Prescribing Responsibly: Navigating the Tides of Deprescribing in Proton Pump Inhibitor Stewardship
Abstract
1. Introduction
2. Methods
Literature Selection Strategy
3. Appropriate Prescribing of PPIs
3.1. Gastroesophageal Reflux Disease
3.2. Eosinophilic Esophagitis
3.3. Peptic Ulcer Disease
3.4. Upper Gastrointestinal Bleeding
3.5. Stress-Related Mucosal Disease
3.6. Dyspepsia
4. Risks Associated with PPI Use
4.1. Malabsorption of Vitamins and Minerals
4.2. Cardiovascular Disease and Death
4.3. Altered Immune Function, Dysbiosis, and Antimicrobial Resistance
4.4. Enteric Infections
4.5. Peritonitis and Hepatic Encephalopathy
4.6. Respiratory Infections
4.7. Malignancy
4.8. Impaired Kidney Function
4.9. Cognitive Impairments
4.10. Myopathy
4.11. Microscopic Colitis
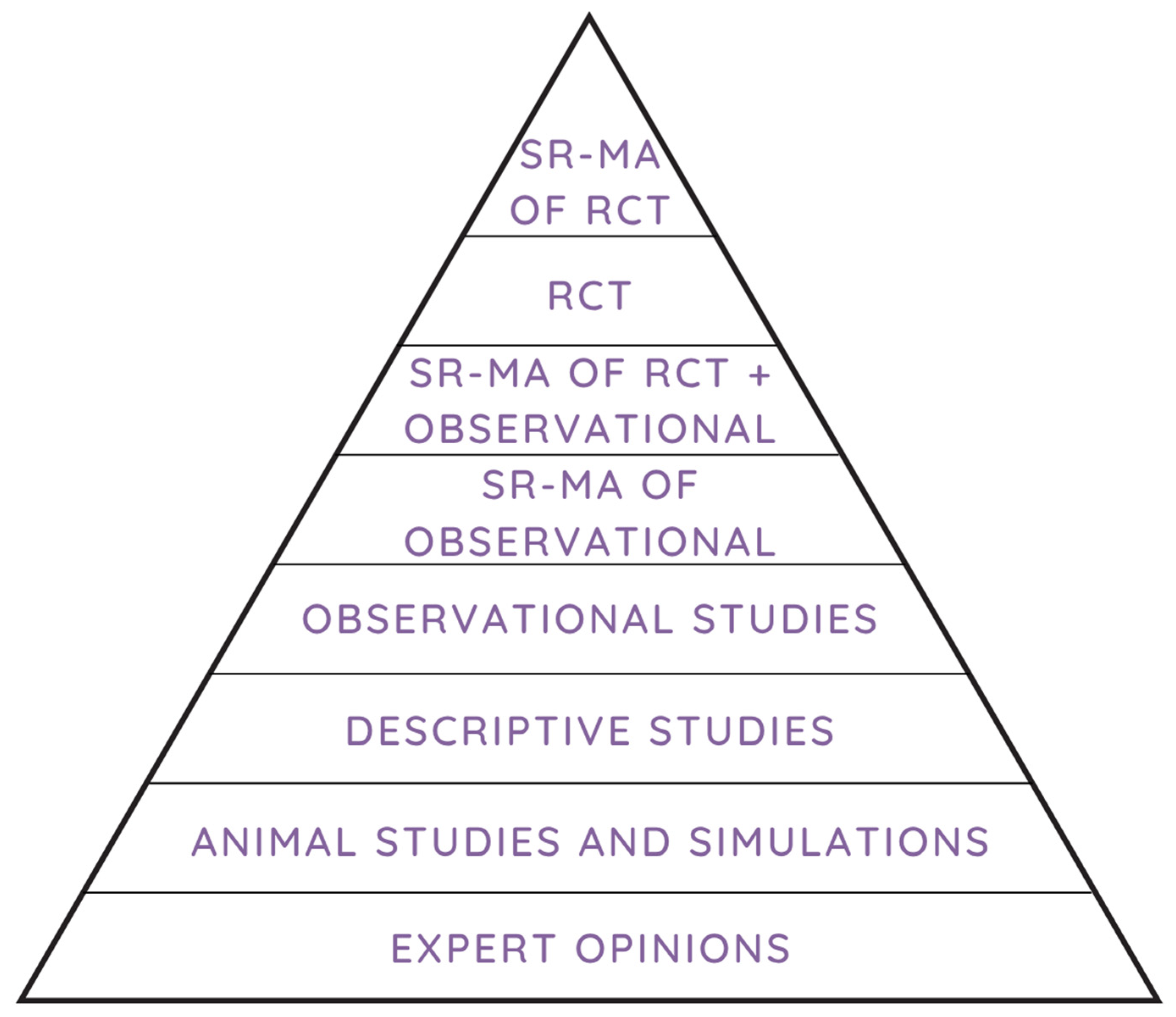
4.12. Limitations of the Evidence Base
5. Recommendations for Deprescribing PPIs
5.1. Deprescribing Strategies
5.2. Criteria for Deprescribing
5.3. Long-Term Monitoring
5.4. Challenges and Barriers
5.5. Policy and Stewardship Considerations
5.6. Future Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Malfertheiner, P.; Kandulski, A.; Venerito, M. Proton-pump inhibitors: Understanding the complications and risks. Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 697–710. [Google Scholar] [CrossRef]
- Boghossian, T.A.; Rashid, F.J.; Thompson, W.; Welch, V.; Moayyedi, P.; Rojas-Fernandez, C.; Pottie, K.; Farrell, B. Deprescribing versus continuation of chronic proton pump inhibitor use in adults. Cochrane Database Syst. Rev. 2017, 3, CD011969. [Google Scholar] [CrossRef]
- Zhang, D.; Liu, S.; Li, Z.; Wang, R. Global, regional and national burden of gastroesophageal reflux disease, 1990–2019: Update from the GBD 2019 study. Ann. Med. 2022, 54, 1372–1384. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.A.; Katz, P.O.; Armstrong, D.; Cohen, H.; Delaney, B.C.; Howden, C.W.; Katelaris, P.; Tutuian, R.I.; Castell, D.O. The Safety of Appropriate Use of Over-the-Counter Proton Pump Inhibitors: An Evidence-Based Review and Delphi Consensus. Drugs 2017, 77, 547–561. [Google Scholar] [CrossRef]
- Clarke, K.; Adler, N.; Agrawal, D.; Bhakta, D.; Sata, S.S.; Singh, S.; Gupta, A.; Pahwa, A.; Pherson, E.; Sun, A.; et al. Indications for the Use of Proton Pump Inhibitors for Stress Ulcer Prophylaxis and Peptic Ulcer Bleeding in Hospitalized Patients. Am. J. Med. 2022, 135, 313–317. [Google Scholar] [CrossRef]
- Farrell, B.; Pottie, K.; Thompson, W.; Boghossian, T.; Pizzola, L.; Rashid, F.J.; Rojas-Fernandez, C.; Walsh, K.; Welch, V.; Moayyedi, P. Deprescribing proton pump inhibitors: Evidence-based clinical practice guideline. Can. Fam. Physician 2017, 63, 354–364. [Google Scholar]
- PRILOSEC (Omeprazole) [Package Insert]; AstraZeneca Pharmaceuticals LP: Wilmington, DE, USA, 2012.
- Fass, R. Gastroesophageal Reflux Disease. N. Engl. J. Med. 2022, 387, 1207–1216. [Google Scholar] [CrossRef]
- Katz, P.O.; Dunbar, K.B.; Schnoll-Sussman, F.H.; Greer, K.B.; Yadlapati, R.; Spechler, S.J. ACG Clinical Guideline for the Diagnosis and Management of Gastroesophageal Reflux Disease. Am. J. Gastroenterol. 2022, 117, 27–56. [Google Scholar] [CrossRef] [PubMed]
- Fackler, W.K.; Ours, T.M.; Vaezi, M.F.; Richter, J.E. Long-term effect of H2RA therapy on nocturnal gastric acid breakthrough. Gastroenterology 2002, 122, 625–632. [Google Scholar] [CrossRef] [PubMed]
- Lima, J.J.; Thomas, C.D.; Barbarino, J.; Desta, Z.; Van Driest, S.L.; El Rouby, N.; Johnson, J.A.; Cavallari, L.H.; Shakhnovich, V.; Thacker, D.L.; et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2C19 and Proton Pump Inhibitor Dosing. Clin. Pharmacol. Ther. 2021, 109, 1417–1423. [Google Scholar] [CrossRef]
- Hunfeld, N.G.; Touw, D.J.; Mathot, R.A.; Mulder, P.G.; RH, V.A.N.S.; Kuipers, E.J.; Kooiman, J.C.; Geus, W.P. A comparison of the acid-inhibitory effects of esomeprazole and pantoprazole in relation to pharmacokinetics and CYP2C19 polymorphism. Aliment. Pharmacol. Ther. 2010, 31, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Dellon, E.S.; Muir, A.B.; Katzka, D.A.; Shah, S.C.; Sauer, B.G.; Aceves, S.S.; Furuta, G.T.; Gonsalves, N.; Hirano, I. ACG Clinical Guideline: Diagnosis and Management of Eosinophilic Esophagitis. Am. J. Gastroenterol. 2025, 120, 31–59. [Google Scholar] [CrossRef]
- Peterson, K.A.; Thomas, K.L.; Hilden, K.; Emerson, L.L.; Wills, J.C.; Fang, J.C. Comparison of esomeprazole to aerosolized, swallowed fluticasone for eosinophilic esophagitis. Dig. Dis. Sci. 2010, 55, 1313–1319. [Google Scholar] [CrossRef]
- Moawad, F.J.; Veerappan, G.R.; Dias, J.A.; Baker, T.P.; Maydonovitch, C.L.; Wong, R.K. Randomized controlled trial comparing aerosolized swallowed fluticasone to esomeprazole for esophageal eosinophilia. Am. J. Gastroenterol. 2013, 108, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Laine, L. CLINICAL PRACTICE. Upper Gastrointestinal Bleeding Due to a Peptic Ulcer. N. Engl. J. Med. 2016, 374, 2367–2376. [Google Scholar] [CrossRef] [PubMed]
- Vakil, N. Peptic Ulcer Disease: A Review. JAMA 2024, 332, 1832–1842. [Google Scholar] [CrossRef]
- Chey, W.D.; Howden, C.W.; Moss, S.F.; Morgan, D.R.; Greer, K.B.; Grover, S.; Shah, S.C. ACG Clinical Guideline: Treatment of Helicobacter pylori Infection. Am. J. Gastroenterol. 2024, 119, 1730–1753. [Google Scholar] [CrossRef]
- Lanza, F.L.; Chan, F.K.; Quigley, E.M.; Practice Parameters Committee of the American College of Gastroenterology. Guidelines for prevention of NSAID-related ulcer complications. Am. J. Gastroenterol. 2009, 104, 728–738. [Google Scholar] [CrossRef]
- Castellsague, J.; Riera-Guardia, N.; Calingaert, B.; Varas-Lorenzo, C.; Fourrier-Reglat, A.; Nicotra, F.; Sturkenboom, M.; Perez-Gutthann, S.; Safety of Non-Steroidal Anti-Inflammatory Drugs (SOS) Project. Individual NSAIDs and upper gastrointestinal complications: A systematic review and meta-analysis of observational studies (the SOS project). Drug Saf. 2012, 35, 1127–1146. [Google Scholar] [CrossRef]
- Yuan, J.Q.; Tsoi, K.K.; Yang, M.; Wang, J.Y.; Threapleton, D.E.; Yang, Z.Y.; Zou, B.; Mao, C.; Tang, J.L.; Chan, F.K. Systematic review with network meta-analysis: Comparative effectiveness and safety of strategies for preventing NSAID-associated gastrointestinal toxicity. Aliment. Pharmacol. Ther. 2016, 43, 1262–1275. [Google Scholar] [CrossRef]
- Lanas, A.; Chan, F.K.L. Peptic ulcer disease. Lancet 2017, 390, 613–624. [Google Scholar] [CrossRef] [PubMed]
- Abraham, N.S.; Hlatky, M.A.; Antman, E.M.; Bhatt, D.L.; Bjorkman, D.J.; Clark, C.B.; Furberg, C.D.; Johnson, D.A.; Kahi, C.J.; Laine, L.; et al. ACCF/ACG/AHA 2010 expert consensus document on the concomitant use of proton pump inhibitors and thienopyridines: A focused update of the ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use. A Report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. J. Am. Coll. Cardiol. 2010, 56, 2051–2066. [Google Scholar] [CrossRef] [PubMed]
- Laine, L.; Barkun, A.N.; Saltzman, J.R.; Martel, M.; Leontiadis, G.I. ACG Clinical Guideline: Upper Gastrointestinal and Ulcer Bleeding. Am. J. Gastroenterol. 2021, 116, 899–917. [Google Scholar] [CrossRef]
- Sachar, H.; Vaidya, K.; Laine, L. Intermittent vs continuous proton pump inhibitor therapy for high-risk bleeding ulcers: A systematic review and meta-analysis. JAMA Intern. Med. 2014, 174, 1755–1762. [Google Scholar] [CrossRef]
- Bardou, M.; Quenot, J.P.; Barkun, A. Stress-related mucosal disease in the critically ill patient. Nat. Rev. Gastroenterol. Hepatol. 2015, 12, 98–107. [Google Scholar] [CrossRef]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; McIntyre, L.; Ostermann, M.; Prescott, H.C.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Crit. Care Med. 2021, 49, e1063–e1143. [Google Scholar] [CrossRef] [PubMed]
- Blackett, J.W.; Faye, A.S.; Phipps, M.; Li, J.; Lebwohl, B.; Freedberg, D.E. Prevalence and Risk Factors for Inappropriate Continuation of Proton Pump Inhibitors After Discharge From the Intensive Care Unit. Mayo Clin. Proc. 2021, 96, 2550–2560. [Google Scholar] [CrossRef]
- Krag, M.; Marker, S.; Perner, A.; Wetterslev, J.; Wise, M.P.; Schefold, J.C.; Keus, F.; Guttormsen, A.B.; Bendel, S.; Borthwick, M.; et al. Pantoprazole in Patients at Risk for Gastrointestinal Bleeding in the ICU. N. Engl. J. Med. 2018, 379, 2199–2208. [Google Scholar] [CrossRef]
- Marker, S.; Perner, A.; Wetterslev, J.; Krag, M.; Lange, T.; Wise, M.P.; Borthwick, M.; Bendel, S.; Keus, F.; Guttormsen, A.B.; et al. Pantoprazole prophylaxis in ICU patients with high severity of disease: A post hoc analysis of the placebo-controlled SUP-ICU trial. Intensive Care Med. 2019, 45, 609–618. [Google Scholar] [CrossRef]
- El-Kersh, K.; Jalil, B.; McClave, S.A.; Cavallazzi, R.; Guardiola, J.; Guilkey, K.; Persaud, A.K.; Furmanek, S.P.; Guinn, B.E.; Wiemken, T.L.; et al. Enteral nutrition as stress ulcer prophylaxis in critically ill patients: A randomized controlled exploratory study. J. Crit. Care 2018, 43, 108–113. [Google Scholar] [CrossRef]
- Alhazzani, W.; Alshamsi, F.; Belley-Cote, E.; Heels-Ansdell, D.; Brignardello-Petersen, R.; Alquraini, M.; Perner, A.; Moller, M.H.; Krag, M.; Almenawer, S.; et al. Efficacy and safety of stress ulcer prophylaxis in critically ill patients: A network meta-analysis of randomized trials. Intensive Care Med. 2018, 44, 1–11. [Google Scholar] [CrossRef] [PubMed]
- The PEPTIC Investigators for the Australian; New Zealand Intensive Care Society Clinical Trials Group; Alberta Health Services Critical Care Strategic Clinical Network; The Irish Critical Care Trials Group; Young, P.J.; Bagshaw, S.M.; Forbes, A.B.; Nichol, A.D.; Wright, S.E.; Bailey, M.; et al. Effect of Stress Ulcer Prophylaxis With Proton Pump Inhibitors vs Histamine-2 Receptor Blockers on In-Hospital Mortality Among ICU Patients Receiving Invasive Mechanical Ventilation: The PEPTIC Randomized Clinical Trial. JAMA 2020, 323, 616–626. [Google Scholar] [CrossRef]
- Lee, T.C.; Goodwin Wilson, M.; Lawandi, A.; McDonald, E.G. Proton Pump Inhibitors Versus Histamine-2 Receptor Antagonists Likely Increase Mortality in Critical Care: An Updated Meta-Analysis. Am. J. Med. 2021, 134, e184–e188. [Google Scholar] [CrossRef]
- Wang, Y.; Ge, L.; Ye, Z.; Siemieniuk, R.A.; Reintam Blaser, A.; Wang, X.; Perner, A.; Moller, M.H.; Alhazzani, W.; Cook, D.; et al. Efficacy and safety of gastrointestinal bleeding prophylaxis in critically ill patients: An updated systematic review and network meta-analysis of randomized trials. Intensive Care Med. 2020, 46, 1987–2000. [Google Scholar] [CrossRef] [PubMed]
- Cook, D.; Deane, A.; Lauzier, F.; Zytaruk, N.; Guyatt, G.; Saunders, L.; Hardie, M.; Heels-Ansdell, D.; Alhazzani, W.; Marshall, J.; et al. Stress Ulcer Prophylaxis during Invasive Mechanical Ventilation. N. Engl. J. Med. 2024, 391, 9–20. [Google Scholar] [CrossRef]
- Wang, Y.; Parpia, S.; Ge, L.; Heels-Ansdell, D.; Lai, H.; Esfahani, M.A.; Pan, B.; Alhazzani, W.; Schandelmaier, S.; Lauzier, F.; et al. Proton-Pump Inhibitors to Prevent Gastrointestinal Bleeding—An Updated Meta-Analysis. NEJM Evid. 2024, 3, EVIDoa2400134. [Google Scholar] [CrossRef]
- MacLaren, R.; Dionne, J.C.; Granholm, A.; Alhazzani, W.; Szumita, P.M.; Olsen, K.; Barletta, J.F.; Moller, M.H.; Karvellas, C.J.; Wischmeyer, P.; et al. Society of Critical Care Medicine and American Society of Health-System Pharmacists Guideline for the Prevention of Stress-Related Gastrointestinal Bleeding in Critically Ill Adults. Crit. Care Med. 2024, 52, e421–e430. [Google Scholar] [CrossRef] [PubMed]
- Granholm, A.; Zeng, L.; Dionne, J.C.; Perner, A.; Marker, S.; Krag, M.; MacLaren, R.; Ye, Z.; Moller, M.H.; Alhazzani, W.; et al. Predictors of gastrointestinal bleeding in adult ICU patients: A systematic review and meta-analysis. Intensive Care Med. 2019, 45, 1347–1359. [Google Scholar] [CrossRef]
- Daou, M.; Dionne, J.C.; Teng, J.F.T.; Taran, S.; Zytaruk, N.; Cook, D.; Wilcox, M.E. Prophylactic acid suppressants in patients with primary neurologic injury: A systematic review and meta-analysis of randomized controlled trials. J. Crit. Care 2022, 71, 154093. [Google Scholar] [CrossRef]
- Moayyedi, P.; Lacy, B.E.; Andrews, C.N.; Enns, R.A.; Howden, C.W.; Vakil, N. ACG and CAG Clinical Guideline: Management of Dyspepsia. Am. J. Gastroenterol. 2017, 112, 988–1013. [Google Scholar] [CrossRef]
- Langan, R.C.; Goodbred, A.J. Vitamin B12 Deficiency: Recognition and Management. Am. Fam. Physician 2017, 96, 384–389. [Google Scholar]
- den Elzen, W.P.; Groeneveld, Y.; de Ruijter, W.; Souverijn, J.H.; le Cessie, S.; Assendelft, W.J.; Gussekloo, J. Long-term use of proton pump inhibitors and vitamin B12 status in elderly individuals. Aliment. Pharmacol. Ther. 2008, 27, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Attwood, S.E.; Ell, C.; Galmiche, J.P.; Fiocca, R.; Hatlebakk, J.G.; Hasselgren, B.; Langstrom, G.; Jahreskog, M.; Eklund, S.; Lind, T.; et al. Long-term safety of proton pump inhibitor therapy assessed under controlled, randomised clinical trial conditions: Data from the SOPRAN and LOTUS studies. Aliment. Pharmacol. Ther. 2015, 41, 1162–1174. [Google Scholar] [CrossRef]
- Lam, J.R.; Schneider, J.L.; Zhao, W.; Corley, D.A. Proton pump inhibitor and histamine 2 receptor antagonist use and vitamin B12 deficiency. JAMA 2013, 310, 2435–2442. [Google Scholar] [CrossRef] [PubMed]
- Choudhury, A.; Jena, A.; Jearth, V.; Dutta, A.K.; Makharia, G.; Dutta, U.; Goenka, M.; Kochhar, R.; Sharma, V. Vitamin B12 deficiency and use of proton pump inhibitors: A systematic review and meta-analysis. Expert Rev. Gastroenterol. Hepatol. 2023, 17, 479–487. [Google Scholar] [CrossRef] [PubMed]
- Dharmarajan, T.S.; Kanagala, M.R.; Murakonda, P.; Lebelt, A.S.; Norkus, E.P. Do acid-lowering agents affect vitamin B12 status in older adults? J. Am. Med. Dir. Assoc. 2008, 9, 162–167. [Google Scholar] [CrossRef]
- Elias, E.; Targownik, L.E. The Clinician’s Guide to Proton Pump Inhibitor Related Adverse Events. Drugs 2019, 79, 715–731. [Google Scholar] [CrossRef]
- Schade, S.G.; Cohen, R.J.; Conrad, M.E. Effect of hydrochloric acid on iron absorption. N. Engl. J. Med. 1968, 279, 672–674. [Google Scholar] [CrossRef]
- Ali, M.D. Proton Pump Inhibitors’ Use and Risk of Iron Deficiency Anaemia: A Systematic Review and Meta-analysis. Curr. Rev. Clin. Exp. Pharmacol. 2023, 18, 158–166. [Google Scholar] [CrossRef]
- Shikata, T.; Sasaki, N.; Ueda, M.; Kimura, T.; Itohara, K.; Sugahara, M.; Fukui, M.; Manabe, E.; Masuyama, T.; Tsujino, T. Use of proton pump inhibitors is associated with anemia in cardiovascular outpatients. Circ. J. 2015, 79, 193–200. [Google Scholar] [CrossRef]
- Lam, J.R.; Schneider, J.L.; Quesenberry, C.P.; Corley, D.A. Proton Pump Inhibitor and Histamine-2 Receptor Antagonist Use and Iron Deficiency. Gastroenterology 2017, 152, 821–829.e1. [Google Scholar] [CrossRef] [PubMed]
- Stewart, C.A.; Termanini, B.; Sutliff, V.E.; Serrano, J.; Yu, F.; Gibril, F.; Jensen, R.T. Iron absorption in patients with Zollinger-Ellison syndrome treated with long-term gastric acid antisecretory therapy. Aliment. Pharmacol. Ther. 1998, 12, 83–98. [Google Scholar] [CrossRef]
- Touyz, R.M.; de Baaij, J.H.F.; Hoenderop, J.G.J. Magnesium Disorders. N. Engl. J. Med. 2024, 390, 1998–2009. [Google Scholar] [CrossRef]
- Hess, M.W.; Hoenderop, J.G.; Bindels, R.J.; Drenth, J.P. Systematic review: Hypomagnesaemia induced by proton pump inhibition. Aliment. Pharmacol. Ther. 2012, 36, 405–413. [Google Scholar] [CrossRef]
- El-Charabaty, E.; Saifan, C.; Abdallah, M.; Naboush, A.; Glass, D.; Azzi, G.; Azzi, Y.; Khan, A.; Baydoun, H.; Rondla, C.; et al. Effects of proton pump inhibitors and electrolyte disturbances on arrhythmias. Int. J. Gen. Med. 2013, 6, 515–518. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Srinutta, T.; Chewcharat, A.; Takkavatakarn, K.; Praditpornsilpa, K.; Eiam-Ong, S.; Jaber, B.L.; Susantitaphong, P. Proton pump inhibitors and hypomagnesemia: A meta-analysis of observational studies. Medicine 2019, 98, e17788. [Google Scholar] [CrossRef]
- Danziger, J.; William, J.H.; Scott, D.J.; Lee, J.; Lehman, L.W.; Mark, R.G.; Howell, M.D.; Celi, L.A.; Mukamal, K.J. Proton-pump inhibitor use is associated with low serum magnesium concentrations. Kidney Int. 2013, 83, 692–699. [Google Scholar] [CrossRef] [PubMed]
- Zipursky, J.; Macdonald, E.M.; Hollands, S.; Gomes, T.; Mamdani, M.M.; Paterson, J.M.; Lathia, N.; Juurlink, D.N. Proton pump inhibitors and hospitalization with hypomagnesemia: A population-based case-control study. PLoS Med. 2014, 11, e1001736. [Google Scholar] [CrossRef]
- Kieboom, B.C.; Kiefte-de Jong, J.C.; Eijgelsheim, M.; Franco, O.H.; Kuipers, E.J.; Hofman, A.; Zietse, R.; Stricker, B.H.; Hoorn, E.J. Proton pump inhibitors and hypomagnesemia in the general population: A population-based cohort study. Am. J. Kidney Dis. 2015, 66, 775–782. [Google Scholar] [CrossRef]
- Lazzerini, P.E.; Bertolozzi, I.; Finizola, F.; Acampa, M.; Natale, M.; Vanni, F.; Fulceri, R.; Gamberucci, A.; Rossi, M.; Giabbani, B.; et al. Proton Pump Inhibitors and Serum Magnesium Levels in Patients With Torsades de Pointes. Front. Pharmacol. 2018, 9, 363. [Google Scholar] [CrossRef]
- Hess, M.W.; de Baaij, J.H.; Broekman, M.; Bisseling, T.M.; Haarhuis, B.; Tan, A.; Te Morsche, R.; Hoenderop, J.G.; Bindels, R.J.; Drenth, J.P. Inulin significantly improves serum magnesium levels in proton pump inhibitor-induced hypomagnesaemia. Aliment. Pharmacol. Ther. 2016, 43, 1178–1185. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.X.; Lewis, J.D.; Epstein, S.; Metz, D.C. Long-term proton pump inhibitor therapy and risk of hip fracture. JAMA 2006, 296, 2947–2953. [Google Scholar] [CrossRef] [PubMed]
- Hansen, K.E.; Jones, A.N.; Lindstrom, M.J.; Davis, L.A.; Ziegler, T.E.; Penniston, K.L.; Alvig, A.L.; Shafer, M.M. Do proton pump inhibitors decrease calcium absorption? J. Bone Miner. Res. 2010, 25, 2786–2795. [Google Scholar] [CrossRef] [PubMed]
- Wright, M.J.; Sullivan, R.R.; Gaffney-Stomberg, E.; Caseria, D.M.; O’Brien, K.O.; Proctor, D.D.; Simpson, C.A.; Kerstetter, J.E.; Insogna, K.L. Inhibiting gastric acid production does not affect intestinal calcium absorption in young, healthy individuals: A randomized, crossover, controlled clinical trial. J. Bone Miner. Res. 2010, 25, 2205–2211. [Google Scholar] [CrossRef]
- O’Connell, M.B.; Madden, D.M.; Murray, A.M.; Heaney, R.P.; Kerzner, L.J. Effects of proton pump inhibitors on calcium carbonate absorption in women: A randomized crossover trial. Am. J. Med. 2005, 118, 778–781. [Google Scholar] [CrossRef]
- Freedberg, D.E.; Kim, L.S.; Yang, Y.X. The Risks and Benefits of Long-term Use of Proton Pump Inhibitors: Expert Review and Best Practice Advice From the American Gastroenterological Association. Gastroenterology 2017, 152, 706–715. [Google Scholar] [CrossRef]
- Poly, T.N.; Islam, M.M.; Yang, H.C.; Wu, C.C.; Li, Y.J. Proton pump inhibitors and risk of hip fracture: A meta-analysis of observational studies. Osteoporos. Int. 2019, 30, 103–114. [Google Scholar] [CrossRef]
- Liu, J.; Li, X.; Fan, L.; Yang, J.; Wang, J.; Sun, J.; Wang, Z. Proton pump inhibitors therapy and risk of bone diseases: An update meta-analysis. Life Sci. 2019, 218, 213–223. [Google Scholar] [CrossRef]
- da Maia, T.F.; de Camargo, B.G.; Pereira, M.E.; de Oliveira, C.S.; Guiloski, I.C. Increased Risk of Fractures and Use of Proton Pump Inhibitors in Menopausal Women: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 13501. [Google Scholar] [CrossRef]
- Yu, E.W.; Bauer, S.R.; Bain, P.A.; Bauer, D.C. Proton pump inhibitors and risk of fractures: A meta-analysis of 11 international studies. Am. J. Med. 2011, 124, 519–526. [Google Scholar] [CrossRef]
- Roux, C.; Goldstein, J.L.; Zhou, X.; Klemes, A.; Lindsay, R. Vertebral fracture efficacy during risedronate therapy in patients using proton pump inhibitors. Osteoporos. Int. 2012, 23, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Castellana, C.; Pecere, S.; Furnari, M.; Telese, A.; Matteo, M.V.; Haidry, R.; Eusebi, L.H. Side effects of long-term use of proton pump inhibitors: Practical considerations. Pol. Arch. Intern. Med. 2021, 131, 541–549. [Google Scholar] [CrossRef]
- Manolis, A.A.; Manolis, T.A.; Melita, H.; Katsiki, N.; Manolis, A.S. Proton pump inhibitors and cardiovascular adverse effects: Real or surreal worries? Eur. J. Intern. Med. 2020, 72, 15–26. [Google Scholar] [CrossRef]
- Sun, S.; Cui, Z.; Zhou, M.; Li, R.; Li, H.; Zhang, S.; Ba, Y.; Cheng, G. Proton pump inhibitor monotherapy and the risk of cardiovascular events in patients with gastro-esophageal reflux disease: A meta-analysis. Neurogastroenterol. Motil. 2017, 29, e12926. [Google Scholar] [CrossRef]
- Xie, Y.; Bowe, B.; Yan, Y.; Xian, H.; Li, T.; Al-Aly, Z. Estimates of all cause mortality and cause specific mortality associated with proton pump inhibitors among US veterans: Cohort study. BMJ 2019, 365, l1580. [Google Scholar] [CrossRef]
- Pang, J.; Wu, Q.; Zhang, Z.; Zheng, T.Z.; Xiang, Q.; Zhang, P.; Liu, X.; Zhang, C.; Tan, H.; Huang, J.; et al. Efficacy and safety of clopidogrel only vs. clopidogrel added proton pump inhibitors in the treatment of patients with coronary heart disease after percutaneous coronary intervention: A systematic review and meta-analysis. Int. J. Cardiol. Heart Vasc. 2019, 23, 100317. [Google Scholar] [CrossRef] [PubMed]
- Charlot, M.; Ahlehoff, O.; Norgaard, M.L.; Jorgensen, C.H.; Sorensen, R.; Abildstrom, S.Z.; Hansen, P.R.; Madsen, J.K.; Kober, L.; Torp-Pedersen, C.; et al. Proton-pump inhibitors are associated with increased cardiovascular risk independent of clopidogrel use: A nationwide cohort study. Ann. Intern. Med. 2010, 153, 378–386. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Liu, F.; Chen, C.; Zhu, W.; Ma, J.; Hu, J.; Xu, J.; Hong, K. Real-World Relationship Between Proton Pump Inhibitors and Cerebro-Cardiovascular Outcomes Independent of Clopidogrel. Int. Heart J. 2019, 60, 910–918. [Google Scholar] [CrossRef]
- Goodman, S.G.; Clare, R.; Pieper, K.S.; Nicolau, J.C.; Storey, R.F.; Cantor, W.J.; Mahaffey, K.W.; Angiolillo, D.J.; Husted, S.; Cannon, C.P.; et al. Association of proton pump inhibitor use on cardiovascular outcomes with clopidogrel and ticagrelor: Insights from the platelet inhibition and patient outcomes trial. Circulation 2012, 125, 978–986. [Google Scholar] [CrossRef]
- Wang, Y.F.; Chen, Y.T.; Luo, J.C.; Chen, T.J.; Wu, J.C.; Wang, S.J. Proton-Pump Inhibitor Use and the Risk of First-Time Ischemic Stroke in the General Population: A Nationwide Population-Based Study. Am. J. Gastroenterol. 2017, 112, 1084–1093. [Google Scholar] [CrossRef]
- Shah, N.H.; LePendu, P.; Bauer-Mehren, A.; Ghebremariam, Y.T.; Iyer, S.V.; Marcus, J.; Nead, K.T.; Cooke, J.P.; Leeper, N.J. Proton Pump Inhibitor Usage and the Risk of Myocardial Infarction in the General Population. PLoS ONE 2015, 10, e0124653. [Google Scholar] [CrossRef]
- Batchelor, R.; Kumar, R.; Gilmartin-Thomas, J.F.M.; Hopper, I.; Kemp, W.; Liew, D. Systematic review with meta-analysis: Risk of adverse cardiovascular events with proton pump inhibitors independent of clopidogrel. Aliment. Pharmacol. Ther. 2018, 48, 780–796. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, D.L.; Cryer, B.L.; Contant, C.F.; Cohen, M.; Lanas, A.; Schnitzer, T.J.; Shook, T.L.; Lapuerta, P.; Goldsmith, M.A.; Laine, L.; et al. Clopidogrel with or without omeprazole in coronary artery disease. N. Engl. J. Med. 2010, 363, 1909–1917. [Google Scholar] [CrossRef]
- Shang, Y.S.; Zhong, P.Y.; Ma, Y.; Bai, N.; Niu, Y.; Wang, Z.L. Efficacy and Safety of Proton Pump Inhibitors in Patients with Coronary Artery Diseases Receiving Oral Antiplatelet Agents and/or Anticoagulants: A Systematic Review and Meta-Analysis. J. Cardiovasc. Pharmacol. 2022, 80, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Farhat, N.; Fortin, Y.; Haddad, N.; Birkett, N.; Mattison, D.R.; Momoli, F.; Wu Wen, S.; Krewski, D. Systematic review and meta-analysis of adverse cardiovascular events associated with proton pump inhibitors used alone or in combination with antiplatelet agents. Crit. Rev. Toxicol. 2019, 49, 215–261. [Google Scholar] [CrossRef]
- Shih, C.J.; Chen, Y.T.; Ou, S.M.; Li, S.Y.; Chen, T.J.; Wang, S.J. Proton pump inhibitor use represents an independent risk factor for myocardial infarction. Int. J. Cardiol. 2014, 177, 292–297. [Google Scholar] [CrossRef]
- Fowler, J.F.; Eubank, T.A.; Garey, K.W. Proton pump inhibitor effect on macrophage and neutrophil function: A systematic review. Front. Immunol. 2024, 15, 1477993. [Google Scholar] [CrossRef]
- Bruno, G.; Zaccari, P.; Rocco, G.; Scalese, G.; Panetta, C.; Porowska, B.; Pontone, S.; Severi, C. Proton pump inhibitors and dysbiosis: Current knowledge and aspects to be clarified. World J. Gastroenterol. 2019, 25, 2706–2719. [Google Scholar] [CrossRef]
- Clooney, A.G.; Bernstein, C.N.; Leslie, W.D.; Vagianos, K.; Sargent, M.; Laserna-Mendieta, E.J.; Claesson, M.J.; Targownik, L.E. A comparison of the gut microbiome between long-term users and non-users of proton pump inhibitors. Aliment. Pharmacol. Ther. 2016, 43, 974–984. [Google Scholar] [CrossRef]
- Mishiro, T.; Oka, K.; Kuroki, Y.; Takahashi, M.; Tatsumi, K.; Saitoh, T.; Tobita, H.; Ishimura, N.; Sato, S.; Ishihara, S.; et al. Oral microbiome alterations of healthy volunteers with proton pump inhibitor. J. Gastroenterol. Hepatol. 2018, 33, 1059–1066. [Google Scholar] [CrossRef]
- Yamamura, K.; Baba, Y.; Nakagawa, S.; Mima, K.; Miyake, K.; Nakamura, K.; Sawayama, H.; Kinoshita, K.; Ishimoto, T.; Iwatsuki, M.; et al. Human Microbiome Fusobacterium Nucleatum in Esophageal Cancer Tissue Is Associated with Prognosis. Clin. Cancer Res. 2016, 22, 5574–5581. [Google Scholar] [CrossRef]
- Willems, R.P.J.; Schut, M.C.; Kaiser, A.M.; Groot, T.H.; Abu-Hanna, A.; Twisk, J.W.R.; van Dijk, K.; Vandenbroucke-Grauls, C. Association of Proton Pump Inhibitor Use with Risk of Acquiring Drug-Resistant Enterobacterales. JAMA Netw. Open 2023, 6, e230470. [Google Scholar] [CrossRef]
- Willems, R.P.J.; van Dijk, K.; Ket, J.C.F.; Vandenbroucke-Grauls, C. Evaluation of the Association Between Gastric Acid Suppression and Risk of Intestinal Colonization with Multidrug-Resistant Microorganisms: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2020, 180, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Jump, R.L.; Pultz, M.J.; Donskey, C.J. Vegetative Clostridium difficile survives in room air on moist surfaces and in gastric contents with reduced acidity: A potential mechanism to explain the association between proton pump inhibitors and C. difficile-associated diarrhea? Antimicrob. Agents Chemother. 2007, 51, 2883–2887. [Google Scholar] [CrossRef] [PubMed]
- Loo, V.G.; Bourgault, A.M.; Poirier, L.; Lamothe, F.; Michaud, S.; Turgeon, N.; Toye, B.; Beaudoin, A.; Frost, E.H.; Gilca, R.; et al. Host and pathogen factors for Clostridium difficile infection and colonization. N. Engl. J. Med. 2011, 365, 1693–1703. [Google Scholar] [CrossRef] [PubMed]
- Inghammar, M.; Svanstrom, H.; Voldstedlund, M.; Melbye, M.; Hviid, A.; Molbak, K.; Pasternak, B. Proton-Pump Inhibitor Use and the Risk of Community-Associated Clostridium difficile Infection. Clin. Infect. Dis. 2021, 72, e1084–e1089. [Google Scholar] [CrossRef]
- Tleyjeh, I.M.; Bin Abdulhak, A.A.; Riaz, M.; Alasmari, F.A.; Garbati, M.A.; AlGhamdi, M.; Khan, A.R.; Al Tannir, M.; Erwin, P.J.; Ibrahim, T.; et al. Association between proton pump inhibitor therapy and clostridium difficile infection: A contemporary systematic review and meta-analysis. PLoS ONE 2012, 7, e50836. [Google Scholar] [CrossRef]
- Janarthanan, S.; Ditah, I.; Adler, D.G.; Ehrinpreis, M.N. Clostridium difficile-associated diarrhea and proton pump inhibitor therapy: A meta-analysis. Am. J. Gastroenterol. 2012, 107, 1001–1010. [Google Scholar] [CrossRef]
- Deshpande, A.; Pant, C.; Pasupuleti, V.; Rolston, D.D.; Jain, A.; Deshpande, N.; Thota, P.; Sferra, T.J.; Hernandez, A.V. Association between proton pump inhibitor therapy and Clostridium difficile infection in a meta-analysis. Clin. Gastroenterol. Hepatol. 2012, 10, 225–233. [Google Scholar] [CrossRef]
- Kwok, C.S.; Arthur, A.K.; Anibueze, C.I.; Singh, S.; Cavallazzi, R.; Loke, Y.K. Risk of Clostridium difficile infection with acid suppressing drugs and antibiotics: Meta-analysis. Am. J. Gastroenterol. 2012, 107, 1011–1019. [Google Scholar] [CrossRef]
- Arriola, V.; Tischendorf, J.; Musuuza, J.; Barker, A.; Rozelle, J.W.; Safdar, N. Assessing the Risk of Hospital-Acquired Clostridium Difficile Infection with Proton Pump Inhibitor Use: A Meta-Analysis. Infect. Control Hosp. Epidemiol. 2016, 37, 1408–1417. [Google Scholar] [CrossRef] [PubMed]
- Tariq, R.; Singh, S.; Gupta, A.; Pardi, D.S.; Khanna, S. Association of Gastric Acid Suppression with Recurrent Clostridium difficile Infection: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2017, 177, 784–791. [Google Scholar] [CrossRef] [PubMed]
- Trifan, A.; Stanciu, C.; Girleanu, I.; Stoica, O.C.; Singeap, A.M.; Maxim, R.; Chiriac, S.A.; Ciobica, A.; Boiculese, L. Proton pump inhibitors therapy and risk of Clostridium difficile infection: Systematic review and meta-analysis. World J. Gastroenterol. 2017, 23, 6500–6515. [Google Scholar] [CrossRef] [PubMed]
- Cao, F.; Chen, C.X.; Wang, M.; Liao, H.R.; Wang, M.X.; Hua, S.Z.; Huang, B.; Xiong, Y.; Zhang, J.Y.; Xu, Y.L. Updated meta-analysis of controlled observational studies: Proton-pump inhibitors and risk of Clostridium difficile infection. J. Hosp. Infect. 2018, 98, 4–13. [Google Scholar] [CrossRef]
- D’Silva, K.M.; Mehta, R.; Mitchell, M.; Lee, T.C.; Singhal, V.; Wilson, M.G.; McDonald, E.G. Proton pump inhibitor use and risk for recurrent Clostridioides difficile infection: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2021, 27, 697–703. [Google Scholar] [CrossRef]
- Tleyjeh, I.M.; Abdulhak, A.B.; Riaz, M.; Garbati, M.A.; Al-Tannir, M.; Alasmari, F.A.; Alghamdi, M.; Khan, A.R.; Erwin, P.J.; Sutton, A.J.; et al. The association between histamine 2 receptor antagonist use and Clostridium difficile infection: A systematic review and meta-analysis. PLoS ONE 2013, 8, e56498. [Google Scholar] [CrossRef]
- Moayyedi, P.; Eikelboom, J.W.; Bosch, J.; Connolly, S.J.; Dyal, L.; Shestakovska, O.; Leong, D.; Anand, S.S.; Stork, S.; Branch, K.R.H.; et al. Safety of Proton Pump Inhibitors Based on a Large, Multi-Year, Randomized Trial of Patients Receiving Rivaroxaban or Aspirin. Gastroenterology 2019, 157, 682–691.e2. [Google Scholar] [CrossRef]
- Lin, C.Y.; Cheng, H.T.; Kuo, C.J.; Lee, Y.S.; Sung, C.M.; Keidan, M.; Rao, K.; Kao, J.Y.; Hsieh, S.Y. Proton Pump Inhibitor-Induced Gut Dysbiosis Increases Mortality Rates for Patients with Clostridioides difficile Infection. Microbiol. Spectr. 2022, 10, e0048622. [Google Scholar] [CrossRef]
- Barletta, J.F.; Sclar, D.A. Proton pump inhibitors increase the risk for hospital-acquired Clostridium difficile infection in critically ill patients. Crit. Care 2014, 18, 714. [Google Scholar] [CrossRef]
- Seo, S.I.; You, S.C.; Park, C.H.; Kim, T.J.; Ko, Y.S.; Kim, Y.; Yoo, J.J.; Kim, J.; Shin, W.G. Comparative risk of Clostridium difficile infection between proton pump inhibitors and histamine-2 receptor antagonists: A 15-year hospital cohort study using a common data model. J. Gastroenterol. Hepatol. 2020, 35, 1325–1330. [Google Scholar] [CrossRef]
- Bavishi, C.; Dupont, H.L. Systematic review: The use of proton pump inhibitors and increased susceptibility to enteric infection. Aliment. Pharmacol. Ther. 2011, 34, 1269–1281. [Google Scholar] [CrossRef]
- Leonard, J.; Marshall, J.K.; Moayyedi, P. Systematic review of the risk of enteric infection in patients taking acid suppression. Am. J. Gastroenterol. 2007, 102, 2047–2056. [Google Scholar] [CrossRef] [PubMed]
- Hafiz, R.A.; Wong, C.; Paynter, S.; David, M.; Peeters, G. The Risk of Community-Acquired Enteric Infection in Proton Pump Inhibitor Therapy: Systematic Review and Meta-analysis. Ann. Pharmacother. 2018, 52, 613–622. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.J.; Lin, C.Y.; Chen, C.W.; Hsu, C.Y.; Hsieh, S.Y.; Chiu, C.T.; Lin, W.R. Risk of Enteric Infection in Patients with Gastric Acid Supressive Drugs: A Population-Based Case-Control Study. J. Pers. Med. 2021, 11, 1063. [Google Scholar] [CrossRef]
- Vilcu, A.M.; Sabatte, L.; Blanchon, T.; Souty, C.; Maravic, M.; Lemaitre, M.; Steichen, O.; Hanslik, T. Association Between Acute Gastroenteritis and Continuous Use of Proton Pump Inhibitors During Winter Periods of Highest Circulation of Enteric Viruses. JAMA Netw. Open 2019, 2, e1916205. [Google Scholar] [CrossRef]
- Lo, W.K.; Chan, W.W. Proton pump inhibitor use and the risk of small intestinal bacterial overgrowth: A meta-analysis. Clin. Gastroenterol. Hepatol. 2013, 11, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Su, T.; Lai, S.; Lee, A.; He, X.; Chen, S. Meta-analysis: Proton pump inhibitors moderately increase the risk of small intestinal bacterial overgrowth. J. Gastroenterol. 2018, 53, 27–36. [Google Scholar] [CrossRef]
- Deshpande, A.; Pasupuleti, V.; Thota, P.; Pant, C.; Mapara, S.; Hassan, S.; Rolston, D.D.; Sferra, T.J.; Hernandez, A.V. Acid-suppressive therapy is associated with spontaneous bacterial peritonitis in cirrhotic patients: A meta-analysis. J. Gastroenterol. Hepatol. 2013, 28, 235–242. [Google Scholar] [CrossRef]
- Xu, H.B.; Wang, H.D.; Li, C.H.; Ye, S.; Dong, M.S.; Xia, Q.J.; Zhang, A.Q.; Pan, K.; Ge, X.L.; Dong, J.H. Proton pump inhibitor use and risk of spontaneous bacterial peritonitis in cirrhotic patients: A systematic review and meta-analysis. Genet. Mol. Res. 2015, 14, 7490–7501. [Google Scholar] [CrossRef]
- Yu, T.; Tang, Y.; Jiang, L.; Zheng, Y.; Xiong, W.; Lin, L. Proton pump inhibitor therapy and its association with spontaneous bacterial peritonitis incidence and mortality: A meta-analysis. Dig. Liver Dis. 2016, 48, 353–359. [Google Scholar] [CrossRef]
- Zhong, H.J.; Lin, D.; Lu, Z.Y.; Yang, W.Y.; Chen, Y. Use of gastric-acid suppressants may be a risk factor for enteric peritonitis in patients undergoing peritoneal dialysis: A meta-analysis. J. Clin. Pharm. Ther. 2019, 44, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Dam, G.; Vilstrup, H.; Watson, H.; Jepsen, P. Proton pump inhibitors as a risk factor for hepatic encephalopathy and spontaneous bacterial peritonitis in patients with cirrhosis with ascites. Hepatology 2016, 64, 1265–1272. [Google Scholar] [CrossRef]
- Nardelli, S.; Gioia, S.; Ridola, L.; Farcomeni, A.; Merli, M.; Riggio, O. Proton Pump Inhibitors Are Associated With Minimal and Overt Hepatic Encephalopathy and Increased Mortality in Patients with Cirrhosis. Hepatology 2019, 70, 640–649. [Google Scholar] [CrossRef]
- De Roza, M.A.; Kai, L.; Kam, J.W.; Chan, Y.H.; Kwek, A.; Ang, T.L.; Hsiang, J.C. Proton pump inhibitor use increases mortality and hepatic decompensation in liver cirrhosis. World J. Gastroenterol. 2019, 25, 4933–4944. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.F.; Chen, M.H.; Wang, Y.P.; Chu, C.J.; Huang, Y.H.; Lin, H.C.; Hou, M.C.; Lee, F.Y.; Su, T.P.; Lu, C.L. Proton Pump Inhibitors Increase Risk for Hepatic Encephalopathy in Patients with Cirrhosis in A Population Study. Gastroenterology 2017, 152, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.J.; Cao, Z.X.; Li, Y.; Feng, S.Y. Proton pump inhibitor use increases hepatic encephalopathy risk: A systematic review and meta-analysis. World J. Gastroenterol. 2019, 25, 2675–2682. [Google Scholar] [CrossRef]
- Xun, X.; Yin, Q.; Fu, Y.; He, X.; Dong, Z. Proton Pump Inhibitors and the Risk of Community-Acquired Pneumonia: An Updated Meta-analysis. Ann. Pharmacother. 2022, 56, 524–532. [Google Scholar] [CrossRef]
- Lambert, A.A.; Lam, J.O.; Paik, J.J.; Ugarte-Gil, C.; Drummond, M.B.; Crowell, T.A. Risk of community-acquired pneumonia with outpatient proton-pump inhibitor therapy: A systematic review and meta-analysis. PLoS ONE 2015, 10, e0128004. [Google Scholar] [CrossRef]
- Marchina, S.; Doros, G.; Modak, J.; Helenius, J.; Aycock, D.M.; Kumar, S. Acid-suppressive medications and risk of pneumonia in acute stroke patients: A systematic review and meta-analysis. J. Neurol. Sci. 2019, 400, 122–128. [Google Scholar] [CrossRef]
- Herzig, S.J.; Howell, M.D.; Ngo, L.H.; Marcantonio, E.R. Acid-suppressive medication use and the risk for hospital-acquired pneumonia. JAMA 2009, 301, 2120–2128. [Google Scholar] [CrossRef]
- Eom, C.S.; Jeon, C.Y.; Lim, J.W.; Cho, E.G.; Park, S.M.; Lee, K.S. Use of acid-suppressive drugs and risk of pneumonia: A systematic review and meta-analysis. Can. Med. Assoc. J. 2011, 183, 310–319. [Google Scholar] [CrossRef]
- Bashar, F.R.; Manuchehrian, N.; Mahmoudabadi, M.; Hajiesmaeili, M.R.; Torabian, S. Effects of ranitidine and pantoprazole on ventilator-associated pneumonia: A randomized double-blind clinical trial. Tanaffos 2013, 12, 16–21. [Google Scholar] [PubMed]
- Pranata, R.; Huang, I.; Lawrensia, S.; Henrina, J.; Lim, M.A.; Lukito, A.A.; Kuswardhani, R.A.T.; Wibawa, I.D.N. Proton pump inhibitor on susceptibility to COVID-19 and its severity: A systematic review and meta-analysis. Pharmacol. Rep. 2021, 73, 1642–1649. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.B.; Kim, J.H.; Wolf, B.J. Acid suppressant use in association with incidence and severe outcomes of COVID-19: A systematic review and meta-analysis. Eur. J. Clin. Pharmacol. 2022, 78, 383–391. [Google Scholar] [CrossRef]
- Zhang, M.L.; Fan, Y.X.; Meng, R.; Cai, W.K.; Yin, S.J.; Zhou, T.; Huang, Y.H.; Wang, P.; Jiang, F.F.; Yang, M.; et al. Proton Pump Inhibitors and Cancer Risk: An Umbrella Review and Meta-analysis of Observational Studies. Am. J. Clin. Oncol. 2022, 45, 475–485. [Google Scholar] [CrossRef]
- Guo, H.; Zhang, R.; Zhang, P.; Chen, Z.; Hua, Y.; Huang, X.; Li, X. Association of proton pump inhibitors with gastric and colorectal cancer risk: A systematic review and meta-analysis. Front. Pharmacol. 2023, 14, 1129948. [Google Scholar] [CrossRef]
- Zhou, W.; Chen, X.; Fan, Q.; Yu, H.; Jiang, W. Using proton pump inhibitors increases the risk of hepato-biliary-pancreatic cancer. A systematic review and meta-analysis. Front. Pharmacol. 2022, 13, 979215. [Google Scholar] [CrossRef]
- Laoveeravat, P.; Thavaraputta, S.; Vutthikraivit, W.; Suchartlikitwong, S.; Mingbunjerdsuk, T.; Motes, A.; Nugent, K.; Rakvit, A.; Islam, E.; Islam, S. Proton pump inhibitors and histamine-2 receptor antagonists on the risk of pancreatic cancer: A systematic review and meta-analysis. QJM 2020, 113, 100–107. [Google Scholar] [CrossRef]
- Nochaiwong, S.; Ruengorn, C.; Awiphan, R.; Koyratkoson, K.; Chaisai, C.; Noppakun, K.; Chongruksut, W.; Thavorn, K. The association between proton pump inhibitor use and the risk of adverse kidney outcomes: A systematic review and meta-analysis. Nephrol. Dial. Transplant. 2018, 33, 331–342. [Google Scholar] [CrossRef]
- Blank, M.L.; Parkin, L.; Paul, C.; Herbison, P. A nationwide nested case-control study indicates an increased risk of acute interstitial nephritis with proton pump inhibitor use. Kidney Int. 2014, 86, 837–844. [Google Scholar] [CrossRef]
- Yang, Y.; George, K.C.; Shang, W.F.; Zeng, R.; Ge, S.W.; Xu, G. Proton-pump inhibitors use, and risk of acute kidney injury: A meta-analysis of observational studies. Drug Des. Dev. Ther. 2017, 11, 1291–1299. [Google Scholar] [CrossRef]
- Ang, S.P.; Chia, J.E.; Valladares, C.; Patel, S.; Gewirtz, D.; Iglesias, J. Association between Proton Pump Inhibitor Use and Risk of Incident Chronic Kidney Disease: Systematic Review and Meta-Analysis. Biomedicines 2024, 12, 1414. [Google Scholar] [CrossRef]
- Zhang, Y.; Deng, D.; Zhang, R.; Yi, J.; Dong, J.; Sha, L. Relationship between Proton Pump Inhibitors and Adverse Effects in Hemodialysis Patients: A Systematic Review and Meta-Analysis. Kidney Blood Press. Res. 2022, 47, 545–555. [Google Scholar] [CrossRef] [PubMed]
- de Wilde, M.C.; Vellas, B.; Girault, E.; Yavuz, A.C.; Sijben, J.W. Lower brain and blood nutrient status in Alzheimer’s disease: Results from meta-analyses. Alzheimer’s Dement. 2017, 3, 416–431. [Google Scholar] [CrossRef]
- Tai, S.Y.; Chien, C.Y.; Wu, D.C.; Lin, K.D.; Ho, B.L.; Chang, Y.H.; Chang, Y.P. Risk of dementia from proton pump inhibitor use in Asian population: A nationwide cohort study in Taiwan. PLoS ONE 2017, 12, e0171006. [Google Scholar] [CrossRef]
- Gomm, W.; von Holt, K.; Thome, F.; Broich, K.; Maier, W.; Fink, A.; Doblhammer, G.; Haenisch, B. Association of Proton Pump Inhibitors With Risk of Dementia: A Pharmacoepidemiological Claims Data Analysis. JAMA Neurol. 2016, 73, 410–416. [Google Scholar] [CrossRef]
- Song, Y.Q.; Li, Y.; Zhang, S.L.; Gao, J.; Feng, S.Y. Proton pump inhibitor use does not increase dementia and Alzheimer’s disease risk: An updated meta-analysis of published studies involving 642305 patients. PLoS ONE 2019, 14, e0219213. [Google Scholar] [CrossRef]
- Li, M.; Luo, Z.; Yu, S.; Tang, Z. Proton pump inhibitor use and risk of dementia: Systematic review and meta-analysis. Medicine 2019, 98, e14422. [Google Scholar] [CrossRef]
- Desai, M.; Nutalapati, V.; Srinivasan, S.; Fathallah, J.; Dasari, C.; Chandrasekhar, V.T.; Mohammad, B.; Kohli, D.; Vaezi, M.; Katz, P.O.; et al. Proton pump inhibitors do not increase the risk of dementia: A systematic review and meta-analysis of prospective studies. Dis. Esophagus 2020, 33, doaa041. [Google Scholar] [CrossRef]
- Khan, M.A.; Yuan, Y.; Iqbal, U.; Kamal, S.; Khan, M.; Khan, Z.; Lee, W.M.; Howden, C.W. No Association Linking Short-Term Proton Pump Inhibitor Use to Dementia: Systematic Review and Meta-analysis of Observational Studies. Am. J. Gastroenterol. 2020, 115, 671–678. [Google Scholar] [CrossRef]
- Wang, H.; Tian, L.; Yan, X. No association between acid suppressant use and risk of dementia: An updated meta-analysis. Eur. J. Clin. Pharmacol. 2022, 78, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.W.; Strandell, J. Myopathy including polymyositis: A likely class adverse effect of proton pump inhibitors? Eur. J. Clin. Pharmacol. 2006, 62, 473–479. [Google Scholar] [CrossRef] [PubMed]
- Colmenares, E.W.; Pappas, A.L. Proton Pump Inhibitors: Risk for Myopathy? Ann. Pharmacother. 2017, 51, 66–71. [Google Scholar] [CrossRef]
- Masclee, G.M.; Coloma, P.M.; Kuipers, E.J.; Sturkenboom, M.C. Increased risk of microscopic colitis with use of proton pump inhibitors and non-steroidal anti-inflammatory drugs. Am. J. Gastroenterol. 2015, 110, 749–759. [Google Scholar] [CrossRef]
- Capurso, G.; Marignani, M.; Attilia, F.; Milione, M.; Colarossi, C.; Zampaletta, C.; Di Giulio, E.; Delle Fave, G. Lansoprazole-induced microscopic colitis: An increasing problem? Results of a prospecive case-series and systematic review of the literature. Dig. Liver Dis. 2011, 43, 380–385. [Google Scholar] [CrossRef]
- Bonderup, O.K.; Nielsen, G.L.; Dall, M.; Pottegard, A.; Hallas, J. Significant association between the use of different proton pump inhibitors and microscopic colitis: A nationwide Danish case-control study. Aliment. Pharmacol. Ther. 2018, 48, 618–625. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.W.; Xu, R.H.; Chen, D. Drug Exposure and Risk of Microscopic Colitis: A Systematic Review and Meta-Analysis. Dig. Dis. 2023, 41, 217–226. [Google Scholar] [CrossRef]
- Tarar, Z.I.; Farooq, U.; Gandhi, M.; Kamal, F.; Tarar, M.F.; Tahan, V.; Chela, H.K.; Daglilar, E. Are Drugs Associated with Microscopic Colitis? A Systematic Review and Meta-Analysis. Diseases 2022, 11, 6. [Google Scholar] [CrossRef]
- Leszcynski, L.; Bente, J. Development and Implementation of a Pharmacist-Led Proton Pump Inhibitor Deprescribing Algorithm in a Geriatric Ambulatory Office. Sr. Care Pharm. 2023, 38, 105–112. [Google Scholar] [CrossRef]
- Lee, T.C.; McDonald, E.G. Deprescribing Proton Pump Inhibitors: Overcoming Resistance. JAMA Intern. Med. 2020, 180, 571–573. [Google Scholar] [CrossRef]
- Tapper, E.B.; Zhao, Z.; Parikh, N.D. An Emulated Clinical Trial of Deprescribing Proton Pump Inhibitors in Patients with Cirrhosis. Am. J. Gastroenterol. 2024, 119, 203–205. [Google Scholar] [CrossRef]
- Maideen, N.M.P. Adverse Effects Associated with Long-Term Use of Proton Pump Inhibitors. Chonnam Med. J. 2023, 59, 115–127. [Google Scholar] [CrossRef] [PubMed]
- By the 2023 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2023 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J. Am. Geriatr. Soc. 2023, 71, 2052–2081. [Google Scholar] [CrossRef]
- Jones, K.F.; Stolzmann, K.; Wormwood, J.; Pendergast, J.; Miller, C.J.; Still, M.; Bokhour, B.G.; Hanlon, J.; Simon, S.R.; Rosen, A.K.; et al. Patient-Directed Education to Promote Deprescribing: A Nonrandomized Clinical Trial. JAMA Intern. Med. 2024, 184, 1339–1346. [Google Scholar] [CrossRef] [PubMed]
- Buzancic, I.; Kummer, I.; Drzaic, M.; Ortner Hadziabdic, M. Community-based pharmacists’ role in deprescribing: A systematic review. Br. J. Clin. Pharmacol. 2022, 88, 452–463. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.; Perrella, L.; Scotti, S.; Olmastroni, E.; Galimberti, F.; Ardoino, I.; Orlando, V.; Menditto, E.; Franchi, C.; Casula, M. Approaches to Deprescribing Proton Pump Inhibitors in Clinical Practice: A Systematic Review. J. Clin. Med. 2024, 13, 6283. [Google Scholar] [CrossRef]
- Schulthess-Lisibach, A.E.; Luthold, R.V.; Tombez, C.; Weir, K.R.; Zangger, M.; Chan, S.; Jenal, F.; Roumet, M.; Mattmann, Y.; Bieri, C.; et al. DepRescribing inapprOpriate Proton Pump InhibiTors (DROPIT): Study protocol of a cluster-randomised controlled trial in Swiss primary care. BMJ Open 2025, 15, e094495. [Google Scholar] [CrossRef]
| Common Indications for PPI Use | Recommendations |
|---|---|
| Uncomplicated GERD (NERD or non-severe EE) |
|
| Complicated GERD (Severe EE or BE) |
|
| Eosinophilic esophagitis |
|
| PUD |
|
| Chronic NSAID or antithrombotic use (primary prevention) |
|
| Upper GI bleed |
|
| SUP in critically ill patients |
|
| Dyspepsia |
|
| PPI | Standard Dose | Low Dose | High Dose | Metabolism |
|---|---|---|---|---|
| Dexlansoprazole (Dexilant), Capsule | 30–60 mg once daily | 30 mg once daily | 60 mg twice daily | CYP2C19, CYP3A4 |
| Esomeprazole (Nexium), IV, Capsule, EC Tablet, Available OTC | 20–40 mg once daily | 20 mg once daily | 40 mg twice daily | CYP2C19, CYP3A4 |
| Lansoprazole (Prevacid), Capsule, Tablet, Available OTC | 30 mg once daily | 15 mg once daily | 30 mg twice daily | CYP2C19, CYP3A4 |
| Omeprazole (Prilosec), Capsule, Tablet, Available OTC | 20 mg once daily | 10 mg once daily | 20 mg twice daily | CYP2C19, CYP3A4 |
| Pantoprazole (Protonix), IV, Tablet, Suspension | 40 mg once daily | 20 mg once daily | 40 mg twice daily | CYP2C19, CYP3A4 |
| Rabeprazole (Aciphex), Tablet, Sprinkle Capsule | 20 mg once daily | 10 mg once daily | 20 mg twice daily | CYP3A4, CYP2C19 |
| Condition | Population | SR-MA Details | Effect Estimate (Ratio [95% CI]) | Heterogeneity (I2) | Ref. |
|---|---|---|---|---|---|
| Vitamin B12 Deficiency | General Population | 25 observational studies, n = 30,922 | ↑ OR 1.42 (1.16–1.73) | 54% | [46] |
| Iron Deficiency Anemia | General Population | 14 observational studies, n = 76,089 | ↑ RR 2.56 (1.43–4.61) | 99% | [50] |
| Hypomagnesemia | General Population | 16 observational studies, n = 131,507 | ↑ OR 1.71 (1.33–2.19) | 88% | [57] |
| Fracture Risk | General Population | 24 observational studies, n = 2,103,800 | ↑ RR 1.20 (1.14–1.28) | 77% | [68] |
| Cardiovascular Events | Patients with GERD | 16 RCTs, n = 7540 | ↑ RR 1.70 (1.13–2.56) | 0% | [75] |
| Cardiovascular Events | Patients taking clopidogrel | 15 RCTs, n = 50,366 | ↑ RR 1.22 (1.14–1.30) | Not Reported | [77] |
| Stroke | Patients taking clopidogrel | 15 RCTs, n = 50,366 | ↑ RR 1.39 (1.32–1.49) | Not Reported | [77] |
| Cardiovascular Events | Patients with CAD | 19 RCTs, n = 43,943 | ↔ RR 1.05 (0.96–1.15) | 0% | [85] |
| All-cause Mortality | Patients with CAD | 19 RCTs, n = 43,943 | ↔ RR 0.84 (0.69–1.01) | 0% | [85] |
| MDRO Colonization | General Population | 26 observational studies, n = 29,382 | ↑ OR 1.74 (1.40–2.16) | 68% | [94] |
| CDI, Incident | General Population | 42 observational studies, n = 313,000 | ↑ OR 1.74 (1.47–2.85) | 85% | [101] |
| CDI, Recurrent | General Population | 42 observational studies, n = 313,000 | ↑ OR 2.51 (1.16–5.44) | 78% | [101] |
| CDI, Recurrent | Patients with prior CDI | 16 observational studies, n = 57,477 | ↑ OR 1.69 (1.46–1.96) | 56% | [106] |
| SIBO | General Population | 19 observational studies, n = 7055 | ↑ OR 1.71 (1.20–2.43) | 84% | [118] |
| SBP | Patients with cirrhosis | 17 observational studies, n = 8204 | ↑ OR 2.17 (1.46–3.23) | 86% | [120] |
| Hepatic Encephalopathy | Patients with cirrhosis | 7 observational studies, n = 4574 | ↑ OR 1.50 (1.25–1.75) | 14% | [127] |
| CAP | General Population | 13 observational studies, n = 2,098,804 | ↑ OR 1.37 (1.22–1.53) | 88% | [128] |
| Severe COVID-19 | General Population | 12 observational studies, n = 290,455 | ↑ OR 1.85 (1.13–3.03) | 90% | [134] |
| Gastric Cancer | General Population | 24 observational studies, n = 8,066,349 | ↑ RR 1.82 (1.46–2.29) | 95% | [137] |
| Colorectal Cancer | General Population | 24 observational studies, n = 8,066,349 | ↔ RR 1.22 (0.95–1.55) | 97% | [137] |
| Hepatocellular Carcinoma | General Population | 24 observational studies, n = 2,741,853 | ↑ OR 1.69 (1.30–2.20) | 94% | [138] |
| Biliary Tract Cancers | General Population | 24 observational studies, n = 2,741,853 | ↑ OR 1.79 (1.63–1.97) | 42% | [138] |
| Pancreatic Cancers | General Population | 24 observational studies, n = 2,741,853 | ↑ OR 1.61 (1.23–2.11) | 99% | [138] |
| AKI | General Population | 7 observational studies, n = 2,404,236 | ↑ RR 1.61 (1.16–2.22) | 98% | [142] |
| CKD | General Population | 12 observational studies and 1 RCT, n = 1,144,056 | ↑ HR 1.26 (1.16–1.38) | 87% | [143] |
| Dementia | General Population | 16 observational studies and 1 RCT, n = 1,251,562 | ↔ HR 0.98 (0.85–1.13) | 99% | [152] |
| Microscopic Colitis | General Population | 13 observational studies, n = 304,482 | ↑OR 2.65 (1.81–3.50) | 98% | [159] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peyton-Navarrete, A.; Nguyen, M.H.C.; FakhriRavari, A. Prescribing Responsibly: Navigating the Tides of Deprescribing in Proton Pump Inhibitor Stewardship. Pharmacoepidemiology 2025, 4, 15. https://doi.org/10.3390/pharma4030015
Peyton-Navarrete A, Nguyen MHC, FakhriRavari A. Prescribing Responsibly: Navigating the Tides of Deprescribing in Proton Pump Inhibitor Stewardship. Pharmacoepidemiology. 2025; 4(3):15. https://doi.org/10.3390/pharma4030015
Chicago/Turabian StylePeyton-Navarrete, Anna, Minh Hien Chau Nguyen, and Alireza FakhriRavari. 2025. "Prescribing Responsibly: Navigating the Tides of Deprescribing in Proton Pump Inhibitor Stewardship" Pharmacoepidemiology 4, no. 3: 15. https://doi.org/10.3390/pharma4030015
APA StylePeyton-Navarrete, A., Nguyen, M. H. C., & FakhriRavari, A. (2025). Prescribing Responsibly: Navigating the Tides of Deprescribing in Proton Pump Inhibitor Stewardship. Pharmacoepidemiology, 4(3), 15. https://doi.org/10.3390/pharma4030015






