Conflict between Science and Superstition in Medical Practices
Abstract
1. Introduction
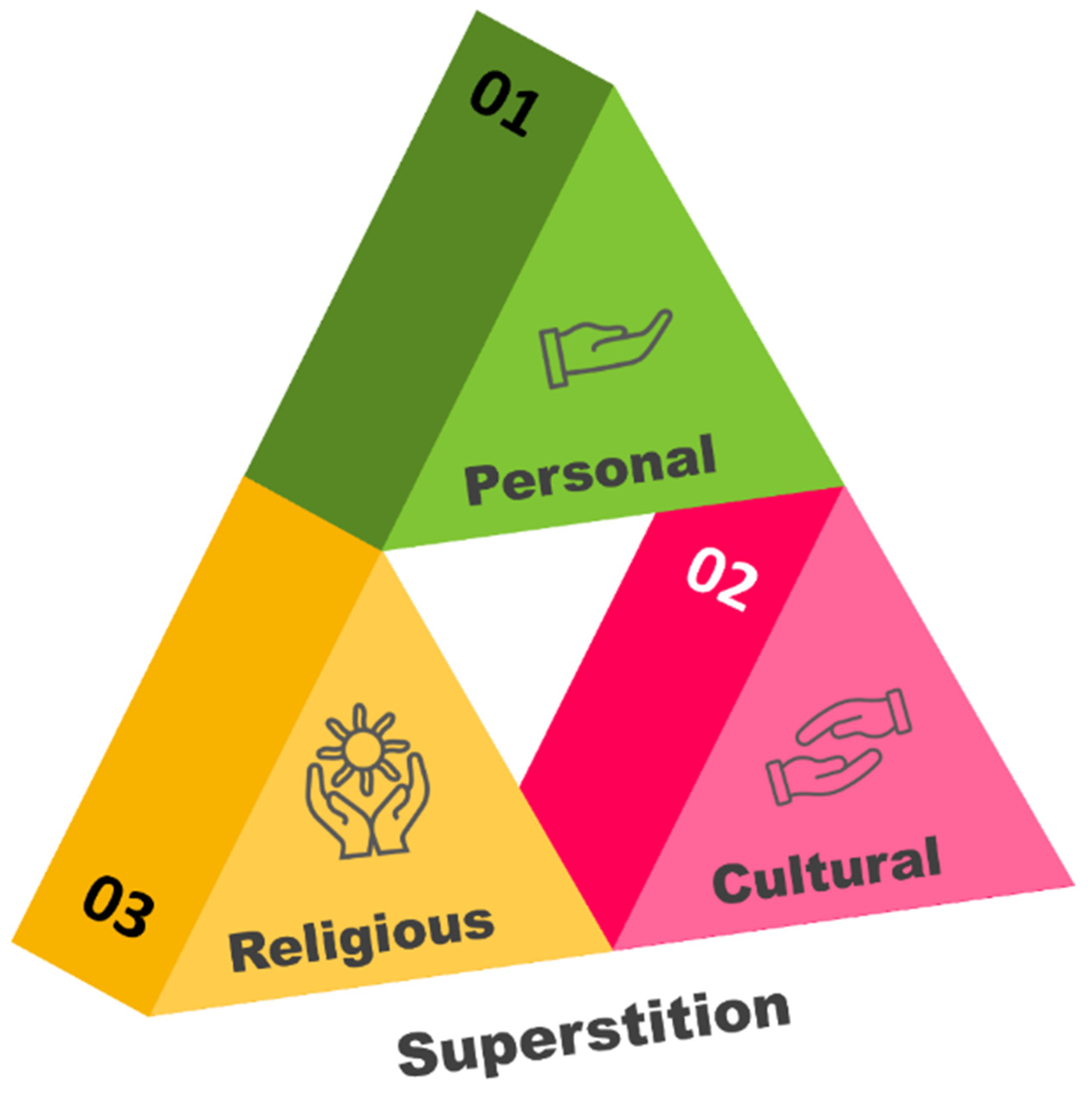
2. Superstition
3. Superstition and Health Care
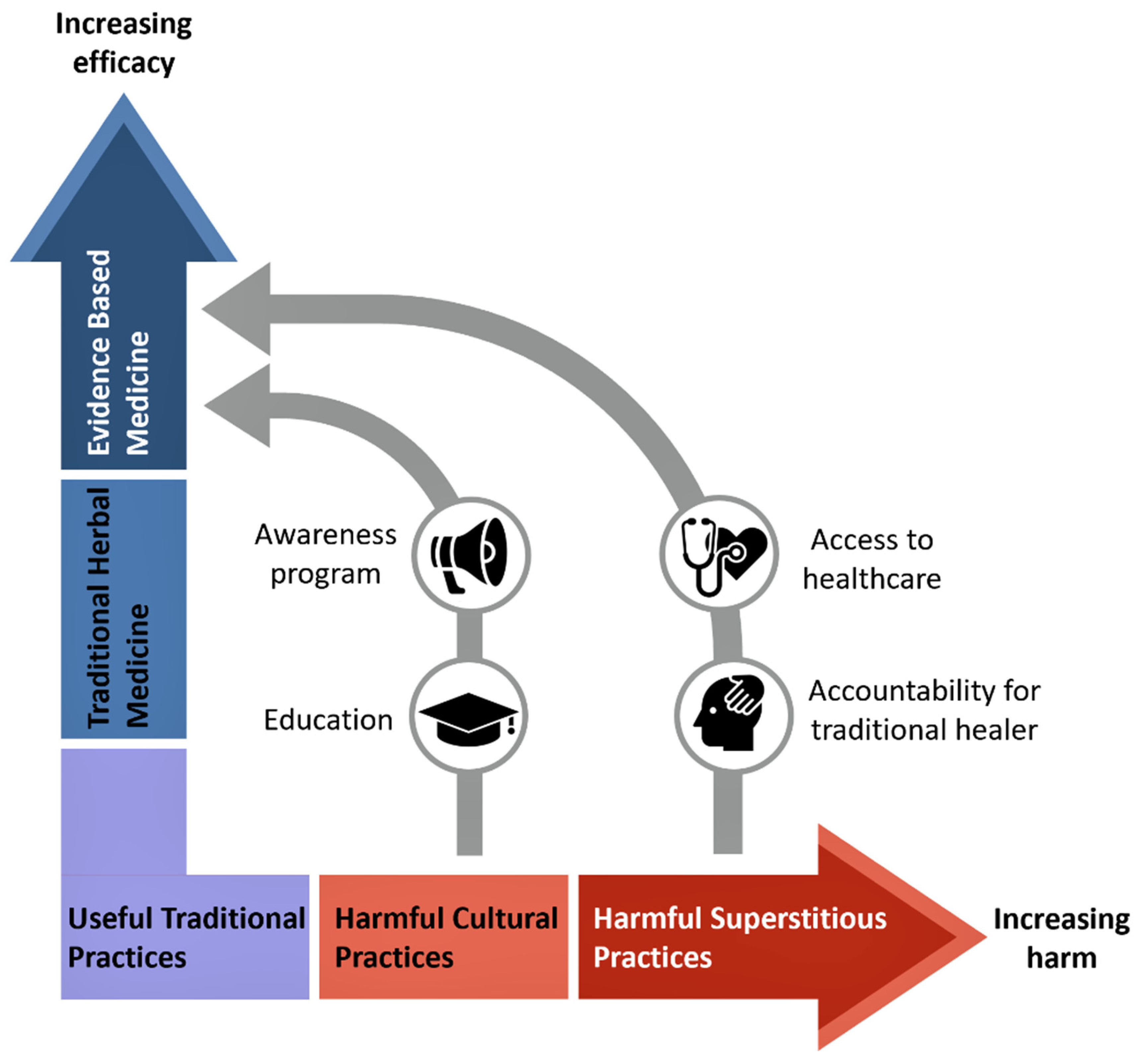
4. Conflict between Superstition and Clinical Practices
5. Conclusions
- Health literacy and awareness of professional health education and promotion in the communities to prevent these unprofessional traditional practices.
- Medical and other Health professionals should educate the community on the harmful effects of traditional practices through community health outreaches.
- The danger of blood-borne infections such as HIV that may occur due to these practices should be emphasized.
- Availability, accessibility, and quality of professional healthcare services in the community should be improved.
- Harmful consequences of unsafe traditional health practices should be included in all health science curricula.
- Traditional healers should be held accountable for unprofessional acts and practices.
- Develop policies, standards, and regulatory frameworks to safely and effectively use helpful traditional medicine.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cleland, C.E. Historical science, experimental science, and the scientific method. Geology 2001, 29, 987–990. [Google Scholar]
- Fischer, M.R.; Fabry, G. Thinking and acting scientifically: Indispensable basis of medical education. GMS Z. Med. Ausbild. 2014, 31, Doc24. [Google Scholar] [PubMed]
- Ziman, J.M. The proliferation of scientific literature: A natural process. Science 1980, 208, 369–371. [Google Scholar] [CrossRef] [PubMed]
- Abraham, R.R.; Upadhya, S.; Torke, S.; Ramnarayan, K. Clinically oriented physiology teaching: Strategy for developing critical-thinking skills in undergraduate medical students. Adv. Physiol. Educ. 2004, 28, 102–104. [Google Scholar] [CrossRef] [PubMed]
- Ezzo, J.; Bausell, B.; Moerman, D.E.; Berman, B.; Hadhazy, V. Reviewing the reviews: How strong is the evidence? How clear are the conclusions? Int. J. Technol. Assess. Health Care 2001, 17, 457–466. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.; Biala, N. A searchable database of medical education objectives–creating a comparable gold standard. BMC Med. Educ. 2018, 18, 31. [Google Scholar] [CrossRef]
- Zirker, J.B. Total eclipses of the sun. Science 1980, 210, 1313–1319. [Google Scholar] [CrossRef]
- Vyse, S.A. Believing in Magic: The Psychology of Superstition; Updated Edition; Oxford University Press: Oxford, UK, 2013. [Google Scholar]
- Berger, A.S. The evil eye—An ancient superstition. J. Relig. Health 2012, 51, 1098–1103. [Google Scholar] [CrossRef] [PubMed]
- Risen, J.L. Believing what we do not believe: Acquiescence to superstitious beliefs and other powerful intuitions. Psychol. Rev. 2016, 123, 182. [Google Scholar] [CrossRef] [PubMed]
- Haque, M.I.; Chowdhury, A.; Shahjahan, M.; Harun, M.G.D. Traditional healing practices in rural Bangladesh: A qualitative investigation. BMC Complement. Altern. Med. 2018, 18, 62. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, C.M.; Iwasa, Y. Cultural evolution of a belief controlling human mate choice: Dynamic modeling of the hinoeuma superstition in Japan. J. Theor. Biol. 2012, 309, 20–28. [Google Scholar] [CrossRef]
- Dömötör, Z.; Ruíz-Barquín, R.; Szabo, A. Superstitious behavior in sport: A literature review. Scand. J. Psychol. 2016, 57, 368–382. [Google Scholar] [CrossRef] [PubMed]
- Crawfurd, R. Of Superstitions concerning Menstruation. Proc. R. Soc. Med. 1916, 9, 49–66. [Google Scholar] [CrossRef]
- Umeora, O.; Egwuatu, V. Menstruation in rural Igbo women of south east Nigeria: Attitudes, beliefs and practices. Afr. J. Reprod. Health 2008, 12, 109–115. [Google Scholar] [PubMed]
- Reiling, J. Superstitions in medicine. JAMA 2006, 295, 113. [Google Scholar]
- Rozin, P.; Nemeroff, C. The laws of sympathetic magic. In Cultural Psychology: Essays on Comparative Human Development; Herdt, G., Stigler, J.W., Schweder, R.A., Eds.; Cambridge University Press: Cambridge, UK, 1990; pp. 205–232. [Google Scholar]
- Rozin, P.; Nemeroff, C. Sympathetic Magical Thinking: The Contagion and Similarity Heuristics; Cambridge University Press: New York, NY, USA, 2002. [Google Scholar]
- Exadaktylos, A.K.; Sclabas, G.; Siegenthaler, A.; Eggli, S.; Kohler, H.P.; Luterbacher, J. Friday the 13th and full-moon the “Worst Case Scenario” or only superstition? Am. J. Emerg. Med. 2001, 19, 319–320. [Google Scholar] [CrossRef] [PubMed]
- Golooba-Mutebi, F.; Tollman, S.M. Confronting HIV/AIDS in a South African village: The impact of health-seeking behaviour 1. Scand. J. Public Health 2007, 35, 175–180. [Google Scholar] [CrossRef]
- Foster, K.R.; Kokko, H. The evolution of superstitious and superstition-like behaviour. Proc. R. Soc. B Biol. Sci. 2008, 276, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Tversky, A.; Kahneman, D. Availability: A heuristic for judging frequency and probability. Cogn. Psychol. 1973, 5, 207–232. [Google Scholar] [CrossRef]
- Tversky, A.; Kahneman, D. Judgment under Uncertainty: Heuristics and Biases. Science 1974, 185, 1124. [Google Scholar] [CrossRef] [PubMed]
- Tversky, A.; Kahneman, D. Extensional versus intuitive reasoning: The conjunction fallacy in probability judgment. Psychol. Rev. 1983, 90, 293–315. [Google Scholar] [CrossRef]
- Hira, K.; Fukui, T.; Endoh, A.; Rahman, M.; Maekawa, M. Influence of superstition on the date of hospital discharge and medical cost in Japan: Retrospective and descriptive study. BMJ 1998, 317, 1680–1683. [Google Scholar] [CrossRef] [PubMed]
- Mjaess, G.; Aoun, F.; Kazzi, H.; Karam, A.; Albisinni, S.; Roumeguère, T. Myths, Superstitions, and Popular Beliefs: Do They Still Impact Our Practice? Ann. Surg. 2021, 274, e641–e642. [Google Scholar] [CrossRef] [PubMed]
- Bukhari, S.S.; Pardhan, A.; Khan, A.S.; Ahmed, A.; Choudry, F.J.; Pardhan, K.; Nayeem, K.; Khan, M. Superstitions regarding health problems in different ethnic groups in Karachi. J. Pak. Med. Assoc. 2002, 52, 383–387. [Google Scholar] [PubMed]
- Anwar, M.; Green, J.; Norris, P. Health-seeking behaviour in Pakistan: A narrative review of the existing literature. Public Health 2012, 126, 507–517. [Google Scholar] [CrossRef] [PubMed]
- Webb, J.Y. Louisiana voodoo and superstitions related to health. HSMHA Health Rep. 1971, 86, 291–301. [Google Scholar] [CrossRef]
- Fouka, G.; Plakas, S.; Taket, A.; Boudioni, M.; Dandoulakis, M. Health-related religious rituals of the Greek Orthodox Church: Their uptake and meanings. J. Nurs. Manag. 2012, 20, 1058–1068. [Google Scholar] [CrossRef] [PubMed]
- Waqas, A.; Zubair, M.; Ghulam, H.; Ullah, M.W.; Tariq, M.Z. Public stigma associated with mental illnesses in Pakistani university students: A cross sectional survey. PeerJ 2014, 2, e698. [Google Scholar] [CrossRef]
- Mandell, D.L.; Claypool, M.L.; Kay, D.J. Superstitions among perioperative nurses. AORN J. 2005, 81, 971–984. [Google Scholar] [CrossRef]
- Sharma, S.; Bansal, R.; Ahmad, S.; Shukla, A.K.; Anand, A.; Gulia, T. Superstitions in Urban Community Affecting Health: Assessment and Interventional study in Meerut, India. SMU Med. J. 2016, 3, 606–615. [Google Scholar]
- Akosa, P. Superstition is a Drawback to Dhana’s Dealth Dare Dystem. 2014. Available online: https://www.ghanaweb.com/GhanaHomePage/NewsArchive/Superstition-is-a-drawback-to-Ghana-s-health-care-system-Prof-Akosa-304704 (accessed on 10 February 2021).
- Tenkorang, E.Y.; Gyimah, S.O.; Maticka-Tyndale, E.; Adjei, J. Superstition, witchcraft and HIV prevention in sub-Saharan Africa: The case of Ghana. Cult. Health Sex. 2011, 13, 1001–1014. [Google Scholar] [CrossRef]
- Okuyaz, S.; İpek, R.; Ögenler, O.; Yıldırım, D.D.; Okuyaz, Ç. Beliefs and behaviors of patients’ relatives towards childhood epilepsy in Turkey. Seizure 2022, 100, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Hillard, J.R.; Rockwell, W.J. Dysesthesia, witchcraft, and conversion reaction. A case successfully treated with psychotherapy. JAMA 1978, 240, 1742–1744. [Google Scholar] [CrossRef] [PubMed]
- Ijaduola, G.T. Uvulectomy in Nigeria. J. Laryngol. Otol. 1981, 95, 1127–1133. [Google Scholar] [CrossRef]
- Miles, S.H.; Ololo, H. Traditional surgeons in sub-Saharan Africa: Images from south Sudan. Int. J. STD AIDS 2003, 14, 505–508. [Google Scholar] [CrossRef]
- Wein, S. Cancer, unproven therapies, and magic. Oncology 2000, 14, 1345–1350, discussion 1355–1349. [Google Scholar]
- Bjalkander, O.; Bangura, L.; Leigh, B.; Berggren, V.; Bergstrom, S.; Almroth, L. Health complications of female genital mutilation in Sierra Leone. Int. J. Womens Health 2012, 4, 321–331. [Google Scholar] [CrossRef]
- Komolafe, O.O.; Ogunleye, O.T.; Fasina, O.O.; Komolafe, O.A. African traditional medication and keloid formation in herpes zoster ophthalmicus. Niger. J. Clin. Pract. 2011, 14, 479–481. [Google Scholar] [CrossRef]
- Manni, J.J. Uvulectomy, a traditional surgical procedure in Tanzania. Ann. Trop. Med. Parasitol. 1984, 78, 49–53. [Google Scholar] [CrossRef]
- Pallangyo, P.; Nicholaus, P.; Mayala, H.; Kabeho, A.; Nkinda, A.; Janabi, M. Human immunodeficiency virus infection acquired through a traditional healer’s ritual: A case report. J. Med. Case Rep. 2017, 11, 301. [Google Scholar] [CrossRef]
- Ezenyeaku, C.; Okeke, T.; Chigbu, C.; Ikeako, L. Survey of Women’s Opinions on Female Genital Mutilation (FGM) in Southeast Nigeria: Study of Patients Attending Antenatal Clinic. Ann. Med. Health Sci. Res. 2011, 1, 15–20. [Google Scholar] [PubMed]
- Iriso, R.; Accorsi, S.; Akena, S.; Amone, J.; Fabiani, M.; Ferrarese, N.; Lukwiya, M.; Rosolen, T.; Declich, S. ‘Killer’ canines: The morbidity and mortality of ebino in northern Uganda. Trop. Med. Int. Health 2000, 5, 706–710. [Google Scholar] [CrossRef] [PubMed]
- Shah, G.; Susan, L.; Furcroy, J. Female circumcision: History, medical and psychological complications, and initiatives to eradicate this practice. Can. J. Urol. 2009, 16, 4576–4579. [Google Scholar]
- Albertyn, R.; Berg, A.; Numanoglu, A.; Rode, H. Traditional burn care in sub-Saharan Africa: A long history with wide acceptance. Burns 2015, 41, 203–211. [Google Scholar] [CrossRef]
- Reid, S.R. Injections that kill: Nosocomial bacteraemia and degedege in Tanzania. Rural Remote Health 2010, 10, 1463. [Google Scholar] [CrossRef]
- Withers, M.; Kharazmi, N.; Lim, E. Traditional beliefs and practices in pregnancy, childbirth and postpartum: A review of the evidence from Asian countries. Midwifery 2018, 56, 158–170. [Google Scholar] [CrossRef]
- Bogale, D.; Markos, D.; Kaso, M. Prevalence of female genital mutilation and its effect on women’s health in Bale zone, Ethiopia: A cross-sectional study. BMC Public Health 2014, 14, 1076. [Google Scholar] [CrossRef]
- Tobian, A.A.; Gray, R.H. The medical benefits of male circumcision. JAMA 2011, 306, 1479–1480. [Google Scholar] [CrossRef][Green Version]
- Tobian, A.A.; Gray, R.H.; Quinn, T.C. Male circumcision for the prevention of acquisition and transmission of sexually transmitted infections: The case for neonatal circumcision. Arch. Pediatr. Adolesc. Med. 2010, 164, 78–84. [Google Scholar] [CrossRef]
- Machumu, R.S.; Fabian-Taylor, F.M. The practice of uvulectomy and related complications among children aged below 6 years in Ilemela district, Mwanza, Tanzania. Tanzan. Dent. J. 2008, 15, 10–14. [Google Scholar]
- De Velasco, A.M. Consequences of early childbearing. Draper Fund Rep. 1982, 11, 26–27. [Google Scholar]
- Saxena, P.; Salhan, S.; Chattopadhyay, B.; Kohli, M.; Nandan, D.; Adhish, S. Obstetric and perinatal outcome of teenage and older primigravidas-a retrospective analysis. Health Popul. Perspect. Issues 2010, 33, 16–22. [Google Scholar]
- Stokoe, U. Determinants of maternal mortality in the developing world. Aust. N. Z. J. Obstet. Gynaecol. 1991, 31, 8–16. [Google Scholar] [CrossRef] [PubMed]
- Suwal, A. Obstetric and perinatal outcome of teenage pregnancy. J. Nepal Health Res. Counc. 2012, 10, 52–56. [Google Scholar]
- Bataringaya, A.; Ferguson, M.; Lalloo, R. The impact of ebinyo, a form of dental mutilation, on the malocclusion status in Uganda. Community Dent. Health 2005, 22, 146–150. [Google Scholar] [PubMed]
- Edwards, P.C.; Levering, N.; Wetzel, E.; Saini, T. Extirpation of the primary canine tooth follicles: A form of infant oral mutilation. J. Am. Dent. Assoc. 2008, 139, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Kemoli, A.; Gjorup, H.; Norregaard, M.M.; Lindholm, M.; Mulli, T.; Johansson, A.; Haubek, D. Prevalence and impact of infant oral mutilation on dental occlusion and oral health-related quality of life among Kenyan adolescents from Maasai Mara. BMC Oral Health 2018, 18, 173. [Google Scholar] [CrossRef] [PubMed]
- Pope, E.A.; Roberts, M.W.; Johnson, E.L.; Morris, C.L. Infant Oral Mutilation. Case Rep. Dent. 2018, 2018, 7586468. [Google Scholar] [CrossRef]
- Wandera, M.N.; Kasumba, B. “Ebinyo”-The Practice of Infant Oral Mutilation in Uganda. Front. Public Health 2017, 5, 167. [Google Scholar] [CrossRef]
- Baba, S.P.; Kay, E.J. The mythology of the killer deciduous canine tooth in southern Sudan. J. Pedod. 1989, 14, 48–49. [Google Scholar] [PubMed]
- Hassanali, J.; Amwayi, P.; Muriithi, A. Removal of deciduous canine tooth buds in Kenyan rural Maasai. East. Afr. Med. J. 1995, 72, 207–209. [Google Scholar] [PubMed]
- Tirwomwe, J.; Agwu, E.; Ssamula, M. The magnitude of tooth bud extraction in Uganda. Int. J. Med. Med. Sci. 2013, 5, 450–455. [Google Scholar]
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef]
- Hersh, L.; Salzman, B.; Snyderman, D. Health Literacy in Primary Care Practice. Am. Fam. Physician 2015, 92, 118–124. [Google Scholar] [PubMed]
- Harms, G.; Schulze, K.; Moneta, I.; Baryomunsi, C.; Mbezi, P.; Poggensee, G. Mother-to-child transmission of HIV and its prevention: Awareness and knowledge in Uganda and Tanzania. Sahara J. 2005, 2, 258–266. [Google Scholar] [CrossRef] [PubMed]
- Kea, A.Z.; Tulloch, O.; Datiko, D.G.; Theobald, S.; Kok, M.C. Exploring barriers to the use of formal maternal health services and priority areas for action in Sidama zone, southern Ethiopia. BMC Pregnancy Childbirth 2018, 18, 96. [Google Scholar] [CrossRef] [PubMed]
- Abbo, C. Profiles and outcome of traditional healing practices for severe mental illnesses in two districts of Eastern Uganda. Glob. Health Action 2011, 4, 7117. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, S.; Imanishi, J.; Satoh, M.; Ozasa, K. Unique place of Kampo (Japanese traditional medicine) in complementary and alternative medicine: A survey of doctors belonging to the regional medical association in Japan. Tohoku J. Exp. Med. 2001, 194, 55–63. [Google Scholar] [CrossRef]
- Evariste, N.; Valens, M.; Donat, U.; Stoufi, E.; Razzaque, M.S. Early childhood tooth bud removal practice (“Ibyinyo”): Preventable dental damage. Adv. Hum. Biolol. 2020, 10, 193–196. [Google Scholar]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uwayezu, D.; Ntigura, E.; Gatarayiha, A.; Erem, A.S.; Haque, M.; Majumder, M.A.A.; Razzaque, M.S. Conflict between Science and Superstition in Medical Practices. Int. Med. Educ. 2022, 1, 33-42. https://doi.org/10.3390/ime1020007
Uwayezu D, Ntigura E, Gatarayiha A, Erem AS, Haque M, Majumder MAA, Razzaque MS. Conflict between Science and Superstition in Medical Practices. International Medical Education. 2022; 1(2):33-42. https://doi.org/10.3390/ime1020007
Chicago/Turabian StyleUwayezu, Donat, Eustache Ntigura, Agnes Gatarayiha, Anna Sarah Erem, Mainul Haque, Md Anwarul Azim Majumder, and Mohammed S. Razzaque. 2022. "Conflict between Science and Superstition in Medical Practices" International Medical Education 1, no. 2: 33-42. https://doi.org/10.3390/ime1020007
APA StyleUwayezu, D., Ntigura, E., Gatarayiha, A., Erem, A. S., Haque, M., Majumder, M. A. A., & Razzaque, M. S. (2022). Conflict between Science and Superstition in Medical Practices. International Medical Education, 1(2), 33-42. https://doi.org/10.3390/ime1020007







