Abstract
Medical schools often rely on clinicians to provide guest lectures in foundational science courses. These guest lecturers may teach only once or sporadically in the undergraduate curriculum, which brings about several challenges that can impact their effectiveness. This guide, drawn from evidence-based teaching principles, medical student feedback, the authors’ training in educational and cognitive psychology, and experience as a clinical teacher, is designed to support clinical guest lecturers in meeting the educational standards and expectations for teaching in the preclinical setting as well as give insight into the needs of foundational science course directors and students.
1. Introduction
Medical schools often rely on clinicians to provide guest lectures in foundational science courses. This trend has increased in recent years as medical schools have modified their preclinical curricula to enhance clinical relevance of foundational science content that is taught and to introduce students to clinical experience and concepts earlier in their training. Clinician guest lecturers may teach only once or sporadically in the undergraduate curriculum, which brings about several challenges. First, many clinicians, who may have extensive experience teaching individual or small groups of learners at the bedside, often have limited experience or training in giving a lecture to a large audience. They may also be unaware of how their lecture fits into the overall course, lack familiarity with the preclinical environment, and lack connection to the students. However, the expectation for all instructors, regardless of the frequency of teaching or training, is that they need to be informed of course expectations and their specific role in both teaching and assessment [1]. This guide, drawn from evidence-based teaching principles, medical student feedback, the authors’ training in educational and cognitive psychology, and experience as a clinical teacher, is addressed to clinical guest lecturers and designed to support them in meeting the educational standards and expectations for teaching in the preclinical setting as well as give insight into the needs of foundational science course directors and students.
2. Initial Questions to Ask before Preparing Your Lecture
The invitation for you to lecture is surely a recognition of your expertise and accomplishments. However, the landscape in which lectures are offered in medical education has changed drastically in recent years [2,3]. It is essential to have a shared understanding of why you were invited. In some instances, lectures remain opportunities for you to share elements of your expertise with a receptive audience that has done little to prepare for your presentation and who may require definitions of even the most basic terms. In other cases, you may be expected to guide students who already possess extensive and relevant prior knowledge of your topic and who would benefit from challenging opportunities to apply ideas and practices intrinsic to your field. Still further, if you are a clinician educator who teaches students in the clinical years (i.e., clerkship director or faculty preceptor), you can use this opportunity to highlight essential concepts or ways of thinking that you hope students will achieve before they come to you as a clerk.
To achieve a shared understanding with the course director, ask questions about the course content, lecture style, and student experiences (Figure 1). Contemporary medical schools seek not only to foster student content knowledge but also seek to promote students’ ability to guide their own learning [4]. It undermines that message when lecturers in courses appear unaware of what has already been addressed and to what degree students are responsible for their own learning. Reviewing the course syllabus will help you gain a sense of the topics that have come before your lecture and topics that will follow your session. As the content expert, reviewing the syllabus will enhance your ability to make meaningful connections between your content and the course overall in ways in which the course director may not be able to do. Linking students’ prior experiences with the information you bring can also enhance student engagement and promote learning.
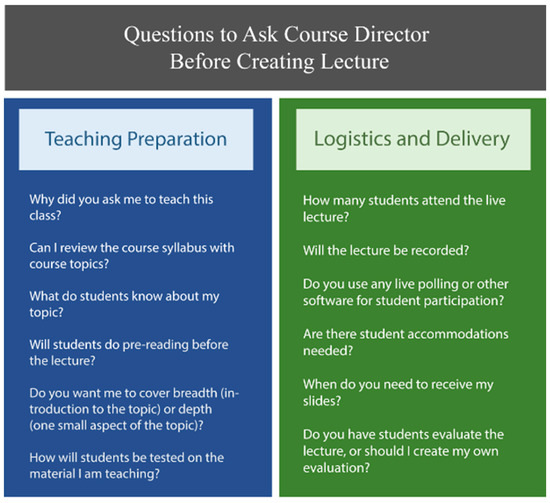
Figure 1.
Preparing for your lecture.
Learning about the course may also involve gaining an understanding of the way content is delivered compared to your personal teaching style. Evaluate where you tend to situate your teaching on the spectrum of student-centered to teacher-centered practices [5]. Is it important for you to engage with students in discussion of material and for you to have some sense of how well students are grasping the content in your lectures? It is intuitive that you will be most effective when you feel you are drawing upon what has worked for you in the past or, if you have little experience, what lecture styles have benefited you in the past. Yet at the same time, it is critical that you plan your lecture with an awareness of the modalities used in the course in which you have been invited to participate and in the curriculum as a whole.
3. Developing the Content and Structure of Your Lecture to Promote Student Learning
To plan a focused and organized lecture, begin with what you hope students will learn or be able to do following your session, and create corresponding learning objectives. Figure 2 summarizes some key ideas to review as you write your learning objectives and organize your lecture content around those objectives. Effective learning objectives follow the mnemonic SMART—specific, measurable, attainable, relevant, and time-bound [6] and use action verbs that try to capture higher levels of Bloom’s cognitive taxonomy. For instance, the most helpful learning objectives are specific enough that students can determine what is important content from the lecture, versus what is secondary or additional information, and objectives should be measured by an assessment item. Students often study for exams using the learning objectives given and find it helpful when lecturers label slides in the lower corner alerting them that a particular objective is being met on that slide or slides. After creating the learning objectives for your lecture, confer with the course director to determine if the objectives are at the appropriate level for the learner and fill the educational need of the course before you create the rest of your lecture content.
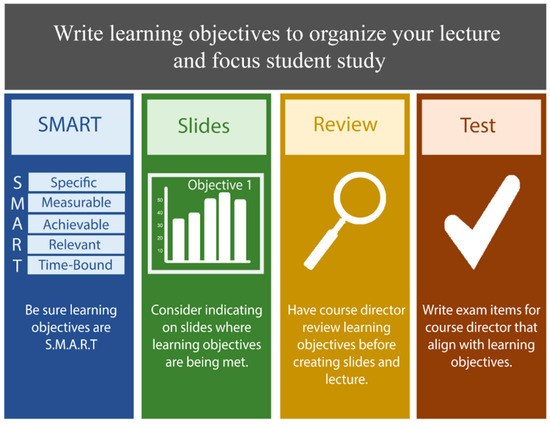
Figure 2.
Writing learning objectives for your lecture.
As an expert in your domain, you may be asked to teach on a topic that could be an entire course itself. However, a learner-centered lecture will focus on key concepts. Research suggests that the denser a lecture, the less students retain basic information and lectures are more effective when they are limited to essential points [7]. To help narrow your content, begin with creating an outline of two to four important points and develop a lecture that is centered around explaining and teaching those points as deeply as possible. Pre- or post-lecture resources to supplement content may also help to reduce students’ cognitive load during a lecture [8]. In addition, if you are using slides, providing a summary slide after a longer series of slides will help students to consolidate learning and know when you are transitioning to a new topic. Keep in mind that slides may not be necessary in all your lectures; use of a board, handouts, other audiovisual aids, or kinesthetic learning activities may be more helpful than slides depending on the information you are trying to convey.
If you are a new lecturer, you may underestimate the time needed to research, organize, and create a lecture. Even when you have significant expertise, organizing references, choosing effective diagrams, and using best practices to enhance student learning takes time and effort. Some instructors take significantly longer the first time they create a lecture and only after teaching the content several times, are they comfortable with brief updating before the day of the class.
Once you have developed your presentation, evaluate your content on applicable dimensions of diversity (e.g., race, gender identity, mental/physical abilities). Are you including results from studies that include participants from backgrounds that reflect your patient population? If these studies do not exist, it may be helpful to explicitly tell students that they have not yet been conducted or how results from existing studies can or should not be applied to other patient populations. Do the images on your slides show examples of findings on multiple skin tones as relevant for your patient population? Programs like Visual Dx are used in many medical schools to enhance diagnostic accuracy and contain a library of images on multiple skin tones. Figure 3 has additional resources on diversity that may be helpful as you plan your lecture.
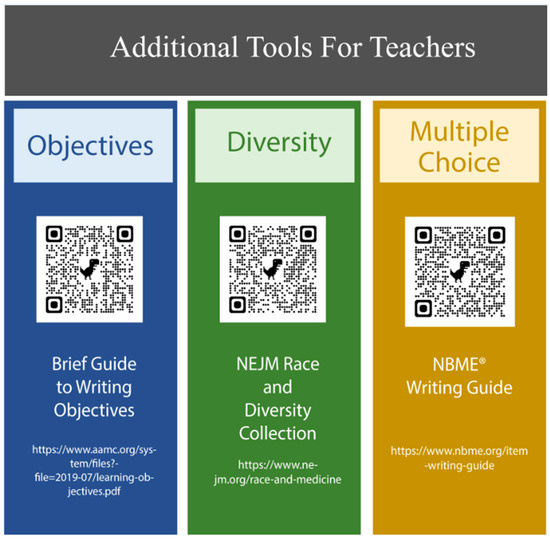
Figure 3.
Additional tools for teachers.
It is particularly helpful for both students and course directors when guest lecturers provide their slides or a handout before the day of the presentation. Students are advised to “preview” lecture content as one strategy of learning before a lecture [9], and having slides early allows for self-regulation of learning preparedness [10]. Consider creating one set of slides for students that does not “give away” answers to any practice problems within your presentation.
Finally, it may be helpful to consult with the course director about whether they would want you to write a few questions to be included in a course exam or help them identify items from a pool of questions that would be relevant to your material. Writing valid exam questions may be difficult for the course director without having delivered the material themselves. Exam items should align with learning objectives to maintain content validity [11]. Therefore, knowing that students will be assessed through multiple-choice items focused on application of knowledge, as opposed to the recall of facts, may influence your lecture objectives. Refer to Figure 3 for a guide to writing effective multiple-choice questions.
4. Delivering and Following Up on the Effectiveness of Your Lecture
On the day you will be teaching, arrive early and plan to stop lecturing early. Whether using a virtual platform or in a physical lecture hall, technology in its many forms may be unreliable. Arriving early allows for time to check if polling features or online questions are working, if there are any mismatches with file types, and to acclimate to any other nuances of the teaching “room”. Beyond mitigating any delays from technological issues, arriving before a lecture begins allows for informal conversations with students and provides a sense of how students typically interact with each other and the course director. Keep a close watch on the time limitations for your lecture and practice with the material so that the last few minutes of class do not entail speeding through 5–7 slides. Planning for slightly less material and more practice problems or discussion of implications at the end will eliminate the frustration for students who may be feverishly taking notes to catch ending concepts. Courses are often stacked in a day as well, so if your lecture continues past the expected time, students may be unable to take the needed break or consolidate any notes before listening to another lecture or going to an additional activity.
Students may have heard a little bit about you from their course director or nothing at all. To break the ice of the first meeting and set the stage for your presentation, begin with a brief introduction of yourself with enough information to establish your credibility and to allow students to understand your context and perspective on the subject matter in which you will be teaching. Your initial depiction of who you are and what you do will help focus student attention, an important first step in memory and learning [12]. Guest lecturers often generate excitement in a course, and students may be motivated to interact with you because of your unique background, research program, or other skill set. Be sure to leave your contact information on a slide for students to follow up with clarifying questions.
Once you have introduced yourself, consider using an attention-grabbing technique such as sharing a personal anecdote, clinical experience, or illustrative case from your practice that you can then use as a springboard to guide the rest of your lecture. During the lecture you can employ skills you may already use in facilitating small groups or teaching at the bedside. There are many benefits of interspersing questions to the audience of a lecture including self-reflection of attitudes, assessment of knowledge on the current topic, reasoning, or problem solving [13]. Choosing the amount and types of questions (e.g., clarifying, recall, application) and planning them at intervals will help maintain student attention and interest (Figure 4).
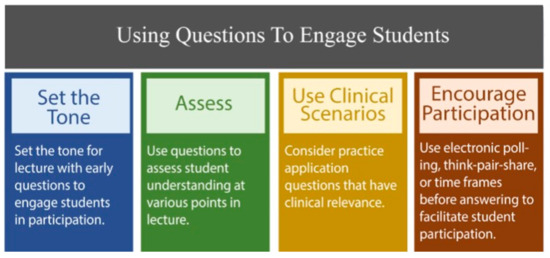
Figure 4.
Using questions to engage students.
Placing questions early in the lecture will help set the tone and signal to students your expectation of their involvement throughout your time together. For example, a thought-provoking question (e.g., How might this recent medical development impact future patient care?) or an ice-breaking question (e.g., What has been the most challenging aspect of learning this course material so far?), indicates to students that you are open and value their interaction. Questions used in the middle or toward the end of the lecture can help students elaborate on ideas, connect new information with prior learning, combine ideas, or restructure knowledge when inconsistencies in their thinking are revealed [14].
Consider implementing specific time intervals before accepting answers to questions posed to allow time for student reflection. Utilize techniques such as asking students to write out their responses, electronic polling, or think-pair-share (students think of their response, discuss with another classmate, and then share with the group) to encourage participation and avoid uncomfortable silences following your questions.
To promote student interaction throughout the lecture, provide encouragement to students when they do participate (e.g., thank you for that answer), do not respond too quickly to the first hand that goes up, and try not to be dismissive when a wrong answer is given (e.g., “that is not correct but can you explain why you think that or how you arrived at that answer?”) to uncover any faulty reasoning processes that other students may share. Be sure to allow time for final clarifying questions or leave students with a question that will keep them thinking even after your lecture is finished. Medical students value teachers who are enthusiastic and open to answering questions [15].
After the conclusion of the lecture, solicit feedback from as many sources as possible. Most courses seek feedback concerning full time instructors; however, for an infrequent lecturer, student feedback may not be collected. If the course in which you are teaching does not already seek student feedback, you could prepare a simple student survey through Google Forms or other survey software to give at the last moments of class. Although student feedback might not represent the sole or most reliable measure of teaching quality, it can highlight areas for improvement that enhance student engagement and perceptions of learning. Suggested evaluative questions may include overall value of the session, clarity of teaching, openness to students, or any other details of your content or delivery. Formal feedback from students or course directors can help improve your teaching and can be saved for promotion documents. To close the loop on your lecture, you can also request that the course director inform you of how any exam items that you wrote or selected performed in their test.
5. Conclusions
Great clinical guest lecturers are vital to medical education and highly sought after to infuse the preclinical learning environment with clinical knowledge and relevant experiences. Because of competing demands in medical education, those who do not teach regularly may not be as skilled in meeting the changing needs in the undergraduate classroom or be used to contemporary teaching style and expectations of the learning environment. These tips are provided to encourage collaboration between the clinical guest lecturer and the course director and to set mutual expectations for success. Similarly, student satisfaction will likely be higher when guest lecturers are informed and prepared to meet student needs. As guest lecturers become more confident and have more teaching experience, the tips can be used as a springboard for deeper learning into teaching techniques.
Author Contributions
Conceptualization, K.M.C., H.R., S.K. and R.L.; writing—original draft preparation, K.M.C., H.R., S.K., and R.L.; writing—review and editing, K.M.C., H.R., S.K. and R.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article.
Acknowledgments
The authors thank James Galt for his help in preparing the figures used in the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Liaison Committee on Medical Education. Functions and Structure of a Medical School: Standards for Accreditation of Medical Education Programs Leading to the MD Degree; Association of American Medical Colleges and American Medical Association: Washington, DC, USA, 2020; Available online: https://lcme.org/publications/ (accessed on 31 May 2023).
- Prober, C.G.; Heath, C. Lecture halls without lectures—A proposal for medical education. N. Engl. J. Med. 2012, 366, 1657–1659. [Google Scholar] [CrossRef] [PubMed]
- Demir, E.A.; Tutuk, O.; Dogan, H.; Egeli, D.; Turner, C. Lecture attendance improves success in medical physiology. Adv. Physiol. Educ. 2017, 41, 599–603. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, D.J.; Englander, R.; Carraccio, C. Developing the master learner: Applying learning theory to the learner, the teacher, and the learning environment. Acad. Med. 2013, 88, 1635–1645. [Google Scholar] [CrossRef] [PubMed]
- Dent, J.; Harden, R.M.; Hunt, D. A Practical Guide for Medical Teachers; Elsevier Health Sciences: New York, NY, USA, 2017. [Google Scholar]
- Adams, N.E. Bloom’s taxonomy of cognitive learning objectives. J. Med. Libr. Assoc. 2015, 103, 52. [Google Scholar] [CrossRef] [PubMed]
- Russell, I.J.; Hendricson, W.D.; Herbert, R.J. Effects of lecture information density on medical student achievement. J. Med. Ed. 1984, 59, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Seery, M.K.; Donnelly, R. The implementation of pre-lecture resources to reduce in-class cognitive load: A case study for higher education chemistry. Br. J. Educ. Technol. 2012, 43, 667–677. [Google Scholar] [CrossRef]
- Lumpkin, A. Metacognition and its contribution to student learning introduction. Coll. Stud. J. 2020, 54, 1–7. [Google Scholar]
- Artino, A.R., Jr.; Hemmer, P.A.; Durning, S.J. Using self-regulated learning theory to understand the beliefs, emotions, and behaviors of struggling medical students. Acad. Med. 2011, 86, S35–S38. [Google Scholar] [CrossRef] [PubMed]
- Krathwohl, D.R. A revision of Bloom’s taxonomy: An overview. Theory Pract. 2002, 41, 212–218. [Google Scholar] [CrossRef]
- Babeck, J.M.; Luther, V.P. Creating and presenting an effective lecture. J. Contin. High. Educ. 2020, 40, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Edmunds, S.; Brown, G. Effective small group learning: AMEE Guide No. 48. Med. Teach. 2010, 32, 715–726. [Google Scholar] [CrossRef] [PubMed]
- Van Blackenstein, F.M.; Dolmans, D.H.J.M.; van der Vlueten, C.P.M.; Schmidt, H.G. Which cognitive structures support learning? The role of providing explanations and listening to others. Instr. Sci. 2011, 39, 189–204. [Google Scholar]
- Paukert, J.; Richards, B. How medical students and residents describe the roles and characteristics of their influential clinical teachers. Acad. Med. 2000, 75, 843–845. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).