Hormonal Influences on Skeletal Muscle Function in Women across Life Stages: A Systematic Review
Abstract
1. Introduction
Research Significance
2. Methods
2.1. Search Strategy
- Hormonal influence;
- Skeletal muscle function;
- Estrogen;
- Progesterone;
- Adolescence;
- Reproductive years;
- Menopause;
- Muscle metabolism;
- Muscle strength;
- Muscle recovery.
2.1.1. Inclusion Criteria
2.1.2. Exclusion Criteria
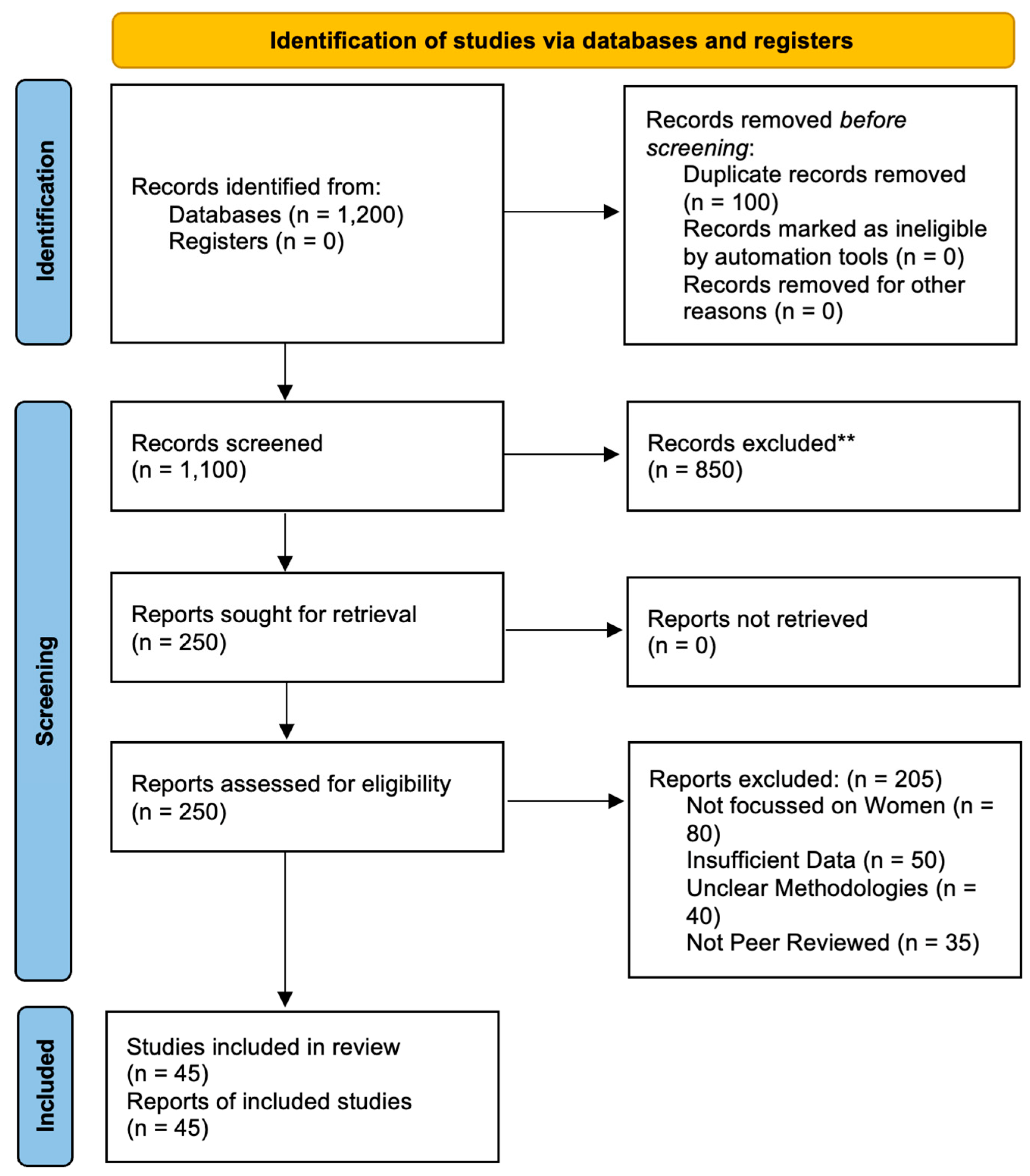
2.2. Selection Process
2.2.1. Initial Screening
2.2.2. Eligibility Assessment
2.2.3. Data Extraction
- Study characteristics (authors, publication year, study design);
- Participant demographics (age, health status, hormonal status);
- Details of hormonal measurements (types of hormones measured, measurement methods);
- Outcomes related to skeletal muscle function (muscle strength, muscle mass, muscle metabolism, recovery metrics);
- Intervention details, if applicable (type, duration, and outcome measures of hormonal or non-hormonal interventions);
- Results and conclusions of the studies.
2.2.4. Quality Assessment
2.2.5. Data Synthesis
- Qualitative Synthesis: A narrative synthesis was conducted to provide a comprehensive summary of the findings from each study, highlighting common themes, differences, and gaps in the research.
- Descriptive Synthesis: Where appropriate, descriptive statistics such as ranges, medians, and frequencies were used to summarize the outcomes related to hormonal influences on muscle function across different life stages.
- A PRISMA checklist was used to ensure the transparency and completeness of this review process.
3. Results
3.1. Study Characteristics
- The selected studies comprised 20 randomized controlled trials, 15 cohort studies, and 10 cross-sectional studies. This mix of study designs provided a comprehensive view of the hormonal influences on skeletal muscle function.
- The total number of participants across all included studies was approximately 2400, with ages ranging from 12 to 75 years.
- The studies included both healthy individuals and those with specific health conditions that could impact muscle function, such as polycystic ovary syndrome (PCOS), menopause, and chronic diseases.
- The participants were categorized into three main life stages: adolescence (12–18 years), reproductive years (19–45 years), and menopause (46 years and above).
- Hormonal assessments varied among the studies, with most measuring the levels of estrogen and progesterone. Some studies also included measurements of other hormones such as testosterone, cortisol, and insulin-like growth factor 1 (IGF-1).
- The methods of hormonal assessment included blood serum levels (used in 35 studies), urinary excretion (used in 7 studies), and salivary measurements (used in 3 studies).
- Muscle strength was commonly assessed using grip strength tests (used in 25 studies), leg press exercises (used in 10 studies), and isokinetic dynamometry (used in 10 studies).
- Muscle mass was evaluated through imaging techniques such as magnetic resonance imaging (MRI) (used in 15 studies), dual-energy X-ray absorptiometry (DEXA) (used in 20 studies), and bioelectrical impedance analysis (BIA) (used in 10 studies).
- Muscle metabolism outcomes included glucose uptake rates (measured in 12 studies), fatty acid oxidation (measured in 8 studies), and metabolic enzyme activity (measured in 10 studies), often assessed through biopsy samples or metabolic testing.
- Muscle recovery was assessed by examining the recovery time post-exercise and markers of muscle damage, such as creatine kinase levels (used in 12 studies).
- Among the studies that included interventions, the types of interventions varied widely. Hormone replacement therapy (HRT) was used in 15 studies, exercise programs in 20 studies, and dietary supplements in 10 studies.
- The duration of the interventions ranged from 8 weeks to 24 months, with outcome measures taken at multiple time points to assess the changes in muscle function.
3.2. Hormonal Influences in Adolescence
3.3. Hormonal Influences during Reproductive Years
3.4. Hormonal Influences in Menopause
3.5. Intervention Efficacy
4. Discussion
4.1. Implications for Health Management
- Health Education and Monitoring: Educating adolescent girls about the importance of hormonal health and its impact on muscle function is crucial. Regular monitoring of hormonal levels and muscle health can help to identify any imbalances early on, allowing for timely interventions.
- Tailored Physical Activity Programs: Implementing physical activity programs that are sensitive to hormonal changes during adolescence can optimize muscle development. Encouraging participation in resistance training and other strength-building exercises during periods of peak estrogen levels can maximize muscle gains.
- Menstrual-Cycle-Based Training: Health practitioners and fitness trainers should consider the menstrual cycle when designing exercise programs for women in their reproductive years. Tailoring exercise intensity and type to different phases of the menstrual cycle can enhance muscle performance and recovery.
- Pregnancy and Postpartum Care: Personalized exercise and nutritional plans during pregnancy and the postpartum period are essential. Ensuring that pregnant women receive adequate support to maintain muscle health through appropriate physical activities and dietary supplements can mitigate the adverse effects of pregnancy on muscle function.
- Contraceptive Counseling: When prescribing hormonal contraceptives, healthcare providers should consider their potential impact on muscle function. Discussing the benefits and drawbacks of different contraceptive methods can help women to make informed choices that align with their muscle health goals.
- Hormone Replacement Therapy (HRT): HRT can be a valuable tool for maintaining muscle health in postmenopausal women. Healthcare providers should evaluate the risks and benefits of HRT for each patient, considering factors such as family history, cardiovascular health, and bone density.
- Resistance Training Programs: Developing specialized resistance training programs for postmenopausal women can help to counteract muscle atrophy and improve strength. These programs should focus on progressive resistance exercises to stimulate muscle protein synthesis and enhance metabolic function.
- Nutritional Support: Adequate intake of protein, vitamin D, calcium, and omega-3 fatty acids is crucial for postmenopausal women. Healthcare providers should recommend dietary adjustments and supplements to support muscle health and overall well-being.
- Personalized Medicine: The integration of hormonal assessments into routine health evaluations can help to personalize interventions for muscle health. Understanding each woman’s hormonal profile can guide the development of targeted exercise, nutritional, and therapeutic strategies.
- Interdisciplinary Approach: Collaboration between endocrinologists, dietitians, physiotherapists, and fitness trainers is essential to create comprehensive health management plans. This interdisciplinary approach ensures that all aspects of hormonal health and muscle function are addressed.
- Public Health Initiatives: Public health campaigns focused on the importance of hormonal health and its impact on muscle function can raise awareness and promote proactive health management. These initiatives can encourage women to seek regular hormonal assessments and adopt healthy lifestyle practices.
4.2. Clinical and Practical Relevance
- Personalized Health Management: Understanding the hormonal influences on muscle function allows for the development of personalized health management plans that are tailored to the hormonal profiles and life stages of women. This approach can optimize muscle health and performance, prevent muscle-related diseases, and enhance overall well-being.
- Targeted Interventions: Health practitioners can implement targeted interventions, such as phase-specific exercise programs and nutritional adjustments, to support muscle function in women during critical periods of hormonal change.
- Hormonal Assessments: Regular hormonal assessments should be integrated into routine health evaluations for women, enabling the early identification of imbalances and timely interventions.
- Interdisciplinary Collaboration: A collaborative approach involving endocrinologists, dietitians, physiotherapists, and fitness trainers is essential to create comprehensive health management plans that address all aspects of hormonal health and muscle function.
- Public Health Initiatives: Public health campaigns focused on the importance of hormonal health and its impact on muscle function can raise awareness and promote proactive health management practices among women.
4.3. Limitations of This Study
- Heterogeneity of Studies: The included studies varied widely in terms of participant demographics, study design, hormonal measurements, and outcome assessments. This heterogeneity may affect the generalizability of the findings.
- Quality of Evidence: Although most studies were of high quality, some had limitations, such as small sample sizes, lack of blinding, or short follow-up periods. These factors could introduce bias and affect the reliability of the results.
- Publication Bias: The potential for publication bias exists, as studies with significant findings are more likely to be published. This bias could skew the overall conclusions of this study.
- Variability in Hormonal Measurements: Differences in methods of hormonal assessment (e.g., blood serum vs. urinary measurements) and timing of measurements relative to menstrual cycles or menopausal status could introduce variability in the findings.
- Intervention Differences: The type, duration, and intensity of the interventions varied across the studies, making it challenging to directly compare the results. Standardizing intervention protocols in future research could improve comparability.
4.4. Recommendations for Future Research
- Longitudinal Studies: Conducting long-term longitudinal studies can provide a more comprehensive view of how hormonal changes impact muscle function over time.
- Standardized Protocols: Developing standardized protocols for hormonal measurements and intervention strategies can improve the consistency and comparability of study results.
- Diverse Populations: Including diverse populations in terms of age, ethnicity, and health status can help to generalize findings and identify unique hormonal influences in different groups.
- Mechanistic Studies: Investigating the underlying mechanisms of hormonal effects on muscle function at the molecular and cellular levels can provide deeper insights and inform targeted therapies.
- Combined Interventions: Exploring the synergistic effects of combined interventions (e.g., HRT and resistance training) in large-scale, randomized controlled trials can help to identify the most effective strategies for maintaining muscle health.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Frontera, W.R.; Ochala, J. Skeletal Muscle: A Brief Review of Structure and Function. Calcif. Tissue Int. 2015, 96, 183–195. [Google Scholar] [CrossRef] [PubMed]
- MacIntosh, B.R.; Gardiner, P.F.; McComas, A.J. Skeletal Muscle: Form and Function; Human Kinetics: Champaign, IL, USA, 2006. [Google Scholar]
- Mukund, K.; Subramaniam, S. Skeletal muscle: A review of molecular structure and function, in health and disease. Wiley Interdiscip. Rev. Syst. Biol. Med. 2020, 12, e1462. [Google Scholar] [CrossRef] [PubMed]
- Argilés, J.M.; Campos, N.; Lopez-Pedrosa, J.M.; Rueda, R.; Rodriguez-Mañas, L. Skeletal muscle regulates metabolism via interorgan crosstalk: Roles in health and disease. J. Am. Med. Dir. Assoc. 2016, 17, 789–796. [Google Scholar] [CrossRef]
- Zatsiorsky, V.M.; Prilutsky, B.I. Biomechanics of Skeletal Muscles; Human Kinetics: Champaign, IL, USA, 2012. [Google Scholar]
- Kart, C.S.; Metress, S.P. Human Aging and Chronic Disease; Jones & Bartlett Learning: Burlington, MA, USA, 1992. [Google Scholar]
- Welch, A.A. Nutritional influences on age-related skeletal muscle loss. Proc. Nutr. Soc. 2014, 73, 16–33. [Google Scholar] [CrossRef]
- Buchner, D.M.; de Lateur, B.J. The importance of skeletal muscle strength to physical function in older adults. Ann. Behav. Med. 1991, 13, 91–98. [Google Scholar] [CrossRef]
- Tieland, M.; Trouwborst, I.; Clark, B.C. Skeletal muscle performance and ageing. J. Cachex-Sarcopenia Muscle 2018, 9, 3–19. [Google Scholar] [CrossRef]
- Vandervoort, A.A.; Hayes, K.C.; Blanger, A. Strength and endurance of skeletal muscle in the elderly. Physiother. Can. 1986, 38, 167–173. [Google Scholar] [CrossRef]
- Ikeda, K.; Horie-Inoue, K.; Inoue, S. Functions of estrogen and estrogen receptor signaling on skeletal muscle. J. Steroid Biochem. Mol. Biol. 2019, 191, 105375. [Google Scholar] [CrossRef] [PubMed]
- Adamo, S.; Pigna, E.; Lugarà, R.; Moresi, V.; Coletti, D.; Bouché, M. Skeletal muscle: A significant novel neurohypophyseal hormone-secreting organ. Front. Physiol. 2019, 9, 1885. [Google Scholar] [CrossRef]
- Sipilä, S.; Narici, M.; Kjaer, M.; Pöllänen, E.; Atkinson, R.A.; Hansen, M.; Kovanen, V. Sex hormones and skeletal muscle weakness. Biogerontology 2013, 14, 231–245. [Google Scholar] [CrossRef]
- Alexander, S.E.; Pollock, A.C.; Lamon, S. The effect of sex hormones on skeletal muscle adaptation in females. Eur. J. Sport Sci. 2022, 22, 1035–1045. [Google Scholar] [CrossRef]
- Kitajima, Y.; Ono, Y. Estrogens maintain skeletal muscle and satellite cell functions. J. Endocrinol. 2016, 229, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Velloso, C.P. Regulation of muscle mass by growth hormone and IGF-I. Br. J. Pharmacol. 2008, 154, 557–568. [Google Scholar] [CrossRef] [PubMed]
- Pierce, J.R.; Clark, B.C.; Ploutz-Snyder, L.L.; Kanaley, J.A. Growth hormone and muscle function responses to skeletal muscle ischemia. J. Appl. Physiol. 2006, 101, 1588–1595. [Google Scholar] [CrossRef] [PubMed]
- Robinson, D.P.; Klein, S.L. Pregnancy and pregnancy-associated hormones alter immune responses and disease pathogenesis. Horm. Behav. 2012, 62, 263–271. [Google Scholar] [CrossRef]
- Burger, H.G.; Dudley, E.C.; Robertson, D.M.; Dennerstein, L. Hormonal changes in the menopause transition. Recent Prog. Horm. Res. 2002, 57, 257–276. [Google Scholar] [CrossRef] [PubMed]
- Buckler, H. The menopause transition: Endocrine changes and clinical symptoms. Br. Menopause Soc. J. 2005, 11, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Takkouche, B.; Norman, G. PRISMA statement. Epidemiology 2011, 22, 128. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; University of Ottawa: Ottawa, ON, Canada, 2000. [Google Scholar]
- Armijo-Olivo, S.; Stiles, C.R.; Hagen, N.A.; Biondo, P.D.; Cummings, G.G. Assessment of study quality for systematic reviews: A comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: Methodological research. J. Eval. Clin. Pract. 2012, 18, 12–18. [Google Scholar] [CrossRef]
- Ramos, E.; Frontera, W.R.; Llopart, A.; Feliciano, D. Muscle Strength and Hormonal Levels in Adolescents: Gender Related Differences. Int. J. Sports Med. 1998, 19, 526–531. [Google Scholar] [CrossRef]
- Round, J.M.; Jones, D.A.; Honour, J.W.; Nevill, A.M. Hormonal factors in the development of differences in strength between boys and girls during adolescence: A longitudinal study. Ann. Hum. Biol. 1999, 26, 49–62. [Google Scholar] [CrossRef]
- Laddu, D.R.; Farr, J.N.; Lee, V.R.; Blew, R.M.; Stump, C.; Houtkooper, L.; Lohman, T.G.; Going, S.B. Muscle density predicts changes in bone density and strength: A prospective study in girls. J. Musculoskelet. Neuronal Interact. 2014, 14, 195–204. [Google Scholar] [PubMed]
- Tiidus, P.M.; Lowe, D.A.; Brown, M. Estrogen replacement and skeletal muscle: Mechanisms and population health. J. Appl. Physiol. 2013, 115, 569–578. [Google Scholar] [CrossRef] [PubMed]
- Collins, B.C.; Laakkonen, E.K.; Lowe, D.A. Aging of the musculoskeletal system: How the loss of estrogen impacts muscle strength. Bone 2019, 123, 137–144. [Google Scholar] [CrossRef]
- Boisseau, N.; Delamarche, P. Metabolic and Hormonal Responses to Exercise in Children and Adolescents. Sports Med. 2000, 30, 405–422. [Google Scholar] [CrossRef]
- Varlamov, O.; Bethea, C.L.; Roberts, C.T., Jr. Sex-specific differences in lipid and glucose metabolism. Front. Endocrinol. 2015, 5, 241. [Google Scholar] [CrossRef]
- Campbell, K.L.; Westerlind, K.C.; Harber, V.J.; Bell, G.J.; Mackey, J.R.; Courneya, K.S. Effects of Aerobic Exercise Training on Estrogen Metabolism in Premenopausal Women: A Randomized Controlled Trial. Cancer Epidemiol. Biomark. Prev. 2007, 16, 731–739. [Google Scholar] [CrossRef]
- Hausswirth, C.; Le Meur, Y. Physiological and nutritional aspects of post-exercise recovery: Specific recommendations for female athletes. Sports Med. 2011, 41, 861–882. [Google Scholar] [CrossRef]
- Williams, T.; Walz, E.; Lane, A.; Pebole, M.; Hackney, A. The effect of estrogen on muscle damage biomarkers following prolonged aerobic exercise in eumenorrheic women. Biol. Sport 2015, 32, 193–198. [Google Scholar] [CrossRef]
- Baird, M.F.; Graham, S.M.; Baker, J.S.; Bickerstaff, G.F. Creatine-Kinase- and Exercise-Related Muscle Damage Implications for Muscle Performance and Recovery. J. Nutr. Metab. 2012, 2012, 960363. [Google Scholar] [CrossRef]
- Ackerman, K.E.; Singhal, V.; Baskaran, C.; Slattery, M.; Reyes, K.J.C.; Toth, A.; Eddy, K.T.; Bouxsein, M.L.; Lee, H.; Klibanski, A.; et al. Oestrogen replacement improves bone mineral density in oligo-amenorrhoeic athletes: A randomised clinical trial. Br. J. Sports Med. 2019, 53, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Prior, J.C. Adolescents’ Use of Combined Hormonal Contraceptives for Menstrual Cycle–Related Problem Treatment and Contraception: Evidence of Potential Lifelong Negative Reproductive and Bone Effects. Women’s Reprod. Health 2016, 3, 73–92. [Google Scholar] [CrossRef]
- Küüsmaa-Schildt, M. Combined Strength and Endurance Training: Effect of Training Order and Time-of-Day on Adaptations in Neuromuscular and Cardiorespiratory Performance, Muscle Hypertrophy, Serum Hormone Concentrations and Wellbeing. Doctoral Dissertations, University of Jyväskylä, Jyväskylä, Finland, 2019. [Google Scholar]
- Stathopoulou, G.; Powers, M.B.; Berry, A.C.; Smits, J.A.J.; Otto, M.W. Exercise Interventions for Mental Health: A Quantitative and Qualitative Review. Clin. Psychol. Sci. Pract. 2006, 13, 179–193. [Google Scholar] [CrossRef]
- Pallavi, L.C.; SoUza, U.J.D.; Shivaprakash, G. Assessment of musculoskeletal strength and levels of fatigue during different phases of menstrual cycle in young adults. J. Clin. Diagn. Res. JCDR 2017, 11, CC11. [Google Scholar] [CrossRef] [PubMed]
- Romero-Moraleda, B.; Del Coso, J.; Gutiérrez-Hellín, J.; Ruiz-Moreno, C.; Grgic, J.; Lara, B. The Influence of the Menstrual Cycle on Muscle Strength and Power Performance. J. Hum. Kinet. 2019, 68, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Beetham, K.S.; Giles, C.; Noetel, M.; Clifton, V.; Jones, J.C.; Naughton, G. The effects of vigorous intensity exercise in the third trimester of pregnancy: A systematic review and meta-analysis. BMC Pregnancy Childbirth 2019, 19, 281. [Google Scholar] [CrossRef]
- Harvey, N.C.; Moon, R.J.; Sayer, A.A.; Ntani, G.; Davies, J.H.; Javaid, M.K.; Southampton Women’s Survey Study Group. Maternal antenatal vitamin D status and offspring muscle development: Findings from the Southampton Women’s Survey. J. Clin. Endocrinol. Metab. 2014, 99, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Myllyaho, M.M.; Ihalainen, J.K.; Hackney, A.C.; Valtonen, M.; Nummela, A.; Vaara, E.; Häkkinen, K.; Kyröläinen, H.; Taipale, R.S. Hormonal Contraceptive Use Does Not Affect Strength, Endurance, or Body Composition Adaptations to Combined Strength and Endurance Training in Women. J. Strength Cond. Res. 2021, 35, 449–457. [Google Scholar] [CrossRef]
- Nolan, D.; McNulty, K.L.; Manninen, M.; Egan, B. The Effect of Hormonal Contraceptive Use on Skeletal Muscle Hypertrophy, Power and Strength Adaptations to Resistance Exercise Training: A Systematic Review and Multilevel Meta-analysis. Sports Med. 2024, 54, 105–125. [Google Scholar] [CrossRef] [PubMed]
- Sabatini, R.; Cagiano, R.; Rabe, T. Adverse effects of hormonal contraception. J. Reprod. Med. Endocrinol. 2011, 8, 130–156. [Google Scholar]
- SantaBarbara, K. Effects of the Menstrual Cycle and Mitigating its Impact in Resistance-Trained Women. Ph.D. Thesis, Auckland University of Technology, Auckland, New Zealand, 2023. [Google Scholar]
- Sung, E.; Han, A.; Hinrichs, T.; Vorgerd, M.; Manchado, C.; Platen, P. Effects of follicular versus luteal phase-based strength training in young women. SpringerPlus 2014, 3, 668. [Google Scholar] [CrossRef]
- Kissow, J.; Jacobsen, K.J.; Gunnarsson, T.P.; Jessen, S.; Hostrup, M. Effects of Follicular and Luteal Phase-Based Menstrual Cycle Resistance Training on Muscle Strength and Mass. Sports Med. 2022, 52, 2813–2819. [Google Scholar] [CrossRef] [PubMed]
- Kochi, M.N.; Marques, N.R.; da Costa, G.D.C.; Reis, J.G.; de Paula, F.J.A.; Ferreiral, C.H.J.; de Abreu, D.C.C. Impact of first 10 years of post menopause on muscle function, muscle mass and bone mineral density in adult women. J. Osteopor. Phys. Act. 2015, 3, 2. [Google Scholar]
- Greeves, J.P.; Cable, N.T.; Reilly, T.; Kingsland, C. Changes in muscle strength in women following the menopause: A longitudinal assessment of the efficacy of hormone replacement therapy. Clin. Sci. 1999, 97, 79–84. [Google Scholar] [CrossRef]
- Colombel, A.; Charbonnel, B. Weight gain and cardiovascular risk factors in the post-menopausal woman. Hum. Reprod. 1997, 12 (Suppl. 1), 134–145. [Google Scholar] [CrossRef]
- Pöllänen, E.; Ronkainen, P.H.A.; Suominen, H.; Takala, T.; Koskinen, S.; Puolakka, J.; Sipilä, S.; Kovanen, V. Muscular transcriptome in postmenopausal women with or without hormone replacement. Rejuvenation Res. 2007, 10, 485–500E. [Google Scholar] [CrossRef] [PubMed]
- Kemmler, W.; Wildt, L.; Engelke, K.; Pintag, R.; Pavel, M.; Bracher, B.; Weineck, J.; Kalender, W. Acute hormonal responses of a high impact physical exercise session in early postmenopausal women. Eur. J. Appl. Physiol. 2003, 90, 199–209. [Google Scholar] [CrossRef] [PubMed]
- Holtzman, B.; Ackerman, K.E. Recommendations and nutritional considerations for female athletes: Health and performance. Sports Med. 2021, 51 (Suppl. 1), 43–57. [Google Scholar] [CrossRef] [PubMed]
- Chien, M.Y.; Wu, Y.T.; Hsu, A.T.; Yang, R.S.; Lai, J.S. Efficacy of a 24-week aerobic exercise program for osteopenic postmenopausal women. Calcif. Tissue Int. 2000, 67, 443–448. [Google Scholar] [CrossRef]
- Bea, J.W.; Cussler, E.C.; Going, S.B.; Blew, R.M.; Metcalfe, L.L.; Lohman, T.G. Resistance training predicts six-year body composition change in postmenopausal women. Med. Sci. Sports Exerc. 2010, 42, 1286. [Google Scholar] [CrossRef] [PubMed]
- Isenmann, E.; Kaluza, D.; Havers, T.; Elbeshausen, A.; Geisler, S.; Hofmann, K.; Flenker, U.; Diel, P.; Gavanda, S. Resistance training alters body composition in middle-aged women depending on menopause-A 20-week control trial. BMC Women’s Health 2023, 23, 526. [Google Scholar] [CrossRef]
- Marín-Cascales, E.; Rubio-Arias, J.A.; Romero-Arenas, S.; Alcaraz, P.E. Effect of 12 weeks of whole-body vibration versus multi-component training in post-menopausal women. Rejuvenation Res. 2015, 18, 508–516. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Caguicla, J.M.C.; Park, S.; Kwak, D.J.; Won, D.Y.; Park, Y.; Kim, J.; Kim, M. Effects of 8-week Pilates exercise program on menopausal symptoms and lumbar strength and flexibility in postmenopausal women. J. Exerc. Rehabil. 2016, 12, 247. [Google Scholar] [CrossRef]
- Verlaan, S.; Maier, A.B.; Bauer, J.M.; Bautmans, I.; Brandt, K.; Donini, L.M.; Maggio, M.; McMurdo, M.E.; Mets, T.; Seal, C.; et al. Sufficient levels of 25-hydroxyvitamin D and protein intake required to increase muscle mass in sarcopenic older adults—The PROVIDE study. Clin. Nutr. 2018, 37, 551–557. [Google Scholar] [CrossRef]
- Dewansingh, P.; Melse-Boonstra, A.; Krijnen, W.P.; van der Schans, C.P.; Jager-Wittenaar, H.; van den Heuvel, E.G. Supplemental protein from dairy products increases body weight and vitamin D improves physical performance in older adults: A systematic review and meta-analysis. Nutr. Res. 2018, 49, 1–22. [Google Scholar] [CrossRef]
- Armstrong, A.L.; Oborne, J.; Coupland, C.A.; MacPherson, M.B.; Bassey, E.J.; Wallace, W.A. Effects of hormone replacement therapy on muscle performance and balance in post-menopausal women. Clin. Sci. 1996, 91, 685–690. [Google Scholar] [CrossRef] [PubMed]
- Carville, S.F.; Rutherford, O.M.; Newham, D.J. Power output, isometric strength and steadiness in the leg muscles of pre-and postmenopausal women; the effects of hormone replacement therapy. Eur. J. Appl. Physiol. 2006, 96, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Ribom, E.L.; Piehl-Aulin, K.; Ljunghall, S.; Ljunggren, Ö.; Naessén, T. Six months of hormone replacement therapy does not influence muscle strength in postmenopausal women. Maturitas 2002, 42, 225–231. [Google Scholar] [CrossRef]
- Jacobsen, D.E.; Samson, M.M.; Kezic, S.; Verhaar, H.J.J. Postmenopausal HRT and tibolone in relation to muscle strength and body composition. Maturitas 2007, 58, 7–18. [Google Scholar] [CrossRef] [PubMed]
- Elliott, K.J.; Sale, C.; Cable, N.T. Effects of resistance training and detraining on muscle strength and blood lipid profiles in postmenopausal women. Br. J. Sports Med. 2002, 36, 340–344. [Google Scholar] [CrossRef]
- Nunes, P.R.P.; Barcelos, L.C.; Oliveira, A.A.; Furlanetto Junior, R.; Martins, F.M.; Orsatti, C.L.; Resende, E.A.M.R.; Orsatti, F.L. Effect of resistance training on muscular strength and indicators of abdominal adiposity, metabolic risk, and inflammation in postmenopausal women: Controlled and randomized clinical trial of efficacy of training volume. Age 2016, 38, 1–13. [Google Scholar] [CrossRef]
- Young, V.R.; Pellett, P.L. Protein intake and requirements with reference to diet and health. Am. J. Clin. Nutr. 1987, 45, 1323–1343. [Google Scholar] [CrossRef]
- Volek, J.S. Influence of nutrition on responses to resistance training. Med. Sci. Sports Exerc. 2004, 36, 689–696. [Google Scholar] [CrossRef]
- Desbrow, B.; McCormack, J.; Burke, L.M.; Cox, G.R.; Fallon, K.; Hislop, M.; Logan, R.; Marino, N.; Sawyer, S.M.; Shaw, G.; et al. Sports Dietitians Australia position statement: Sports nutrition for the adolescent athlete. Int. J. Sport Nutr. Exerc. Metab. 2014, 24, 570–584. [Google Scholar] [CrossRef]
- Damanti, S.; Azzolino, D.; Roncaglione, C.; Arosio, B.; Rossi, P.; Cesari, M. Efficacy of nutritional interventions as stand-alone or synergistic treatments with exercise for the management of sarcopenia. Nutrients 2019, 11, 1991. [Google Scholar] [CrossRef]
- Dedeyne, L.; Dupont, J.; Koppo, K.; Verschueren, S.; Tournoy, J.; Gielen, E. Exercise and Nutrition for Healthy AgeiNg (ENHANce) project–effects and mechanisms of action of combined anabolic interventions to improve physical functioning in sarcopenic older adults: Study protocol of a triple blinded, randomized controlled trial. BMC Geriatr. 2020, 20, 532. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.A.F. Combined exercise and dietary intervention to optimize body composition in aging. Ann. N. Y. Acad. Sci. 1998, 854, 378–393. [Google Scholar] [CrossRef] [PubMed]
- Davitt, P.M.; Pellegrino, J.K.; Schanzer, J.R.; Tjionas, H.; Arent, S.M. The effects of a combined resistance training and endurance exercise program in inactive college female subjects: Does order matter? J. Strength Cond. Res. 2014, 28, 1937–1945. [Google Scholar] [CrossRef] [PubMed]
- Brellenthin, A.G.; Lanningham-Foster, L.M.; Kohut, M.L.; Li, Y.; Church, T.S.; Blair, S.N.; Lee, D.C. Comparison of the cardiovascular benefits of resistance, aerobic, and combined exercise (CardioRACE): Rationale, design, and methods. Am. Heart J. 2019, 217, 101–111. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kodete, C.S.; Thuraka, B.; Pasupuleti, V.; Malisetty, S. Hormonal Influences on Skeletal Muscle Function in Women across Life Stages: A Systematic Review. Muscles 2024, 3, 271-286. https://doi.org/10.3390/muscles3030024
Kodete CS, Thuraka B, Pasupuleti V, Malisetty S. Hormonal Influences on Skeletal Muscle Function in Women across Life Stages: A Systematic Review. Muscles. 2024; 3(3):271-286. https://doi.org/10.3390/muscles3030024
Chicago/Turabian StyleKodete, Chandra Shikhi, Bharadwaj Thuraka, Vikram Pasupuleti, and Saiteja Malisetty. 2024. "Hormonal Influences on Skeletal Muscle Function in Women across Life Stages: A Systematic Review" Muscles 3, no. 3: 271-286. https://doi.org/10.3390/muscles3030024
APA StyleKodete, C. S., Thuraka, B., Pasupuleti, V., & Malisetty, S. (2024). Hormonal Influences on Skeletal Muscle Function in Women across Life Stages: A Systematic Review. Muscles, 3(3), 271-286. https://doi.org/10.3390/muscles3030024









