Abstract
The purpose of this study was to establish a quantitative method to classify lingual frenulum as normal and altered. Methods: 98 people were included in this study. All measurements were made with maxium opening of the mouth. A digital caliper was used to measure the length of the frenulum under three conditions: a) with the tongue tip on the incisal papilla; b) with the tongue sucked up and maintained against the hard palate; and c) with tongue stretching over a spatula. Results: observations indicated that the most useful and statistically significant way of measuring frenulum length was achieved with maximum mouth opening and the tongue tip on the incisal papilla. Conclusion: this quantitative method was demonstrated to be effective for identifying and distinguishing normal and altered frenular length.
INTRODUCTION
Speech therapists find many patients with
various complaints leading to the hypothesis
that some alteration in the anatomy of the
lingual frenulum (or frenum) is the cause for
the problems, or at least, may aggravate
them. The most common symptoms that
may raise such hypotheses would be:
imprecision of speech; soft /r/ phoneme with
change for other phonemes or with
distortion; small opening of the mouth during
speech; imprecision or inefficacy of tongue
movements in isolated movements; the
tongue, when protruded, forming a heart in
its apex, with little protrusion capability, or
with protrusion bending its apex downward;
a tongue rest posture on the floor of the
mouth; difficulties of performing movements
with the tip of the tongue, such as licking ice
cream cone; history of difficulty to suckling
during breast-feeding; inefficient mastication
and deglutition with alteration for difficulty of
coupling the tongue in the hard palate.
The most frequent problem mentioned in the
literature related to an altered lingual
frenulum is speech production (Garcia-Pola
et all, 2002; Lee et all, 1989; Mukai et all,
1993; Velanovich, 1994; Wright, 1995;
Kotlow, 1999; Sanchez-Ruiz et all, 1999;
Messner et al, 2000 and 2002; Elias-
Podesta et all, 2001 & Lalakea et all, 2003).
Issues related to feeding, mainly during the breast-feeding phase, are the next most
frequently cited problem related to an
altered frenulum (Velanovich, 1994; Kotlow,
1999; Messner et all 2000; Elias-Podesta et
all, 2001; Berg, 1990; Marmet et all, 1990 &
Ballard et all 2002). These are followed by
problems with range of motion of the tongue
(Garcia-Pola et all, 2002; Wright, 1995;
Messner et al, 2000, 2002; Lalakea et all,
2003 & Defabianis, 2000); and deglutition
alterations (Wright, 1995; Kotlow, 1999 &
Sanches-Ruiz et all, 1999).
Various terms for and classifications of
lingual frenulum alterations are found in the
literature: tongue-tie, ankyloglossia,
hypertropic frenulum, thick frenulum,
muscular frenulum, fibrotic frenulum, and
frenulum with anterior insertion, short
frenulum and short frenulum with anterior
insertion (Kotlow, 1999; Singh & Kent, 2000;
Houaiss, 2001; Moore & Dalley, 2001 &
Marchesan, 2004). While many of
classifications address the form of the
frenulum, other characteristics are also
important. Singh and Kent (2000) describe
the lingual frenulum as a mucous membrane
fold that extends from the underside of the
tongue to the floor of the mouth. A large
median fold of mucous membrane cover
arises from the gingival on the lingual
surface of the tongue (Moore & Dalley, 2001). The foreshortened, small or absent
lingual frenulum characterizes
ankyloglossia. This can occur with full
fusion or partial fusion of the tongue with the
floor of the mouth.
Ankyloglossia is also characterized as the
tongue’s movement limited by a short or
absent lingual frenulum (Singh & Kent,
2000). Partial ankyloglossia, or tongue-tie,
is a congenital condition, the membrane
under the tongue is very short or its insertion
is very close to the tip of the tongue,
hindering the tongue’s protrusion (Berg,
1990). Ankyloglossia continues to be
defined as being a developmental anomaly,
characterized by short and thick lingual
frenulum resulting in limitations of tongue
movements (Garcia-Pola et all, 2002).
Some researchers have attempted to
differentiate and classify the frenulum. In
one study the lingual frenulum is
differentiated and classified according to:
short mucous membrane; mandibular insert
and hypertropic long mucous membrane
inserted into the crest of the alveolar edge
(Elias-Podesta et all, 2001). In another
study, the frenulum is classified as: short;
anterior insertion; and short with anterior
insertion (Marhesan, 2004). This
classification is similar to the
aforementioned definition, where the
tongue-tie or ankyloglossia is defined as a
short membrane, or inserted very close of
the tip of the tongue (Berg, 1990). These
classifications depend on the qualitative
criteria used, which is often fundamentally
based on the evaluator’s experience.
Few studies have been designed to quantify
the frenulum through direct measurements.
This may be due to the difficulty and
imprecision in measuring the soft tissues
involved. Only three studies have been
identified that used quantitative criteria to
measure and classify the lingual frenulum.
In the first study (Lee, Kim, & Lim, 1989) the
lingual frenulum was measured with a ruler
created for this purpose. The length of the
lingual frenulum was classified in the
following manner: average length of
frenulum with less than 10 mm - a mild
ankyloglossia; between 10 and 15 mm -
moderate; more than 15 mm (type-1) severe
ankyloglossia; and, a frenulum clinically considered as representing severe
ankyloglossia eventhough frenulum length
was less than 15-mm length (2 subjects
were classified as type-2 severe
ankyloglossia). The authors of this study
noted that the longer the frenulum, the more
anterior it would be inserted and the less the
mobility and autonomy of the tongue (Lee
et.al., 1989).
In the second study (Kotlow, 1990), the
individual was requested to protrude the
tongue out of the mouth as far as possible
while the length of the tongue was
measured using a ruler. The frenulum was
designated as clinically acceptable when
longer than 16 mm; Class I as medium
ankyloglossia of 12 to 16mm; Class II as
moderate ankyloglossia of 8 to 11 mm;
Class III as severe ankyloglossia of 3 to 7
mm; and Class IV or as full ankyloglossia if
smaller than 3 mm (Kotlow, 1990). In the
last study the authors used the Hazelbaker
(1993) scale for assessing the frenulum.
Criteria were developed with this scale to
observe the appearance and movements of
the tongue, as well as the elasticity and
insertion point of the frenulum. The length
of tongue’s frenulum was measured with the
tongue in an elevated position, with the
following measurements recorded: big,
small or equal to 1 cm (Ballard et all, 2002).
For this study, a normal frenulum insertion
was considered as approximately 1-cm from
the apex.
A review of the literature indicates that
disagreement persists among some health
professionals regarding how to classify the
frenulum as normal or altered. Differences
in clinical judgment also exist regarding the
indications for/against surgery. Due to the
variety of professional opinions regarding
surgical treatment of an altered lingual
frenulum, patients are often insecure or
confused about their options regarding
intervention. While a lingual frenulum may
be characterized as normal or altered
depending on the evaluation criteria used by
the evaluator, those classified as altered
may or may not be indicated for surgery. If
a uniform method of classification and
evaluation quantification and qualification
were developed, it should result in higher
examiner reliability and accuracy in
distinguishing between a normal and altered frenulum and more consistency in
recommendations for surgery. Accordingly
the purpose of this study was to develop a
method of differentiating between a normal
frenulum and an altered frenulum using
qualitative evaluation and numeric
quantification. This study aims, therefore, to
determine and report a quantitative method
to classify a lingual frenulum as either
normal or altered.
METHODS
98 subjects were enrolled in this research.
They were accompanied by a parent or
relative. They were patients of the Clinic -
School CEFAC’s. Authorization for the
subjects’ participation in the study was
obtained after they had been informed in
writing about the procedures and the
purpose of the research. The subjects
included in this study were 18 years of age
or older, were not receiving speech therapy,
did not have any temporomandibular joint
problems, had not previously had a lingual
frenectomy, had their central upper and
lower incisors, and did not have anterior
open bite.
Two speech therapists evaluated the
frenulum and characterized it as normal or
altered using the qualitative protocol
proposed by Marchesan (2004) according to
the following criteria: a) short or smaller than
most frenulum, although inserted correctly
(Moore & Dalley, 2001) at the halfway back
area on the undersurface of the tongue and
extending to the floor of the mouth (Singh &
Kent, 2000) (Figure 1); b) with anterior
insertion, demonstrating normal size while
being inserted at any point forward from the
halfway area along the underside of the
tongue; it may be inserted close to the apex
(Figure 2); c) short with anterior insertion,
this being a mix of the previous two (Figure
3).
In addition to a qualitative evaluation, each
subject was requested to perform various
movements of the tongue to assess lingual
range of movement. The requested
movements were: protrude the tongue
outside the mouth; tongue moved laterally to
each labial commissure; and upward and
downward vertical movements of the tongue. Any difficulty with the requested movements resulted in the frenulum being
classified as altered.
Following the classification of the frenulum
as normal or altered, four measurements
were obtained using the digital Starret slide
caliper. All measurements were taken by a
single speech therapist. The recorded
measurements included: a) maximum
mouth opening (with no tongue interference)
as measured at the incisal edges of the left
upper and lower central incisors. This
measurement served as a reference support
point for the slide caliper (Figure 4), and was
taken as an absolute value reference for
subsequent comparison with other
measurements; b) for the second
measurement each subject was requested
to put the apex of his/her tongue on the
palatine (incisal) papilla, maintaining this
posture with the mouth open maximally and
with the support points for the slide caliper
maintained at the left central incisors (Figure
5); c) the third measurement was obtained
while the subject created a negative
pressure by sucking the tongue against the
hard palate area, maintaining this position
with the mouth open (Figure 6); d) the last
measurement was taken while each subject
protruded the tongue and stretched it
maximally over a wooden spatula held by
the examiner at the lower incisors (Figure 7).
A mark made with a black pencil was
recorded on the spatula at the place of the
longest measurement of the tongue. Using
the slide caliper, this measurement, from the
tip of the spatula to the place where the
tongue had reached in extension was
measured (Figure 8). All measurements
were logged onto a previously designed
table consisting of the following data: initials
of subject’s name and age, collection date,
classification of frenulum as normal or
altered, the measurements taken at full
mouth opening, tongue on the papilla,
tongue sucked against the hard palate, and
tongue on the spatula. The rule of three
was applied, comparing the wide-open
mouth reference valus with each of the other
three measurements. The data were
collected between the months - August 2002
to December 2003.
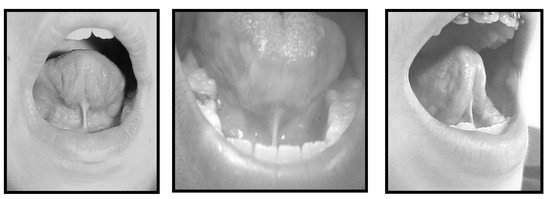
Figure 1.
Short Frenulum.
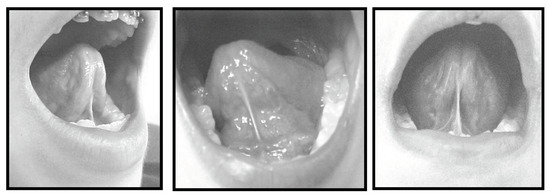
Figure 2.
Frenulum with Anterior Insertion.
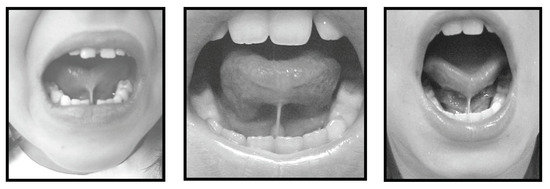
Figure 3.
Frenulum with Anterior Insertion and Short.
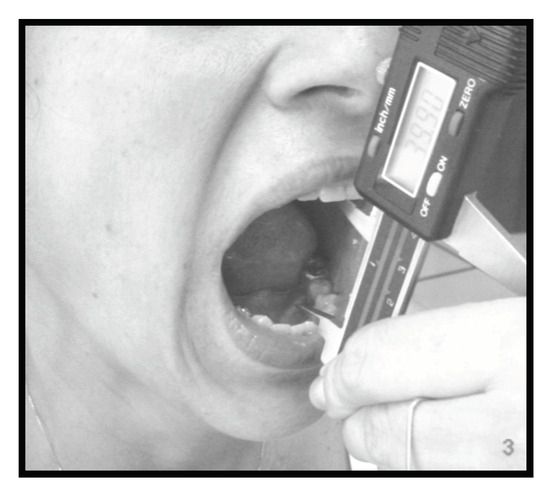
Figure 4.
Full Mouth Opening.

Figure 5.
Tongue on the Papilla.
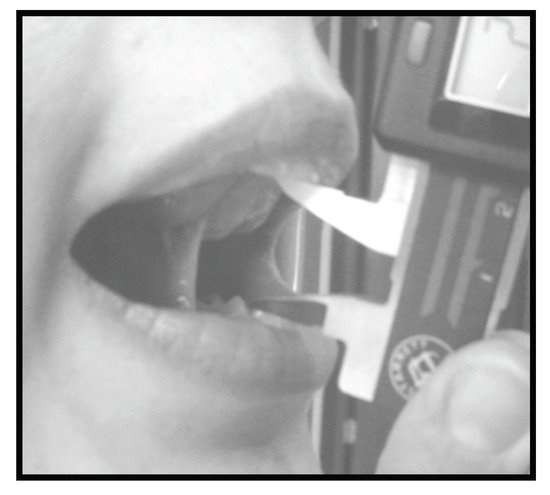
Figure 6.
Tongue Suctioned on the Hard Palate.
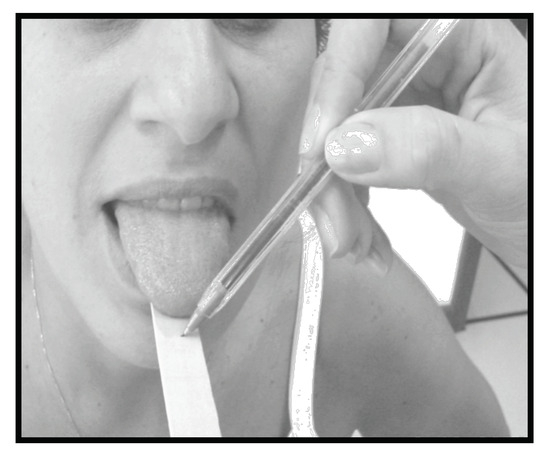
Figure 7.
Tongue on the Spatula.
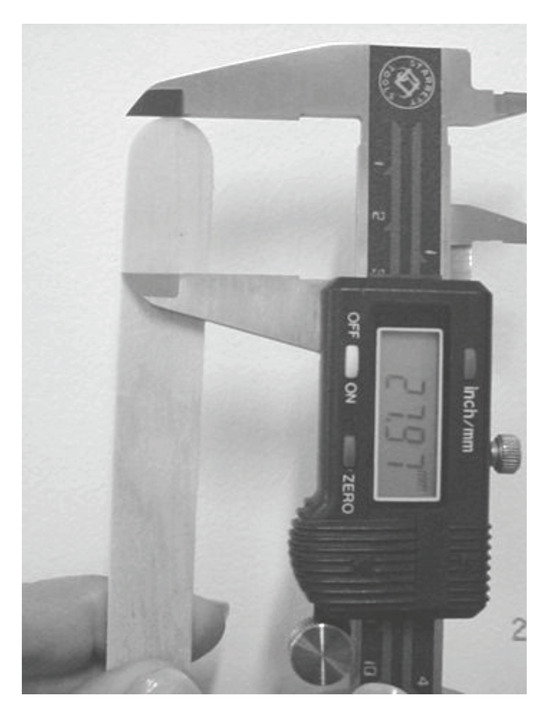
Figure 8.
Measuring the Spatula.
The Mann-Whitney U test was adopted as the
statistical instrument to evaluate differences among the normal and altered
groups. 5% (0.050)
significance level was adopted for statistical tests. This research was
approved by the Committee of Ethics in Research under Nº. 100/03. It was
considered without risk, but informed written consent was necessary.
RESULTS
Table 1 displays the comparison data for the 98 subjects. For the open mouth task there was no significant difference
among the medians of the frenulum (p>0.05). For the normal frenulum, the median of the tongue on the papilla (33.2),
the median of the tongue sucked against the hard palate (27.1), and tongue on the spatula (29.9) was larger than for the altered group, 27.7; 25.1 and 26.2 respectively. These findings were statistically significant (p < 0.05).

Table 1.
Distribution of 98 cases above 18 years old in relation with the normal frenulum versus altered frenulum.
Table 2 displays the distribution of differences among the tongue measurements on the incisal papilla and wide-open mouth with relation to the normal versus altered frenulum in the 98 adults subjects. The differences in the measurements were significantally larger among the altered frenulum group. The median of the difference between wide-open mouth and mouth open with the tongue on the papilla was 12.2 for normal frenulum and 21 for altered frenulum. Also, the median of the difference between wide-open mouth and tongue on the papilla was 13.4 (6.1) and for altered frenulum 19.4 (7.7).

Table 2.
- Distribution of the differences among the tongue measurements on the papilla and open mouth with relation to the normal frenulum versus altered frenulum of all the 98 adults older than 18 years.
DISCUSSION
After the measurement phase of the study was completed, from the examiner’s point of view, the more-easily obtained measurement was with the tongue on the incisal papilla. It was possible to obtain this measurement with any type of frenulum alteration. The measurement obtained with the tongue sucked onto the hard palate by negative pressure is difficult to obtain, since few subjects were able to maintain this posture while the measurement was taken. The posture of the tongue required for this measurement was particularly difficult to maintain in subjects with a short frenulum, especially for subjects with short frenulum who also had an anterior attachment.
The measurement of the tongue on the spatula in subjects whose frenulum had severe anterior insertion was much lower when compared with the wide-open mouth. However, in the subjects with a short frenulum that attached posteriorly on the undersurface of the tongue, which allowed freedom in the anterior portion of the tongue, little measurement differences were found when compared with the wide-open mouth measurement. For subjects with a short frenulum or with slight anterior insertion, no significant differences were identified, while in normal subjects there were relevant differences. While measurements for tongue protrusion are easily collected, this measurement condition is not considered to be critical in the comparison and differentiation between a normal and altered frenulum. In contrast, it seems important to point out that the significant difference between the measurement of the tongue on the incisal papilla and the measurement for the open mouth has the most potential for differentiating between a normal and altered frenulum, with a 33.2 median for a normal frenulum and of 27.7. for an altered frenulum.
The findings submitted in Table 1 indicate that there is no statistical difference (p = 0.6071) among subjects with either a normal frenulum (46.0) for the open mouth measurements or an altered frenulum (47.2 median). Accordingly, this measurement can be considered as absolute value and can serve as a reference for other measures of the frenulum.
The quantitative classifications found in the three unique studies mentioned in the literature (Lee et al, 1989; Kotlow, 1999 &
Ballard et al, 2002)) used frenulum measuring forms that differ from those used in this study. For this reason, it is not possible to compare the data with these studies.
To facilitate the physician’s analysis of the frenulum, the percentages of all sampled subjects were calculated by dividing the measurement of the tongue on the incisal papilla by the measurement obtained with the wide-open mouth. It was determined that for the subjects whose frenulum had been classified as normal, a percentage above approximately 60% was found, while, for subjects whose frenulum had been classified as altered, a percentage around 50% or less was obtained.
There is obviously no measurement (percentile) that can be strictly adopted that clearly designates a frenulum as normal or altered, because some normal subjects, although few, also showed a value below 50%, while some subjects with altered frenulum showed values above 50%. This variation may have occurred due to a lack of differentiation of the data for the group with an altered frenulum when compared with the data for the group with normal frenulum.
All subjects with an altered frenulum were grouped together for statistical purposes, and treated as a single group. It was noted that for the subjects with altered frenulum with anterior insertion, the percentage with mouth fully open, compared with mouth open with tongue on the papilla was above 50%. Even though this occurred with few subjects it should be considered. A trend was identified that subjects with an altered frenulum had low percentile values, while normal subjects, tended to have higher percentile values when comparing relationships between the wide-open mouth measurements with those of the tongue on the incisal papilla.
Based on the results of this study, it can be infered that the smaller the relationship between the measurement of the tongue on the incisal papilla and the measurement of mouth opening, the larger the chance that the frenulum is altered. There is no value in making a recommendation for surgery based only on a calculated figure. An appropriate suggestion based on the data in this study is that quantitative data should be analyzed together with the qualitative data in evaluating the normal or altered state of a lingual frenulum. For this purpose, use one of the frenulum classifications proposed in the literature (Garcia-Pola et all, 2002; Elias-
Podesta et all, 2001;; Berg, 1990; Singh & Kent, 2000; Marchesan, 2004 & Halzebaker,
1993).
Additional research should be conducted to increase the precision criteria for measuring the lingual frenulum. As a limiting factor, it should be noted that such measurements are of soft tissue structures which can possess a great degree of variation. Depending on the place of contact for tongue support with maximal opening of the mouth, and while attempting to sustain a specific posture of the tongue during the measurement, subject performances may show differing numerical values in repeated measures.
The data obtained with the classification of a frenulum, when using qualitative or quantitative classifications, or both, should always be analyzed together with the clinical history and with the data found in the clinical examination.
It is hoped that this study may aid other health professionals in evaluating weather a lingual frenulum is normal or altered. Additional research is needed to fully identify all the pertinent factors and variations that may be found when assessing a lingual frenum.
CONCLUSION
The comparison of the values obtained with the measurement of the mouth maximally open with the values found when the mouth is open with the tongue tip touching the incisal papilla, seems to be a viable clinical tool for determining whether a lingual frenulum is normal or altered.
References
- Ballard, J. L., C. E. Auer, and J. C. Khoury. 2002. Ankyloglossia: Assessment, incidence, and effect of frenuloplasty on the breastfeeding dyad. Pediatrics 110: 63. [Google Scholar] [CrossRef] [PubMed]
- Berg, K. L. 1990. Tongue-tie (ankyloglossia) and breastfeeding: A review. Journal Human Lactent 6: 109–112. [Google Scholar] [CrossRef] [PubMed]
- Defabianis, P. 2000. Ankyloglossia and its influence on maxillary and mandibular development. (A seven-year follow-up case report). Function. Orthodontic 17: 25–33. [Google Scholar]
- Elias-Podesta, M. C., M Seclén-Nunez del Arco, P. G. Tello-Meléndez, and B. A. Cháves-González. 2001. Diagnóstico clínico de anquiloglosia, posibles complicaciones y propuesta de solución quirúrgica. Revista Odontologica 3: 13–17. [Google Scholar]
- Garcia-Pola, M. J., J. M. Garcia-Martin, and M. Gonzalez-Garcia. 2002. Prevalence of oral lesions in the 6 years-old pediatric population of Oviedo (Spain). Medicina Oral 7: 184–191. [Google Scholar] [PubMed]
- Halzelbaker, A. K. 1993. The assessment tool for lingual frenulum function (ATLFF): Use in a lactation consultant private practice . Ph. D. Thesis, Pasadena, CA. Pacific Oaks College. [Google Scholar]
- Houaiss, A. 2001. Dicionário da língua portuguesa. Objetiva. [Google Scholar]
- Kotlow, L. A. 1999. Ankyloglossia (tongue-tie): A diagnostic and treatment quandary. Quintessence International 30: 259–262. [Google Scholar] [PubMed]
- Lalakea, M. L., and A. H. Messner. 2003. Ankyloglossia: The adolescent and adult perspective. Otolaryngology Head and Neck Surgery 128: 746–752. [Google Scholar] [CrossRef] [PubMed]
- Lee, S. K., Y. S. Kim, and C. Y. Lim. 1989. A pathological consideration of ankyloglossia and lingual myoplasty. Taehan Chikkwa Uisa hyophoe Chi 27: 287–308. [Google Scholar] [PubMed]
- Marchesan, I. Q. 2004. Lingual frenulum: Classification and speech interference. International Journal of Orofacial Myology 30: 31–38. [Google Scholar] [CrossRef]
- Marmet, C., E. Shell, and R. Marmet. 1990. Neonatal frenotomy may be necessary to correct breastfeeding problems. Journal Human Lactent 6: 117–121. [Google Scholar] [CrossRef] [PubMed]
- Messner, A. H., M. L. Lalakea, J. Aby, J. MacMahon, and E. Bair. 2000. Ankyloglossia incidence and associated feeding difficulties. Archives Otolaryngology Head Neck Surgery 126: 36–39. [Google Scholar] [CrossRef] [PubMed]
- Messner, A. H., and M. L. Lalakea. 2002. The effect of ankyloglossia on speech in children. Otolaryngology Head and Neck Surgery 127: 539–545. [Google Scholar] [CrossRef] [PubMed]
- Moore, K. L., and A. F. Dalley. 2001. Anatomia orientada para a clínica, 4th ed. Guanabara Koogan. [Google Scholar]
- Mukai, S., C. Mukai, and K. Asaoka. 1993. Congenital ankyloglossia with deviation of the epiglottis and larynx: Symptoms and respiratory function in adults. Annals Otology Rhinology Laryngology 102: 620–624. [Google Scholar] [CrossRef] [PubMed]
- Sanches-Ruiz, I., G. Gonzalez-Landa, V. Perez-González, L. Sanchez-Fernández, C. Prado-Fernández, and I. Azcona-Zorrilla. 1999. Section of the sublingual frenulum: Are the indications correct? Cirurgia Pediatrica 12: 161–164. [Google Scholar]
- Singh, S., and R. D. Kent. 2000. Dictionary of speech-language pathology. Singular. [Google Scholar]
- Velanovich, V. 1994. The transverse-vertical frenuloplasty for ankyloglossia. Mil. Medicine 159: 714–715. [Google Scholar] [CrossRef]
- Wright, J. E. 1995. Tongue-tie. Journal Pediatric Child Health 31: 276–278. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2008 by the authors. 2008 Irene Queiroz Marchesan