Role and Function of Receptor Tyrosine Kinases in BRAF Mutant Cancers
Abstract
1. Introduction
2. Receptor Tyrosine Kinases and Ras/MAPK/ERK Signaling
3. Receptor Tyrosine Kinases in BRAF Mutant Cancers
3.1. EGFR, HER2, and HER3 (ErbB Receptors)
3.1.1. ErbB Receptors, Kinase Inhibitors, Main Mechanisms, and Targets
3.1.2. Additional Mechanisms and Factors of EGFR-Mediated BRAF Inhibitor Resistance
3.1.3. Clinical Trials of EGFR Inhibitors in BRAF Mutant Cancers and Adjuvant Molecules
3.2. VEGFR and BRAF Mutant Cancers
3.2.1. VEGFRs, Inhibitors, and Mechanisms
3.2.2. Additional Mechanisms and Factors of VEGFR-Mediated BRAF Inhibitor Resistance
3.2.3. Clinical Trials of VEGFR Inhibitors in BRAF Mutant Cancers
3.3. PDGFR and KIT in BRAF Mutant Cancers
3.3.1. PDGFRs and KIT Receptors, Inhibitors, and Mechanisms
3.3.2. Clinical Trials of PDGFR and KIT Inhibitors in BRAF Mutant Cancers
3.4. FGFR in BRAF Mutant Cancers
3.5. MET Kinase/HGFR in BRAF Mutant Cancers
3.6. IGFRs in BRAF Mutant Cancers
3.7. Other RTKs and BRAF Mutant Cancers
3.7.1. AXL and MERTK
3.7.2. ALK
3.7.3. DDR
3.7.4. EphA2
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Halle, B.R.; Johnson, D.B. Defining and targeting BRAF mutations in solid tumors. Curr. Treat. Options Oncol. 2021, 22, 30. [Google Scholar] [CrossRef]
- Pearson, G.; Robinson, F.; Gibson, T.B.; Xu, B.E.; Karandikar, M.; Berman, K.; Cobb, M.H. Mitogen-activated protein (MAP) kinase pathways. Endocr. Rev. 2001, 22, 153–183. [Google Scholar]
- Rushworth, L.K.; Hindley, A.D.; O’Neill, E.; Kolch, W. Regulation and role of Raf-1/B-Raf heterodimerization. Mol. Cell. Biol. 2006, 26, 2262–2272. [Google Scholar] [CrossRef] [PubMed]
- Wee, P.; Wang, Z. Epidermal growth factor receptor cell proliferation signaling pathways. Cancers 2017, 9, 52. [Google Scholar] [CrossRef]
- Freudlsperger, C.; Burnett, J.R.; Friedman, J.A.; Kannabiran, V.R.; Chen, Z.; van Waes, C. EGFR-PI3K-AKT-mTOR signaling in head and neck squamous cell carcinomas: Attractive targets for molecular-oriented therapy. Expert Opin. Ther. Targets 2011, 15, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Zhong, J.; Yan, W.; Wang, C.; Liu, W.; Lin, X.; Zou, Z.; Sun, W.; Chen, Y. BRAF inhibitor resistance in melanoma: Mechanisms and alternative therapeutic strategies. Curr. Treat. Options Oncol. 2022, 23, 1503–1521. [Google Scholar] [CrossRef] [PubMed]
- Santarpia, L.; Lippman, S.M.; El-Naggar, A.K. Targeting the MAPK-RAS-RAF signaling pathway in cancer therapy. Expert Opin. Ther. Targets 2012, 16, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Lovly, C.M.; Dahlman, K.B.; Fohn, L.E.; Su, Z.; Dias-Santagata, D.; Hicks, D.J.; Hucks, D.; Berry, E.; Terry, C.; Duke, M.; et al. Routine multiplex mutational profiling of melanomas enables enrollment in genotype-driven therapeutic trials. PLoS ONE 2012, 7, e35309. [Google Scholar] [CrossRef]
- Rubinstein, J.C.; Sznol, M.; Pavlick, A.C.; Ariyan, S.; Cheng, E.; Bacchiocchi, A.; Kluger, H.M.; Narayan, D.; Halaban, R. Incidence of the V600K mutation among melanoma patients with BRAF mutations, and potential therapeutic response to the specific BRAF inhibitor PLX4032. J. Transl. Med. 2010, 8, 67. [Google Scholar] [CrossRef]
- Dankner, M.; Rose, A.A.N.; Rajkumar, S.; Siegel, P.M.; Watson, I.R. Classifying BRAF alterations in cancer: New rational therapeutic strategies for actionable mutations. Oncogene 2018, 37, 3183–3199. [Google Scholar] [CrossRef]
- Flaherty, K.T. BRAF inhibitors and melanoma. Cancer J. 2011, 17, 505–511. [Google Scholar] [CrossRef]
- Holderfield, M.; Deuker, M.M.; McCormick, F.; McMahon, M. Targeting RAF kinases for cancer therapy: BRAF-mutated melanoma and beyond. Nat. Rev. Cancer 2014, 14, 455–467. [Google Scholar] [CrossRef] [PubMed]
- Grothey, A.; Fakih, M.; Tabernero, J. Management of BRAF-mutant metastatic colorectal cancer: A review of treatment options and evidence-based guidelines. Ann. Oncol. 2021, 32, 959–967. [Google Scholar] [CrossRef] [PubMed]
- Long, G.V.; Stroyakovskiy, D.; Gogas, H.; Levchenko, E.; de Braud, F.; Larkin, J.; Garbe, C.; Jouary, T.; Hauschild, A.; Grob, J.J.; et al. Combined BRAF and MEK inhibition versus BRAF inhibition alone in melanoma. N. Engl. J. Med. 2014, 371, 1877–1888. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.M.; Esmail, A.; Abdelrahim, M. Triple-regimen of verumafenib, irinotecan, and cetuximab for the treatment of BRAFV600E-mutant CRC: A case report and review. Front. Pharmacol. 2021, 12, 795381. [Google Scholar] [CrossRef]
- Eriksen, M.; Pfeiffer, P.; Rohrberg, K.S.; Yde, C.W.; Petersen, L.N.; Poulsen, L.O.; Qvortrup, C. A phase II study of daily encorafenib in combination with biweekly cetuximab in patients with BRAF V600E mutated metastatic colorectal cancer: The NEW BEACON study. BMC Cancer 2022, 22, 1321. [Google Scholar] [CrossRef]
- Yao, Z.; Yaeger, R.; Rodrik-Outmezguine, V.S.; Tao, A.; Torres, N.M.; Chang, M.T.; Drosten, M.; Zhao, H.; Cecchi, F.; Hembrough, T.; et al. Tumours with class 3 BRAF mutants are sensitive to the inhibition of activated RAS. Nature 2017, 548, 234–238. [Google Scholar] [CrossRef]
- Huang, L.; Fu, L. Mechanisms of resistance to EGFR tyrosine kinase inhibitors. Acta Pharm. Sin. B 2015, 5, 390–401. [Google Scholar] [CrossRef]
- Sale, M.J.; Balmanno, K.; Cook, S.J. Resistance to ERK1/2 pathway inhibitors; sweet spots, fitness deficits and drug addiction. Cancer Drug Resist. 2019, 2, 365–380. [Google Scholar] [CrossRef]
- Saraon, P.; Pathmanathan, S.; Snider, J.; Lyakisheva, A.; Wong, V.; Stagljar, I. Receptor tyrosine kinases and cancer: Oncogenic mechanisms and therapeutic approaches. Oncogene 2021, 40, 4079–4093. [Google Scholar] [CrossRef]
- Lemmon, M.A.; Schlessinger, J. Cell signaling by receptor tyrosine kinases. Cell 2010, 141, 1117–1134. [Google Scholar] [CrossRef]
- Wheeler, D.L.; Yarden, Y. Receptor Tyrosine Kinases: Family and Subfamilies; Springer: New York, NY, USA, 2015. [Google Scholar]
- Mohammadi, M.; Schlessinger, J.; Hubbard, S.R. Structure of the FGF receptor tyrosine kinase domain reveals a novel autoinhibitory mechanism. Cell 1996, 86, 577–587. [Google Scholar] [CrossRef]
- Niu, X.L.; Peters, K.G.; Kontos, C.D. Deletion of the carboxyl terminus of Tie2 enhances kinase activity, signaling, and function. Evidence for an autoinhibitory mechanism. J. Biol. Chem. 2002, 277, 31768–31773. [Google Scholar] [CrossRef]
- Till, J.H.; Becerra, M.; Watty, A.; Lu, Y.; Ma, Y.; Neubert, T.A.; Burden, S.J.; Hubbard, S.R. Crystal structure of the MuSK tyrosine kinase: Insights into receptor autoregulation. Structure 2002, 10, 1187–1196. [Google Scholar] [CrossRef] [PubMed]
- Du, Z.; Lovly, C.M. Mechanisms of receptor tyrosine kinase activation in cancer. Mol. Cancer 2018, 17, 58. [Google Scholar] [CrossRef] [PubMed]
- Weigand, M.; Hantel, P.; Kreienberg, R.; Waltenberger, J. Autocrine vascular endothelial growth factor signalling in breast cancer. Evidence from cell lines and primary breast cancer cultures in vitro. Angiogenesis 2005, 8, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.; Snyder, D.S.; Chu, P.; Gaal, K.K.; Chang, K.L.; Weiss, L.M. PDGFRA rearrangement leading to hyper-eosinophilia, T-lymphoblastic lymphoma, myeloproliferative neoplasm and precursor B-cell acute lymphoblastic leukemia. Leukemia 2011, 25, 371–375. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Longo, P.A.; Tarrant, M.K.; Kim, K.; Head, S.; Leahy, D.J.; Cole, P.A. Mechanistic insights into the activation of oncogenic forms of EGF receptor. Nat. Struct. Mol. Biol. 2011, 18, 1388–1393. [Google Scholar] [CrossRef] [PubMed]
- Ha, S.Y.; Lee, J.; Kang, S.Y.; Do, I.G.; Ahn, S.; Park, J.O.; Kang, W.K.; Choi, M.-G.; Sohn, T.S.; Bae, J.M.; et al. MET overexpression assessed by new interpretation method predicts gene amplification and poor survival in advanced gastric carcinomas. Mod. Pathol. 2013, 26, 1632–1641. [Google Scholar] [CrossRef]
- Gallant, J.N.; Sheehan, J.H.; Shaver, T.M.; Bailey, M.; Lipson, D.; Chandramohan, R.; Brewer, M.R.; York, S.J.; Kris, M.G.; Pietenpol, J.A.; et al. EGFR kinase domain duplication (EGFR-KDD) is a novel oncogenic driver in lung cancer that is clinically responsive to afatinib. Cancer Discov. 2015, 5, 1155–1163. [Google Scholar] [CrossRef]
- Casaletto, J.B.; McClatchey, A.I. Spatial regulation of receptor tyrosine kinases in development and cancer. Nat. Rev. Cancer 2012, 12, 387–400. [Google Scholar] [CrossRef]
- Chan, B.A.; Hughes, B.G. Targeted therapy for non-small cell lung cancer: Current standards and the promise of the future. Transl. Lung Cancer Res. 2014, 4, 36–54. [Google Scholar]
- Lin, Y.; Wang, X.; Jin, H. EGFR-TKI resistance in NSCLC patients: Mechanisms and strategies. Am. J. Cancer Res. 2014, 4, 411–435. [Google Scholar] [PubMed]
- Simasi, J.; Schubert, A.; Oelkrug, C.; Gillissen, A.; Nieber, K. Primary and secondary resistance to tyrosine kinase inhibitors in lung cancer. Anticancer Res. 2014, 34, 2841–2850. [Google Scholar] [PubMed]
- Lai, C.-J.; Bao, R.; Tao, X.; Wang, J.; Atoyan, R.; Qu, H.; Wang, D.-G.; Yin, L.; Samson, M.; Forrester, J.; et al. CUDC-101. A multitargeted inhibitor of histone deacetylase, epidermal growth factor receptor, and human epidermal growth factor receptor 2, exerts potent anticancer activity. Cancer Res. 2010, 70, 3647–3656. [Google Scholar] [CrossRef] [PubMed]
- Biersack, B.; Polat, S.; Höpfner, M. Anticancer properties of chimeric HDAC and kinase inhibitors. Semin. Cancer Biol. 2022, 83, 472–486. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.; Liu, X.; Zeng, Y.; Liu, J.; Wu, F. DNA methyltransferase inhibitors combination therapy for the treatment of solid tumor: Mechanism and clinical application. Clin. Epigenet. 2021, 13, 166. [Google Scholar] [CrossRef] [PubMed]
- Wittinghofer, A.; Waldmann, H. Ras—A molecular switch in tumor formation. Angew. Chem. Int. Ed. 2000, 39, 4192–4214. [Google Scholar] [CrossRef]
- Krauss, G. Biochemistry of Signal Transduction and Regulation, 2nd ed.; Wiley-VCH: Weinheim, Germany, 2001. [Google Scholar]
- Jung, D.; Bachmann, H.S. Regulation of protein prenylation. Biomed. Pharmacother. 2023, 164, 114915. [Google Scholar] [CrossRef]
- Mazieres, J.; Pradines, A.; Favre, G. Perspectives on farnesyl transferase inhibitors in cancer therapy. Cancer Lett. 2004, 206, 159–167. [Google Scholar] [CrossRef]
- Marchwicka, A.; Kaminska, D.; Monirialamdari, M.; Błazewska, K.M.; Gendaszewska-Darmach, E. Protein prenyltransferases and their inhibitors: Structural and functional characterization. Int. J. Mol. Sci. 2022, 23, 5424. [Google Scholar] [CrossRef] [PubMed]
- Mörchen, B.; Shkura, O.; Stoll, R.; Helfrich, I. Targeting the “undruggable” RAS—New strategies—New hope? Cancer Drug Resist. 2019, 2, 813–826. [Google Scholar] [CrossRef]
- Davies, H.; Bignell, G.R.; Cox, C.; Stephens, P.; Edkins, S.; Clegg, S.; Teague, J.; Woffendin, H.; Garnett, M.J.; Bottomley, W.; et al. Mutations of the BRAF gene in human cancer. Nature 2002, 417, 949–954. [Google Scholar] [CrossRef]
- Pratilas, C.A.; Solit, D.B. Targeting the mitogen-activated protein kinase pathway: Physiological feedback and drug response. Clin. Cancer Res. 2010, 16, 3329–3334. [Google Scholar] [CrossRef] [PubMed]
- Yaeger, R.; Corcoran, R.B. Targeting alterations in the RAF-MEK pathway. Cancer Discov. 2019, 9, 329–341. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Liu, S.; Zhang, G.; Kwong, L.N.; Zhu, Y.; Miller, J.P.; Hu, Y.; Zhong, W.; Zeng, J.; Wu, L.; et al. Oncogenic BRAF-mediated melanoma cell invasion. Cell Rep. 2016, 15, 2012–2024. [Google Scholar] [CrossRef] [PubMed]
- Houles, T.; Gravel, S.P.; Lavoie, G.; Shin, S.; Savall, M.; Méant, A.; Grondin, B.; Gaboury, L.; Yoon, S.-O.; St-Pierre, J.; et al. RSK regulates PFK-2 activity to promote metabolic rewiring in melanoma. Cancer Res. 2018, 78, 2191–2204. [Google Scholar] [CrossRef] [PubMed]
- Wilhelm, S.; Carter, C.; Lynch, M.; Lowinger, T.; Dumas, J.; Smith, R.A.; Schwartz, B.; Simantov, R.; Kelley, S. Discovery and development of sorafenib: A multikinase inhibitor for treating cancer. Nat. Rev. Drug Discov. 2006, 5, 835–844. [Google Scholar] [CrossRef]
- Swaika, A.; Crozier, J.A.; Joseph, R.W. Vemurafenib: An evidence-based review of its clinical utility in the treatment of metastatic melanoma. Drug Des. Develop. Ther. 2014, 8, 775–787. [Google Scholar]
- Dummer, R.; Goldinger, S.M.; Turtschi, C.P.; Eggmann, N.B.; Michielin, O.; Mitchell, L.; Veronese, L.; Hilfiker, P.R.; Felderer, L.; Rinderknecht, J.D. Vemurafenib in patients with BRAF(V600) mutation-positive melanoma with symptomatic brain metastases: Final results of an open-label pilot study. Eur. J. Cancer 2014, 50, 611–621. [Google Scholar] [CrossRef]
- Singh, A.K.; Sonawane, P.; Kumar, A.; Singh, H.; Naumovich, V.; Pathak, P.; Grishina, M.; Khalilullah, H.; Jaremko, M.; Emwas, A.-H.; et al. Challenges and opportunities in the crusade of BRAF inhibitors: From 2002 to 2022. ACS Omega 2023, 8, 27819–27844. [Google Scholar] [CrossRef]
- McGettigan, S. Dabrafenib: A new therapy for use in BRAF-mutant metastatic melanoma. J. Adv. Pract. Oncol. 2014, 5, 211–215. [Google Scholar]
- Robert, C.; Grob, J.J.; Stroyakovskiy, D.; Karaszewska, B.; Hauschild, A.; Levchenko, E.; Sileni, V.C.; Schachter, J.; Garbe, C.; Bondarenko, I.; et al. Five-year outcomes with dabrafenib plus trametinib in metastatic melanoma. N. Engl. J. Med. 2019, 381, 626–636. [Google Scholar] [CrossRef]
- Trojaniello, C.; Festino, L.; Vanella, V.; Ascierto, P.A. Encorafenib in combination with binimetinib for unresectable or metastatic melanoma with BRAF mutations. Expert Rev. Clin. Pharmacol. 2019, 12, 259–266. [Google Scholar] [CrossRef]
- Tian, Y.; Guo, W. A review of the molecular pathways involved in resistance to BRAF inhibitors in patients with advanced-stage melanoma. Med. Sci. Monit. 2020, 26, e920957. [Google Scholar] [CrossRef] [PubMed]
- Grassilli, E.; Cerrito, M.G. Emerging actionable targets to treat therapy-resistant colorectal cancers. Cancer Drug Resist. 2022, 5, 36–63. [Google Scholar] [CrossRef] [PubMed]
- Herbst, R.S. Review of epidermal growth factor receptor biology. Int. J. Radiat. Oncol. Biol. Phys. 2004, 59, S21–S26. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Abbas, A.; Aster, J. Robbins Basic Pathology; Elsevier/Saunders: Philadelphia, PA, USA, 2013; p. 179. [Google Scholar]
- Prenzel, N.; Fischer, O.M.; Streit, S.; Hart, S.; Ullrich, A. The epidermal growth factor receptor family as a central element for cellular signal transduction and diversification. Endocr. Relat. Cancer 2001, 8, 11–31. [Google Scholar] [CrossRef]
- Schlam, I.; Swain, S.M. HER2-positive breast cancer and tyrosine kinase inhibitors: The time is now. NPJ Breast Cancer 2021, 7, 56. [Google Scholar] [CrossRef]
- Johnson, G.L.; Stuhlmiller, T.J.; Angus, S.P.; Zawistowski, J.S.; Graves, L.M. Molecular pathways: Adaptive kinome reprogramming in response to targeted inhibition of the BRAF-MEK-ERK pathway in cancer. Clin. Cancer Res. 2014, 20, 2516–2522. [Google Scholar] [CrossRef]
- Kim, S.; Carvajal, R.; Kim, M.; Yang, H.W. Kinetics of RTK activation determine ERK reactivation and resistance to dual BRAF/MEK inhibition in melanoma. Cell Rep. 2023, 42, 112570. [Google Scholar] [CrossRef]
- Corcoran, R.B.; Ebi, H.; Turke, A.B.; Coffee, E.M.; Nishino, M.; Cogdill, A.P.; Brown, R.D.; Della Pelle, P.; Dias-Santagata, D.; Hung, K.E.; et al. EGFR-mediated re-activation of MAPK signaling contributes to insensitivity of BRAF mutant colorectal cancers to RAF inhibition with vemurafenib. Cancer Discov. 2012, 2, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Held, M.A.; Langdon, C.G.; Platt, J.T.; Graham-Steed, T.; Liu, Z.; Chakraborty, A.; Bacchiocchi, A.; Koo, A.; Haskins, J.W.; Bosenberg, M.W.; et al. Genotype-selective combination therapies for melanoma identified by high-throughput drug screening. Cancer Discov. 2013, 3, 52–67. [Google Scholar] [CrossRef] [PubMed]
- Kennessey, I.; Kramer, Z.; István, L.; Cserepes, M.T.; Garay, T.; Hegedüs, B.; Dobos, J.; Tímár, J.; Tóvári, J. Inhibition of epidermal growth factor receptor improves antitumor efficacy of vemurafenib in BRAF-mutant human melanoma in preclinical model. Melanoma Res. 2018, 28, 536–546. [Google Scholar] [CrossRef] [PubMed]
- Oddo, D.; Sennott, E.M.; Barault, L.; Valtorta, E.; Arena, S.; Cassingena, A.; Filiciotto, G.; Marzolla, G.; Elez, E.; van Geel, R.M.J.M.; et al. Molecular landscape of acquired resistance to targeted therapy combinations in BRAF mutant colorectal cancer. Cancer Res. 2016, 76, 4504–4515. [Google Scholar] [CrossRef] [PubMed]
- Tiedt, R.; King, F.J.; Stamm, C.; Niederst, M.J.; Delach, S.; Zumstein-Mecker, S.; Meltzer, J.; Mulford, I.J.; Labrot, E.; Schacher Engstler, B.; et al. Integrated CRISPR screening and drug profiling identifies combination opportunities for EGFR, ALK, and BRAF/MEK inhibitors. Cell Rep. 2023, 42, 112297. [Google Scholar] [CrossRef]
- Molnár, E.; Garay, T.; Donia, M.; Baranyi, M.; Rittler, D.; Berger, W.; Timár, J.; Grusch, M.; Hegedüs, B. Long-term vemurafenib exposure induced alterations of cell phenotypes in melanoma: Increased cell migration and its association with EGFR expression. Int. J. Mol. Sci. 2019, 20, 4484. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Jin, J.; Guo, D.; Tao, Z.; Hu, X. Immune checkpoint inhibitors combined with targeted therapy: The recent advances and future potentials. Cancers 2023, 15, 2858. [Google Scholar] [CrossRef]
- Dugo, M.; Nicolini, G.; Tragni, G.; Bersani, I.; Tomassetti, A.; Colonna, V.; Del Vecchio, M.; De Braud, F.; Canevari, S.; Anichini, A.; et al. A melanoma subtype with intrinsic resistance to BRAF inhibition identified by receptor tyrosine kinase gene-driven classification. Oncotarget 2015, 6, 5118–5133. [Google Scholar] [CrossRef]
- Fukushima, H.; Iwata, Y.; Saito, K.; Sugiura, K. Successful rechallenge therapy for BRAF/MEK inhibitor resistant multiple brain metastases of melanoma. J. Dermatol. 2021, 48, 1291–1295. [Google Scholar] [CrossRef]
- Baur, F.; Nietzer, S.L.; Kunz, M.; Saal, F.; Jeromin, J.; Matschos, S.; Linnebacher, M.; Walles, H.; Dandekar, T.; Dandekar, G. Connecting cancer pathways to tumor engines: A stratification tool for colorectal cancer combining human in vitro tissue models with Boolean in silico models. Cancers 2020, 12, 28. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Huang, S.K.; Marzese, D.M.; Hsu, S.C.; Kawas, N.P.; Chong, K.K.; Long, G.V.; Menzies, A.M.; Scolyer, R.A.; Izraely, S.; et al. Epigenetic changes of EGFR have an important role in BRAF inhibitor-resistant cutaneous melanomas. J. Investig. Dermatol. 2015, 135, 532–541. [Google Scholar] [CrossRef] [PubMed]
- Song, Q.; Sun, X.; Guo, H.; Yu, Q. Concomitant inhibition of receptor tyrosine kinases and downstream AKT synergistically inhibited growth of KRAS/BRAF mutant colorectal cancer cells. Oncotarget 2017, 8, 5003–5015. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cheng, L.; Jin, Y.; Liu, M.; Ruan, M.; Chen, L. HER inhibitor promotes BRAF/MEK inhibitor-induced redifferentiation in papillary thyroid cancer harboring BRAFV600E. Oncotarget 2017, 8, 19843–19854. [Google Scholar] [CrossRef] [PubMed]
- Miele, E.; Abballe, L.; Spinelli, G.P.; Besharat, Z.M.; Catanzaro, G.; Chiacchiarini, M.; Vacca, A.; Po, A.; Capalbo, C.; Ferretti, E. BRAF mutant colorectal cancer: ErbB2 expression levels as predictive factor for the response to combined BRAF/ErbB inhibitors. BMC Cancer 2020, 20, 129. [Google Scholar] [CrossRef] [PubMed]
- Dent, P.; Booth, L.; Poklepovic, A.; Kirkwood, J.M. Neratinib kills B-RAF V600E melanoma via ROS-dependent autophagosome formation and death receptor signaling. Pigment Cell Melanoma Res. 2022, 35, 66–77. [Google Scholar] [CrossRef] [PubMed]
- Ng, Y.-K.; Lee, J.-Y.; Supko, K.M.; Khan, A.; Torres, S.M.; Berwick, M.; Ho, J.; Kirkwood, J.M.; Siegfried, J.M.; Stabile, L.P. Pan-erbB inhibition potentiates BRAF inhibitors for melanoma treatment. Melanoma Res. 2014, 24, 207–218. [Google Scholar] [CrossRef]
- Cronise, K.E.; Hernandez, B.G.; Gustafson, D.L.; Duval, D.L. Identifying the ErbB/MAPK signaling cascade as a therapeutic target in canine bladder cancer. Mol. Pharmacol. 2019, 96, 36–46. [Google Scholar] [CrossRef]
- Okimoto, R.A.; Lin, L.; Olivas, V.; Chan, E.; Markegard, E.; Rymar, A.; Neel, D.; Chen, X.; Hemmati, G.; Bollag, G.; et al. Preclinical efficacy of a RAF inhibitor that evades paradoxical MAPK pathway activation in protein kinase BRAF-mutant lung cancer. Proc. Natl. Acad. Sci. USA 2016, 113, 13456–13461. [Google Scholar] [CrossRef]
- Tang, Z.; Yuan, X.; Du, R.; Cheung, S.-H.; Zhang, G.; Wei, J.; Zhao, Y.; Feng, Y.; Peng, Y.; Zhang, Y.; et al. BGB-283, a novel RAF kinase and EGFR inhibitor, displays potent antitumor activity in BRAF-mutated colorectal cancers. Mol. Cancer Ther. 2015, 14, 2187–2197. [Google Scholar] [CrossRef] [PubMed]
- Kotani, H.; Adachi, Y.; Kitai, H.; Tomida, S.; Bando, H.; Faber, A.C.; Yoshino, T.; Voon, D.C.; Yano, S.; Ebi, H. Distinct dependencies on receptor tyrosine kinases in the regulation of MAPK signaling between BRAF V600E and non-V600E mutant lung cancers. Oncogene 2018, 37, 1775–1787. [Google Scholar] [CrossRef]
- Desai, J.; Gan, H.; Barrow, C.; Jameson, M.; Atkinson, V.; Haydon, A.; Millward, M.; Begbie, S.; Brown, M.; Markman, B.; et al. Phase I, open-label, dose-escalation/dose-expansion study of lifirafenib (BGB-283), an RAF family kinase inhibitor, in patients with solid tumors. J. Clin. Oncol. 2020, 38, 2140–2150. [Google Scholar] [CrossRef]
- Yuan, X.; Tang, Z.; Du, R.; Yao, Z.; Cheung, S.-H.; Zhang, X.; Wie, J.; Zhao, Y.; Du, Y.; Liu, Y.; et al. RAF dimer inhibition enhances the antitumor activity of MEK inhibitors in KRAS mutant tumors. Mol. Oncol. 2020, 14, 1833–1849. [Google Scholar] [CrossRef] [PubMed]
- Aboubakar Nana, F.; Ocak, S. Targeting BRAF activation as acquired resistance mechanism to EGFR tyrosine kinase inhibitors in EGFR-mutant non-small-cell lung cancer. Pharmaceutics 2021, 13, 1478. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, M.F.S.A.; Knebel, F.H.; Bettoni, F.; Saddi, R.; Sacardo, K.P.; Canedo, F.S.N.A.; Alessi, J.V.M.; Shimada, A.K.; Marin, J.F.G.; Camargo, A.A.; et al. Impressive response to dabrafenib, trametinib, and osimertinib in a metastatic EGFT-mutant/BRAF V600E lung adenocarcinoma patient. NPJ Precis. Oncol. 2021, 5, 5. [Google Scholar] [CrossRef] [PubMed]
- Zeng, R.; Luo, L.; Sun, X.; Bao, Z.; Du, W.; Dai, R.; Tang, W.; Gao, B.; Xiang, Y. EGFR/BRAF/MEK co-inhibition for EGFR-mutated lung adenocarcinoma patients with an acquired BRAFV600E mutation: A case report and review of literature. Cancer Drug Resist. 2021, 4, 1019–1027. [Google Scholar] [CrossRef] [PubMed]
- Orciulo, C.; Cappuzzo, F.; Landi, L.; Resuli, B.; Carpano, S.; Vidiri, A.; Buglioni, S.; Mandoj, C.; Ciliberto, G.; Minuti, G. Pretreated EGFRdel19/BRAFV600E lung adenocarcinoma with leptomeningeal disease achieving long-lasting disease control on osimertinib, dabrafenib, and trametinib: A case report. JTO Clin. Res. Rep. 2023, 4, 100545. [Google Scholar]
- Leduc, C.; Merlio, J.P.; Besse, B.; Blons, H.; Debieuvre, D.; Bringuier, P.P.; Monnet, I.; Rouquette, I.; Fraboulet-Moreau, S.; Lemoine, A.; et al. Clinical and molecular characteristics of non-small-cell lung cancer (NSCLC) harboring EGFR mutation: Results of the nationwide French Cooperative Intergroup (IFCT) program. Ann. Oncol. 2017, 28, 2715–2724. [Google Scholar] [CrossRef]
- Kong, W.-M.; Guo, Y.-J.; Ma, J.; Shi, C. BTN2A1-BRAF fusion may be a novel mechanism of resistance to osimertinib in lung adenocarcinoma: A case report. Transl. Cancer Res. 2023, 12, 186–193. [Google Scholar] [CrossRef]
- Kirkpatrick, P.; Graham, J.; Muhsin, M. Cetuximab. Nat. Rev. Drug Discov. 2004, 3, 549–550. [Google Scholar] [CrossRef]
- Kong, L.; Zhang, Q.; Mao, J.; Cheng, L.; Shi, X.; Yu, L.; Hu, J.; Yang, M.; Li, L.; Liu, B.; et al. A dual-targeted molecular therapy of PP242 and cetuximab plays an anti-tumor effect through EGFR downstream signaling pathways in colorectal cancer. J. Gastrointest. Oncol. 2021, 12, 1625–1642. [Google Scholar] [CrossRef] [PubMed]
- Veluchamy, J.P.; Spanholtz, J.; Tordoir, M.; Thijssen, V.L.; Heideman, D.A.M.; Verheul, H.M.W.; de Gruijl, T.D.; van der Vliet, H.J. Combination of NK cells and cetuximab to enhance anti-tumor responses in RAS mutant metastatic colorectal cancer. PLoS ONE 2016, 11, e0157830. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Huang, M.; Gong, Y.; Lin, C.; Guo, W. BRAF and EGFR inhibitors synergize to increase cytotoxic effects and decrease stem cell capacities in BRAF(V600E)-mutant colorectal cancer cells. Acta Biochim. Biophys. Sin. 2018, 50, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Chung, Y.-C.; Chiu, H.-H.; Wei, W.-C.; Chang, K.-J.; Chao, W.-T. Application of trastuzumab emtansine in HER-2-positive and KRAS/BRAF-mutated colon cancer cells. Eur. J. Clin. Investig. 2020, 29, e13255. [Google Scholar] [CrossRef] [PubMed]
- Tchekmedyian, V.; Dunn, L.; Sherman, E.; Baxi, S.S.; Grewal, R.K.; Larson, S.M.; Pentlow, K.S.; Haque, S.; Tuttle, R.M.; Sabra, M.M.; et al. Enhancing radioiodine incorporation in BRAF-mutant, radioiodine-refractory thyroid cancers with vemurafenib and the anti-ErbB3 monoclonal antibody CDX-3379: Results of a pilot clinical trial. Thyroid 2022, 32, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Roller, D.G.; Capaldo, B.; Bekiranov, S.; Mackey, A.J.; Conaway, M.R.; Petricoin, E.F.; Gioeli, D.; Weber, M.J. Combinatorial drug screening and molecular profiling reveal diverse mechanisms of intrinsic and adaptive resistance to BRAF inhibition in V600E BRAF mutant melanomas. Oncotarget 2015, 7, 2734–2753. [Google Scholar] [CrossRef] [PubMed]
- Ma, W.; Tian, M.; Hu, L.; Ruan, X.; Zhang, W.; Zheng, X.; Gao, M. Early combined SHP2 targeting reverses the therapeutic resistance of vemurafenib in thyroid cancer. J. Cancer 2023, 14, 1592–1604. [Google Scholar] [CrossRef]
- Invrea, F.; Punzi, S.; Petti, C.; Minelli, R.; Peoples, M.D.; Bristow, C.A.; Vurchio, V.; Corrado, A.; Bragoni, A.; Marchiò, C.; et al. Synthetic lethality screening highlights colorectal cancer vulnerability to concomitant blockade of NEDD8 and EGFR pathways. Cancers 2021, 13, 3805. [Google Scholar] [CrossRef]
- Forsythe, N.; Refaat, A.; Javadi, A.; Khawaja, H.; Weir, J.-A.; Emam, H.; Allen, W.L.; Burkamp, F.; Popovici, V.; Jithesh, P.V.; et al. The unfolded protein response: A novel therapeutic target for poor prognostic BRAF mutant colorectal cancer. Mol. Cancer Ther. 2018, 17, 1280–1290. [Google Scholar] [CrossRef]
- Delgado-Goni, T.; Galobart, T.C.; Wantuch, S.; Normantaite, D.; Leach, M.O.; Whittaker, S.R.; Beloueche-Babari, M. Increased inflammatory lipid metabolism and anaplerotic mitochondrial activation follow acquired resistance to vemurafenib in BRAF-mutant melanoma cells. Br. J. Cancer 2020, 122, 72–81. [Google Scholar] [CrossRef]
- Girotti, M.R.; Pedersen, M.; Sanchez-Laorden, B.; Viros, A.; Turajilic, S.; Niculescu-Duvaz, D.; Zambon, A.; Sinclair, J.; Hayes, A.; Gore, M.; et al. Inhibiting EGF receptor or SRC family kinase signaling overcomes BRAF inhibitor resistance in melanoma. Cancer Discov. 2013, 3, 158–167. [Google Scholar] [CrossRef]
- Lin, L.; Sabnis, A.J.; Chan, E.; Olivas, V.; Cade, L.; Pazarentzos, E.; Asthana, S.; Neel, D.; Yan, J.J.; Lu, X.; et al. The Hippo effector YAP promotes resistance to RAF- and MEK-targeted cancer therapies. Nat. Genet. 2015, 47, 250–256. [Google Scholar] [CrossRef]
- Garcia-Rendueles, M.E.R.; Krishnamoorthy, G.; Saqcena, M.; Acuna-Ruiz, A.; Revilla, G.; de Stanchina, E.; Knauf, J.A.; Lester, R.; Xu, B.; Ghossein, R.A.; et al. Yap governs a lineage-specific neuregulin1 pathway-driven adaptive resistance to RAF kinase inhibitors. Mol. Cancer 2022, 21, 213. [Google Scholar] [CrossRef] [PubMed]
- Shao, D.D.; Xue, W.; Krall, E.B.; Bhutkar, A.; Piccioni, F.; Wang, X.; Schinzel, A.C.; Sood, S.; Rosenbluh, J.; Kim, J.W.; et al. KRAS and YAP1 converge to regulate EMT and tumor survival. Cells 2014, 158, 171–184. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Chen, W.; Zhang, X.; Hu, L.; Tang, G.; Kong, J.; Wang, Z. E26 transformation (ETS)-specific related transcription factor-3 (ELF3) orchestrates a positive feedback loop that constitutively activates the MAPK/Erk pathway to drive thyroid cancer. Oncol. Rep. 2019, 41, 570–578. [Google Scholar] [CrossRef]
- Sun, C.; Wang, L.; Huang, S.; Heynen, G.J.J.E.; Prahallad, A.; Robert, C.; Haanen, J.; Blank, C.; Wesseling, J.; Willems, S.M.; et al. Reversible and adaptive resistance to BRAF(V600E) inhibition in melanoma. Nature 2014, 508, 118–122. [Google Scholar] [CrossRef] [PubMed]
- Abel, E.V.; Basile, K.J.; Kugel III, C.H.; Witkiewicz, A.K.; Le, K.; Amaravadi, R.K.; Karakousis, G.C.; Xu, X.; Lu, W.; Schuchter, L.M.; et al. Melanoma adapts to RAF/MEK inhibitors through FOXD3-mediated upregulation of ERBB3. J. Clin. Investig. 2013, 123, 2155–2168. [Google Scholar] [CrossRef] [PubMed]
- Herr, R.; Halbach, S.; Heizmann, M.; Busch, H.; Boerries, M.; Brummer, T. BRAF inhibition upregulates a variety of receptor tyrosine kinases and their downstream effector Gab2 in colorectal cancer cell lines. Oncogene 2018, 37, 1576–1593. [Google Scholar] [CrossRef]
- Dang, H.; Sui, M.; He, Q.; Xie, J.; Liu, Y.; Hou, P.; Ji, M. Pin1 inhibitor API-1 sensitizes BRAF-mutant thyroid cancers to BRAF inhibitors by attenuating HER3-mediated feedback activation of MAPK/ERK and PI3K/AKT pathways. Int. J. Biol. Macromol. 2023, 248, 125867. [Google Scholar] [CrossRef]
- Sun, X.; Li, J.; Sun, Y.; Zhang, Y.; Dong, L.; Shen, C.; Yang, L.; Yang, M.; Li, Y.; Shen, G.; et al. miR-7 reverses the resistance to BRAFi in melanoma by targeting EGFR/IGF-1R/CRAF and inhibiting the MAPK and PI3K/AKT signaling pathways. Oncotarget 2016, 7, 53558–53570. [Google Scholar] [CrossRef]
- Liu, S.; Tetzlaff, M.T.; Wang, T.; Yang, R.; Xie, L.; Zhang, G.; Krepler, C.; Xiao, M.; Beqiri, M.; Xu, W.; et al. miR-200c/Bmi1 axis and epithelial-mesenchymal transition, contribute to acquired resistance to BRAF inhibitor treatment. Pigment Cell Melanoma Res. 2015, 28, 431–441. [Google Scholar] [CrossRef]
- Biersack, B. Interactions between anticancer active platinum complexes and non-coding RNAs/microRNAs. Non-Coding RNA Res. 2017, 2, 1–17. [Google Scholar] [CrossRef]
- Biersack, B. Alkylating anticancer agents and their relations to microRNAs. Cancer Drug Resist. 2019, 2, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Sanz-Garcia, E.; Argiles, G.; Elez, E.; Tabernero, J. BRAF mutant colorectal cancer: Prognosis, treatment, and new perspectives. Ann. Oncol. 2017, 28, 2648–2657. [Google Scholar] [CrossRef] [PubMed]
- Tabernero, J.; Grothey, A.; Van Cutsem, E.; Yaeger, R.; Wasan, H.; Yoshino, T.; Desai, J.; Ciardiello, F.; Loupakis, F.; Hong, Y.S.; et al. Encorafenib plus cetuximab as a new standard of care for previously treated BRAF V600E-mutant metastatic colorectal cancer: Updated survival results and subgroup analyses from the BEACON study. J. Clin. Oncol. 2021, 39, 273–284. [Google Scholar] [CrossRef]
- Tan, L.; Tran, B.; Tie, J.; Markman, B.; Ananda, S.; Tebbutt, N.C.; Michael, M.; Link, E.; Wong, S.Q.; Chandrashekar, S.; et al. A phase Ib/II trial of combined BRAF and EGFR inhibition in BRAF V600E positive metastatic colorectal cancer and other cancers: The EVICT (erlotinib and vemurafenib in combination trial) study. Clin. Cancer Res. 2023, 29, 1017–1030. [Google Scholar] [CrossRef]
- Martini, G.; Ciardiello, D.; Napolitano, S.; Martinelli, E.; Troiani, T.; Latiano, T.P.; Acallone, A.; Normanno, N.; Di Maio, M.; Maiello, E.; et al. Efficacy and safety of a biomarker-driven cetuximab-based treatment regimen over 3 treatment lines in mCRC patients with RAS/BRAF wild type tumors at start of first line: The CAPRI 2 GOIM trial. Front. Oncol. 2023, 13, 1069370. [Google Scholar] [CrossRef]
- Kopetz, S.; Guthrie, K.A.; Morris, V.K.; Lenz, H.-J.; Magliocco, A.M.; Maru, D.; Yan, Y.; Lanman, R.; MAnyam, G.; Hong, D.S.; et al. Randomized trial of irinotecan and cetuximab with or without vemurafenib in BRAF-mutant metastatic colorectal cancer (SWOG S1406). J. Clin. Oncol. 2021, 39, 285–294. [Google Scholar] [CrossRef]
- Xu, Y.; Wang, G.; Zheng, X.; Chang, W.; Fu, J.; Zhang, T.; Lin, Q.; Lv, Y.; Zhu, Z.; Tang, W.; et al. Treatment of metastatic colorectal cancer with BRAF V600E mutation: A multicenter real-world study in China. Eur. J. Surg. Oncol. 2023, 49, 106981. [Google Scholar] [CrossRef] [PubMed]
- Yaeger, R.; Kotani, D.; Mondaca, S.; Parikh, A.; Bando, H.; Van Seventer, E.; Taniguchi, H.; Zhao, H.Y.; Thant, C.; de Stanchina, E.; et al. Response to anti-EGFR therapy in patients with BRAF non-V600 mutant metastatic colorectal cancer. Clin. Cancer Res. 2019, 25, 7089–7097. [Google Scholar] [CrossRef]
- Wang, Y.; Jones, J.C.; Kipp, B.R.; Grothey, A. Activity of EGFR antibody in non-V600 BRAF mutant metastatic colorectal cancer. Ann. Oncol. 2019, 30, 148–149. [Google Scholar] [CrossRef]
- Randon, G.; Intini, R.; Cremolini, C.; Elez, E.; Overman, M.J.; Lee, J.; Manca, P.; Bergamo, F.; Pagani, F.; Antista, M.; et al. Tumour mutational burden predicts resistance to EGFR/BRAF blockade in BRAF-mutated microsatellite stable metastatic colorectal cancer. Eur. J. Cancer 2022, 161, 90–98. [Google Scholar] [CrossRef]
- Dankner, M.; Wang, Y.; Fazelzad, R.; Johnson, B.; Nebhan, C.A.; Dagogo-Jack, I.; Myall, N.J.; Richtig, G.; Bracht, J.W.P.; Gerlinger, M.; et al. Clinical activity of mitogen.activated protein kinase-targeted therapies in patients with non-V600 BRAF-mutant tumors. JCO Precis. Oncol. 2022, 6, e2200107. [Google Scholar] [CrossRef]
- Su, X.; Shen, Z.; Yang, Q.; Sui, F.; Pu, J.; Ma, J.; Ma, S.; Yao, D.; Ji, M.; Hou, P. Vitamin C kills thyroid cancer cells through ROS-dependent inhibition of MAPK/ERK and PI3K/AKT pathways via distinct mechanisms. Theranostics 2019, 9, 4461–4473. [Google Scholar] [CrossRef]
- Farhan, M. Insights on the role of polyphenols in combating cancer drug resistance. Biomedicines 2023, 11, 1709. [Google Scholar] [CrossRef]
- Lev-Ari, S.; Starr, A.; Vexler, A.; Karaush, V.; Loew, V.; Greif, J.; Fenig, E.; Aderka, D.; Ben-Yosef, R. Inhibition of pancreatic and lung adenocarcinoma cell survival by curcumin is associated with increased apoptosis, down-regulation of COX-2 and EGFR and inhibition of Erk1/2 activity. Anticancer Res. 2006, 26, 4423–4430. [Google Scholar]
- Nautiyal, J.; Banerjee, S.; Kanwar, S.S.; Yu, Y.; Patel, B.B.; Sarkar, F.H.; Majumdar, A.P.N. Curcumin enhances dasatinib-induced inhibition of growth and transformation of colon cancer cells. Int. J. Cancer 2011, 128, 951–961. [Google Scholar] [CrossRef]
- Chen, A.; Xu, J.; Johnson, A.C. Curcumin inhibits human colon cancer cell growth by suppressing gene expression of epidermal growth factor receptor through reducing the activity of the transcription factor Egr1. Oncogene 2006, 25, 278–287. [Google Scholar] [CrossRef]
- Chen, A.; Xu, J. Activation of PPAR{gamma} by curcumin inhibits Moser cell growth and mediates suppression of gene expression of cyclin D1 and EGFR. Am. J. Physiol. Gastrointest. Liver Physiol. 2005, 288, G447–G456. [Google Scholar] [CrossRef]
- Kane, A.M.; Liu, C.; Akhter, D.T.; McKeone, D.M.; Bell, C.A.; Thurecht, K.J.; Leggett, B.A.; Whitehall, V.L.J. Curcumin chemoprevention reduces the incidence of Braf mutant colorectal cancer in a preclinical study. Dig. Dis. Sci. 2021, 66, 4326–4332. [Google Scholar] [CrossRef]
- Luo, H.; Umebayashi, M.; Doi, K.; Morisaki, T.; Shirasawa, S.; Tsunoda, T. Resveratrol overcomes cellular resistance to vemurafenib through dephosphorylation of AKT in BRAF-mutant melanoma cells. Anticancer Res. 2016, 36, 3585–3590. [Google Scholar]
- Lu, M.-D.; Li, H.; Nie, J.-H.; Li, S.; Ye, H.-S.; Li, T.-T.; Wu, M.-L.; Liu, J. Dual inhibition of BRAF-MAPK and STAT3 signaling pathways in resveratrol-suppressed anaplastic thyroid cancer cells with BRAF mutations. Int. J. Mol. Sci. 2022, 23, 14385. [Google Scholar] [CrossRef]
- Akiyama, T.; Ishida, J.; Nakagawa, S.; Ogawara, H.; Watanabe, S.; Itoh, N.; Shibuya, M.; Fukami, Y. Genistein, a specific inhibitor of tyrosine-specific protein kinases. J. Biol. Chem. 1987, 262, 5592–5595. [Google Scholar] [CrossRef]
- Chae, H.-S.; Xu, R.; Won, J.-Y.; Chin, Y.-W.; Yim, H. Molecular targets of genistein and its related flavonoids to exert anticancer effects. Int. J. Mol. Sci. 2019, 20, 2420. [Google Scholar] [CrossRef]
- Lazarevic, B.; Boezelijn, G.; Diep, L.M.; Kvernrod, K.; Ogren, O.; Ramberg, H.; Moen, A.; Wessel, N.; Berg, R.E.; Egge-Jacobsen, W.; et al. Efficacy and safety of short-term genistein intervention in patients with localized prostate cancer prior to radical prostatectomy: A randomized, placebo-controlled, double-blind Phase 2 clinical trial. Nutr. Cancer 2011, 63, 889–898. [Google Scholar] [CrossRef]
- Yoon, H.-S.; Ramachandiran, S.; Chacko, M.A.S.; Monks, T.J.; Lau, S.S. Tuberous sclerosis-2 tumor suppressor modulates ERK and B-Raf activity in transformed renal epithelial cells. Am. J. Physiol. Renal Physiol. 2004, 286, F417–F424. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Li, Y.; Yang, G.; Zhang, J.; Tang, P.; Yang, C.; Wang, G.; Chen, J.; Liu, J.; Zhang, L.; Ouyang, L. Discovery, synthesis, and evaluation of highly selective vascular endothelial growth factor receptor 3 (VEGFR3) inhibitor for the potential treatment of metastatic triple-negative breast cancer. J. Med. Chem. 2021, 64, 12022–12048. [Google Scholar] [CrossRef]
- Yang, J.; Yan, J.; Liu, B. Targeting VEGF/VEGFR to modulate antitumor immunity. Front. Immunol. 2018, 9, 978. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Bove, A.M.; Simone, G.; Ma, B. Molecular bases of VEGFR-2-mediated physiological function and pathological role. Front. Cell Dev. Biol. 2020, 8, 599281. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Li, Y.; Wang, Y.; Lin, C.; Zhang, D.; Chen, J.; Ouyang, L.; Wu, F.; Zhang, J.; Chen, L. Recent progress on vascular endothelial growth factor receptor inhibitors with dual targeting capabilities for tumor therapy. J. Hematol. Oncol. 2022, 15, 89. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zou, J.-Y.; Wang, Z.; Wang, Y. Fruquintinib: A novel antivascular endothelial growth factor receptor tyrosine kinase inhibitor for the treatment of metastatic colorectal cancer. Cancer Manag. Res. 2019, 11, 7787–7803. [Google Scholar] [CrossRef]
- Wang-Gillam, A.; Schelman, W.; Ukrainskyj, S.; Chien, C.; Gonzalez, M.; Yang, Z.; Kania, M.; Yeckes-Rodin, H. Phase 1/1b open-label, dose-escalation study of fruquintinib in patients with advanced solid tumors in the United States. Investig. New Drugs 2023, 41, 851–860. [Google Scholar] [CrossRef]
- Mahipal, A.; Grothey, A. Role of biologics in first-line treatment of colorectal cancer. J. Oncol. Pract. 2016, 12, 1219–1228. [Google Scholar] [CrossRef]
- Jung, H.; Bae, K.; Lee, J.Y.; Kim, J.-H.; Han, H.-J.; Yoon, H.-Y.; Yoon, K.-A. Establishment of canine transitional cell carcinoma cell lines harboring BRAF V595E mutation as a therapeutic target. Int. J. Mol. Sci. 2021, 22, 9151. [Google Scholar] [CrossRef]
- Broecker-Preuss, M.; Müller, S.; Britten, M.; Worm, K.; Schmid, K.W.; Mann, K.; Fuhrer, D. Sorafenib inhibits intracellular signaling pathways and induces cell cycle arrest and cell death in thyroid carcinoma cells irrespective of histological origin or BRAF mutation status. BMC Cancer 2015, 15, 184. [Google Scholar] [CrossRef]
- Wang, H.; Quan, H.; Lou, L. AKT is critically involved in the antagonism of BRAF inhibitor sorafenib against dabrafenib in colorectal cancer cells harboring both wild-type and mutant (V600E) BRAF genes. Biochem. Biophys. Res. Commun. 2017, 489, 14–20. [Google Scholar] [CrossRef]
- Kim, J.E.; Kim, K.K.; Kim, S.Y.; Lee, J.; Park, S.H.; Park, J.O.; Park, Y.S.; Lim, H.Y.; Kang, W.K.; Kim, S.T. MAP2K1 mutation in colorectal cancer patients: Therapeutic challenge using patient-derived tumor cell lines. J. Cancer 2017, 8, 2263–2268. [Google Scholar] [CrossRef]
- Iglesias-Martinez, L.F.; Rauch, N.; Wynne, K.; McCann, B.; Kolch, W.; Rauch, J. Interactome dynamics of RAF1-BRAF kinase monomers and dimers. Sci. Data 2023, 10, 203. [Google Scholar] [CrossRef]
- Mooz, J.; Oberoi-Khanuja, T.K.; Harms, G.S.; Wang, W.; Jaiswal, B.S.; Seshagiri, S.; Tikkanen, R.; Rajalingam, K. Dimerization of the kinase ARAF promotes MAPK pathway activation and cell migration. Sci. Signal. 2014, 7, ra73. [Google Scholar] [CrossRef]
- Imielinski, M.; Greulich, H.; Kaplan, B.; Araujo, L.; Amann, J.; Horn, L.; Schiller, J.; Villalona-Calero, M.A.; Meyerson, M.; Carbone, D.P. Oncogenic and sorafenib-sensitive ARAF mutations in lung adenocarcinoma. J. Clin. Investig. 2014, 124, 1582–1586. [Google Scholar] [CrossRef]
- Botton, T.; Yeh, I.; Nelson, T.; Vemula, S.S.; Sparatta, A.; Garrido, M.C.; Allegra, M.; Rocchi, S.; Bahadoran, P.; McCalmont, T.H.; et al. Recurrent BRAF kinase fusions in melanocytic tumors offer an opportunity for targeted therapy. Pigment Cell Melanoma Res. 2013, 26, 845–851. [Google Scholar] [CrossRef]
- Mologni, L.; Costanza, M.; Sharma, G.G.; Viltadi, M.; Massimino, L.; Citterio, S.; Purgante, S.; Raman, H.; Pirola, A.; Zucchetti, M.; et al. Concomitant BCORL1 and BRAF mutations in vemurafenib-resistant melanoma cells. Neoplasia 2018, 20, 467–477. [Google Scholar] [CrossRef] [PubMed]
- Mullaguri, S.C.; Akula, S.; Ashireddygari, V.R.; Sahoo, P.S.; Burra, V.L.S.P.; Silveri, R.; Mupparapu, V.; Korikani, M.; Amanchi, N.R.; Subramaniam, J.; et al. Estimated sensitivity profiles of lung cancer specific uncommon BRAF mutants towards experimental and clinically approved kinase inhibitors. Toxicol. Appl. Pharmacol. 2022, 453, 116213. [Google Scholar] [CrossRef] [PubMed]
- Molnár, E.; Rittler, D.; Baranyi, M.; Grusch, M.; Berger, W.; Döme, B.; Tóvári, J.; Aigner, C.; Timár, J.; Garay, T.; et al. Pan-RAF and MEK vertical inhibition enhances therapeutic response in non-V600 BRAF mutant cells. BMC Cancer 2018, 18, 542. [Google Scholar] [CrossRef] [PubMed]
- Nagaria, T.S.; Williams, J.L.; Leduc, C.; Squire, J.A.; Greer, P.A.; Sangrar, W. Flavopiridol synergizes with sorafenib to induce cytotoxicity and potentiate antitumorigenic activity in EGFR/HER-2 and mutant RAS/RAF breast cancer model systems. Neoplasia 2013, 15, 939–951. [Google Scholar] [CrossRef] [PubMed]
- Hilhorst, R.; van den Berg, A.; Boender, P.; van Wezel, T.; Kievits, T.; de Wijn, R.; Ruijtenbeek, R.; Corver, W.E.; Morreau, H. Differentiating benign from malignant thyroid tumors by kinase activity profiling and dabrafenib BRAF V600E targeting. Cancers 2023, 15, 4477. [Google Scholar] [CrossRef]
- Ricci, M.S.; Kim, S.-H.; Ogi, K.; Plastaras, J.P.; Ling, J.; Wang, W.; Jin, Z.; Liu, Y.Y.; Dicker, D.T.; Chiao, P.J.; et al. Reduction of TRAIL-induced Mcl-1 and cIAP2 by c-Myc or sorafenib sensitizes resistant human cancer cells to TRAIL-induced death. Cancer Cell 2007, 12, 66–80. [Google Scholar] [CrossRef] [PubMed]
- Oikonomuu, E.; Koc, M.; Sourkova, V.; Andera, L.; Pintzas, A. Selective BRAFV600E inhibitor PLX4720, requires TRAIL assistance to overcome oncogenic PIK3CA resistance. PLoS ONE 2011, 6, e21632. [Google Scholar] [CrossRef] [PubMed]
- Martinelli, E.; Troiani, T.; Morgillo, F.; Rodolico, G.; Vitagliano, D.; Morelli, M.P.; Tuccillo, C.; Vecchione, L.; Capasso, A.; Orditura, M.; et al. Synergistic antitumor activity of sorafenib in combination with epidermal growth factor receptor inhibitors in colorectal and lung cancer cells. Clin. Cancer Res. 2010, 16, 4990–5001. [Google Scholar] [CrossRef]
- Piscazzi, A.; Costantino, E.; Maddalena, F.; Natalicchio, M.I.; Gerardi, A.M.T.; Antonetti, R.; Cignarelli, M.; Landriscina, M. Activation of the RAS/RAF/ERK signaling pathway contributes to resistance to sunitinib in thyroid carcinoma cell lines. J. Clin. Endocrinol. Metab. 2012, 97, E898–E906. [Google Scholar] [CrossRef][Green Version]
- Gril, B.; Palmieri, D.; Qian, Y.; Smart, D.D.; Ileva, L.; Liewehr, D.J.; Steinberg, S.M.; Steeg, P.S. Pazopanib reveals a role for tumor cell B-Raf in the prevention of HER2+ breast cancer metastasis. Clin. Cancer Res. 2011, 17, 142–153. [Google Scholar] [CrossRef] [PubMed]
- Gunda, V.; Ghosh, C.; Hu, J.; Zhang, L.; Zhang, Y.-Q.; Shen, M.; Kebebew, E. Combination BRAFV600E inhibition with the multitargeting tyrosine kinase inhibitor axitinib shows additive anticancer activity in BRAFV600E-mutant anaplastic thyroid cancer. Thyroid 2023, 33, 1201–1214. [Google Scholar] [CrossRef] [PubMed]
- Tran, K.T.; Kolekar, S.; Wang, Q.; Shih, J.-H.; Buchanan, C.M.; Deva, S.; Shepherd, P.R. Response to BRAF-targeted therapy is enhanced by cotargeting VEGFRs or WNT/β-catenin signaling in BRAF-mutant colorectal cancer models. Mol. Cancer Ther. 2022, 21, 1777–1787. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, C.; Kumar, S.; Kushchayeva, Y.; Gaskins, K.; Boufraqech, M.; Wei, D.; Gara, S.K.; Zhang, L.; Zhang, Y.; Shen, M.; et al. A combinatorial strategy for targeting BRAFV600E-mmtant cancers with BRAFV600E inhibitor (PLX4720) and tyrosine kinase inhibitor (ponatinib). Clin. Cancer Res. 2020, 26, 2022–2036. [Google Scholar] [CrossRef]
- Mordant, P.; Loriot, Y.; Leteur, C.; Calderaro, J.; Bourhis, J.; Wislez, M.; Soria, J.-C.; Deutsch, E. Dependence on phosphoinositide 3-kinase and RAS-RAF pathways drive the activity of RAF265, a novel RAFA/VEGFR2 inhibitor, and RAD001 (everolimus) in combination. Mol. Cancer Ther. 2010, 9, 358–368. [Google Scholar] [CrossRef]
- Chow, A.K.M.; Cheng, N.S.M.; Lam, C.S.C.; Ng, L.; Wong, S.K.M.; Wan, T.M.H.; Man, J.H.W.; Cheung, A.H.K.; Yau, T.C.C.; Poon, J.T.C.; et al. Preclinical analysis of the anti-tumor and anti-metastatic effects of Raf265 on colon cancer cells and CD26+ cancer stem cells in colorectal carcinoma. Mol. Cancer 2015, 14, 80. [Google Scholar] [CrossRef]
- Su, Y.; Vilgelm, A.E.; Kelley, M.C.; Hawkins, O.E.; Liu, Y.; Boyd, K.L.; Kantrow, S.; Splittgerber, R.C.; Short, S.P.; Sobolik, T.; et al. RAF265 inhibits the growth of advanced human melanoma tumors. Clin. Cancer Res. 2012, 18, 2184–2198. [Google Scholar] [CrossRef] [PubMed]
- Barollo, S.; Bertazza, L.; Baldini, E.; Ulisse, S.; Cavedon, E.; Boscaro, M.; Pezzani, R.; Mian, C. The combination of RAF265, SB590885, ZSTK474 on thyroid cancer cell lines deeply impact on proliferation and MAPK and PI3K/Akt signaling pathways. Investig. New Drugs 2014, 32, 626–635. [Google Scholar] [CrossRef]
- Saleh, K.; Al Sakhen, M.; Kanaan, S.; Yasin, S.; Höpfner, M.; Tahtamouni, L.; Biersack, B. Antitumor activity of the new tyrphostin briva against BRAFV600E-mutant colorectal carcinoma cells. Investig. New Drugs 2023, 41, 791–801. [Google Scholar] [CrossRef]
- Caporali, S.; Alvino, E.; Lacal, P.M.; Levati, L.; Giurato, G.; Memoli, D.; Caprini, E.; Cappellini, G.C.A.; D’Atri, S. Targeting the PI3K/AKT/mTOR pathway overcomes the stimulating effect of dabrafinib on the invasive behavior of melanoma cells with acquired resistance to the BRAF inhibitor. Int. J. Oncol. 2016, 49, 1164–1174. [Google Scholar] [CrossRef]
- Caporali, S.; Amaro, A.; Levati, L.; Alvino, E.; Lacal, P.M.; Mastroeni, S.; Ruffini, F.; Bonmassar, L.; Cappellini, G.C.A.; Felli, N.; et al. miR-126-3p down-regulation contributes to dabrafenib acquired resistance in melanoma by up-regulating ADAM9 and VEGF-A. J. Exp. Clin. Cancer Res. 2019, 38, 272. [Google Scholar] [CrossRef]
- Martin, M.J.; Hayward, R.; Viros, A.; Marais, R. Metformin accelerates the growth of BRAFV600E-driven melanoma by upregulating VEGF-A. Cancer Discov. 2012, 2, 344–355. [Google Scholar] [CrossRef]
- Kurenova, E.; Ucar, D.; Liao, J.; Yemma, M.; Gogate, P.; Bshara, W.; Sunar, U.; Seshadri, M.; Hochwald, S.N.; Cance, W.G. A FAK scaffold inhibitor disrupts FAK and VEGFR-3 signaling and blocks melanoma growth by targeting both tumor and endothelial cells. Cell Cycle 2014, 13, 2542–2553. [Google Scholar] [CrossRef]
- Coupe, N.; Guo, L.; Bridges, E.; Campo, L.; Espinosa, O.; Colling, R.; Marshall, A.; Nandakumar, A.; van Stiphout, R.; Buffa, F.M.; et al. WNT5A-ROR2 axis mediates VEGF dependence of BRAF mutant melanoma. Cell. Oncol. 2023, 46, 391–407. [Google Scholar] [CrossRef]
- Ott, P.A.; Hamilton, A.; Min, C.; Safarzadeh-Amiri, S.; Goldberg, L.; Yoon, J.; Yee, H.; Buckley, M.; Christos, P.J.; Wright, J.J.; et al. A phase II trial of sorafenib in metastatic melanoma with tissue correlates. PLoS ONE 2010, 5, e15588. [Google Scholar] [CrossRef]
- Wilson, M.A.; Zhao, F.; Letrero, R.; D’Andrea, K.; Rimm, D.L.; Kirkwood, J.M.; Kluger, H.M.; Lee, S.J.; Schuchter, L.M.; Flaherty, K.T.; et al. Correlation of somatic mutations and clinical outcome in melanoma patients treated with carboplatin, paclitaxel, and sorafenib. Clin. Cancer Res. 2014, 20, 3328–3337. [Google Scholar] [CrossRef]
- Al-Marrawi, M.Y.; Saroya, B.S.; Brennan, M.C.; Yang, Z.; Dykes, T.M.; El-Deiry, W.S. Off-label use of cetuximab plus sorafenib and panitumumab plus regorafenib to personalize therapy for a patient with V600E BRAF-mutant metastatic colon cancer. Cancer Biol. Ther. 2013, 15, 703–710. [Google Scholar] [CrossRef] [PubMed]
- Janku, F.; Sakamuri, D.; Kato, S.; Huang, H.J.; Call, G.; Naing, A.; Holley, V.R.; Patel, S.P.; Amaria, R.N.; Falchook, G.S.; et al. Dose-escalation study of vemurafenib with sorafenib or critozinib in patients with BRAF-mutated advanced cancers. Cancer 2021, 127, 391–402. [Google Scholar] [CrossRef] [PubMed]
- Grothey, A.; Van Cutsem, E.; Sobrero, A.; Siena, S.; Falcone, A.; Ychou, M.; Humblet, Y.; Bouché, O.; Mineur, L.; Barone, C.; et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): An international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet 2013, 381, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Qin, S.; Xu, R.; Yau, T.C.C.; Ma, B.; Pan, H.; Xu, J.; Bai, Y.; Chi, Y.; Wang, L.; et al. Regorafenib plus best supportive care versus placebo plus best supportive care in Asian patients with previously treated metastatic colorectal cancer (CONCUR): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2015, 16, 619–629. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, T.; Ikoma, T.; Yamamura, S.; Miura, K.; Tsukidi, T.; Watanabe, T.; Nagai, H.; Takatani, M.; Yasui, H. Regorafenib is suitable for advanced colorectal cancer patients who have previously received trifluridine/tipiracil plus bevacizumab. Sci. Rep. 2023, 13, 2433. [Google Scholar] [CrossRef] [PubMed]
- Izar, B.; Sharfman, W.; Hodi, F.S.; Lawrence, D.; Flaherty, K.T.; Amaravadi, R.; Kim, K.B.; Puzanov, I.; Sosman, J.; Dummer, R.; et al. A first-in-human phase I, multicenter, open-label, dose-escalation study of the oral RAF/VEGFR-2 inhibitor (RAF265) in locally advanced or metastatic melanoma independent from BRAF mutation status. Cancer Med. 2017, 6, 1904–1914. [Google Scholar] [CrossRef] [PubMed]
- Xu, T.; Li, J.; Wang, Z.; Zhang, X.; Zhou, J.; Lu, Z.; Shen, L.; Wang, X. Real-world treatment and outcomes of patients with metastatic BRAF mutant colorectal cancer. Cancer Med. 2023, 12, 10473–10484. [Google Scholar] [CrossRef]
- Stintzing, S.; Heinrich, K.; Tougeron, D.; Modest, D.P.; Schwaner, I.; Eucker, J.; Pihusch, R.; Stauch, M.; Kaiser, F.; Kahl, C.; et al. FOLFOXIRI plus cetuximab or bevacizumab as first-line treatment of BRAFV600E-mutant metastatic colorectal cancer: The randomized phase II FIRE-4.5 (AIO KRK0116) study. J. Clin. Oncol. 2023, 41, 4143–4153. [Google Scholar] [CrossRef] [PubMed]
- Gelsomino, F.; Casadei-Gardini, A.; Rossini, D.; Boccaccino, A.; Masi, G.; Cremolini, C.; Spallanzani, A.; Viola, M.G.; Garajovà, I.; Salati, M.; et al. The role of anti-angiogenics in pre-treated metastatic BRAF-mutant colorectal cancer: A pooled analysis. Cancers 2020, 12, 1022. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Lee, M.-W.; Song, I.-C.; Lee, H.-J.; Yun, H.-J.; Jo, D.-Y.; Kim, J.S.; Kwon, J.H.; Kim, J.-Y.; Lee, K.-H.; et al. Maintenance therapy with fluoropyrimidine and cetuximab or bevacizumab after first line FOLFOX-chemotherapy in metastatic colorectal cancer according to RAS or BRAFV600E mutation status. J. Cancer Res. Clin. Oncol. 2023, 149, 7819–7829. [Google Scholar] [CrossRef] [PubMed]
- Yoshino, T.; Portnoy, D.C.; Obermannová, R.; Bodoky, G.; Prausová, J.; Garcia-Carbonero, R.; Ciuleanu, T.; García-Alfonso, P.; Cohn, A.L.; Van Cutsem, E.; et al. Biomarker analysis beyond angiogenesis: RAS/RAF mutation status, tumour sidedness, and second-line ramucirumab efficacy in patients with metastatic colorectal carcinoma from RAISE-a global phase III study. Ann. Oncol. 2019, 30, 124–131. [Google Scholar] [CrossRef]
- Astorga, B.G.; Ballabrera, F.S.; Aguilar, E.A.; Fernández, E.É.; García-Alfonso, P.; Flores, E.G.; García, R.V.; Montes, A.E.; Munoz, A.M.L.; Salvia, A.S. Patient profiles as an aim to optimize selection in the second line setting: The role of aflibercept. Clin. Transl. Oncol. 2021, 23, 1520–1528. [Google Scholar] [CrossRef]
- El-Deiry, W.S.; Winer, A.; Slifker, M.; Taylor, S.; Adamson, B.J.S.; Meropol, N.J.; Ross, E.A. Disease control with FOLFIRI plus ziv-aflibercept (zFOLFIRI) beyond FOLFIRI plus bevacizumab: Case series in metastatic colorectal cancer (mCRC). Front. Oncol. 2019, 9, 142. [Google Scholar] [CrossRef]
- Fredriksson, L.; Li, H.; Eriksson, U. The PDGF family: Four gene products form five dimeric isoforms. Cytokine Growth Factor. Rev. 2004, 15, 197–204. [Google Scholar] [CrossRef]
- Valius, M.; Kazlauskas, A. Phospholipase C-gamma 1 and phosphatidylinositol 3 kinase are the downstream mediators of the PDGF receptor’s mitogenic signal. Cell 1993, 73, 321–334. [Google Scholar] [CrossRef]
- Lassus, H.; Sihto, H.; Leminen, A.; Nordling, S.; Joensuu, H.; Nupponen, N.N.; Butzow, R. Genetic alterations and protein expression of KIT and PDGFRA in serous ovarian carcinoma. Br. J. Cancer 2004, 91, 2048–2055. [Google Scholar] [CrossRef]
- Blom, T.; Roselli, A.; Häyry, V.; Tynninen, O.; Wartiovaara, K.; Korja, M.; Nordfors, K.; Haapasalo, H.; Nupponen, N.N. Amplification and overexpression of KIT, PDGFRA, and VEGFR2 in medulloblastomas and primitive neuroectodermal tumors. J. Neurooncol. 2010, 97, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Tsao, A.S.; Wei, W.; Kuhn, E.; Spencer, L.; Solis, L.M.; Suraokar, M.; Lee, J.J.; Hong, W.K.; Wistuba, I.I. Immunohistochemical overexpression of platelet-derived growth factor receptor-beta (PDGFR-β) is associated with PDGFRB gene copy number gain in sarcomatoid non-small-cell lung cancer. Clin. Lung Cancer 2011, 12, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Ong, H.S.; Gokavarapu, S.; Tian, Z.; Li, J.; Xu, Q.; Cao, W.; Zhang, C.P. PDGFRA mRNA is overexpressed in oral cancer patients as compared to normal subjects with a significant trend of overexpression among tobacco users. J. Oral Pathol. Med. 2017, 46, 591–597. [Google Scholar] [CrossRef] [PubMed]
- Ong, H.S.; Gokavarapu, S.; Tian, Z.; Li, J.; Xu, Q.; Zhang, C.P.; Cao, W. PDGFRA mRNA overexpression is associated with regional metastasis and reduced survival in oral squamous cell carcinoma. J. Oral Pathol. Med. 2018, 47, 652–659. [Google Scholar] [CrossRef] [PubMed]
- Penzel, R.; Aulmann, S.; Moock, M.; Schwarzbach, M.; Rieker, R.J.; Mechtersheimer, G. The location of KIT and PDGFRA gene mutations in gastrointestinal stromal tumours is site and phenotype associated. J. Clin. Pathol. 2005, 58, 634–639. [Google Scholar] [CrossRef] [PubMed]
- Lasota, J.; Miettinen, M. KIT and PDGFRA mutations in gastrointestinal stromal tumors (GISTs). Semin. Diagn. Pathol. 2006, 23, 91–102. [Google Scholar] [CrossRef]
- Heinrich, M.C.; Corless, C.L.; Duensing, A.; McGreevey, L.; Chen, C.J.; Joseph, N.; Singer, S.; Griffith, D.J.; Haley, A.; Town, A.; et al. PDGFRA activating mutations in gastrointestinal stromal tumors. Science 2003, 299, 708–710. [Google Scholar] [CrossRef] [PubMed]
- Daniels, M.; Lurkin, I.; Pauli, R.; Erbstösser, E.; Hildebrandt, U.; Hellwig, K.; Zschille, U.; Lüders, P.; Krüger, G.; Knolle, J.; et al. Spectrum of KIT/PDGFRA/BRAF mutations and phosphatidylinositol 3-kinase pathway gene alterations in gastrointestinal stromal tumors (GIST). Cancer Lett. 2011, 312, 43–54. [Google Scholar] [CrossRef]
- Joensuu, H.; Rutkowski, P.; Nishida, T.; Steigen, S.E.; Brabec, P.; Plank, L.; Nilsson, B.; Braconi, C.; Bordoni, A.; Magnusson, M.K.; et al. KIT and PDGFRA mutations and the risk of GI stromal tumor recurrence. J. Clin. Oncol. 2015, 33, 634–642. [Google Scholar] [CrossRef] [PubMed]
- Velghe, A.I.; Van Cauwenberghe, S.; Polyansky, A.A.; Chand, D.; Montano-Almendras, C.P.; Charni, S.; Hallberg, B.; Essaghir, A.; Demoulin, J.-B. PDGFRA alterations in cancer: Characterization of a gain-of-function V536E transmembrane mutant as well as loss-of-function and passenger mutations. Oncogene 2014, 33, 2568–2576. [Google Scholar] [CrossRef] [PubMed]
- Stover, E.H.; Chen, J.; Folens, C.; Lee, B.H.; Mentens, N.; Marynen, P.; Williams, I.R.; Gilliland, D.G.; Cools, J. Activation of FIP1L1-PDGFRalpha requires disruption of the juxtamembrane domain of PDGFRalpha and is FIP1L1-independent. Proc. Natl. Acad. Sci. USA 2006, 103, 8078–8083. [Google Scholar] [CrossRef] [PubMed]
- Campregher, P.V.; Halley, N.D.S.; Vieira, G.A.; Fernandes, J.F.; Velloso, E.D.R.P.; Ali, S.; Mughal, T.; Miller, V.; Mangueira, C.L.P.; Odone, V.; et al. Identification of a novel fusion TBL1XR1-PDGFRB in a patient with acute myeloid leukemia harboring the DEK-Nup214 fusion and clinical response to dasatinib. Leuk. Lymphoma 2017, 58, 2969–2972. [Google Scholar] [CrossRef] [PubMed]
- Sheng, G.; Zeng, Z.; Pan, J.; Kou, L.; Wang, Q.; Yao, H.; Wen, L.; Ma, L.; Wu, D.; Qiu, H.; et al. Multiple MYO18A-PDGFRB fusion transcripts in a myeloproliferative neoplasm patient with T(5;17)(q32;q11). Mol. Cytogenet. 2017, 10, 4. [Google Scholar] [CrossRef] [PubMed]
- Matei, D.; Emerson, R.E.; Lai, Y.C.; Baldridge, L.A.; Rao, J.; Yiannoutsos, C.; Donner, D.D. Autocrine activation of PDGFRalpha promotes the progression of ovarian cancer. Oncogene 2006, 25, 2060–2069. [Google Scholar] [CrossRef] [PubMed]
- Adewuyi, E.E.; Deschenes, J.; Lopez-Campistrous, A.; Kattar, M.M.; Ghosh, S.; McMullen, T.P.W. Autocrine activation of platelet-derived growth factor receptor α in metastatic papillary thyroid cancer. Hum. Pathol. 2018, 75, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Lokker, N.A.; Sullivan, C.M.; Hollenbach, S.J.; Israel, M.A.; Giese, N.A. Platelet-derived growth factor (PDGF) autocrine signaling regulates survival and mitogenic pathways in glioblastoma cells: Evidence that the novel PDGF-C and PDGF-D ligands may play a role in the development of brain tumors. Cancer Res. 2002, 62, 3729–3735. [Google Scholar]
- Jechlinger, M.; Sommer, A.; Moriggl, R.; Seither, P.; Kraut, N.; Capodiecci, P.; Donovan, M.; Cordon-Cardo, C.; Beug, H.; Grünert, S. Autocrine PDGFR signaling promotes mammary cancer metastasis. J. Clin. Investig. 2006, 116, 1561–1570. [Google Scholar] [CrossRef]
- Oliveira, S.; Lukacs, N. Stem cell factor: A hemopoietic cytokine with important targets in asthma. Curr. Drug Targets Inflamm. Allergy 2003, 2, 313–318. [Google Scholar] [CrossRef]
- Nagata, H.; Worobec, A.S.; Oh, C.K.; Chowdhury, B.A.; Tannenbaum, S.; Suzuki, Y.; Metcalfe, D.D. Identification of a point mutation in the catalytic domain of the protooncogene c-kit in peripheral blood mononuclear cells of patients who have mastocytosis with an associated hematologic disorder. Proc. Natl. Acad. Sci. USA 1995, 92, 10560–10564. [Google Scholar] [CrossRef]
- Beghini, A.; Peterlongo, P.; Ripamonti, C.B.; Larizza, L.; Cairoli, R.; Morra, E.; Mecucci, C. c-kit mutations in core binding factor leukemias. Blood 2000, 95, 726–728. [Google Scholar] [CrossRef]
- Louveau, B.; Jouenne, F.; de Moura, C.R.; Sadoux, A.; Baroudjian, B.; Delyon, J.; Herms, F.; De Masson, A.; Da Meda, L.; Battistella, M.; et al. Baseline genomic features in BRAFV600-mutated metastatic melanoma patients treated with BRAF inhibitor + MEK inhibitor in routine care. Cancers 2019, 11, 1203. [Google Scholar] [CrossRef]
- Hongyo, T.; Li, T.; Syaifudin, M.; Baskar, R.; Ikeda, H.; Kanakura, Y.; Aozasa, K.; Nomura, T. Specific c-kit mutations in sinonasal natural killer/T-cell lymphoma in China and Japan. Cancer Res. 2000, 60, 2345–2347. [Google Scholar] [PubMed]
- Büttner, C.; Henz, B.M.; Welker, P.; Sepp, N.T.; Grabbe, J. Identification of activating c-kit mutations in adult-, but not in childhood-onset indolent mastocytosis: A possible explanation for divergent clinical behavior. J. Investig. Dermatol. 1998, 111, 1227–1231. [Google Scholar] [CrossRef] [PubMed]
- Ashman, L.K.; Ferrao, P.; Cole, S.R.; Cambareri, A.C. Effects of mutant c-kit in early myeloid cells. Leuk. Lymphoma 1999, 34, 451–461. [Google Scholar] [CrossRef] [PubMed]
- Babaei, M.A.; Kamalidehghan, B.; Saleem, M.; Huri, H.Z.; Ahmadipour, F. Receptor tyrosine kinase (c-Kit) inhibitors: A potential therapeutic target in cancer cells. Drug Des. Dev. Ther. 2016, 10, 2443–2459. [Google Scholar] [CrossRef] [PubMed]
- Jonas, O.; Oudin, M.J.; Kosciuk, T.; Whitman, M.; Gertler, F.B.; Cima, M.J.; Flaherty, K.T.; Langer, R. Parallel in-vivo assessment of drug phenotypes at various time points during systemic BRAF inhibition reveals tumor adaption and altered treatment vulnerabilities. Clin. Cancer Res. 2016, 22, 6031–6038. [Google Scholar] [CrossRef] [PubMed]
- Nazarian, R.; Shi, H.; Wang, Q.; Kong, X.; Koya, R.C.; Lee, H.; Chen, Z.; Lee, M.-K.; Attar, N.; Sazegar, H.; et al. Melanomas acquire resistance to BRAF(V600E) inhibition by RTK or N-RAS upregulation. Nature 2010, 468, 973–977. [Google Scholar] [CrossRef]
- Shi, H.; Kong, X.; Ribas, A.; Lo, R.S. Combinatorial treatments that overcome PDGFRβ-driven resistance of melanoma cells to V600EB-RAF inhibition. Cancer Res. 2011, 71, 5067–5074. [Google Scholar] [CrossRef]
- Rebecca, V.W.; Wood, E.; Fedorenko, I.V.; Paraiso, K.H.T.; Haarberg, H.E.; Chen, Y.; Xiang, Y.; Sarnaik, A.; Gibney, G.T.; Sondak, V.K.; et al. Evaluating melanoma drug response and therapeutic escape with quantitative proteomics. Mol. Cell. Proteom. 2014, 13, 1844–1854. [Google Scholar] [CrossRef] [PubMed]
- Vella, L.J.; Behren, A.; Coleman, B.; Greening, D.W.; Hill, A.F.; Cebon, J. Intercellular resistance to BRAF inhibition can be mediated by extracellular vesicle-asssociated PDGFRβ. Neoplasia 2017, 19, 932–940. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Hong, A.; Kong, X.; Koya, R.C.; Song, C.; Moriceau, G.; Hugo, W.; Yu, C.C.; Ng, C.; Chodon, T.; et al. A novel AKT1 mutant amplifies an adaptive melanoma response to BRAF inhibition. Cancer Discov. 2014, 4, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Adam, C.; Fusi, L.; Weiss, N.; Goller, S.G.; Meder, K.; Frings, V.G.; Kneitz, H.; Goebeler, M.; Houben, R.; Schrama, D.; et al. Efficient suppression of NRAS-driven melanoma by co-inhibition of ERK1/2 and ERK5 MAPK pathways. J. Investig. Dermatol. 2020, 140, 2455–2465. [Google Scholar] [CrossRef]
- Guida, T.; Anaganti, S.; Provitera, L.; Gedrich, R.; Sullivan, E.; Wilhelm, S.M.; Santoro, M.; Carlomagno, F. Sorafenib inhibits imatinib-resistant KIT and platelet-derived growth factor receptor beta gatekeeper mutants. Clin. Cancer Res. 2007, 13, 3363–3369. [Google Scholar] [CrossRef] [PubMed]
- Tiago, M.; Capparelli, C.; Erkes, D.A.; Purwin, T.J.; Heilman, S.A.; Berger, A.C.; Davies, M.A.; Aplin, A.E. Targeting BRD/BET proteins inhibits adaptive kinome upregulation and enhances the effects of BRAF/MEK inhibitors in melanoma. Br. J. Cancer 2020, 122, 789–800. [Google Scholar] [CrossRef]
- Sabbatino, F.; Wang, Y.; Wang, X.; Flaherty, K.T.; Yu, L.; Pepin, D.; Scognamiglio, G.; Pepe, S.; Kirkwood, J.M.; Cooper, Z.A.; et al. PDGFRa up-regulation mediated by Sonic Hedgehog pathway activation leads to BRAF inhibitor resistance in melanoma cells with BRAF mutation. Oncotarget 2014, 5, 1926–1941. [Google Scholar] [CrossRef]
- Li, Y.; Li, Y.; Liu, Q.; Wang, A. Typrhostin AG1296, a platelet-derived growth factor receptor inhibitor, induces apoptosis, and reduces viability and migration of PLX4032-resistant melanoma cells. OncoTargets Ther. 2015, 8, 1043–1051. [Google Scholar] [CrossRef]
- Che, H.; Guo, H.; Si, X.; You, Q.; Lou, W. Additive effect by combination of Akt inhibitor, MK-2206, and PDGFR inhibitor, tyrphostin AG 1296, in suppressing anaplastic thyroid carcinoma cell viability and motility. OncoTargets Ther. 2014, 7, 425–432. [Google Scholar]
- Friedman, A.A.; Amzallag, A.; Pruteanu-Malinici, I.; Baniya, S.; Cooper, Z.A.; Piris, A.; Hargreaves, L.; Igras, V.; Frederick, D.T.; Lawrence, D.P.; et al. Landscape of targeted anti-cancer drug synergies in melanoma identifies a novel BRAF-VEGFR/PDGFR combination treatment. PLoS ONE 2015, 10, e0140310. [Google Scholar] [CrossRef]
- Recagni, M.; Tassinari, M.; Doria, F.; Cimino-Reale, G.; Zaffaroni, N.; Freccero, M.; Folini, M.; Richter, S.N. The oncogenic signaling pathways in BRAF-mutant melanoma cells are modulated by naphthalene diimide-like G-quadruple ligands. Cells 2019, 8, 1274. [Google Scholar] [CrossRef]
- Singleton, K.R.; Crawford, L.; Tsui, E.; Manchester, H.E.; Maertens, O.; Liu, X.; Liberti, M.V.; Magpusao, A.N.; Stein, E.M.; Tingley, J.P.; et al. Melanoma therapeutic strategies that select against resistance by exploiting MYC-driven evolutionary convergence. Cell Rep. 2017, 21, 2796–2812. [Google Scholar] [CrossRef]
- Ablain, J.; Liu, S.; Moriceau, G.; Lo, R.S.; Zon, L.I. SPRED1 deletion confers resistance to MAPK inhibition in melanoma. J. Exp. Med. 2020, 218, e20201097. [Google Scholar] [CrossRef]
- Guo, T.; Agaram, N.P.; Wong, G.C.; Hom, G.; D’Alamo, D.; Maki, R.G.; Schwartz, G.K.; Veach, D.; Clarkson, B.D.; Singer, S.; et al. Sorafenib inhibits the imatinib-resistant KITT670I gatekeeper mutation in gastrointestinal stromal tumor. Clin. Cancer Res. 2007, 13, 4874–4881. [Google Scholar] [CrossRef] [PubMed]
- Miranda, C.; Nucifora, M.; Molinari, F.; Conca, E.; Anania, M.C.; Bordoni, A.; Saletti, P.; Mazzucchelli, L.; Pilotti, S.; Pierotti, M.A.; et al. KRAS and BRAF mutations predict primary resistance to imatinib in gastrointestinal stromal tumors. Clin. Cancer Res. 2012, 18, 1769–1776. [Google Scholar] [CrossRef]
- Menzer, C.; Hassel, J.C. Targeted therapy for melanomas without BRAF V600 mutations. Curr. Treat. Options Oncol. 2022, 23, 831–842. [Google Scholar] [CrossRef]
- Smith, B.D.; Kaufman, M.D.; Lu, W.-P.; Gupta, A.; Leary, C.B.; Wise, S.C.; Rutkoski, T.J.; Ahn, Y.M.; Al-Ani, G.; Bulfer, S.L.; et al. Ripretinib (DCC-2618) is a switch control kinase inhibitor of a broad spectrum of oncogenic and drug-resistant KIT and PDGFRA variants. Cancer Cell 2019, 35, 738–751. [Google Scholar] [CrossRef]
- Golcic, M.; Jones, R.L.; Huang, P.; Napolitano, A. Evaluation of systemic treatment options for gastrointestinal stromal tumours. Cancers 2023, 15, 4081. [Google Scholar] [CrossRef] [PubMed]
- Franck, C.; Rosania, R.; Franke, S.; Haybaeck, J.; Canbay, A.; Venerito, M. The BRAF status may predict response to sorafenib in gastrointestinal stromal tumors resistant to imatinib, sunitinib, and regorafenib: Case series and review of the literature. Digestion 2019, 99, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Gelderblom, H.; Jones, R.L.; Blay, J.-Y.; George, S.; von Mehren, M.; Zalcberg, J.R.; Kng, Y.-K.; Razak, A.A.; Trent, J.; Attia, S.; et al. Patient-reported outcomes and tolerability in patients receiving ripretinib versus sunitinib after treatment with imatinib in INTRIGUE, a phase 3, open-label study. Eur. J. Cancer 2023, 192, 113245. [Google Scholar] [CrossRef]
- Falchook, G.S.; Trent, J.C.; Heinrich, M.C.; Beadling, C.; Patterson, J.; Bastida, C.C.; Blackman, S.C.; Kurzrock, R. BRAF mutant gastrointestinal stromal tumor: First report of regression with BRAF inhibitor dabrafenib (GSK2118436) and whole exomic sequencing for analysis of acquired resistance. Oncotarget 2013, 4, 310–315. [Google Scholar] [CrossRef]
- Demetri, G.D.; Reichardt, P.; Kang, Y.-K.; Blay, J.-Y.; Rutkowski, P.; Gelderblom, H.; Hohenberger, P.; Leahy, M.; von Mehren, M.; Joensuu, H.; et al. Efficacy and safety of regorafenib for advanced gastrointestinal stromal tumours after failure of imatinib and sunitinib: An international, multicentre, prospective, randomised, placebocontrolled phase 3 trial (GRID). Lancet 2013, 381, 295–302. [Google Scholar] [CrossRef]
- Nannini, M.; Valerio, D.S.; Gruppioni, E.; Altimari, A.; Chiusole, B.; Saponara, M.; Pantaleo, M.A.; Brunello, A. Complete radiological response to first-line regorafenib in a patient with abdominal relapse of BRAF V600E mutated GIST. Ther. Adv. Gastroenterol. 2020, 13, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Martin-Broto, J.; Valverde, C.; Hindi, N.; Vincenzi, B.; Martinez-Trufero, J.; Grignani, G.; Italiano, A.; Lavernia, J.; Vallejo, A.; Dei Tos, P.; et al. REGISTRI: Regorafenib in first-line of KIT/PDGFRA wild type metastatic GIST: A collaborative Spanish (GEIS), Italian (ISG) and French Sarcoma Group (FSG) phase II trial. Mol. Cancer 2023, 22, 127. [Google Scholar] [CrossRef] [PubMed]
- Krook, M.A.; Reeser, J.W.; Ernst, G.; Barker, H.; Wilberding, M.; Li, G.; Chen, H.-Z.; Roychowdhury, S. Fibroblast growth factor receptors in cancer: Genetic alterations, diagnostics, therapeutic targets and mechanisms of resistance. Br. J. Cancer 2021, 124, 880–892. [Google Scholar] [CrossRef]
- Szymczyk, J.; Sluzalska, K.D.; Materla, I.; Opalinski, L.; Otlewski, J.; Zakrzewska, M. FGF/FGFR-dependent molecular mechanisms underlying anti-cancer drug resistance. Cancers 2021, 13, 5796. [Google Scholar] [CrossRef] [PubMed]
- Metzner, T.; Bedeir, A.; Held, G.; Peter-Vörösmarty, B.; Ghassemi, S.; Heinzle, C.; Spiegl-Kreinecker, S.; Marian, B.; Holzmann, K.; Grasl-Kraupp, B.; et al. Fibroblast growth factor receptors as therapeutic targets in human melanoma: Synergism with BRAF inhibition. J. Investig. Dermatol. 2011, 131, 2087–2095. [Google Scholar] [CrossRef] [PubMed]
- Grimm, J.; Hufnagel, A.; Wobser, M.; Borst, A.; Haferkamp, S.; Houben, R.; Meierjohann, S. BRAF inhibition causes resilience of melanoma cell lines by inducing the secretion of FGF1. Oncogenesis 2018, 7, 71. [Google Scholar] [CrossRef] [PubMed]
- Ghassemi, S.; Vejdovszky, K.; Sahin, E.; Ratzinger, L.; Schelch, K.; Mohr, T.; Peter-Vörösmarty, B.; Brankovic, J.; Lackner, A.; Leopoldi, A.; et al. FGF5 is expressed in melanoma and enhances malignancy in vitro and in vivo. Oncotarget 2017, 8, 87750–87762. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tassone, E.; Valacca, C.; Mignatti, P. Membrane-type 1 matrix metalloproteinase downregulates fibroblast growth factor-2 binding to the cell surface and intracellular signaling. J. Cell. Physiol. 2015, 230, 366–377. [Google Scholar] [CrossRef]
- Garay, T.; Molnár, E.; Juhász, É.; László, V.; Barbai, T.; Dobos, J.; Schelch, K.; Pirker, C.; Grusch, M.; Berger, W.; et al. Sensitivity of melanoma cells to EGFR and FGFR activation but not inhibition is influenced by oncogenic BRAF and NRAS mutations. Pathol. Oncol. Res. 2015, 21, 957–968. [Google Scholar] [CrossRef] [PubMed]
- Yadav, V.; Zhang, X.; Liu, J.; Estrem, S.; Li, S.; Gong, X.-Q.; Buchanan, S.; Henry, J.R.; Starling, J.J.; Peng, S.-B. Reactivation of mitogen-activated protein kinase (MAPK) pathway by FGF receptor 3 (FGFR3)/Ras mediates resistance to vemurafenib in human B-RAF V600E mutant melanoma. J. Biol. Chem. 2012, 287, 28087–28098. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-K.; Lee, M.-E.; Lee, W.S.; Kim, J.M.; Park, K.H.; Kim, T.S.; Lee, K.Y.; Ahn, J.B.; Chung, H.C.; Rha, S.Y. Dovitinib (TKI258), a multi-target angiokinase inhibitor, is effective regardless of KRAS and BRAF mutation status in colorectal cancer. Am. J. Cancer Res. 2015, 5, 72–86. [Google Scholar]
- Langdon, C.G.; Held, M.A.; Platt, J.T.; Meeth, K.; Iyidogan, P.; Mamillapalli, R.; Koo, A.B.; Klein, M.; Liu, Z.; Bosenberg, M.W.; et al. The broad spectrum receptor tyrosine kinase inhibitor dovitinib suppresses growth of BRAF mutant melanoma cells in combination with other signaling pathway inhibitors. Pigment Cell Melanoma Res. 2015, 28, 417–430. [Google Scholar] [CrossRef] [PubMed]
- Kane, A.M.; Liu, C.; Fennell, L.J.; McKeone, D.M.; Bond, C.E.; Pollock, P.M.; Young, G.; Leggett, B.A.; Whitehall, V.L.J. Aspirin reduces the incidence of metastasis in a pre-clinical study of Braf mutant serrated colorectal neoplasia. Br. J. Cancer 2021, 124, 1820–1827. [Google Scholar] [CrossRef] [PubMed]
- Eigner, K.; Filik, Y.; Mark, F.; Schütz, B.; Klambauer, G.; Moriggl, R.; Hengstschläger, M.; Stangl, H.; Mikula, M.; Röhrl, C. The unfolded protein response impacts melanoma progression by enhancing FGF expression and can be antagonized by a chemical chaperone. Sci. Rep. 2017, 7, 17498. [Google Scholar] [CrossRef]
- Xie, Y.; Su, N.; Yang, J.; Tan, Q.; Huang, S.; Jin, M.; Ni, Z.; Zhang, B.; Zhang, D.; Luo, F.; et al. FGF/FGFR signaling in health and disease. Signal Transduct. Target Ther. 2020, 5, 181. [Google Scholar] [CrossRef]
- Czyz, M. Fibroblast growth factor receptor signaling in skin cancers. Cells 2019, 8, 540. [Google Scholar] [CrossRef]
- Kumar, R.; Jain, A.G.; Rashid, M.U.; Ali, S.; Khetpal, N.; Hussain, I.; Ahmad, S. HGFR and FGR2: Their roles in progression and metastasis of esophageal cancer. In Role of Tyrosine Kinases in Gastrointestinal Malignancies; Nagaraju, G.P., Ed.; Springer: Singapore, 2018; pp. 1–14. [Google Scholar]
- Gumustekin, M.; Kargi, A.; Bulut, G.; Gozukizil, A.; Ulukus, C.; Oztop, I.; Atabey, N. HGF/c-Met overexpressions, but not met mutation, correlates with progression of non-small cell lung cancer. Pathol. Oncol. Res. 2012, 18, 209–218. [Google Scholar] [CrossRef]
- Awad, M.M.; Oxnard, G.R.; Jackman, D.M.; Savukoski, D.O.; Hall, D.; Shivdasani, P.; Heng, J.C.; Dahlberg, S.E.; Jänne, P.A.; Verma, S.; et al. MET exon 14 mutations in non-small-cell lung cancer are associated with advanced age and stage-dependent MET genomic amplification and c-Met overexpression. J. Clin. Oncol. 2016, 34, 721–730. [Google Scholar] [CrossRef]
- Zhao, X.; Qu, J.; Hui, Y.; Zhang, H.; Sun, Y.; Liu, X.; Zhao, X.; Zhao, Z.; Yang, Q.; Wang, F.; et al. Clinicopathological and prognostic significance of c-Met overexpression in breast cancer. Oncotarget 2017, 8, 56758–56767. [Google Scholar] [CrossRef]
- Blanc-Durand, F.; Alameddine, R.; Iafrate, A.J.; Tran-Thanh, D.; Lo, Y.C.; Blais, N.; Routy, B.; Tehfé, M.; Leduc, C.; Romeo, P.; et al. Tepotinib efficacy in a patient with non-small cell lung cancer with brain metastasis harboring an HLA-DRB1-MET gene fusion. Oncologist 2020, 25, 916–920. [Google Scholar] [CrossRef]
- Davies, K.D.; Ng, T.L.; Estrada-Bernal, A.; Le, A.T.; Ennever, P.R.; Camidge, D.R.; Doebele, R.C.; Aisner, D.L. Dramatic response to crizotinib in a patient with lung cancer positive for an HLA-DRB1-MET gene fusion. JCO Precis. Oncol. 2017, 1, 1–6. [Google Scholar] [CrossRef]
- Zhu, Y.C.; Wang, W.X.; Song, Z.B.; Zhang, Q.X.; Xu, C.W.; Chen, G.; Zhuang, W.; Lv, T.; Song, Y. MET-UBE2H fusion as a novel mechanism of acquired EGFR resistance in lung adenocarcinoma. J. Thorac. Oncol. 2018, 13, e202–e204. [Google Scholar] [CrossRef]
- Karagonlar, Z.F.; Koc, D.; Iscan, E.; Erdal, E.; Atabey, N. Elevated hepatocyte growth factor expression as an autocrine c-Met activation mechanism in acquired resistance to sorafenib in hepatocellular carcinoma cells. Cancer Sci. 2016, 107, 407–416. [Google Scholar] [CrossRef]
- Horiguchi, N.; Takayama, H.; Toyoda, M.; Otsuka, T.; Fukusato, T.; Merlino, G.; Takagi, H.; Mori, M. Hepatocyte growth factor promotes hepatocarcinogenesis through c-Met autocrine activation and enhanced angiogenesis in transgenic mice treated with diethylnitrosamine. Oncogene 2002, 21, 1791–1799. [Google Scholar] [CrossRef]
- Rasola, A.; Fassetta, M.; De Bacco, F.; D’Alessandro, L.; Gramaglia, D.; Di Renzo, M.F.; Comoglio, P.M. A positive feedback loop between hepatocyte growth factor receptor and beta-catenin sustains colorectal cancer cell invasive growth. Oncogene 2007, 26, 1078–1087. [Google Scholar] [CrossRef]
- Kentsis, A.; Reed, C.; Rice, K.L.; Sanda, T.; Rodig, S.J.; Tholouli, E.; Christie, A.; Valk, P.J.M.; Delwel, R.; Ngo, V.; et al. Autocrine activation of the MET receptor tyrosine kinase in acute myeloid leukemia. Nat. Med. 2012, 18, 1118–1122. [Google Scholar] [CrossRef]
- Trusolino, L.; Bertotti, A.; Comoglio, P.M. MET signalling: Principles and functions in development, organ regeneration and cancer. Nat. Rev. Mol. Cell. Biol. 2010, 11, 834–848. [Google Scholar] [CrossRef]
- Byeon, H.K.; Na, H.J.; Yang, Y.J.; Kwon, H.J.; Chang, J.W.; Ban, M.J.; Kim, W.S.; Shin, D.Y.; Lee, E.J.; Koh, Y.W.; et al. c-Met-mediated reactivation of PI3K/AKT signaling contributes to insensitive of BRAF(V600E) mutant thyroid cancer to BRAF inhibition. Mol. Carcinogen. 2016, 55, 1678–1687. [Google Scholar] [CrossRef]
- Byeon, H.K.; Na, H.J.; Yang, Y.J.; Ko, S.; Yoon, S.O.; Ku, M.; Yang, J.; Kim, J.W.; Ban, M.J.; Kim, J.-H.; et al. Acquired resistance to BRAF inhibition induces epithelial-to-mesenchymal transition in BRAF (V600E) mutant thyroid cancer by c-Met-mediated AKT activation. Oncotarget 2017, 8, 596–609. [Google Scholar] [CrossRef][Green Version]
- Knauf, J.A.; Luckett, K.A.; Chen, K.-Y.; Voza, F.; Socci, N.D.; Ghossein, R.; Fagin, J.A. Hgf/Met activation mediates resistance to BRAF inhibition in murine anaplastic thyroid cancers. J. Clin. Investig. 2018, 128, 4086–4097. [Google Scholar] [CrossRef]
- Vergani, E.; Vallacchi, V.; Frigerio, S.; Deho, P.; Mondellini, P.; Perego, P.; Cassinelli, G.; Lanzi, C.; Testi, M.A.; Rivoltini, L.; et al. Identification of MET and SRC activation in melanoma cell lines showing primary resistance to PLX4032. Neoplasia 2011, 13, 1132–1142. [Google Scholar] [CrossRef]
- Straussman, R.; Morikawa, T.; Shee, K.; Barzily-Rokni, M.; Qian, Z.R.; Du, J.; Davis, A.; Mongare, M.M.; Gould, J.; Frederick, D.T.; et al. Tumor microenvironment induces innate RAF-inhibitor resistance through HFG secretion. Nature 2012, 487, 500–504. [Google Scholar] [CrossRef]
- Caenepeel, S.; Cooke, K.; Wadsworth, S.; Huang, G.; Robert, L.; Moreno, B.H.; Parisi, G.; Cajulis, E.; Kendall, R.; Beltran, P.; et al. MAPK pathway inhibition induces MET and GAB1 levels, priming BRAF mutant melanoma for rescue by hepatocyte growth factor. Oncotarget 2017, 8, 17795–17809. [Google Scholar] [CrossRef] [PubMed]
- Das, I.; Wilhelm, M.; Hölom, V.; Marquez, R.F.; Svedman, F.C.; Hansson, J.; Tuominen, R.; Brage, S.E. Combining ERBB family and MET inhibitors is an effective therapeutic strategy in cutaneous malignant melanoma independent of BRAF/NRAS mutation status. Cell Death Dis. 2019, 10, 663. [Google Scholar] [CrossRef] [PubMed]
- Carson, R.; Celtikci, B.; Fenning, C.; Javadi, A.; Crawford, N.; Carbonell, L.P.; Lawler, M.; Longley, D.B.; Johnston, P.G.; Van Schaeybroeck, S. HDAC inhibition overcomes acute resistance to MEK inhibition in BRAF mutant colorectal cancer by down-regulation of c-FLIPL. Clin. Cancer Res. 2015, 21, 3230–3240. [Google Scholar] [CrossRef]
- Xu, T.; Wang, X.; Wang, Z.; Deng, T.; Qi, C.; Liu, D.; Li, Y.; Ji, C.; Shen, L. Molecular mechanisms underlying the resistance of BRAF V600E-mutant metastatic colorectal cancer to EGFR/BRAF inhibitors. Ther. Adv. Med. Oncol. 2022, 14, 1–12. [Google Scholar] [CrossRef]
- Oddo, D.; Siravegna, G.; Gloghini, A.; Vernieri, C.; Mussolin, B.; Morano, F.; Crisafulli, G.; Berenato, R.; Corti, G.; Volpi, C.C.; et al. Emergence of MET hyper-amplification at progression to MET and BRAF inhibition in colorectal cancer. Br. J. Cancer 2017, 117, 347–352. [Google Scholar] [CrossRef]
- Dong, Y.; Xu, J.; Sun, B.; Wang, J.; Wang, Z. MET-targeted therapies and clinical outcomes. A systematic literature review. Mol. Diagn. Ther. 2022, 26, 203–227. [Google Scholar] [CrossRef]
- Li, S.; Li, X.; Sun, S.; Li, S.; Zhou, C. Response to osimertinib plus trametinib in a heavily treated epidermal growth factor receptor (EGFR)-positive NSCLC harboring a rare, acquired rapidly accelerated fibrosarcoma B-type (BRAF) p.D594N mutation: A case report. Anticancer Drugs 2022, 33, 963–965. [Google Scholar] [CrossRef]
- Recondo, G.; Bahcall, M.; Spurr, L.F.; Che, J.; Ricciuti, B.; Leonardi, G.C.; Lo, Y.-C.; Li, Y.Y.; Lamberti, G.; Nguyen, T.; et al. Molecular mechanisms of acquired resistance to MET tyrosine kinase inhibitors in patients with MET exon 14-mutant NSCLC. Clin. Cancer Res. 2020, 26, 2615–2625. [Google Scholar] [CrossRef]
- Chen, H.X.; Sharon, E. IGF-1R as an anticancer target—Trials and tribulations. Chin. J. Cancer 2013, 32, 242–252. [Google Scholar] [CrossRef]
- Hakuno, F.; Takahashi, S.-I. IGF1 receptor signaling pathways. J. Mol. Endocrinol. 2018, 61, T69–T86. [Google Scholar] [CrossRef]
- Chapuis, N.; Tamburini, J.; Cornillet-Lefebvre, P.; Gillot, L.; Bardet, V.; Willems, L.; Park, S.; Green, A.S.; Ifrah, N.; Dreyfus, F.; et al. Autocrine IGF-1/IGF-1R signaling is responsible for constitutive PI3K/Akt activation in acute myeloid leukemia: Therapeutic value of neutralizing anti-IGF-1R antibody. Haematologica 2010, 95, 415–423. [Google Scholar] [CrossRef]
- Rasmussen, A.A.; Cullen, K.J. Paracrine/autocrine regulation of breast cancer by the insulin-like growth factors. Breast Cancer Res. Treat. 1998, 47, 219–233. [Google Scholar] [CrossRef] [PubMed]
- Pavelić, J.; Radaković, B.; Pavelić, K. Insulin-like growth factor 2 and its receptors (IGF 1R and IGF 2R/mannose 6-phosphate) in endometrial adenocarcinoma. Gynecol. Oncol. 2007, 105, 727–735. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Lu, G.; Yao, Y.; Gu, W. An autocrine IL-6/IGF-1R loop mediates EMT and promotes tumor growth in non-small cell lung cancer. Int. J. Biol. Sci. 2019, 15, 1882–1891. [Google Scholar] [CrossRef] [PubMed]
- Villanueva, J.; Vultur, A.; Lee, J.T.; Somasundaram, R.; Fukunaga-Kalabis, M.; Cipolla, A.K.; Wubbenhorst, B.; Xu, X.; Gimotty, P.A.; Kee, D.; et al. Acquired resistance to BRAF inhibitors mediated by a RAF kinase switch in melanoma can be overcome by cotargeting MEK and IGF-1R/PI3K. Cancer Cell 2010, 18, 683–695. [Google Scholar] [CrossRef]
- Gopal, Y.N.V.; Deng, W.; Woodman, S.E.; Komurov, K.; Ram, P.; Smith, P.D.; Davies, M.A. Basal and treatment-induced activation of AKT mediates resistance to cell death by AZD6244 (ARRY-142886) in Braf-mutant human cutaneous melanoma cells. Cancer Res. 2010, 70, 8736–8747. [Google Scholar] [CrossRef]
- Benito-Jardón, L.; Díaz-Martínez, M.; Arellano-Sánchez, N.; Vaquero-Morales, P.; Esparís-Ogando, A.; Teixidó, J. Resistance to MAPK inhibitors in melanoma involves activation of the IGF1R-MEK5-Erk5 pathway. Cancer Res. 2019, 79, 2244–2256. [Google Scholar] [CrossRef]
- Flanigan, S.A.; Pitts, T.M.; Newton, T.P.; Kulikowski, G.N.; Tan, A.C.; McManus, M.C.; Spreafico, A.; Kachaeva, M.I.; Selby, H.M.; Tentler, J.J.; et al. Overcoming IGF1R/IR resistance through inhibition of MEK signaling in colorectal cancer models. Clin. Cancer Res. 2013, 19, 6219–6229. [Google Scholar] [CrossRef]
- Wu, X.; Marmarelis, M.E.; Hodi, F.S. Activity of the heat shock protein 90 inhibitor gantespib in melanoma. PLoS ONE 2013, 8, e56134. [Google Scholar]
- Olbryt, M.; Rusin, A.; Fokt, I.; Habryka, A.; Tudrej, P.; Student, S.; Sochanik, A.; Zielinski, R.; Priebe, W. Bis-antracycline WP760 abrogates melanoma growth by transcription inhibition, p53 activation and IGF1R downregulation. Investig. New Drugs 2017, 35, 545–555. [Google Scholar] [CrossRef]
- Ramcharan, R.; Aleksic, T.; Kamdoum, W.P.; Gao, S.; Pfister, S.X.; Tanner, J.; Bridges, E.; Asher, R.; Watson, A.J.; Margison, G.P.; et al. IGF-1R inhibition induces schedule-dependent sensitization of human melanoma to temozolomide. Oncotarget 2015, 6, 39877–39890. [Google Scholar] [CrossRef]
- Herkert, B.; Kauffmann, A.; Mollé, S.; Schnell, C.; Ferrat, T.; Voshol, H.; Juengert, J.; Erasimus, H.; Marszalek, G.; Kazic-Legueux, M.; et al. Maximizing the efficacy of MAPK-targeted treatment in PTENLOF/BRAFMUT melanoma through PI3K and IGF1R inhibition. Cancer Res. 2016, 76, 390–402. [Google Scholar] [CrossRef]
- Huether, A.; Höpfner, M.; Baradari, V.; Schuppan, D.; Scherübl, H. Sorafenib alone or as combination therapy for growth control of cholangiocarcinoma. Biochem. Pharmacol. 2007, 73, 1308–1317. [Google Scholar] [CrossRef]
- Bugide, S.; Parajuli, K.R.; Chava, S.; Pattanayak, R.; Della Manna, D.L.; Shrestha, D.; Yang, E.S.; Cai, G.; Johnson, D.B.; Gupta, R. Loss of HAT1 expression confers BRAFV600E inhibitor resistance to melanoma cells by activating MAPK signaling via IGF1R. Oncogenesis 2020, 9, 44. [Google Scholar] [CrossRef]
- Strub, T.; Ghiraldini, F.G.; Carcamo, S.; Li, M.; Wroblewska, A.; Singh, R.; Goldberg, M.S.; Hasson, D.; Wang, Z.; Gallagher, S.J.; et al. SIRT6 haploinsufficiency induces BRAFV600E melanoma cell resistance to MAPK inhibitors via IGF signaling. Nat. Commun. 2018, 9, 3440. [Google Scholar] [CrossRef]
- Werner, H.; Sarfstein, R.; Bruchim, I. Investigational IGF1R inhibitors in early stage clinical trials for cancer therapy. Expert Opin. Invest. Drugs 2019, 28, 1101–1112. [Google Scholar] [CrossRef]
- Wilky, B.A.; Rudek, M.A.; Ahmed, S.; Laheru, D.A.; Cosgrove, D.; Donehower, R.C.; Nelkin, B.; Ball, D.; Doyle, L.A.; Chen, H.; et al. A phase I trial of vertical inhibition of IGF signaling using cixutumumab, and anti-IGF-1R antibody, and selumetinib, an MEK1/2 inhibitor, in advanced solid tumors. Br. J. Cancer 2015, 112, 24–31. [Google Scholar] [CrossRef]
- Zhu, C.; Wei, Y.; Wei, X. AXL receptor tyrosine kinase as a promising anti-cancer approach: Functions, molecular mechanisms and clinical applications. Mol. Cancer 2019, 18, 153. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.; Zang, H.; Wen, Q.; Fan, S. AXL in cancer: A modulator of drug resistance and therapeutic target. J. Exp. Clin. Cancer Res. 2023, 42, 148. [Google Scholar] [CrossRef] [PubMed]
- Zuo, Q.; Liu, J.; Huang, L.; Qin, Y.; Hawley, T.; Seo, C.; Merlino, G.; Yu, Y. AXL/AKT axis mediated-resistance to BRAF inhibitor depends on PTEN status in melanoma. Oncogene 2018, 37, 3275–3289. [Google Scholar] [CrossRef]
- Nyakas, M.; Fleten, K.G.; Haugen, M.H.; Engedal, N.; Sveen, C.; Farstad, I.N.; Florenes, V.A.; Prasmickaite, L.; Maeleandsmo, G.M.; Seip, K. AXL inhibition improves BRAF-targeted treartment in melanoma. Sci. Rep. 2022, 12, 5076. [Google Scholar] [CrossRef]
- Konieczkowski, D.J.; Johannessen, C.M.; Abudayyeh, O.; Kim, J.W.; Cooper, Z.A.; Piris, A.; Frederick, D.T.; Barzily-Rokni, M.; Straussman, R.; Haq, R.; et al. A melanoma cell state distinction influences sensitivity to MAPK pathway inhibitors. Cancer Discov. 2014, 4, 816–827. [Google Scholar] [CrossRef] [PubMed]
- Boshuizen, J.; Koopman, L.A.; Krijgsman, O.; Sharabi, A.; Gresnigt-van den Heuvel, E.; Ligtenberg, M.A.; Vredevoogd, D.W.; Kemper, K.; Kuilman, T.; Song, J.-Y.; et al. Cooperative targeting of melanoma heterogeneity with an AXL antibody-drug conjugate and BRAF/MEK inhibitors. Nat. Med. 2018, 24, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Xue, G.; Kohler, R.; Tang, F.; Hynx, D.; Wang, Y.; Orso, F.; Pretre, V.; Ritschard, R.; Hirschmann, P.; Cron, P.; et al. mTORC1/autophagy-regulated MerTK in mutant BRAFV600 melanoma with acquired resistance to BRAF inhibition. Oncotarget 2017, 8, 69204–69218. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sinik, L.; Minson, K.A.; Tentler, J.J.; Carrico, J.; Bagby, S.M.; Robinson, W.A.; Kami, R.; Burstyn-Cohen, T.; Eckhardt, S.G.; Wang, X.; et al. Inhibition of MERTK promotes suppression of tumor growth in BRAF mutant and BRAF wild-type melanoma. Mol. Cancer Ther. 2019, 18, 278–288. [Google Scholar] [CrossRef]
- Rosen, E.Y.; Won, H.H.; Zheng, Y.; Cocco, E.; Selcuklu, D.; Gong, Y.; Friedman, N.D.; de Bruijn, I.; Sumer, O.; Bielski, C.M.; et al. The evolution of RET inhibitor resistance in RET-driven lung and thyroid cancers. Nat. Commun. 2022, 13, 1450. [Google Scholar] [CrossRef]
- George, R.E.; Sanda, T.; Hanna, M.; Fröhling, S.; Luther II, W.; Zhang, J.; Ahn, Y.; Zhou, W.; London, W.B.; McGrady, P.; et al. Activating mutations in ALK provide a therapeutic target in neuroblastoma. Nature 2008, 455, 975–978. [Google Scholar] [CrossRef]
- Lamant, L.; Dastugue, N.; Pulford, K.; Delsol, G.; Mariamé, B. A new fusion gene TPM3-ALK in anaplastic large cell lymphoma created by a (1;2) (q25;p23) translocation. Blood 1999, 93, 3088–3095. [Google Scholar] [CrossRef]
- Roskoski, R., Jr. Anaplastic lymphoma kinase (ALK): Structure, oncogenic activation, and pharmacological inhibition. Pharmacol. Res. 2013, 68, 68–94. [Google Scholar] [CrossRef]
- Soda, M.; Choi, Y.L.; Enomoto, M.; Takada, S.; Yamashita, Y.; Ishikawa, S.; Fujiwara, S.; Watanabe, H.; Kurashina, K.; Hatanaka, H.; et al. Identification of the transforming EML4-ALK fusion gene in non-small cell lung cancer. Nature 2007, 448, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Elliott, J.; Bai, Z.; Hsieh, S.-C.; Kelly, S.E.; Chen, L.; Skidmore, B.; Yousef, S.; Zheng, C.; Stewart, D.J.; Wells, G.A. ALK inhibitors for non-small cell lung cancer: A systematic review and network meta-analysis. PLoS ONE 2020, 15, e0229179. [Google Scholar] [CrossRef]
- Janostiak, R.; Malvi, P.; Wajapeyee, N. Anaplastic lymphoma kinase confers resistance to BRAF kinase inhibitors in melanoma. iScience 2019, 16, 453–467. [Google Scholar] [CrossRef]
- Guo, W.; Liang, J.; Zhang, D.; Huang, X.; Lv, Y. Lung adenocarcinoma harboring complex EML4-ALK fusion and BRAF V600E co-mutation responded to alectenib. Medicine 2022, 101, 40. [Google Scholar] [CrossRef]
- Sui, A.; Song, H.; Li, Y.; Guo, L.; Wang, K.; Yuan, M.; Chen, R. BRAF V600E mutation as a novel mechanisms of acquired resistance to ALK inhibition in ALK-rearranged lung adenocarcinoma—A case report. Medicine 2021, 100, 8. [Google Scholar] [CrossRef]
- Pasau, T.; Wauters, E.; Wauters, I.; Duplaquet, F.; Pirard, L.; Pop-Stanciu, C.; D’Haene, N.; Dupont, M.; Vander Borght, T.; Rondelet, B.; et al. Case report: BRAF A598-T599insV mutation as a potential resistance mechanism to alectinib in ALK-rearranged lung adenocarcinoma. Front. Oncol. 2022, 12, 985446. [Google Scholar] [CrossRef]
- Fu, H.-L.; Valiathan, R.R.; Arkwright, R.; Sohail, A.; Mihai, C.; Kumarasiri, M.; Mahasenan, K.V.; Mobashery, S.; Huang, P.; Agarwal, G.; et al. Discoidin domain receptors: Unique receptor tyrosine kinases in collagen-mediated signaling. J. Biol. Chem. 2013, 288, 7430–7437. [Google Scholar] [CrossRef]
- De Moura, C.R.; Battistella, M.; Sohail, A.; Caudron, A.; Feugeas, J.P.; Podgorniak, M.-P.; Pages, C.; Dorval, S.M.; Marco, O.; Menashi, S.; et al. Discoidin domain receptors: A promising target in melanoma. Pigment Cell Melanoma Res. 2019, 32, 697–707. [Google Scholar] [CrossRef]
- De Moura, C.R.; Prunotto, M.; Sohail, A.; Battistella, M.; Jouenne, F.; Marbach, D.; Lebbé, C.; Fridman, R.; Mourah, S. Discoidin domain receptors in melanoma: Potential therapeutic targets to overcome MAPK inhibitor resistance. Front. Oncol. 2020, 10, 1748. [Google Scholar] [CrossRef]
- Berestjuk, I.; Lecacheur, M.; Carminati, A.; Diazzi, S.; Rovera, C.; Prod’homee, V.; Ohanna, M.; Popovic, A.; Mallavialle, A.; Larbret, F.; et al. Targeting discoidin domain receptors DDR1 and DDR2 overcomes matrix-mediated tumor cell adaption and tolerance to BRAF-targeted therapy in melanoma. EMBO Mol. Med. 2022, 14, e11814. [Google Scholar] [CrossRef]
- Lyon, A.; Tripathi, R.; Meeks, C.; He, D.; Wu, Y.; Liu, J.; Wang, C.; Chen, J.; Zhu, H.; Mukherjee, S.; et al. ABL1/2 and DDR1 drive MEKi resistance in NRAS-mutant melanomas by stabilizing RAF/MYC/ETS1 and promoting RAF homodimerization. Cancers 2023, 15, 954. [Google Scholar] [CrossRef]
- Belli, V.; Napolitano, S.; De Falco, V.; Suarato, G.; Perrone, A.; Guerrera, L.P.; Martini, G.; Della Corte, C.M.; Martinelli, E.; Morgillo, F.; et al. Targeting EphA2 and DDR signaling can overcome BRAF and MEK inhibitors acquired resistance in melanoma cell lines. Transl. Med. Commun. 2023, 8, 3. [Google Scholar] [CrossRef]
- Xiao, T.; Xiao, Y.; Wang, W.; Tang, Y.Y.; Xiao, Z.; Su, M. Targeting EphA2 in cancer. J. Hematol. Oncol. 2020, 13, 114. [Google Scholar] [CrossRef]
- Peng, Q.; Chen, L.; Wu, W.; Wang, J.; Zheng, X.; Chen, Z.; Jiang, Q.; Han, J.; Wei, L.; Wang, L.; et al. EPH receptor A2 governs a feedback loop that activates Wnt/β-catenin signaling in gastric cancer. Cell Death Dis. 2018, 9, 1146. [Google Scholar] [CrossRef]
- Hamaoka, Y.; Negishi, M.; Katoh, H. EphA2 is a key effector of the MEK/ERK/RSK pathway regulating glioblastoma cell proliferation. Cell Signal. 2016, 28, 937–945. [Google Scholar] [CrossRef]
- Wilson, K.; Shiuan, E.; Brantley-Sieders, D.M. Oncogenic functions and therapeutic targeting of EphA2 in cancer. Oncogene 2021, 40, 2483–2495. [Google Scholar] [CrossRef]
- Miao, B.; Ji, Z.; Tan, L.; Taylor, M.; Zhang, J.; Choi, H.G.; Frederick, D.T.; Kumar, R.; Wargo, J.A.; Flaherty, K.T.; et al. EphA2 is a mediator of vemurafenib resistance and a novel therapeutic target in melanoma. Cancer Discov. 2015, 5, 274–287. [Google Scholar] [CrossRef]
- Paraiso, K.H.T.; Thakur, M.D.; Fang, B.; Koomen, J.M.; Fedorenko, I.V.; John, J.K.; Tsao, H.; Flaherty, K.T.; Sondak, V.K.; Messina, J.L.; et al. Ligand independent EphA2 signaling drives the adoption of a targeted therapy-mediated metastatic melanoma phenotype. Cancer Discov. 2015, 5, 264–273. [Google Scholar] [CrossRef]
- Soumoy, L.; Schepkens, C.; Krayem, M.; Najem, A.; Tagliatti, V.; Ghanem, G.E.; Saussez, S.; Colet, J.-M.; Journe, F. Metabolic reprogramming in metastatic melanoma with acquired resistance to targeted therapies: Integrative metabolomic and proteomic analysis. Cancers 2020, 12, 1323. [Google Scholar] [CrossRef]
- Zhang, C.; Smalley, I.; Emmons, M.F.; Sharma, R.; Izumi, V.; Messina, J.; Koomen, J.M.; Pasquale, E.B.; Forsyth, P.A.; Smalley, K.S.M. Noncanonical EphA2 signaling is a driver of tumor-endothelial cell interactions and metastatic dissemination in BRAF inhibitor-resistant melanoma. J. Investig. Dermatol. 2021, 141, 840–851. [Google Scholar] [CrossRef] [PubMed]
- Azimi, A.; Tuominen, R.; Svedman, F.C.; Caramuta, S.; Pernemalm, M.; Stolt, M.F.; Kanter, L.; Kharaziha, P.; Lehtiö, J.; Johansson, C.H.; et al. Silencing FLI or targeting CD13/ANPEP lead to dephosphorylation of EPHA2, a mediator of BRAF inhibitor resistance, and induce growth arrest or apoptosis in melanoma cells. Cell Death Dis. 2017, 8, e3029. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Huang, J.; Ivan, C.; Sun, Y.; Ma, S.; Mangala, L.S.; Fellman, B.M.; Urbauer, D.L.; Jennings, N.B.; Ram, P.; et al. MEK inhibition overcomes resistance to EphA2-targeted therapy in uterine cancer. Gynecol. Oncol. 2021, 163, 181–190. [Google Scholar] [CrossRef]
- Huang, J.; Hu, W.; Bottsford-Miller, J.; Liu, T.; Han, H.D.; Zand, B.; Pradeep, S.; Roh, J.-W.; Thanapprapasr, D.; Dalton, H.J.; et al. Crosstalk between EphA2 and BRaf/CRaf is a key determinant of response to dasatinib. Clin. Cancer Res. 2014, 20, 1846–1855. [Google Scholar] [CrossRef]
- Annunziata, C.M.; Kohn, E.C.; LoRusso, P.; Houston, N.D.; Coleman, R.L.; Buzoianu, M.; Robbie, G.; Lechleider, R. Phase 1, open-label study of MEDI-547 in patients with relapsed or refractory solid tumors. Investig. New Drugs 2013, 31, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Gan, H.K.; Parakh, S.; Lee, F.T.; Tebbutt, N.C.; Ameratunga, M.; Lee, S.T.; O’Keefe, G.J.; Gong, S.J.; Vanrenen, C.; Caine, J.; et al. A phase 1 safety and bioimaging trial of antibody DS-8895a against EphA2 in patients with advanced or metastatic EphA2 positive cancers. Investig. New Drugs 2022, 40, 747–755. [Google Scholar] [CrossRef]
- Sen, B.; Peng, S.; Tang, X.; Erickson, H.S.; Galindo, H.; Mazumdar, T.; Stewart, D.J.; Wistuba, I.; Johnson, F.M. Kinase impaired BRAF mutations confer lung cancer sensitivity to dasatinib. Sci. Transl. Med. 2012, 4, 136ra70. [Google Scholar] [CrossRef]
- Storkus, W.J.; Maurer, D.; Lin, Y.; Ding, F.; Bose, A.; Lowe, D.; Rose, A.; DeMark, M.; Karapetyan, L.; Taylor, J.L.; et al. Dendritic cell vaccines targeting tumor blood vessel antigens in combination with dasatinib induce therapeutic immune responses in patients with checkpoint-refractory advanced melanoma. J. Immunother. Cancer 2021, 9, e003675. [Google Scholar] [CrossRef]
- Dev, S.S.; Abidin, S.A.Z.; Farghadani, R.; Ithman, I.; Naidu, R. Receptor tyrosine kinases and their signaling pathways as therapeutic targets of curcumin in cancer. Front. Pharmacol. 2021, 12, 772510. [Google Scholar]
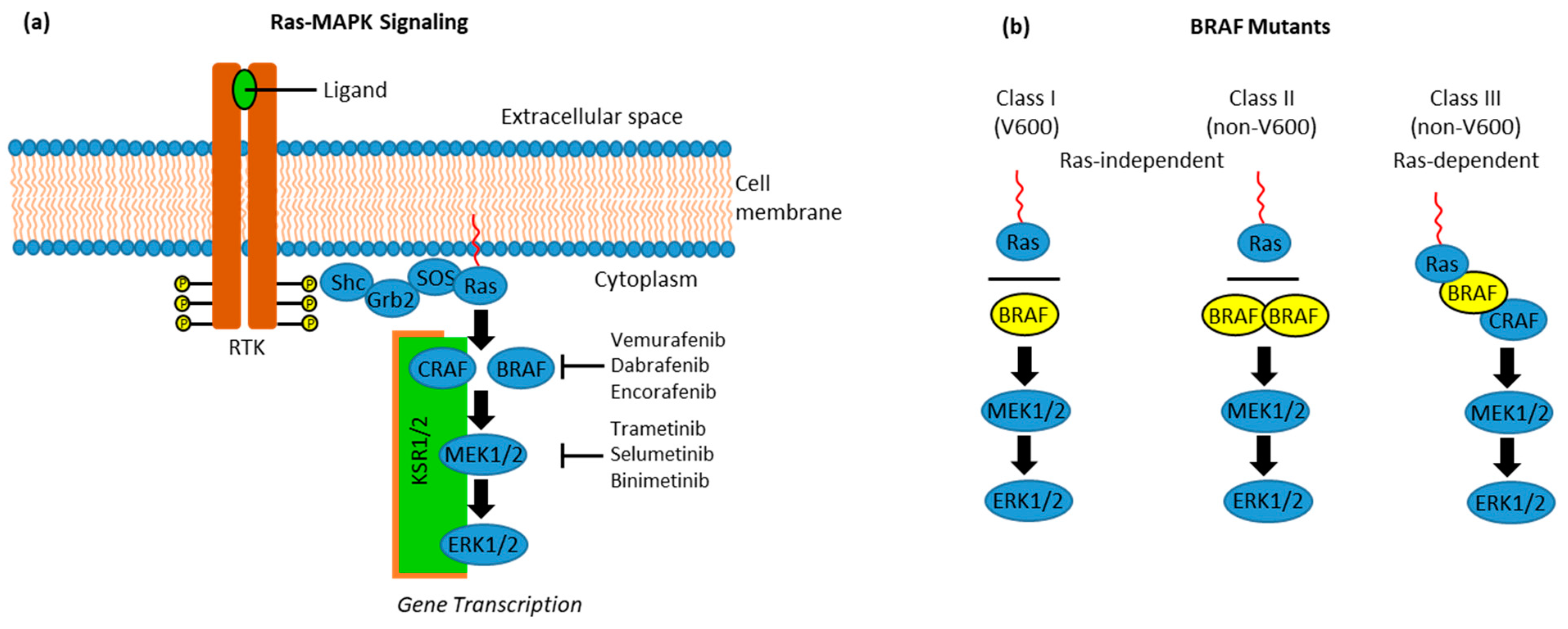
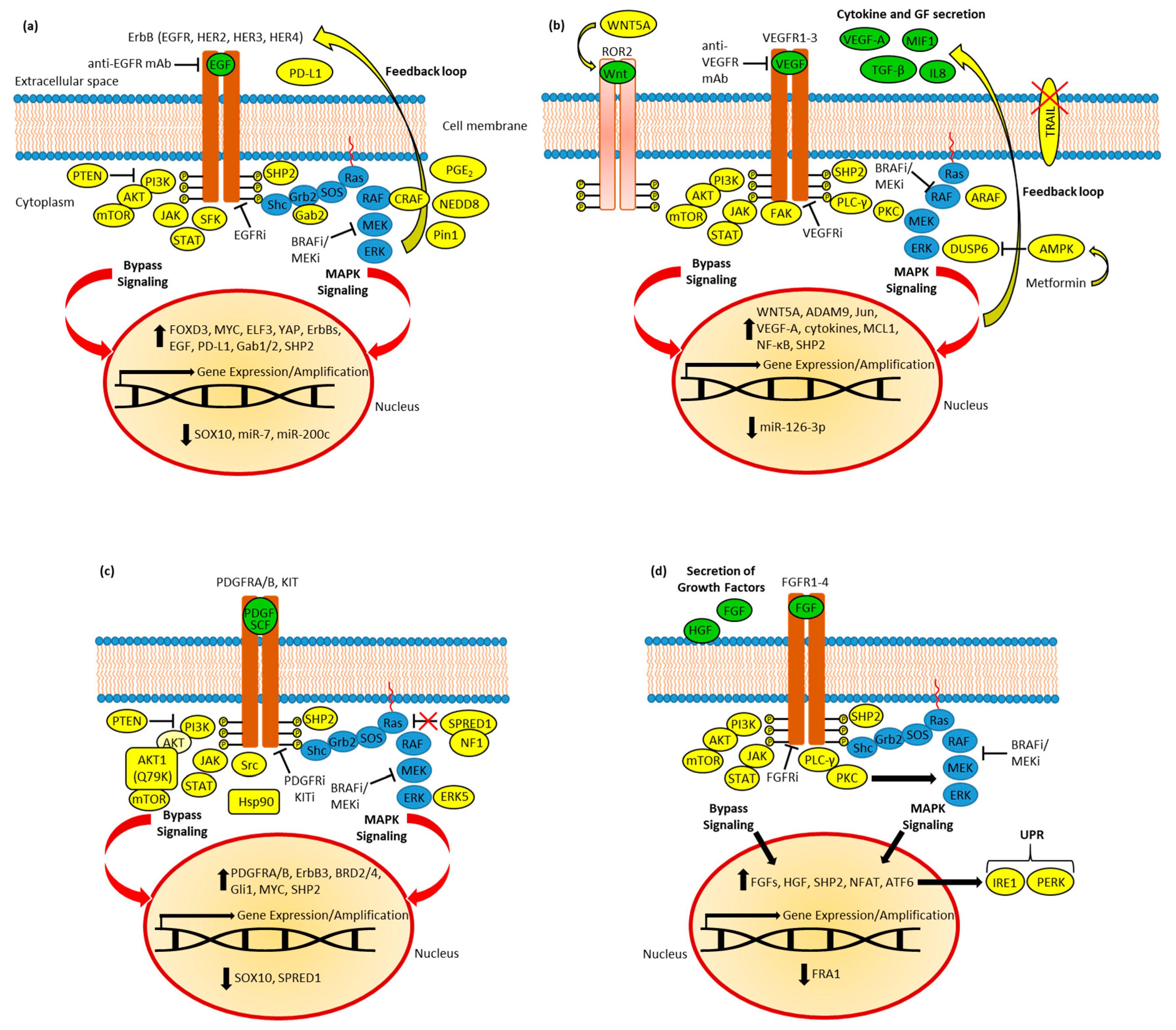
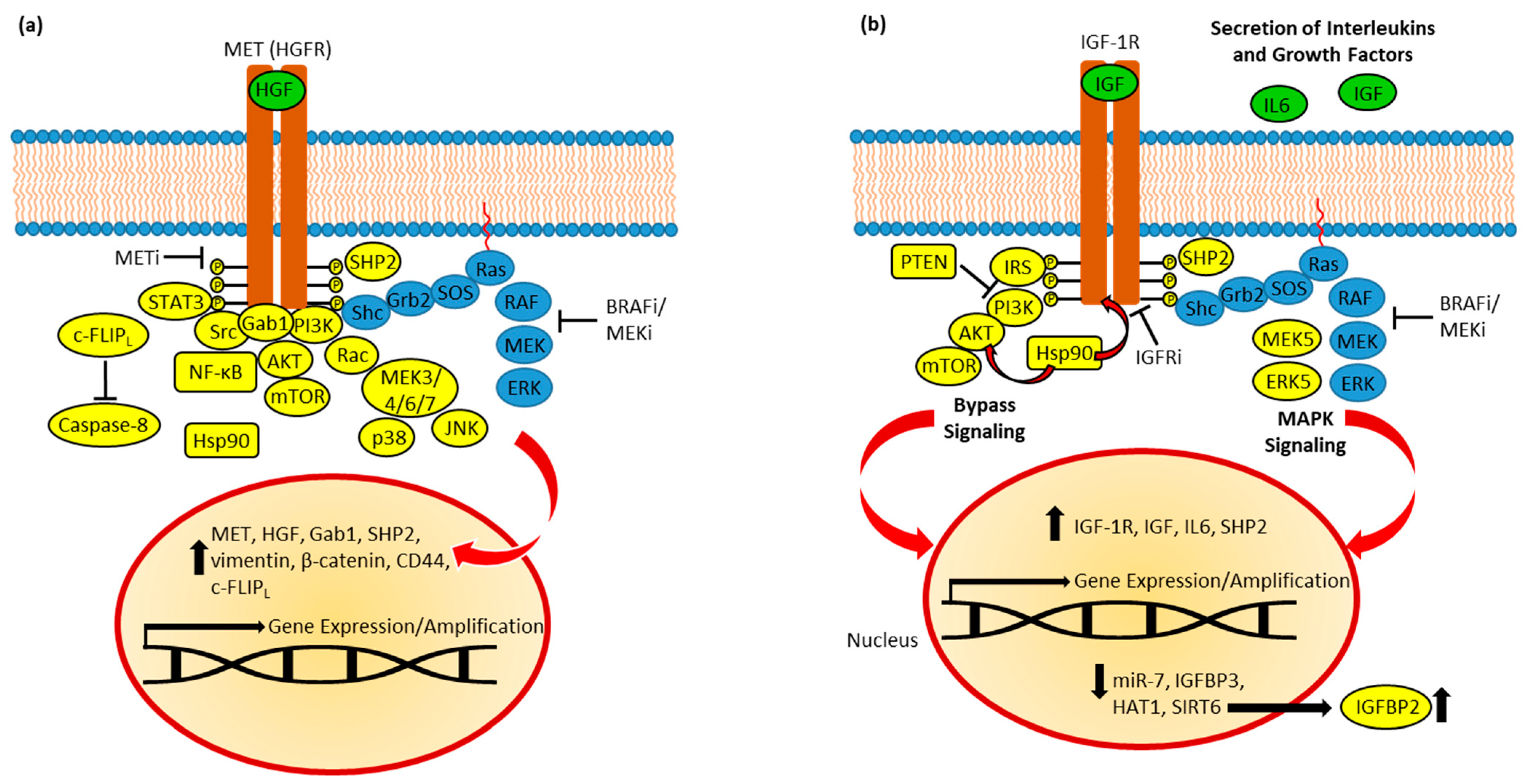
| ErbB Inhibitor | Mechanisms (Cancers/Cell Lines) | Clinical Studies | References |
|---|---|---|---|
| Gefitinib | Additive effects; suppression of colony formation and migration (BRAF mutant melanoma); resistance formation by MET and AKT activation (BRAF mutant CRC) | Increased activity by upregulated prostaglandin upon acquired vemurafenib resistance (BRAF mutant melanoma) | [66,67,74,103] |
| Erlotinib | Suppression of BRAF mutant CRC growth in vitro and in vivo (HT-29 and WiDr); overcomes acquired PLX8394 resistance (lung adenocarcinoma); overcomes acquired BRAF inhibitor resistance based on high EGFR levels (cutaneous melanoma) | Overall response of 32% in combination with vemurafenib (phase 1b/2 EVICT study, BRAFV600E CRC) | [65,82,99,119] |
| Afatinib | Active in combination with AKT inhibitors and vemurafenib (BRAF mutant melanoma); additive effects in combination with vemurafenib (BRAFV600E CRC) | - | [66,78] |
| Lapatinib | Synergy combined with the BRAF inhibitor PLX4720 (BRAF inhibitor-resistant BRAF mutant melanoma), and in combination with the AKT inhibitor MK2206, which revealed distinct synergistic effects (BRAF mutant CRC cells); efficient in blocking feedback loops when combined with NEDD8 inhibitor (BRAF mutant CRC); suppression of MAPK rebound effect and re-sensitization to BRAF/MEK inhibitor treatment and radioiodine therapy (BRAFV600E thyroid cancer cells); promising anticancer effects in combination with the YAP inhibitor (BRAFV600E thyroid cancer cells) | - | [75,76,77,101,106] |
| Neratinib | Synergistic effects with HDAC inhibitors; ROS-dependent autophagosome formation (BRAFV600E cutaneous melanoma cells) | - | [79] |
| Canertinib | Apoptosis induction; blocked ErbB signaling; blocking of EGF-induced AKT; inhibition of p-STAT3 in EGF’s absence (BRAF mutant melanoma cells) | - | [80] |
| Sapitinib | Re-sensitization effect (vemurafenib-resistant BRAF mutant canine transitional cell carcinoma) | - | [81] |
| Lifirafenib | Reversible inhibition of RAF dimers of wild-type ARAF, BRAF, and CRAF, and also BRAFV600E and EGFR; higher activity than vemurafenib and dabrafenib (BRAF mutant CRC); overcomes vemurafenib resistance and suppresses EGFR-mediated MAPK re-activation (non-V600 BRAF mutant lung cancers) | Clinical responses in BRAF mutant melanoma, thyroid cancer, and ovarian cancer (phase 1); ongoing clinical phase 1b/2 study in combination with the MEK inhibitor mirdametinib with KRAS and RAF mutant solid tumors | [83,84,85,86] |
| Osimertinib | Leads to acquired V600 and non-V600 BRAF mutations (NSCLC) | Clinical responses to triple combination therapy (plus dabrafenib and trametinib), including the breach of BRAFV600E-mediated osimertinib resistance (EGFR mutant/BRAF mutant lung adenocarcinoma with bone metastases and EGFR(del19) mutant/BRAFV600E NSCLC with leptomeningeal brain metastasis); problematic BRAF fusion gene (BTN2A1-BRAF) as acquired osimertinib resistance factor (advanced NSCLC) | [87,88,89,90,92] |
| Cetuximab | Combination with the mTOR inhibitor PP242 inhibited tumor growth (BRAFV600E mutant HT-29 xenografts); increased cell killing activity of peripheral blood natural killer (NK) cells (HT-29 cells); combination with dabrafenib induced PTEN and suppressed Src and c-Myc (BRAFV600E mutant CRC cells); sensitive class III BRAF mutant cancers (lung and colorectal cancers); efficient blocking of feedback loops when combined with the NEDD8 inhibitor (BRAF mutant CRC) | Prolonged overall and progression-free survival in combination with encorafenib (BEACON phase 3 with BRAFV600E mutant metastatic CRC); complete response in combination with vemurafenib and the topoisomerase I inhibitor irinotecan (case report of advanced pretreated BRAFV600E CRC with liver metastases); ongoing phase 2 study plus irinotecan as “re-challenge” third-line therapy of pretreated Ras/BRAF mutant CRC; superior effects of this cetuximab-based triple therapy (SWOG phase 2 study, BRAF mutant metastatic CRC); prolonged overall response rate and disease control in combination with vemurafenib and irinotecan (VIC) as a first-line therapy (unresectable BRAFV600E mutant CRC); activity against class III BRAF mutants (several trials, advanced or metastatic CRCs) | [15,17,58,94,95,96,101,118,120,121,122,123] |
| Panitumumab | - | Remarkable response (case report, pretreated non-V600 metastatic CRC); activity against class III BRAF mutants (several trials, advanced or metastatic CRCs) | [58,123,124] |
| Trastuzumab emtansine | Highly active; combination with metformin upregulates endocytic calveolin-1 expression and increased anticancer activity (HER2-positive BRAF mutant CRC cells and xenograft models) | - | [97] |
| Ascorbic acid | ROS formation, ATP depletion, MAPK and AKT suppression (BRAF mutant thyroid cancer cells), and suppression of thyroid cancer growth in vivo | - | [126,127] |
| Curcumin | COX-2-dependent MAPK suppression (pancreatic and lung adenocarcinoma), suppression of p-EGFR and EGFR expression (CRC), and prevention of BRAF mutant CRC formation (murine BRAFV637E/+/Villin-CreERT2/+ model) | - | [129,130,131,132,133] |
| Resveratrol | AKT dephosphorylation (BRAFV600E melanoma) and STAT3 suppression (THJ-16T MKRN1-BRAF fusion mutation and THJ-21T BRAFV600E ATC cells) | - | [134,135] |
| Genistein | Suppression of BRAF and ERK (QT-RRE cells) | - | [139] |
| VEGFR Inhibitor | Mechanisms (Cancers/Cell Lines) | Clinical Studies | References |
|---|---|---|---|
| Sorafenib | Superior to vemurafenib (BRAFV595E canine transitional cell carcinoma cells); apoptosis induction; suppression of MAPK and AKT; reduced p-VEGFR1/2/3 (BRAFV600E thyroid carcinoma cells); active against vemurafenib-insensitive melanoma cell cells with BRAF fusion protein, drug resensitization (vemurafenib-resistant BRAFV600E mutant A431 melanoma cells with BRAFV600E loci and BCORL1 mutations); active against non-V600 mutation (BRAF-G469R and BRAF-N581S mutant lung cancer cells); synergy in combination with the MEK inhibitor selumetinib or the CDK inhibitor flavopiridol in non-V600 tumors (MDA-MB-231 triple-negative breast carcinoma (G464V)); sensitization to TRAIL (BRAFV600E HT-29 CRC) | Stable disease for seven months in combination with cetuximab (case report, pretreated BRAFV600E mutant CRC patient); partial response in combination with vemurafenib (BRAFV600E mutant melanoma, lung adenocarcinoma, papillary thyroid cancer, and ovarian cancer) | [147,148,154,155,156,157,158,160,180,181] |
| Regorafenib | Activity against BRAFV600E and non-V600 mutant thyroid cancers | Combination with panitumumab slowed down disease progression (case report, pretreated BRAFV600E mutant CRC patient) | [159,180] |
| Sunitinib | Sunitinib resistance by upregulation of RAS/MAPK (BRAF mutant thyroid cancers) | - | [163] |
| Pazopanib | Blocking of MAPK signaling (BRAF mutant HER2-positive breast cancer cells); reduced p-MEK1/2, p-ERK1/2, and p-VEGFR1/2 (HER2-transfected MDA-MB-231 tumor cells and brain metastases); no interaction with BRAFV600E but with exon 11 BRAF mutant | - | [164] |
| Axitinib | Additive effect in combination with dabrafenib or PLX4720; blocking of invasion and migration; induction of c-Jun signaling and suppression of p-H3 and p-AURKA (BRAFV600E mutant ATC); tumor growth inhibition and prolonged survival (orthotopic ATC mouse model); combination with vemurafenib suppressed tumor growth; cytokine and growth factor release (BRAFV600E HT-29 and COLO-205 CRC xenografts) | - | [165,166] |
| Ponatinib | Synergistic activity in combination with PLX4720; pro-apoptotic; suppression of p-MEK/ERK and c-Jun (BRAFV600E ATC cells); re-sensitization to PLX4720 (PLX4720-resistant BRAFV600E ATC); inhibition of tumor growth (orthotopic ATC mouse models) | - | [167] |
| RAF265 | Strong antiproliferative activities (BRAFV600E HT-29 and BRAFG463V MDA-MB-231 cells); inhibition of tumor growth (HT-29 and MDA-MB-231 xenografts); active against patient-derived advanced melanomas; synergistic effects in combination with PI3K inhibitor ZSTK474 (thyroid carcinoma cells including BRAF mutant cell lines) | Four partial responses and significant decrease in VEGFR-2 levels (first-in-human phase 1 clinical trial, melanoma with the BRAFV600E mutation) | [168,169,170,171,185] |
| Bevacizumab | Inhibition of pro-invasive properties of dabrafenib (dabrafenib-resistant A431R melanoma cells) | Clinically applied as first-line therapy of RAS and/or BRAF mutant CRC; promising second-line combination therapy plus fluoropyrimidine with high disease control (74%) and overall survival (25.6 months, FOLFOX pre-treated BRAFV600E metastatic CRC) | [146,173,186,187,189] |
| Ramucirumab | - | Efficacy as a second-line treatment of pre-treated BRAF mutant CRC; substantial benefit plus FOLFIRI in BRAF mutant patient groups (global phase 3 RAISE trial; metastatic CRC patients pre-treated with bevacizumab, oxaliplatin, and fluoropyrimidine) | [188,190] |
| Aflibercept | Inhibition of VEGF and PlGF and breach of bevacizumab resistance | Efficacy as a second-line treatment of pre-treated BRAF mutant CRC; improved overall and progression-free survival in combination with FOLFIRI (phase 3 VELOUR trial, oxaliplatin-pretreated metastatic CRC); pronounced response and stable disease for more than four months as follow-up therapy in combination with FOLFIRI (case report, pretreated metastatic BRAFV600E mutant CRC); progression-free survival (ca. one year) in combination with FOLFIRI (case report, pretreated metastatic BRAFD594N CRC) | [188,191,192] |
| PDGFR/KIT Inhibitor | Mechanisms (Cancers/Cell Lines) | Clinical Studies | References |
|---|---|---|---|
| Imatinib | Suppression of p-AKT and p-ERK in combination with BRAF inhibitors; restoration of PLX4720 activity (animals with BRAFV600E A375 melanoma); suppression of mutant KIT activity but no inhibition of MAPK signaling (imatinib-resistant BRAF mutant GIST) | Inactive against BRAF mutant GIST | [221,238,241,244] |
| Masatinib | Synergy in combination with BRAF inhibitor PLX4720 independent from AKT and MAPK reactivation (BRAFV600E melanoma) | - | [75] |
| Crenolanib | Active in combination with Hsp90 inhibitor XL888 (BRAF inhibitor-resistant melanoma cells); pro-apoptotic effects (BRAF inhibitor-sensitive and -resistant BRAFV600E melanoma cells) | - | [224,230] |
| Sunitinib | Pro-apoptotic effects (BRAF inhibitor-sensitive and -resistant BRAFV600E melanoma) cells | Inactive against BRAF mutant GIST | [230,244] |
| AG1296 | Suppression of p-PDGFRA and p-PDGFRB; apoptosis induction and inhibition of cell migration; inhibition of tumor growth in vivo (vemurafenib-resistant BRAFV600E A375 melanoma) | - | [231] |
| Cediranib | Suppression of p-PDGFRA/B; synergistic effects in combination with PLX4720 and selumetinib (PLX4720-resistant BRAFV600E melanoma cells) | - | [233] |
| Regorafenib | - | Complete response by first-line treatment (case report, BRAFV600E mutant KIT/PDGFRA-wild-type metastatic GIST); progression-free survival of 3.45 months of a BRAFV600E mutant succinate dehydrogenase (SDH)-proficient GIST patient (phase 2 REGISTRI trial with regorafenib as a first-line treatment for KIT/PDGFRA-wild-type metastatic GIST) | [246,247] |
| Inhibitor | Mechanisms (Cancers/Cell Lines) | Clinical Studies | References |
|---|---|---|---|
| SU5402 and PD166866 (FGFR inhibitors) | Antiproliferative and pro-apoptotic, suppressed p-AKT5 and p-STAT3, and synergy with sorafenib and BRAFV600E-selective inhibitor RG7204 (BRAFV600E melanomas) | - | [250] |
| Dovitinib (FGFR inhibitor) | Suppression of p-FGFR1, p-ERK, and tumor growth (BRAFV600E mutant HT-29 xenograft), drug sensitization (vemurafenib-resistant RKO CRC cells), enforced vemurafenib and selumetinib activity (BRAF/MEK inhibitor-resistant BRAF mutant YUKSI melanoma cells, and vemurafenib-resistant YUMAC XR4MC8 melanoma xenograft) | - | [256,257] |
| BGJ-398 (FGFR inhibitor) | Antiproliferative (BRAFV600E melanoma cells) | Currently being investigated (LOGIC-2 phase 2 trial with patients suffering from BRAF/MEK inhibitor-resistant advanced or metastatic BRAFV600E melanoma) | [254,261] |
| Aspirin | Suppression of FGFR, PI3K, and Notch signaling, reduced lesion size and number of distant colorectal cancer metastases (BrafV637E/+ and Villin-CreERT2/+ mice) | - | [258] |
| PHA665752 (MET inhibitor) | Combination with vemurafenib inhibited MET, p-AKT, and p-ERK, increased anticancer activity (BRAF mutant ATC cells; orthotopic BRAFV600E mutant ATC xenograft), and combination with vemurafenib reversed EMT (BRAFV600E ATC cells) | - | [274,275] |
| Crizotinib (MET inhibitor) | Active against recurrent ATCs treated with the RAF/MEK inhibitor, in combination with afatinib antiproliferative, pro-apoptotic, and anti-invasive activities (cutaneous melanoma cells), reduced WEE1 and IGF1R levels and suppressed in vivo tumor growth (A375 melanoma), and abrogation of anti-apoptotic c-FLIPL in combination with selumetinib (BRAF mutant CRC) | Well tolerated and response rate of 23% in combination with vemurafenib (BRAF/MEK inhibitor pre-treated BRAF mutant advanced melanoma and lung adenocarcinoma) | [181,276,280,281] |
| PF-04217903 (MET inhibitor) | Active against recurrent ATCs treated with RAF/MEK inhibitor; in vivo activity against a MET-amplified ATC allograft model | - | [276] |
| Picropodophyllin (IGF-1R inhibitor) | Combination with a MEK inhibitor (GSK1120212 or selumetinib) suppressed tumor growth (BRAF inhibitor-resistant melanoma cells and spheroids) | - | [293] |
| Linsitinib (IGF-1R inhibitor) | Suppression of ERK5 and tumor growth in vitro (3D spheroids) and in vivo (MAPK inhibitor-resistant melanoma), synergy with MEK1/2 inhibitor U0126 (CRC cell lines), combination with AZ3801 sensitized cells to temozolomide (BRAF mutant and wild-type melanoma), combination with temozolomide led to distinct growth inhibition (BRAFV600E/p53-wild-type A375M melanoma xenografts), combination with dabrafinib suppressed p-IGF-1R and p-AKT, and breaks resistance in vitro and in vivo (SIRT6 haploinsufficient BRAFV600E melanoma) | Weak data so far | [295,296,299,303,304] |
| AZ3801 (IGF-1R inhibitor) | Sensitization of BRAF mutant and BRAF wild-type (p53-wild-type) melanoma cells to temozolomide | - | [299] |
| Cixutumumab (IGF-1R inhibitor) | - | Progression-free survival of more than 6 months in combination with selumetinib (phase 1, BRAF mutant thyroid cancer and CRC) | [305] |
| Inhibitor | Mechanisms (Cancers/Cell Lines) | Clinical Studies | References |
|---|---|---|---|
| Bemcentinib (AXL inhibitor) | Suppression of p-AXL and p-AKT; re-sensitization to vemurafenib (resistant melanoma cells and tumors); suppressed p-ERK and p-S6, augmented vemurafenib activity (in vitro, ex vivo, and in vivo); enhanced apoptosis and ferroptosis; suppressed autophagy (resistant melanoma); suppression of p-AKT and p-ERK (BRAF inhibitor-resistant BRAFV600 mutant melanoma) | Clinical trials started and ongoing | [307,308,309,310] |
| Cabozantinib (AXL inhibitor) | Suppression of p-AKT and p-ERK (BRAF inhibitor-resistant BRAFV600 mutant melanoma) | - | [310] |
| XL880 (AXL inhibitor) | Suppression of p-AKT and p-ERK (BRAF inhibitor-resistant BRAFV600 mutant melanoma) | - | [310] |
| AXL-107-MMAE (AXL inhibitor) | Cooperative activity in combination with AXL-upregulating BRAF/MEK inhibitors (melanoma) | - | [311] |
| UNC2025 (AXL inhibitor) | Induction of cell death; suppression of ERK, AKT, STAT6, and tumor growth in combination with vemurafenib (BRAF mutant melanoma cells and xenografts) | - | [313] |
| Ceritinib (ALK inhibitor) | Suppression of vemurafenib resistance in vitro and in vivo; formation of dual vemurafenib–ceritinib resistance by suppressed apoptosis overcome by pro-apoptotic AT101 (melanoma) | - | [313] |
| Alectenib (ALK inhibitor) | - | Complete remission and progression-free survival for over 26 months (case report, pretreated EML4-ALK fusion and BRAFV600E mutant NSCLC) | [321] |
| DDR1-IN-1 (DDR inhibitor) | Suppression of BRAF mutant melanoma xenografts | - | [325] |
| Imatinib (DDR inhibitor) | Breach of BRAF/MEK inhibitor resistance induced by the extracellular matrix (BRAFV600E melanoma); increased vemurafenib activity by suppression of collagen remodeling (BRAFV600E melanoma xenografts) | - | [327] |
| ALW-II-41-27 (DDR inhibitor) | Antiproliferative and anti-migratory activities; suppression of p-DDR1/2, p-AKT, and p-MEK (vemurafenib/cobimetinib-resistant BRAFV600E melanoma) | - | [329] |
| ALW-II-41-27 (EphA2 inhibitor) | Synergy; re-sensitization to vemurafenib; suppression of p-AKT and p-ERK, pro-apoptotic effects; tumor growth inhibition (BRAFV600E mutant vemurafenib-resistant and -sensitive melanoma cells and xenografts); downregulation of p-EphA2, p-AKT, and p-MEK (vemurafenib/cobimetinib-resistant BRAFV600E melanoma) | - | [329,334] |
| Dasatinib (EphA2 inhibitor) | Sensitivity accompanied by MAPK signaling suppressor caveolin-1 upregulation (uterine cancer cells) | High response and disease-free for a min. of 4 years (case report, patient with kinase impaired non-V600 BRAFY472C mutation NSCLC); immune response (CD8+ T cell response) and clinical response (46%) in combination with dendritic cell vaccines (phase 2 trial, advanced checkpoint-refractory and BRAF mutant melanoma) | [340,343,344] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biersack, B.; Tahtamouni, L.; Höpfner, M. Role and Function of Receptor Tyrosine Kinases in BRAF Mutant Cancers. Receptors 2024, 3, 58-106. https://doi.org/10.3390/receptors3010005
Biersack B, Tahtamouni L, Höpfner M. Role and Function of Receptor Tyrosine Kinases in BRAF Mutant Cancers. Receptors. 2024; 3(1):58-106. https://doi.org/10.3390/receptors3010005
Chicago/Turabian StyleBiersack, Bernhard, Lubna Tahtamouni, and Michael Höpfner. 2024. "Role and Function of Receptor Tyrosine Kinases in BRAF Mutant Cancers" Receptors 3, no. 1: 58-106. https://doi.org/10.3390/receptors3010005
APA StyleBiersack, B., Tahtamouni, L., & Höpfner, M. (2024). Role and Function of Receptor Tyrosine Kinases in BRAF Mutant Cancers. Receptors, 3(1), 58-106. https://doi.org/10.3390/receptors3010005








