Abstract
Heart disease and cancer are the main causes of morbidity and mortality worldwide. As the number of cancer survivors increases, cardiotoxicity associated with cancer treatment has become a major concern as it presents a substantial challenge in the follow-up of these patients. Here, we aimed to map the clinical indicators for cardiovascular risk in adult patients undergoing chemotherapy. A scoping review protocol adhering to the PRISMA-P statement and in accordance with the JBI guidelines will be conducted. Cochrane Library, MEDLINE/PubMed, Cochrane Library, EMBASE, Scopus, Web of Science, and PsycINFO as well as register sites such as ClinicalTrials.gov and WHO-ICTRP will be searched. Additional sources, including Google Scholar, The British Library, and medRXiv, will also be searched, with no date or idiom restrictions. A combination of subject headings, MeSH terms, Emtree terms, CINAHL Headings, and APA Thesaurus, using the Boolean terms AND/OR, will be performed. In addition, two independent researchers will conduct the overall steps of this review. The results will be presented via narrative summaries, considering the types of clinical indicators. To the best of our knowledge, this will be the first scoping review in the cardio-oncology field to map, via a rigorous review method, the clinical indicators for cardiovascular risk in adult cancer patients receiving chemotherapy.
1. Introduction
Heart disease and cancer are the main causes of morbidity and mortality worldwide [1]. In this scenario, the prognosis of cancer patients has developed significantly in recent decades, mainly due to advances in therapy and the investigation of new drugs, as well as the use of complex multi-drug regimens and multiple treatment modalities, which have resulted in improvements in mortality rates and 5-year survival rates in these patients [2,3,4,5]. Despite such advancements, cardiotoxicity associated with cancer treatment has become a major concern and presents a substantial challenge in the follow-up of these patients [6].
Cardiotoxicity in cancer patients undergoing chemotherapy is most commonly characterized by an asymptomatic decrease in the left ventricular ejection fraction (LVEF), but it can take many forms, including congestive heart failure (CHF), hypertension, arrhythmias, cardiac ischemia, venous thromboembolism, and pericardial and valvular diseases [7,8,9].
Recently, the term cardio-oncology has emerged in the scientific literature as an interdisciplinary concept in the specialized medical field and is used to indicate cardiotoxicity during the treatment of malignant diseases [10,11,12,13]. However, these interdisciplinary fields have concentrated efforts especially on treating adverse effects rather than on their prevention [8,9].
The most recent World Health Organization (WHO) data show that cancer incidence and cancer mortality are second only to cardiovascular disease, which is still the leading cause of mortality in the world [14]. In addition, cardiovascular diseases and cancer are, in isolation, the main causes of mortality worldwide. The literature has shown that, due to advances in oncological therapy, cardiovascular diseases in cancer patients are increasingly frequent and are events of concern [15]. Progress in oncological treatment has also resulted in greater exposure of patients to cardiovascular risk factors and chemotherapy, which favors cardiotoxicity [16,17]. It is worth noting that the onset of a cardiovascular complication can determine the interruption of chemotherapy treatment and compromise cure or even cancer control [18].
Considering the toxic effects of chemotherapy on the cardiovascular system, with emphasis on the increased risk of developing hypertension, venous and arterial thromboembolic events, pulmonary hypertension, vasospasm, atherosclerosis, decline in the left ventricular ejection fraction, congestive heart failure, arrhythmia, myocarditis, pericardial disease, and others, it is clear that further studies are needed to synthesize and better understand what the clinical indicators are of cardiovascular risk for these cancer patients. The identification of the risks that can predict the event is crucial and will allow for the design of new studies that address the prevention of cardiovascular events [11,12,13].
Hence, the aim of this study is to map the clinical indicators for cardiovascular risk in adult patients undergoing chemotherapy.
2. Methods
2.1. Study Design
This is a scoping review protocol (ScR) that has high compliance with the JBI Manual for Evidence Synthesis [19] and will be reported in line with the PRISMA extension for scoping reviews checklist—PRISMA-ScR [20].
One of the main reasons for conducting scoping reviews is that, unlike other reviews that tend to address precise questions with predefined sets of outcomes, ScR is very useful for mapping the key concepts underlying a topic of interest [19]. In addition, one study pointed out that the three most common reasons for conducting an ScR were to explore the extent of the literature, map and synthesize evidence, and illuminate future research [21]. According to Munn et al. [22], the indications for ScR include, (I) as a precursor to a systematic review, (II) the identification of the available evidence in an area, (III) the identification and focus on the literature gaps, (IV) the clarification of the key concepts/definitions, (V) the evaluation of the ways the research is carried out on a certain topic/field, and (VI) the identification of the characteristics/factors underlying a concept [23].
The nine steps of the ScR include: (1) elaborating the research objective/research question; (2) establishing the inclusion criteria in accordance with the objective/research question; (3) planning the searching strategy, selecting the studies, mapping the data, and presenting the results; (4) designing a clear and reproducible search strategy; (5) selecting the studies; (6) extracting data; (7) evaluating the evidence; (8) presenting the evidence; and (9) summarizing the results in accordance with the ScR objective, drawing conclusions [19].
This ScR protocol has been registered in the Open Science Framework under ID: osf.io/gdw3c.
2.2. Research Question
The research question was constructed using the PCC (Population, Concept, and Context) search acronym [21], and was employed to identify the main concepts described as follows: Population/Problem—adult patients ≥18 years of age diagnosed with malignancy; Concept—clinical indicators of cardiovascular risk [24]; Context—under chemotherapy.
After applying the acronym PCC [21], the following research question arose: “What clinical indicators can predict cardiovascular risk in adult patients undergoing chemotherapy?”.
2.3. Searching for the Evidence
Cochrane Library, MEDLINE/PubMed, Cochrane Library, EMBASE, Scopus, Web of Science, and PsycINFO, in addition to register sites such as ClinicalTrials.gov and WHO ICTRP will be searched. Additional sources, including Google Scholar, The British Library-UK, and medRXiv, will also be searched, with no date or idiom restrictions. A combination of subject headings, for instance, MeSH terms, Emtree terms, and PsycINFO APA Thesaurus, as well as their synonyms (keywords) using the Boolean terms AND/OR [25], will be performed. Moreover, the search will be carried out using the identified descriptors and, in a broader sense, without database filters so that significant samples are preserved and the risk of losses reduced. Additionally, the list of final references included in the primary studies will be manually analyzed in order to find relevant studies to be added. There are no publication date or idiom restrictions. In addition, two independent researchers will conduct the overall steps of this scoping review.
Following the PCC acronym, a preliminary search strategy was developed for MEDLINE/PubMed and is shown in (Table 1), which will later be adjusted for each database.

Table 1.
Search strategy in MEDLINE/PubMed.
2.4. Selecting Evidence
For the inclusion criteria, we established that all primary studies will be included, as well as the gray literature related to the clinical indicators that can predict cardiovascular risk in adult patients undergoing chemotherapy. Qualitative studies and experimental studies conducted in animal models, in vivo and ex vivo, on this topic will be excluded.
It should be noted that the evaluation of duplicate records in databases and additional sources will be carried out in EndNote web. The retrieved articles will be exported directly to the Rayyan™ app [26] for screening and selection. Initially, titles and abstracts will be independently assessed by two researchers (JG and KZN) on the Rayyan™ app. Subsequently, the same two researchers will evaluate the full-text articles for inclusion/exclusion. In case of disagreements, a third reviewer, an expert in review studies (LCLJ), will resolve the inconsistencies regarding the eligibility of the articles.
2.5. Collating Evidence
Data extraction will be performed using previously published forms [27,28,29,30] and will be done by the same two researchers (JG and KZN). The expected completion date for ScR is August 2023. Data to be charted include (a) study characteristics and objectives, (b) study type, (c) sampling or population, (d) exposure, (e) methodological characteristics, (f) recruitment, (g) measurements, (h) follow-up, (i) primary/secondary outcomes, (j) results, (k) clinical and epidemiological significance, and (l) final considerations/implications/conclusions [27,28,29,30].
2.6. Analyzing Evidence
The retrieved studies will be classified in accordance with the Center for Evidence-Based Medicine based on the study design hierarchy that classifies studies into five hierarchies (1A, 1B, 1C; 2A, 2B, 2C; 3A, 3B, 4, and 5) [31].
The critical appraisal of the studies regarding the risk of bias will not be addressed since this is an ScR that aims to map and extend the literature rather than a methodological evaluation of the evidence, as in systematic reviews [19].
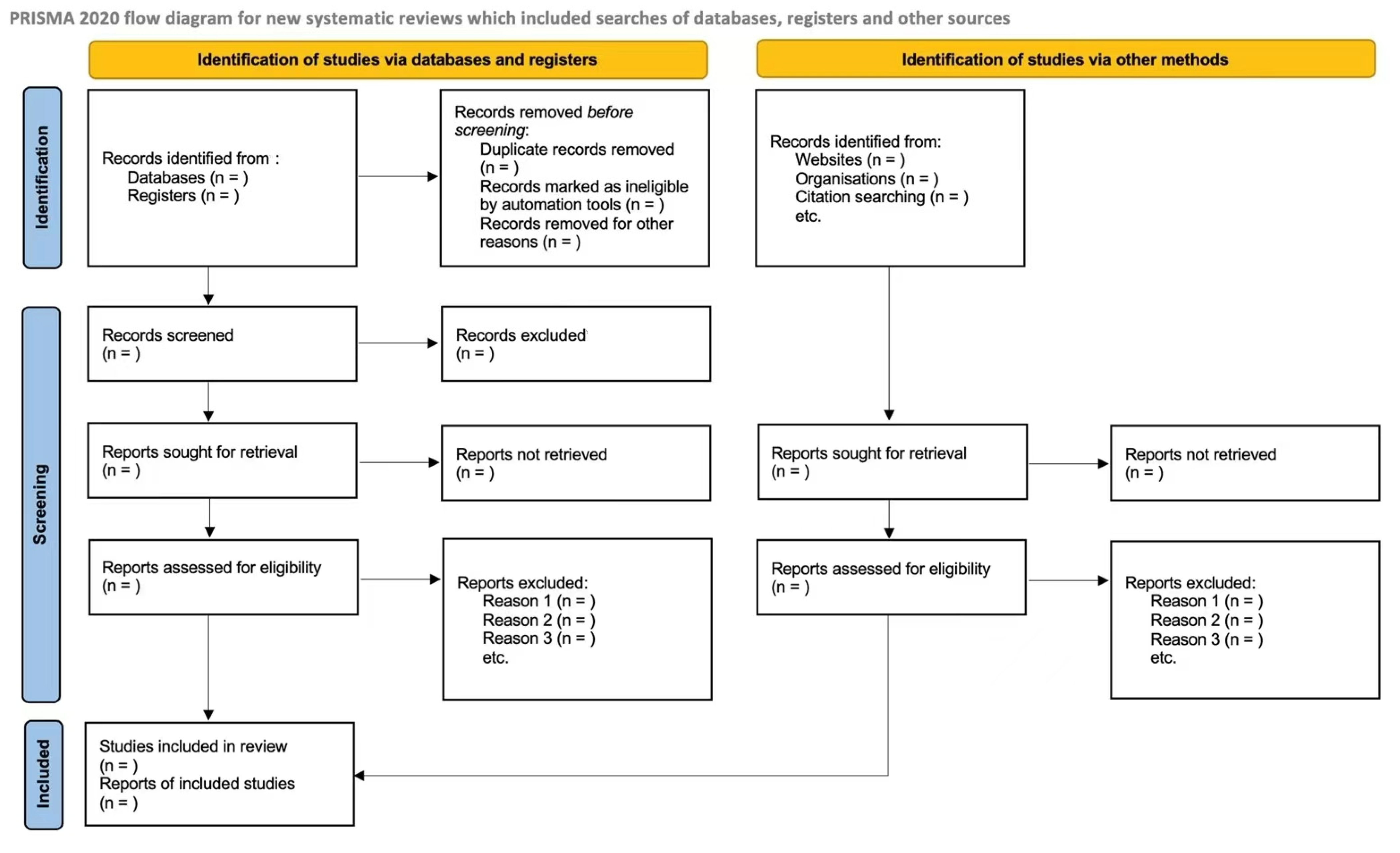
Study selection will be presented in accordance with the PRISMA flowchart—Figure 1 [32]. The results are presented via narrative summaries, considering the type of data and outcomes. In addition, a VOSviewer® tool was used to visualize bibliometric networks.
Figure 1.
PRISMA Flowchart.
2.7. Patient and Public Involvement
This ScR protocol analyzes existing evidence and thus does not involve patients. Therefore, ethical approval was not required for this study design.
3. Discussion
Recent advances in cancer detection and treatment have resulted in an exponential increase in the number of survivors worldwide [33,34]. Antineoplastic therapy can result in the manifestation of numerous symptoms during and after treatment [35,36,37,38]. Cardiovascular disease associated with cancer treatment is the first established cause of non-cancer morbidity and mortality [39,40,41,42]. It is important to emphasize that some chemotherapy drugs, such as doxorubicin in combination with cyclophosphamide, can further increase cardiotoxic effects [43].
In this context, it is extremely important that health professionals are aware of the cardiotoxic effects of chemotherapy and follow strategies recommended by the guideline of the American Society of Clinical Oncology (ASCO) to minimize risks, such as clinical history and physical examination directed to the cardiovascular system, pre-chemotherapy echocardiography, and even the use of the drug Dexrazoxane, considered cardioprotective [44]. Thus, health professionals need, besides the knowledge on chemotherapy drugs [5], to guide patients explaining their toxic effects, improving the quality of care when guidance is provided, identifying and clarifying the existing doubts, and contributing to selfcare [45].
A possible limitation may be the number of studies retrieved, even if a broad and systematic search strategy is performed. The results of this study will provide an updated understanding of cardiovascular risk indicators in adult patients undergoing chemotherapy treatment for future directions of new guidelines in the follow-up of patients undergoing cancer treatment at risk of developing cardiovascular alterations.
4. Conclusions
To the best of our knowledge, this ScR will be the first to map the clinical indicators of cardiovascular risk in adult patients undergoing chemotherapy. Additionally, in this ScR, we will adopt a rigorous approach, adhering to the PRISMA-ScR guidelines and conducting a comprehensive and systematic search strategy that will include primary studies and gray literature, with no publication date or language restrictions.
Author Contributions
L.C.L.-J. and K.Z.N. conceptualized and designed the study. J.G., K.Z.N. and L.C.L.-J. drafted the initial manuscript, and reviewed the final manuscript. J.G., K.Z.N., A.B.L. and L.C.L.-J. performed the study protocol and data interpretation and critically reviewed the final manuscript. J.G., K.Z.N., A.B.L., L.D.A.R., J.A.C., K.N.G., J.A.D.d.S. and L.C.L.-J. participated in data interpretation, provided critical insights, and reviewed the final manuscript. All authors approved and contributed to the final written manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
Fundação de Amparo à Pesquisa do Estado do Espírito Santo (FAPES). Edital n. 14/2022—Women in Science—Process Number 2022-NZXP7.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Fuster, V.; Voûte, J. MDGs: Chronic diseases are not on the agenda. Lancet 2005, 366, 1512–1514. [Google Scholar] [CrossRef] [PubMed]
- Miller, K.D.; Nogueira, L.; Devasia, T.; Mariotto, A.B.; Yabroff, K.R.; Jemal, A.; Kramer, J.; Siegel, R.L. Cancer treatment and survivorship statistics, 2022. CA Cancer J. Clin. 2022, 72, 409–436. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Lopes-Júnior, L.C.; Lima, R.A.G. Cancer care and interdisciplinary practice. Cad. Saude Publica 2019, 35, e00193218. [Google Scholar] [CrossRef]
- Levis, B.E.; Binkley, P.F.; Shapiro, C.L. Cardiotoxic effects of anthracycline-based therapy: What is the evidence and what are the potential harms? Lancet Oncol. 2017, 18, e445–e456. [Google Scholar] [CrossRef]
- Colombo, A.; Cipolla, C.; Beggiato, M.; Cardinale, D. Cardiac toxicity of anticancer agents. Curr. Cardiol. Rep. 2013, 15, 362. [Google Scholar] [CrossRef]
- O’Hare, M.; Sharma, A.; Murphy, K.; Mookadam, F.; Lee, H. Cardio-oncology Part I: Chemotherapy and cardiovascular toxicity. Expert. Rev. Cardiovasc. Ther. 2015, 13, 511–518. [Google Scholar] [CrossRef]
- O’Hare, M.; Murphy, K.; Mookadam, F.; Sharma, A.; Lee, H. Cardio-oncology Part II: The monitoring, prevention, detection and treatment of chemotherapeutic cardiac toxicity. Expert. Rev. Cardiovasc. Ther. 2015, 13, 519–527. [Google Scholar] [CrossRef]
- Armstrong, G.T.; Oeffinger, K.C.; Chen, Y.; Kawashima, T.; Yasui, Y.; Leisenring, W.; Stovall, M.; Chow, E.J.; Sklar, C.A.; Mulrooney, D.A.; et al. Modifiable risk factors and major cardiac events among adult survivors of childhood cancer. J. Clin. Oncol. 2013, 31, 3673–3680. [Google Scholar] [CrossRef]
- Pan, J.; Garza, F.; Lyon, A.R. Cardio-oncology: Rationale, aims and future directions. Curr. Opin. Support. Palliat. Care 2021, 15, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Kostakou, P.M.; Kouris, N.T.; Kostopoulos, V.S.; Damaskos, D.S.; Olympios, C.D. Cardio-oncology: A new and developing sector of research and therapy in the field of cardiology. Heart Fail. Rev. 2019, 24, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Karlstaedt, A.; Barrett, M.; Hu, R.; Gammons, S.T.; Ky, B. Cardio-Oncology: Understanding the Intersections Between Cardiac Metabolism and Cancer Biology. JACC Basic Transl. Sci. 2021, 6, 705–718. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Health Statistics and Information Systems: Disease Burden and Mortality Estimates; WHO: Geneva, Switzerland, 2022; Available online: http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html (accessed on 1 August 2022).
- Ewer, M.S.; Ewer, S.M. Cardiotoxicity of anticancer treatments: What the cardiologist needs to know. Nat. Rev. Cardiol. 2010, 7, 564–575. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.H. Cardiotoxic drugs: Clinical monitoring and decision making. Heart 2008, 94, 1503–1509. [Google Scholar] [CrossRef] [PubMed]
- Monsuez, J.J.; Charniot, J.C.; Vignat, N.; Artigou, J.Y. Cardiac side-effects of cancer chemotherapy. Int. J. Cardiol. 2010, 144, 3–15. [Google Scholar] [CrossRef]
- Yeh, E.T.; Bickford, C.L. Cardiovascular complications of cancer therapy: Incidence, pathogenesis, diagnosis, and management. J. Am. Coll. Cardiol. 2009, 53, 2231–2247. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Chapter 11: Scoping Reviews (2020 version). In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: North Adelaide, Australia, 2020. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. Theory Pract. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing be-tween a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.; Colquhoun, H.; Kastner, M.; Levac, D.; Ng, C.; Sharpe, J.P.; Wilson, K.; et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med. Res. Methodol. 2016, 16, 15. [Google Scholar] [CrossRef] [PubMed]
- Lotufo, P.A. O escore de risco de Framingham para doenças cardiovasculares. Rev. Med. 2008, 87, 232–237. [Google Scholar] [CrossRef]
- Lopes-Júnior, L.C.; Bomfim, E.; Olson, K.; Neves, E.T.; Silveira, D.S.C.; Nunes, M.D.R.; Nascimento, L.C.; Pereira-da-Silva, G.; Lima, R.A.G. Effectiveness of hospital clowns for symptom management in paediatrics: Systematic review of randomised and non-randomised controlled trials. BMJ 2020, 371, m4290. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Lopes-Júnior, L.C.; Lima, R.A.G.; Zonta, J.B.; Sulino, M.C.; Looman, W.S.; Correa, L.M.; Okido, A.C.C. Biomarkers of stress in caregivers of children with special health care needs: A protocol for systematic review. Medicine 2022, 101, e31448. [Google Scholar] [CrossRef]
- Da Silva Junior, F.J.G.; de Souza Monteiro, C.F.; Costa, A.P.C.; Campos, L.R.B.; Miranda, P.I.G.; de Souza Monteiro, T.A.; Lima, R.A.G.; Lopes-Junior, L.C. Impact of COVID-19 pandemic on mental health of young people and adults: A systematic review protocol of observational studies. BMJ Open 2020, 10, e039426. [Google Scholar] [CrossRef]
- Pessanha, R.M.; Schuab, S.I.P.D.C.; Nunes, K.Z.; Lopes-Júnior, L.C. Use of family history taking for hereditary neoplastic syndromes screening in primary health care: A systematic review protocol. PLoS ONE 2022, 17, e0271286. [Google Scholar] [CrossRef]
- Lopes-Júnior, L.C.; Ferrarini, T.; Pires, L.B.C.; Rodrigues, J.G.; Salaroli, L.B.; Nunes, K.Z. Cancer symptom clusters in adult patients undergoing chemotherapy: A systematic review and meta-analysis protocol. PLoS ONE 2022, 17, e0273411. [Google Scholar] [CrossRef]
- Centre for Evidence Based Medicine. Available online: http://www.cebm.net (accessed on 1 November 2021).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Moslehi, J.J. Cardiovascular Toxic Effects of Targeted Cancer Therapies. N. Engl. J. Med. 2016, 375, 1457–1467. [Google Scholar] [CrossRef]
- Hajjar, L.A.; Costa, I.B.S.D.S.D.; Lopes, M.A.C.Q.; Hoff, P.M.G.; Diz, M.D.P.E.; Fonseca, S.M.R.; Bittar, C.S.; Rehder, M.H.H.D.S.; Rizk, S.I.; Almeida, D.R.; et al. Diretriz Brasileira de Cardio-oncologia—2020. Arq. Bras. Cardiol. 2020, 115, 1006–1043. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Barsevick, A.M.; Fang, C.Y.; Miaskowski, C. Common biological pathways underlying the psycho- neurological symptom cluster in cancer patients. Cancer Nurs. 2012, 35, E1–E20. [Google Scholar] [CrossRef] [PubMed]
- Dodd, M.J.; Miaskowski, C.; Lee, K.A. Occurrence of symptom clusters. J. Natl. Cancer Inst. Monogr. 2004, 2004, 76–78. [Google Scholar] [CrossRef] [PubMed]
- Lopes-Júnior, L.C. Cancer symptom clusters: From the lab bench to clinical practice. Rev. Bras. Enferm. 2022, 75, e2022v75n5inov. [Google Scholar] [CrossRef] [PubMed]
- Lopes-Júnior, L.C.; Tuma, M.C.; Amorim, M.H.C. Psychoneuroimmunology and oncology nursing: A theoretical study. Rev. Esc. Enferm. USP 2021, 55, e20210159. [Google Scholar] [CrossRef] [PubMed]
- Hull, M.C.; Morris, C.G.; Pepine, C.J.; Mendenhall, N.P. Valvular dysfunction and carotid, subclavian, and coronary artery disease in survivors of hodgkin lymphoma treated with radiation therapy. JAMA 2003, 290, 2831–2837. [Google Scholar] [CrossRef]
- Oeffinger, K.C.; Mertens, A.C.; Sklar, C.A.; Kawashima, T.; Hudson, M.M.; Meadows, A.T.; Friedman, D.L.; Marina, N.; Hobbie, W.; Kadan-Lottick, N.S.; et al. Childhood Cancer Survivor Study. Chronic health conditions in adult survivors of childhood cancer. N. Engl. J. Med. 2006, 355, 1572–1582. [Google Scholar] [CrossRef]
- Geenen, M.M.; Cardous-Ubbink, M.C.; Kremer, L.C.; van den Bos, C.; van der Pal, H.J.; Heinen, R.C.; Jaspers, M.W.; Koning, C.C.; Oldenburger, F.; Langeveld, N.E.; et al. Medical assessment of adverse health outcomes in long-term survivors of childhood cancer. JAMA 2007, 297, 2705–2715. [Google Scholar] [CrossRef]
- Reulen, R.C.; Winter, D.L.; Frobisher, C.; Lancashire, E.R.; Stiller, C.A.; Jenney, M.E.; Skinner, R.; Stevens, M.C.; Hawkins, M.M. British Childhood Cancer Survivor Study Steering Group. Long-term cause-specific mortality among survivors of childhood cancer. JAMA 2010, 304, 172–179. [Google Scholar] [CrossRef]
- Pinto, C.M.; Silva, D.C.; Pinto, G.H.; Santos, M.H.H. Quimioterapia e cardiotoxicidade. Rev. Soc. Cardiol. Estado São Paulo 2017, 27, 266–273. [Google Scholar] [CrossRef]
- Armenian, S.H.; Lacchetti, C.; Lenihan, D. Prevention and Monitoring of Cardiac Dysfunction in Survivors of Adult Cancers: American Society of Clinical Oncology Clinical Practice Guideline Summary. J. Oncol. Pract. 2017, 13, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Da Costa, A.G.; Costa, M.S.C.R.; da Silva Ferreira, E.; de Sousa, P.C.; dos Santos, M.M.; Lima, D.E.D.O.B.; Ramos, A.M.P.C. Conhecimento dos Profissionais de Enfermagem sobre Segurança do Paciente Oncológico em Quimioterapia. Rev. Bras. Cancerol. 2019, 65, e04274. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).