, M.; Morgan, D.J.; Anderson, D.; Bearman, G. Touchless Technologies for Decontamination in the Hospital: A Review of Hydrogen Peroxide and UV Devices. Curr. Infect. Dis. Rep. 2015, 17, 44. [Google Scholar] [CrossRef]
- Weber, D.J.; Kanamori, H.; Rutala, W.A. ‘No touch’ technologies for environmental decontamination. Opin. Infect. Dis. 2016, 29, 424–431. [Google Scholar] [CrossRef]
- Arundel, A.V.; Sterling, E.M.; Biggin, J.H.; Sterling, T.D. Indirect health effects of relative humidity in indoor environments. Environ. Health Perspect. 1986, 65, 351–361. [Google Scholar] [CrossRef]
- Nerandzic, M.M.; Thota, P.; Sankar, T.; Jencson, A.; Cadnum, J.L.; Ray, A.J.; Salata, R.A.; Watkins, R.R.; Donskey, C.J. Evaluation of a pulsed xenon ultraviolet disinfection system for reduction of healthcare-associated pathogens in hospital rooms. Infect. Control Hosp. Epidemiol. 2015, 36, 192–197. [Google Scholar] [CrossRef]
- Nerandzic, M.M.; Cadnum, J.L.; Pultz, M.J.; Donskey, C.J. Evaluation of an automated ultraviolet radiation device for decontamination of Clostridium difficile and other healthcare-associated pathogens in hospital rooms. BMC Infect. Dis. 2010, 10, 197. [Google Scholar] [CrossRef]
- Boyce, J.M.; Havill, N.L.; Moore, B.A. Terminal Decontamination of Patient Rooms Using an Automated Mobile UV Light Unit. Infect. Control Hosp. Epidemiol. 2011, 32, 737–742. [Google Scholar] [CrossRef] [PubMed]
- Mahida, N.; Vaughan, N.; Boswell, T. First UK evaluation of an automated ultraviolet-C room decontamination device (Tru-D™). J. Hosp. Infect. 2013, 84, 332–335. [Google Scholar] [CrossRef] [PubMed]
- Anderson, D.J.; Gergen, M.F.; Smathers, E.; Sexton, D.J.; Chen, L.F.; Weber, D.J.; Rutala, W.A. Decontamination of Targeted Pathogens from Patient Rooms Using an Automated Ultraviolet-C-Emitting Device. Infect. Control Hosp. Epidemiol. 2013, 34, 466–471. [Google Scholar] [CrossRef]
- Eames, I.; Shoaib, D.; Klettner, C.A.; Taban, V. Movement of airborne contaminants in a hospital isolation room. J. R. Soc. Interface 2009, 6, S757–S766. [Google Scholar] [CrossRef] [PubMed]
- Tung, Y.-C.; Shih, Y.-C.; Hu, S.-C. Numerical study on the dispersion of airborne contaminants from an isolation room in the case of door opening. Appl. Therm. Eng. 2009, 29, 1544–1551. [Google Scholar] [CrossRef]
- Rosero-Montalvo, P.D.; Caraguay-Procel, J.A.; Jaramillo, E.D.; Michilena-Calderon, J.M.; Umaquinga-Criollo, A.C.; Mediavilla-Valverde, M.; Ruiz, M.A.; Beltran, L.A.; Peluffo, D.H. Air Quality Monitoring Intelligent System Using Machine Learning Techniques. In Proceedings of the 3rd International Conference on Information, Systems and Computer Science (INCISCOS 2018), Quito, Ecuador, 14–16 November 2018; IEEE: New York, NY, USA, 2018; pp. 75–80. [Google Scholar] [CrossRef]
- Taştan, M.; Gökozan, H. Real-Time Monitoring of Indoor Air Quality with Internet of Things-Based E-Nose. Appl. Sci. 2019, 9, 3435. [Google Scholar] [CrossRef]
- Salamone, F.; Belussi, L.; Currò, C.; Danza, L.; Ghellere, M.; Guazzi, G.; Lenzi, B.; Megale, V.; Meroni, I. Integrated Method for Personal Thermal Comfort Assessment and Optimization through Users’ Feedback, IoT and Machine Learning: A Case Study. Sensors 2018, 18, 1602. [Google Scholar] [CrossRef]
- Iqbal, U.; Dar, M.A.; Bukhari, S.N. Intelligent Hospitals based on IOT. In Proceedings of the 2018 Fourth International Conference on Advances in Electrical, Electronics, Information, Communication and Bio-Informatics (AEEICB), Chennai, India, 27–28 February 2018; IEEE: New York, NY, USA, 2018; pp. 1–3. [Google Scholar] [CrossRef]
| Key Ventilation Terms | Space Terms | Miscellaneous |
|---|---|---|
| Ventilation (systems) | Healthcare | Disease |
| Ventilation rate | Hospitals | Air quality |
| Air change rate | Operating room | COVID-19 |
| Airflow | Isolation room |
| Original Data (YES) | Original Data (NO) |
|---|---|
| Q1—Observational | Q5—Systematic review |
| Q2—Hybrid | Q6—Selective Literature review |
| Q3—Experimental | Q7—Opinion |
| Q4—Simulation/Numerical |
| Study | No. of Samples | Virus Detected | Location | Key Notes |
|---|---|---|---|---|
| [19] | 10 | ❌ No | Hospital rooms (2–5 m from beds) | All samples negative; precautions still advised |
| [20] | 14 | ✅ Yes (2 positive) | ICU and general ward (1.5 m height, ≥2 m from beds) | 2 samples positive; airborne transmission possible |
| [21] | 31 | ❌ No | ER, ICU, CT-Scan, Laundry | All samples negative; attributed to negative pressure ventilation |
| [22] | 33 | ❌ No | 8 hospital locations | No virus found; airborne spread unlikely in negative pressure rooms |
| [23] | Not specified | ✅ Yes | COVID-19 patient rooms and adjacent corridors | High RNA levels detected, esp. in poorly ventilated corridors (2600–4000 c/m3) |
| Study | No. of Samples | Virus Detected | Location | Key Notes |
|---|---|---|---|---|
| [25] | 107 surface, 46 air, 2 exhaled condensate, 2 expired air | ✅ Yes (mainly surfaces) | Four three-bed isolation rooms (patient rooms, toilets, corridors, anterooms) | Toilet was the most contaminated; virus detected on surfaces, not emphasized in air |
| [26] | 130 surface, 28 air | ✅ Yes (nursing station & isolation ward air) | Isolation ward, nursing station, pre-check triages, fever clinic | Positive in isolation ward air and nursing station; negative in high-airflow/open areas (triage, fever clinic) |
| [27] | Air samples before & after ventilation change (ACH 5.9 h−1) | ✅ Yes (before the increase in fresh air); ❌ No (after 100% OA) | Hospital rooms & isolated care units | Viable virus up to 4 m from patients before the increase in fresh air; none detected after switching to 100% outdoor air; vent swabs all negative |
| [28] | Various surfaces; 12 air samples | ✅ Yes (1 air sample) | Ship hospital, nursing home, 3 hospital wards, long-term care facility | Only 1 air sample positive (2.5 m from patient without mask); multiple surface samples tested |
| [29] | 5 air, 37 surface | ✅ Yes (24.3% surfaces); ❌ No (air) | COVID isolation ward, ICU, undressing room, clean areas | High surface contamination (dispensers, equipment, bed rails, handles); no positives in clean areas; air samples all negative |
| Recommendation | Post-COVID-19 Paper | Before-COVID-19 Paper |
|---|---|---|
| R1. Recommends optimal inlet-outlet optimization | [30,31,32,33,34,35,36,37,38,40,41,42,66] | [67,68,69,70,71] |
| R2. Hospitals to provide PPE | [19,20,23,25,26,28,43] | [72,73,74,75,76] |
| R3. Adhere to national and international guidelines | [19,21,22,33,43,77,78] | [79,80,81,82] |
| R4. Increase surface cleaning, disinfection, and promote hand hygiene | [25,26,29] | [83,84,85,86,87,88,89] |
| R5. Fresh air in lieu of recirculation | [27,33,39] | [90,91] |
| R6. Space-zoning-optimization | [32,34,38,92] | - |
| R7. Further experiments on airborne transmission of SARS-CoV-2 | [19,20,24] | [93,94,95,96,97] |
| R8. Comprehensive and institutional IAQ and ventilation standards | [77,98] | [99,100] |
| R9. Air filtration can be used as a measure to limit community respiratory infection transmission. (Use HEPA filters), (Increasing air filtration (using MERV-8 or higher filters)) | [39,77,101] | [102,103,104,105,106] |
| R10. Implementing physical barriers (to minimize the spread of respiratory infections) | [29,30] | [107,108,109] |
| R11. Recommends sliding (automated) doors | [31,110] | [111,112,113] |
| R12. Mandating the wide use of monitors displaying the state of IAQ (Real-time monitoring of particulates and CO2) | [46,77] | [114,115,116,117,118] |
| R13. The potential of ultraviolet germicidal irradiation as a method for air disinfection (UV air cleaner can reduce exposure to SARS-CoV-2) | [38,77] | [119,120,121,122,123] |
| R14. Warrant the role of ventilation in airborne transmission (Improving ventilation reduces respiratory infection transmission) | [77,124] | [70,125,126,127,128] |
| R15. Increasing airflow rate (the rate of air change) | [33,101] | [129,130,131] |
| R16. Separate personnel for the observation and isolation ward areas, strictly prohibiting movement between the areas, and exclusive use of objects within each area. | [26] | [132] |
| R17. Further research on airborne natural ventilation | [42] | [90,133,134,135,136,137] |
| R18. PPE when exposed to sewage | [28] | [138,139] |
| R19. Recognizing the continuous global hazard of airborne respiratory infection to control the risk | [77] | [140,141,142,143,144] |
| R20. Masks may be effective in preventing the spread of the virus due to reduced air velocity | [124] | [145,146,147,148,149,150] |
| R21. Limiting traffic in surgical suite reduces airborne particles in hallway | [110] | [151,152,153,154,155] |
| R22. Recommends social distancing | [156] | [157,158,159,160] |
| R23. T2FLC is better than PID and T1FLC at maintaining indoor air quality | [161] | [162,163,164,165,166] |
| R24. ORs pose lower exposure risk | [45] | [167,168] |
| R25. Higher temperature and RH | [169] | [170,171,172,173] |
| R26. Direct monitoring of SARS-CoV-2 to prevent unexpected viral exposures | [23] | - |
| R27. Continuous evaluation of ventilation systems of all units | [23] | - |
| R28. Recommend stronger hospital discharge standards using breath samples | [98] | - |
| R29. Sun screening the building or applying insulation on external or internal surfaces | [34] | - |
| R30. Shorter exposures at lower ACH may be preferential relative to higher ACH | [39] | - |
| R31. suggests using Total Maximum Time (TMT) and Overall Particle Concentration (OPC) to evaluate air distribution proposals | [36] | - |
| Recommendation | Post-COVID-19 Paper | Before-COVID-19 Paper |
|---|---|---|
| R1. Use of no-touch techniques and innovative finishing materials | [61,64,65] | [174,175,176,177,178] |
| R2. Use of evaporative humidifiers | [60] | [179] |
| R3. Automated room disinfection with ultraviolet light for one hour | [49] | [180,181,182,183,184] |
| R4. Keep hallway doors closed | [55] | [112,113,185,186] |
| R5. The use of advanced technologies such as IoT and ML for enhanced real-time monitoring and management of IAQ | [63] | [187,188,189,190] |
| R6. Install supplemental exhaust ventilation | [55] | - |
| Theme | Key Recommendations | Purpose/Implication |
|---|---|---|
| Impact on knowledge |
| Build resilient healthcare environments that optimize infection control while being environmentally friendly. |
| Unsubstantiated Recommendations |
| Ensure that new recommendations are based on solid evidence, rigorously evaluated, and transparently communicated. |
| Reliance on experience |
| Improve readiness for future crises by combining existing best practices with adaptable, evidence-based, globally coordinated strategies. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nikoopayan Tak, M.S.; Mousavi, E. Ventilation and Infection Control in Healthcare Facilities: A Post-COVID-19 Literature Synthesis. Air 2025, 3, 30. https://doi.org/10.3390/air3040030
Nikoopayan Tak MS, Mousavi E. Ventilation and Infection Control in Healthcare Facilities: A Post-COVID-19 Literature Synthesis. Air. 2025; 3(4):30. https://doi.org/10.3390/air3040030
Chicago/Turabian StyleNikoopayan Tak, Mohammad Saleh, and Ehsan Mousavi. 2025. "Ventilation and Infection Control in Healthcare Facilities: A Post-COVID-19 Literature Synthesis" Air 3, no. 4: 30. https://doi.org/10.3390/air3040030
APA StyleNikoopayan Tak, M. S., & Mousavi, E. (2025). Ventilation and Infection Control in Healthcare Facilities: A Post-COVID-19 Literature Synthesis. Air, 3(4), 30. https://doi.org/10.3390/air3040030






