Facial Burn During Orthognathic Surgery: Case Report
Abstract
:INTRODUCTION
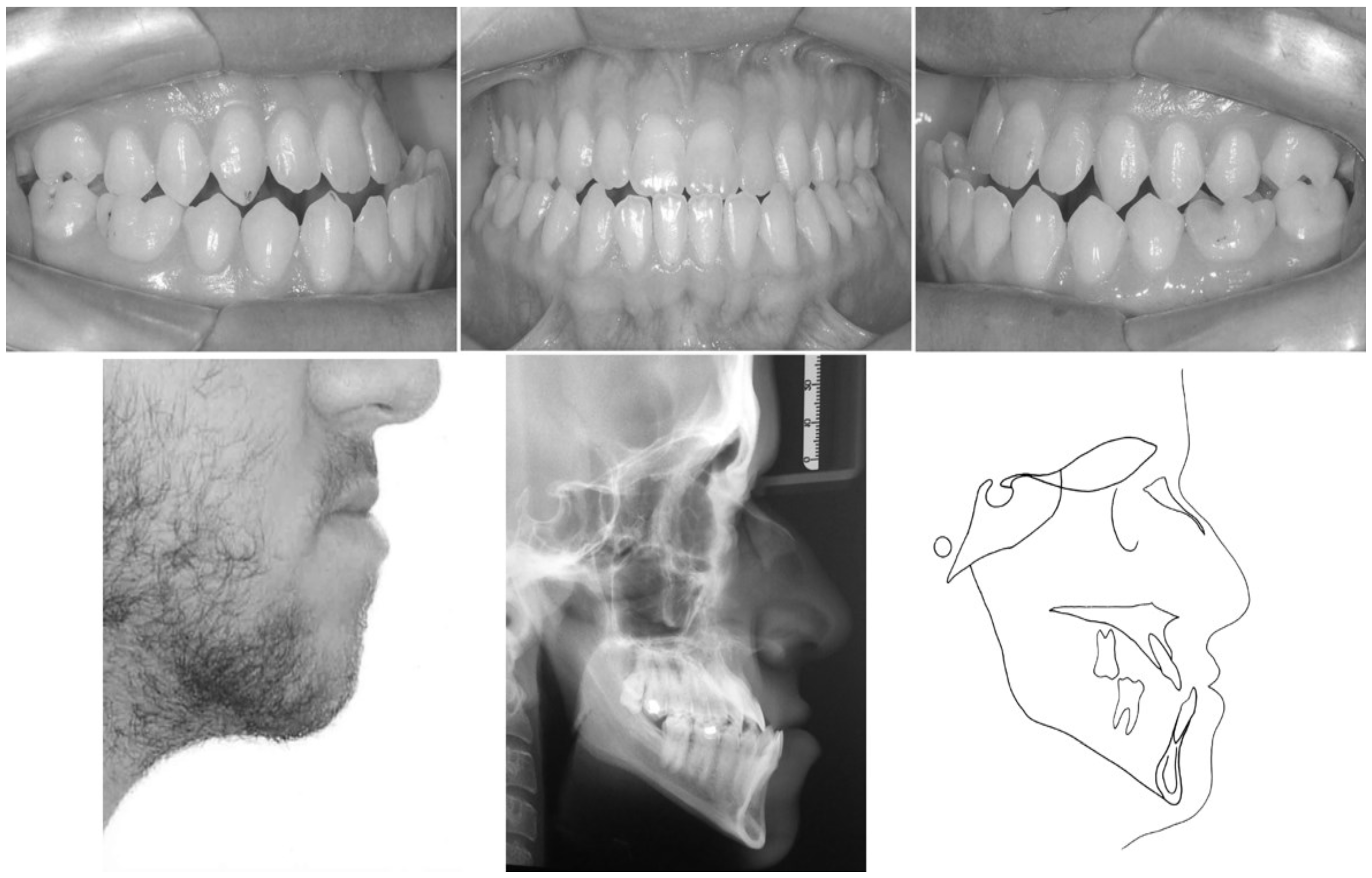
CASE REPORT
DISCUSSION
CONCLUSION
SUPPLEMENTARY MATERIALS
References
- Bays, R.; Bouloux, G. Complications of Orthognathic Surgery. Oral and Maxillofacial Surgery Clinics of North America 2003, 15, 229–42. [Google Scholar] [CrossRef] [PubMed]
- Chow, L. K.; Singh, B.; Chiu, W. K.; Samman, N. Prevalence of Postoperative Complications After Orthognathic Surgery: A 15-Year Review. Journal of Oral Maxillofacial Surgery 2007, 65, 984–92. [Google Scholar] [CrossRef] [PubMed]
- De Mol van Otterloo, J. J.; Tuinzing, D. B.; Greebe, R. B.; Van Der Kwast, W. A. M. Intra- and Early Postoperative Complications of the Le Fort I Osteotomy. A Retrospective Study on 410 Cases. Journal of Cranio-Maxillo-Facial Surgery 1991, 19, 217–22. [Google Scholar] [CrossRef] [PubMed]
- De Queiroz, S. B. F.; Curioso, P. A. B.; Carvalho, F. S. R.; de Lima, V. N. Submandibular-Space Abscess from Loss of a Bonded Molar Tube During Orthognathic Surgery. American Journal of Orthodontics and Dentofacial Orthopedics 2013, 143, 735–7. [Google Scholar] [CrossRef] [PubMed]
- Iannetti, G.; Fadda, T. M.; Riccardi, E.; Mitro, V.; Filiaci, F. Our Experience in Complications of Orthognathic Surgery: A Retrospective Study on 3236 Patients. European Review for Medical and Pharmacological Sciences 2013, 17, 379–84. [Google Scholar] [PubMed]
- Kenji, S.; Yutaka, T.; Makoto, T.; Genji, S. Characterization of Different Paresthesias Following Orthognathic Surgery of The Mandible. Journal of Oral Maxillofacial Surgery 2005, 63, 298–303. [Google Scholar] [CrossRef]
- Kim, J. W.; Chin, B. R.; Park, H. S.; Lee, S. H.; Kwon, T. G. Cranial Nerve Injury After Le Fort I Osteotomy. International Journal of Oral Maxillofacial Surgery 2011, 40, 327–9. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Park, S. Incidence of Complications and Problems Related to Orthognathic Surgery. Journal of Oral Maxillofacial Surgery 2007, 65, 2438–44. [Google Scholar] [CrossRef] [PubMed]
- Lanigan, D. T.; Hey, J. H.; West, R. A. Aseptic Necrosis Following Maxillary Osteotomies: Report of 36 Cases. Journal of Oral Maxillofacial Surgery 1990, 48, 142–56. [Google Scholar] [CrossRef] [PubMed]
- Lanigan, D. T.; Hey, J. H.; West, R. A. Major Vascular Complications of Orthognathic Surgery: Hemorrhage Associated with Le Fort I Osteotomies. Journal of Oral Maxillofacial Surgery 1990, 48, 561–73. [Google Scholar] [CrossRef] [PubMed]
- Lanigan, D. T.; Romanchuk, K.; Olson, C. K. Ophthalmic Complications Associated With Orthognathic Surgery. Journal of Oral Maxillofacial Surgery 1993, 51, 480–94. [Google Scholar] [CrossRef] [PubMed]
- Laureano Filho, J. R.; Godoy, F.; O’Ryan, F. Orthodontic Bracket Lost in The Airway During Orthognathic Surgery. American Journal of Orthodontics and Dentofacial Orthopedics 2008, 134, 288–90. [Google Scholar] [CrossRef] [PubMed]
- Morris, D.; Lo, L. J.; Margulis, A. Pitfalls in Orthognathic Surgery: Avoidance and Management of Complications. Clinics in Plastic Surgery 2007, 34, e17–29. [Google Scholar] [CrossRef] [PubMed]
- Panula, K.; Finne, K.; Oikarinen, K. Incidence of Complications and Problems Related to Orthognathic Surgery: A Review of 655 Patients. Journal of Oral Maxillofacial Surgery 2001, 59, 1128–36. [Google Scholar] [CrossRef] [PubMed]
- Piñeiro-Aguilar, A.; Somoza-Martín, M.; Gandara-Rey, J. M.; García-García, A. J. Blood Loss in Orthognathic Surgery: A Systematic Review. Journal of Oral Maxillofacial Surgery 2011, 69, 885–92. [Google Scholar] [CrossRef] [PubMed]
- Robl, M. T.; Farrell, B. B.; Tucker, M. R. Complications in Orthognathic Surgery A Report of 1000 Cases. Oral and Maxillofacial Surgery Clinics of North America 2014, 26, 599–609. [Google Scholar] [CrossRef] [PubMed]
- Steel, B. J.; Cope, M. R. Unusual and Rare Complications of Orthognathic Surgery: A Literature Review. Journal of Oral Maxillofacial Surgery 2012, 70, 1678–91. [Google Scholar] [CrossRef] [PubMed]
- Teltzrow, T.; Kramer, F. J.; Schulze, A.; Baethge, C.; Brachvogel, P. Perioperative complications following sagittal split osteotomy of the mandible. Journal of Cranio-Maxillo-Facial Surgery 2005, 33, 307–13. [Google Scholar] [CrossRef] [PubMed]
- Van de Perre, J. P.; Stoelinga, P. J.; Blijdorp, P. A.; Brouns, J. J.; Hoppenreijs, T. J. Perioperative Morbidity in Maxillofacial Orthopedic Surgery: Retrospective Study. Journal of Cranio-Maxillo-Facial Surgery 1996, 24, 263–70. [Google Scholar] [CrossRef] [PubMed]
- Watts, P. G. Unilateral Abducent Nerve Palsy: A Rare Complications Following Le Fort I Osteotomy. British Journal of Oral and Maxillofacial Surgery 1984, 22, 212. [Google Scholar] [CrossRef] [PubMed]


© 2018 by the authors. 2018 Jéssica Cristina Avelar, Marcio José da Silva Campos, Raphaella Barcellos Fernandes, Sérgio Luiz da Mota Júnior, Marcelo Reis Fraga, Robert Willer Farinazzo Vitral
Share and Cite
Avelar, J.C.; da Silva Campos, M.J.; Fernandes, R.B.; da Mota Júnior, S.L.; Fraga, M.R.; Vitral, R.W.F. Facial Burn During Orthognathic Surgery: Case Report. Int. J. Orofac. Myol. Myofunct. Ther. 2018, 44, 42-51. https://doi.org/10.52010/ijom.2018.44.1.3
Avelar JC, da Silva Campos MJ, Fernandes RB, da Mota Júnior SL, Fraga MR, Vitral RWF. Facial Burn During Orthognathic Surgery: Case Report. International Journal of Orofacial Myology and Myofunctional Therapy. 2018; 44(1):42-51. https://doi.org/10.52010/ijom.2018.44.1.3
Chicago/Turabian StyleAvelar, Jéssica Cristina, Marcio José da Silva Campos, Raphaella Barcellos Fernandes, Sérgio Luiz da Mota Júnior, Marcelo Reis Fraga, and Robert Willer Farinazzo Vitral. 2018. "Facial Burn During Orthognathic Surgery: Case Report" International Journal of Orofacial Myology and Myofunctional Therapy 44, no. 1: 42-51. https://doi.org/10.52010/ijom.2018.44.1.3
APA StyleAvelar, J. C., da Silva Campos, M. J., Fernandes, R. B., da Mota Júnior, S. L., Fraga, M. R., & Vitral, R. W. F. (2018). Facial Burn During Orthognathic Surgery: Case Report. International Journal of Orofacial Myology and Myofunctional Therapy, 44(1), 42-51. https://doi.org/10.52010/ijom.2018.44.1.3



