Disparities in Substance Co-Use among Sexual Minority and Heterosexual Adult Hookah Smokers: Findings from Wave 4 (2016–2018) and Wave 5 (2018–2019) of the Population Assessment of Tobacco and Health Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Measures
2.2.1. Socio-Demographic Characteristics
2.2.2. Hookah Use and Substance Use
2.3. Statistical Analyses
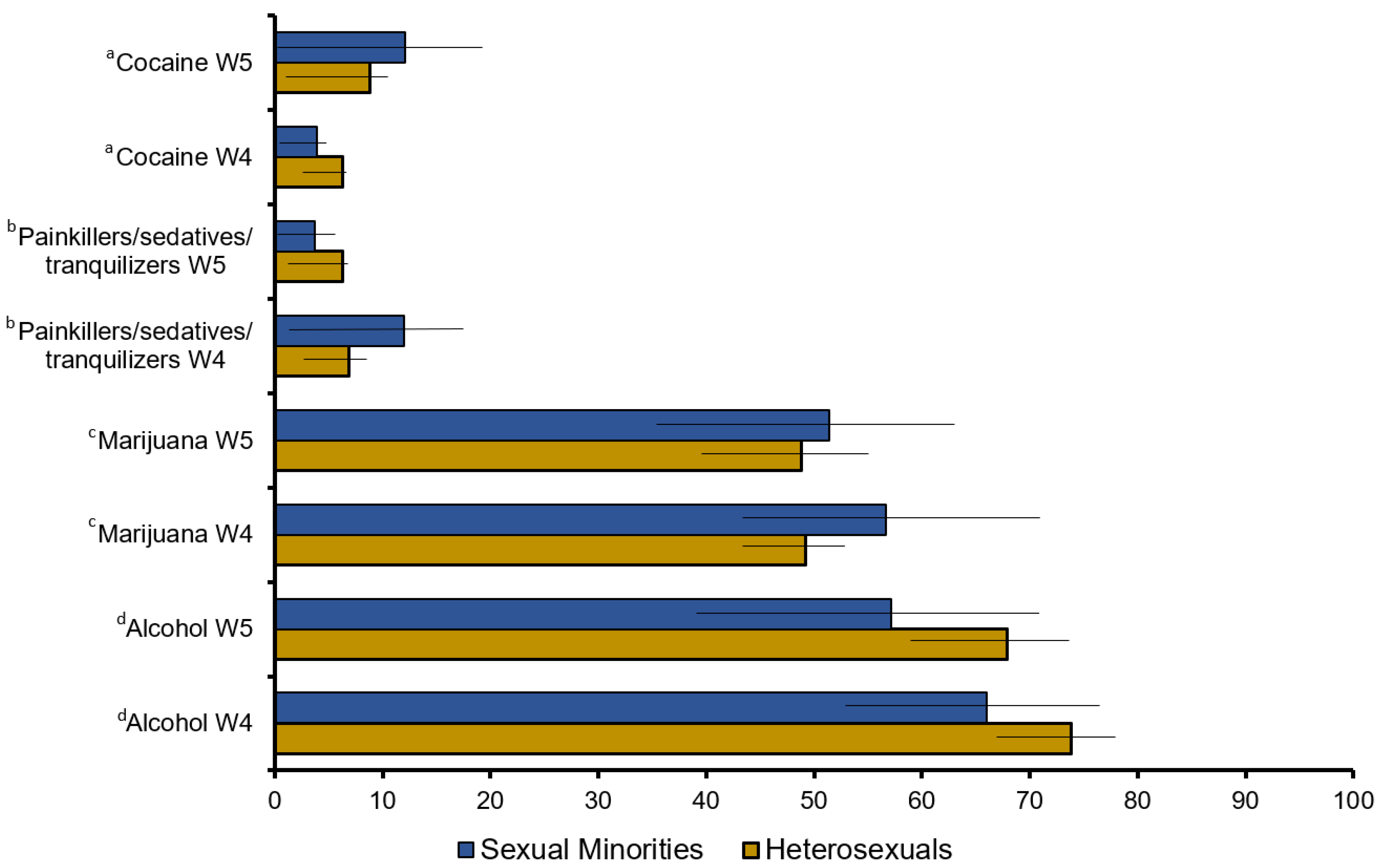
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Diease Control and Prevention. Smoking and Tobaco Use: Tobacco-Related Mortality. 2020. Available online: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/tobacco_related_mortality/index.htm (accessed on 10 November 2022).
- Cook, B.L.; Wayne, G.F.; Keithly, L.; Connolly, G. One size does not fit all: How the tobacco industry has altered cigarette design to target consumer groups with specific psychological and psychosocial needs. Addiction 2003, 98, 1547–1561. [Google Scholar] [CrossRef] [PubMed]
- Maziak, W.; Taleb, Z.B.; Bahelah, R.; Islam, F.; Jaber, R.; Auf, R.; Salloum, R.G. The global epidemiology of waterpipe smoking. Tob. Control 2015, 24 (Suppl. 1), i3–i12. [Google Scholar] [CrossRef] [PubMed]
- Bhatnagar, A.; Maziak, W.; Eissenberg, T.; Ward, K.D.; Thurston, G.; King, B.A.; Sutfin, E.L.; Cobb, C.O.; Griffiths, M.; Goldstein, L.B.; et al. Water Pipe (Hookah) Smoking and Cardiovascular Disease Risk: A Scientific Statement From the American Heart Association. Circulation 2019, 139, e917–e936. [Google Scholar] [CrossRef] [PubMed]
- Sharma, E.; Bansal-Travers, M.; Edwards, K.C.; Halenar, M.J.; Taylor, K.A.; Kasza, K.A.; Day, H.; Hammad, H.T.; Anic, G.; Limpert, J.; et al. Longitudinal pathways of exclusive and polytobacco hookah use among youth, young adults and adults in the USA: Findings from the PATH Study Waves 1–3 (2013–2016). Tob. Control 2020, 29 (Suppl. 3), s155–s162. [Google Scholar] [CrossRef]
- Fallin-Bennett, A.; Lisha, N.E.; Ling, P.M. Other Tobacco Product Use Among Sexual Minority Young Adult Bar Patrons. Am. J. Prev. Med. 2017, 53, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Haardörfer, R.; Vu, M.; Windle, M.; Berg, C.J. Sex and sexual orientation in relation to tobacco use among young adult college students in the US: A cross-sectional study. BMC Public Health 2018, 18, 1244. [Google Scholar] [CrossRef] [PubMed]
- Rezk-Hanna, M.; Holloway, I.W.; Toyama, J.; Warda, U.S.; Berteau, L.C.; Brecht, M.L.; Sarna, L. Transitions in hookah (Waterpipe) smoking by U.S. sexual minority adults between 2013 and 2015: The population assessment of tobacco and health study wave 1 and wave 2. BMC Public Health 2021, 21, 445. [Google Scholar] [CrossRef] [PubMed]
- Azagba, S.; Shan, L. Disparities in the frequency of tobacco products use by sexual identity status. Addict. Behav. 2021, 122, 107032. [Google Scholar] [CrossRef]
- Sönmez, İ.; Palamar, J.J. Sexual Orientation and Age of First Drug Use Among Adults in the United States. Subst. Use Misuse 2022, 57, 1313–1321. [Google Scholar] [CrossRef]
- Ehlke, S.J.; Kendzor, D.E.; Smith, M.A.; Sifat, M.S.; Boozary, L.K.; Cohn, A.M. Single-use, co-use, and polysubstance use of alcohol, tobacco, and cannabis in sexual minority and heterosexual females. Am. J. Addict. 2022, 32, 66–75. [Google Scholar] [CrossRef]
- Rodríguez-Bolaños, R.; Arillo-Santillán, E.; Guzmán-Rodríguez, C.; Barrientos-Gutiérrez, I.; Gallegos-Carrillo, K.; Titus, A.; Cruz-Jiménez, L.; Thrasher, J.F. Similarities and Differences in Substance Use Patterns Among Lesbian, Gay, Bisexual, and Heterosexual Mexican Adult Smokers. LGBT Health 2021, 8, 545–553. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.M.; Gilmore, A.K.; Rhew, I.C.; Hodge, K.A.; Kaysen, D.L. Minority stress is longitudinally associated with alcohol-related problems among sexual minority women. Addict. Behav. 2016, 61, 80–83. [Google Scholar] [CrossRef] [PubMed]
- Hequembourg, A.L.; Blayney, J.A.; Bostwick, W.; Van Ryzin, M. Concurrent Daily Alcohol and Tobacco Use among Sexual Minority and Heterosexual Women. Subst. Use Misuse 2020, 55, 66–78. [Google Scholar] [CrossRef] [PubMed]
- Dobrin, D.; Means, A.; Cheng, C.W.; Adolfo, A.; Anderson, S.; Warda, U.W.; Brecht, M.L.; Rezk-Hanna, M. Concurrent Hookah (Waterpipe) and Substance Use among Sexual Minority Adults in the United States: Findings from the Population Assessment of Tobacco and Health Study. Psychoactives 2022, 1, 89–101. [Google Scholar] [CrossRef]
- Medina-Martínez, J.; Saus-Ortega, C.; Sánchez-Lorente, M.M.; Sosa-Palanca, E.M.; García-Martínez, P.; Mármol-López, M.I. Health Inequities in LGBT People and Nursing Interventions to Reduce Them: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 11801. [Google Scholar] [CrossRef] [PubMed]
- Frost, D.M.; Fingerhut, A.W.; Meyer, I.H. Social change and relationship quality among sexual minority individuals: Does minority stress still matter? J. Marriage Fam. 2022, 84, 920–933. [Google Scholar] [CrossRef] [PubMed]
- Stevens, P.; Carlson, L.M.; Hinman, J.M. An analysis of tobacco industry marketing to lesbian, gay, bisexual, and transgender (LGBT) populations: Strategies for mainstream tobacco control and prevention. Health Promot. Pract. 2004, 5 (Suppl. 3), 129s–134s. [Google Scholar] [CrossRef]
- Omare, M.O.; Kibet, J.K.; Cherutoi, J.K.; Kengara, F.O. A review of tobacco abuse and its epidemiological consequences. Z. Gesundh. Wiss 2022, 30, 1485–1500. [Google Scholar] [CrossRef]
- Linden-Carmichael, A.N.; Stamates, A.L.; Lau-Barraco, C. Simultaneous Use of Alcohol and Marijuana: Patterns and Individual Differences. Subst. Use Misuse 2019, 54, 2156–2166. [Google Scholar] [CrossRef]
- Hawari, F.I.; Obeidat, N.A.; Ayub, H.; Ghonimat, I.; Eissenberg, T.; Dawahrah, S.; Beano, H. The acute effects of waterpipe smoking on lung function and exercise capacity in a pilot study of healthy participants. Inhal. Toxicol. 2013, 25, 492–497. [Google Scholar] [CrossRef]
- Rezk-Hanna, M.; Benowitz, N.L. Cardiovascular Effects of Hookah Smoking: Potential Implications for Cardiovascular Risk. Nicotine Tob. Res. 2019, 21, 1151–1161. [Google Scholar] [CrossRef] [PubMed]
- Waziry, R.; Jawad, M.; Ballout, R.A.; Al Akel, M.; Akl, E.A. The effects of waterpipe tobacco smoking on health outcomes: An updated systematic review and meta-analysis. Int. J. Epidemiol. 2017, 46, 32–43. [Google Scholar] [CrossRef] [PubMed]
- Ashurst, J.V.; Urquhart, M.; Cook, M.D. Carbon monoxide poisoning secondary to hookah smoking. J. Am. Osteopath. Assoc. 2012, 112, 686–688. [Google Scholar] [PubMed]
- Nguyen, V.; Salama, M.; Fernandez, D.; Sperling, J.D.; Regina, A.; Rivera, R.; Wang, J.; Friedman, B.W.; Smith, S.W. Comparison between carbon monoxide poisoning from hookah smoking versus other sources. Clin. Toxicol. 2020, 58, 1320–1325. [Google Scholar] [CrossRef] [PubMed]
- Daher, N.; Saleh, R.; Jaroudi, E.; Sheheitli, H.; Badr, T.; Sepetdjian, E.; Al Rashidi, M.; Saliba, N.; Shihadeh, A. Comparison of carcinogen, carbon monoxide, and ultrafine particle emissions from narghile waterpipe and cigarette smoking: Sidestream smoke measurements and assessment of second-hand smoke emission factors. Atmos Environ. 2010, 44, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Hyland, A.; Ambrose, B.K.; Conway, K.P.; Borek, N.; Lambert, E.; Carusi, C.; Taylor, K.; Crosse, S.; Fong, G.T.; Cummings, K.M.; et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tob. Control 2017, 26, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Hassane, M.; Rahal, Z.; Karaoghlanian, N.; Zhang, J.; Sinjab, A.; Wong, J.W.; Lu, W.; Scheet, P.; Lee, J.J.; Raso, M.G.; et al. Chronic Exposure to Waterpipe Smoke Elicits Immunomodulatory and Carcinogenic Effects in the Lung. Cancer Prev. Res. 2022, 15, 423–434. [Google Scholar] [CrossRef]
- Qasim, H.; Alarabi, A.B.; Alzoubi, K.H.; Karim, Z.A.; Alshbool, F.Z.; Khasawneh, F.T. The effects of hookah/waterpipe smoking on general health and the cardiovascular system. Environ. Health Prev. Med. 2019, 24, 58. [Google Scholar] [CrossRef]
- Underner, M.; Perriot, J.; Peiffer, G.; Dewitte, J.D.; Jaafari, N. Carbon monoxide poisoning in active or passive shisha smokers. Rev. Mal. Respir. 2020, 37, 376–388. [Google Scholar] [CrossRef]
- Misek, R.; Patte, C. Carbon monoxide toxicity after lighting coals at a hookah bar. J. Med. Toxicol. 2014, 10, 295–298. [Google Scholar] [CrossRef]
- Goldbach, J.T.; Tanner-Smith, E.E.; Bagwell, M.; Dunlap, S. Minority stress and substance use in sexual minority adolescents: A meta-analysis. Prev. Sci. 2014, 15, 350–363. [Google Scholar] [CrossRef] [PubMed]
- Dilley, J.A.; Spigner, C.; Boysun, M.J.; Dent, C.W.; Pizacani, B.A. Does tobacco industry marketing excessively impact lesbian, gay and bisexual communities? Tob. Control 2008, 17, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.A.; Thomson, K.; Offen, N.; Malone, R.E. “If you know you exist, it’s just marketing poison”: Meanings of tobacco industry targeting in the lesbian, gay, bisexual, and transgender community. Am. J. Public Health 2008, 98, 996–1003. [Google Scholar] [CrossRef] [PubMed]
- King, B.A.; Dube, S.R.; Tynan, M.A. Current tobacco use among adults in the United States: Findings from the National Adult Tobacco Survey. Am. J. Public Health 2012, 102, e93–e100. [Google Scholar] [CrossRef] [PubMed]
- Agaku, I.T.; King, B.A.; Dube, S.R. Current cigarette smoking among adults—United States, 2005–2012. MMWR Morb. Mortal. Wkly. Rep. 2014, 63, 29–34. [Google Scholar] [PubMed]
- Smith, T.W. Public Attitudes toward Homosexuality. NORC/University of Chicago. 2011. Available online: https://www.norc.org/PDFs/2011%20GSS%20Reports/GSS_Public%20Attitudes%20Toward%20Homosexuality_Sept2011.pdf (accessed on 8 December 2020).
- Glick, S.N.; Cleary, S.D.; Golden, M.R. Brief Report: Increasing Acceptance of Homosexuality in the United States Across Racial and Ethnic Subgroups. J. Acquir. Immune Defic. Syndr. 2015, 70, 319–322. [Google Scholar] [CrossRef] [PubMed]
- Rijst, V.; Garfield, J.L. Adverse Effects of Tobacco Products (Cigarettes, E-Cigarettes, Hookah, Smokeless Tobacco) Use on Health. In Tobacco Dependence. Respiratory Medicine; Eakin, M.N., Kathuria, H., Eds.; Humana: Cham, Switzerland, 2023; pp. 23–24. [Google Scholar] [CrossRef]
- Hodges, J.C.; Goings, T.C.; Vaughn, M.G.; Oh, S.; Salas-Wright, C.P. Sexual minorities and substance use treatment utilization: New evidence from a national sample. J. Subst. Use Addict. Treat. 2023, 150, 209060. [Google Scholar] [CrossRef]
| Sexual Minority Adults N = 200 | Heterosexual Adults N = 720 | |||
|---|---|---|---|---|
| Wave 4 n = 116 | Wave 5 n = 84 | Wave 4 n = 411 | Wave 5 n = 309 | |
| Age | ||||
| 18–24 Yr | 61.94 (49.46–74.42) | 51.90 (35.94–67.87) | 54.64 (46.65–62.64) | 38.33 (29.80–46.87) |
| 25–34 Yr | 30.39 (17.61–43.17) | 44.24 (28.66–59.82) | 34.04 (27.27–40.80) | 45.49 (37.26–53.72) |
| 35–44 Yr | 3.49 (0.00–7.83) | 2.69 (0.00–6.19) | 4.53 (2.52–6.53) | 8.78 (4.35–13.22) |
| 45–54 Yr | 0.33 (0.00–1.05) | 1.17 (0.00–2.77) | 3.79 (1.00–6.58) | 4.05 (0.58–7.52) |
| ≥55 Yr | 3.84 (0.00–9.32) | - | 3.00 (0.33–5.68) | 3.35 (0.18–6.52) |
| Sex a | ||||
| Male | 20.75 (9.86–31.65) | 43.97 (26.98–60.96) | 55.94 (48.26–63.61) | 54.63 (46.07–63.18) |
| Female | 79.25 (68.35–90.14) | 56.03 (39.04–73.02) | 44.06 (36.39–51.74) | 45.37 (36.82–53.93) |
| Race | ||||
| White, Non-Hispanic | 43.42 (27.48–59.36) | 39.11 (21.05–57.18) | 42.35 (35.20–49.49) | 29.96 (22.52–37.40) |
| Black, Non-Hispanic | 23.11 (8.92–37.30) | 18.75 (6.96–30.53) | 11.66 (7.18–16.15) | 19.16 (13.25–25.08) |
| Other, Non-Hispanic | 10.02 (4.56–15.48) | 11.14 (1.33–20.94) | 14.99 (9.96–20.02) | 12.07 (7.04–17.10) |
| Hispanic | 23.45 (10.92–35.99) | 31.00 (16.13–45.87) | 31.00 (23.48–38.53) | 38.80 (30.41–47.19) |
| Education Level | ||||
| No College | 39.45 (24.88–54.02) | 36.58 (20.73–52.43) | 36.90 (28.56–45.23) | 39.53 (29.15–49.91) |
| Some College | 60.55 (45.98–75.12) | 63.42 (47.57–79.27) | 63.10 (54.77–71.44) | 60.47 (50.09–70.85) |
| Income | ||||
| <USD 25,000 | 58.14 (44.68–71.61) | 43.44 (25.25–61.63) | 44.32 (38.08–50.56) | 33.97 (26.06–41.88) |
| USD 25,000–49,999 | 18.85 (8.13–29.57) | 25.69 (11.12–40.27) | 27.96 (20.55–35.37) | 28.40 (20.39–36.40) |
| USD 50,000–99,000 | 14.24 (4.12–24.36) | 20.00 (4.22–35.78) | 18.30 (12.72–23.89) | 25.22 (17.33–33.12) |
| ≥USD 100,000 | 8.77 (1.51–16.02) | 10.86 (2.39–19.33) | 9.42 (5.81–13.02) | 12.41 (6.60–18.23) |
| Health Insurance | ||||
| No | 22.07 (11.30–32.84) | 28.12 (13.64–42.60) | 19.59 (13.56–25.61) | 22.99 (16.43–29.55) |
| Yes | 77.93 (67.16–88.70) | 77.88 (57.40–86.36) | 80.41 (74.39–86.44) | 77.01 (70.45–83.57) |
| Wave 4 SM vs. Heterosexual Individuals | Wave 5 SM vs. Heterosexual Individuals | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| Cocaine | ||||||
| Adjusted for gender | 0.52 | 0.14–2.00 | 0.34 | 1.41 | 0.19–10.70 | 0.74 |
| Adjusted for all covariates | 0.37 | 0.08–1.79 | 0.21 | 1.64 | 0.23–11.55 | 0.61 |
| Pain killers/sedatives/tranquilizers | ||||||
| Adjusted for gender | 1.48 | 0.47–4.63 | 0.45 | 0.53 | 0.12–2.30 | 0.39 |
| Adjusted for all covariates | 1.56 | 0.49–5.02 | 0.45 | 0.86 | 0.20–3.66 | 0.84 |
| Marijuana | ||||||
| Adjusted for gender | 1.32 | 0.67–2.59 | 0.42 | 1.06 | 0.46–2.46 | 0.89 |
| Adjusted for all covariates | 1.20 | 0.59–2.47 | 0.60 | 1.94 | 0.50–2.87 | 0.69 |
| Alcohol | ||||||
| Adjusted for gender | 0.65 | 0.34–1.25 | 0.19 | 0.59 | 0.25–1.42 | 0.23 |
| Adjusted for all covariates | 0.62 | 0.26–1.45 | 0.26 | 0.57 | 0.24–1.33 | 0.19 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sakthi, C.; Adolfo, A.; Warda, U.S.; Khaled, A.; Brecht, M.-L.; Rezk-Hanna, M. Disparities in Substance Co-Use among Sexual Minority and Heterosexual Adult Hookah Smokers: Findings from Wave 4 (2016–2018) and Wave 5 (2018–2019) of the Population Assessment of Tobacco and Health Study. Psychoactives 2024, 3, 123-131. https://doi.org/10.3390/psychoactives3010008
Sakthi C, Adolfo A, Warda US, Khaled A, Brecht M-L, Rezk-Hanna M. Disparities in Substance Co-Use among Sexual Minority and Heterosexual Adult Hookah Smokers: Findings from Wave 4 (2016–2018) and Wave 5 (2018–2019) of the Population Assessment of Tobacco and Health Study. Psychoactives. 2024; 3(1):123-131. https://doi.org/10.3390/psychoactives3010008
Chicago/Turabian StyleSakthi, Chandni, Amanda Adolfo, Umme Shefa Warda, Asmaa Khaled, Mary-Lynn Brecht, and Mary Rezk-Hanna. 2024. "Disparities in Substance Co-Use among Sexual Minority and Heterosexual Adult Hookah Smokers: Findings from Wave 4 (2016–2018) and Wave 5 (2018–2019) of the Population Assessment of Tobacco and Health Study" Psychoactives 3, no. 1: 123-131. https://doi.org/10.3390/psychoactives3010008
APA StyleSakthi, C., Adolfo, A., Warda, U. S., Khaled, A., Brecht, M.-L., & Rezk-Hanna, M. (2024). Disparities in Substance Co-Use among Sexual Minority and Heterosexual Adult Hookah Smokers: Findings from Wave 4 (2016–2018) and Wave 5 (2018–2019) of the Population Assessment of Tobacco and Health Study. Psychoactives, 3(1), 123-131. https://doi.org/10.3390/psychoactives3010008





