Statistical Analysis of Ceiling and Floor Effects in Medical Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Eligibility
2.2. Patient Selection
2.3. Treatment and Response Profiles
2.4. Statistical Analysis
- (a)
- Providing insights into data characteristics, features, and patterns.
- (b)
- Producing graphical representations of data for the purpose of visualisation.
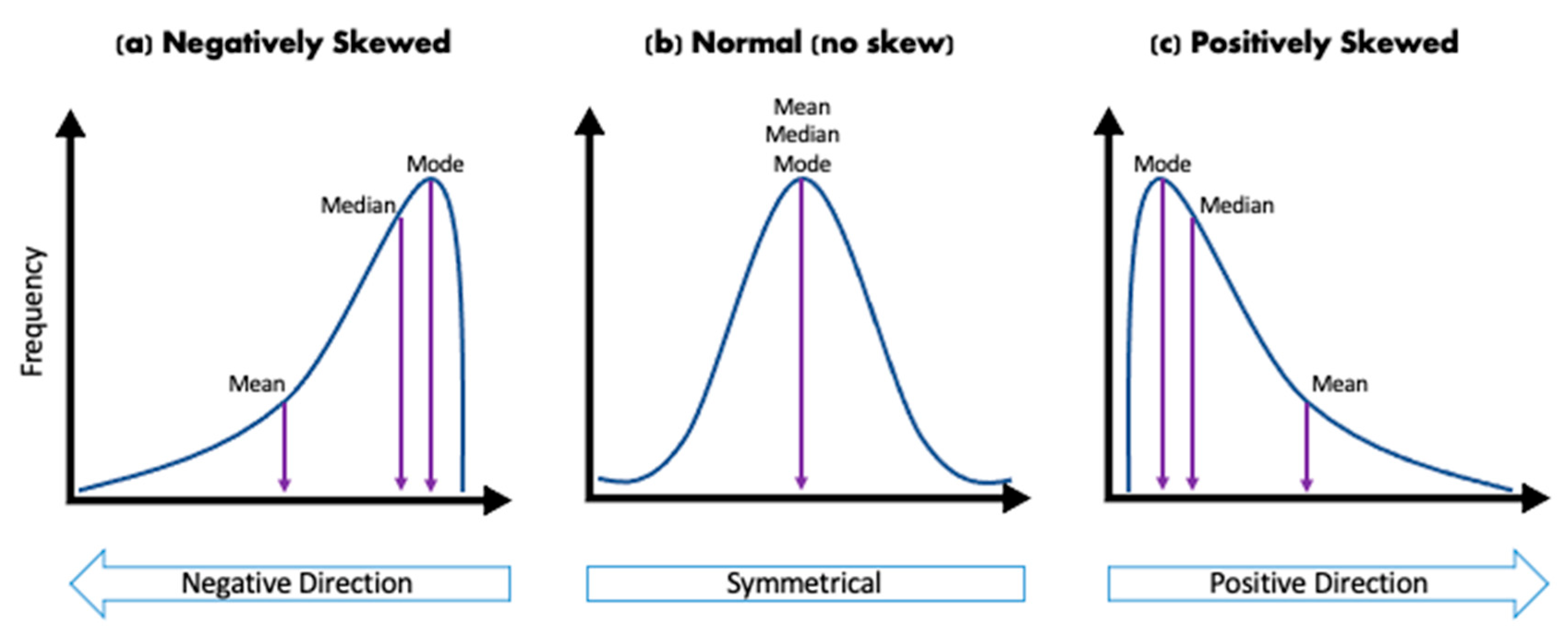
- If the statistical distribution is highly skewed.
- If 0.5 < the statistical distribution is moderately skewed.
- If the statistical distribution is approximately symmetrical.
3. Results
3.1. Summary Statistics
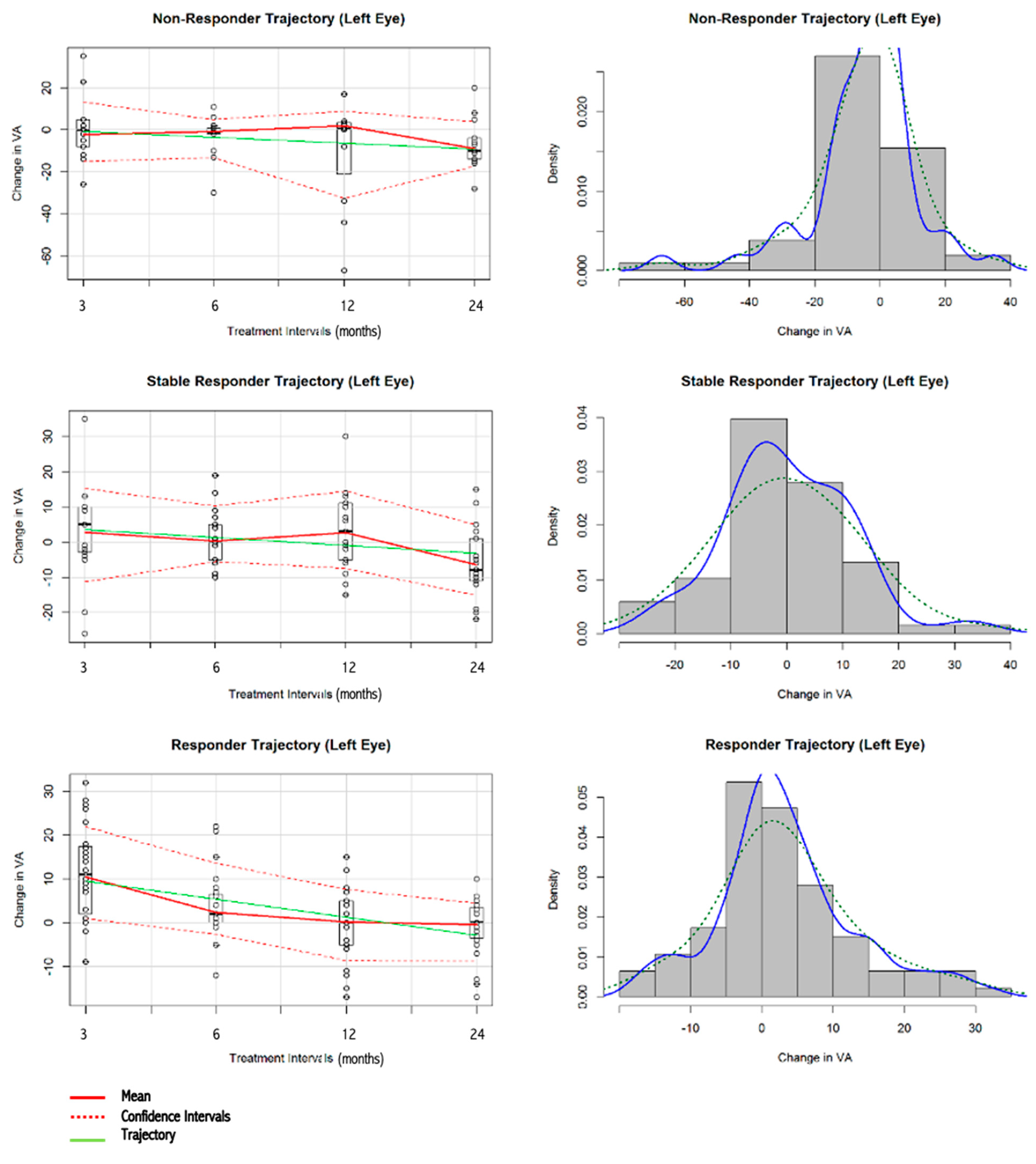
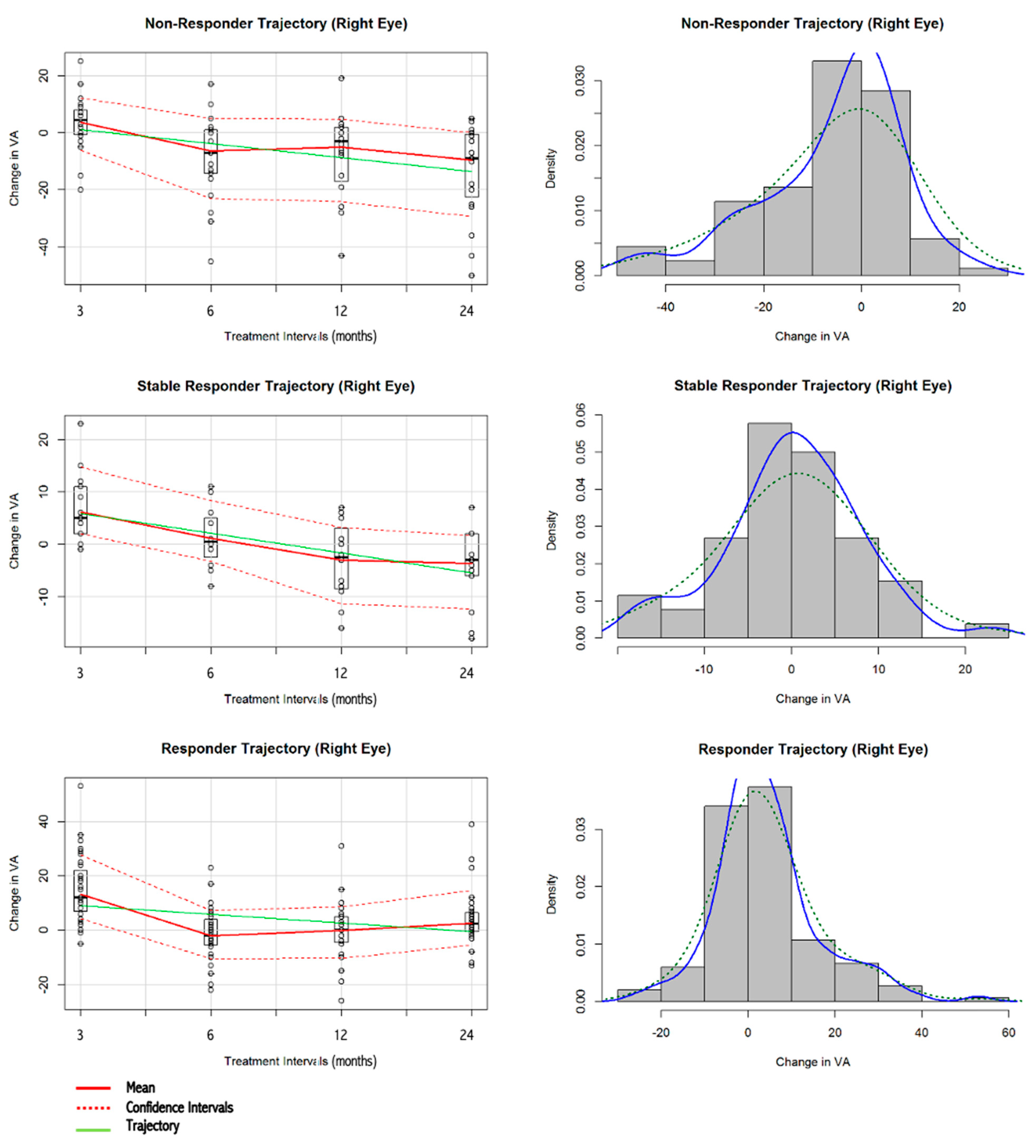
3.2. Visualisation and Skewness Statistics of VA Data
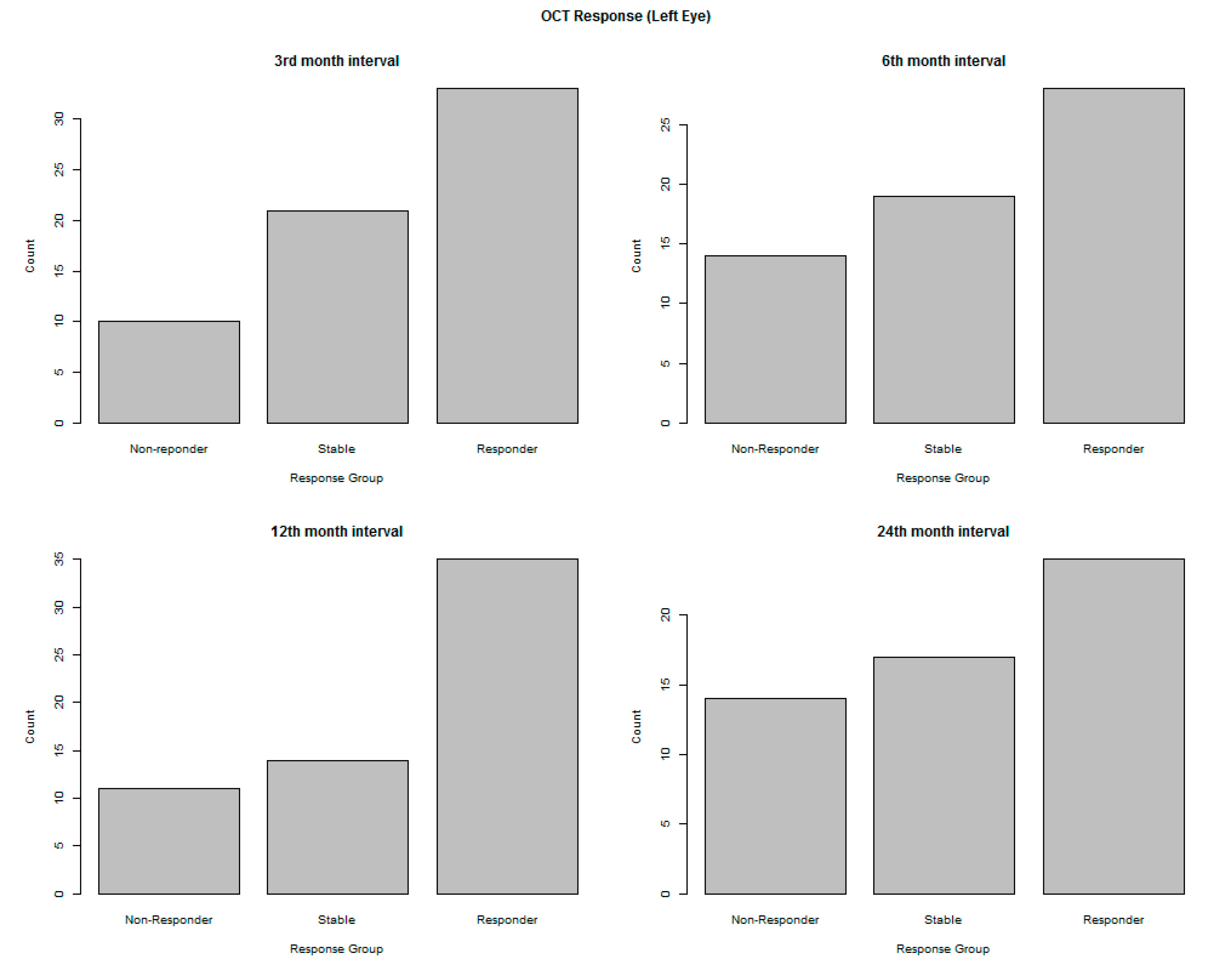
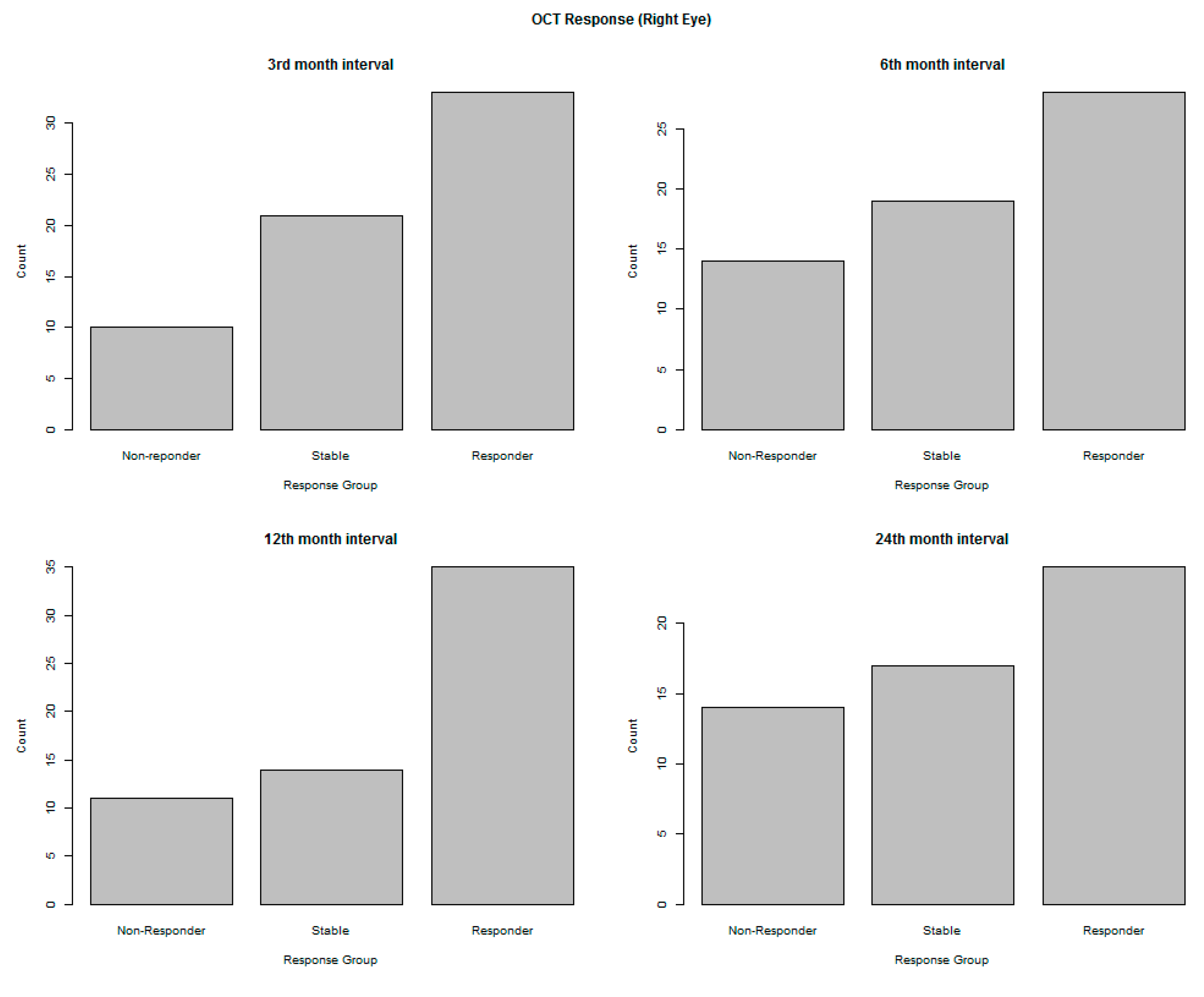
3.3. Visualisation and Summary of OCT Data
4. Discussion
- There is great difficulty in ranking patients in order of treatment effect, as the patient responses are the same or tightly clustered.
- If most patients have the same response, there is difficulty in correlation with potential patient-related predictors, such as age, obesity, or smoking status.
- If the statistical distribution is very skewed along the measurement scale, the arithmetic mean (as a measure of central tendency) and the variance of the patient responses are no longer representative of the group. A parametric confidence interval may even have a negative bound because the symmetrical normal distribution was assumed, rather than a skewed distribution.
- There are errors introduced in the application of standard parametric statistical tests of significance, as well as hypothesis tests, such as the comparison between the arithmetic means (treatment group vs. control group).
- It is difficult, if not impossible, to reliably fit prediction models, including machine learning algorithms.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chakravarthy, U.; Harding, S.P.; Rogers, C.A.; Downes, S.M.; Lotery, A.J.; Culliford, L.A.; Reeves, B.C.; IVAN study investigators. Alternative treatments to inhibit VEGF in age-related choroidal neovascularisation: 2-year findings of the IVAN randomised controlled trial. Lancet 2013, 382, 1258–1267. [Google Scholar] [CrossRef] [PubMed]
- Bora, N.S.; Matta, B.; Lyzogubov, V.V.; Bora, P.S. Relationship between the complement system, risk factors and prediction models in age-related macular degeneration. Mol. Immunol. 2015, 63, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Buck, D.A.; Dawkins, R.; Kawasaki, R.; Sandhu, S.S.; Allen, P.J. Survey of Victorian ophthalmologists who use ranibizumab to treat age-related macular degeneration: To identify current practice and modifiable risk factors relevant to post-injection endophthalmitis. Clin. Exp. Ophthalmol. 2015, 43, 277–279. [Google Scholar] [CrossRef]
- Wong, W.L.; Su, X.; Li, X.; Cheung, C.M.; Klein, R.; Cheng, C.Y.; Wong, T.Y. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: A systematic review and meta-analysis. Lancet Glob. Health 2014, 2, e106–e116. [Google Scholar] [CrossRef] [PubMed]
- Parmeggiani, F.; Gemmati, D.; Costagliola, C.; Sebastiani, A.; Incorvaia, C. Predictive role of C677T MTHFR polymorphism in variable efficacy of photodynamic therapy for neovascular age-related macular degeneration. Pharmacogenomics 2009, 10, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Horie-Inoue, K.; Inoue, S. Genomic aspects of age-related macular degeneration. Biochem. Biophys. Res. Commun. 2014, 452, 263–275. [Google Scholar] [CrossRef] [PubMed]
- Coleman, H.R.; Chan, C.C.; Ferris, F.L., 3rd; Chew, E.Y. Age-related macular degeneration. Lancet 2008, 372, 1835–1845. [Google Scholar] [CrossRef]
- Schramm, E.C.; Clark, S.J.; Triebwasser, M.P.; Raychaudhuri, S.; Seddon, J.; Atkinson, J.P. Genetic variants in the complement system predisposing to age-related macular degeneration: A review. Mol. Immunol. 2014, 61, 118–125. [Google Scholar] [CrossRef]
- Australian Government. Department of Health and Aged Care. Section Two: The Epidemiology and Impact of Blindness and Vision Loss in Australia. Available online: http://www.health.gov.au/internet/main/publishing.nsf/ContentD1A5409787D800F2CA257C73007F12F3/$File/2.pdf (accessed on 30 September 2014).
- Ambati, J.; Ambati, B.K.; Yoo, S.H.; Ianchulev, S.; Adamis, A.P. Age-related macular degeneration: Etiology, pathogenesis, and therapeutic strategies. Surv. Ophthalmol. 2003, 48, 257–293. [Google Scholar] [CrossRef]
- Ratnapriya, R.; Chew, E.Y. Age-related macular degeneration-clinical review and genetics update. Clin. Genet. 2013, 84, 160–166. [Google Scholar] [CrossRef]
- Holz, F.G.; Pauleikhoff, D.; Spaide, R.F.; Bird, A.C. (Eds.) Age-Related Macular Degeneration, 2nd ed.; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Francis, P.J. The influence of genetics on response to treatment with ranibizumab (Lucentis) for age-related macular degeneration: The Lucentis Genotype Study (an American Ophthalmological Society thesis). Trans. Am. Ophthalmol. Soc. 2011, 109, 115–156. [Google Scholar] [PubMed]
- Fauser, S.; Lambrou, G.N. Genetic predictive biomarkers of anti-VEGF treatment response in patients with neovascular age-related macular degeneration. Surv. Ophthalmol. 2015, 60, 138–152. [Google Scholar] [CrossRef] [PubMed]
- National Library of Medicine. ClinicalTrials.gov. 2015. Available online: https://clinicaltrials.gov/ (accessed on 30 October 2015).
- Anand, A.; Sharma, K.; Chen, W.; Sharma, N.K. Using current data to define new approach in age related macular degeneration: Need to accelerate translational research. Curr. Genom. 2014, 15, 266–277. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mitchell, P. Eyes on the Future: A Clear Outlook on Age-Related Macular Degeneration; Macquaire University: Sydney, Australia, 2011. [Google Scholar]
- Bartlett, J.D. Ophthalmic Drug Facts; Facts & Comparisons; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013. [Google Scholar]
- Shastry, B.S. Genetic Risk Factors in Age-Relatd Macular Degeneration. In Encyclopedia of Eye Research; Nova Science Publishers, Inc.: Hauppauge, NY, USA, 2012; pp. 1365–1376. [Google Scholar]
- Rovner, B.W.; Casten, R.J.; Hegel, M.T.; Massof, R.W.; Leiby, B.E.; Ho, A.C.; Tasman, W.S. Improving function in age-related macular degeneration: A randomized clinical trial. Ophthalmology 2013, 120, 1649–1655. [Google Scholar] [CrossRef] [PubMed]
- Amoaku, W.M.; Chakravarthy, U.; Gale, R.; Gavin, M.; Ghanchi, F.; Gibson, J.; Harding, S.; Johnston, R.L.; Kelly, S.P.; Lotery, A.; et al. Defining response to anti-VEGF therapies in neovascular AMD. Eye 2015, 29, 721–731. [Google Scholar] [CrossRef] [PubMed]
- McBee, M. Modeling outcomes with floor or ceiling effects: An introduction to the Tobit model. Gift. Child Q. 2010, 54, 314–320. [Google Scholar] [CrossRef]
- Arslan, J.; Benke, K.K. Application of Machine Learning to Ranking Predictors of Anti-VEGF Response. Life 2022, 12, 1926. [Google Scholar] [CrossRef]
- Andrade, C. The Ceiling Effect, the Floor Effect, and the Importance of Active and Placebo Control Arms in Randomized Controlled Trials of an Investigational Drug. Indian J. Psychol. Med. 2021, 43, 360–361. [Google Scholar] [CrossRef]
- Gelman, A. Exploratory Data Analysis for Complex Models. J. Comput. Graph. Stat. 2004, 13, 755–779. [Google Scholar] [CrossRef]
- Behrens, J.T. Principles and procedures of exploratory data analysis. Psychol. Methods 1997, 2, 131–160. [Google Scholar] [CrossRef]
- Huang, I.C.; Frangakis, C.; Atkinson, M.J.; Willke, R.J.; Leite, W.L.; Vogel, W.B.; Wu, A.W. Addressing ceiling effects in health status measures: A comparison of techniques applied to measures for people with HIV disease. Health Serv. Res. 2008, 43, 327–339. [Google Scholar] [CrossRef]
- Doane, D.P.; Seward, L.E. Measuring Skewness: A Forgotten Statistic? J. Stat. Educ. 2011, 19, 1–18. [Google Scholar] [CrossRef]
- George, D.; Mallery, M. SPSS for Windows Step by Step: A Simple Guide and Reference, 17.0 Update, 10th ed.; Pearson: Boston, MA, USA, 2010. [Google Scholar]
- Hair, J.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Pearson Educational International: Upper Saddle River, NJ, USA, 2010. [Google Scholar]
- Liu, Q.; Wang, L. t-Test and ANOVA for data with ceiling and/or floor effects. Behav. Res. Methods 2021, 53, 264–277. [Google Scholar] [CrossRef]
- Šimkovic, M.; Träuble, B. Robustness of statistical methods when measure is affected by ceiling and/or floor effect. PLoS ONE 2019, 14, e0220889. [Google Scholar] [CrossRef]
- Benke, K.K.; Norng, S.; Robinson, N.J.; Benke, L.R.; Peterson, T.J. Error propagation in computer models: Analytic approaches, advantages, disadvantages and constraints. Stoch. Environ. Res. Risk Assess. 2018, 32, 2971–2985. [Google Scholar] [CrossRef]

| Sex, n (%) | |
|---|---|
| Female | 85 (56.7) |
| Male | 65 (43.3) |
| Age (yrs) | |
| Mean ± SD | 78.9 ± 7.3 |
| Range | 54–102 |
| Baseline VA, LE | |
| Mean ± SD | 53.5 ± 24.0 |
| Range | 0–88 |
| Baseline VA, RE | |
| Mean ± SD | 48.4 ± 24.3 |
| Range | 2–90 |
| Treatment Administered, n (%) | |
| Ranibizumab | 122 (81.3) |
| Bevacizumab | 28 (18.7) |
| Smoking Status, n (%) | |
| No | 53 (35.3) |
| Yes—Past | 64 (42.7) |
| Yes—Present | 19 (12.7) |
| Yes—Virtually Never | 8 (5.3) |
| Missing | 6 (4.0) |
| Smoker Packs (years) | |
| Mean ± SD | 39.1 ± 28.7 |
| Range | 2–126 |
| Treated Eye, n (%) | |
| LE | 64 (42.7) |
| RE | 86 (57.3) |
| Hypertension, n (%) | |
| No | 48 (32) |
| Yes | 102 (68) |
| Diabetes, n (%) | |
| No | 118 (78.7) |
| Yes | 25 (16.7) |
| Missing | 7 (4.6) |
| Responders | Non-Responders | Stable Responders | All | |
|---|---|---|---|---|
| Fisher–Pearson Skewness | 0.5391 | −1.1474 | 0.3215 | −0.7333 |
| z-value | 2.1534 | −3.2047 | 1.1576 | −4.29 |
| p-value | 3.13 10−2 | 1.35 10−3 | 0.247 | 0.00001787 |
| Kurtosis | 3.603363 | 6.589836 | 3.637867 | 7.257142 |
| Mean | 3.419355 | −4.711538 | 0.2058824 | 0.4533898 |
| Standard Error | 1.017073 | 2.252924 | 1.381484 | 0.8023191 |
| Median | 2 | −1 | −1 | 0 |
| Standard Deviation | 9.808296 | 16.24607 | 11.39201 | 12.32546 |
| Sample Variance | 96.20266 | 263.9348 | 129.7779 | 151.917 |
| Minimum | −17 | −67 | −26 | −67 |
| Maximum | 32 | 35 | 35 | 35 |
| Sum | 318 | −245 | 14 | 107 |
| Count | 96 | 56 | 68 | 256 |
| Responders | Non-Responders | Stable Responders | All | |
|---|---|---|---|---|
| Fisher–Pearson Skewness | 0.8378 | −0.8684 | −0.0251 | −0.2567 |
| z-value | 3.8919 | −3.1761 | −0.082 | −1.8709 |
| p-value | 9.95 10−5 | 1.49 10−3 | 0.9346 | 0.06136 |
| Kurtosis | 4.738163 | 3.596595 | 3.535297 | 5.483278 |
| Mean | 4.413333 | −6.056818 | 0.2307692 | 0.452229 |
| Standard Error | 0.9851782 | 1.583727 | 1.115372 | 0.734788 |
| Median | 2.5 | −1 | 0 | 0 |
| Standard Deviation | 12.06592 | 14.85668 | 8.043059 | 13.02048 |
| Sample Variance | 145.5864 | 220.7209 | 64.6908 | 169.5329 |
| Minimum | −26 | −50 | −18 | −50 |
| Maximum | 53 | 25 | 23 | 53 |
| Sum | 662 | −533 | 12 | 142 |
| Count | 156 | 96 | 56 | 344 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arslan, J.; Benke, K. Statistical Analysis of Ceiling and Floor Effects in Medical Trials. Appl. Biosci. 2023, 2, 668-681. https://doi.org/10.3390/applbiosci2040042
Arslan J, Benke K. Statistical Analysis of Ceiling and Floor Effects in Medical Trials. Applied Biosciences. 2023; 2(4):668-681. https://doi.org/10.3390/applbiosci2040042
Chicago/Turabian StyleArslan, Janan, and Kurt Benke. 2023. "Statistical Analysis of Ceiling and Floor Effects in Medical Trials" Applied Biosciences 2, no. 4: 668-681. https://doi.org/10.3390/applbiosci2040042
APA StyleArslan, J., & Benke, K. (2023). Statistical Analysis of Ceiling and Floor Effects in Medical Trials. Applied Biosciences, 2(4), 668-681. https://doi.org/10.3390/applbiosci2040042






