Air Pollution Effects on Mental Health Relationships: Scoping Review on Historically Used Methodologies to Analyze Adult Populations
Abstract
1. Introduction
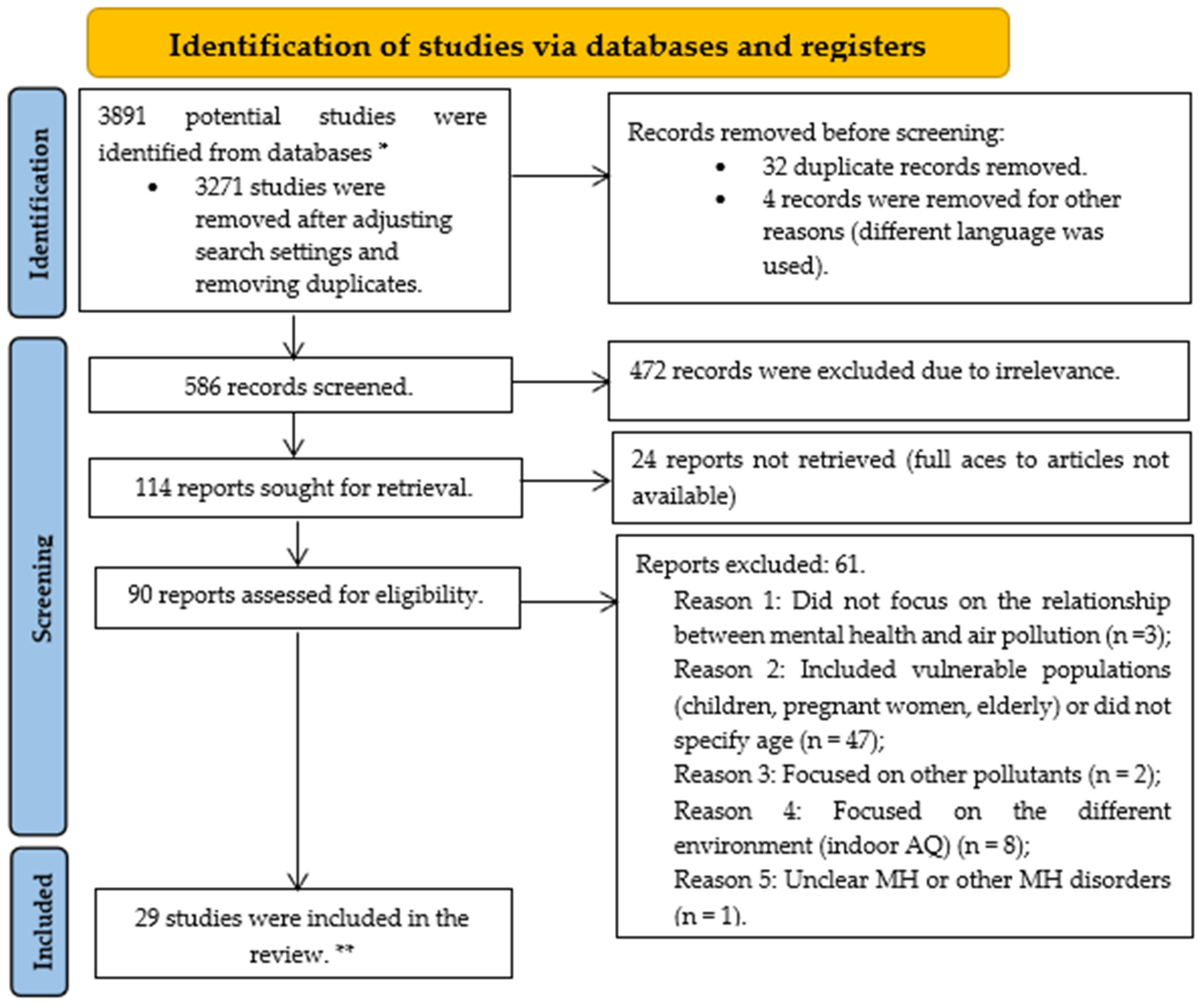
2. Methods
2.1. Research Strategy
2.2. Search Criteria
2.3. Inclusion and Exclusion Criteria
2.4. Screening Criteria and Quality
- Descriptive summary of the publication (including the authors’ names, year of publication, publication name, country of origin, publication type, publication design, types of setting (urban, suburban, or rural), participants of interest (e.g., adults, young adults, elderly, children, etc.), study aim)
- Content analysis (methodologies used for mental health and air pollution, as well as how the two subjects were linked)
- Results analysis (was the link between air quality/pollution and mental health achieved when experimentation was used)
- Decision (whether the article is deemed suitable or not for the review)
2.5. Data Analysis
3. Results
3.1. Regions of Studies
3.2. Types of Methodologies Used
3.2.1. Mental Health
3.2.2. Air Quality
3.2.3. Statistical Methods
3.3. Study Types and Design
4. Discussion
4.1. Principal Findings
4.2. Method Suitability
4.2.1. Air Quality Methods
AQ Monitors and Databases—Stationary and Portable
Land Use Models
4.2.2. Mental Health Methods
Qualitative and Quantitative Methods
Surveying
Face-to-Face Sampling/Assessment
Medical/Healthcare Data
4.3. Statistical Methods
5. Limitations and Recommendations
- (1)
- Most studies included in this review are cross-sectional, limiting the ability to draw causal inferences. Cross-sectional designs capture a snapshot in time and cannot establish temporality, making it difficult to determine whether air pollution exposure precedes the onset of mental health symptoms [49,50]. Meanwhile, some studies employed longitudinal designs [47,48], which are excellent in tracking changes in mental health over time but may also face significant challenges such as systematic biases, high costs, measurement consistency, data management, changing contexts, participant burden, complex analysis, and ethical considerations limiting the feasibility of the literature [210,211,212,213]. Instead, prospective cohort studies may be more helpful in establishing causality and understanding the long-term impacts of air pollution on mental health due to their focus on identifying risk factors for disease or health outcomes by following a healthy cohort over time and assessing effects for the future. It is also important to note the abundance of quantitative methods assessed in the scoping review and the lack of qualitative methods used in the selected studies. None of the studies included qualitative methods, which could provide deeper insights into the subjective experiences of individuals affected by air pollution. Qualitative data could help portray the mechanisms through which air pollution impacts mental health and provide a more holistic understanding of these relationships through individual cohort perspectives.
- (2)
- The obtained literature is biased geographically. Most studies were conducted in Asia and Europe, lacking representation from other continents and countries. This leaves significant gaps in knowledge regarding the impact of air pollution on mental health in different regions, such as Africa and South America, where no studies were identified in the scoping review. There could be various reasons for a lack of similar research, including focusing on physical health outcomes, such as respiratory and cardiovascular diseases, rather than mental health [21,73,214,215]. Funding may prioritize other public health issues perceived as more immediate or severe, leading to fewer research resources linking air quality and mental health. For example, African countries combat health risks such as HIV/AIDS, malaria, and tuberculosis while lacking a public budget or immediate concern and dedication to mitigate air pollution and focus on mental health research [216]. Furthermore, awareness of the potential links between air quality and mental health is relatively recent compared to more established areas of environmental health research. As a result, the body of research is still growing, and fewer reviews might have been conducted to synthesize existing studies. Additionally, collecting reliable air quality and mental health data can be challenging due to limited access to high-quality, long-term air pollution data and comprehensive mental health records, especially in developing countries. In some parts of South America and Africa, limited research infrastructure and resources can impede conducting extensive research [217,218,219,220,221]. There might be a lack of local expertise or interest in the intersection of air quality and mental health. Mental health research, in general, might be underprioritized due to cultural stigmas or SES challenges in certain regions [222]. Addressing these challenges requires targeted efforts to enhance research infrastructure, foster interdisciplinary collaboration, increase funding for mental health research in environmental health contexts, and raise awareness about the importance of studying the links between air quality and mental health.
- (3)
- Many studies relied on self-reported measures for assessing mental health outcomes, such as the CES-D and PHQ-9 scales. Although these are validated tools, they are subject to reporting biases due to predetermined closed-end questions, which can affect the accuracy and reliability of the data. A mixed-method approach, such as quantitative and qualitative methods in the study design, could enhance the accuracy and reliability of mental health evaluations.
- (4)
- This study primarily focused on the link between PM and MH, while other pollutants such as O3, volatile organic compounds (VOCs), SO2, CO, and NO2 have not been addressed. These pollutants warrant consideration in future research as their potential neurotoxic effects could contribute to a broader understanding of how various air pollutants impact the nervous system and, consequently, MH. For example, O3 exposure has been linked to activated stress responses [92], psychiatric emergency services admissions, depression, and other MH disorders [223,224,225], including the use of antidepressants [226]. VOCs are neurotoxic and can damage the central nervous system and affect sleep [227]. However, the association between VOCs and certain MH disorders, such as depression, remains unclear and requires more research [228,229]. Augmented risk of MH when exposed to SO2, CO, and NO2, especially depression and stress, has been observed in numerous studies [65,92,230,231,232,233]. While CO is predominantly associated with suicide [234,235] and has been previously used in several countries as a suicide method [236,237,238], it is also associated with cognitive impairments [239,240]. NO2 and NOX produce the most apparent association with adverse MH, such as anxiety [241], schizophrenia [242,243], depression [28,242,244], and various neurodevelopment disorders [245,246,247,248] in urban areas [249]. NO2 and NOX are commonly associated with motor vehicle exhausts [250]. Future research should aim to fill these gaps and consider the combined effects of multiple pollutants to provide a more comprehensive understanding of how air quality influences mental health.
- (5)
- Several studies did not adequately control for potential confounders, such as meteorological, SES, lifestyle factors, and pre-existing health conditions, which could influence the observed associations between air pollution and mental health [45,46]. It is well acknowledged that meteorological conditions affect PM concentration in the atmosphere [251,252,253,254,255,256,257]. Lower SES populations, including minorities [258], often reside in areas lacking green spaces and higher pollution levels due to proximity to industrial zones, heavy traffic, and other pollution sources, work in jobs involving harmful exposures, and are more exposed to extreme weather events [259]. Future studies should better incorporate comprehensive adjustments for these variables to isolate the effects of air pollution on mental health.
- (6)
- The variability in air pollution measurement methods in the selected studies may present a challenge. While some studies used fixed monitoring stations or LUR models, others solely relied on portable sensors or governmental databases, leading to potential inconsistencies in exposure assessment. Standardizing or using a mixed-method approach (e.g., LUR model with databases or portable monitors) to compare results and air quality measurement approaches across studies could improve the findings.
- (7)
- Due to the strict inclusion criteria, many studies, including those of vulnerable populations such as children and the elderly (>69), were excluded from the scoping review. While the review identified the gap in research on assessing air quality effects on mental health in working-age urban adult populations, vulnerable populations might experience different or more severe implications of air pollution on mental health due to heightened sensitivities. Including vulnerable groups, including those with pre-existing mental health conditions, in future research is crucial as it could provide a more detailed understanding of the health impacts of air pollution [11]. This could have been why little to no research was discovered on other continents, such as South America and Africa—the lack of South American and African studies represents a significant research gap. These regions face unique environmental challenges and socio-economic conditions that could influence the relationship between air pollution and mental health differently, especially in South America and Africa, compared to more industrialized areas [74]. In many South American and African countries, limited funding, lack of infrastructure for air quality monitoring, and insufficient public health research capacities hinder comprehensive studies on environmental health [51]. Furthermore, political and economic challenges often divert attention and resources from environmental health issues, exacerbating the research gap [74]. Addressing this gap is essential for comprehensively understanding global health impacts and informing policies in these underrepresented regions.
- (8)
- Exploring the interactive effects of multiple pollutants and other environmental stressors (e.g., noise pollution, green space) on mental health could provide more understanding of these complex relationships [45]. Green spaces are widely viewed as a health-promoting characteristic of residential environments, which could be useful to include in studies to broaden the understanding of how mental health could be improved when exposed to air pollution [260]. Advanced statistical techniques, such as structural equation modeling and machine learning, could be employed to unravel these multifaceted interactions [56].
- (9)
- To widen the literature search, it is advisable to complement multiple databases, such as Medline, Web of Science, Google Scholar, or discipline-specific databases. Utilizing multiple databases can help broaden your search scope, ensure comprehensive coverage, and minimize potential biases or omissions in the literature.
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Ambient (Outdoor) Air Pollution. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (accessed on 10 July 2024).
- American Lung Association. Health Impact of Pollution|State of the Air. 2024. Health Impact of Pollution | State of the Air. 2024. Available online: https://www.lung.org/research/sota/health-risks (accessed on 26 July 2024).
- European Environment Association (EEA). How Air Pollution Affects Our Health. 2023. Available online: https://www.eea.europa.eu/en/topics/in-depth/air-pollution/eow-it-affects-our-health (accessed on 26 July 2024).
- United States Environmental Protection Agency (US EPA). Research on Health Effects from Air Pollution. 2020. Available online: https://www.epa.gov/air-research/research-health-effects-air-pollution (accessed on 26 July 2024).
- Pykett, J.; Campbell, N.; Fenton, S.-J.; Gagen, E.; Lavis, A.; Newbigging, K.; Parkin, V.; Williams, J. Urban precarity and youth mental health: An interpretive scoping review of emerging approaches. Soc. Sci. Med. 2023, 320, 115619. [Google Scholar] [CrossRef] [PubMed]
- Neufeld, S.A.S. The burden of young people’s mental health conditions in Europe: No cause for complacency. Lancet Reg. Health-Eur. 2022, 16, 100364. [Google Scholar] [CrossRef] [PubMed]
- Appleton, R.; Barnett, P.; Chipp, B.; Clark, M.; Goldblatt, P.; Jeffreys, S.; Machin, K.; Needle, J.J.; Shah, P.; Thompson, G.; et al. Development of a conceptual framework to guide description and evaluation of social interventions for people with serious mental health conditions. SSM-Ment. Health 2023, 4, 100271. [Google Scholar] [CrossRef]
- Chen, F.; Zhang, X.; Chen, Z. Air pollution and mental health: Evidence from China Health and Nutrition Survey. J. Asian Econ. 2023, 86, 101611. [Google Scholar] [CrossRef]
- Schraufnagel, D.E. The health effects of ultrafine particles. Exp. Mol. Med. 2020, 52, 311–317. [Google Scholar] [CrossRef]
- Hamanaka, R.B.; Mutlu, G.M. Particulate Matter Air Pollution: Effects on the Cardiovascular System. Front Endocrinol. 2018, 9. Available online: https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2018.00680/full (accessed on 28 July 2024). [CrossRef] [PubMed]
- Block, M.L.; Calderón-Garcidueñas, L. Air pollution: Mechanisms of neuroinflammation and CNS disease. Trends Neurosci. 2009, 32, 506–516. [Google Scholar] [CrossRef]
- Pun, V.C.; Manjourides, J.; Suh, H. Association of Ambient Air Pollution with Depressive and Anxiety Symptoms in Older Adults: Results from the NSHAP Study. Environ. Health Perspect. 2017, 125, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Perera, F.P.; Wang, S.; Rauh, V.; Zhou, H.; Stigter, L.; Camann, D.; Jedrychowski, W.; Mroz, E.; Majewska, R. Prenatal Exposure to Air Pollution, Maternal Psychological Distress, and Child Behavior. Pediatrics 2013, 132, e1284–e1294. [Google Scholar] [CrossRef]
- Fonken, L.K.; Xu, X.; Weil, Z.M.; Chen, G.; Sun, Q.; Rajagopalan, S.; Nelson, R.J. Air pollution impairs cognition, provokes depressive-like behaviors and alters hippocampal cytokine expression and morphology. Mol. Psychiatry 2011, 16, 987–995. [Google Scholar] [CrossRef]
- Tran, N.Q.V.; Miyake, K. Neurodevelopmental Disorders and Environmental Toxicants: Epigenetics as an Underlying Mechanism. Int. J. Genom. 2017, 2017, 7526592. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, D.P.; Puig, K.L.; Gorr, M.W.; Wold, L.E.; Combs, C.K. A Pilot Study to Assess Effects of Long-Term Inhalation of Airborne Particulate Matter on Early Alzheimer-Like Changes in the Mouse Brain. PLoS ONE 2015, 10, e0127102. [Google Scholar] [CrossRef]
- Kyi-Tha-Thu, C.; Fujitani, Y.; Hirano, S.; Win-Shwe, T.-T. Early-Life Exposure to Traffic-Related Air Pollutants Induced Anxiety-like Behaviors in Rats via Neurotransmitters and Neurotrophic Factors. Int. J. Mol. Sci. 2022, 24, 586. [Google Scholar] [CrossRef]
- Zundel, C.G.; Ryan, P.; Brokamp, C.; Heeter, A.; Huang, Y.; Strawn, J.R.; Marusak, H.A. Air Pollution, Depressive and Anxiety Disorders, and Brain Effects: A Systematic Review. Neurotoxicology 2022, 93, 272–300. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Lu, C. Air Quality, Pollution Perception, and Residents’ Health: Evidence from China. Toxics 2023, 11, 591. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.-H.; Mao, Y.-C.; Li, Y.; Zhang, S.; Hu, H.-Y.; Liu, Z.-Y.; Liu, X.-J.; Zhao, J.-W.; Huang, K.; Chen, M.-L.; et al. Joint effects of prenatal exposure to air pollution and pregnancy-related anxiety on birth weight: A prospective birth cohort study in Ma’anshan, China. Environ. Res. 2023, 238, 117161. [Google Scholar] [CrossRef] [PubMed]
- Kanner, J.; Pollack, A.Z.; Ranasinghe, S.; Stevens, D.R.; Nobles, C.; Rohn, M.C.H.; Sherman, S.; Mendola, P. Chronic exposure to air pollution and risk of mental health disorders complicating pregnancy. Environ. Res. 2021, 196, 110937. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Huang, L.; Han, B.; Van Der Kuijp, T.J.; Xia, Y.; Chen, K. Exposure and perception of PM2.5 pollution on the mental stress of pregnant women. Environ. Int. 2021, 156, 106686. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.M.; Mishra, G.D.; Moss, K.M.; Yang, I.A.; Lycett, K.; Knibbs, L.D. Maternal and Childhood Ambient Air Pollution Exposure and Mental Health Symptoms and Psychomotor Development in Children: An Australian Population-Based Longitudinal Study. Environ. Int. 2022, 158, 107003. [Google Scholar] [CrossRef]
- Iglesias-Vázquez, L.; Binter, A.-C.; Canals, J.; Hernández-Martínez, C.; Voltas, N.; Ambròs, A.; Fernández-Barrés, S.; Pérez-Crespo, L.; Guxens, M.; Arija, V. Maternal exposure to air pollution during pregnancy and child’s cognitive, language, and motor function: ECLIPSES study. Environ. Res. 2022, 212, 113501. [Google Scholar] [CrossRef]
- Zou, M.-L.; Jiang, C.-B.; Chen, Y.-H.; Wu, C.-D.; Candice Lung, S.-C.; Chien, L.-C.; Kallawicha, K.; Yang, Y.-T.; Lo, Y.-C.; Chao, H.J. Effects of air pollution, land-use type, and maternal mental health on child development in the first two years of life in the Greater Taipei area. Environ. Res. 2021, 197, 111168. [Google Scholar] [CrossRef] [PubMed]
- Reuben, A.; Arseneault, L.; Beddows, A.; Beevers, S.D.; Moffitt, T.E.; Ambler, A.; Latham, R.M.; Newbury, J.B.; Odgers, C.L.; Schaefer, J.D.; et al. Association of Air Pollution Exposure in Childhood and Adolescence with Psychopathology at the Transition to Adulthood. JAMA Netw. Open 2021, 4, e217508. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). More than 90% of the World’s Children Breathe Toxic Air Every Day. 2018. Available online: https://www.who.int/news/item/29-10-2018-more-than-90-of-the-worlds-children-breathe-toxic-air-every-day (accessed on 23 June 2024).
- Roberts, S.; Arseneault, L.; Barratt, B.; Beevers, S.; Danese, A.; Odgers, C.L.; Moffitt, T.E.; Reuben, A.; Kelly, F.J.; Fisher, H.L. Exploration of NO2 and PM2.5 air pollution and mental health problems using high-resolution data in London-based children from a UK longitudinal cohort study. Psychiatry Res. 2019, 272, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Campbell, C.E.; Cotter, D.L.; Bottenhorn, K.L.; Burnor, E.; Ahmadi, H.; Gauderman, W.J.; Cardenas-Iniguez, C.; Hackman, D.; McConnell, R.; Berhane, K.; et al. Air pollution and age-dependent changes in emotional behavior across early adolescence in the U.S. Environ. Res. 2024, 240, 117390. [Google Scholar] [CrossRef] [PubMed]
- Kelly, F.J.; Fussell, J.C. Size, source and chemical composition as determinants of toxicity attributable to ambient particulate matter. Atmos. Environ. 2012, 60, 504–526. [Google Scholar] [CrossRef]
- Yun, G.; Yang, C.; Ge, S. Understanding Anthropogenic PM2.5 Concentrations and Their Drivers in China during 1998–2016. Int. J. Environ. Res. Public Health 2022, 20, 695. [Google Scholar] [CrossRef] [PubMed]
- European Environment Association (EEA). Premature Deaths Due to Air Pollution Continue to Fall in the EU, More Efforts Needed to Deliver a Toxic-Free Environment. 2022. Available online: https://www.eea.europa.eu/en/newsroom/news/premature-deaths-due-air-pollution (accessed on 28 July 2024).
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Baker, E.; Barlow, C.F.; Daniel, L.; Morey, C.; Bentley, R.; Taylor, M.P. Mental health impacts of environmental exposures: A scoping review of evaluative instruments. Sci. Total Environ. 2024, 912, 169063. [Google Scholar] [CrossRef] [PubMed]
- Mazumder, H.; Rimu, F.H.; Shimul, M.H.; Das, J.; Gain, E.P.; Liaw, W.; Hossain, M.M. Maternal health outcomes associated with ambient air pollution: An umbrella review of systematic reviews and meta-analyses. Sci. Total Environ. 2024, 914, 169792. [Google Scholar] [CrossRef]
- Theron, L.C.; Abreu-Villaça, Y.; Augusto-Oliveira, M.; Brennan, C.; Crespo-Lopez, M.E.; de Paula Arrifano, G.; Glazer, L.; Gwata, N.; Lin, L.; Mareschal, I.; et al. A systematic review of the mental health risks and resilience among pollution-exposed adolescents. J. Psychiatr. Res. 2022, 146, 55–66. [Google Scholar] [CrossRef]
- Lu, J.G. Air pollution: A systematic review of its psychological, economic, and social effects. Curr. Opin. Psychol. 2020, 32, 52–65. [Google Scholar] [CrossRef] [PubMed]
- Buoli, M.; Grassi, S.; Caldiroli, A.; Carnevali, G.S.; Mucci, F.; Iodice, S.; Cantone, L.; Pergoli, L.; Bollati, V. Is there a link between air pollution and mental disorders? Environ. Int. 2018, 118, 154–168. [Google Scholar] [CrossRef] [PubMed]
- Embase. 2024. Available online: https://www.embase.com/search/quick?phase=continueToApp (accessed on 10 February 2024).
- PubMed. 2024. Available online: https://pubmed.ncbi.nlm.nih.gov/ (accessed on 10 February 2024).
- Ponsoni, A.; Branco, L.D.; Cotrena, C.; Shansis, F.M.; Grassi-Oliveira, R.; Fonseca, R.P. Self-reported inhibition predicts history of suicide attempts in bipolar disorder and major depression. Compr. Psychiatry 2018, 82, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Chesney, E.; Goodwin, G.M.; Fazel, S. Risks of all-cause and suicide mortality in mental disorders: A meta-review. World Psychiatry 2014, 13, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, H.; Hino, K.; Ito, T.; Abe, T.; Nomoto, M.; Furuno, T.; Takeuchi, I.; Hishimoto, A. Relationship of emergency department visits for suicide attempts with meteorological and air pollution conditions. J. Affect. Disord. 2023, 333, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Mouly, T.A.; Mishra, G.D.; Hystad, P.; Nieuwenhuijsen, M.; Knibbs, L.D. Residential greenspace and anxiety symptoms among Australian women living in major cities: A longitudinal analysis. Environ. Int. 2023, 179, 108110. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Kwan, M.-P.; Tse, L.A.; He, S.Y. How People’s COVID-19 Induced-Worries and Multiple Environmental Exposures Are Associated with Their Depression, Anxiety, and Stress during the Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 6620. [Google Scholar] [CrossRef] [PubMed]
- Kandola, A.; Hayes, J.F. Real-time air pollution and bipolar disorder symptoms: Remote-monitored cross-sectional study. BJPsych Open 2023, 9, e107. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Wang, J.; Huang, J.; Kelly, F.J.; Li, G. Long-term Exposure to Multiple Ambient Air Pollutants and Association with Incident Depression and Anxiety. JAMA Psychiatry 2023, 80, 305–313. [Google Scholar] [CrossRef]
- Roberts, H.; Helbich, M. Multiple environmental exposures along daily mobility paths and depressive symptoms: A smartphone-based tracking study. Environ. Int. 2021, 156, 106635. [Google Scholar] [CrossRef]
- Lan, Y.; Roberts, H.; Kwan, M.-P.; Helbich, M. Daily space-time activities, multiple environmental exposures, and anxiety symptoms: A cross-sectional mobile phone-based sensing study. Sci. Total Environ. 2022, 834, 155276. [Google Scholar] [CrossRef] [PubMed]
- Ji, Y.; Liu, B.; Song, J.; Cheng, J.; Wang, H.; Su, H. Association between traffic-related air pollution and anxiety hospitalizations in a coastal Chinese city: Are there potentially susceptible groups? Environ. Res. 2022, 209, 112832. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Managi, S. Spatial Variability of the Relationship between Air Pollution and Well-being. Sustain. Cities Soc. 2022, 76, 103447. [Google Scholar] [CrossRef]
- Lohmann, P.M.; Gsottbauer, E.; You, J.; Kontoleon, A. Air pollution and anti-social behaviour: Evidence from a randomised lab-in-the-field experiment. Soc. Sci. Med. 2023, 320, 115617. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.; Tian, M.; Yuan, L. Do objective and subjective traffic-related pollution, physical activity and nature exposure affect mental wellbeing? Evidence from Shenzhen, China. Sci. Total Environ. 2023, 869, 161819. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Cai, M.; Qian, Z. (Min); Zhang, S.; Yang, Y.; McMillin, S.E.; Chen, G.; Hua, J.; Tabet, M.; Wang, C.; et al. The effects of long-term exposure to air pollution on incident mental disorders among patients with prediabetes and diabetes: Findings from a large prospective cohort. Sci. Total Environ. 2023, 897, 165235. [Google Scholar] [CrossRef] [PubMed]
- Zu, D.; Zhai, K.; Qiu, Y.; Pei, P.; Zhu, X.; Han, D. The Impacts of Air Pollution on Mental Health: Evidence from the Chinese University Students. Int. J. Environ. Res. Public Health 2020, 17, 6734. [Google Scholar] [CrossRef] [PubMed]
- Tao, Y.; Kou, L.; Chai, Y.; Kwan, M.-P. Associations of co-exposures to air pollution and noise with psychological stress in space and time: A case study in Beijing, China. Environ. Res. 2021, 196, 110399. [Google Scholar] [CrossRef]
- Kim, H.-J.; Kim, H.-S.; Kim, S.; Hwang, J.; Lee, H.; Park, B.; Kim, B. Effects of vitamin D on associations between air pollution and mental health outcomes in Korean adults: Results from the Korea National Health and Nutrition Examination Survey (KNHANES). J. Affect. Disord. 2023, 320, 390–396. [Google Scholar] [CrossRef]
- Kim, H.-J.; Min, J.; Seo, Y.-S.; Min, K. Relationship between chronic exposure to ambient air pollution and mental health in Korean adult cancer survivors and the general population. BMC Cancer 2021, 21, 1298. [Google Scholar] [CrossRef]
- Sakhvidi, M.J.Z.; Lafontaine, A.; Lequy, E.; Berr, C.; de Hoogh, K.; Vienneau, D.; Goldberg, M.; Zins, M.; Lemogne, C.; Jacquemin, B. Ambient air pollution exposure and depressive symptoms: Findings from the French CONSTANCES cohort. Environ. Int. 2022, 170, 107622. [Google Scholar] [CrossRef] [PubMed]
- Hao, G.; Zuo, L.; Xiong, P.; Chen, L.; Liang, X.; Jing, C. Associations of PM2.5 and road traffic noise with mental health: Evidence from UK Biobank. Environ. Res. 2022, 207, 112221. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Xia, Y.; Cao, L.; Chang, Q.; Zhao, Y. Associations between long term exposures to outdoor air pollution and indoor solid fuel use and depression in China. J. Environ. Manag. 2022, 302, 113982. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Ma, W.; Pan, Y.; Guo, W.; Chen, Y. PM2.5 exposure and anxiety in China: Evidence from the prefectures. BMC Public Health 2021, 21, 429. [Google Scholar] [CrossRef] [PubMed]
- Díaz, J.; López-Bueno, J.A.; López-Ossorio, J.J.; Gónzález, J.L.; Sánchez, F.; Linares, C. Short-term effects of traffic noise on suicides and emergency hospital admissions due to anxiety and depression in Madrid (Spain). Sci. Total Environ. 2020, 710, 136315. [Google Scholar] [CrossRef]
- Wang, R.; Xue, D.; Liu, Y.; Liu, P.; Chen, H. The Relationship between Air Pollution and Depression in China: Is Neighbourhood Social Capital Protective? Int. J. Environ. Res. Public Health 2018, 15, 1160. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.; Park, J.Y.; Choi, J. Long-term exposure to ambient air pollutants and mental health status: A nationwide population-based cross-sectional study. PLoS ONE 2018, 13, e0195607. [Google Scholar] [CrossRef]
- Wan, S.; Rojas-Rueda, D.; Pretty, J.; Roscoe, C.; James, P.; Ji, J.S. Greenspace and mortality in the U.K. Biobank: Longitudinal cohort analysis of socio-economic, environmental, and biomarker pathways. SSM-Popul. Health 2022, 19, 101194. [Google Scholar] [CrossRef]
- Rahman, M.M.; Lorenzo, M.; Ban-Weiss, G.; Hasan, Z.; Azzouz, M.; Eckel, S.P.; Conti, D.V.; Lurmann, F.; Schlaerth, H.; Johnston, J.; et al. Ambient temperature and air pollution associations with suicide and homicide mortality in California: A statewide case-crossover study. Sci. Total Environ. 2023, 874, 162462. [Google Scholar] [CrossRef]
- Carroll, M.; Gao, C.X.; Campbell, T.C.H.; Smith, C.L.; Dimitriadis, C.; Berger, E.; Maybery, D.; Ikin, J.; Abramson, M.J.; Sim, M.R.; et al. Impacts of coal mine fire-related PM2.5 on the utilisation of ambulance and hospital services for mental health conditions. Atmos. Pollut. Res. 2022, 13, 101415. [Google Scholar] [CrossRef]
- Zhang, W.; Peng, S.; Fu, J.; Xu, K.; Wang, H.; Jin, Y.; Yang, T.; Cottrell, R.R. Urban Air Pollution and Mental Stress: A Nationwide Study of University Students in China. Front. Public Health 2021, 9, 685431. [Google Scholar] [CrossRef] [PubMed]
- Helbich, M.; Browning, M.H.E.M.; Huss, A. Outdoor light at night, air pollution and depressive symptoms: A cross-sectional study in the Netherlands. Sci. Total Environ. 2020, 744, 140914. [Google Scholar] [CrossRef] [PubMed]
- Generaal, E.; Timmermans, E.J.; Dekkers, J.E.C.; Smit, J.H.; Penninx, B.W.J.H. Not urbanization level but socioeconomic, physical and social neighbourhood characteristics are associated with presence and severity of depressive and anxiety disorders. Psychol. Med. 2019, 49, 149–161. [Google Scholar] [CrossRef] [PubMed]
- Radua, J.; De Prisco, M.; Oliva, V.; Fico, G.; Vieta, E.; Fusar-Poli, P. Impact of air pollution and climate change on mental health outcomes: An umbrella review of global evidence. World Psychiatry 2024, 23, 244–256. [Google Scholar] [CrossRef]
- Bhui, K.; Newbury, J.B.; Latham, R.M.; Ucci, M.; Nasir, Z.A.; Turner, B.; O’Leary, C.; Fisher, H.L.; Marczylo, E.; Douglas, P.; et al. Air quality and mental health: Evidence, challenges and future directions. BJPsych Open 2023, 9, e120. [Google Scholar] [CrossRef] [PubMed]
- Braithwaite, I.; Zhang, S.; Kirkbride, J.B.; Osborn, D.P.J.; Hayes, J.F. Air Pollution (Particulate Matter) Exposure and Associations with Depression, Anxiety, Bipolar, Psychosis and Suicide Risk: A Systematic Review and Meta-Analysis. Environ. Health Perspect. 2019, 127, 126002. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Liu, C.; Chen, R.; Wang, W.; Li, W.; Kan, H.; Fu, C. Ambient air pollution and daily hospital admissions for mental disorders in Shanghai, China. Sci. Total Environ. 2018, 613–614, 324–330. [Google Scholar] [CrossRef]
- Rentschler, J.; Leonova, N. Global air pollution exposure and poverty. Nat. Commun. 2023, 14, 4432. [Google Scholar] [CrossRef] [PubMed]
- Ju, K.; Lu, L.; Wang, W.; Chen, T.; Yang, C.; Zhang, E.; Xu, Z.; Li, S.; Song, J.; Pan, J.; et al. Causal effects of air pollution on mental health among Adults—An exploration of susceptible populations and the role of physical activity based on a longitudinal nationwide cohort in China. Environ. Res. 2023, 217, 114761. [Google Scholar] [CrossRef]
- Chen, H.; Quick, M.; Kaufman, J.S.; Chen, C.; Kwong, J.C.; Van Donkelaar, A.; Meng, J.; Martin, R.V.; Kim, J.; Lavigne, E.; et al. Impact of lowering fine particulate matter from major emission sources on mortality in Canada: A nationwide causal analysis. Proc. Natl. Acad. Sci. USA 2022, 119, e2209490119. [Google Scholar] [CrossRef]
- Zeng, J.; Bao, R.; McFarland, M. Clean energy substitution: The effect of transitioning from coal to gas on air pollution. Energy Econ. 2022, 107, 105816. [Google Scholar] [CrossRef]
- Cai, W.; Zhang, C.; Suen, H.P.; Ai, S.; Bai, Y.; Bao, J.; Chen, B.; Cheng, L.; Cui, X.; Dai, H.; et al. The 2020 China report of the Lancet Countdown on health and climate change. Lancet Public Health 2021, 6, e64–e81. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Su, H.; Chen, C.; Tao, W.; Streets, D.G.; Lu, Z.; Zheng, B.; Carmichael, G.R.; Lelieveld, J.; Pöschl, U.; et al. Natural gas shortages during the “coal-to-gas” transition in China have caused a large redistribution of air pollution in winter 2017. Proc. Natl. Acad. Sci. USA 2020, 117, 31018–31025. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Wu, D.; Zhang, W.; Cottrell, R.R.; Rockett, I.R.H. Comparative Stress Levels among Residents in Three Chinese Provincial Capitals, 2001 and 2008. PLoS ONE 2012, 7, e48971. [Google Scholar] [CrossRef] [PubMed]
- Fuller, R.; Landrigan, P.J.; Balakrishnan, K.; Bathan, G.; Bose-O’Reilly, S.; Brauer, M.; Caravanos, J.; Chiles, T.; Cohen, A.; Corra, L.; et al. Pollution and health: A progress update. Lancet Planet. Health 2022, 6, e535–e547. [Google Scholar] [CrossRef] [PubMed]
- Ji, H.; Wang, J.; Meng, B.; Cao, Z.; Yang, T.; Zhi, G.; Chen, S.; Wang, S.; Zhang, J. Research on adaption to air pollution in Chinese cities: Evidence from social media-based health sensing. Environ. Res. 2022, 210, 112762. [Google Scholar] [CrossRef]
- AQLI. China. 2024. Available online: https://aqli.epic.uchicago.edu/country-spotlight/china/?lang=zh-hans (accessed on 26 July 2024).
- Xu, Q.; Li, H.; Zhu, D. Socioeconomic status, personality, and major mental disorders: A bidirectional Mendelian randomization study. Schizophrenia 2024, 10, 49. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Shi, B.; Shi, Y.; Marvin, S.; Zheng, Y.; Xia, G. Air pollution dispersal in high density urban areas: Research on the triadic relation of wind, air pollution, and urban form. Sustain. Cities Soc. 2020, 54, 101941. [Google Scholar] [CrossRef]
- Rockey, S. Considering Sex as a Biological Variable in Research—Your Input is Requested—NIH Extramural Nexus. 2014. Available online: https://nexus.od.nih.gov/all/2014/09/11/considering-sex-as-a-biological-variable-in-research-your-input-is-requested/ (accessed on 16 July 2024).
- Qiu, X.; Danesh-Yazdi, M.; Wei, Y.; Di, Q.; Just, A.; Zanobetti, A.; Weisskopf, M.; Dominici, F.; Schwartz, J. Associations of short-term exposure to air pollution and increased ambient temperature with psychiatric hospital admissions in older adults in the USA: A case–crossover study. Lancet Planet. Health 2022, 6, e331–e341. [Google Scholar] [CrossRef]
- Liu, G.; Sun, B.; Yu, L.; Chen, J.; Han, B.; Li, Y.; Chen, J. The Gender-Based Differences in Vulnerability to Ambient Air Pollution and Cerebrovascular Disease Mortality: Evidences Based on 26781 Deaths. Glob. Heart 2020, 15, 46. [Google Scholar] [CrossRef]
- Kim, H.; Noh, J.; Noh, Y.; Oh, S.S.; Koh, S.-B.; Kim, C. Gender Difference in the Effects of Outdoor Air Pollution on Cognitive Function Among Elderly in Korea. Front. Public Health 2019, 7, 375. [Google Scholar] [CrossRef] [PubMed]
- Szyszkowicz, M.; Kousha, T.; Kingsbury, M.; Colman, I. Air Pollution and Emergency Department Visits for Depression: A Multicity Case-Crossover Study. Environ. Health Insights 2016, 10, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Lødrup Carlsen, K.C.; Løvik, M.; Granum, B.; Mowinckel, P.; Carlsen, K.H. Soluble CD14 at 2 yr of age: Gender-related effects of tobacco smoke exposure, recurrent infections and atopic diseases. Pediatr. Allergy Immunol. 2006, 17, 304–312. [Google Scholar] [CrossRef] [PubMed]
- Luginaah, I.N.; Fung, K.Y.; Gorey, K.M.; Webster, G.; Wills, C. Association of Ambient Air Pollution with Respiratory Hospitalization in a Government-Designated “Area of Concern”: The Case of Windsor, Ontario. Environ. Health Perspect. 2005, 113, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Franklin, M.; Zeka, A.; Schwartz, J. Association between PM2.5 and all-cause and specific-cause mortality in 27 US communities. J. Expo. Sci. Environ. Epidemiol. 2007, 17, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Vollmer, W.M.; Enright, P.L.; Pedula, K.L.; Speizer, F.; Kuller, L.H.; Kiley, J.; Weinmann, G.G. Race and Gender Differences in the Effects of Smoking on Lung Function. Chest 2000, 117, 764–772. [Google Scholar] [CrossRef] [PubMed]
- Yunginger, J.W.; Reed, C.E.; O’Connell, E.J.; Melton, L.J.; O’Fallon, W.M.; Silverstein, M.D. A Community-based Study of the Epidemiology of Asthma: Incidence Rates, 1964–1983. Am. Rev. Respir. Dis. 1992, 146, 888–894. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Zou, L.; Lin, W.; Becker, B.; Yeung, A.; Cuijpers, P.; Li, H. Does gender role explain a high risk of depression? A meta-analytic review of 40 years of evidence. J. Affect. Disord. 2021, 294, 261–278. [Google Scholar] [CrossRef] [PubMed]
- Verma, R.; Balhara, Y.S.; Gupta, C. Gender differences in stress response: Role of developmental and biological determinants. Ind. Psychiatry J. 2011, 20, 4. [Google Scholar] [CrossRef]
- Clougherty, J.E. A Growing Role for Gender Analysis in Air Pollution Epidemiology. Environ. Health Perspect. 2010, 118, 167–176. [Google Scholar] [CrossRef]
- Wang, J.-X.; Liu, X.-Q. Climate change, ambient air pollution, and students’ mental health. World J. Psychiatry 2024, 14, 204–209. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Zhou, J.; Li, M.; Huang, J.; Dou, D. Urbanites’ mental health undermined by air pollution. Nat. Sustain. 2023, 6, 470–478. [Google Scholar] [CrossRef]
- Zhang, X.; Chen, X.; Zhang, X. The impact of exposure to air pollution on cognitive performance. Proc. Natl. Acad. Sci. USA 2018, 115, 9193–9197. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.-Z.; Li, L.; Song, Y.-F.; Zhou, Y.-X.; Shen, S.-Q.; Ou, C.-Q. The impact of ambient air pollution on suicide mortality: A case-crossover study in Guangzhou, China. Environ. Health 2016, 15, 90. [Google Scholar] [CrossRef]
- Li, H.; Li, M.; Zhang, S.; Qian, Z. (Min); Zhang, Z.; Zhang, K.; Wang, C.; Arnold, L.D.; McMillin, S.E.; Wu, S.; et al. Interactive effects of cold spell and air pollution on outpatient visits for anxiety in three subtropical Chinese cities. Sci. Total Environ. 2022, 817, 152789. [Google Scholar] [CrossRef] [PubMed]
- Vongruang, P.; Pimonsree, S. Biomass burning sources and their contributions to PM10 concentrations over countries in mainland Southeast Asia during a smog episode. Atmos. Environ. 2020, 228, 117414. [Google Scholar] [CrossRef]
- United States Environmental Protection Agency (US EPA). Best Practices for Review and Validation of Ambient Air Monitoring Data; Report No.: EPA-454/B-21-007; U.S. Environmental Protection Agency, Office of Air Quality Planning and Standards, Air Quality Assessment Division: Washington, DC, USA, 2021. [Google Scholar]
- Department for Environment, Food & Rural Affairs (DEFRA). Quality Assurance and Quality Control (QA/QC) Procedures for UK Air Quality Monitoring under the Air Quality Standards Regulations; Department for Environment, Food and Rural Affairs: London, UK, 2023. [Google Scholar]
- European Commission (EC). Guide to the Demonstration of Equivalence of Ambient Air Monitoring Methods; Working Group on Guidance for the Demonstration of Equivalence: EU; European Commission (EC): Brussels, Belgium, 2010; Volume 92. [Google Scholar]
- European Environment Agency (EEA). Air Quality in Europe—2020 Report—European Environment Agency. Europe: European Environment Agency. 2020. Report No.: 9/2020. Available online: https://www.eea.europa.eu/publications/air-quality-in-europe-2020-report (accessed on 22 June 2024).
- Mooney, P. Connecting Data and Environmental Research at the Environmental Protection Agency; Report No.: 192; Environmental Protection Agency (EPA): Wexford, Ireland, 2016. [Google Scholar]
- Gupta, P.; Christopher, S.A.; Wang, J.; Gehrig, R.; Lee, Y.; Kumar, N. Satellite remote sensing of particulate matter and air quality assessment over global cities. Atmos. Environ. 2006, 40, 5880–5892. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, Z.; Bai, K.; Wei, Y.; Xie, Y.; Zhang, Y.; Ou, Y.; Cohen, J.; Zhang, Y.; Peng, Z.; et al. Satellite remote sensing of atmospheric particulate matter mass concentration: Advances, challenges, and perspectives. Fundam. Res. 2021, 1, 240–258. [Google Scholar] [CrossRef]
- Geddes, J.A.; Martin, R.V.; Boys, B.L.; Van Donkelaar, A. Long-Term Trends Worldwide in Ambient NO2 Concentrations Inferred from Satellite Observations. Environ. Health Perspect. 2016, 124, 281–289. [Google Scholar] [CrossRef]
- Wang, Z.; Chen, L.; Tao, J.; Zhang, Y.; Su, L. Satellite-based estimation of regional particulate matter (PM) in Beijing using vertical-and-RH correcting method. Remote Sens. Environ. 2010, 114, 50–63. [Google Scholar] [CrossRef]
- Mukonza, S.S.; Chiang, J.-L. Meta-Analysis of Satellite Observations for United Nations Sustainable Development Goals: Exploring the Potential of Machine Learning for Water Quality Monitoring. Environments 2023, 10, 170. [Google Scholar] [CrossRef]
- White, A.R. Human expertise in the interpretation of remote sensing data: A cognitive task analysis of forest disturbance attribution. Int. J. Appl. Earth Obs. Geoinf. 2019, 74, 37–44. [Google Scholar] [CrossRef]
- Cheung, Y.; Pang, M.; Lin, H.; Lee, C.K.J. Enable Spatial Thinking Using GIS and Satellite Remote Sensing—A Teacher-Friendly Approach. Procedia-Soc. Behav. Sci. 2011, 21, 130–138. [Google Scholar] [CrossRef]
- van Donkelaar, A.; Martin, R.V.; Brauer, M.; Kahn, R.; Levy, R.; Verduzco, C.; Villeneuve, P.J. Global Estimates of Ambient Fine Particulate Matter Concentrations from Satellite-Based Aerosol Optical Depth: Development and Application. Environ. Health Perspect. 2010, 118, 847–855. [Google Scholar] [CrossRef]
- Duncan, B.N.; Yoshida, Y.; Damon, M.R.; Douglass, A.R.; Witte, J.C. Temperature dependence of factors controlling isoprene emissions. Geophys. Res. Lett. 2009, 36, 2008GL037090. [Google Scholar] [CrossRef]
- United States Environmental Protection Agency (US EPA). Frequent Questions About Air Sensors. 2020. Available online: https://19january2021snapshot.epa.gov/air-sensor-toolbox/frequent-questions-about-air-sensors (accessed on 10 July 2024).
- Ferguson-Moore, J. Can Emerging Air Monitoring Solutions Overcome Current Measurement Limitations? 2023. Available online: https://www.awe.international/article/1851688?utm_source=website&utm_medium=social (accessed on 2 August 2024).
- Sokhi, R.S.; Moussiopoulos, N.; Baklanov, A.; Bartzis, J.; Coll, I.; Finardi, S.; Friedrich, R.; Geels, C.; Grönholm, T.; Halenka, T.; et al. Advances in air quality research—Current and emerging challenges. Atmos. Chem. Phys. 2022, 22, 4615–4703. [Google Scholar] [CrossRef]
- Su, L.; Gao, C.; Ren, X.; Zhang, F.; Cao, S.; Zhang, S.; Chen, T.; Liu, M.; Ni, B.; Liu, M. Understanding the spatial representativeness of air quality monitoring network and its application to PM2.5 in the mainland China. Geosci. Front. 2022, 13, 101370. [Google Scholar] [CrossRef]
- Ippolito, A.R. Toxicities That Matter: Slow Bureaucracy and Polluting Temporalities in a Southern Italian City. Environment and Planning C: Politics and Space. 2022. Available online: https://journals.sagepub.com/doi/full/10.1177/23996544221107517 (accessed on 4 August 2024).
- Li, Z. Bureaucratic response to performance information: How mandatory information disclosure affects environmental inspections. Public Adm. Rev. 2023, 83, 750–762. [Google Scholar] [CrossRef]
- McCarron, A.; Semple, S.; Braban, C.F.; Swanson, V.; Gillespie, C.; Price, H.D. Public engagement with air quality data: Using health behaviour change theory to support exposure-minimising behaviours. J. Expo. Sci. Environ. Epidemiol. 2023, 33, 321–331. [Google Scholar] [CrossRef]
- Jiao, W.; Hagler, G.; Williams, R.; Sharpe, R.; Brown, R.; Garver, D.; Judge, R.; Caudill, M.; Rickard, J.; Davis, M.; et al. Community Air Sensor Network (CAIRSENSE) project: Evaluation of low-costsensor performance in a suburban environment in the southeastern United States. Atmos. Meas. Tech. 2016, 9, 5281–5292. [Google Scholar] [CrossRef]
- Snyder, E.G.; Watkins, T.H.; Solomon, P.A.; Thoma, E.D.; Williams, R.W.; Hagler, G.S.W.; Shelow, D.; Hindin, D.A.; Kilaru, V.J.; Preuss, P.W. The Changing Paradigm of Air Pollution Monitoring. Environ. Sci. Technol. 2013, 47, 11369–11377. [Google Scholar] [CrossRef] [PubMed]
- Clements, A.; Duvall, R.; Greene, D.; Dye, T. The Enhanced Air Sensor Guidebook. U.S. Environmental Protection Agency. 2022. Available online: https://cfpub.epa.gov/si/si_public_record_report.cfm?Lab=CEMM&dirEntryId=356426 (accessed on 20 March 2024).
- De Nazelle, A.; Bode, O.; Orjuela, J.P. Comparison of air pollution exposures in active vs. passive travel modes in European cities: A quantitative review. Environ. Int. 2017, 99, 151–160. [Google Scholar] [CrossRef]
- Holstius, D.M.; Pillarisetti, A.; Smith, K.R.; Seto, E. Field calibrations of a low-cost aerosol sensor at a regulatory monitoring site in California. Atmos. Meas. Tech. 2014, 7, 1121–1131. [Google Scholar] [CrossRef]
- Badura, M.; Batog, P.; Drzeniecka-Osiadacz, A.; Modzel, P. Evaluation of Low-Cost Sensors for Ambient PM2.5 Monitoring. J. Sens. 2018, 2018, 5096540. [Google Scholar] [CrossRef]
- Amegah, A.K.; Agyei-Mensah, S. Urban air pollution in Sub-Saharan Africa: Time for action. Environ. Pollut. 2017, 220, 738–743. [Google Scholar] [CrossRef]
- Sousan, S.; Koehler, K.; Hallett, L.; Peters, T.M. Evaluation of the Alphasense Optical Particle Counter (OPC-N2) and the Grimm Portable Aerosol Spectrometer (PAS-1.108). Aerosol Sci. Technol. J. Am. Assoc. Aerosol Res. 2016, 50, 1352–1365. [Google Scholar] [CrossRef] [PubMed]
- Jerrett, M.; Donaire-Gonzalez, D.; Popoola, O.; Jones, R.; Cohen, R.C.; Almanza, E.; de Nazelle, A.; Mead, I.; Carrasco-Turigas, G.; Cole-Hunter, T.; et al. Validating novel air pollution sensors to improve exposure estimates for epidemiological analyses and citizen science. Environ. Res. 2017, 158, 286–294. [Google Scholar] [CrossRef]
- Castell, N.; Dauge, F.R.; Schneider, P.; Vogt, M.; Lerner, U.; Fishbain, B.; Broday, D.; Bartonova, A. Can commercial low-cost sensor platforms contribute to air quality monitoring and exposure estimates? Environ. Int. 2017, 99, 293–302. [Google Scholar] [CrossRef]
- Larkin, A.; Geddes, J.A.; Martin, R.V.; Xiao, Q.; Liu, Y.; Marshall, J.D.; Brauer, M.; Hystad, P. Global Land Use Regression Model for Nitrogen Dioxide Air Pollution. Environ. Sci. Technol. 2017, 51, 6957–6964. [Google Scholar] [CrossRef] [PubMed]
- Hoek, G.; Beelen, R.; de Hoogh, K.; Vienneau, D.; Gulliver, J.; Fischer, P.; Briggs, D. A review of land-use regression models to assess spatial variation of outdoor air pollution. Atmos. Environ. 2008, 42, 7561–7578. [Google Scholar] [CrossRef]
- Ryan, P.H.; LeMasters, G.K. A Review of Land-use Regression Models for Characterizing Intraurban Air Pollution Exposure. Inhal. Toxicol. 2007, 19, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Jerrett, M.; Arain, A.; Kanaroglou, P.; Beckerman, B.; Potoglou, D.; Sahsuvaroglu, T.; Morrison, J.; Giovis, C. A review and evaluation of intraurban air pollution exposure models. J. Expo. Sci. Environ. Epidemiol. 2005, 15, 185–204. [Google Scholar] [CrossRef] [PubMed]
- De Hoogh, K.; Chen, J.; Gulliver, J.; Hoffmann, B.; Hertel, O.; Ketzel, M.; Bauwelinck, M.; Van Donkelaar, A.; Hvidtfeldt, U.A.; Katsouyanni, K.; et al. Spatial PM2.5, NO2, O3 and BC models for Western Europe—Evaluation of spatiotemporal stability. Environ. Int. 2018, 120, 81–92. [Google Scholar] [CrossRef] [PubMed]
- Beelen, R.; Hoek, G.; Pebesma, E.; Vienneau, D.; De Hoogh, K.; Briggs, D.J. Mapping of background air pollution at a fine spatial scale across the European Union. Sci. Total Environ. 2009, 407, 1852–1867. [Google Scholar] [CrossRef] [PubMed]
- Gulliver, J.; Briggs, D.J. Time–space modeling of journey-time exposure to traffic-related air pollution using GIS. Environ. Res. 2005, 97, 10–25. [Google Scholar] [CrossRef] [PubMed]
- Beelen, R.; Hoek, G.; Vienneau, D.; Eeftens, M.; Dimakopoulou, K.; Pedeli, X.; Tsai, M.-Y.; Künzli, N.; Schikowski, T.; Marcon, A.; et al. Development of NO2 and NOx land use regression models for estimating air pollution exposure in 36 study areas in Europe—The ESCAPE project. Atmos. Environ. 2013, 72, 10–23. [Google Scholar] [CrossRef]
- Mays, N. Qualitative research in health care: Assessing quality in qualitative research. BMJ 2000, 320, 50–52. [Google Scholar] [CrossRef] [PubMed]
- Tenny, S.; Brannan, J.M.; Brannan, G.D. Qualitative Study. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: http://www.ncbi.nlm.nih.gov/books/NBK470395/ (accessed on 23 June 2024).
- McCusker, K.; Gunaydin, S. Research using qualitative, quantitative or mixed methods and choice based on the research. Perfusion 2015, 30, 537–542. [Google Scholar] [CrossRef] [PubMed]
- Denzin, N.K.; Lincoln, Y.S. The SAGE Handbook of Qualitative Research, 4th ed.; SAGE Publications: Thousand Oaks, CA, USA, 2011. [Google Scholar]
- Robins, C.S.; Ware, N.C.; dosReis, S.; Willging, C.E.; Chung, J.Y.; Lewis-Fernández, R. Dialogues on Mixed-Methods and Mental Health Services Research: Anticipating Challenges, Building Solutions. Psychiatr. Serv. 2008, 59, 727–731. [Google Scholar] [CrossRef]
- Barbour, R.S. Checklists for improving rigour in qualitative research: A case of the tail wagging the dog? BMJ 2001, 322, 1115–1117. [Google Scholar] [CrossRef]
- Pope, C. Qualitative research in health care: Analysing qualitative data. BMJ 2000, 320, 114–116. [Google Scholar] [CrossRef]
- LaMarre, A.; Chamberlain, K. Innovating qualitative research methods: Proposals and possibilities. Methods Psychol. 2022, 6, 100083. [Google Scholar] [CrossRef]
- Pilar, M.; Jost, E.; Walsh-Bailey, C.; Powell, B.J.; Mazzucca, S.; Eyler, A.; Purtle, J.; Allen, P.; Brownson, R.C. Quantitative measures used in empirical evaluations of mental health policy implementation: A systematic review. Implement. Res. Pract. 2022, 3, 26334895221141116. [Google Scholar] [CrossRef]
- Johnson, R.B.; Onwuegbuzie, A.J. Mixed Methods Research: A Research Paradigm Whose Time Has Come. Educ. Res. 2004, 33, 14–26. [Google Scholar] [CrossRef]
- Elmer, T.; Fernández, A.; Stadel, M.; Kas, M.; Langener, A. Bidirectional Associations Between Smartphone Usage and Momentary Well-being in Young Adults: Tackling Methodological Challenges by Combining Experience Sampling Methods with Passive Smartphone Data. PsyArXiv, 2023. [Google Scholar] [CrossRef]
- Krohne, N.; Gomboc, V.; Lavrič, M.; Podlogar, T.; Poštuvan, V.; Šedivy, N.Z.; De Leo, D. Slovenian Validation of the Mental Health Literacy Scale (S-MHLS) on the General Population: A Four-Factor Model. INQUIRY 2022, 59, 004695802110471. [Google Scholar] [CrossRef]
- Johnson, S.; Dalton-Locke, C.; Vera San Juan, N.; Foye, U.; Oram, S.; Papamichail, A.; Landau, S.; Rowan Olive, R.; Jeynes, T.; Shah, P.; et al. Impact on mental health care and on mental health service users of the COVID-19 pandemic: A mixed methods survey of UK mental health care staff. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Chiang, J.J.; Lam, P.H. Commentary: Ecology momentary assessment as a tool for understanding dynamic patterns in child and adolescent health and development—Reflections on Russell and Gajos (2020). J. Child Psychol. Psychiatry 2020, 61, 395–398. [Google Scholar] [CrossRef] [PubMed]
- Vaingankar, J.A.; Chong, S.A.; Abdin, E.; Siva Kumar, F.D.; Chua, B.Y.; Sambasivam, R.; Shafie, S.; Jeyagurunathan, A.; Seow, E.; Subramaniam, M. Understanding the relationships between mental disorders, self-reported health outcomes and positive mental health: Findings from a national survey. Health Qual. Life Outcomes 2020, 18, 55. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; McGrath, P.J.; Hayden, J.; Kutcher, S. Mental health literacy measures evaluating knowledge, attitudes and help-seeking: A scoping review. BMC Psychiatry 2015, 15, 291. [Google Scholar] [CrossRef]
- Shiffman, S.; Stone, A.A.; Hufford, M.R. Ecological Momentary Assessment. Annu. Rev. Clin. Psychol. 2008, 4, 1–32. [Google Scholar] [CrossRef]
- Schmidt-Stiedenroth, K.; Mambrey, V.; Dreher, A.; Loerbroks, A. Psychosocial working conditions and mental health among medical assistants in Germany: A scoping review. BMC Public Health 2024, 24, 716. [Google Scholar] [CrossRef] [PubMed]
- Lauwers, L.; Trabelsi, S.; Pelgrims, I.; Bastiaens, H.; De Clercq, E.; Guilbert, A.; Guyot, M.; Leone, M.; Nawrot, T.; Van Nieuwenhuyse, A.; et al. Urban environment and mental health: The NAMED project, protocol for a mixed-method study. BMJ Open 2020, 10, e031963. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.; Myron, R.; Stansfeld, S.; Candy, B. A systematic review of the evidence on the effect of the built and physical environment on mental health. J. Public Ment. Health 2007, 6, 14–27. [Google Scholar] [CrossRef]
- Heavens, D.; Hodgekins, J.; Lower, R.; Spauls, J.; Carroll, B.; Gee, B.; Clarke, T.; Wilson, J. Service user experience of the Norfolk youth service. Ment. Health Rev. J. 2020, 25, 85–98. [Google Scholar] [CrossRef]
- Khoo, J.; Hasan, H.; Eagar, K. Utilisation patterns of privately funded mental health services in Australia. J. Health Organ. Manag. 2019, 33, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Roberts, L.R.; Sadan, V.; Siva, R.; Sathiyaseelan, M.; Rosalind, S.E.; Suresh, P.; Montgomery, S.B. Factors Predicting Mental Health Among Women in Low-Income Communities of a Changing Society: A Mixed-Methods Study. Int. J. Womens Health 2023, 15, 381–394. [Google Scholar] [CrossRef] [PubMed]
- Wen, J.; Fang, Y.; Su, Z.; Cai, J.; Chen, Z. Mental health and its influencing factors of maintenance hemodialysis patients: A semi-structured interview study. BMC Psychol. 2023, 11, 84. [Google Scholar] [CrossRef] [PubMed]
- Alderman, A.K.; Salem, B. Survey Research. Plast. Reconstr. Surg. 2010, 126, 1381–1389. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Brown, G. Beck Depression Inventory–II. 1996. Available online: https://doi.apa.org/doi/10.1037/t00742-000 (accessed on 22 June 2024).
- Creswell, J.W. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches, 4th ed.; SAGE Publications: Thousand Oaks, CA, USA, 2014. [Google Scholar]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Guest, G.; Bunce, A.; Johnson, L. How Many Interviews Are Enough?: An Experiment with Data Saturation and Variability. Field Methods 2006, 18, 59–82. [Google Scholar] [CrossRef]
- Boyatzis, R.E. Transforming Qualitative Information: Thematic Analysis and Code Development; Sage Publications, Inc.: Thousand Oaks, CA, USA, 1998. [Google Scholar]
- Singh, S.; Sagar, R. A critical look at online survey or questionnaire-based research studies during COVID-19. Asian J. Psychiatry 2021, 65, 102850. [Google Scholar] [CrossRef] [PubMed]
- van Ballegooijen, W.; Riper, H.; Klein, B.; Ebert, D.D.; Kramer, J.; Meulenbeek, P.; Cuijpers, P. An Internet-Based Guided Self-Help Intervention for Panic Symptoms: Randomized Controlled Trial. J. Med. Internet Res. 2013, 15, e154. [Google Scholar] [CrossRef] [PubMed]
- Kocalevent, R.-D.; Hinz, A.; Brähler, E. Standardization of the depression screener Patient Health Questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry 2013, 35, 551–555. [Google Scholar] [CrossRef] [PubMed]
- Mays, N.; Pope, C. Qualitative Research: Rigour and qualitative research. BMJ 1995, 311, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Andrade, C. The Limitations of Online Surveys. Indian J. Psychol. Med. 2020, 42, 575–576. [Google Scholar] [CrossRef] [PubMed]
- Snowden, L.R. Bias in Mental Health Assessment and Intervention: Theory and Evidence. Am. J. Public Health 2003, 93, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Andrews, G.; Slade, T.; Peters, L. Classification in psychiatry: ICD–10 versus DSM–IV. Br. J. Psychiatry 1999, 174, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Czeisler, M.É.; Wiley, J.F.; Czeisler, C.A.; Rajaratnam, S.M.W.; Howard, M.E. Uncovering survivorship bias in longitudinal mental health surveys during the COVID-19 pandemic. Epidemiol. Psychiatr. Sci. 2021, 30, e45. [Google Scholar] [CrossRef]
- DeJonckheere, M.; Vaughn, L.M. Semistructured interviewing in primary care research: A balance of relationship and rigour. Fam. Med. Community Health 2019, 7, e000057. [Google Scholar] [CrossRef]
- Smith, J.A.; Osborn, M. Interpretative phenomenological analysis as a useful methodology for research on the lived experience of pain. Br. J. Pain 2015, 9, 41–42. [Google Scholar] [CrossRef] [PubMed]
- Chartrand, T.L.; Maddux, W.W.; Lakin, J.L. Beyond the Perception-Behavior Link: The Ubiquitous Utility and Motivational Moderators of Nonconscious Mimicry. In The New Unconscious; Hassin, R.R., Uleman, J.S., Bargh, J.A., Eds.; Oxford University Press: Oxford, UK, 2012; pp. 334–361. ISBN 978-0-19-530769-6. [Google Scholar]
- Renjith, V.; Yesodharan, R.; Noronha, J.A.; Ladd, E.; George, A. Qualitative Methods in Health Care Research. Int. J. Prev. Med. 2021, 12, 20. [Google Scholar] [CrossRef] [PubMed]
- Horsfall, M.; Eikelenboom, M.; Draisma, S.; Smit, J.H. The Effect of Rapport on Data Quality in Face-to-Face Interviews: Beneficial or Detrimental? Int. J. Environ. Res. Public. Health 2021, 18, 10858. [Google Scholar] [CrossRef] [PubMed]
- Newby, D.; Taylor, N.; Joyce, D.W.; Winchester, L.M. Optimising the use of electronic medical records for large scale research in psychiatry. Transl. Psychiatry 2024, 14, 232. [Google Scholar] [CrossRef] [PubMed]
- Hecht, J. The future of electronic health records. Nature 2019, 573, S114–S116. [Google Scholar] [CrossRef] [PubMed]
- Russ, T.C.; Woelbert, E.; Davis, K.A.S.; Hafferty, J.D.; Ibrahim, Z.; Inkster, B.; John, A.; Lee, W.; Maxwell, M.; McIntosh, A.M.; et al. How data science can advance mental health research. Nat. Hum. Behav. 2018, 3, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Hjollund, N.H.I.; Valderas, J.M.; Kyte, D.; Calvert, M.J. Health Data Processes: A Framework for Analyzing and Discussing Efficient Use and Reuse of Health Data with a Focus on Patient-Reported Outcome Measures. J. Med. Internet Res. 2019, 21, e12412. [Google Scholar] [CrossRef]
- Lowe, H.J.; Ferris, T.A.; Hernandez, P.M.; Weber, S.C. STRIDE—An Integrated Standards-Based Translational Research Informatics Platform. AMIA. Annu. Symp. Proc. 2009, 2009, 391–395. [Google Scholar] [PubMed]
- Casey, J.A.; Schwartz, B.S.; Stewart, W.F.; Adler, N.E. Using Electronic Health Records for Population Health Research: A Review of Methods and Applications. Annu. Rev. Public Health 2016, 37, 61–81. [Google Scholar] [CrossRef]
- Smit, J.-A.; van der Graaf, R.; Mostert, M.; Vaartjes, I.; Zuidgeest, M.; Grobbee, D.; van Delden, J.J.M. Overcoming ethical and legal obstacles to data linkage in health research: Stakeholder perspectives. Int. J. Popul. Data Sci. 2023, 8, 2151. [Google Scholar] [CrossRef]
- Gehrmann, J.; Herczog, E.; Decker, S.; Beyan, O. What prevents us from reusing medical real-world data in research. Sci. Data 2023, 10, 459. [Google Scholar] [CrossRef] [PubMed]
- Kass, N.E.; Natowicz, M.R.; Hull, S.C.; Faden, R.R.; Plantinga, L.; Gostin, L.O.; Slutsman, J. The Use of Medical Records in Research: What Do Patients Want? J. Law Med. Ethics J. Am. Soc. Law Med. Ethics 2003, 31, 429–433. [Google Scholar] [CrossRef] [PubMed]
- Crawley, M.J. The R Book, 1st ed.; Wiley: Hoboken, NJ, USA, 2012; Available online: https://onlinelibrary.wiley.com/doi/book/10.1002/9781118448908 (accessed on 8 July 2024).
- Muñoz-Pichardo, J.M.; Pino-Mejías, R.; García-Heras, J.; Ruiz-Muñoz, F.; Luz González-Regalado, M. A multivariate Poisson regression model for count data. J. Appl. Stat. 2021, 48, 2525–2541. [Google Scholar] [CrossRef]
- Hidalgo, B.; Goodman, M. Multivariate or Multivariable Regression? Am. J. Public Health 2013, 103, 39–40. [Google Scholar] [CrossRef] [PubMed]
- Gelman, A.; Hill, J. Data Analysis Using Regression and Multilevel/Hierarchical Models, 1st ed.; Cambridge University Press: Cambridge, UK, 2006; Available online: https://www.cambridge.org/core/product/identifier/9780511790942/type/book (accessed on 4 July 2024).
- Raudenbush, S.W.; Bryk, A.S. Hierarchical Linear Models: Applications and Data Analysis Methods; SAGE: Thousand Oaks, CA, USA, 2002. [Google Scholar]
- Peng, C.-Y.J.; Lee, K.L.; Ingersoll, G.M. An Introduction to Logistic Regression Analysis and Reporting. J. Educ. Res. 2002, 96, 3–14. [Google Scholar] [CrossRef]
- Koletsi, D.; Pandis, N. Conditional logistic regression. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 1191–1192. [Google Scholar] [CrossRef] [PubMed]
- van der Net, J.B.; Janssens, A.C.J.W.; Eijkemans, M.J.C.; Kastelein, J.J.P.; Sijbrands, E.J.G.; Steyerberg, E.W. Cox proportional hazards models have more statistical power than logistic regression models in cross-sectional genetic association studies. Eur. J. Hum. Genet. 2008, 16, 1111–1116. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Berdine, G. The Negative Binomial regression. Southwest Respir. Crit. Care Chron. 2015, 3, 50–54. [Google Scholar]
- Lu, B. Propensity Score Matching with Time-Dependent Covariates. Biometrics 2005, 61, 721–728. [Google Scholar] [CrossRef]
- Wang, M. Generalized Estimating Equations in Longitudinal Data Analysis: A Review and Recent Developments. Adv. Stat. 2014, 303728. [Google Scholar] [CrossRef]
- Thurman, S.L. Ethical considerations in longitudinal studies of human infants. Infant Behav. Dev. 2015, 38, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Hedeker, D.; Gibbons, R.D. Longitudinal Data Analysis | Wiley Series in Probability and Statistics; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2006; Available online: https://onlinelibrary.wiley.com/doi/book/10.1002/0470036486 (accessed on 22 June 2024).
- Singer, J.D.; Willett, J.B. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence; Oxford University Press: Oxford, UK, 2003; Available online: https://academic.oup.com/book/41753 (accessed on 23 June 2024).
- Diggle, P.J.; Heagerty, P.; Liang, K.Y.; Zeger, S.L. The Analysis of Longitudinal Data, 2nd ed.; Oxford University Press: Oxford, UK, 2002. [Google Scholar]
- Campbell, C.E.; Cotter, D.L.; Bottenhorn, K.L.; Burnor, E.; Ahmadi, H.; Gauderman, W.J.; Cardenas-Iniguez, C.; Hackman, D.; McConnell, R.; Berhane, K.; et al. Air pollution and emotional behavior in adolescents across the U.S. medRxiv, 2023; preprint. [Google Scholar] [CrossRef]
- Bishop, K.; Ketcham, J.; Kuminoff, N. Hazed and Confused: The Effect of Air Pollution on Dementia; National Bureau of Economic Research: Cambridge, MA, USA, 2018; Available online: http://www.nber.org/papers/w24970.pdf (accessed on 26 July 2024).
- Yeung, J.; CNN. Chinese People Are Living Two Years Longer Thanks to ‘War on Pollution’, Report Says. 2023. Available online: https://www.cnn.com/2023/08/30/asia/air-pollution-report-china-south-asia-intl-hnk-scn/index.html (accessed on 27 July 2024).
- Mead, M.I.; Okello, G.; Mbandi, A.M.; Pope, F.D. Spotlight on air pollution in Africa. Nat. Geosci. 2023, 16, 930–931. [Google Scholar] [CrossRef]
- Husaini, D.C.; Reneau, K.; Balam, D. Air pollution and public health in Latin America and the Caribbean (LAC): A systematic review with meta-analysis. Beni-Suef Univ. J. Basic Appl. Sci. 2022, 11, 122. [Google Scholar] [CrossRef] [PubMed]
- Fuller, C.H.; Amegah, A.K. Limited Air Pollution Research on the African Continent: Time to Fill the Gap. Int. J. Environ. Res. Public Health 2022, 19, 6359. [Google Scholar] [CrossRef]
- La Colla, N.S.; Botté, S.E.; Marcovecchio, J.E. Atmospheric particulate pollution in South American megacities. Environ. Rev. 2021, 29, 415–429. [Google Scholar] [CrossRef]
- Gómez Peláez, L.M.; Santos, J.M.; de Almeida Albuquerque, T.T.; Reis, N.C.; Andreão, W.L.; de Fátima Andrade, M. Air quality status and trends over large cities in South America. Environ. Sci. Policy 2020, 114, 422–435. [Google Scholar] [CrossRef]
- Rössler, W. The stigma of mental disorders: A millennia-long history of social exclusion and prejudices. EMBO Rep. 2016, 17, 1250–1253. [Google Scholar] [CrossRef]
- Clavo, B.; Cánovas-Molina, A.; Díaz-Garrido, J.A.; Cañas, S.; Ramallo-Fariña, Y.; Laffite, H.; Federico, M.; Rodríguez-Abreu, D.; Galván, S.; García-Lourve, C.; et al. Effects of ozone therapy on anxiety and depression in patients with refractory symptoms of severe diseases: A pilot study. Front. Psychol. 2023, 14, 1176204. [Google Scholar] [CrossRef]
- Manczak, E.M.; Miller, J.G.; Gotlib, I.H. Census tract ambient ozone predicts trajectories of depressive symptoms in adolescents. Dev. Psychol. 2022, 58, 485–492. [Google Scholar] [CrossRef]
- Gładka, A.; Rymaszewska, J.; Zatoński, T. Impact of air pollution on depression and suicide. Int. J. Occup. Med. Environ. Health 2018, 31, 711–721. [Google Scholar] [CrossRef] [PubMed]
- Kioumourtzoglou, M.-A.; Power, M.C.; Hart, J.E.; Okereke, O.I.; Coull, B.A.; Laden, F.; Weisskopf, M.G. The Association Between Air Pollution and Onset of Depression Among Middle-Aged and Older Women. Am. J. Epidemiol. 2017, 185, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, Y.; Li, L.; Zhang, Y.; Dai, F. Associations of exposure to volatile organic compounds with sleep health and potential mediators: Analysis of NHANES data. Front. Public Health 2024, 12, 1423771. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.; Liu, M.; Tian, J. Volatile organic compounds exposure associated with depression among U.S. adults: Results from NHANES 2011–2020. Chemosphere 2024, 349, 140690. [Google Scholar] [CrossRef] [PubMed]
- Fiedler, N.; Laumbach, R.; Kelly-McNeil, K.; Lioy, P.; Fan, Z.-H.; Zhang, J.; Ottenweller, J.; Ohman-Strickland, P.; Kipen, H. Health Effects of a Mixture of Indoor Air Volatile Organics, Their Ozone Oxidation Products, and Stress. Environ. Health Perspect. 2005, 113, 1542–1548. [Google Scholar] [CrossRef] [PubMed]
- Tota, M.; Karska, J.; Kowalski, S.; Piątek, N.; Pszczołowska, M.; Mazur, K.; Piotrowski, P. Environmental pollution and extreme weather conditions: Insights into the effect on mental health. Front. Psychiatry 2024, 15, 1389051. [Google Scholar] [CrossRef] [PubMed]
- Szyszkowicz, M.; Rowe, B.H. Ambient Air Pollution and Depressive Symptoms. 2014. Available online: https://peerj.com/preprints/757v1 (accessed on 3 August 2024).[Green Version]
- Yang, A.C.; Tsai, S.-J.; Huang, N.E. Decomposing the association of completed suicide with air pollution, weather, and unemployment data at different time scales. J. Affect. Disord. 2011, 129, 275–281. [Google Scholar] [CrossRef]
- Szyszkowicz, M.; Rowe, B.; Colman, I. Air pollution and daily emergency department visits for depression. Int. J. Occup. Med. Environ. Health 2009, 22, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Szyszkowicz, M.; Willey, J.B.; Grafstein, E.; Rowe, B.H.; Colman, I. Air Pollution and Emergency Department Visits for Suicide Attempts in Vancouver, Canada. Environ. Health Insights 2010, 4, EHI.S5662. [Google Scholar] [CrossRef]
- Hopkins, R.O.; Woon, F.L.M. Neuroimaging, Cognitive, and Neurobehavioral Outcomes Following Carbon Monoxide Poisoning. Behav. Cogn. Neurosci. Rev. 2006, 5, 141–155. [Google Scholar] [CrossRef]
- Pan, Y.-J.; Liao, S.-C.; Lee, M.-B. Suicide by charcoal burning in Taiwan, 1995–2006. J. Affect. Disord. 2010, 120, 254–257. [Google Scholar] [CrossRef]
- Lee, E.; Leung, C.-M. Clinical predictors of psychiatric and medical morbidities of charcoal-burning suicide attempt in Hong Kong. Gen. Hosp. Psychiatry 2008, 30, 561–563. [Google Scholar] [CrossRef]
- Liu, K.Y.; Beautrais, A.; Caine, E.; Chan, K.; Chao, A.; Conwell, Y.; Law, C.; Lee, D.; Li, P.; Yip, P. Charcoal burning suicides in Hong Kong and urban Taiwan: An illustration of the impact of a novel suicide method on overall regional rates. J. Epidemiol. Community Health 2007, 61, 248–253. [Google Scholar] [CrossRef]
- Lo, C.-P.; Chen, S.-Y.; Lee, K.-W.; Chen, W.-L.; Chen, C.-Y.; Hsueh, C.-J.; Huang, G.-S. Brain Injury After Acute Carbon Monoxide Poisoning: Early and Late Complications. Am. J. Roentgenol. 2007, 189, W205–W211. [Google Scholar] [CrossRef] [PubMed]
- Ho, R.C.M.; Cheng, W.; Chua, A.N.C.; Mak, A. Neuropsychiatric aspects of carbon monoxide poisoning: Diagnosis and management. Adv. Psychiatr. Treat. 2012, 18, 94–101. [Google Scholar] [CrossRef]
- Hautekiet, P.; Saenen, N.D.; Demarest, S.; Keune, H.; Pelgrims, I.; Van der Heyden, J.; De Clercq, E.M.; Nawrot, T.S. Air pollution in association with mental and self-rated health and the mediating effect of physical activity. Environ. Health 2022, 21, 29. [Google Scholar] [CrossRef] [PubMed]
- Nobile, F.; Forastiere, A.; Michelozzi, P.; Forastiere, F.; Stafoggia, M. Long-term exposure to air pollution and incidence of mental disorders. A large longitudinal cohort study of adults within an urban area. Environ. Int. 2023, 181, 108302. [Google Scholar] [CrossRef] [PubMed]
- Bai, L.; Zhang, X.; Zhang, Y.; Cheng, Q.; Duan, J.; Gao, J.; Xu, Z.; Zhang, H.; Wang, S.; Su, H. Ambient concentrations of NO2 and hospital admissions for schizophrenia. Occup. Environ. Med. 2019, 76, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Vert, C.; Sánchez-Benavides, G.; Martínez, D.; Gotsens, X.; Gramunt, N.; Cirach, M.; Molinuevo, J.L.; Sunyer, J.; Nieuwenhuijsen, M.J.; Crous-Bou, M.; et al. Effect of long-term exposure to air pollution on anxiety and depression in adults: A cross-sectional study. Int. J. Hyg. Environ. Health 2017, 220, 1074–1080. [Google Scholar] [CrossRef]
- Gignac, F.; Righi, V.; Toran, R.; Paz Errandonea, L.; Ortiz, R.; Mijling, B.; Naranjo, A.; Nieuwenhuijsen, M.; Creus, J.; Basagaña, X. Short-term NO2 exposure and cognitive and mental health: A panel study based on a citizen science project in Barcelona, Spain. Environ. Int. 2022, 164, 107284. [Google Scholar] [CrossRef]
- Yan, W.; Yue, H.; Ji, X.; Li, G.; Sang, N. Prenatal NO2 exposure and neurodevelopmental disorders in offspring mice: Transcriptomics reveals sex-dependent changes in cerebral gene expression. Environ. Int. 2020, 138, 105659. [Google Scholar] [CrossRef] [PubMed]
- Shang, L.; Yang, L.; Yang, W.; Huang, L.; Qi, C.; Yang, Z.; Fu, Z.; Chung, M.C. Effects of prenatal exposure to NO2 on children’s neurodevelopment: A systematic review and meta-analysis. Environ. Sci. Pollut. Res. Int. 2020, 27, 24786–24798. [Google Scholar] [CrossRef] [PubMed]
- Min, J.; Min, K. Exposure to ambient PM10 and NO2 and the incidence of attention-deficit hyperactivity disorder in childhood. Environ. Int. 2017, 99, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Bakolis, I.; Hammoud, R.; Stewart, R.; Beevers, S.; Dajnak, D.; MacCrimmon, S.; Broadbent, M.; Pritchard, M.; Shiode, N.; Fecht, D.; et al. Mental health consequences of urban air pollution: Prospective population-based longitudinal survey. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 1587–1599. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Ambient Air Pollution: A Global Assessment of Exposure and Burden of Disease; World Health Organization: Geneva, Switzerland, 2016; Available online: https://iris.who.int/handle/10665/250141 (accessed on 26 July 2024).
- Pope, C.A.; Dockery, D.W. Health Effects of Fine Particulate Air Pollution: Lines that Connect. J. Air Waste Manag. Assoc. 2006, 56, 709–742. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, G.T.H.; La, L.T.; Hoang-Cong, H.; Le, A.H. An exploration of meteorological effects on PM2.5 air quality in several provinces and cities in Vietnam. J. Environ. Sci. 2024, 145, 139–151. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Chen, D.; Zhao, C.; Kwan, M.; Cai, J.; Zhuang, Y.; Zhao, B.; Wang, X.; Chen, B.; Yang, J.; et al. Influence of meteorological conditions on PM2.5 concentrations across China: A review of methodology and mechanism. Environ. Int. 2020, 139, 105558. [Google Scholar] [CrossRef]
- Dung, N.A.; Son, D.H.; Hanh, N.T.D.; Tri, D.Q. Effect of Meteorological Factors on PM10 Concentration in Hanoi, Vietnam. J. Geosci. Environ. Prot. 2019, 7, 138–150. [Google Scholar] [CrossRef]
- Usman, F.; Zeb, B.; Alam, K.; Valipour, M.; Ditta, A.; Sorooshian, A.; Roy, R.; Ahmad, I.; Iqbal, R. Exploring the Mass Concentration of Particulate Matter and Its Relationship with Meteorological Parameters in the Hindu-Kush Range. Atmosphere 2022, 13, 1628. [Google Scholar] [CrossRef]
- Banks, A.; Kooperman, G.J.; Xu, Y. Meteorological Influences on Anthropogenic PM2.5 in Future Climates: Species Level Analysis in the Community Earth System Model v2. Earths Future 2022, 10, e2021EF002298. [Google Scholar] [CrossRef]
- Zeb, B.; Ditta, A.; Alam, K.; Sorooshian, A.; Din, B.U.; Iqbal, R.; Habib ur Rahman, M.; Raza, A.; Alwahibi, M.S.; Elshikh, M.S. Wintertime investigation of PM10 concentrations, sources, and relationship with different meteorological parameters. Sci. Rep. 2024, 14, 154. [Google Scholar] [CrossRef] [PubMed]
- Reuben, A.; Manczak, E.M.; Cabrera, L.Y.; Alegria, M.; Bucher, M.L.; Freeman, E.C.; Miller, G.W.; Solomon, G.M.; Perry, M.J. The Interplay of Environmental Exposures and Mental Health: Setting an Agenda. Environ. Health Perspect. 2022, 130, 025001. [Google Scholar] [CrossRef] [PubMed]
- Rataj, E.; Kunzweiler, K.; Garthus-Niegel, S. Extreme weather events in developing countries and related injuries and mental health disorders—A systematic review. BMC Public Health 2016, 16, 1020. [Google Scholar] [CrossRef] [PubMed]
- Beyer, K.M.M.; Kaltenbach, A.; Szabo, A.; Bogar, S.; Nieto, F.J.; Malecki, K.M. Exposure to Neighborhood Green Space and Mental Health: Evidence from the Survey of the Health of Wisconsin. Int. J. Environ. Res. Public Health 2014, 11, 3453–3472. [Google Scholar] [CrossRef]
| Keyword | Search Terms Used |
|---|---|
| Urban | “Urban” OR “city” |
| Suburban | “Suburban” OR “Neighbourhood” OR “Residential” |
| Air Quality | “Air Quality” OR “Air Pollution”, OR “ambient pollution “, OR “air contaminants”, OR “outdoor air pollution”, OR “air pollutants” OR “particulate matter”, OR “PM” OR “PM2.5” OR “PM10” OR “Fine particulates” OR “course particulates” OR “Ultrafine particulates” OR “environmental effects” OR “environmental stressors” |
| Mental Health | “Mental health” OR “anxiety” OR “depression” OR “stress” OR “anxiety disorder” OR “Anxious neurosis” OR “Depressive neurosis” OR “Nervous” OR “Feeling of anxiety” OR “Worry” OR “Depression test” OR “Mental stress” OR “Occupational stress” OR “Psychological pressure” OR “Stress management” OR “bipolar disorder” OR “suicide” * |
| Population | “adults” OR “young adults” |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Published in English | Published in languages other than English |
| Location: Worldwide—any country or studies including more than one country. | Studies do not specify the location. |
| Environment: Urban, suburban, AND/OR rural setting; outdoor AQ only. | Focusing only on indoor AQ. |
| Cohort: Includes adults (18–69) with or without existing mental health disorders, including various socioeconomic backgrounds and lifestyles. | Includes vulnerable populations (elderly (>69), children (<18), only people with disabilities, and/or only pregnant women). |
| Mental health: depressive AND/OR anxiety symptoms, AND/OR stress | Any other mental health-related issue, relating to other health-related complications and diseases such as cardiovascular or respiratory, economic and political indicators, and generally any publication that does not analyze depressive, anxiety and stress symptoms in their studies and primarily focuses on other health issues, identities, aggressive behavior, alcohol, tobacco and similar products, and/or drug consumption/addiction, sleeping disorders, general wellbeing (not defining MH), school performances and/or learning difficulties, physical activity, obesity, image distortion and/or eating disorders, recovery, financial security, growth, community belonging and social security, rights/respect, personal relationships, cultural differences and awareness strategies, politics, people’s perspectives, without including the relationship between AQ and MH. |
| Air quality: Relating to PM. | Any other pollutants excluding PM in the literature. |
| Explores the relationship between PM and mental health. | Sources that focus only on mental health or air quality/pollution without exploring the possible relationship between the two subjects. |
| Any available full-text research that includes methodology and involves human cohorts, observational studies (e.g., cohort studies, case-control studies, cross-sectional studies, longitudinal, structured observations, and participant observation), controlled studies, major clinical studies, case studies, time series, etc. | Review publications such as scoping reviews, systematic reviews, meta-analyses, literature reviews, general narrative reviews, non-human related studies and reviews, practice guidelines, protocols, conference abstracts, letters, or any other publication that does not specify the methodology used. |
| Study design: qualitative, quantitative, or mixed methods. | - |
| Date: Sources published between 2010 and 2024. | Any study published before 2010. |
| Results: Makes or does not make a connection between air pollution and mental health in the end—methodologies are key. | Any studies that do not specify the methodology used in their publication to achieve results, whether successful or not. |
| Study | Study Name | Authors | Year | Country | Methodology—AQ | Methodology—MH | Controlled | Statistical Analysis | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Meteorological | Demographics | Socioeconomic Status | ||||||||
| Study 1 | Relationship of emergency department visits for suicide attempts with meteorological and air pollution conditions | Miyazaki et al. [43] | 2023 | Japan | Monitoring stations | Medical (ED) data | Yes | Yes | No | Multivariate Poisson regression |
| Study 2 | Residential greenspace and anxiety symptoms among Australian women living in major cities: A longitudinal analysis | Mouly et al. [44] | 2023 | Australia | Land-use regression (LUR) model | GAD | Yes | Yes | Yes | Generalized estimating equation (GEE) |
| Study 3 | How People’s COVID-19-Induced-Worries and Multiple Environmental Exposures Are Associated with Their Depression, Anxiety, and Stress during the Pandemic | Huang et al. [45] | 2023 | Hong Kong | Portable air pollutant sensors. | PHQ-4 and self-reported scale of stress symptoms. | No | Yes | Yes | Linear regression models |
| Study 4 | Real-time air pollution and bipolar disorder symptoms: a remote-monitored cross-sectional study | Kandola and Hayes [46] | 2023 | UK | Air quality index (AQI) | PHQ-8 and ASRM scale | Yes | Yes | No | Linear regression |
| Study 5 | Long-term Exposure to Multiple Ambient Air Pollutants and Association with Incident Depression and Anxiety | Yang et al. [47] | 2023 | UK | LUR | Medical data | No | Yes | Yes | Cox proportional hazards models |
| Study 6 | Multiple environmental exposures along daily mobility paths and depressive symptoms: A smartphone-based tracking study | Roberts & Helbich [48] | 2021 | Netherlands | LUR | PHQ-9 | No | Yes | Yes | Multiple regression analyses |
| Study 7 | Daily space-time activities, multiple environmental exposures, and anxiety symptoms: A cross-sectional mobile phone-based sensing study | Lan et al. [49] | 2022 | Netherlands | LUR | GAD-7 | No | Yes | Yes | Multiple linear regressions, including the Random Forest (RF) model |
| Study 8 | Association between traffic-related air pollution and anxiety hospitalizations in a coastal Chinese city: are there potentially susceptible groups? | Ji et al. [50] | 2022 | China | Monitoring stations | Medical data | Yes | Yes | No | Generalized additive model (GAM) |
| Study 9 | Spatial Variability of the Relationship between Air Pollution and Well-Being | Li & Managi [51] | 2022 | Japan | Database | Survey | No | Yes | Yes | Linear analyses |
| Study 10 | Air pollution and anti-social behavior: Evidence from a randomized lab-in-the-field experiment | Lohmann et al. [52] | 2023 | China | Air Quality Index (AQI) |
| Yes | Yes | No | Linear regression |
| Study 11 | Do objective and subjective traffic-related pollution, physical activity, and nature exposure affect mental wellbeing? Evidence from Shenzhen, China | Huang, Tian & Yuan [53] | 2023 | China | NASA Sedac database |
| No | Yes | Yes | Multivariate linear regression |
| Study 12 | The effects of long-term exposure to air pollution on incident mental disorders among patients with prediabetes and diabetes: Findings from a large prospective cohort | Feng et al. [54] | 2016 | UK | UK Air database | Healthcare data | Yes | Yes | Yes | Time-varying covariates Cox model and generalized propensity score (GPS) |
| Study 13 | The Impacts of Air Pollution on Mental Health: Evidence from the Chinese University Students | Zu et al. [55] | 2020 | China | The Air Quality Index (AQI) data | CES-D | No | Yes | Yes | Multivariable models |
| Study 14 | Associations of co-exposures to air pollution and noise with psychological stress in space and time: A case study in Beijing, China | Tao et al. [56] | 2021 | China | The Airbeam sensor | EMA | Yes | Yes | Yes | Multilevel ordinal logistic regression models |
| Study 15 | Effects of vitamin D on associations between air pollution and mental health outcomes in Korean adults: Results from the Korea National Health and Nutrition Examination Survey (KNHANES) | Kim et al. [57] | 2023 | S. Korea | Monitoring stations | Self-reported questionnaire | No | Yes | Yes | Multiple logistic regression |
| Study 16 | Relationship between chronic exposure to ambient air pollution and mental health in Korean adult cancer survivors and the general population | Kim et al. [58] | 2021 | S. Korea | Monitoring stations | Self-reported questionnaire | No | Yes | Yes | Multiple logistic regression |
| Study 17 | Ambient air pollution exposure and depressive symptoms: Findings from the French CONSTANCES cohort | Sakhvidi et al. [59] | 2022 | France | LUR | CES-D | No | Yes | Yes | Negative binomial regressions |
| Study 18 | Associations of PM2.5 and road traffic noise with mental health: Evidence from UK Biobank | Hao et al. [60] | 2022 | UK | LUR | PHQ and the SCID-I | No | Yes | Yes | Logistic regression model |
| Study 19 | Associations between long term exposures to outdoor air pollution and indoor solid fuel use and depression in China | Zhang et al. [61] | 2022 | China | Monitoring stations | PHQ-9 | No | Yes | Yes | Multiple logistic regression |
| Study 20 | PM2.5 exposure and anxiety in China: evidence from the prefectures | Chen et al. [62] | 2021 | China | Air Quality Online Monitoring and Analysis Platform | Internet search behavior | No | No | Yes | Two-way fixed effect (FE) regression model |
| Study 21 | Short-term effects of traffic noise on suicides and emergency hospital admissions due to anxiety and depression in Madrid (Spain) | Díaz et al. [63] | 2020 | Spain | Monitoring stations | Medical (ED) data | Yes | No | No | Linear models and Poisson regression. |
| Study 22 | The relationship between air pollution and depression in China: Is neighborhood social capital protective? | Wang et al. [64] | 2018 | China | Airborne Fine Particulate Matter and Air Quality Index | CES-D | No | Yes | Yes | Multilevel linear regression analyses |
| Study 23 | Long-term exposure to ambient air pollutants and mental health status: A nationwide population-based cross-sectional study | Shin, Park & Choi [65] | 2018 | S. Korea | Monitoring stations | EQ-5D index | Yes | Yes | Yes | Multiple logistic regression |
| Study 24 | Greenspace and mortality in the U.K. Biobank: Longitudinal cohort analysis of socio-economic, environmental, and biomarker pathways | Wan et al. [66] | 2022 | UK | LUR | PHQ-4 and EPQR-Short | Yes | Yes | Yes | Cox proportional hazards model |
| Study 25 | Ambient temperature and air pollution associations with suicide and homicide mortality in California: A statewide case-crossover study | Rahman et al. [67] | 2023 | US | United States Environmental Protection’s (US EPA’s) AQ System | Healthcare (death) data | Yes | No | No | Conditional logistic regression models |
| Study 26 | Impacts of coal mine fire related PM2.5 on the utilization of ambulance and hospital services for mental health conditions | Carroll et al. [68] | 2022 | Australia | The Air Pollution Model (TAPM) | Medical (ED) data | Yes | No | No | GAMs |
| Study 27 | Urban Air Pollution and Mental Stress: A Nationwide Study of University Students in China | Zhang et al. [69] | 2021 | China | National Bureau of Statistics | CPSS | No | Yes | Yes | Multilevel logistic regression |
| Study 28 | Outdoor light at night, air pollution, and depressive symptoms: A cross-sectional study in the Netherlands | Helbich, Browning & Huss [70] | 2020 | Netherlands | LUR | PHQ–9 | No | Yes | Yes | GAM |
| Study 29 | Not urbanization level but socioeconomic, physical, and social neighborhood characteristics are associated with the presence and severity of depressive and anxiety disorders | Generaal et al. [71] | 2019 | Netherlands | LUR | IDS, BAI, and FQ | No | Yes | Yes | Multilevel logistic and linear regression |
| Study Characteristics (Total n = 29) | Count n (%) | |
|---|---|---|
| Year of publication | 2023 | 10 (34.48) |
| 2022 | 8 (27.59) | |
| 2021 | 5 (17.24) | |
| 2020 | 3 (10.34) | |
| 2019 | 1 (3.45) | |
| 2018 | 2 (6.90) | |
| Continent | Asia | 15 (51.72) |
| Europe | 11 (37.93) | |
| North America | 1 (3.45) | |
| Australia or New Zealand | 2 (6.90) | |
| Results achieved (MH and AQ link realized) | Yes | 27 (93.10) |
| No | 2 (3.45) | |
| MH methods | Quantitative methods | 29 (100) |
| Healthcare/medical records | 7 (24.14) | |
| Surveys/questionnaires and diagnostic classification/rating scales | 21 (72.41) | |
| Other * | 1 (3.45) | |
| AQ methods | Monitoring data | 19 (65.52) |
| -Data from stationary (national/local) monitors | 17 (58.62) | |
| -Portable AQ monitors | 2 (6.90) | |
| Land-use models | 10 (34.48) | |
| -LUR | 9 (31.03) | |
| -TAPM | 1 (3.45) | |
| Study design | Cross-sectional | 19 (65.52) |
| Longitudinal | 4 (13.79) | |
| Time series | 2 (6.90) | |
| Case study | 1 (3.45) | |
| Prospective cohort | 1 (3.45) | |
| Randomized experiment | 1 (3.45) | |
| Statistical methods | Linear regression models ** | 14 (48.28) |
| Logistic regression models *** | 8 (27.59) | |
| Survival analysis models **** | 3 (10.34) | |
| Other ***** | 4 (13.79) | |
| Studies including PM | Only PM | 10 (34.48) |
| Includes other pollutants ****** | 19 (65.52) | |
| Studies MH focus | Anxiety | 4 (13.79) |
| Depression | 10 (34.48) | |
| Stress | 4 (13.79) | |
| -Anxiety & depression | 6 (20.69) | |
| -Depression & stress | 4 (13.79) | |
| -Depression, anxiety, and stress | 1 (3.45) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leontjevaite, K.; Donnelly, A.; MacIntyre, T.E. Air Pollution Effects on Mental Health Relationships: Scoping Review on Historically Used Methodologies to Analyze Adult Populations. Air 2024, 2, 258-291. https://doi.org/10.3390/air2030016
Leontjevaite K, Donnelly A, MacIntyre TE. Air Pollution Effects on Mental Health Relationships: Scoping Review on Historically Used Methodologies to Analyze Adult Populations. Air. 2024; 2(3):258-291. https://doi.org/10.3390/air2030016
Chicago/Turabian StyleLeontjevaite, Kristina, Aoife Donnelly, and Tadhg Eoghan MacIntyre. 2024. "Air Pollution Effects on Mental Health Relationships: Scoping Review on Historically Used Methodologies to Analyze Adult Populations" Air 2, no. 3: 258-291. https://doi.org/10.3390/air2030016
APA StyleLeontjevaite, K., Donnelly, A., & MacIntyre, T. E. (2024). Air Pollution Effects on Mental Health Relationships: Scoping Review on Historically Used Methodologies to Analyze Adult Populations. Air, 2(3), 258-291. https://doi.org/10.3390/air2030016






