Abstract
Medical students (MS) are at higher risk for depression than their peers. Incoming U.S. MS completed a survey that included the validated RS-14, which measures resilience and its two subcomponents: self-assuredness and drive. Surveys were administered before classes started in 2019 (pre-pandemic-cohort; n = 178) and 2020 (pandemic-cohort; n = 181). Resiliency, self-assuredness, and drive were not different between cohorts. Demographic subgroup analyses revealed that underrepresented in medicine (URiM) MS in the pre-pandemic-cohort scored higher on drive (p = 0.007) than non-URiM MS (6.07 ± 1.00 vs. 5.59 ± 0.97); however, this difference was not significant in the pandemic-cohort. Additionally, students in the pandemic-cohort were more likely to agree that peer discussions about emotional challenges would be beneficial (p = 0.014). Qualitative analysis revealed that 45.9% of pandemic-cohort respondents felt more motivated to pursue medicine. This is the first study to report differences in drive between URiM MS cohorts matriculating before and during a pandemic, a positive correlation between multiple-mini-interview (MMI) scores and drive, and a negative correlation between MCAT scores and drive. Collectively, these results suggest that the circumstances of 2020 may have negatively influenced the drive of URiM students, positively impacted the receptivity of MS to peer discussions, and motivated students to pursue medicine.
1. Introduction
Researchers have consistently demonstrated the devastating impact of the COVID-19 pandemic on healthcare workers. In an early study of healthcare workers in February 2020 in Wuhan, China (n = 5062), 29.8% of respondents reported stress, 24.1% reported anxiety, and 13.5% reported symptoms of depression. Many of these healthcare workers have also cited fear for themselves or their families, with 56.9% of respondents stating they fear for their own lives due to possible infection and 92.1% of respondents stating they are fearful their loved ones may become infected. Furthermore, while this study was conducted early into the pandemic, 8 and 10 February 2020, 10.1% of respondents cited thoughts of resigning from the medical field due to the pandemic [1]. Medical students (MS) were particularly vulnerable because of interruptions in medical education, which included an abrupt transition to electronic learning, suspended clinical rotations, decreased career exploration opportunities, and a high risk of infection and transmission to loved ones [2]. Most U.S. medical schools abruptly halted clinical training and transitioned to an electronic learning environment [3,4]. Digital learning has been associated with mental health deterioration and increased levels of cynicism among MS [4].
Researchers have reported that MS have higher rates of burnout and lower quality of life than age-matched populations [5,6,7]. These trends continue as students transition to residency and become practicing physicians [8]. Unfortunately, despite relative plateaus in burnout rates amongst other working professionals, they have continued to rise among U.S. physicians [9]. Chronic stressors experienced by healthcare workers contribute to burnout rates, leading to clinician attrition and negative impacts on patient care [6,10,11,12,13,14,15].
1.1. Resilience
Understanding positive wellness factors, such as resilience, is necessary when considering MS’ well-being. In alignment with the definition put forth by Forycka et al. (2022) and Howe et al. (2012), we define resilience as a dynamic process involving both adaptability and flexibility, in which one effectively bounces back from negative experiences and adapts to new stressful situations [16,17]. Resilient people are more likely to respond constructively to stress by furthering self-improvement despite challenges. Resilience positively affects well-being while decreasing burnout and perceived stress [18,19,20,21]. Encouraging a growth mindset, the belief that people can positively change and adapt to obstacles and challenges, supports increased resilience [22,23]. One study found that most MS had low measures of resilience and higher burnout during the pandemic. Importantly, those with higher resilience levels maintained better attitudes toward electronic learning and exhibited lower rates of burnout, exhaustion, and cynicism [16].
Resilience has been assessed through various scales and metrics [24]. The Resilience Scale (RS-14) is a validated 14-item survey with Cronbach’s alphas ranging from 0.89 to 0.96 that has been licensed to measure resilience [25,26]. The RS-14 is relatively efficient while maintaining high validity and reliability and has been used to study resilience in MS globally [23,27,28,29,30]. The RS-14 has been significantly positively correlated with measures of positive concepts, including optimism, self-efficacy, and gratitude, and negatively correlated with indices of psychological distress [31].
1.2. Racial Injustices in the United States
Racial injustices that took place in the summer of 2020, including the murders of Breonna Taylor, Ahmaud Arbery, and George Floyd, led to protests across the U.S. and in over 60 countries [32]. It is important to consider that MS may have been impacted by these events, particularly those who have self-categorized via AMCAS as under-represented in medicine (URiM). Data from the 2016–2017 Association of American Medical Colleges Graduation Questionnaire showed that URiM students were more likely to feel exhausted by the pressures of medical school [33]. In another multi-institutional study conducted prior to COVID-19 (n = 3080), URiM students reported that their race/ethnicity had adversely affected their medical school experiences (11% vs. 2%; p < 0.001), citing various causative factors, including racial discrimination, prejudice, feelings of isolation, and contrasting cultural expectations [34]. In the current study about resilience, it is critical to consider the impact of these events amidst the COVID-19 pandemic, especially on incoming URiM students.
This study assessed resilience in MS matriculating before and during the COVID-19 pandemic and racial injustices of 2020 (as they cannot be separated). In addition, we assessed the attitudes of incoming MS toward discussing resilience with peers and their feelings about pursuing a medical career amidst a pandemic. We also aimed to determine if any relationships exist between resiliency scores and admission metrics, including MMI, Casper, and MCAT scores. Findings from this study may support an understanding of incoming MS’ well-being and resilience and could help us understand whether admissions tools effectively assess elements of resiliency.
2. Materials and Methods
A voluntary, anonymous, cross-sectional study was conducted. An electronic survey was administered during the New York Medical College (NYMC) first-year MS orientation in August 2019 to the entire MS Class of 2023 (pre-pandemic-cohort) and September 2020 to the entire MS Class of 2024 (pandemic-cohort). The Qualtrics survey included the validated RS-14 questions and three school-specific Likert scale questions about tools of resilience, benefits of open discussion, and resilience as a teachable skill (Appendix A.1). The initial purpose of the survey, prior to the pandemic, was to measure resiliency over the course of a four-year medical school program; however, the survey was amended for the incoming pandemic-cohort to include seven questions related to COVID-19 (Appendix A.2). Participation was voluntary. An electronic consent form appeared prior to the survey; if a MS declined, the survey was not administered.
The RS-14 uses a Likert scale with seven possible responses for each item ranging from 1 (strongly disagree) to 7 (strongly agree); higher scores indicate greater resilience [35]. Burgis-Kasthala (2019) confirmed the validity of the RS-14; exploratory factor analysis suggested two latent factors: “self-assuredness” and “drive.” Self-assuredness relates to nine items on the RS-14 scale, while drive relates to three items [36].
AMCAS demographic subgroup categories included the following: sex, URiM, fee assistance program (FAP) participation, and socioeconomically disadvantaged (SED) status. Accommodation status, defined as having registered with the institution’s disability office within the first year of medical school, as well as MCAT, multiple-mini-interview (MMI), and Computer-based Assessment for Sampling Personal Characteristics (Casper) scores were explored for relationships with resilience measures.
2.1. Quantitative Data Analysis
The Mann–Whitney–Wilcoxon tests assessed differences in overall resilience, self-assuredness, and drive between cohorts. Classes were stratified by sex, URiM, FAP, SED, and accommodation status. We performed demographic subgroup stratified analyses and examined possible differences between subgroups in overall resilience, self-assuredness, and drive with univariate analysis of variance (UNIANOVA). Asymptotic significance p-values (two-tailed) were used when exact significance values were unavailable.
2.2. Qualitative Data Analysis
A qualitative analysis of the survey’s open responses was performed using inductive analysis [37] through open coding, category creation, and abstraction. Open coding was conducted by reading participants’ responses and noting repeated themes to create categories. Subsequently, all team members reviewed and agreed on suggested categories. (Appendix B.1) The process of abstraction was performed, combining categories to develop succinct, specific categories that included each response. Again, all team members reviewed and agreed on the combined categories.
This study was reviewed and approved by the NYMC IRB (14107).
3. Results
The survey was emailed to the incoming pre-pandemic (n = 215) and pandemic-cohorts (n = 217). Of those invited, 178 pre-pandemic MS (82.8%) and 181 pandemic MS (83.4%) participated (Table 1).

Table 1.
Characteristics of entering medical student participants by class.
3.1. Quantitative Analysis
In aggregate, the RS-14 overall resilience scores did not differ significantly between the two MS cohorts (p = 0.938; Table 2). Additionally, there was no significant difference in self-assuredness (p = 0.796) or drive (p = 0.983). Demographic subgroup analyses between class years by sex, URiM, FAP participant, and SED status revealed no significant differences in overall resilience or self-assuredness (Table 2). Similarly, accommodation status showed no significant differences in overall resilience or self-assuredness. In subgroup analyses of drive, URiM pre-pandemic MS were found to have significantly higher drive than URiM MS in the pandemic-cohort (p = 0.011). In comparative analyses between URiM and non-URiM by class, URiM MS scored significantly higher in drive in the pre-pandemic cohort (6.07 ± 1.00 vs. 5.59 ± 0.97, p = 0.007), whereas no significant difference was found in the pandemic-cohort (Table 3).

Table 2.
Differences in resilience, self-assuredness, and drive: a. in the overall cohorts and b. in the demographic subcategories. c: Likelihood of agreeing with the open-response questions between the CO23 and CO24. Mann–Whitney U tests were performed in cohort comparisons (with z corresponding to effect size), and UNIANOVA was performed in demographics subcategory comparisons. UNIANOVA values are represented as mean (SD), except for p values. Statistically significant p values are marked with an asterisk.

Table 3.
Self-assuredness and drive in UriM vs. non-UriM students in the CO23 and CO24. Mann–Whitney U tests were performed, and effect size (z) and p-values are reported. Statistically significant p values are marked with an asterisk.
Three school-specific questions were analyzed for agreement between the two entering classes. There were no significant differences in responses to the questions about having tools to maintain resilience and mental health (p = 0.395; Table 2) or whether resilience is a skill that can be taught (p = 0.438). However, pandemic-cohort MS were significantly more likely than pre-pandemic MS to agree that it would be beneficial to have open peer discussions about the emotional challenges of medical school (p = 0.014).
The relationship of overall resilience, self-assuredness, and drive with other factors was further analyzed. Drive was statistically positively correlated with the multiple mini-interview score (p = 0.020) and statistically negatively correlated with the MCAT score. There was no significant relationship between any of the resilience measures and Casper.
3.2. Qualitative Analysis
Of 181 survey respondents in the pandemic cohort, 157 (86.7%) responded to the open-response question regarding how the pandemic changed their attitude toward becoming a physician or raised new concerns about entering the healthcare workforce. Responses comprised five categories: (1) indifference, (2) attitude unchanged with acknowledgment of how the pandemic has changed the field, (3) increased fear or anxiety due to the pandemic, (4) more motivation, and (5) more motivation with apprehension about the field (Appendix B.2).
While the pandemic had varying impacts on each student’s attitude toward becoming a physician, nearly half (45.9%, 72/157) reported being more motivated, with or without apprehension. Specifically, of all respondents, 30.6% (48/157) expressed increased motivation without caveat, and 15.3% (24/157) indicated more motivation in addition to apprehension. While 22.3% (35/157) stated the pandemic led to increased anxiety and fear toward entering medicine, 24.2% (38/157) noted an indifference toward the pandemic, and 7.6% (12/157) reported their attitude was unchanged.
Those expressing increased motivation without caveat discussed excitement around enacting positive change in medicine and a sense of duty to combat challenges presented by the pandemic. One respondent encapsulated this experience:
“No, it has strengthened my desire to be a part of emergent solutions to new and long-standing problems in healthcare” (R150).
Those who expressed motivation with apprehension wrote about their sense of duty in taking on major health crises. However, they also expressed uncertainty regarding their self-efficacy in taking on the challenges presented by the pandemic. The students who showed increased anxiety and fear cited new concerns about the future of the field, while those with unchanged attitudes believed the pandemic would have lasting effects on the medical field without personally affecting them. The students expressing indifference toward the pandemic clarified in open responses that they did not feel it would have long-lasting effects on the medical field.
4. Discussion
This is the first study to measure the resilience of incoming MS before and during a pandemic and to report differences in the drive of URiM students between cohorts. While the overall resilience of incoming MS was not significantly different across cohorts, we observed significantly higher drive in the pre-pandemic cohort URiM students compared to non-URiM students; we did not observe the same trend in the pandemic cohort. The loss of this trend has led us to hypothesize that the drive of URiM students was disproportionately affected during the pandemic and accompanying racial injustices. Studies have explored the relationship between peer support of URiM in medical school, arguing that a lack of peer support contributes to feelings of isolation in URiM MS [38]. Furthermore, studies have also shown that among URiM MS, discussion of social justice and community are impactful for URiM MS [39]. When comparing the school-specific survey responses, pandemic students were significantly more likely to believe they would benefit from open discussions with peers about the emotional challenges of medical school. In addition, despite the rising anxiety of general and healthcare professional populations during COVID-19 [40,41], nearly half of the pandemic-cohort respondents reported feeling more motivated to enter the healthcare field. Notably, this is the first study to report a positive correlation between drive and MMI score and a negative correlation between drive and MCAT score.
Resilience scores across cohorts were consistent with existing literature that suggests entering MS have high baseline resilience [42]. Studies exploring the pandemic’s impact on student well-being, burnout, or resilience have reported mixed results [4,43]. One study using the RS-14 scale reported lower MS resilience during the pandemic [16]. It is important to note that our research surveyed two separate student cohorts before starting medical school, so the results do not reflect the lived experience of students attending medical school during the pandemic.
One longitudinal study examined U.S. MS resilience before and throughout their first year of medical school using the Brief Resilience Scale; MS’ resilience significantly decreased during the first year [44]. However, this study occurred before the pandemic, and results suggested that attending medical school negatively impacted resilience. Another longitudinal study published in 2021 used the Perceived Medical School Stress Instrument (PMSS) to evaluate German MS and reported that perceived stress significantly increased during the first two years [45]. Our findings, in conjunction with current literature, suggest that further research is needed to determine what factors impact students’ resilience during medical school. Initiatives for promoting MS’ resilience and decreasing stress have improved MS and resident well-being in a few settings [17,46,47]. The NYMC Resiliency Curriculum aims to improve MS’ resilience [48,49]. Future work will examine the efficacy of this curriculum and its impact on MS’ resilience.
In this study, we also examined demographic subgroups within each cohort and found no significant difference in resilience based on sex. However, other studies have demonstrated increased psychological distress in female MS, with resilience being inversely proportional to psychological distress and decreased mental health [50,51]. Disproportionately poor mental health in university female students has been demonstrated both before [52] and during the pandemic [53,54,55,56]. In addition, our study found no difference in the overall resilience of SED students between cohorts. However, studies of university students have shown that SED status was associated with decreased wellness before and during the pandemic [51,52]. Further research is needed to explore how medical school may impact female and SED students’ resilience and wellness.
When comparing the school-specific survey responses of both classes, pandemic-cohort MS expressed an increased desire for open discussions with peers about the emotional challenges of medical school. We propose that several factors may have contributed. Firstly, incoming students in August 2020 likely felt particularly isolated as they moved to a new community during a quarantine. Even before the pandemic, studies have shown that MS suffer from feelings of isolation and loneliness, which can contribute to distress [57,58]. During the pandemic, one study reported that 58.8% of MS respondents reported experiencing social isolation; students expressed that quarantine contributed to missing interactions with peers and teachers [59]. Prior to the pandemic, researchers reported that creating a peer belonging program significantly decreased social isolation scores in MS [60]. Given that quarantining and medical school are both independently associated with feelings of isolation, MS who matriculated during a quarantine were likely feeling especially isolated and looking for opportunities to have discussions with peers. In fact, among the MS who submitted qualitative answers, a recurrent theme was that students felt a desire to have their “feelings (of anxiety and isolation) validated in ‘student led discussions’” or some form of support groups that fostered connections between students. Consequently, stakeholders increased peer-to-peer discussion opportunities available remotely and on campus.
In our study, pre-pandemic URiM students entered medical school with higher drive than their classmates. In the class entering during the pandemic, however, no differences in drive were observed between URiM and non-URiM students. While we cannot make a direct comparison as they represent different cohorts, this finding is compelling given the escalation of racial injustices in the US in 2020, which drew attention to the impact of systemic oppression and racism on URiM students and physicians [61,62,63]. Pre-pandemic, URiM MS were at greater risk of depression due to poor diversity and inclusion climates, alienation, and lack of peer and faculty support [62,63,64,65,66]. Another pre-pandemic study demonstrated that URiM students felt that their race and ethnicity had negatively affected their medical school experience (11% vs. 2%; p < 0.001) [34]. The barriers URiM students face in medical school were intensified by the events of 2020, which may have impacted differences in drive in the incoming URiM pandemic cohort.
The MMI score’s positive correlation with drive suggests that the MMI score is a useful admission tool to assess drive, one of the important subcomponents of resiliency, whereas the MCAT (which demonstrated a negative correlation with drive) is not. This further bolsters the importance of using the MMI as part of a holistic approach to admissions by identifying candidates who are more likely to exhibit strong drive.
Surprisingly, in our study, nearly half of the incoming CO24 reported feeling more motivated to enter the healthcare field. Qualitative analysis revealed that students felt a strong obligation to become physicians to positively impact others. This is mirrored by another recent study [67], which found that most pre-med student participants were more motivated to pursue medicine in the face of the pandemic. Similarly, MS volunteers during COVID-19 reported that their motivation to volunteer stemmed from a greater sense of duty [68].
While many students in our study felt more motivated to pursue medicine, some (22.3%; 35/157) reported feeling hesitant. This subgroup cited various factors, including feelings of stress and dangers related to virus exposure. Another major theme involved fear surrounding the apparent public distrust of the healthcare field, specifically referring to political movements such as “anti-vaccine” and general “anti-science” mentalities. To our knowledge, no studies have examined how these movements have impacted MS or healthcare workers.
While the pandemic and the period of racial unrest during this time were unusual circumstances, we believe this study can be viewed as a model for potential consequences during a time when there are limited opportunities for peer support. Studies have shown that a lack of peer support contributes to feelings of isolation [39,69]. This type of isolation is not uncommon in the medical field; many studies demonstrate that among physicians who experience burnout, peer support is an integral part of improving mental health [70,71,72]. Furthermore, many URiM MS value discussions of social injustice; hence, it is imperative to endeavor to communicate support for our colleagues in the medical profession [38,39]. As such, while the pandemic may fade in relevance in peoples’ minds, we hope to learn from this period to further bolster our understanding of mental health and resilience during a time of decreased peer support and racial injustice.
This study has several limitations. First, our study cohorts are not directly comparable as they were distinct incoming classes. In addition, each cohort’s resilience was not measured over time, thereby limiting the scope of the study to resilience upon matriculation. Students were not obligated to complete the free-response questions, creating a potential bias towards students with stronger feelings. Finally, findings in the analysis of stratified subgroups are limited by the sample size and single institution methodology.
5. Conclusions
Although no significant difference was found between the overall resilience of incoming MS cohorts before and during the pandemic, URiM students’ drive was significantly higher than non-URiM MS in the pre-pandemic-cohort. No such difference was found in the pandemic-cohort. Furthermore, pandemic MS demonstrated an increased desire for open discussions with peers regarding the emotional challenges of medical school and reported feeling an increased motivation to practice medicine. Notably, the MMI score’s positive correlation with drive, alongside the MCAT’s negative correlation with drive, further bolsters the importance of using the MMI as part of a holistic approach to admissions.
Future work includes studying whether the resilience of each cohort changes during medical school and whether the NYMC resilience curriculum improves student resilience and overall well-being. Additional studies should examine how current events impact student resilience, which could support the targeted development of support resources. Finally, multi-institutional studies are needed to analyze trends in larger student populations to reduce institutional and geographic bias and improve external validity.
Author Contributions
The contributions of this work are as follows: conceptualization was performed by K.H.P., R.Y., C.B., and D.P.A. Methodology was created by K.H.P., Y.M., and C.B. No software was developed for this work as all data was analyzed in “R.” Formal analysis was performed by K.K.P., K.H.P., Y.M., and C.B. The investigation was performed by Y.M. and C.B. Data curation was performed by Y.M. and K.H.P. Writing original draft presentation and writing review and editing were performed by K.H.P., Y.M., R.S., C.B., K.K.P., and D.P.A. Visualization was completed by Y.M. and C.B. Project supervision, administration, and funding acquisition were performed by K.H.P. All authors have read and agreed to the published version of the manuscript.
Funding
The New York Medical College Student Senate funded the use of the RS-14 survey for research purposes in association with the NYMC Resiliency Curriculum.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of New York Medical College (protocol code 14107, approved 16 July 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study after IRB approval. Those who responded to the survey in 2019 were contacted by email three times and given the opportunity to opt out.
Data Availability Statement
Dataset available on request from the authors.
Acknowledgments
We are grateful to the creators of the RS-14 and acknowledge the New York Medical College Student Senate for funding the use of RS-14 for resiliency student research. We are especially grateful to Kate Morant and Jessica Palmer for their advocacy in establishing a resiliency curriculum at NYMC. We appreciate the work Donald Risucci performed to support this study.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A
Appendix A.1
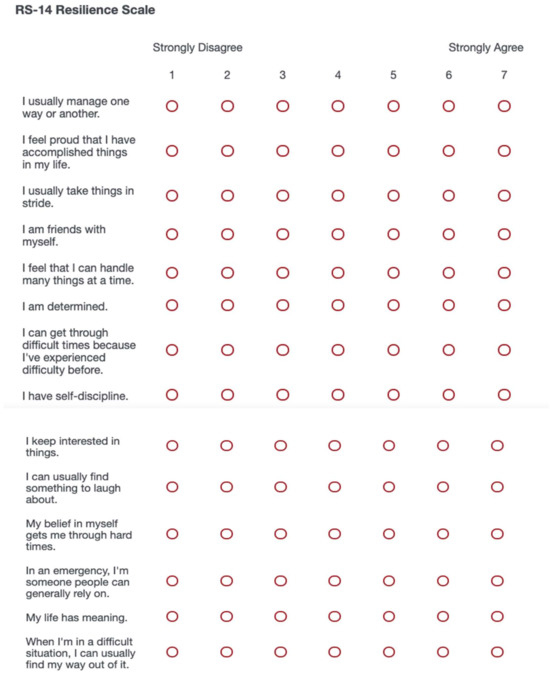
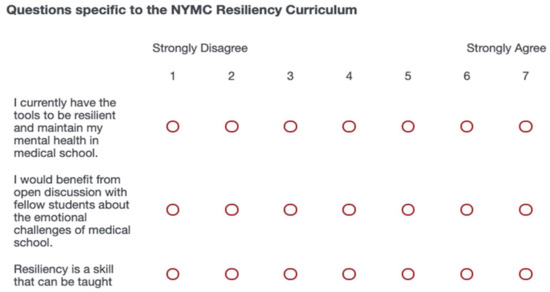
Figure A1.
Survey Administered to the CO23.
Appendix A.2
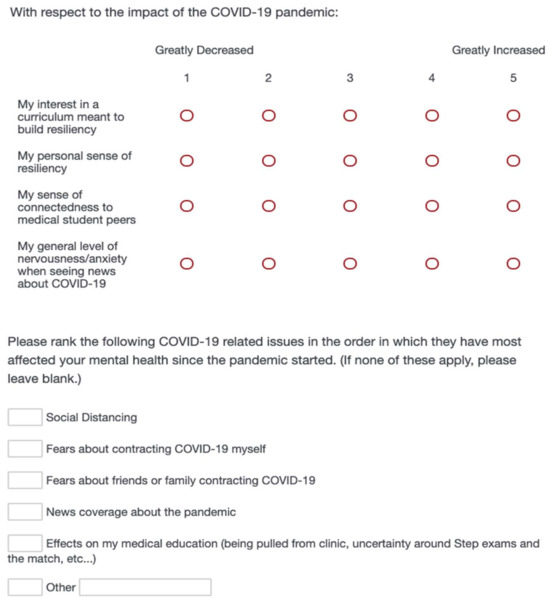
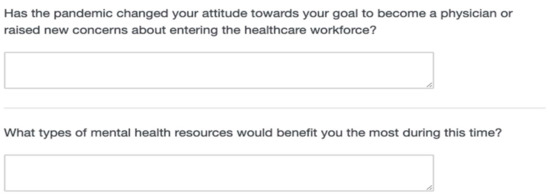
Figure A2.
COVID- Related Questions Added to the Questionnaire above and Administered to the CO24.
Appendix B
Appendix B.1
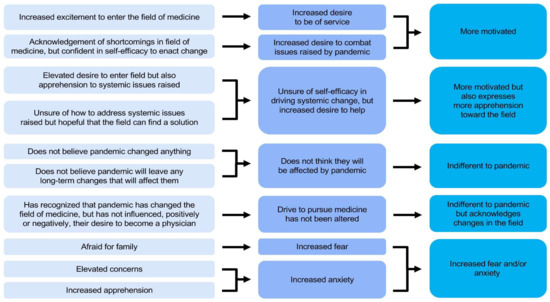
Figure A3.
Open Coding Was Used to Analyze Responses to: “Has the Pandemic Changed Your Attitude towards Your Goal to Become a Physician or Raised New Concerns about Entering the Healthcare Workforce?”.
Appendix B.2

Table A1.
Criteria Used to Place Open Responses in Each Response Category.
Table A1.
Criteria Used to Place Open Responses in Each Response Category.
| Response Category | Criteria for Placement |
|---|---|
| Indifferent | The pandemic has not influenced participants’ opinions about entering the medical field. |
| Indifferent with caveat | The pandemic has not influenced participants’ personal opinions about entering the medical field, but acknowledges the change brought about by the pandemic. |
| Increased fear and/or anxiety | The pandemic has heightened the participants’ fear and/or anxiety about entering the medical field. |
| More motivated | The pandemic has increased the participants’ motivation to enter the medical field, often citing a desire to address issues the pandemic has highlighted or caused within the medical field. |
| More motivated with caveat | The pandemic has increased the participants’ motivation to enter the medical field, but participants are unsure of their capacity to enact positive change. |
References
- Zhu, Z.; Xu, S.; Wang, H.; Liu, Z.; Wu, J.; Li, G.; Miao, J.; Zhang, C.; Yang, Y.; Sun, W.; et al. COVID-19 in Wuhan: Sociodemographic characteristics and hospital support measures associated with the immediate psychological impact on healthcare workers. eClinicalMedicine 2020, 24, 100443. [Google Scholar] [CrossRef]
- Rolak, S.; Keefe, A.M.; Davidson, E.L.; Aryal, P.; Parajuli, S. Impacts and challenges of United States medical students during the COVID-19 pandemic. World J. Clin. Cases 2020, 8, 3136–3141. [Google Scholar] [CrossRef] [PubMed]
- O’Byrne, L.; Gavin, B.; McNicholas, F. Medical students and COVID-19: The need for pandemic preparedness. J. Med. Ethics 2020, 46, 623–626. [Google Scholar] [CrossRef] [PubMed]
- Zis, P.; Artemiadis, A.; Bargiotas, P.; Nteveros, A.; Hadjigeorgiou, G.M. Medical Studies during the COVID-19 Pandemic: The Impact of Digital Learning on Medical Students’ Burnout and Mental Health. Int. J. Environ. Res. Public Health 2021, 18, 349. [Google Scholar] [CrossRef] [PubMed]
- Yun, J.Y.; Kim, K.H.; Joo, G.J.; Kim, B.N.; Roh, M.S.; Shin, M.S. Changing characteristics of the empathic communication network after empathy-enhancement program for medical students. Sci. Rep. 2018, 8, 15092. [Google Scholar] [CrossRef] [PubMed]
- Dyrbye, L.N.; Thomas, M.R.; Massie, F.S.; Power, D.V.; Eacker, A.; Harper, W.; Durning, S.; Moutier, C.; Szydlo, D.W.; Novotny, P.J.; et al. Burnout and suicidal ideation among U.S. medical students. Ann. Intern. Med. 2008, 149, 334–341. [Google Scholar] [CrossRef]
- Zisook, S.; Young, I.; Doran, N.; Downs, N.; Hadley, A.; Kirby, B.; McGuire, T.; Moutier, C.; Norcross, W.; Tiamson-Kassab, M. Suicidal Ideation Among Students and Physicians at a U.S. Medical School: A Healer Education, Assessment and Referral (HEAR) Program Report. OMEGA—J. Death Dying 2016, 74, 35–61. [Google Scholar]
- Mata, D.A.; Ramos, M.A.; Bansal, N.; Khan, R.; Guille, C.; Di Angelantonio, E.; Sen, S. Prevalence of Depression and Depressive Symptoms Among Resident Physicians: A Systematic Review and Meta-analysis. JAMA 2015, 314, 2373–2383. [Google Scholar] [CrossRef]
- Gold, K.J.; Sen, A.; Schwenk, T.L. Details on suicide among US physicians: Data from the National Violent Death Reporting System. Gen. Hosp. Psychiatry 2013, 35, 45–49. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Boone, S.; Tan, L.; Dyrbye, L.N.; Sotile, W.; Satele, D.; West, C.P.; Sloan, J.; Oreskovich, M.R. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch. Intern. Med. 2012, 172, 1377–1385. [Google Scholar] [CrossRef]
- Rothenberger, D.A. Physician Burnout and Well-Being: A Systematic Review and Framework for Action. Dis. Colon. Rectum 2017, 60, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Balch, C.M.; Dyrbye, L.; Bechamps, G.; Russell, T.; Satele, D.; Rummans, T.; Swartz, K.; Novotny, P.J.; Sloan, J.; et al. Special report: Suicidal ideation among American surgeons. Arch. Surg. 2011, 146, 54–62. [Google Scholar] [CrossRef] [PubMed]
- DiMatteo, M.R.; Sherbourne, C.D.; Hays, R.D.; Ordway, L.; Kravitz, R.L.; McGlynn, E.A.; Kaplan, S.; Rogers, W.H. Physicians’ characteristics influence patients’ adherence to medical treatment: Results from the Medical Outcomes Study. Health Psychol. 1993, 12, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Linn, L.S.; Brook, R.H.; Clark, V.A.; Davies, A.R.; Fink, A.; Kosecoff, J. Physician and patient satisfaction as factors related to the organization of internal medicine group practices. Med. Care 1985, 23, 1171–1178. [Google Scholar] [CrossRef] [PubMed]
- Grol, R.; Mokkink, H.; Smits, A.; van Eijk, J.; Beek, M.; Mesker, P.; Mesker-Niesten, J. Work satisfaction of general practitioners and the quality of patient care. Fam. Pract. 1985, 2, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Forycka, J.; Pawlowicz-Szlarska, E.; Burczynska, A.; Cegielska, N.; Harendarz, K.; Nowicki, M. Polish medical students facing the pandemic-Assessment of resilience, well-being and burnout in the COVID-19 era. PLoS ONE 2022, 17, e0261652. [Google Scholar] [CrossRef] [PubMed]
- Howe, A.; Smajdor, A.; Stockl, A. Towards an understanding of resilience and its relevance to medical training. Med. Educ. 2012, 46, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Neufeld, A.; Malin, G. Exploring the relationship between medical student basic psychological need satisfaction, resilience, and well-being: A quantitative study. BMC Med. Educ. 2019, 19, 405. [Google Scholar] [CrossRef]
- Abram, M.D.; Jacobowitz, W. Resilience and burnout in healthcare students and inpatient psychiatric nurses: A between-groups study of two populations. Arch. Psychiatr. Nurs. 2021, 35, 1–8. [Google Scholar] [CrossRef]
- Edmonds, V.S.; Chatterjee, K.; Girardo, M.E.; Butterfield, R.J., 3rd; Stonnington, C.M. Evaluation of a Novel Wellness Curriculum on Medical Student Wellbeing and Engagement Demonstrates a Need for Student-Driven Wellness Programming. Teach. Learn. Med. 2023, 35, 52–64. [Google Scholar] [CrossRef]
- Snapp, C.; Bassett, C.; Baldwin, A.; Hill, J.R.; DeBusk, R. Peer-Assisted Learning in Undergraduate Medical Education for Resilience and Well-being. Med. Sci. Educ. 2023, 33, 5–6. [Google Scholar] [CrossRef]
- Yeager, D.S.; Dweck, C.S. Mindsets that promote resilience: When students believe that personal characteristics can be developed. Educ. Psychol. 2012, 47, 302–314. [Google Scholar] [CrossRef]
- Zeng, G.; Hou, H.; Peng, K. Effect of Growth Mindset on School Engagement and Psychological Well-Being of Chinese Primary and Middle School Students: The Mediating Role of Resilience. Front. Psychol. 2016, 7, 1873. [Google Scholar] [CrossRef] [PubMed]
- Windle, G.; Bennett, K.M.; Noyes, J. A methodological review of resilience measurement scales. Health Qual. Life Outcomes 2011, 9, 8. [Google Scholar] [CrossRef] [PubMed]
- Wagnild, G.; Young, H.M. Resilience among older women. Image J. Nurs. Sch. 1990, 22, 252–255. [Google Scholar] [CrossRef]
- Wagnild, G.M.; Young, H.M. Development and psychometric evaluation of the Resilience Scale. J. Nurs. Meas. 1993, 1, 165–178. [Google Scholar]
- Wagnild, G. A review of the Resilience Scale. J. Nurs. Meas. 2009, 17, 105–113. [Google Scholar] [CrossRef]
- Tempski, P.; Santos, I.S.; Mayer, F.B.; Enns, S.C.; Perotta, B.; Paro, H.B.; Gannam, S.; Peleias, M.; Garcia, V.L.; Baldassin, S.; et al. Relationship among Medical Student Resilience, Educational Environment and Quality of Life. PLoS ONE 2015, 10, e0131535. [Google Scholar] [CrossRef]
- Oliveira, A.C.P.M.; Machado, A.P.G.M.; Aranha, R.N.M. Identification of factors associated with resilience in medical students through a cross-sectional census. BMJ Open 2017, 7, e017189. [Google Scholar] [CrossRef]
- Lin, Y.K.; Lin, C.D.; Lin, B.Y.; Chen, D.Y. Medical students’ resilience: A protective role on stress and quality of life in clerkship. BMC Med. Educ. 2019, 19, 473. [Google Scholar] [CrossRef]
- Barnett, J.E.; Baker, E.K.; Elman, N.S.; Schoener, G.R. In pursuit of wellness: The self-care imperative. Prof. Psychol. Res. Pract. 2007, 38, 603–612. [Google Scholar] [CrossRef]
- Weine, S.; Kohrt, B.A.; Collins, P.Y.; Cooper, J.; Lewis-Fernandez, R.; Okpaku, S.; Wainberg, M.L. Justice for George Floyd and a reckoning for global mental health. Glob. Ment. Health 2020, 7, e22. [Google Scholar] [CrossRef] [PubMed]
- O’Marr, J.M.; Chan, S.M.; Crawford, L.; Wong, A.H.; Samuels, E.; Boatright, D. Perceptions on Burnout and the Medical School Learning Environment of Medical Students Who Are Underrepresented in Medicine. JAMA Netw. Open 2022, 5, e220115. [Google Scholar] [CrossRef] [PubMed]
- Dyrbye, L.N.; Thomas, M.R.; Eacker, A.; Harper, W.; Massie, F.S., Jr.; Power, D.V.; Huschka, M.; Novotny, P.J.; Sloan, J.A.; Shanafelt, T.D. Race, ethnicity, and medical student well-being in the United States. Arch. Intern. Med. 2007, 167, 2103–2109. [Google Scholar] [CrossRef] [PubMed]
- Wagnild, G.M. The Resilience Scale User’s Guide; Resilience Center: Worden, MT, USA, 2016. [Google Scholar]
- Burgis-Kasthala, S.; Elmitt, N.; Smyth, L.; Moore, M. Predicting future performance in medical students. A longitudinal study examining the effects of resilience on low and higher performing students. Med. Teach. 2019, 41, 1184–1191. [Google Scholar] [CrossRef] [PubMed]
- Elo, S.; Kyngas, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Morrison, N.; Machado, M.; Blackburn, C. Student perspectives on barriers to performance for black and minority ethnic graduate-entry medical students: A qualitative study in a West Midlands medical school. BMJ Open 2019, 9, e032493. [Google Scholar] [CrossRef]
- Bazargan-Hejazi, S.; Negrete Manriquez, J.A.; McDermoth-Grimes, M.; Parra, E.A.; Prothrow-Stith, D. Underrepresented in medicine students’ perspectives on impactful medical education. BMC Med. Educ. 2022, 22, 904. [Google Scholar] [CrossRef]
- Bauerle, A.; Teufel, M.; Musche, V.; Weismuller, B.; Kohler, H.; Hetkamp, M.; Dorrie, N.; Schweda, A.; Skoda, E.M. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: A cross-sectional study in Germany. J. Public Health 2020, 42, 672–678. [Google Scholar] [CrossRef]
- Myran, D.T.; Cantor, N.; Rhodes, E.; Pugliese, M.; Hensel, J.; Taljaard, M.; Talarico, R.; Garg, A.X.; McArthur, E.; Liu, C.W.; et al. Physician Health Care Visits for Mental Health and Substance Use During the COVID-19 Pandemic in Ontario, Canada. JAMA Netw. Open 2022, 5, e2143160. [Google Scholar] [CrossRef]
- Brazeau, C.M.; Shanafelt, T.; Durning, S.J.; Massie, F.S.; Eacker, A.; Moutier, C.; Satele, D.V.; Sloan, J.A.; Dyrbye, L.N. Distress among matriculating medical students relative to the general population. Acad. Med. 2014, 89, 1520–1525. [Google Scholar] [CrossRef] [PubMed]
- Lyons, Z.; Wilcox, H.; Leung, L.; Dearsley, O. COVID-19 and the mental well-being of Australian medical students: Impact, concerns and coping strategies used. Australas. Psychiatry 2020, 28, 649–652. [Google Scholar] [CrossRef]
- Jordan, R.K.; Shah, S.S.; Desai, H.; Tripi, J.; Mitchell, A.; Worth, R.G. Variation of stress levels, burnout, and resilience throughout the academic year in first-year medical students. PLoS ONE 2020, 15, e0240667. [Google Scholar] [CrossRef] [PubMed]
- Voltmer, E.; Koslich-Strumann, S.; Voltmer, J.B.; Kotter, T. Stress and behavior patterns throughout medical education—A six year longitudinal study. BMC Med. Educ. 2021, 21, 454. [Google Scholar] [CrossRef] [PubMed]
- Redwood, S.K.; Pollak, M.H. Student-led stress management program for first-year medical students. Teach. Learn. Med. 2007, 19, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Slavin, S.J.; Schindler, D.L.; Chibnall, J.T. Medical student mental health 3.0: Improving student wellness through curricular changes. Acad. Med. 2014, 89, 573–577. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Yang, R.; Briskin, C.; Alper, D.; Morant, K.; Palmer, J.; Petersen, K.H. Resiliency Among Medical Students and Initial Review of a Student-Run Resiliency Curriculum. In Proceedings of the AMA Research Symposium, Virtual Meeting, 16–19 November 2020. [Google Scholar]
- Kim, H.; Cohen, A.; Evans, K.; Lee, K.R.; Longo, J.L.; McCafferty, J.; Morant, K.; Palmer, J.S.; Zhang, S.; Ludmer, P.; et al. NYMC Resiliency Curriculum. In Proceedings of the The AAMC Annual Meeting: Learn Serve Lead, Phoenix, AZ, USA, 8–12 November 2019. [Google Scholar]
- Bacchi, S.; Licinio, J. Resilience and Psychological Distress in Psychology and Medical Students. Acad. Psychiatry 2017, 41, 185–188. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Sznajder, K.; Cheng, D.; Wang, S.; Cui, C.; Yang, X. Coping Styles for Mediating the Effect of Resilience on Depression Among Medical Students in Web-Based Classes During the COVID-19 Pandemic: Cross-sectional Questionnaire Study. J. Med. Internet Res. 2021, 23, e25259. [Google Scholar] [CrossRef]
- Said, D.; Kypri, K.; Bowman, J. Risk factors for mental disorder among university students in Australia: Findings from a web-based cross-sectional survey. Soc. Psychiatry Psychiatr. Epidemiol. 2013, 48, 935–944. [Google Scholar] [CrossRef]
- Wathelet, M.; Duhem, S.; Vaiva, G.; Baubet, T.; Habran, E.; Veerapa, E.; Debien, C.; Molenda, S.; Horn, M.; Grandgenevre, P.; et al. Factors Associated With Mental Health Disorders Among University Students in France Confined During the COVID-19 Pandemic. JAMA Netw. Open 2020, 3, e2025591. [Google Scholar] [CrossRef]
- Ehmke, M.D.; Katare, B.; Kiesel, K.; Bergtold, J.S.; Penn, J.M.; Boys, K.A. U.S. agricultural university students’ mental well-being and resilience during the first wave of COVID-19: Discordant expectations and experiences across genders. Appl. Econ. Perspect. Policy 2022, 44, 129–161. [Google Scholar] [CrossRef] [PubMed]
- Amendola, S.; von Wyl, A.; Volken, T.; Zysset, A.; Huber, M.; Dratva, J. A Longitudinal Study on Generalized Anxiety Among University Students During the First Wave of the COVID-19 Pandemic in Switzerland. Front. Psychol. 2021, 12, 643171. [Google Scholar] [CrossRef] [PubMed]
- Wathelet, M.; Vincent, C.; Fovet, T.; Notredame, C.E.; Habran, E.; Martignene, N.; Baubet, T.; Vaiva, G.; D’Hondt, F. Evolution in French University Students’ Mental Health One Month After the First COVID-19 Related Quarantine: Results From the COSAMe Survey. Front. Psychiatry 2022, 13, 868369. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.; Hasan, S.; Malik, S.; Sreeramareddy, C.T. Perceived stress, sources and severity of stress among medical undergraduates in a Pakistani medical school. BMC Med. Educ. 2010, 10, 2. [Google Scholar] [CrossRef] [PubMed]
- Langness, S.; Rajapuram, N.; Marshall, M.; Rahman, A.S.; Sammann, A. Risk factors associated with student distress in medical school: Associations with faculty support and availability of wellbeing resources. PLoS ONE 2022, 17, e0265869. [Google Scholar] [CrossRef] [PubMed]
- Wurth, S.; Sader, J.; Cerutti, B.; Broers, B.; Bajwa, N.M.; Carballo, S.; Escher, M.; Galetto-Lacour, A.; Grosgurin, O.; Lavallard, V.; et al. Medical students’ perceptions and coping strategies during the first wave of the COVID-19 pandemic: Studies, clinical implication, and professional identity. BMC Med. Educ. 2021, 21, 620. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.M.; Taylor, D.L.; Fitzgerald, A.A.; Kuo, C.C.; Graves, K.D. Build & Belong: A Peer-Based Intervention to Reduce Medical Student Social Isolation. Teach. Learn. Med. 2022, 34, 504–513. [Google Scholar] [CrossRef] [PubMed]
- Lucey, C.R.; Saguil, A. The Consequences of Structural Racism on MCAT Scores and Medical School Admissions: The Past Is Prologue. Acad. Med. 2020, 95, 351–356. [Google Scholar] [CrossRef]
- Nguemeni Tiako, M.J.; Ray, V.; South, E.C. Medical Schools as Racialized Organizations: How Race-Neutral Structures Sustain Racial Inequality in Medical Education-a Narrative Review. J. Gen. Intern. Med. 2022, 37, 2259–2266. [Google Scholar] [CrossRef]
- Cyrus, K.D. A piece of my mind: Medical Education and the Minority Tax. JAMA 2017, 317, 1833–1834. [Google Scholar] [CrossRef]
- Hardeman, R.R.; Przedworski, J.M.; Burke, S.; Burgess, D.J.; Perry, S.; Phelan, S.; Dovidio, J.F.; van Ryn, M. Association Between Perceived Medical School Diversity Climate and Change in Depressive Symptoms Among Medical Students: A Report from the Medical Student CHANGE Study. J. Natl. Med. Assoc. 2016, 108, 225–235. [Google Scholar] [CrossRef] [PubMed]
- Hardeman, R.R.; Przedworski, J.M.; Burke, S.E.; Burgess, D.J.; Phelan, S.M.; Dovidio, J.F.; Nelson, D.; Rockwood, T.; van Ryn, M. Mental Well-Being in First Year Medical Students: A Comparison by Race and Gender: A Report from the Medical Student CHANGE Study. J. Racial Ethn. Health Disparities 2015, 2, 403–413. [Google Scholar] [CrossRef] [PubMed]
- Garcia, L.C.; Shanafelt, T.D.; West, C.P.; Sinsky, C.A.; Trockel, M.T.; Nedelec, L.; Maldonado, Y.A.; Tutty, M.; Dyrbye, L.N.; Fassiotto, M. Burnout, Depression, Career Satisfaction, and Work-Life Integration by Physician Race/Ethnicity. JAMA Netw. Open 2020, 3, e2012762. [Google Scholar] [CrossRef] [PubMed]
- Leigh, J.K. “What are you signing up for?”: Pre-medical students’ perception of physicians’ risk and responsibility during COVID-19. Soc. Sci. Med. 2021, 287, 114320. [Google Scholar] [CrossRef] [PubMed]
- Tempski, P.; Arantes-Costa, F.M.; Kobayasi, R.; Siqueira, M.A.M.; Torsani, M.B.; Amaro, B.; Nascimento, M.; Siqueira, S.L.; Santos, I.S.; Martins, M.A. Medical students’ perceptions and motivations during the COVID-19 pandemic. PLoS ONE 2021, 16, e0248627. [Google Scholar] [CrossRef] [PubMed]
- Abrams, M.P.; Salzman, J.; Espina Rey, A.; Daly, K. Impact of Providing Peer Support on Medical Students’ Empathy, Self-Efficacy, and Mental Health Stigma. Int. J. Environ. Res. Public Health 2022, 19, 5135. [Google Scholar] [CrossRef]
- Ortega, M.V.; Hidrue, M.K.; Lehrhoff, S.R.; Ellis, D.B.; Sisodia, R.C.; Curry, W.T.; Del Carmen, M.G.; Wasfy, J.H. Patterns in Physician Burnout in a Stable-Linked Cohort. JAMA Netw. Open 2023, 6, e2336745. [Google Scholar] [CrossRef] [PubMed]
- Horne, I.M.T.; Veggeland, F.; Bååthe, F.; Drewes, C.; Rø, K.I. Understanding peer support: A qualitative interview study of doctors one year after seeking support. BMC Health Serv. Res. 2023, 23, 324. [Google Scholar] [CrossRef]
- Bruce, S.M.; Conaglen, H.M.; Conaglen, J.V. Burnout in physicians: A case for peer-support. Intern. Med. J. 2005, 35, 272–278. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).