Orally Administered N-Oleoyl Alanine Blocks Acute Opioid Withdrawal Induced-Conditioned Place Preference and Attenuates Somatic Withdrawal following Chronic Opioid Exposure in Rats
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Drugs
2.3. Apparatus
2.4. Surgery
2.5. Procedures
2.5.1. Experiment 1
2.5.2. Experiment 2
2.6. Data Analysis
3. Results
3.1. Experiment 1
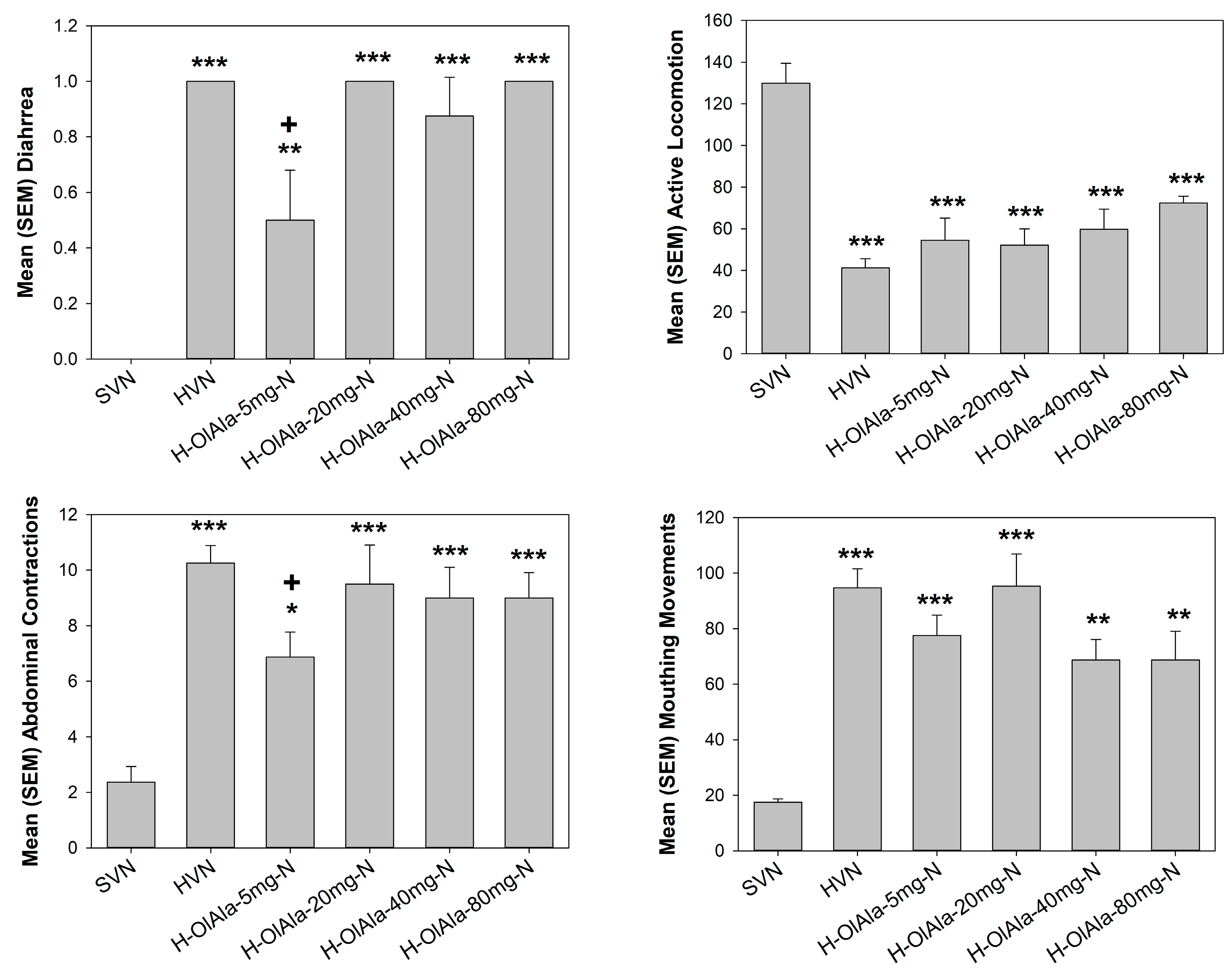
3.2. Experiment 2
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Burstein, S.H.; McQuain, C.A.; Ross, A.H.; Salmonsen, R.A.; Zurier, R.E. Resolution of inflammation by N-arachidonoylglycine. J. Cell Biochem. 2011, 112, 3227–3233. [Google Scholar] [CrossRef] [PubMed]
- Dludla, P.V.; Nkambule, B.B.; Mazibuko-Mbeje, S.E.; Nyambuya, T.M.; Marcheggiani, F.; Cirilli, I.; Ziqubu, K.; Shabalala, S.C.; Johnson, R.; Louw, J.; et al. N-Acetyl Cysteine Targets Hepatic Lipid Accumulation to Curb Oxidative Stress and Inflammation in NAFLD: A Comprehensive Analysis of the Literature. Antioxidants 2020, 9, 1283. [Google Scholar] [CrossRef] [PubMed]
- Raboune, S.; Stuart, J.M.; Leishman, E.; Takacs, S.M.; Rhodes, B.; Basnet, A.; Jameyfield, E.; McHugh, D.; Widlanski, T.; Bradshaw, H.B. Novel endogenous N-acyl amides activate TRPV1-4 receptors, BV-2 microglia, and are regulated in brain in an acute model of inflammation. Front. Cell Neurosci. 2014, 8, 195. [Google Scholar] [CrossRef] [PubMed]
- Long, J.Z.; Svensson, K.J.; Bateman, L.A.; Lin, H.; Kamenecka, T.; Lokurkar, I.A.; Lou, J.; Rao, R.R.; Chang, M.R.; Jedrychowski, M.P.; et al. The Secreted Enzyme PM20D1 Regulates Lipidated Amino Acid Uncouplers of Mitochondria. Cell 2016, 166, 424–435. [Google Scholar] [CrossRef]
- Wang, S.; Xu, Q.; Shu, G.; Wang, L.; Gao, P.; Xi, Q.; Zhang, Y.; Jiang, Q.; Zhu, X. N-Oleoyl glycine, a lipoamino acid, stimulates adipogenesis associated with activation of CB1 receptor and Akt signaling pathway in 3T3-L1 adipocyte. Biochem. Biophys. Res. Commun. 2015, 466, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.M.; Bisogno, T.; Petros, T.J.; Chang, S.Y.; Zavitsanos, P.A.; Zipkin, R.E.; Sivakumar, R.; Coop, A.; Maeda, D.Y.; De Petrocellis, L.; et al. Identification of a new class of molecules, the arachidonyl amino acids, and characterization of one member that inhibits pain. J. Biol. Chem. 2001, 276, 42639–42644. [Google Scholar] [CrossRef] [PubMed]
- Mostyn, S.N.; Wilson, K.A.; Schumann-Gillett, A.; Frangos, Z.J.; Shimmon, S.; Rawling, T.; Ryan, R.M.; O’Mara, M.L.; Vandenberg, R.J. Identification of an allosteric binding site on the human glycine transporter, GlyT2, for bioactive lipid analgesics. Elife 2019, 8, e47150. [Google Scholar] [CrossRef] [PubMed]
- Vuong, L.A.; Mitchell, V.A.; Vaughan, C.W. Actions of N-arachidonyl-glycine in a rat neuropathic pain model. Neuropharmacology 2008, 54, 189–193. [Google Scholar] [CrossRef] [PubMed]
- Lauritano, A.; Cipollone, I.; Verde, R.; Kalkan, H.; Moriello, C.; Iannotti, F.A.; Di Marzo, V.; Piscitelli, F. The endocannabinoidome mediator N-oleoylglycine is a novel protective agent against 1-methyl-4-phenyl-pyridinium-induced neurotoxicity. Front. Aging Neurosci. 2022, 14, 926634. [Google Scholar] [CrossRef]
- Donvito, G.; Piscitelli, F.; Muldoon, P.; Jackson, A.; Vitale, R.M.; D’Aniello, E.; Giordano, C.; Ignatowska-Jankowska, B.M.; Mustafa, M.A.; Guida, F.; et al. N-Oleoyl-glycine reduces nicotine reward and withdrawal in mice. Neuropharmacology 2019, 148, 320–331. [Google Scholar] [CrossRef]
- Lin, Q.; Hai, J.; Yao, L.Y.; Lu, Y. Neuroprotective effects of NSTyr on cognitive function and neuronal plasticity in rats of chronic cerebral hypoperfusion. Brain Res. 2010, 1325, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Petrie, G.N.; Wills, K.L.; Piscitelli, F.; Smoum, R.; Limebeer, C.L.; Rock, E.M.; Humphrey, A.E.; Sheppard-Perkins, M.; Lichtman, A.H.; Mechoulam, R.; et al. Oleoyl glycine: Interference with the aversive effects of acute naloxone-precipitated MWD, but not morphine reward, in male Sprague-Dawley rats. Psychopharmacology 2019, 236, 2623–2633. [Google Scholar] [CrossRef] [PubMed]
- Egashira, N.; Shirakawa, A.; Abe, M.; Niki, T.; Mishima, K.; Iwasaki, K.; Oishi, R.; Fujiwara, M. N-acetyl-L-cysteine inhibits marble-burying behavior in mice. J. Pharmacol. Sci. 2012, 119, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Ayoub, S.M.; Piscitelli, F.; Silvestri, C.; Limebeer, C.L.; Rock, E.M.; Smoum, R.; Farag, M.; de Almeida, H.; Sullivan, M.T.; Lacroix, S.; et al. Spontaneous and Naloxone-Precipitated Withdrawal Behaviors from Chronic Opiates are Accompanied by Changes in N-Oleoylglycine and N-Oleoylalanine Levels in the Brain and Ameliorated by Treatment With These Mediators. Front. Pharmacol. 2021, 12, 706703. [Google Scholar] [CrossRef] [PubMed]
- Ayoub, S.M.; Smoum, R.; Farag, M.; Atwal, H.; Collins, S.A.; Rock, E.M.; Limebeer, C.L.; Piscitelli, F.; Iannotti, F.A.; Lichtman, A.H.; et al. Oleoyl alanine (HU595): A stable monomethylated oleoyl glycine interferes with acute naloxone precipitated morphine withdrawal in male rats. Psychopharmacology 2020, 237, 2753–2765. [Google Scholar] [CrossRef] [PubMed]
- Rock, E.M.; Ayoub, S.M.; Limebeer, C.L.; Gene, A.; Wills, K.L.; DeVuono, M.V.; Smoum, R.; Di Marzo, V.; Lichtman, A.H.; Mechoulam, R.; et al. Acute naloxone-precipitated morphine withdrawal elicits nausea-like somatic behaviors in rats in a manner suppressed by N-oleoylglycine. Psychopharmacology 2020, 237, 375–384. [Google Scholar] [CrossRef] [PubMed]
- Piscitelli, F.; Guida, F.; Luongo, L.; Iannotti, F.A.; Boccella, S.; Verde, R.; Lauritano, A.; Imperatore, R.; Smoum, R.; Cristino, L.; et al. Protective Effects of N-Oleoylglycine in a Mouse Model of Mild Traumatic Brain Injury. ACS Chem. Neurosci. 2020, 11, 1117–1128. [Google Scholar] [CrossRef] [PubMed]
- Shahen-Zoabi, S.; Smoum, R.; Bingor, A.; Grad, E.; Nemirovski, A.; Shekh-Ahmad, T.; Mechoulam, R.; Yaka, R. N-oleoyl glycine and N-oleoyl alanine attenuate alcohol self-administration and preference in mice. Transl. Psychiatry 2023, 13, 273. [Google Scholar] [CrossRef]
- Rock, E.M.; Limebeer, C.L.; Sullivan, M.T.; DeVuono, M.V.; Lichtman, A.H.; Di Marzo, V.; Mechoulam, R.; Parker, L.A. N-Oleoylglycine and N-Oleoylalanine Do Not Modify Tolerance to Nociception, Hyperthermia, and Suppression of Activity Produced by Morphine. Front. Synaptic Neurosci. 2021, 13, 620145. [Google Scholar] [CrossRef]
- Bradshaw, H.B.; Rimmerman, N.; Hu, S.S.; Burstein, S.; Walker, J.M. Novel endogenous N-acyl glycines identification and characterization. Vitam. Horm. 2009, 81, 191–205. [Google Scholar] [CrossRef]
- Abadji, V.; Lin, S.; Taha, G.; Griffin, G.; Stevenson, L.A.; Pertwee, R.G.; Makriyannis, A. (R)-methanandamide: A chiral novel anandamide possessing higher potency and metabolic stability. J. Med. Chem. 1994, 37, 1889–1893. [Google Scholar] [CrossRef] [PubMed]
- Gracy, K.N.; Dankiewicz, L.A.; Koob, G.F. Opiate withdrawal-induced fos immunoreactivity in the rat extended amygdala parallels the development of conditioned place aversion. Neuropsychopharmacology 2001, 24, 152–160. [Google Scholar] [CrossRef] [PubMed]
- Wills, K.L.; Petrie, G.N.; Millett, G.; Limebeer, C.L.; Rock, E.M.; Niphakis, M.J.; Cravatt, B.F.; Parker, L.A. Double Dissociation of Monoacylglycerol Lipase Inhibition and CB1 Antagonism in the Central Amygdala, Basolateral Amygdala, and the Interoceptive Insular Cortex on the Affective Properties of Acute Naloxone-Precipitated Morphine Withdrawal in Rats. Neuropsychopharmacology 2016, 41, 1865–1873. [Google Scholar] [CrossRef] [PubMed]
- Huestis, M.A. Human cannabinoid pharmacokinetics. Chem. Biodivers. 2007, 4, 1770–1804. [Google Scholar] [CrossRef] [PubMed]
- Izzo, A.A.; Sharkey, K.A. Cannabinoids and the gut: New developments and emerging concepts. Pharmacol. Ther. 2010, 126, 21–38. [Google Scholar] [CrossRef] [PubMed]
- Shahen-Zoabi, S.; Smoum, R.; Beiser, T.; Nemirovski, A.; Mechoulam, R.; Yaka, R. N-Oleoyl Glycine and Its Derivatives Attenuate the Acquisition and Expression of Cocaine-Induced Behaviors. Cannabis Cannabinoid Res. 2023, 8, 812–823. [Google Scholar] [CrossRef] [PubMed]
- Dunn, K.E.; Weerts, E.M.; Huhn, A.S.; Schroeder, J.R.; Tompkins, D.A.; Bigelow, G.E.; Strain, E.C. Preliminary evidence of different and clinically meaningful opioid withdrawal phenotypes. Addict. Biol. 2020, 25, e12680. [Google Scholar] [CrossRef] [PubMed]
- Ware, O.D.; Ellis, J.D.; Dunn, K.E.; Hobelmann, J.G.; Finan, P.; Huhn, A.S. The association of chronic pain and opioid withdrawal in men and women with opioid use disorder. Drug Alcohol. Depend. 2022, 240, 109631. [Google Scholar] [CrossRef]
- Bodnar, R.J.; Kest, B. Sex differences in opioid analgesia, hyperalgesia, tolerance and withdrawal: Central mechanisms of action and roles of gonadal hormones. Horm. Behav. 2010, 58, 72–81. [Google Scholar] [CrossRef]
- Bobzean, S.A.M.; Kokane, S.S.; Butler, B.D.; Perrotti, L.I. Sex differences in the expression of morphine withdrawal symptoms and associated activity in the tail of the ventral tegmental area. Neurosci. Lett. 2019, 705, 124–130. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ayoub, S.M.; Rock, E.M.; Limebeer, C.L.; DeVuono, M.V.; Parker, L.A. Orally Administered N-Oleoyl Alanine Blocks Acute Opioid Withdrawal Induced-Conditioned Place Preference and Attenuates Somatic Withdrawal following Chronic Opioid Exposure in Rats. Psychoactives 2024, 3, 184-193. https://doi.org/10.3390/psychoactives3020012
Ayoub SM, Rock EM, Limebeer CL, DeVuono MV, Parker LA. Orally Administered N-Oleoyl Alanine Blocks Acute Opioid Withdrawal Induced-Conditioned Place Preference and Attenuates Somatic Withdrawal following Chronic Opioid Exposure in Rats. Psychoactives. 2024; 3(2):184-193. https://doi.org/10.3390/psychoactives3020012
Chicago/Turabian StyleAyoub, Samantha M., Erin M. Rock, Cheryl L. Limebeer, Marieka V. DeVuono, and Linda A. Parker. 2024. "Orally Administered N-Oleoyl Alanine Blocks Acute Opioid Withdrawal Induced-Conditioned Place Preference and Attenuates Somatic Withdrawal following Chronic Opioid Exposure in Rats" Psychoactives 3, no. 2: 184-193. https://doi.org/10.3390/psychoactives3020012
APA StyleAyoub, S. M., Rock, E. M., Limebeer, C. L., DeVuono, M. V., & Parker, L. A. (2024). Orally Administered N-Oleoyl Alanine Blocks Acute Opioid Withdrawal Induced-Conditioned Place Preference and Attenuates Somatic Withdrawal following Chronic Opioid Exposure in Rats. Psychoactives, 3(2), 184-193. https://doi.org/10.3390/psychoactives3020012





