Abstract
The Interdisciplinary Orofacial Examination Protocol for Children and Adolescents (Protocolo de exploración interdisciplinaria orofacial para niños y adolescents, Barcelona, 2008) is very useful in providing a fast, initial, expedient detection of possible morphological and functional disorders, and to guide the patient toward the appropriate professionals. With this tool it is possible to detect the risk factors which can negatively affect morphological and functional harmony and guide patients toward the necessary treatment as early as possible. This Protocol, developed by 4 orthodontists, 1 ENT and 3 speech language therapists, also contributes to the unification of concepts and nomenclature used by distinct specialists, thus making professional understanding easier and more dynamic.
INTRODUCTION
The intervention to treat alterations and dysfunctions of the stomatognatic system (SS) isn’t always conducted at the most opportune moment, since the patient often arrives after their dysfunctions have been present for some time. Also, these dysfunctions may have led to a dental malocclusion or aggravated a pre-existing malocclusion. On the other hand, one of the most serious difficulties frequently experienced by the different professionals who work with the stomatognatic system is the absence of a common interdisciplinary code, be it for the patient evaluation or establishing of a course of action. Certainly, diagnosis and treatment would be easier with an interdisciplinary detection of the morphological alterations and dysfunctions of the stomatognatic system, as well as a common interdisciplinary terminology and classification system.
To facilitate the achievement of these goals, a resource was created by a team of professionals from Barcelona in 2008. The team consisted of an ENT (Jordi Coromina), four orthodontists (Pablo Echarri, Alberto Carrasco, Elsa Bottini & Emma Vila) and three speech language pathologists (Graciela Donato, Lyda Lapitz & Diana Grandi) who live in Catalonia, Spain. This resource, the Interdisciplinary Orofacial Examination Protocol For Children and Adolescents was designed for the fast, easy detection of possible morphological alterations and orofacial dysfunctions of the SS. It was not intended to be a diagnostic tool, but simply an aid for initial detection. After this initial detection, the patient can be directed to the appropriate professional/s responsible for conducting both the diagnosis and treatment.
This protocol was first introduced at the 5th Speech Therapy and Odontology Workshop at the Mediterranean Dentistry Forum in Barcelona, January 2009. Since that time it has become widely used by professionals from diverse disciplines, especially odontologists, ENTs, paediatricians and speech therapists. It is also a very useful resource for speech therapists who are not specialized in the orofacial myofunctional area.
In August 2010, the Protocol was presented at the 39th Convention of the International Association of Orofacial Myology (IAOM) held in Sao Paulo, Brazil. It was well received by attendees, who inquired of members of the Convention Committee as to how the Protocol could be obtained for their use. For this reason and with great pleasure, the authors would like to share it with all the members of the IAOM, as well as any other professionals who would like to use it. It is hoped that this will help facilitate detection, diagnosis and treatment of stomatognatic system alterations and dysfunctions, while promoting further interdisciplinary study and investigation in this field.
INSTRUCTIONS FOR USING THE PROTOCOL
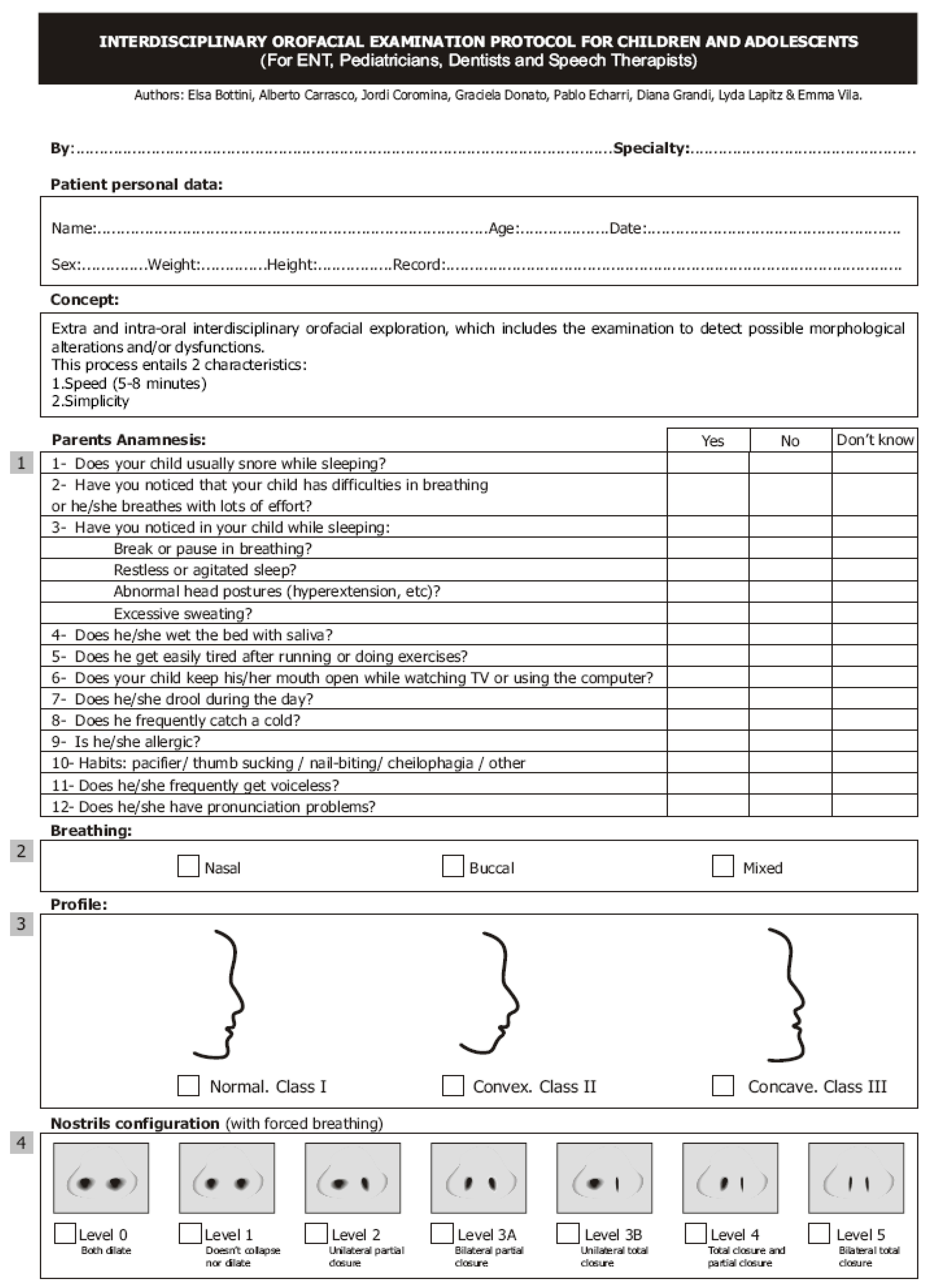
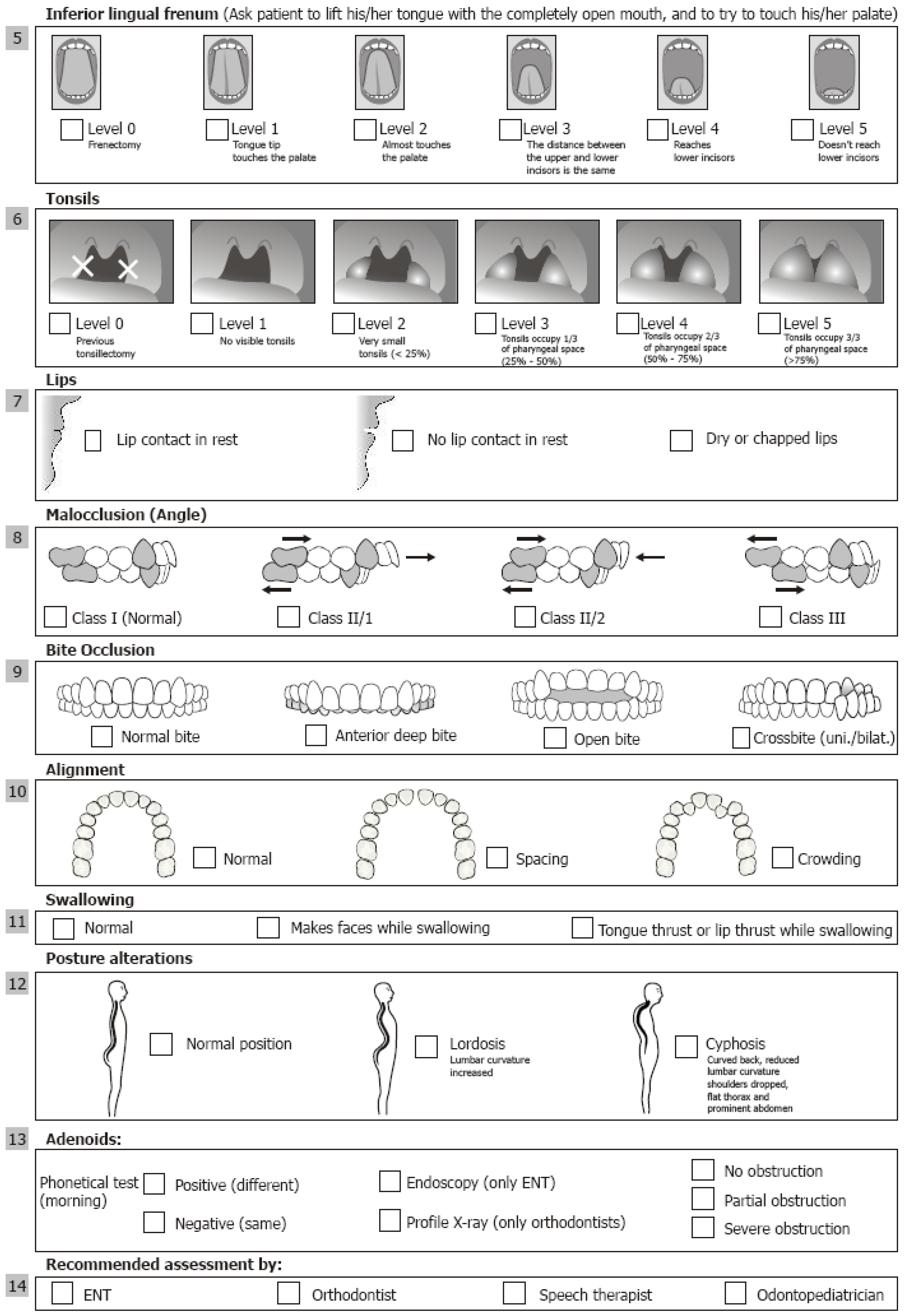
The Protocol is a two page document consisting of 13 items (aside from items pertaining to personal information such as name, age), that can be quickly completed. Its sole requirement is clinical observation, as it includes no other types of exploration or examination. The Protocol for Children and Adolescents is provided in Appendix A and the different items and their use are described in this article, accompanied by some graphics to aid in observation and use. The adult version of the Protocol is provided in Appendix B.
The alteration of a factor is cause for referral to different professionals. So, for each of the 13 factors or items, consideration is given to which professional the patient should be referred.
The authors have also codified the different factors, giving each a specific point value. This is not necessary to do at the time the Protocol is completed, but is of use for the diverse scientific studies that may be conducted thereafter. A value of 0 is given to those factors which exhibit no alteration, while other codes are used to assign a value to the alterations of distinct factors.
- 1.
- Parents Anamnesis:
This section consists of 12 questions which are intended to obtain basic information about possible key signs related to the SS, such as type of respiration, presence of deleterious sucking habits and phono-articulatory disorders. Responses to these questions may be: Yes, No or Unknown.
Patients with alterations in questions 1 to 9 must be directed to an ENT, pediatrician and/or speech therapist. Patients with alterations in question 10 must be directed to an odontologist and a speech therapist. Patients with alterations in questions 11-12 must be directed to a speech therapist. The point system assigns a value of 0 to answers of “No”, a value of 1 to answers of “Yes”, and a value of 2 to answers of “Unknown”.
- 2.
- Breathing:
This section focuses on determining the patient’s respiratory pattern: nasal, oral or mixed. The respiratory pattern may be modified due to obstructions or habits, which puts in motion a chain reaction of alterations that affect the SS; which may in turn, affect the patient’s quality of life and craneofacial growth and development.
Patients with respiratory alteration must be directed to an ENT and a speech therapist. The point system assigns a value of 0 to nasal respiration, a value of 1 to mixed respiration, and a value of 2 to oral respiration.
- 3.
- Profile:
Three types of facial profiles are considered, based on the profile classification conducted by Dr. Arnett (1993).
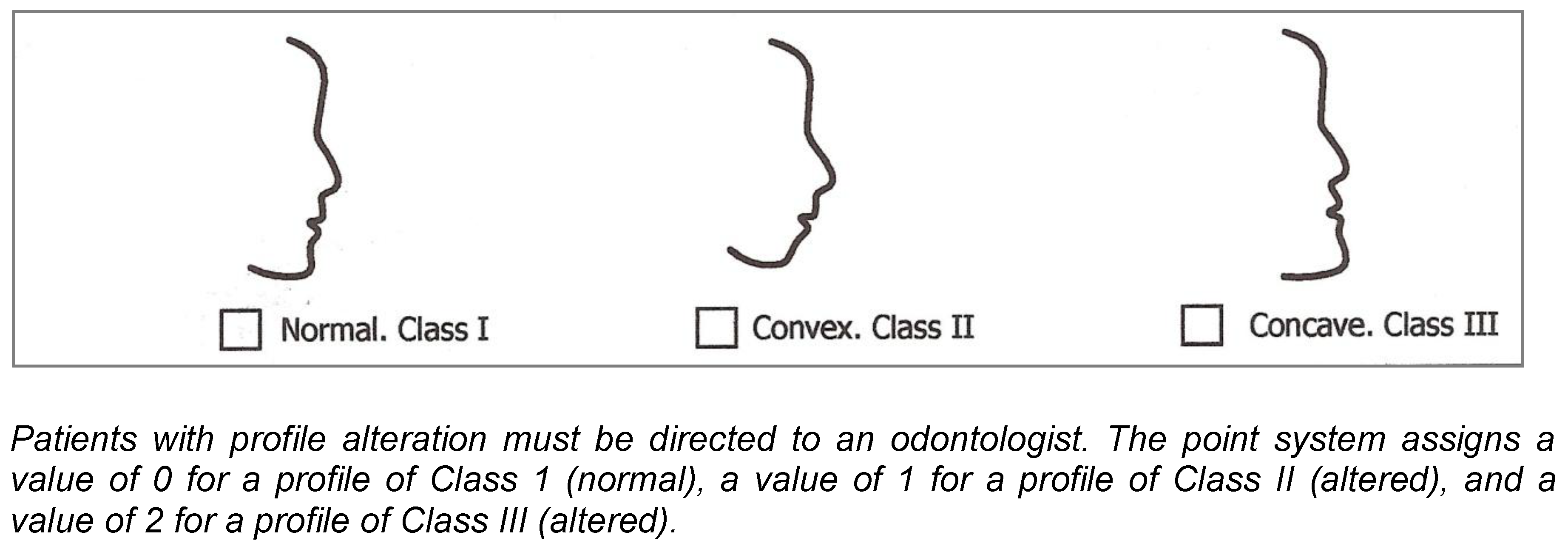
- 4.
- Nostril configuration (with forced breathing):
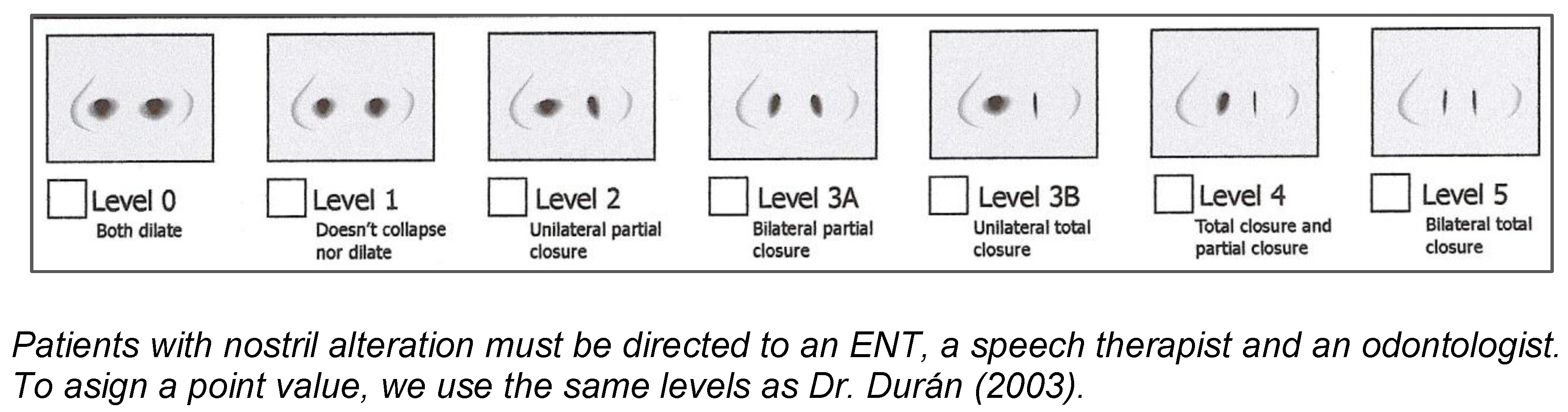
This section evaluates the configuration of the nostrils according to the degree of nasal collapse, as described by Dr. Durán (2003), in function with the activity of the nostrils during forced inhalation:
- Level 0: Bilateral dilation of the nostrils in inhalation
- Level 1: Neither dilation nor collapse of the nostrils in inhalation
- Level 2: Partial unilateral collapse in inhalation
- Level 3: Partial bilateral collapse (3-A) or total unilateral collapse (3-B) in inhalation
- Level 4: Total unilateral collapse of one side and partial collapse of other side in inhalation
- Level 5: Total bilateral collapse in inhalation
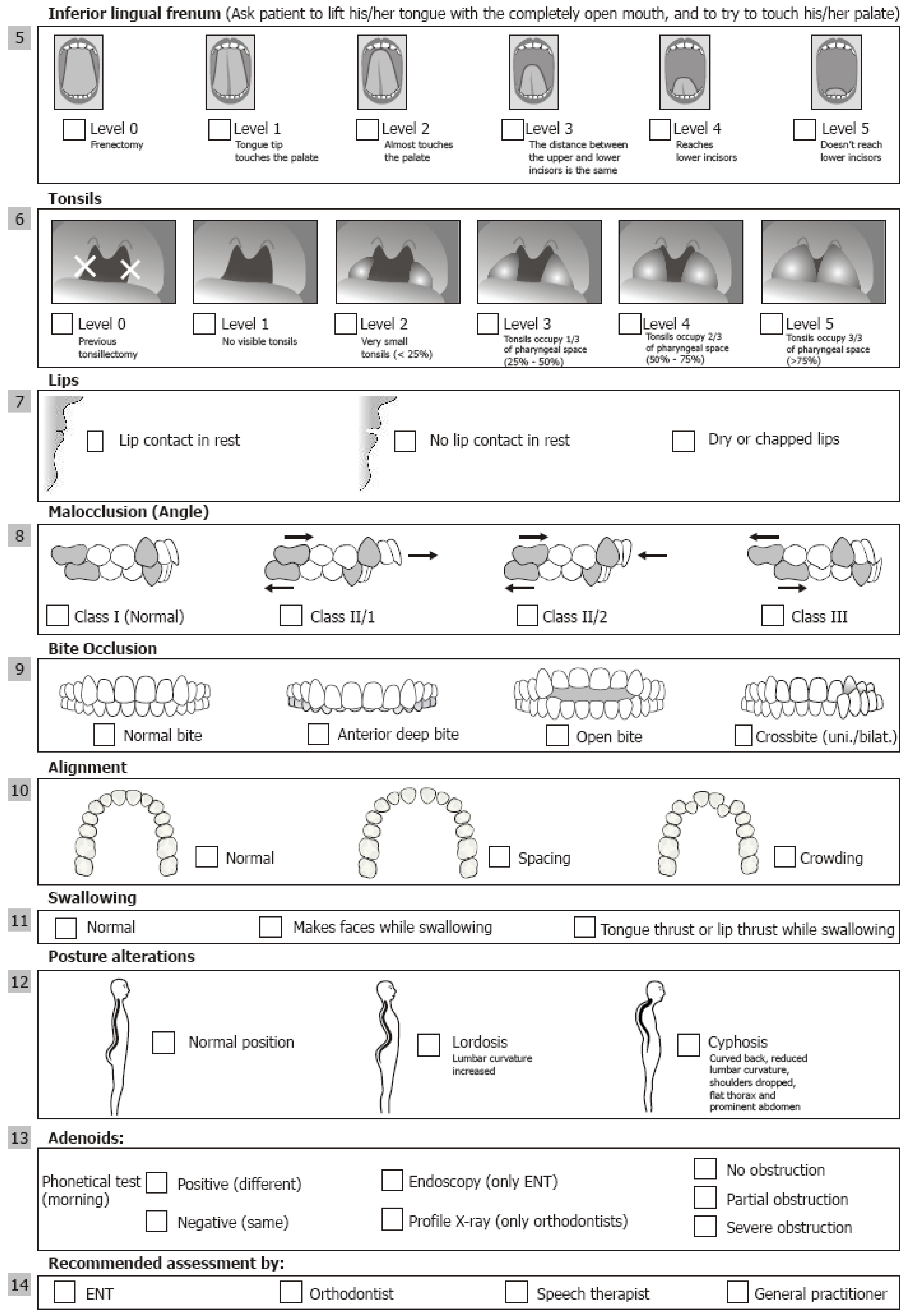
- 5.
- Inferior lingual frenum:
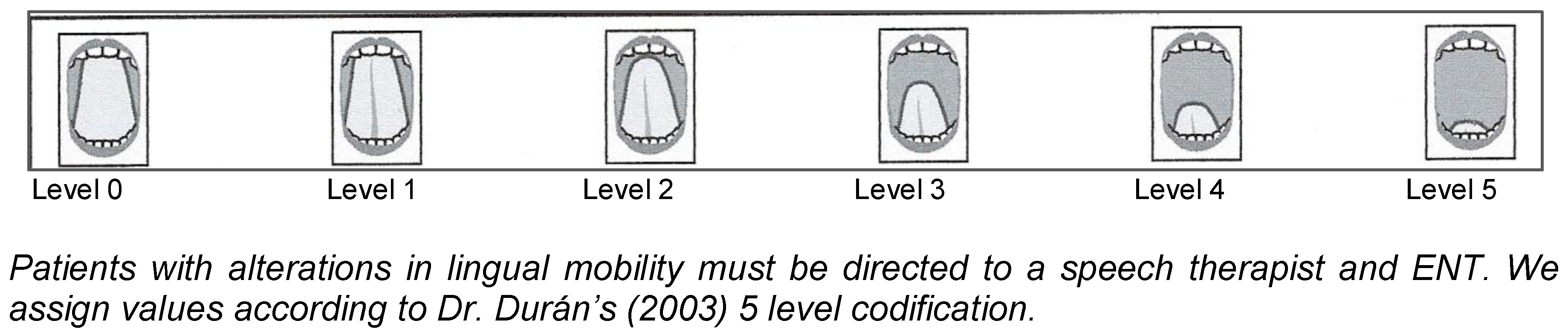
Dr. Durán’s (2003) codification system, is used which presents five degrees of lingual mobility and a value of zero for complete absence of a problem, as a function of the height to which the tip of the tongue reaches when the mouth is open:
- Level 0: Previous Frenectomy
- Level 1: Tip of the tongue touches the palate behind the upper incisors at maximum mandibular opening
- Level 2: Tip of the tongue almost touches the palate behind the upper incisors at maximum mandibular opening
- Level 3: Distance between the upper and lower incisors is the same at maximum mandibular opening
- Level 4: Tip of the tongue reaches lower incisors at maximum mandibular opening
- Level 5: Tip of the tongue doesn’t reach lower incisors (very close to ankyloglossia) at maximum mandibular opening
- 6.
- Tonsils:
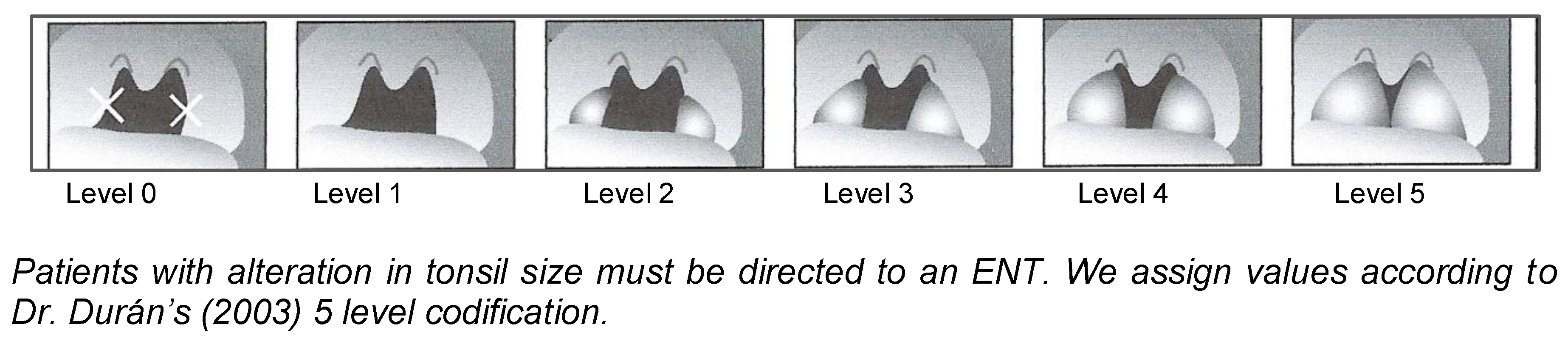
Tonsil size is encoded in a 5 level system, including a level of 0 for the total absence of a problem (tonsillectomy), in function with the relation to the pharyngeal space where:
- Level 0: Previous tonsillectomy
- Level 1: No visible tonsils
- Level 2: The tonsils are very small (<25% of the pharyngeal space)
- Level 3: Tonsils occupy 1/3 of pharyngeal space (25-50%)
- Level 4: Tonsils occupy 2/3 of pharyngeal space, although they do not quite touch along the medial line (50-75%)
- Level 5: Tonsils occupy 3/3 of pharyngeal space and touch one another (>75%)
- 7.
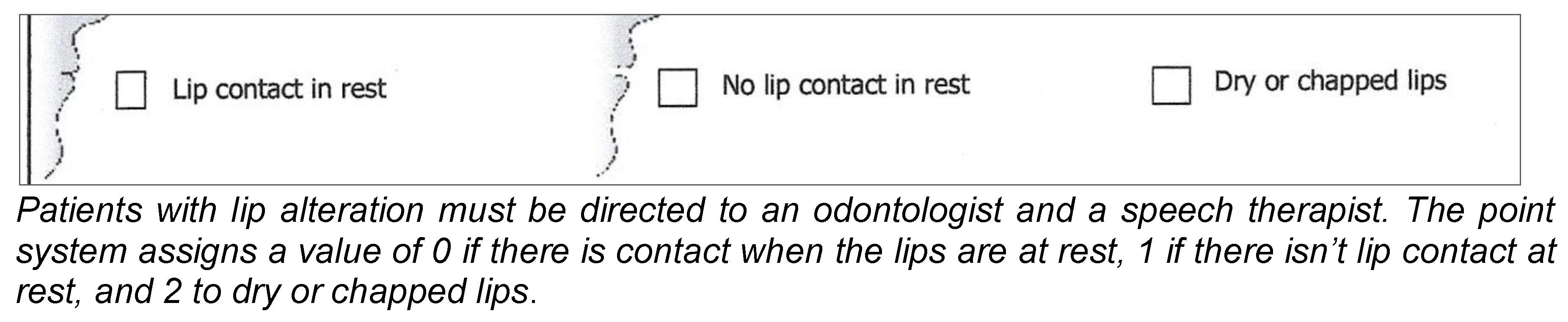
- Lips:
Lip relationship is examined. An upper/lower ratio of 1/3 to 2/3 is considered normal.
Also considered are:
- Incompetent upper lip at rest (no contact with the lower)
- Dry, chapped lips.
- 8.
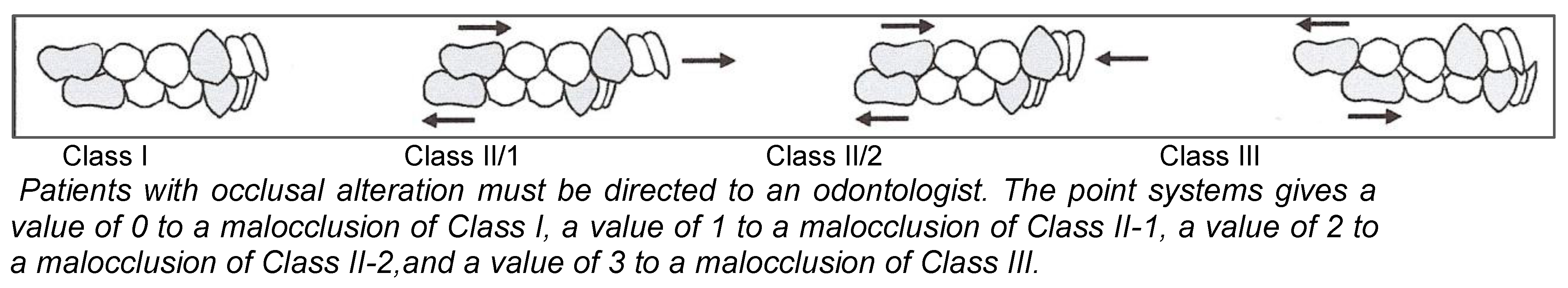
- Malocclusion (Angle, 1907):
Class I (normal): The mesiolabial cusp of the first upper molar occludes in mesiolabial sulcus (groove) of the first lower molar. The upper canine occludes between the distal side of the lower canine cusp and mesial side of the first lower molar cusp. The incisors present an overbite or 2-3 mm of anteroposterior difference (upper incisor is in advanced position in relation to the lower incisor).
Class II/1: The upper first molar, canine and incisors are in advanced position in relation to the lower ones.
Class II/2: The upper first molar and canine are in advanced position in relation to the lower ones. The upper central incisors are tipped towards the palate.
Class III: The upper first molar, canine and incisors are in a backward position in relation to the lower ones.
- 9.
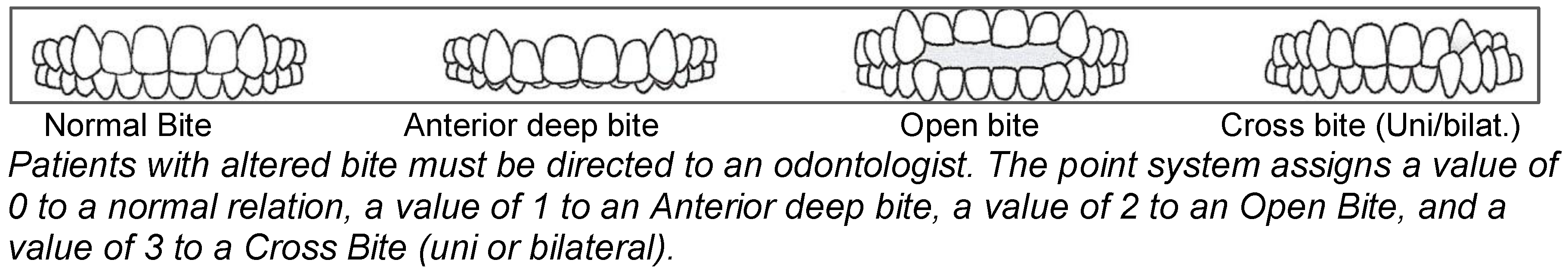
- Bite Occlusion:
Occlusal alterations are examined from a vertical and transverse point of view. On the vertical plane, identify if there is:
- -
- Anterior deep bite: upper incisors cover more than 2-3 mm of the lower
- -
- Open Bite: upper incisors cover less than 0 mm of the uppers
- -
- On the transverse plane, identify if there is Cross Bite (uni or bilateral):
- -
- the labial cusp of the premolars or the upper molars occludes inside the labial cusp of the lower molars
- 10.
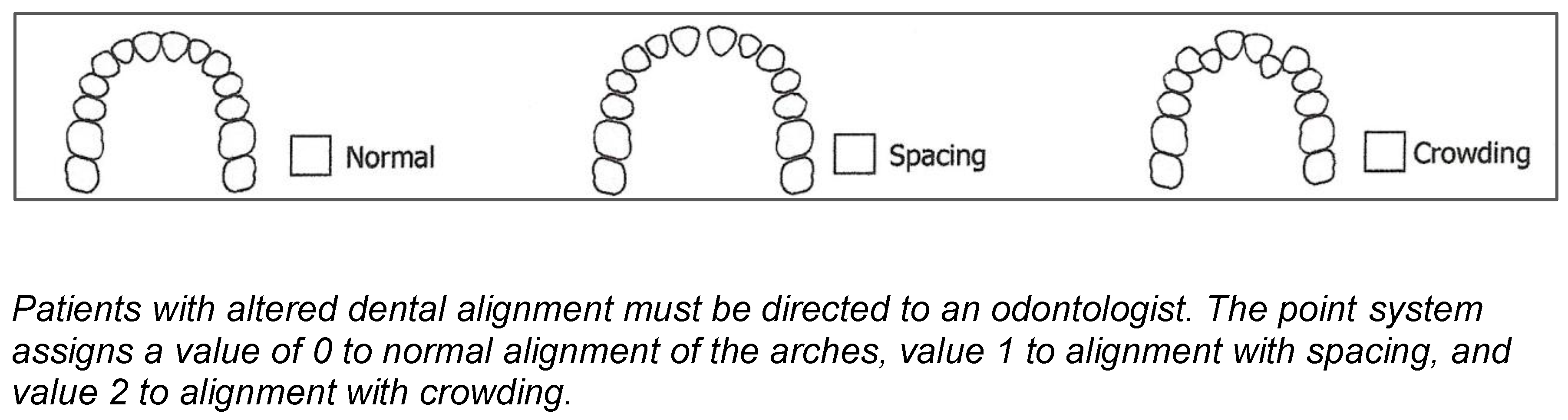
- Alignment:
Normal: Teeth are correctly positioned, aligned in their basal bone. There is neither excessive space nor over-crowding.
Spacing: There are spaces or diastema between the teeth
Crowding: The space available to the dental arches is insufficient and the teeth are crowded.
- 11.
- Swallowing:
Around 4 years of age, swallowing patterns reach maturity, exhibiting characteristics similar to those of an adult: lip seal, contact between tongue and palate, and lack of peribuccal tension or contraction. When these characteristics are not present, the result is so-called dysfunctional or atypical swallowing, the most common signs of which are:
- interposition of tongue between the dental arches
- tongue thrust against the upper or lower dental arch
- upper incisors above the lower lip
- contraction of peribuccal musculature, among others.
In accordance with the objective of this protocol, in order to conduct a quick and easy observation of swallowing, one must be aware of the following requirements: the patient sits or stands (the torso is in a vertical position) while the examiner looks for the natural pattern of swallowing (while speaking, drinking water, etc).
With this protocol, the presence of alterations in swallowing is examined using two easy observations which are:
- Does the patient make a face when swallowing?
- Is there interposition of the tongue or lip when swallowing?
Patients with altered swallowing must be directed to a speech therapist. The point system assigns a value of 0 for normal swallowing, a value of 1 when the patient makes faces while swallowing, and a value of 2 when we observe tongue thrust or lip thrust while swallowing.
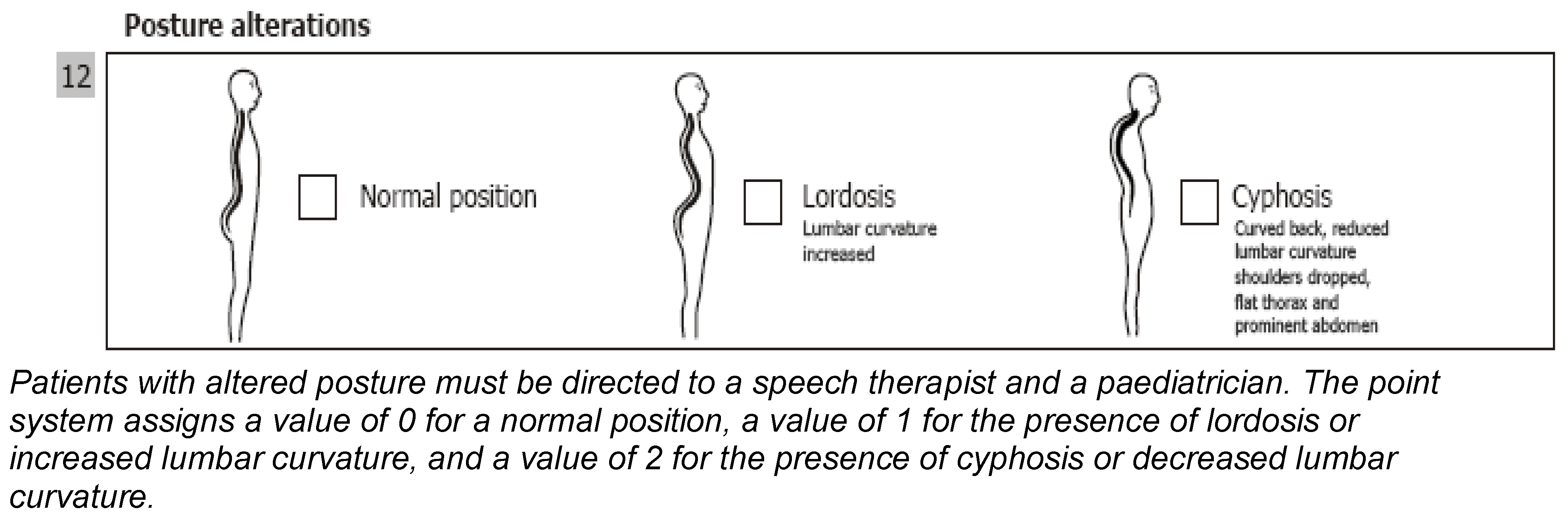
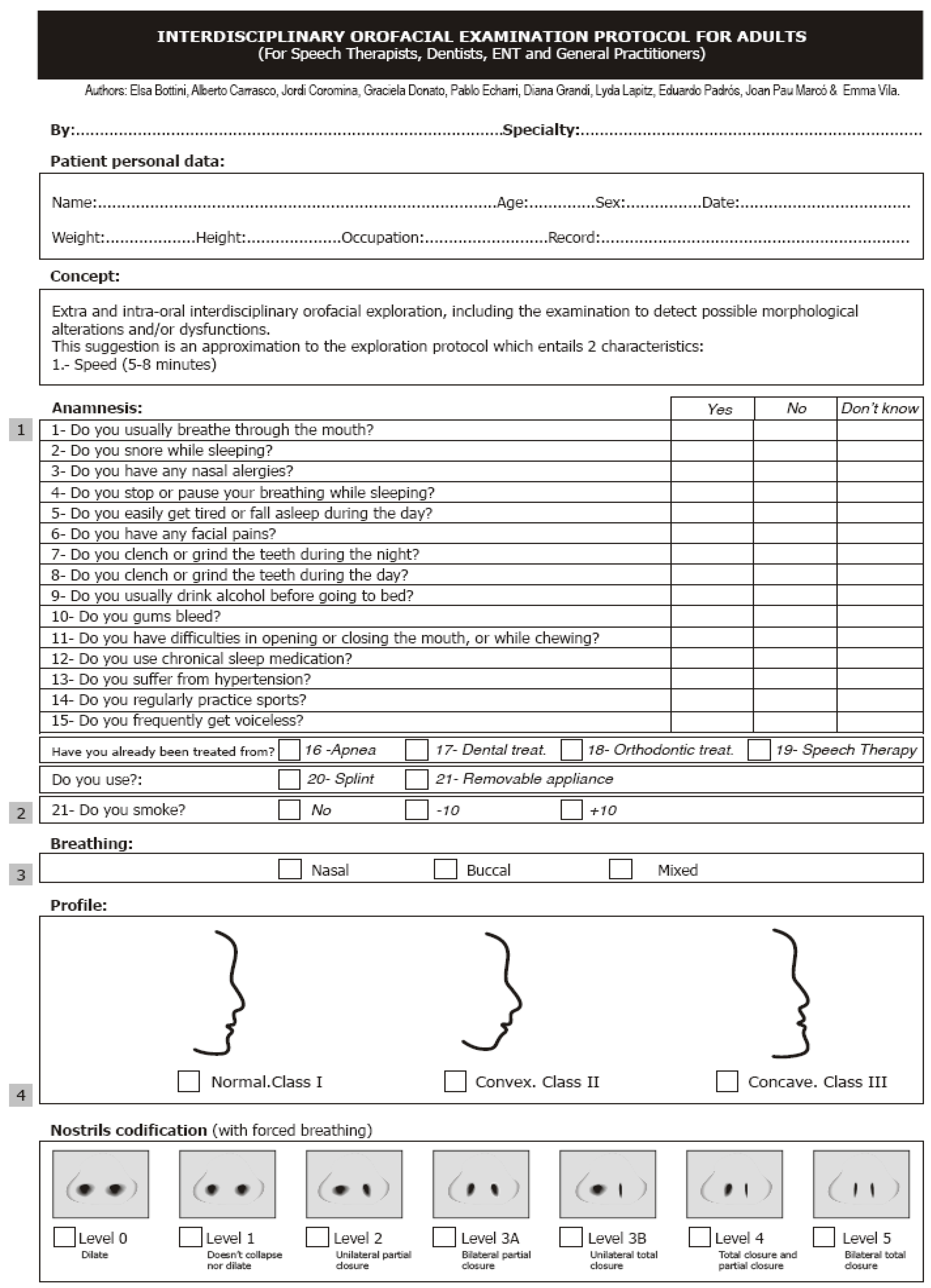
- 12.
- Posture alterations:
Altered posture refers to habits or incorrect habits in posture which result in the imbalance of body musculature. Changes produced in the craniofacial appearance (cervical hyper- or hypo-extension) lead to alterations in the appearance of the mandible.
In the protocol, the posture of the patient is indicated as:
- Normal position
- Lordosis: increased lumbar curvature
- Cyphosis: curved back, decreased lumbar curvature, shouldersdropped, flat thorax and prominent abdomen
- 13.
- Adenoids:
A phonetic test is given to collect information on the adenoids by asking the patient to repeat a word that contains nasal consonants, for example “morning.” This is initially done with the nostrils open and then with the nostrils close (pinched). When the timbre of voice is different the result is normal; when the timbre is the same, the result is altered. The ENTs do the endoscopy and the orthodontists can do the profile X-ray, to see if there is a partial obstruction, severe obstruction, or no obstruction.
Patients with alteration in adenoids must be directed to an ENT. The point system assigns a value of 0 to no obstruction, a value of 1 to partial obstruction, and a value of 2 to severe obstruction.
- 14.
- Recommended assessment by:
Finally, a section is included in which the professional or professionals to whom the patient must be referred for accurate diagnosis and appropriate treatments are identified: ENT, Orthodontist, Speech Therapist, Odontopediatrician.
A codification system has been developed for the type of professional who must assess the patient: A value of 1 is assigned to the need for assessment by an ENT, a value of 2 is assigned to the need for an assessment by an odontologist, a value of 3 is assigned to the need for an assessment by a speech therapist, a value of 4 is assigned to the need for an assessment by a paediatrician, and a value of 5 is assigned to the need for an assessment by a combination of any of the above.
We use the same codification (from 1 to 4) to classify which professional has conducted the study.
SUMMARY
The Interdisciplinary Orofacial Examination Protocol for Children and Adolescents has been designed and developed as an interdisciplinary resource for the efficient detection of orofacial alert signs. It is an easy, quick clinical procedure that allows us to conduct a patient’s initial evaluation.
The specific objectives of this protocol are: to determine which specialists from the multi-disciplinary team must intervene first in the patient’s diagnosis and treatment in order to facilitate the correction of anomalies and dysfunctions, to conduct an etiological treatment, and to obtain the most stable results.
This protocol also contributes to the unification of concepts and nomenclature used by distinct specialists in an effort to promote, facilitate and make dynamic their mutual understanding.
Appendix A
Appendix B
References
- Arnett, G. W.; Bergman, R. T. Facial Keys to orthodontic diagnosis and treatment planning-Part I. American Journal of Orthodontics and Dentofacial Orthopedics 1993, 103, 299–312. [Google Scholar] [PubMed]
- Arnett, G. W.; Bergman, R. T. Facial Keys to orthodontic diagnosis and treatment planning-Part II. American Journal of Orthodontics and Dentofacial Orthopedics 1993, 103, 395–411. [Google Scholar] [PubMed]
- Coromina, J.; Estivill, E. Coromina, J., Estivill, E., Eds.; Tratamiento del niño roncador y/o con apnea obstructiva del sueño: La reducción amigdalar con láser. In El niño roncador. El niño con síndrome de apnea obstructiva del sueño, 2nd ed.; EDIMSA: Barcelona, 2006; 41-68. [Google Scholar]
- Donato, G.; Lapitz, L.; Grandi, D. Protocolo de exploración Interdisciplinar orofacial para niños y adolescentes. Revista Logopèdia, (16). Col·legi de Logopedes de Catalunya. 2009. [Google Scholar]
- Durán, J. Multifunction System “MFS”. Las 8 claves de la matriz funcional. Revista Ortodoncia Clínica 2003, 6, 10–13. [Google Scholar]
- Durán, J. Técnica MFS: Diagnóstico de la matriz funcional: Codificación. Revista Ortodoncia Clínica 2003, 6, 138–140. [Google Scholar]
- Echarri, P.; Carrasco, A.; Vila, E.; Bottini, E. Protocolo de exploración Interdisciplinar orofacial para niños y adolescentes. Revista Ortodoncia Española 2009, 49(2), 107–115. [Google Scholar]
- Echarri, P.; Pérez, J. J. Echarri, P., Ed.; Historia clínica, examen clínico y estudio de modelos. In Diagnóstico en ortodoncia: Estudio multidisciplinario; Nexus: Barcelona, 2002; 57-102. [Google Scholar]
- Grandi, D.; Donato, G. Terapia miofuncional. Diagnóstico y tratamiento. Ediciones lebón; Barcelona, 2006. [Google Scholar]
- Segovia, M. L.; Infante, L. Disgnacias. In Programa de actualización en fonoaudiología; Primer ciclo. Módulos 1 y 2; Editorial Médica Panamericana: Bs.As. Argentina, 2001. [Google Scholar]
- Segre, R.; Naidich, S. Principios de foniatría; Editorial Médica Panamericana: Bs.As., Argentina, 1981. [Google Scholar]
- Ustrell, J.; Durán, J. Ustrell, J., Ed.; Diagnóstico en ortodoncia. In Durán journal. Ortodoncia, Primera edición; Editorial Universitat de Barcelona: Barcelona, 2001; 61-100. [Google Scholar]
© 2012 by the author. 2012 Diana Grandi.