Poster 4: Multitasking Properties of Some Orofacial Muscles
Abstract
INTRODUCTION
Genioglossus (GG)
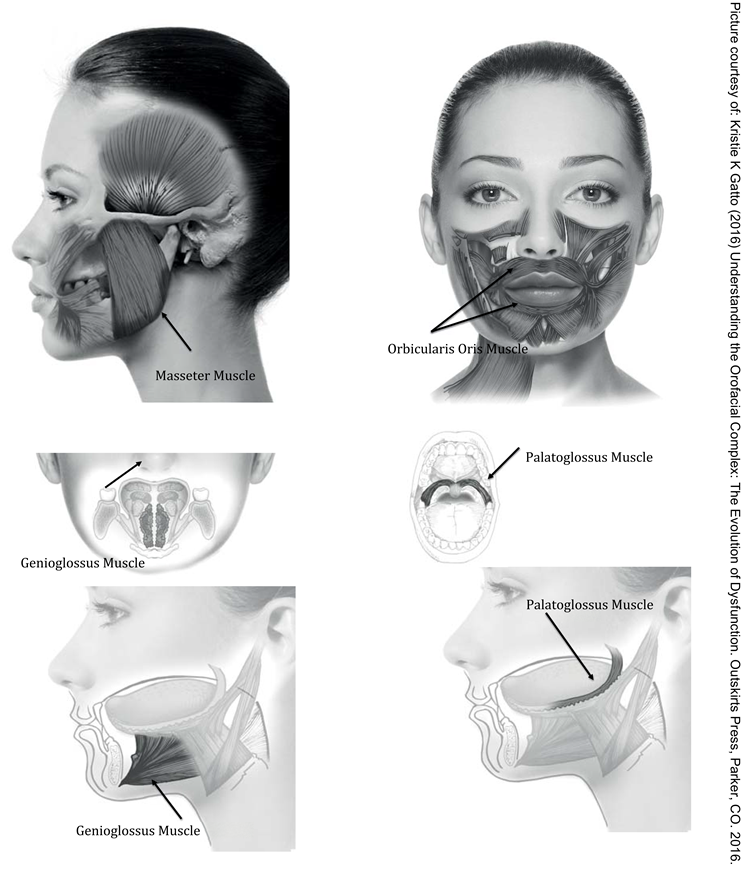
Palatoglossus (PG)
Masseters (MM)
Orbicularis Oris
References
- Arens, R.; Marcus, C. L. Pathophysiology of upper airway obstruction: A developmental perspective. Sleep 2003, 27, 997–1019. [Google Scholar]
- Baumgartner, C.; Barth, D. S.; Levesque, M. F.; Sutherling, W. W. Human hand and lip sensorimotor cortex as studied on electrocorticography. Electroencephalography Clinical Neurophysiology 1992, 84(2), 115–126. [Google Scholar] [CrossRef] [PubMed]
- Busanello-Stella, A. R.; Blanco-Dutra, A. P.; Corrêa, E. C.; Silva, A. M. Electromyographic fatigue of orbicular oris muscles during exercises in mouth and nasal breathing children. CoDAs 2015, 27(1), 80–88, [Article in English, Portuguese]. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Clark, H. M. Neuromuscular treatments for speech and swallowing: A tutorial. American Journal of Speech Language Pathology 2003, 12, 400–415. [Google Scholar]
- De Felício, C. M.; Ferreira, C. L.; Medeiros, A. P.; Rodrigues Da Silva, M. A.; Tartaglia, G. M.; Sforza, C. Electromyographic indices, orofacial myofunctional status and temporomandibular disorders severity: A correlation study. Journal of Electromyography Kinesiology 2012, 22(2), 266–272. [Google Scholar]
- Eastwood, P. R.; Curran, A. K.; Smith, C. A.; Dempsey, J. A. Effect of upper airway negative pressure on inspiratory drive during sleep. Journal of Applied Physiology 1998, 84, 1063–1075. [Google Scholar]
- Engelke, W.; Jung, K.; Knosel, M.W.E. Intra-oral compartment pressures: A biofunctional model and experimental measurements under different conditions of posture. Journal of Clinical Oral Investigations 2011, 15(2), 165–176. [Google Scholar]
- Escudiero Santos, C.; de Freitas, O.; Spadaro, A. C. C.; Mestriner-Junior, W. Development of a Colorimetric System for Evaluation of the Masticatory Efficiency. Brazilian Dental Journal 2006, 17(2), 9599. [Google Scholar]
- Fitzpatrick, M. F.; McLean, H.; Urton, A. M.; Tan, A.; O’Donnell, D.; Driver, H. S. Effect of nasal or oral breathing route on upper airway resistance during sleep. European Respiratory Journal 2003, 22, 827–832. [Google Scholar]
- Fogel, R. B.; Malhotra, A.; White, P. Pathophysiology of obstructive sleep Apnoea/Hypopnoea Syndrome. Thorax 2004, 59, 159–163. [Google Scholar] [CrossRef]
- Gallo, L. M.; Gross, S. S.; Palla, S. Nocturnal masseter activity of healthy subjects in a natural environment. Journal of Dental Research 1999, 78, 1436–1444. [Google Scholar] [PubMed]
- Gatto, K.K. Understanding the orofacial complex: The evolution of dysfunction; Outskirts Press, 2016. [Google Scholar]
- Gómez, F.M.; Ortega, J.E.; Horrillo, I.; Meana, J.J. Relationship between non-functional masticatory activity and central dopamine in stressed rats. Journal of Oral Rehabilitation 2010, 37, 827–833. [Google Scholar] [PubMed]
- Guimarães, K.C.; Drager, L.F.; Genta, P.R.; Marcondes, B.F.; Lorenzi-Filho, G. Effects of Oropharyngeal Exercises on Patients with Moderate Obstructive Sleep Apnea Syndrome. American Journal of Respiratory and Critical Care Medicine 2009, 15, 179 & 962–966. [Google Scholar]
- Hyama, S.; Ono, T.; Ishiwata, Y.; Kuroda, T.; Ohyama, K. Effects of experimental nasal obstruction on human masseter and suprahyoid muscle activities during sleep. Angle Orthodontist 2003, 73(2), 151–157. [Google Scholar]
- Hori, N.; Lee, M. C.; Sasaguri, K.; Ishii, H.; Kamei, M.; Kimoto, K.; Toyoda, M.; Sato, S. Suppression of Stress-induced nNOS Expression in the Rat Hypothalamus by Biting. Journal of Dental Research 2005, 84(7), 624–628. [Google Scholar]
- Jordan, A. S.; White, D. P.; Lo, Y. L.; Wellman, A.; Eckert, D. J.; Yim-Yeh, S.; Eikermann, M.; Smith, S. A.; Stevenson, K. E.; Malhotra, A. Airway Dilator Muscle Activity and Lung Volume During Stable Breathing in Obstructive Sleep Apnea. Sleep 2009, 32(3), 361–368. [Google Scholar]
- Malhotra, A.; Pillar, G.; Fogel, R. B.; Edwards, J. K.; Ayas, N.; Akahoshi, T.; Hess, D.; White, D. P. Pharyngeal pressure and flow effects on genioglossus activation in normal subjects. American Journal of Respiratory Critical Care and Medicine 2002, 165, 71–77. [Google Scholar]
- Mathur, R.; Mortimore, I. L.; Jan, M. A.; Douglas, N. J. Effect of breathing, pressure and posture on palatoglossal and genioglossal tone. Clinical Science 1995, 89, 441–445. [Google Scholar]
- McFarland, D. H.; Lund, J. P. Modification of mastication and respiration during swallowing in the adult human. Journal of Neurophysiology 1995, 74, 1509–1517. [Google Scholar]
- McFarland, D. H.; Lund, J. P.; Gagner, M. Effects of posture on the coordination of respiration and swallowing. Journal of Neurophysiology 1994, 72, 2431–2437. [Google Scholar]
- Miles, T. S.; Flavel, S. C.; Nordstrom, M. A. Stretch reflexes in the human masticatory muscles: A brief review and a new functional role. Human Movement Science 2004, 40, 337–349. [Google Scholar] [CrossRef] [PubMed]
- Miles, T. S. Postural control of the human mandible. Archives of Oral Biology 2007, 52(4), 347–352. [Google Scholar] [CrossRef] [PubMed]
- Mortimore, I. L.; Mathur, R.; Douglas, N. J. Effect of posture, route of respiration, and negative pressure on palatal muscle activity in humans. Journal of Applied Physiology 1995, 79(2), 448–454. [Google Scholar] [CrossRef] [PubMed]
- Napadow, V. J.; Chen, Q.; Weeden, V. J.; Gilbert, R. J. Intramural mechanics of the human tongue in association with physiological deformation. Journal of Biomechanics 1999, 32, 1–12. [Google Scholar] [CrossRef]
- Patil, S.P.; Schneider, H.; Marx, J.J.; Gladmon, E.; Schwartz, A.R.; Smith, P.L. Neuromechanical Control of Upper Airway Patency During Sleep. Journal of Applied Physiology 2006, 102(2), 547–556. [Google Scholar] [CrossRef]
- Popovic, R.M.; White, D.P. Influence of waking genioglossal electromyogram and upper airway resistance. American Journal of Respiratory Critical Care and Medicine 1995, 152, 725–731. [Google Scholar] [CrossRef]
- Saboisky, J. P.; Butler, J. E.; Fogel, R. B.; Taylor, J. L.; Trinder, J. A.; White, D. P.; Gandevia, S. C. Tonic and Phasic Respiratory Drives to Human Genioglossus Motoneurons During Breathing. Journal of Neurophysiology 2006, 95(4), 2213–2221. [Google Scholar] [CrossRef]
- Sant’Ambrogio, G.; Tsubone, H.; Sant’Ambrogio, F. B. Sensory information from the upper airway: Role in the control of breathing. Respiratory Physiology 1995, 1021-16. [Google Scholar] [CrossRef]
- Sawczuk, A.; Mosier, K. M. Neural Control of Tongue Movement With Respect To Respiration and Swallowing. Critical Reviews in Oral Biology & Medicine 2001, 12(l), 18–37. [Google Scholar]
- Shea, S. A.; Edwards, J. K.; White, D. P. Effect of wake-sleep transitions and rapid eye movement sleep on pharyngeal muscle response to negative pressure in humans. Journal of Physiology 1999, 520 Pt 3, 897–908. [Google Scholar] [CrossRef]
- Tartaglia, G. M.; Lodetti, G.; Paiva, G.; De Felicio, C. M.; Sforza, C. Surface electromyographic assessment of patients with long lasting temporomandibular joint disorder pain. Journal of Electromyography and Kinesiology 2011, 21(4), 659–64. [Google Scholar] [CrossRef]
- Toda, T.; Taoka, M. Integration of the upper and lower lips in the postcentral area 2 of conscious macaque monkeys (Macaca fuscata). Archives of Oral Biology 2002, 47(6), 449–456. [Google Scholar] [CrossRef]
© 2016 by the author. 2016 Licia Coceani Paskay
Share and Cite
Paskay, L.C. Poster 4: Multitasking Properties of Some Orofacial Muscles. Int. J. Orofac. Myol. Myofunct. Ther. 2016, 42, 61-65. https://doi.org/10.52010/ijom.2016.42.1.8
Paskay LC. Poster 4: Multitasking Properties of Some Orofacial Muscles. International Journal of Orofacial Myology and Myofunctional Therapy. 2016; 42(1):61-65. https://doi.org/10.52010/ijom.2016.42.1.8
Chicago/Turabian StylePaskay, Lucia Coceani. 2016. "Poster 4: Multitasking Properties of Some Orofacial Muscles" International Journal of Orofacial Myology and Myofunctional Therapy 42, no. 1: 61-65. https://doi.org/10.52010/ijom.2016.42.1.8
APA StylePaskay, L. C. (2016). Poster 4: Multitasking Properties of Some Orofacial Muscles. International Journal of Orofacial Myology and Myofunctional Therapy, 42(1), 61-65. https://doi.org/10.52010/ijom.2016.42.1.8



