1. Introduction
Orthopedic medical education is rapidly advancing in the era of artificial intelligence (AI), virtual reality (VR), and mixed reality (MR) technologies. These technologies address persistent issues in traditional orthopedic medical education, including limited access to cadaver labs, inconsistent operating room exposure, and the lack of personalized training frameworks. Traditional methods rely on didactic lectures, cadaveric dissection, and supervised clinical experience. While somewhat effective, these approaches may not provide sufficient opportunities for repeated practice, exposure to rare or complex cases, or individualized feedback [
1].
AI and MR platforms offer innovative solutions to these longstanding challenges. AI algorithms provide individualized learning trajectories by using student performance data to create customized learning experiences that close the gaps in knowledge and learning styles [
1]. This individualized approach has greatly enhanced the efficiency of orthopedic educational experiences. New advanced VR platforms like the Microsoft HoloLens, Apple Vision Pro, and HTC Vive Pro have significantly influenced increased procedural confidence and skill development in orthopedic residents [
2]. In fact, one study found that 67.28% of participants agreed that VR training improved resident confidence in procedural skills [
2,
3].
AI and MR platforms provide high-fidelity anatomical simulations and immersive procedural environments that allow trainees to repeatedly practice surgical techniques without putting patients at risk [
4]. MR technology enables trainees to visualize complex 3D anatomical structural relationships, facilitating deeper understanding than textbook images or traditional 2D materials [
5,
6,
7]. These simulators replicate the tactile and visual aspects of orthopedic procedures, offering realistic training scenarios and mechanical feedback that closely mimic real surgical experiences. Additionally, these platforms support remote participation and observation, expanding access to expert-led instruction and live surgical demonstrations [
5,
6,
7].
Beyond procedural training, new orthopedic imaging interpretation using AI diagnostic systems is rapidly evolving, with new radiology graduates reaching diagnostic accuracy levels equal to someone with decades of training. Fully involved ML models have also been developed to predict surgical outcomes and reduce complications, assisting residents in decision-making and patient risk stratification. AI has also been shown to improve the residency training experience by guaranteeing residents receive balanced exposure to procedures and adapting the curriculum through performance analytics. In this regard, these tools are advancing educational methodologies and facilitating the technological expertise of orthopedic surgeons [
7].
Compelling statistics further substantiate the argument for the positive impact of AI and MR on orthopedic education and surgical performance. In a study on percutaneous transforaminal endoscopic discectomy (PTED) training, students using MR-assisted learning demonstrated a 33.4% increase in accuracy (from 53.3% to 86.7%) compared to only a 6.7% improvement (from 60.0% to 66.7%) in those using traditional methods [
8]. A randomized clinical trial found that orthopedic residents trained with immersive VR completed reverse shoulder arthroplasty procedures 47.4 min faster than their traditionally trained counterparts, achieving a transfer effectiveness ratio of 0.79 [
8]. Similarly, VR-based training for tibial intramedullary nail procedures led to fewer incorrect steps (3.1–3.2 out of 16) compared to those using only a technique guide (5.7 out of 16), while VR-trained participants demonstrated significantly higher procedure completion rates (75–78% versus 25% for those relying solely on a technique guide) [
8]. Across multiple trials, VR-trained groups completed procedures 12% faster on average, showed a 19.9% improvement in overall performance, and exhibited a reduced learning curve, particularly in unicompartmental knee arthroplasty. Furthermore, trainee satisfaction remains high, with over 70% of participants reporting VR learning as at least “helpful” or “useful” in their training [
8].
Moreover, AI-driven systems enhance orthopedic education by continuously tracking learner performance, identifying individual strengths and weaknesses, and delivering adaptive feedback. This personalized instruction accelerates skill acquisition, improves the retention of anatomical knowledge, and helps trainees address specific deficits in technique. MR and VR platforms enable unlimited, risk-free practice, exposure to rare procedures, and real-time objective performance feedback—capabilities not feasible with conventional methods [
6,
7,
8,
9]. AI-powered analytics can also predict outcomes and provide actionable insights, supporting clinical decision-making and risk stratification during training [
2,
5].
These results highlight the changing impact of AI and MR technologies in orthopedic education, including enhanced learning opportunities, increased accuracy of surgical procedures, and increased efficiency in performing procedures. As research and development continue, these technologies will have an important part in advancing the next generation of orthopedic surgeons and their preparation for practicing in a technology-enhanced period in medicine [
2,
3,
4,
5,
6,
7,
8,
9].
However, challenges remain in adopting AI and MR technology in orthopedic education. Cost, practicality, and the need to modify the curriculum often present significant challenges. AI also raises ethical issues related to data privacy and external ethical issues about algorithmic bias when determining how to leverage AI in orthopedic education [
2]. While these technologies show great potential, their full incorporation into orthopedic education necessitates continued research, development, and equitable access across institutions [
5,
6,
7,
8,
9].
Unlike prior reviews that have broadly explored AR/VR technologies in healthcare, this review specifically examines the practical integration, educational outcomes, and comparative effectiveness of MR platforms within orthopedic training contexts.
2. Methods
This review evaluates the role of AI and MR technologies in orthopedic medical education, focusing on their applications, benefits, and limitations across major commercial platforms. A comprehensive literature search was performed using databases including PubMed, Google Scholar, and ScienceDirect, and was supplemented by relevant literature such as press releases and product documentation from device manufacturers. Search terms included combinations of “artificial intelligence”, “mixed reality”, “orthopedic education”, “virtual reality surgical training”, “Microsoft HoloLens”, “Apple Vision Pro”, “HTC Vive Pro”, “VR in medical education”, and “MR surgical simulation.”
Articles were included in the review if published between 2018 and 2025, focused on educational or clinical simulation applications of AI or MR in orthopedic or surgical training, and reported either quantitative or qualitative outcomes—such as performance metrics or user satisfaction. Exclusion criteria included purely theoretical AI papers without applied relevance to orthopedic education, and editorials or non-peer-reviewed opinion pieces (except for industry announcements relevant to device usage).
The review focused on three commercially significant MR and VR platforms: Microsoft HoloLens (Microsoft Corporation, Remond, WA, USA), Apple Vision Pro (Apple Inc., Cupertino, CA, USA), and HTC Vive Pro (HTC Corporation, Taoyuan City, Taiwan). These platforms were selected based on peer-reviewed studies of their educational utility, hardware capabilities (e.g., haptics and field of view), relevance to orthopedic and anatomical training, and the availability of surgical simulation platforms. Apple Vision Pro, operating on visionOS version 1.1, was utilized for extended reality (XR) visualization. HTC Vive Pro was employed for immersive virtual reality simulations, configured using Vive Console version 2.1.22.6 and SteamVR version 1.27.6. HoloLens supported mixed reality applications and ran on Windows Holographic OS version 23H1. Comparative features across these platforms were extracted and evaluated in key domains, including educational effectiveness, tactile feedback, immersive experience, cost, clinical integration, and overall accessibility.
3. Results
The review identified consistent and measurable improvements in procedural training, learner engagement, and educational outcomes when AI and mixed reality (MR) platforms were integrated into orthopedic medical education. Across several studies, using MR-assisted learning significantly enhanced procedural accuracy and efficiency. For example, in training for percutaneous transforaminal endoscopic discectomy (PTED), students using MR technologies demonstrated a 33.4% improvement in procedural accuracy—rising from 53.3% to 86.7%—compared to only a 6.7% improvement using traditional educational methods. Similarly, a randomized clinical trial revealed that orthopedic residents trained in reverse shoulder arthroplasty through immersive virtual reality completed procedures 47.4 min faster than their traditionally trained peers, yielding a transfer effectiveness ratio of 0.79. In tibial intramedullary nailing procedures, VR-trained participants made significantly fewer errors (3.1–3.2 incorrect steps out of 16) compared to those relying solely on a technique guide (5.7 incorrect steps), and they demonstrated higher completion rates—75–78% versus 25% [
8].
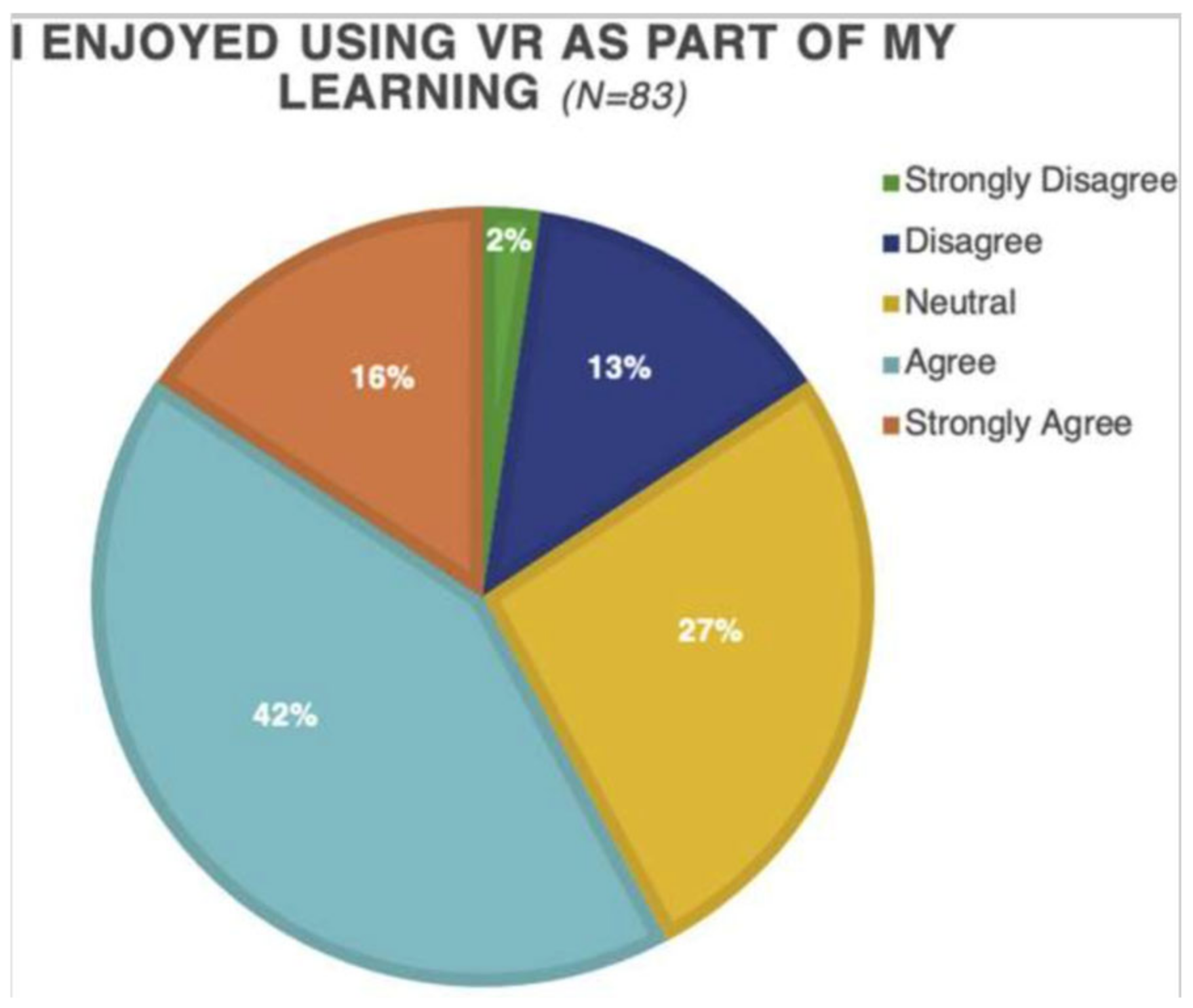
In addition to improving performance, MR and VR platforms also increased learner satisfaction and perceived educational value. Over 70% of trainees across multiple studies reported that mixed reality and virtual reality learning environments were either “helpful” or “very helpful” in enhancing their confidence and procedural understanding. MR anatomy instruction using platforms like Microsoft HoloLens led to statistically significant gains in learner satisfaction and knowledge retention, outperforming or equaling traditional cadaver-based education. In controlled studies, students reported greater engagement, improved spatial understanding, and enhanced visualization experiences when using MR platforms [
4,
5,
8].
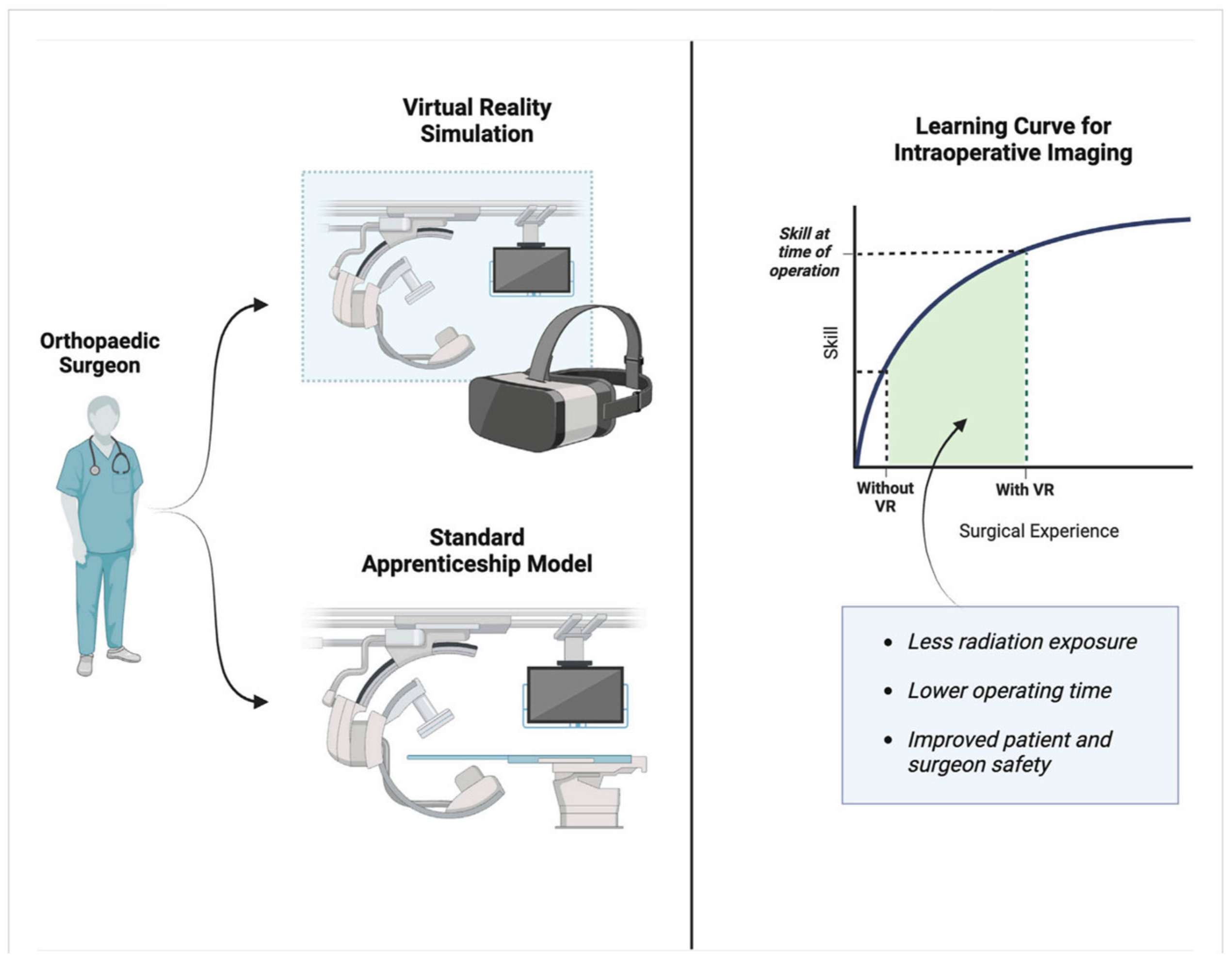
Mixed reality also facilitates procedural training, allowing students to repeatedly perform techniques without any danger to patients in a way that expedites the learning curve for complex orthopedic procedures. A personalized learning experience is another significant advantage that arises in the context of mixed reality, wherein AI platforms adjust to adapt to individual learning styles and the speed of the learners. As a result of this personalization, knowledge retention and skill acquisition are enhanced. Lenz et al. (2021a) led a study that utilized a VR simulator called xRayWorld, which employed gamification and visuospatial tasks to help students develop an understanding of X-ray imaging. In this example, the versatility of mixed reality tools in medical education is further reinforced [
10,
11,
12,
13,
14].
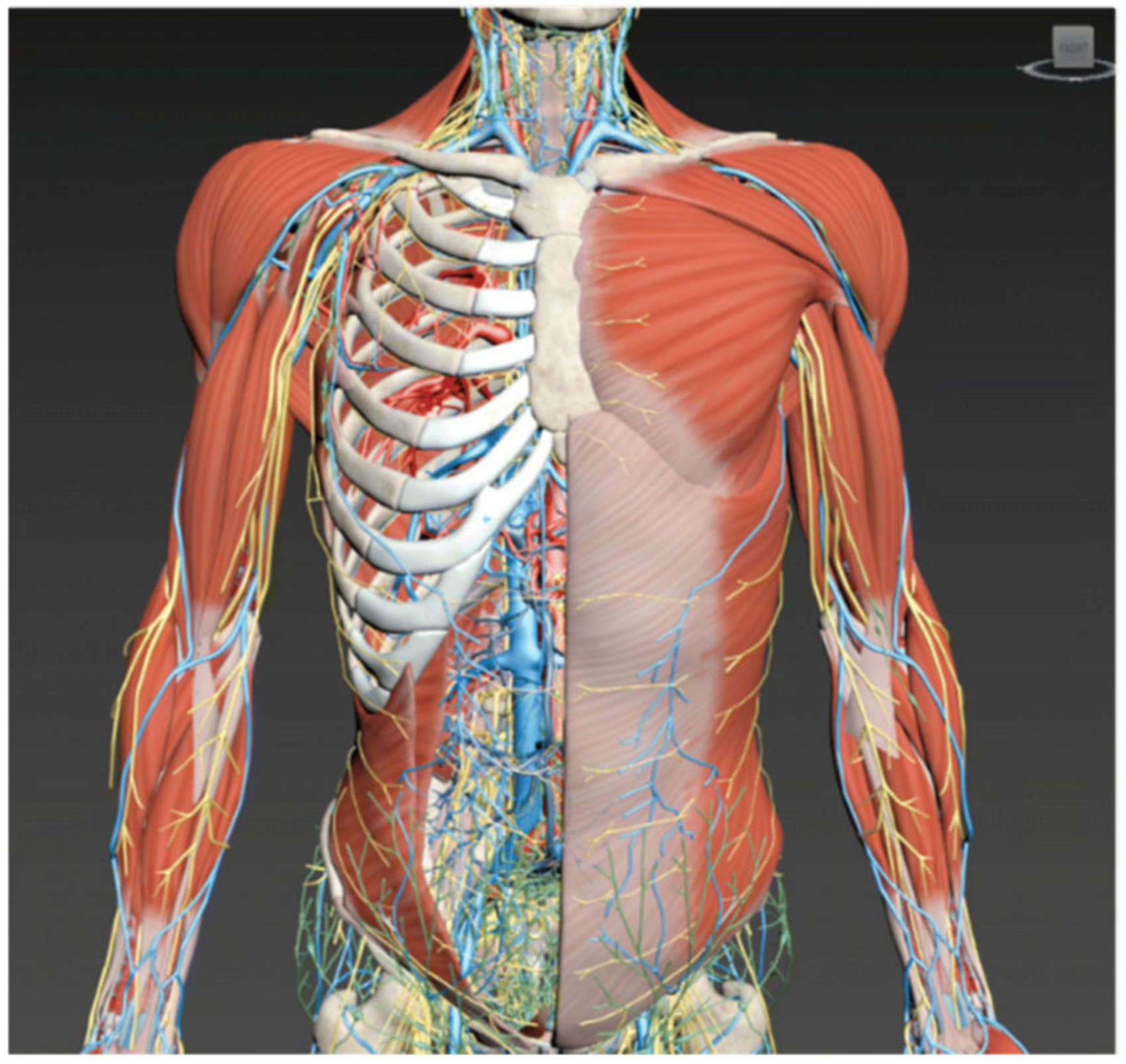
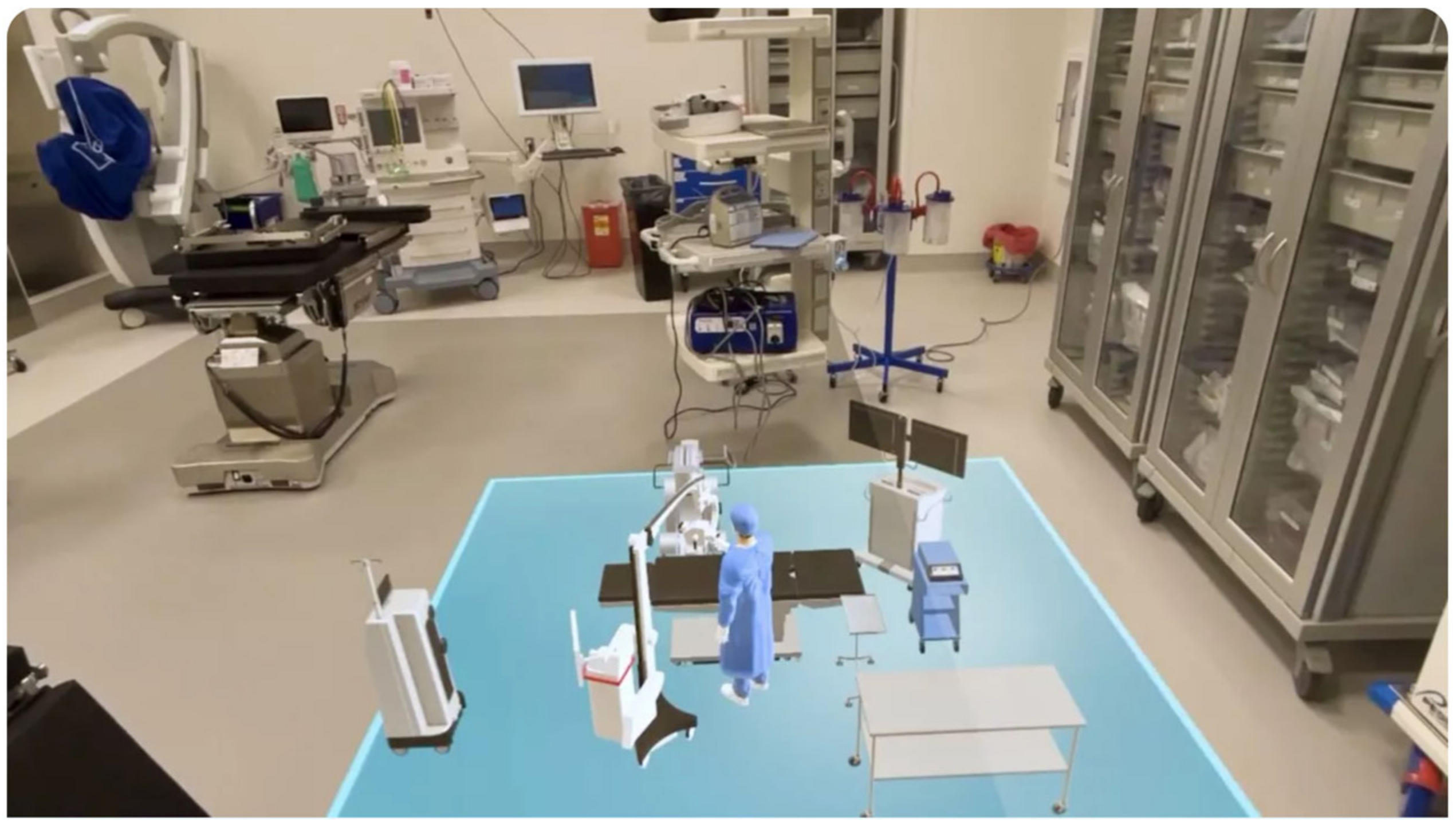
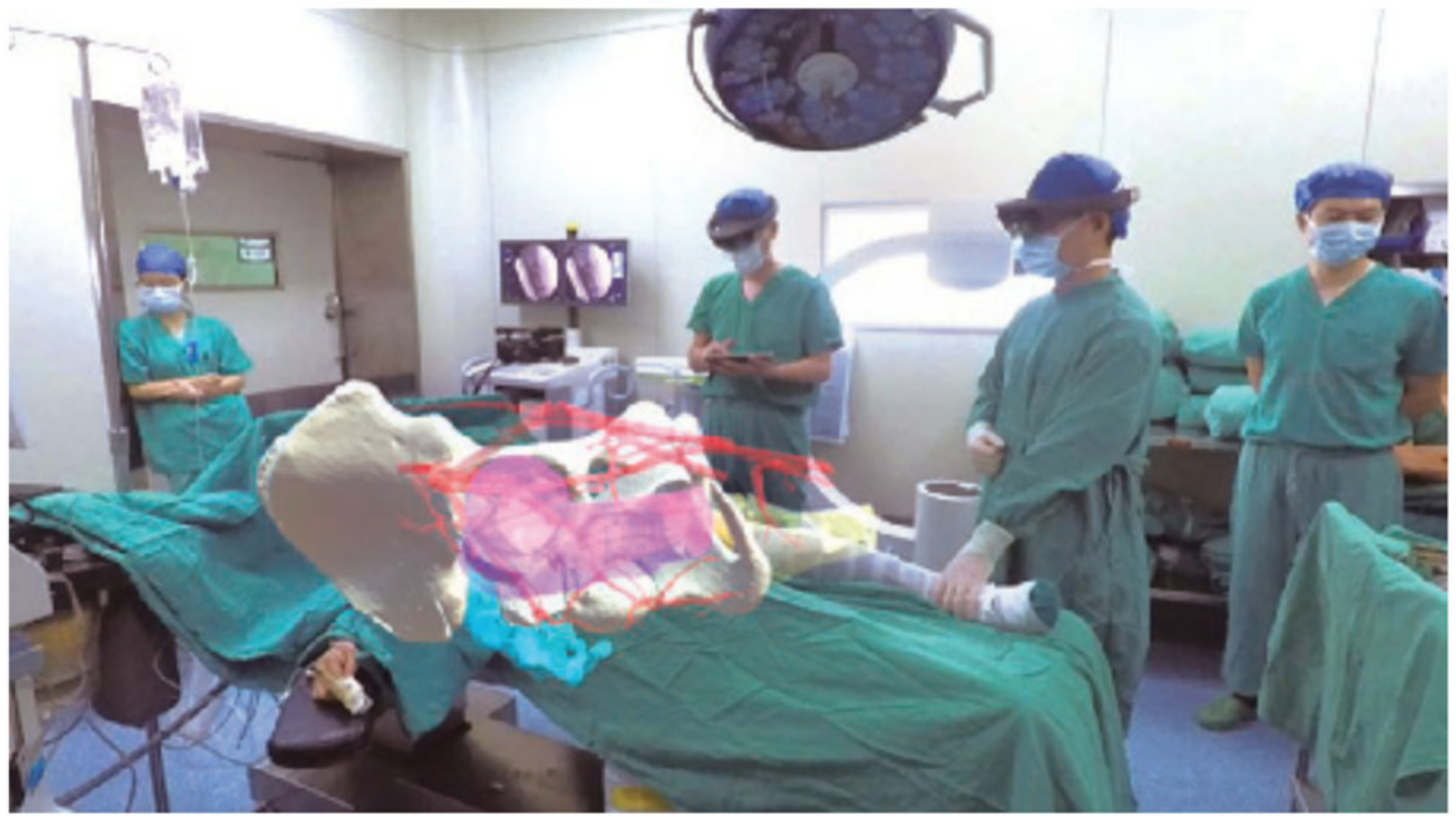
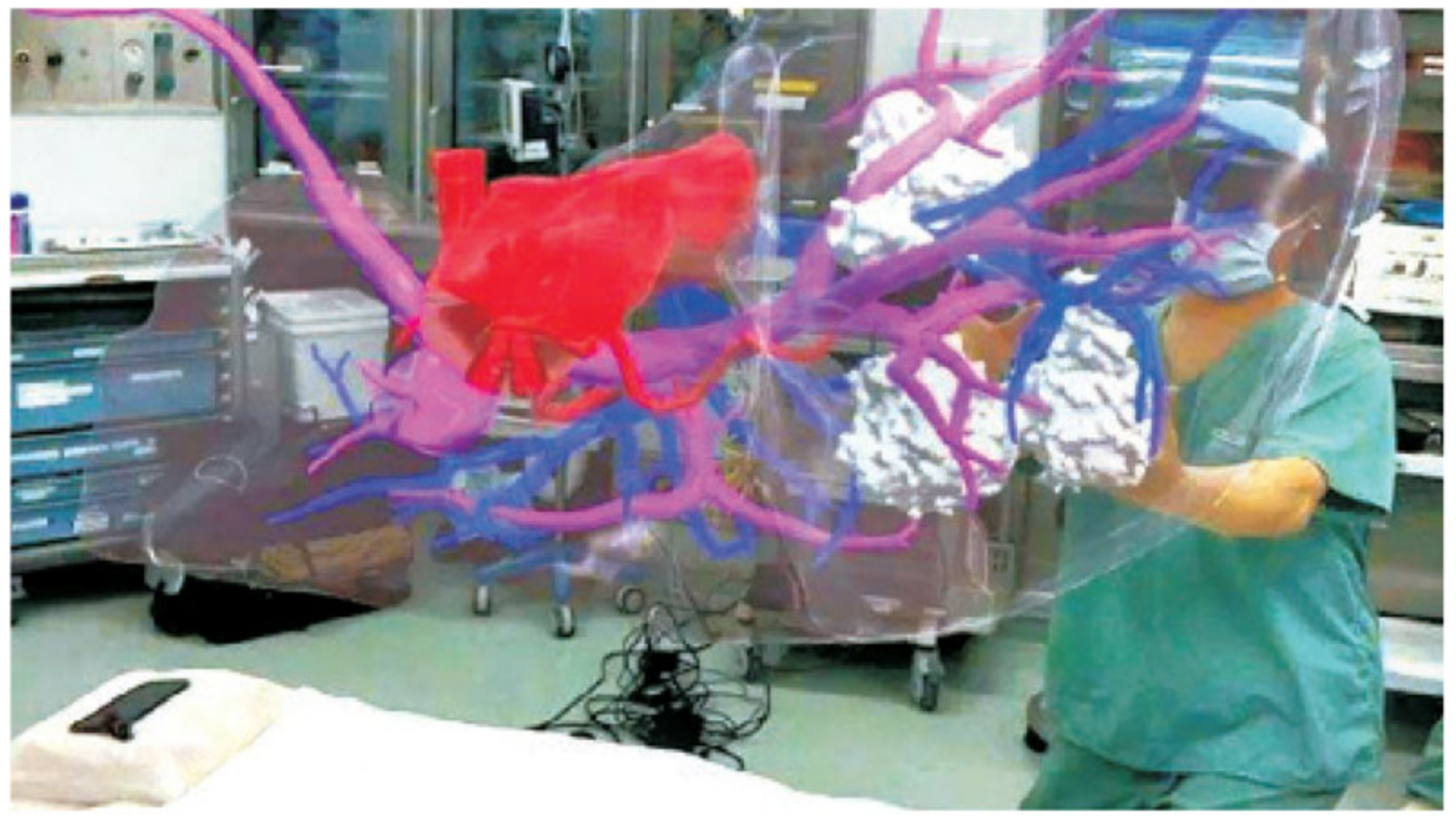
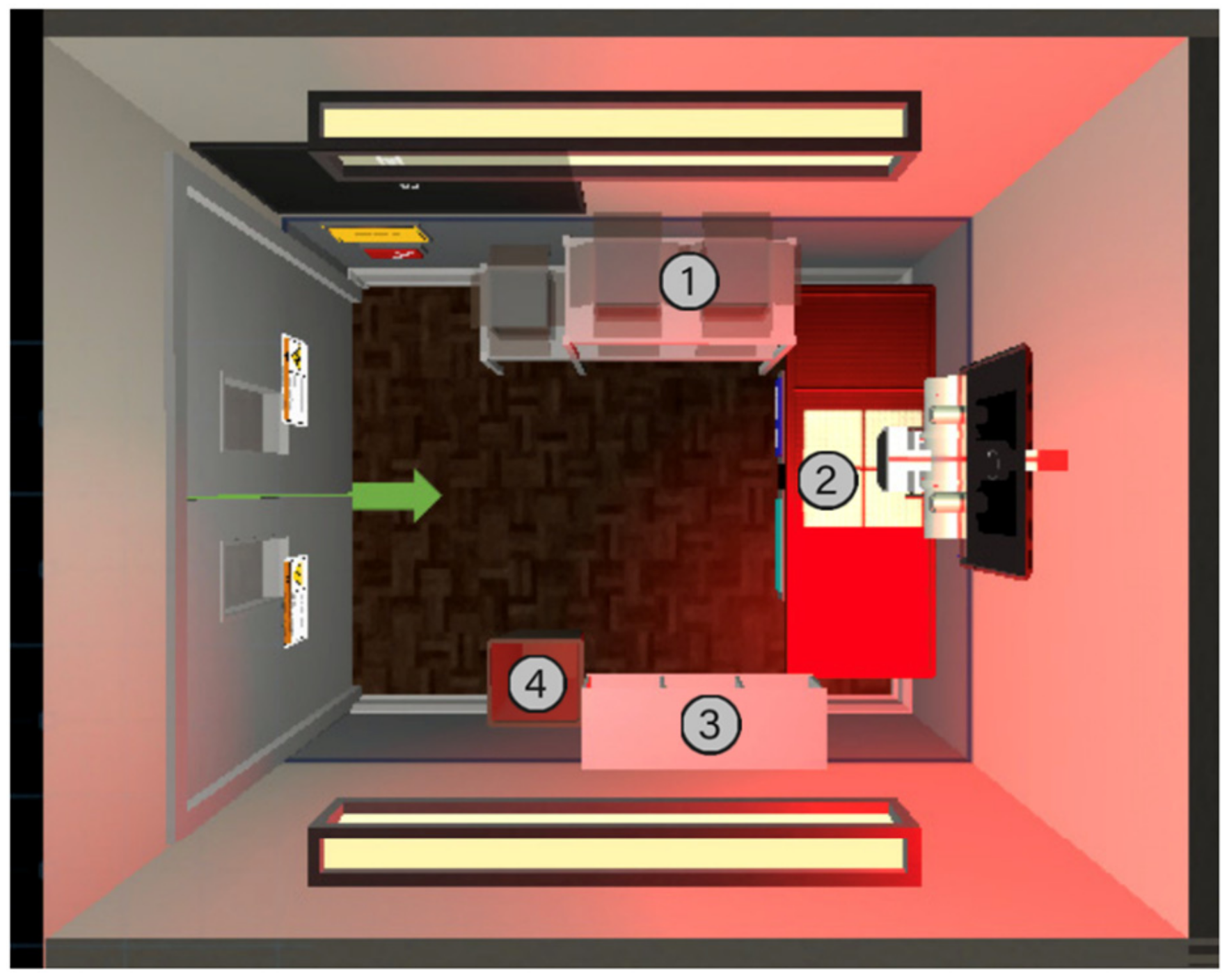
Beyond procedural instruction, mixed reality applications also support clinical practice in the context of diagnostic assessments since virtual environments allow practitioners to view, observe, and/or manipulate complex anatomical structures to make quality assessments (
Figure 1). These tools also hold value in patient care and education as immersive simulations can improve patients’ understanding of their medical conditions, leading to higher rates of adherence. Additionally, mixed reality improves learning opportunities as the technologies are remote, increasing opportunities for equitable learning via remote collaboration between learners and educators or educators from around the world or community or organizational partnerships that may be located outside of the geographical area. Studies suggest immersive experiences activate the prefrontal cortex, enhancing engagement, retention, and cognitive learning functions [
15].
Social distancing has made learning remotely more important and mixed reality technologies can provide high-quality distance learning opportunities when face-to-face teaching would otherwise not be possible [
15]. AI can also promote data-driven education by providing educators with performance data in simulations to provide valuable insight into areas of the curriculum where individual students may need additional support [
8].
A comparative analysis of the platforms revealed that each platform, including the Microsoft HoloLens, Apple Vision Pro, and HTC Vive Pro, offered distinct strengths (
Table 1). The Microsoft HoloLens excelled in collaborative learning and anatomical visualization through holographic overlays, making it ideal for remote teaching and preoperative planning. However, its relatively narrow field of view and high cost (
$3500) presented barriers to widespread adoption [
5,
8,
16,
17,
18,
19,
20,
21,
22,
23,
24,
25].
The Apple Vision Pro delivered high-resolution immersive experiences with spatial computing and was successfully implemented in live surgical environments—improving workflow efficiency by an estimated 150–200%. Despite its clinical potential, the limited battery life, high price point (
$3499), and ergonomic limitations restricted extended or repeated use in educational settings [
21,
26,
27,
28,
29,
30,
31,
32,
33,
34,
35].
The HTC Vive Pro, meanwhile, offered the most tactile realism through haptic feedback and room-scale tracking, enhancing procedural training for tasks such as pedicle screw placement and dynamic hip screw insertion. Its more accessible price (~
$1500) made it a cost-effective option. However, issues with cybersickness—experienced by up to 30% of users—and relatively short battery life (about 2.5 h) were noted as potential limitations [
36,
37,
38,
39,
40,
41,
42].
As mixed reality and AI evolve, they promise to transform orthopedic education by bridging theoretical knowledge with practical application. Addressing current limitations will be key to unlocking their full potential and ensuring equitable access across institutions globally.
The integration of these platforms into real-world clinical settings further underscored their impact. For instance, the Apple Vision Pro has already been used in live orthopedic surgeries to project anatomical overlays and digital instruments, facilitating faster, more precise procedures [
29,
33,
43]. Likewise, HTC Vive Pro-based systems like VirtX significantly reduced intraoperative imaging needs, including up to 75% fewer fluoroscopy uses and 66% fewer X-rays, without compromising procedural quality [
26,
34]. These outcomes highlight the potential for AI and MR technologies to improve educational processes and clinical performance and patient safety in orthopedic practice.
Despite their potential, these technologies face implementation challenges. High upfront costs limit their widespread adoption and accessibility in educational institutions [
5,
8]. Technical limitations persist, with current devices often lacking the fidelity to fully replicate tactile feedback crucial for orthopedic procedures [
15]. Educators also face difficulties integrating these tools into existing curricula while ensuring alignment with traditional teaching methods [
8]. Finally, more longitudinal research is needed to validate the long-term benefits of AI-enhanced education on clinical competence [
5].
Table 1.
Detailed comparison of the mentioned AI-based platforms used for enterprise and educational purposes.
Table 1.
Detailed comparison of the mentioned AI-based platforms used for enterprise and educational purposes.
| Feature | Microsoft HoloLens 2 [8,10,11,35] | Apple Vision Pro [4,10,11,35,39] | HTC Vive Pro [10,11,35,36,39,42] |
| Primary Uses | Industrial, medical, and professional AR applications | Entertainment, creative work, and personal productivity | VR gaming, surgical training, and enterprise applications |
| Display Technology | Transparent holographic lenses and a 60 Hz refresh rate | Micro-OLED displays with 4K per eye, and a 100 Hz refresh rate | OLED 2800 × 1600 resolution, and a 90 Hz refresh rate |
| Field of View (FOV) | Narrow (~52), optimized for AR applications | Wide (~110), extending to peripheral vision for immersive VR | Moderate (~110), designed for VR applications |
| Processing Power | Qualcomm Snapdragon XR1 processor; custom holographic processing unit | Apple M2 and R1 chips for multitasking and real-time sensor data | PC-powered, Intel Core i9 compatibility, and NVIDIA GeForce GTX |
| Battery Life | ~3 h | ~2 h | ~2.5 h |
| Tracking and Interaction | Hand-tracking, eye-tracking, and voice commands | Eye-tracking, hand gestures, and spatial computing | External base stations for precise tracking and controllers |
| Comfort and Ergonomics | Flip-up visor for convenience | Lightweight, premium materials | Heavier due to the external tracking setup |
| Cybersickness Risk | Low (AR-based with real-world blending) | Moderate (eye-tracking helps reduce strain) | High (~30% of users) |
| Unique Features | Real-time holographic overlays for surgical planning and anatomical visualization | Spatial computing with eye-tracking and intuitive controls; immersive simulations | Haptic feedback enabling tactile realism; room-scale tracking for full-body movement simulations |
| Applications in Orthopedics | Used in preoperative planning (e.g., spine surgeries); collaborative learning via remote guidance | High-fidelity simulations for procedures like knee arthroplasty and carpal tunnel release | VR-based training improves procedural accuracy (e.g., tibial intramedullary nailing) |
| Performance Metrics | Improves surgical planning accuracy by projecting anatomical overlays onto patients | Reduces learning curve and improves step completion rates in orthopedic procedures | Decreases incorrect steps in procedures by ~45%; reduces completion times by ~12% |
| Cost | ~$3500 | ~$3500 | ~$1500 |
| Limitations Compared to Others | Limited immersion due to narrow FOV; higher cognitive load during simulations; bulky design | Shorter battery life, ergonomic strain from prolonged use, and requires integration into sterile environments. | Cybersickness in dynamic simulations and lower visual resolution than Apple Vision Pro |
4. Discussion
Integrating AI and MR technologies into orthopedic education represents a transformative advancement in medical training methodologies. These tools address several longstanding challenges in the field, offering innovative solutions to enhance learning and skill development. Orthopedic education requires a strong grasp of three-dimensional anatomical relationships, and mixed reality technologies provide an unparalleled way to visualize and interact with complex structures.
4.1. AI-Driven Technologies in Orthopedic Education
4.1.1. Microsoft HoloLens
The Microsoft HoloLens (
Figure 2), a mixed reality (MR) platform, projects interactive 3D holographs into real-world environments, allowing users to explore and interact with anatomical structures in new ways without needing to use cadavers. It has already led to changes in medical education and surgical practice. While not unique to the HoloLens, the capability to engage one another with anatomical models in 3D is a new pedagogical method of instruction that holds immense potential to advance interactivity, immersive learning, and information retention when it comes to the complexities of anatomy, as students can view the complexities of anatomy in three dimensions (
Figure 3) [
16].
Research has indicated the HoloLens’s efficacy in teaching musculoskeletal anatomy and ear anatomy, showing that students who learned through mixed reality (MR) demonstrated comparable or improved performance compared with students that learned through traditionally delivered education. In a learning study focused on ear anatomy, all groups demonstrated statistically significant test score improvement (
p < 0.001) with the HoloLens-based anatomy instruction receiving statistically higher satisfaction ratings than traditional anatomy education (
p < 0.001) [
16,
17,
44]. A randomized controlled trial of musculoskeletal anatomy also showed no statistical significance in test scores between students learning through MR or through cadaveric dissection (
p > 0.05) [
17], supporting MR as an alternative or supplemental education tool. Finally, a strong positive correlation was detected between mixed reality training and scores on cadaver examinations (r = 0.74,
p < 0.01), which suggests that MR-based education can influence anatomical understanding in an educational context that translates well to traditional assessments [
23]. Students reported higher quality engagement, visualization experiences, and better knowledge acquisition while learning in an MR environment as an interactive pedagogical tool (
Figure 4 and
Figure 5) [
17,
23,
24,
25,
36,
37,
38,
44].
The HoloLens also offers further documentation of anatomical training that goes beyond just anatomy education, specifically applicable for clinical and surgical procedures (
Figure 2). The use of preoperative planning has enabled surgeons to engage with patient-specific anatomical structures in a three-dimensional environment, improving accuracy and decision-making. For example, preoperative planning has introduced capabilities to plan joint replacements, upper arm fractures, and trauma surgery with patient-specific three-dimensional models generated from CT imaging displayed in the environment as an overlay [
16]. In spine surgery, the HoloLens allows for the visualization of pre-planned screw routes on top of holographic overlays during procedures, further increasing accuracy (
Figure 5 and
Figure 6). The HoloLens also introduces opportunities for collaborative learning in this space. Remote subject matter experts can lead the procedure by sharing the same holographic view of the procedure at a distance from the intern/fellow (
Figure 6) [
18].
One major benefit of the HoloLens for anatomy education is the potential it creates to develop standardized training modules on a global scale for students and residents. Traditional anatomical education relies on cadaver availability—an availability that varies greatly from institution to institution and region to region. A medical school or training center can use MR technology to provide consistent, repeatable learning experiences to all students, irrespective of the anatomical education they receive on-site. The HoloLens also supports remote learning by allowing multiple users to interact with the same holographic model in real-time, thus providing an effective medium for distance education and supervised education by experts in a subject area [
17].
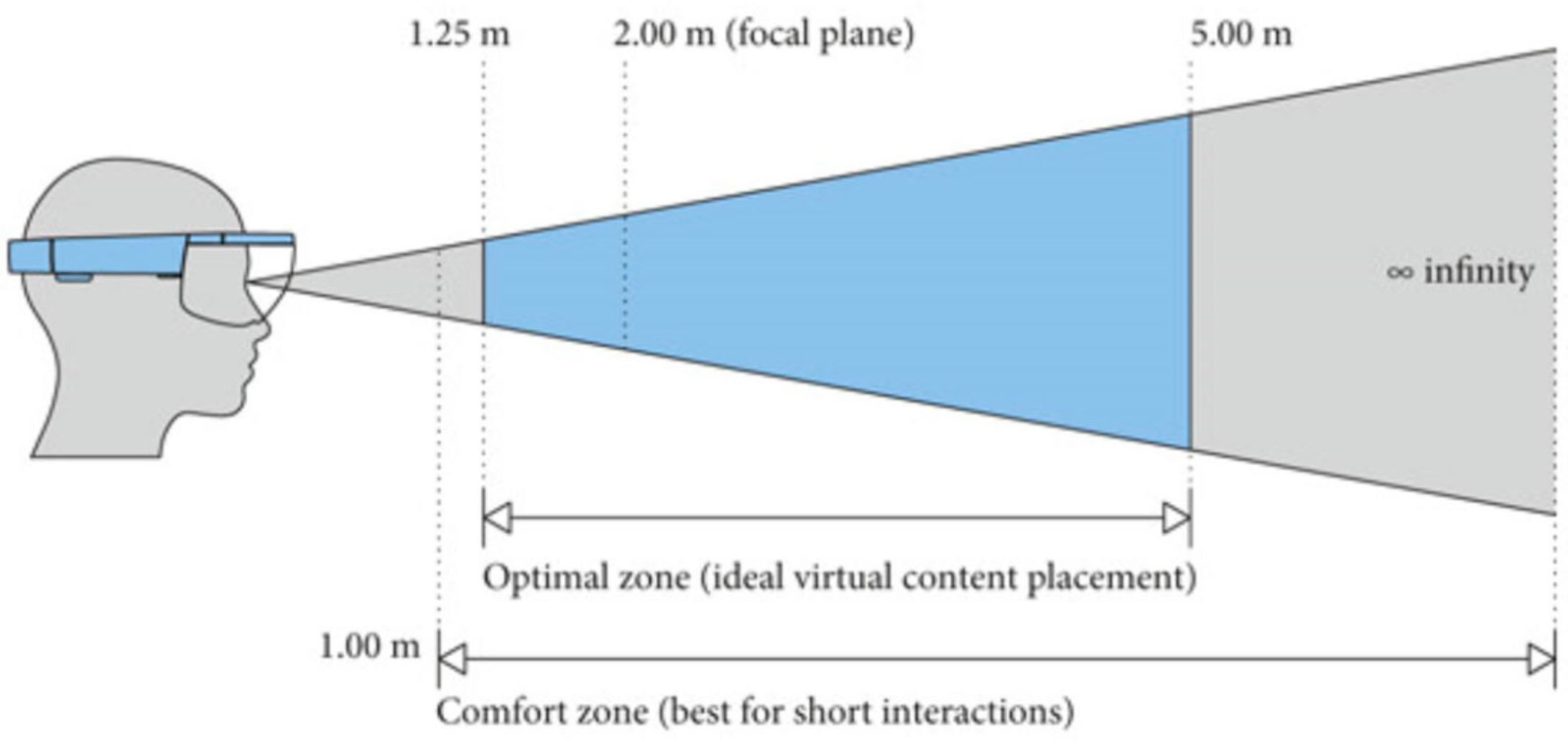
Despite these benefits and advantages of the HoloLens, challenges remain which need further optimization. The narrow field of view on the HoloLens also reduces immersion compared to its competitors, requiring students to adjust their perspective frequently. Some studies have shown that students may experience a higher cognitive load when learning via MR during simulated procedures, potentially impacting performance and the retention of tasks and knowledge [
19]. Cost remains as a further challenge, especially for places of education and token health care sites, which may struggle to pay for the technology [
19]. Finally, hardware challenges such as depth sensor noise and spatial–temporal mismatches between the virtual and real space continue to challenge seamless integration [
17].
The platform can go beyond training and planning and into worst-case scenario simulations for surgical residents. Trainees can handle complications, like a fracture or unexpected bleeding, using holographic patients’ anatomy. This creates a standardized global experience for surgical training and exposes residents to rare complications so that they can manage the complication multiple times before encountering it in real life [
17].
Medical education is changing, and MR technologies like the HoloLens will bridge theoretical learning and practice with experience, creating improved training and precision during surgery. Ongoing hardware and software improvements, such as embracing and expanding the field of view, resolution, and ease of use will enhance their utility. Continued research and development will allow the HoloLens to serve as a key part of medical education and surgical practice while transforming the teaching of anatomy and its clinical application [
20].
4.1.2. Apple Vision Pro
The Apple Vision Pro (
Figure 7 and
Figure 8) is emerging as an innovative technology and tool for orthopedic medical education and surgical practice, taking advantage of spatial computing and advanced technologies to transform education, pre-planning, and intraoperative processes. The high-resolution displays and field of view (~180 degrees) provide for immersive surgical simulations and can be especially effective in complex surgical procedures [
26,
29,
34].
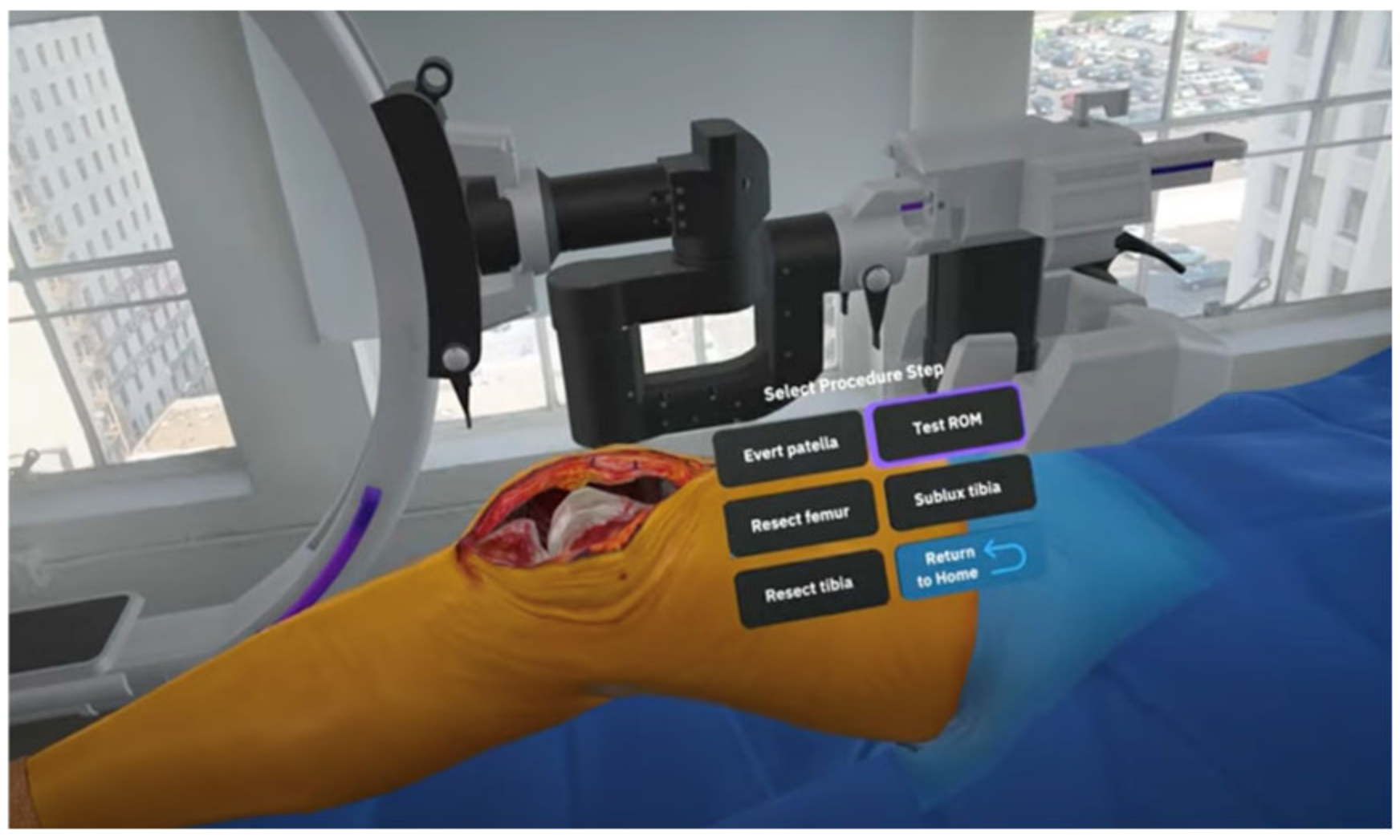
Osso VR, the first company to develop a virtual reality product for surgical education, recently developed the Osso Health app for the Apple Vision Pro (i.e., Osso Health). The app focuses on summary orthopedic surgical procedures, including carpal tunnel release (
Figure 9) and total knee replacement (
Figure 10), but uses spatial computing to walk users through key procedural steps and, to the extent possible, create a virtually lag-free learning environment. Dr. Justin Barad, co-founder and chief strategy officer at Osso VR, indicated the app would help scale spatial computing for healthcare and provide an important new way to address educational gaps [
26,
28,
29,
34,
39].
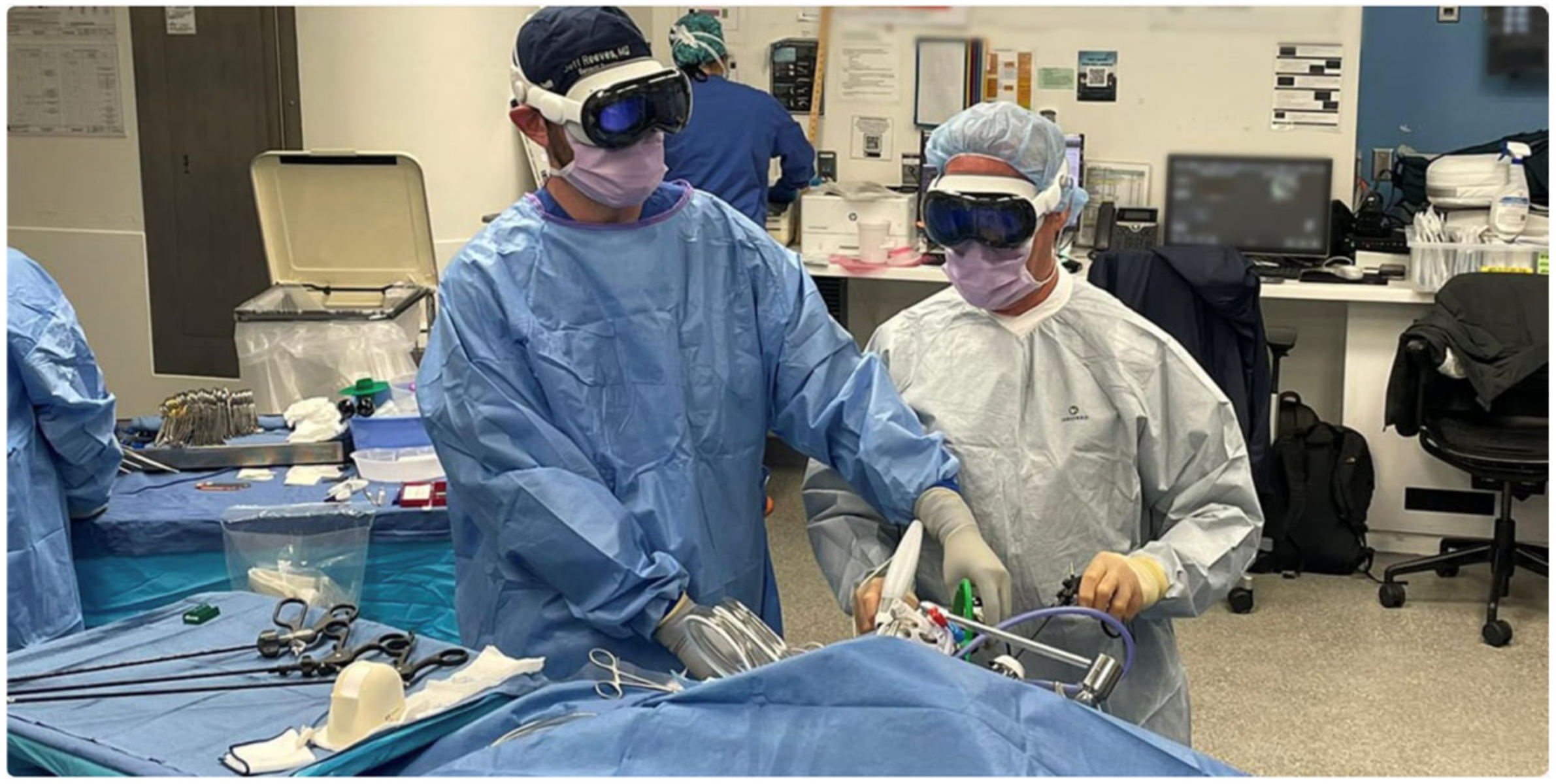
In clinical applications, Apple Vision Pro has already been used in real surgical settings. At Cromwell Hospital in London, the device has assisted surgical teams with real-time visualization of anatomical structures during spine surgeries [
26]. Similarly, at AdventHealth Surgery Center Innovation Tower, a surgical tech wore the Vision Pro goggles during a total shoulder replacement surgery, projecting mixed reality digital images of instruments needed and procedural steps (
Figure 11) [
27]. This implementation is estimated to increase operating room efficiency by 150% to 200%, ultimately benefiting patient safety.
UC San Diego Health has initiated a clinical trial to evaluate the use of spatial computing apps on Apple Vision Pro in the operating room (
Figure 12). The study aims to assess whether this technology can enhance the surgical experience by displaying patient medical imaging, vital signs, and surgical camera views in real time, potentially improving surgeons’ ergonomics [
33].
Though the Apple Vision Pro has the potential to lessen the number of changes needed for trainees to master procedures and improve accuracy (
Figure 13), there exist challenges. The relatively short battery life (~2 h) and expensive price point (~
$3499) could inhibit its usage by professionals for long periods, or in widespread educational settings. Ergonomics for long-term use in addition to use in a sterile procedure could require more research and development [
33,
34,
35].
As the field of orthopedic education and surgery continues to evolve, Apple Vision Pro and similar spatial computing technologies are poised to play an increasingly important role in bridging theoretical knowledge with practical application [
31]. Ongoing advancements and clinical trials will likely address current limitations, paving the way for more widespread integration into medical curricula and surgical workflows [
30,
31,
32,
33,
34,
35].
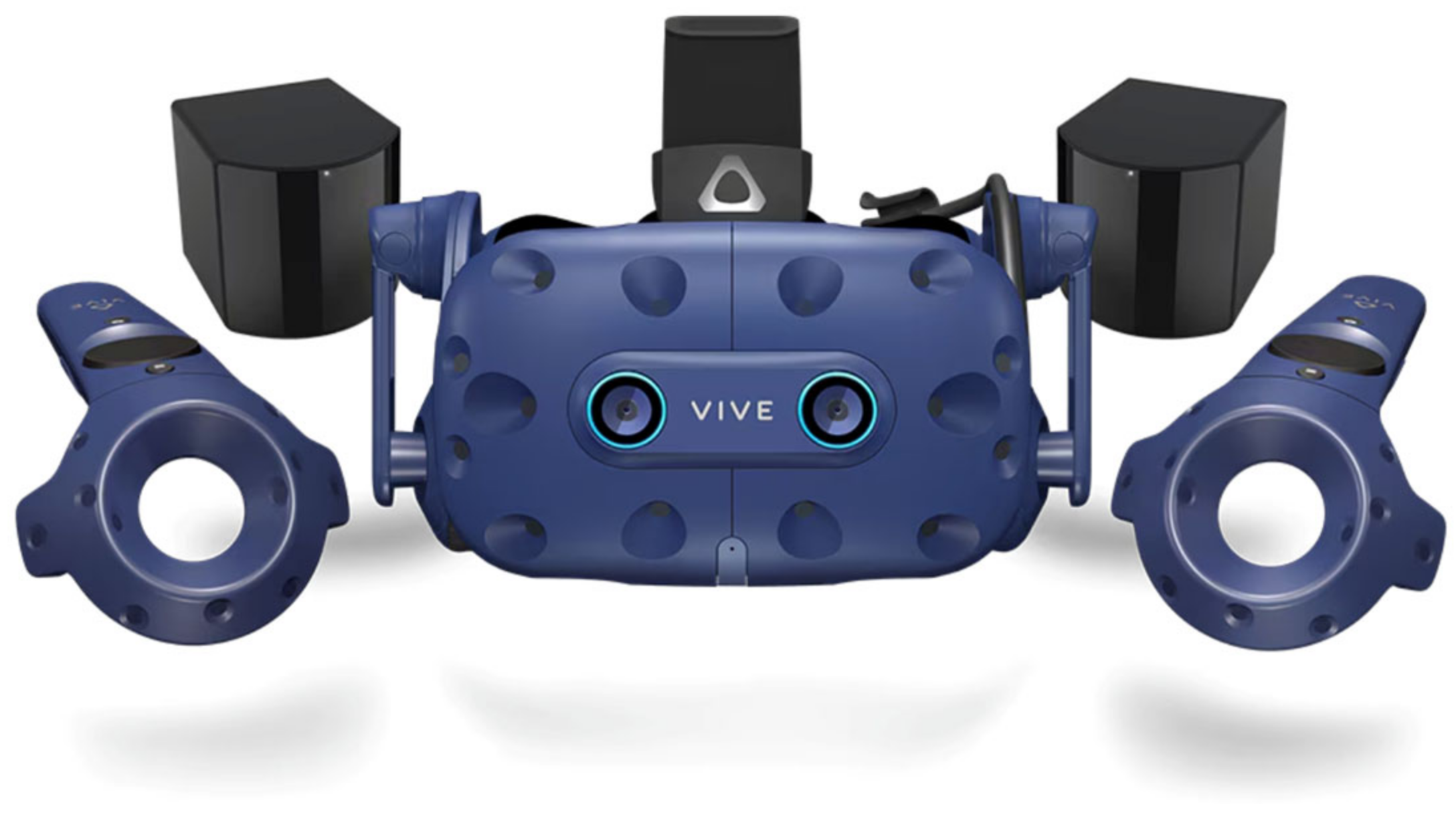
4.1.3. HTC Vive Pro
The HTC Vive Pro (
Figure 14) organizes an easy-to-use device with haptic feedback and room-scale tracking, making it a valuable tool for simulations in orthopedic training that need haptic fidelity and the ability to move the whole body. Multiple research studies have shown its advantages across a variety of surgical training modalities (
Figure 15 and
Figure 16). When trainees participated in pedicle screw placement through VR-training using the Vive Pro, there were improvements in screw placement accuracy from increased perceptual feedback on the angulation and depth of the screw placement [
36]. In this vein, the VirtX VR-system, based on the Vive Pro device, was shown to utilize less fluoroscopy for the same quality of images [
36]. In dynamic hip screw procedures, performance metrics improved based on the Vive Pro VR training, including reductions in incorrect steps and improved completion time [
36,
37,
38,
39,
40]. Further, a VR simulator for dynamic hip screw procedures showed that intraoperative imaging was improved, with trainees who had virtual training using the Vive Pro utilizing 75% less fluoroscopy and taking 66% fewer X-rays at the same level of post-training performance (
Figure 15 and
Figure 16) [
36,
37,
38,
39,
40].
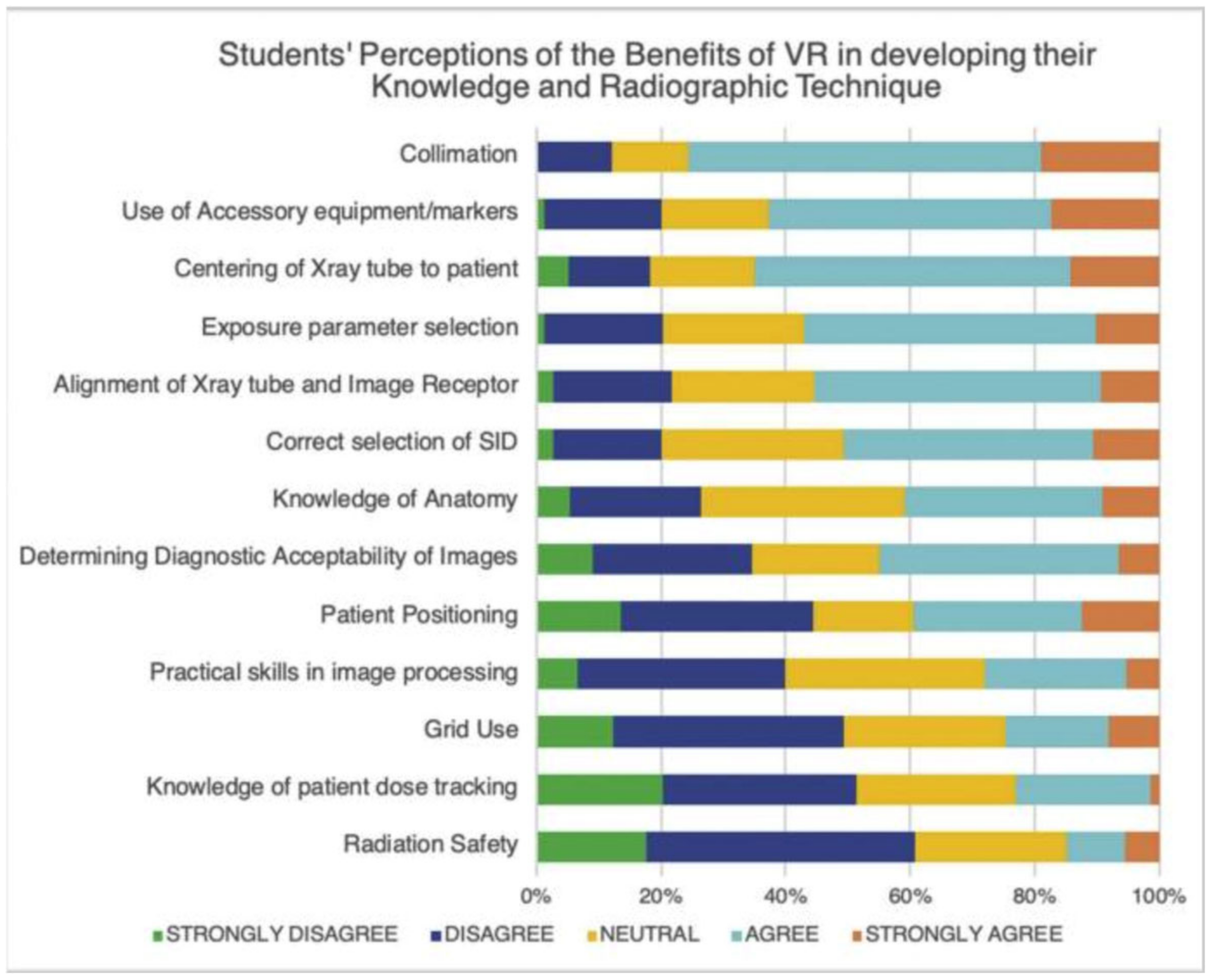
The HTC Vive Pro has proven effective in surgical training as an immersive and affordable alternative to other comparable devices such as the Microsoft HoloLens and the Apple Vision Pro. Its haptic feedback and room-scale tracking enhance tactile realism, making it particularly useful in orthopedic procedures and radiographic training. A study by O’Connor et al. (2021) demonstrated that a VR simulator increased student confidence in beam collimation, anatomical marker placement, the centering of the X-ray tube, and exposure parameter selection [
14,
37,
38,
39,
40].
Despite its strengths, HTC Vive Pro also has limitations due to cybersickness (CS), the cost of materials, and battery life. Approximately 30% of HTC Vive Pro users experience CS, representing a considerable barrier to long-term use in medical training. A systematic review of 223 articles on CS explains that there are three main factors involved: user-related factors, technology–system factors, and environmental–content factors. Some of the main contributors to CS are age, gender, pre-VR experience, postural stability, the refresh rate of the visual display, latency, the field of view (FoV), and inconsistency in motion. It is important to note that CS increases with latency >20 ms and a refresh rate for the visual display of <60Hz. A wider FoV, >110°, may also increase immersion but could also increase motion sickness due to excessive optical flow. Three general strategies, related to hardware, software, and user adaptation, can all help address issues associated with CS. Increasing the refresh rate to 90 Hz, reducing latency, and offering dynamic FoV control can all distinctly reduce symptoms. Software techniques like foveated rendering and vignette effects help to manage the visual burden, and slowly letting individuals expose themselves to VR environments will allow the individual time to adapt [
38,
39,
40].
Another recently published study in
Advances in Medical Education and Practice revealed the efficacy of VR (Osso VR) in orthopedic trauma training. The study’s authors tested the impact of Osso VR’s immersive and interactive platform and concluded that VR training provided better learning and proficiency (the execution of procedural steps) than curriculum-based training in teaching anatomy (
Figure 17) and aiding in surgery (
Figure 18) [
38,
39,
40].
4.2. Comparative Analysis and Limitations of MR Technologies in Orthopedic Rehabilitation
Each technology has different strengths to address different orthopedic education and rehabilitation objectives, and institutions need to consider their priorities, and the considerations provided. The HoloLens by Microsoft is superior in augmented reality applications and is a great option when real-time holographic overlay information would be helpful (e.g., preoperative planning or collaborative learning where surgeons could provide guidance to residents remotely using shared holographic views).
A limitation of the HoloLens when using it in the context of the orthopedic rehabilitation population includes ergonomic discomfort to the user. For example, when using the HoloLens for long periods in a single session (e.g., 40 min) it may cause postural discomfort or visual fatigue during use. There are also system registration errors rating an average of ~1.5–2.5 cm that may cause the virtual overlay to not be aligned or the closest to the physical anatomy, which is vital when precision is required in therapeutic exercise implementation (
Figure 19). However, these are just some of the issues imposed by the device; there are also limitations with people wearing corrective lens and/or costs to further develop the technology, which limit the use of the HoloLens in many rehabilitative programs [
41,
42,
43,
44,
45,
46].
In contrast, the Apple Vision Pro excels at providing an immersive experience using spatial computing to create a realistic atmosphere for complex procedural simulations such as total knee arthroplasty, which could potentially shorten the learning curve for trainees. Despite its high-fidelity spatial computing, the Vision Pro has specific limitations with rehabilitation. At 600 g, wearing the Vision Pro for a long time presents the potential for neck fatigue, lessening its value for prolonged rehabilitation. More seriously, in real time, challenges to overlay calibration such as latency or misalignment could interfere with motion-tracking reliability during guided therapeutic movements. Further, it is not designed to be used for medical procedures, which means the operating room workflow will need to be adjusted for sterility and for use with rehabilitation modalities, as noted by surgeons who reported sustained vision focus with mixed reality screens led to eye strain that could pose potential risk to patients undergoing vision-referenced motor retraining [
8,
41,
47].
The HTC Vive Pro stands out with its haptic feedback and room-scale tracking, making it particularly effective for hands-on surgical training. This tactile realism, as demonstrated by reduced errors and improved procedural efficiency in various studies, is critical for skill acquisition. For basic X-ray imaging, first-year radiography students reported increased confidence in beam collimation, anatomical marker placement, and the centering of the X-ray tube when using the HTC Vive Pro [
14,
15,
40]. In addition, VR simulator xRayWorld also helped students build a visuospatial understanding of X-ray imaging (
Figure 20 and
Figure 21) [
48].
The Vive Pro’s haptic feedback and room-scale tracking face rehabilitation-specific hurdles, including cybersickness, which up to 30% of users experience during dynamic simulations, posing problems for patients with vestibular impairments. Cybersickness, characterized by nausea, disorientation, and visual discomfort, varies based on VR content attributes such as camera movement, the field of view, and controllability. A study analyzing cybersickness across 52 VR scenes with 154 participants identified significant correlations between its severity and six brain activity biomarkers (e.g., Fp1 delta, Fp2 gamma, and T4 beta waves) with a determination coefficient exceeding 0.9. Individual characteristics, including age and susceptibility, also influence cybersickness levels. Using this data, researchers developed predictive models to quantify and anticipate cybersickness, making the dataset broadly applicable for optimizing VR experiences and minimizing adverse effects [
39,
49].
Furthermore, patients may struggle with controller operations, necessitating extensive pre-training that delays therapy initiation. The high hardware costs (~
$1500/headset) and limited evidence of long-term efficacy raise questions about ROI in outpatient settings [
50,
51].
Ultimately, platform choice will depend on the institutional priority, such as prioritizing AR-guided anatomy visualization with HoloLens, immersive spatial computing with Vision Pro, and tactile skill development with Vive Pro, while remaining budget conscious. All of these will factor into the platforms’ general effectiveness and appropriateness regarding orthopedic education and training.
All of the platforms face the same issues: standardization gaps in tracking protocols and ethical dilemmas of maintaining data privacy. While all platforms aid in promoting engagement, if a person relies too much on a platform, it can detract from the hands-on opportunities with the patient themselves and from using indirect observational measures to evaluate subtle patient biomechanical cues [
17,
51]. Improving the shortcomings of these platforms will rely on iterative hardware updates, cost mitigation, and completing rigorous clinical studies to support rehabilitation claims made on patient outcomes [
41,
46,
51].
5. Limitations to Integration of AI-Based Platforms in Orthopedic Medical Education
The integration of artificial intelligence (AI) into orthopedic education faces several significant barriers that need to be addressed for successful implementation. These challenges span various domains, including data standardization, algorithm evaluation, ethics, and curriculum integration.
Data standardization remains a critical hurdle in AI adoption for orthopedic education. The heterogeneity of medical data sources, formats, and terminologies poses significant challenges for AI model development and deployment. A study by SignalFire (2024) highlights that most healthcare data currently reside in siloed systems within individual health organizations, making it difficult to access and utilize for AI training. Furthermore, regulations such as HIPAA and GDPR often complicate the sharing of patient data. The study also notes that while standards like FHIR and OMOP have improved data-sharing capabilities, they lack the flexibility required for the multimodal longitudinal datasets increasingly used in AI research [
52].
Algorithm evaluation presents another significant barrier. The accuracy and reliability of AI algorithms in orthopedic applications are crucial for their acceptance in educational and clinical settings. A recent study published in
Bone and Joint Research (2023) emphasizes the need for robust reporting and validation frameworks to prevent avoidable errors and biases in AI applications for orthopedic surgery [
51]. The study also highlights the importance of establishing systematic validation processes to allow for the safe adoption of AI technology in clinical practice.
Ethical considerations form a substantial barrier to AI integration in orthopedic education. A comprehensive ethical framework is essential to address issues such as algorithmic bias, data privacy, and equitable access to AI-driven healthcare innovations. A study published in the
World Journal of Gastroenterology (2024) proposes an ethical framework centered around the four key principles of medical ethics: respect for autonomy, beneficence, non-maleficence, and justice. The framework emphasizes the need for regular audits of AI systems for bias and the implementation of corrective measures when disparities are identified (
Figure 22) [
53].
Integrating AI into the medical school curriculum presents its own set of challenges. Despite the growing use of AI in healthcare, there is a notable lack of formal AI instruction in undergraduate medical education. A study published in PMC (2022) highlights that only 5.9% of medical schools in the United States offer formal AI training. The study identifies several barriers to AI curriculum integration, including uncertainty about effective delivery methods, limitations in available curricular hours, and a lack of faculty expertise in AI. The study goes on to propose that students may start to rely on AI for clinical decision-making and hamper their growth as physicians [
54].
Addressing these barriers requires a multifaceted approach involving collaboration between medical educators, technology developers, and policymakers. As AI continues to evolve and become more prevalent in healthcare, overcoming these challenges will be crucial for preparing future orthopedic surgeons to effectively utilize and critically evaluate AI technologies in their practice.
6. Conclusions
The incorporation of AI and mixed reality technology into orthopedic medical education constitutes a significant change in how we will train future orthopedic surgeons. The benefits of immersive and interactive education are unparalleled with the availability of devices like the Microsoft HoloLens, Apple Vision Pro, and HTC Vive Pro, facilitating the acquisition of complex orthopedic skills and knowledge [
18,
36,
42,
55].
While challenges related to implementation and integration persist, particularly related to costs and technical constraints, as well as further integration into the curriculum, the potential benefits of these technologies are worth it. Benefits in spatial understanding, procedural training, and personalized learning are readily identified advantages of these technologies, with ongoing research looking to explore the optimal utilization of AI, enabling even more personalized and optimal learning pathways [
14,
15,
31,
46,
47,
48,
56]. As we continue to grow into these technologies, there will clearly be increasing utilization in orthopedic education. Therefore, it will be paramount for educators, technology developers, and AI researchers to continue to collaborate in developing these innovations and moving forward in orthopedic medical education [
46].
Future research should focus on developing standardized protocols for integrating these technologies into medical curricula and conducting longitudinal studies to assess the long-term impact on clinical competence and patient outcomes. With ongoing refinement and thoughtful implementation, AI and MR platforms have the potential to redefine the landscape of orthopedic education and shape the next generation of surgical leaders.
Author Contributions
Conceptualization, Writing—Original Draft, Writing—Review and Editing, Visualization, and Methodology, K.S.; Writing—Review and Editing, Supervision, and Validation, R.K.; Methodology, Supervision, Validation, and Writing—Review and Editing, P.P.; Project Administration, Supervision, and Writing—Review and Editing, J.O.; Formal Analysis and Writing—Review and Editing, T.S.; Writing—Review and Editing and Visualization, S.V.; Supervision, Methodology, and Writing—Review and Editing, T.H.; Supervision and Writing—Review and Editing, E.W.; Formal Analysis and Writing—Review and Editing, C.G.; Formal Analysis and Writing—Review and Editing, R.J.; Formal Analysis and Writing—Review and Editing, N.Z.; Methodology and Writing—Review and Editing, A.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
Thank you to Boomie Xiong for providing us with an APC waiver.
Conflicts of Interest
Ram Jagadeesan has a conflict of interest as an employee that holds stock interest in Cisco.
References
- Rasouli, S.; Alkurdi, D.; Jia, B. The Role of Artificial Intelligence in Modern Medical Education and Practice: A Systematic Literature Review. medRxiv 2024. [Google Scholar] [CrossRef]
- Misir, A. Enhancing Orthopedic Residency Training with Artificial Intelligence. Linkedin.com. 28 February 2025. Available online: https://www.linkedin.com/pulse/enhancing-orthopedic-residency-training-artificial-abdulhamit-misir-siyff (accessed on 26 March 2025).
- Nair, V.; Todkar, A.; Kumar, H. The Future of Orthopaedic Education and Training: Embracing Innovation for a Changing Landscape. Cureus 2024, 16, e67146. [Google Scholar] [CrossRef] [PubMed]
- Cooper, H.J. A View of Mixed-Reality Tech’s Future in Orthopedics. OrthoFeed. 30 March 2024. Available online: https://orthofeed.com/2024/03/30/a-view-of-mixed-reality-techs-future-in-orthopedics/ (accessed on 26 March 2025).
- Yang, J.; Zhang, J.; Zeng, C.; Fang, Y.; Xue, M.; Wang, H.; Zhou, H.; Xie, Y.; Liu, P.; Ye, Z. Application and prospect of mixed reality technology in orthopedics. Digit. Med. 2023, 9, e00010. [Google Scholar] [CrossRef]
- Combalia, A.; Sanchez-Vives, M.V.; Donegan, T. Immersive virtual reality in orthopaedics—A narrative review. Int. Orthop. 2024, 48, 21–30. [Google Scholar] [CrossRef]
- Lu, L.; Wang, H.; Liu, P.; Liu, R.; Zhang, J.; Xie, Y.; Liu, S.; Huo, T.; Xie, M.; Wu, X.; et al. Applications of Mixed Reality Technology in Orthopedics Surgery: A Pilot Study. Front. Bioeng. Biotechnol. 2022, 10, 740507. [Google Scholar] [CrossRef]
- Gupta, N.; Walker, J.; Turnow, M.; Kasmenn, M.; Patel, H.; Sydow, E.; Manes, T.; Williamson, T.; Patel, J. Use of Mixed Reality Technologies by Orthopedic Surgery Residents: A Cross-Sectional Study of Trainee Perceptions. J. Orthop. Exp. Innov. 2024, 5, 2–10. [Google Scholar] [CrossRef]
- Tingey, M.T.; Taylor, P.R. Orthopaedic Surgery in the Metaverse: Current Data on Virtual-Reality Based Training. Int. J. Med. Stud. 2023, 11, S78. [Google Scholar] [CrossRef]
- Ogundairo, P. Hololens vs. Vision Pro: Which Is a Better Buy? TechWriteable. 13 March 2024. Available online: https://techwriteable.com/microsoft-hololens-2-vs-apple-vision-pro-which-is-a-better-buy/ (accessed on 26 March 2025).
- Bowden, Z. Apple’s AR Vision Pro Headset Isn’t the HoloLens Competitor I Thought It Was Going to Be. Windows Central. 6 June 2023. Available online: https://www.windowscentral.com/apple/apples-ar-vision-pro-headset-isnt-the-hololens-competitor-i-thought-it-was-going-to-be (accessed on 26 March 2025).
- Lamb, A.; McKinney, B.; Frousiakis, P.; Diaz, G.; Sweet, S. A Comparative Study of Traditional Technique Guide versus Virtual Reality in Orthopedic Trauma Training. Adv. Med. Educ. Pract. 2023, 14, 947–955. [Google Scholar] [CrossRef]
- Pratap, J.; Laane, C.; Chen, N.; Bhashyam, A. Virtual reality training for intraoperative imaging in orthopaedic surgery: An overview of current progress and future direction. Front. Virtual Real. 2024, 5, 1392825. [Google Scholar] [CrossRef]
- O’Connor, M.; Stowe, J.; Potocnik, J.; Giannotti, N.; Murphy, S.; Rainford, L. 3D virtual reality simulation in radiography education: The students’ experience. Radiography 2021, 27, 208–214. [Google Scholar] [CrossRef]
- D’Urso, F.; Priscitelli, P.; Miani, A.; Broccolo, F. Revolutionizing Medical Education: The Impact of Virtual and Mixed Reality on Training and Skill Acquisition. Trends Telemed. E-Health 2024, 4, 000598. [Google Scholar] [CrossRef]
- Texas, S. Revolutionizing Medical Education: The HoloAnatomy Experience|IT.tamu.edu. 18 February 2025. Available online: https://it.tamu.edu/about/news/2024/05/hololens-news-story.php (accessed on 26 March 2025).
- Tătaru, O.S.; Ferro, M.; Marchioni, M.; Veccia, A.; Coman, O.; Lasorsa, F.; Brescia, A.; Crocetto, F.; Barone, B.; Catellani, M.; et al. HoloLens® platform for healthcare professionals simulation training, teaching, and its urological applications: An up-to-date review. Ther. Adv. Urol. 2024, 16, 17562872241297554. [Google Scholar] [CrossRef]
- Khoo, G.; Yap, A.; Yak, W.Y. Medical Education Goes Holographic with Mixed Reality from Microsoft. Singapore News Center. 11 January 2022. Available online: https://news.microsoft.com/en-sg/2022/01/11/medical-education-goes-holographic-with-mixed-reality-from-microsoft/ (accessed on 26 March 2025).
- Connolly, M.; Iohom, G.; O’brien, N.; Volz, J.; O’muircheartaigh, A.; Serchan, P.; Biculescu, A.; Gadre, K.G.; Soare, C.; Griseto, L.; et al. Delivering clinical tutorials to medical students using the Microsoft HoloLens 2: A mixed-methods evaluation. BMC Med. Educ. 2024, 24, 498. [Google Scholar] [CrossRef]
- Cleveland Clinic. Case Western Reserve, Cleveland Clinic Collaborate with Microsoft on Earth-Shattering Mixed-Reality Technology for Education. 2015. Available online: https://case.edu/hololens/ (accessed on 26 March 2025).
- Roettgers, J. Microsoft HoloLens Costs Developers $3000, Starts Shipping Next Month. Variety. 29 February 2016. Available online: https://variety.com/2016/digital/news/microsoft-hololens-dev-kit-3000-dollars-preorders-1201718230/ (accessed on 26 March 2025).
- Chen, C.; Zhang, L.; Luczak, T.; Smith, E.; Burch, R.F. Using Microsoft HoloLens to improve memory recall in anatomy and physiology: A pilot study to examine the efficacy of using augmented reality in education. J. Educ. Technol. Dev. Exch. 2019, 12, 2. [Google Scholar] [CrossRef]
- Stojanovska, M.; Tingle, G.; Tan, L.; Ulrey, L.; Simonson-Shick, S.; Mlakar, J.; Eastman, H.; Gotschall, R.; Boscia, A.; Enterline, R.; et al. Mixed Reality Anatomy Using Microsoft HoloLens and Cadaveric Dissection: A Comparative Effectiveness Study. Med. Sci. Educ. 2019, 30, 173–178. [Google Scholar] [CrossRef]
- Richards, S. Student Engagement Using HoloLens Mixed-Reality Technology in Human Anatomy Laboratories for Osteopathic Medical Students: An Instructional Model. Med. Sci. Educ. 2023, 33, 223–231. [Google Scholar] [CrossRef]
- Ali, A.; Baseer, N.; Huma, Z.; Yousafzai, Y.M.; Shah, I.; Zia, A.; Alorini, M.; Sethia, N. Mixed reality model for learning and teaching in anatomy using peer assisted learning approach. Eur. J. Anat. 2023, 27, 129–138. [Google Scholar] [CrossRef]
- Osso, V.R. Osso Health Medical Training App Launches for Apple Vision Pro. 11 April 2024. Available online: https://www.ossovr.com/press-releases/osso-health-medical-training-apple-vision-pro (accessed on 26 March 2025).
- Koblentz, E. Apple Highlights Stryker, an NJIT Alum’s Medical Tech Group, for VisionPro App. NJIT News. 15 March 2024. Available online: https://news.njit.edu/apple-highlights-stryker-njit-alums-medical-tech-group-visionpro-app (accessed on 27 March 2025).
- Orthopedics Today. Osso VR Launches Immersive Reality Medical Training App. 14 April 2024. Available online: https://www.healio.com/news/orthopedics/20240412/osso-vr-launches-immersive-reality-medical-training-app (accessed on 26 March 2025).
- Whooley, S. Osso VR Launches Medical Training App for Apple Vision Pro. MassDevice. 11 April 2024. Available online: https://www.massdevice.com/osso-vr-launches-app-apple-vision-pro/ (accessed on 26 March 2025).
- Apple. Apple Vision Pro Unlocks New Opportunities for Health App Developers. Apple Newsroom. 11 March 2024. Available online: https://www.apple.com/newsroom/2024/03/apple-vision-pro-unlocks-new-opportunities-for-health-app-developers/ (accessed on 26 March 2025).
- Egger, J.; Gsaxner, C.; Luijten, G.; Chen, J.; Chen, X.; Bian, J.; Kleesiek, J.; Puladi, B. Is the Apple Vision Pro the Ultimate Display? A First Perspective and Survey on Entering the Wonderland of Precision Medicine. JMIR Serious Games 2024, 12, e52785. [Google Scholar] [CrossRef]
- Apple Inc. Introducing Apple Vision Pro: Apple’s First Spatial Computer. Apple Newsroom. 5 June 2023. Available online: https://www.apple.com/newsroom/2023/06/introducing-apple-vision-pro/ (accessed on 26 March 2025).
- Brubaker, M. Clinical Trial Evaluates Spatial Computing App on Apple Vision Pro in Operating Room. UC San Diego Health. 16 September 2024. Available online: https://health.ucsd.edu/news/press-releases/2024-09-16-clinical-trial-evaluates-spatial-computing-app-on-apple-vision-pro-in-operating-room/ (accessed on 26 March 2025).
- Dermody, T. Osso VR Launches Surgical Training App for Apple Vision Pro. Perplexity AI. 11 April 2024. Available online: https://www.mobihealthnews.com/news/osso-vr-launches-surgical-training-app-apple-vision-pro (accessed on 26 March 2025).
- Sarwar, F. Apple Vision Pro vs. Microsoft HoloLens: Battle of XR Headsets. Syntech. 14 February 2025. Available online: https://syntechhome.com/blogs/news/apple-vision-pro-vs-microsoft-hololens (accessed on 26 March 2025).
- Camp, J.V. HTC Vive Pro Review: An Expensive VR Upgrade. WIRED. 11 May 2018. Available online: https://www.wired.com/review/review-htc-vive-pro/ (accessed on 26 March 2025).
- Lohre, R.; Bois, A.J.; Pollock, J.W.; Lapner, P.; McIlquham, K.; Athwal, G.S.; Goel, D.P. Effectiveness of Immersive Virtual Reality on Orthopedic Surgical Skills and Knowledge Acquisition Among Senior Surgical Residents. JAMA Netw. Open 2020, 3, e2031217. [Google Scholar] [CrossRef]
- Biswas, N.; Mukherjee, A.; Bhattacharya, S. “Are you feeling sick?”—A systematic literature review of cybersickness in virtual reality. ACM Comput. Surv. 2024, 56, 284. [Google Scholar] [CrossRef]
- Osso, V.R. New Study Shows Virtual Reality Training Outperforms Traditional Methods in Orthopedic Surgical Education. 9 November 2023. Available online: https://www.ossovr.com/press-releases/vr-training-outperforms-traditional-methods-in-orthopedic-surgical-education (accessed on 26 March 2025).
- Waisberg, E.; Ong, J.; Masalkhi, M.; Zaman, N.; Sarker, P.; Lee, A.G.; Tavakkoli, A. Apple Vision Pro: The future of surgery with advances in virtual and augmented reality. Ir. J. Med. Sci. 2024, 193, 345–346. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.-Z.; Feng, X.-B.; Shao, Z.-W.; Xie, M.; Xu, S.; Wu, X.-H.; Ye, Z.-W. Application and Prospect of Mixed Reality Technology in Medical Field. Curr. Med. Sci. 2019, 39, 1–6. [Google Scholar] [CrossRef] [PubMed]
- HTC Vive Pro. VIVE Pro Eye Launches Today in North America, Setting a New Standard for Enterprise Virtual Reality. 2019. Available online: https://www.htc.com/us/newsroom/2019-06-06/ (accessed on 27 March 2025).
- Johnson, T. Surgical Team at AdventHealth Performs World’s First of Its Kind Procedure Using Apple Vision Pro Mixed Reality System. AdventHealth. 11 November 2024. Available online: https://www.adventhealth.com/business/adventhealth-central-florida-media-resources/news/surgical-team-adventhealth-performs-worlds-first-its-kind-procedure-using-apple-vision-pro-mixed (accessed on 26 March 2025).
- Paladugu, P.; Kumar, R.; Ong, J.; Waisberg, E.; Sporn, K. Virtual reality-enhanced rehabilitation for improving musculoskeletal function and recovery after trauma. J. Orthop. Surg. Res. 2025, 20, 404. [Google Scholar] [CrossRef]
- Asim, A. This New Apple Vision Pro App Lets You Practice Complex Medical Surgeries in Mixed Reality. PhoneArena. 22 April 2024. Available online: https://www.phonearena.com/ar-vr/news/apple-vision-pro-app-medical-surgeries-mixed-reality_id157582 (accessed on 24 April 2025).
- Condino, S.; Turini, G.; Parchi, P.D.; Viglialoro, R.M.; Piolanti, N.; Gesi, M.; Ferrari, M.; Ferrari, V. How to Build a Pa-tient-Specific Hybrid Simulator for Orthopaedic Open Surgery: Benefits and Limits of Mixed-Reality Using the Microsoft HoloLens. J. Healthc. Eng. 2018, 2018, 5435097. [Google Scholar] [CrossRef]
- Wong, K.C.; Sun, Y.E.; Kumta, S.M. Review and Future/Potential Application of Mixed Reality Technology in Orthopaedic Oncology. Orthop. Res. Rev. 2022, 14, 169–186. [Google Scholar] [CrossRef]
- Lenz, F.; Fock, M.; Kramer, T.; Petersen, Y.; Teistler, M. A Virtual Reality Game to Support Visuospatial Understanding of Medical X-Ray Imaging. 2021. Available online: https://hs-flensburg.de/sites/default/files/2022-02/xrayworld_segah2021_finalsubmission.pdf (accessed on 27 March 2025).
- Liu, T.W.; Siu, P.K.T.; Wong, T.M. Virtual Reality in Sport Rehabilitation: A Narrative Review. J. Athl. Enhanc. 2022, 11, 6. [Google Scholar]
- Lazar, M. A Guide to Applying Virtual Reality in Medical Training. HyperSense Blog. 27 September 2024. Available online: https://hypersense-software.com/blog/2024/09/25/virtual-reality-medical-training/ (accessed on 27 March 2025).
- Lisacek-Kiosoglous, A.B.; Powling, A.S.; Fontalis, A.; Gabr, A.; Mazomenos, E.; Haddad, F.S. Artificial intelligence in orthopaedic surgery. Bone Jt. Res. 2023, 12, 447–454. [Google Scholar] [CrossRef]
- Pezzullo, T.; Rahoof, S.; Simcox, E. How Standardized Data and Smarter Sharing Can Unlock Healthcare AI’s Full Potential. 20 November 2024. Available online: https://www.signalfire.com/blog/healthcare-ai-data (accessed on 28 March 2025).
- Abujaber, A.A.; Nashwan, A.J. Ethical framework for artificial intelligence in healthcare research: A path to integrity. World J. Methodol. 2024, 14, 94071. [Google Scholar] [CrossRef]
- Ngo, B.; Nguyen, D.; Vansonnenberg, E. The Cases for and against Artificial Intelligence in the Medical School Curriculum. Radiol. Artif. Intell. 2022, 4, e220074. [Google Scholar] [CrossRef]
- Shanbhag, N.M.; Bin Sumaida, A.; Al Shamisi, K.; Balaraj, K. Apple Vision Pro: A Paradigm Shift in Medical Technology. Cureus 2024, 16, e69608. [Google Scholar] [CrossRef]
- Oh, H.; Son, W. Cybersickness and Its Severity Arising from Virtual Reality Content: A Comprehensive Study. Sensors 2022, 22, 1314. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Academic Society for International Medical Education. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).