PERSISTENT ARTICULATORY IMPAIRMENTS
In the literature, the term "persistent sound system disorder" has been used to describe the speech problems that do not readily respond to treatment (
Powell, 1996).
Shelton (
1993) referred to "persistent sound system disorder" as an umbrella term to describe relatively a small group of children who are resistant to treatment. There exists an evidence of heterogeneity in persistent sound system disorders. In this study, "persistent articulatory impairments" refer to a category of articulatory disorders that may be due to various anatomical and physiological causes including psychological and behavioral factors. These disorders are highly resistant to treatment due to various reasons, for example decreased motivation, abnormal orofacial structures, inadequate oromotor skills, inadequate environment for learning, insufficient maintenance and carry-over, etc.(
Shelton, 1993).
Many orofacial myofunctional disorders (e.g., moderate to severe malocclusions, prolonged upper respiratory tract infections, tongue thrust etc.) that are detrimental to overall orofacial dynamicity, including speech are found in cases with persistent articulatory impairments.
OROFACIAL MYOFUNCTIONAL DISORDERS (OMD)
The face is a conglomeration of morphological features related to both communication and socialization. An OMD involves oral or orofacial musculature that interferes with normal growth, development, or function of structures (ASHA, 1993). OMDs usually originate from morphological deficiencies in lingual, labial, dental, skeletal, soft tissue, abnormal oral habits, mouth breathing, abnormal lip resting postures, and speech differences (Kellum 1994).
According to Pahkala, Laine, & Narhi (1995), certain aspects of dental malocclusion such as large overjet, anterior open bite, lateral cross bite, palpatory tenderness of temporomandibular joint, jaw deviation on opening, and bruxism are related to misarticulation of speech sounds. Despite maturation of the oromotor skills with age, various orofacial dysfunctions indicate fixation of certain speech misarticualtions.
Pierce (
1996) reported that 51 % of 100 clients diagnosed with tongue thrust evidenced articulation errors at the time of initial evaluation.
Garretto (
2001) reported OMD in 129 children of both genders, ranging in age from five to nine years. On evaluation, children demonstrated dysfunctional swallowing, upper tongue thrust, lower tongue thrust, lower lip interposition, anterior, posterior, and complete tongue interposition, short upper lip, low resting tongue posture, mouth breathing, and sucking habits.
Malocclusion traits and related articulation disorders were studied by
Laine (
1992). Consonants are produced much more anteriorly in case of various open and cross-bite conditions. Incisal open bite associated with mesial occlusion is related to severe misarticulation problems.
Keatley and Coulson (
1989) documented three categories of articulation disorders in 100 subjects ranging in age from four years to 48 years, diagnosed with various OMDs. Sibilants /s/, /z/, and /sh/ were affected in 48% of the subjects. Dentalization of lingua-alveolar sounds was found in 28% of the subjects. Nine percent of the subjects showed problems with affricates and glides.
Vallino & Tompson (
1993) studied class II and class II malocclusions with and without open bites. Overall, most of the subjects evidenced increased errors involving fricatives and affricates. Less frequent errors were noticed with stops (/p, b, t, d, n/).
To treat OMD, a specialized multidisciplinary remedial program is used to correct oral facial structures and functions, which is known as orofacial myofunctional therapy (OMT). A significant corpus of research demonstrates that OMT is effective in restoring the structural and functional integrity of orofacial systems related to swallowing and speech. OMT has also been proven to be effective in many clinical domains when used with other interdisciplinary treatments.
OROMYOFUNCTIONAL THERAPY (OMT)
OMT has been reported to be successful in improving morphology and function of the muscles in mouth-breathing patients without nasal airway obstruction (Schievano, Rontani, & Berzin, 1999), skeletal Class III open bite (
Kondo & Aoba, 2000), breathing, feeding, and orofacial habits (
Bacha & Rispoli, 1999), and in enhancement of oral postures, orofacial muscle balance, swallowing, and speech (
Benkert, 1997; Bigenzhan, Fischman, & Mayrhofer-Krammel, 1992;
Hahn & Hahn, 1992). OMT has also been found to be effective in preventing malocclusion and orthodontic relapse (
Hanson & Andrianopoulos, 1982;
Andrianopoulos & Hanson, 1987).
OMT has been useful in eradicating misarticulation and tongue thrust in a number of studies (e.g.,
Gommerman & Hodge, 1995;
Pierce, 1996;
Umberger & Johnston, 1997).
Pierce (
1996) treated 100 clients using OMT and found that all but four had corrected their frontal lisps and liquid distortions.
Santoni (
2001) studied the effect of button-pull exercise to determine changes in lip posture and power. 91 patients were tested before and after the myofunctional treatment. The author found significant increase in lip strength in the experimental group. Patients who were able to develop appropriate lip rest postures demonstrated increased lip seals. It is important to identify through research what type of intervening variable may affect the outcome of OMT. Variables that may be considered include nasal allergies, enlarged tonsils, body posture, and face type. The author concludes that it is difficult to measure success in lip strength due to button pull exercise alone, because of existing extraneous factors. Extraneous factors in OMT are better controlled by the use of team members involved in assessment and treatment of various OMD.
The interdisciplinary team includes otorhinolaryngologist, orofacial myologist, speech-language pathologist, orthodontist, maxillofacial surgeon, pediatrician, physician, neurologist, etc. Interdisciplinary team work is needed to identify morphological anomalies in the orofacial region in order to reach a precise diagnosis and efficient treatment. Combined approaches (orthodontic and OMT) have been found to be effective in a number of studies (e.g., Daglio, Schwitzer, Wuthrich, & Kalivroussis, 1993; Grunert, Krenkel, Furtenbach, & Barner, 1989;
Yamaguchi & Sebata, 1995). Combined treatment approaches have been helpful in correction of lip and tongue resting postures, swallowing patterns, speech patterns, prevention of relapses, and in various functional gains.
Little research has examined the nature of persistent sound system disorders or articulatory impairments in adults who need treatment in order to improve oral and speech skills after many years of termination of speech therapy during the school years. In the OMT arena to date, there is virtually no systematic study to understand the role of OMT in facilitating speech sound production and speech intelligibility. However a number of studies recommended initiating oromotor postures and movement patterns early in the treatment plan (e.g., Hall, Jordan, & Robin, 1993). The purpose of this study is to understand the impact of OMT in adults with persistent articulatory impairments and various co-existing OMD that were treated in the past.
SUBJECTS
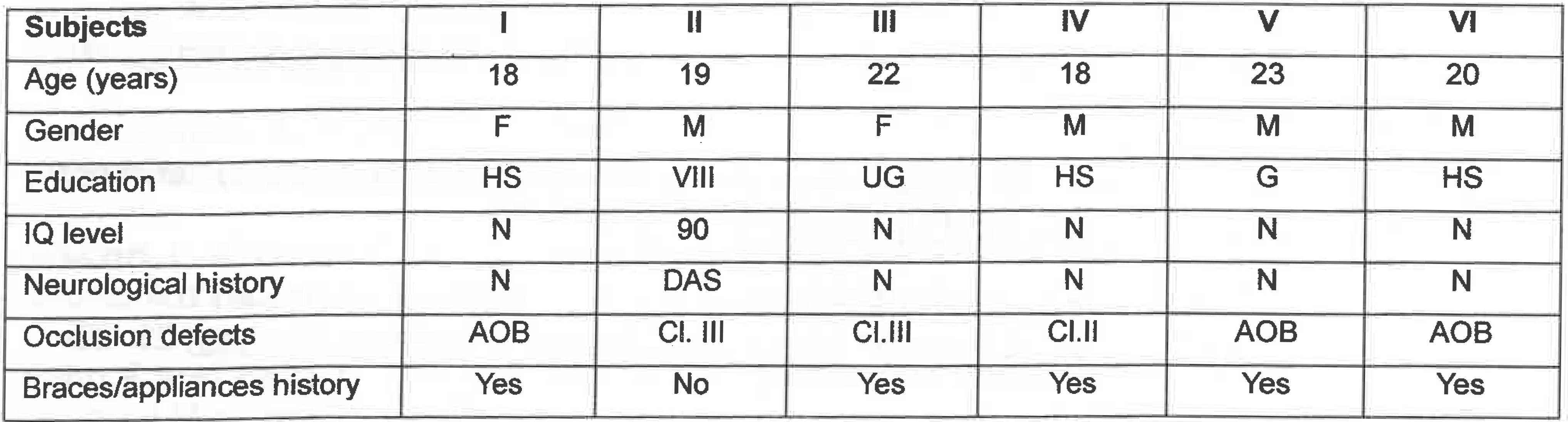
Six subjects in the age range of 18-23 years participated in the study (see
Appendix A &
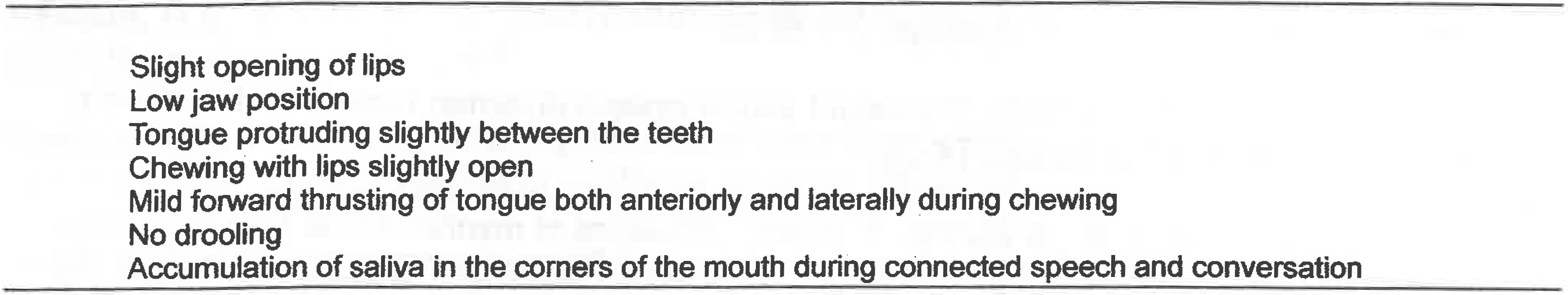
Appendix B). Three subjects had anterior open bites due to relapse of orthodontic treatment and were unable to maintain proper occlusion secondary to functional mouth-breathing. Anterior open bite is a myofunctional disorder is characterized by protrusion of tongue into the space between the upper and lower teeth during swallowing. Because of anterior bites the subjects demonstrated frontal and lateral lisps, open bites, and mild tongue thrust swallowing. Anterior open bite is quite difficult to treat in an adult.
One of the subjects had Class III malocclusion. One of them had Class II malocclusion. Occlusion is defined as the coordinated functional interaction between the components of the masticatory system (
Mc Neill, 2000). Class II malocclusion refers to extra growth of maxillary arch and Class III malocclusion deals with extra mandibular growth. Another subject had a Class III malocclusion with mild developmental verbal apraxia. Developmental verbal apraxia is characterized by inconsistent articulatory breakdowns due to motor planning deficits. All subjects had articulation problems mainly with sound classes (e.g., fricatives, affricates, or liquids).
None of the subjects had received OMT in the past. All of them had received speech therapy to correct misarticulation of speech sounds. All of them were enrolled in speech therapy in school districts for more than two years. An insignificant amount of progress was made in speech as well as oral postures. Subjects provided informed consent and agreed to receive traditional OMT for six weeks (once in a week for 45 minutes each session) and then, if needed, receive traditional speech treatment. During the time of the study none of the subjects had dental braces or other appliances. All clients demonstrated varying degrees of low and forward tongue resting postures. Low and forward tongue resting postures affect the growth of orofacial complex. Lower tongue resting posture leads to reduced maxillary arch width (
Nowak & Warren, 2000). Lower face height and retrusive mandible are results of open-mouth resting postures.
BASELINE TESTING
Portions of the Dworkin-Culatta Oral Mechanism Examination (
Dworkin & Culatta, 1980) were used to assess the structural and functional integrity of the oral mechanism. To establish baselines for speech intelligibility subjects were asked to read aloud 30 single words and 10 sentences containing fricatives, affricates, and liquids (
Yorkston & Beukelman, 1984) (see
Appendix C). One 250-word spontaneous speech sample was collected to examine overall speech intelligibility. All speech samples were tape recorded. A narrow phonetic transcription (
Shriberg & Kent, 1995) was used to identify deviation of speech sounds.
Intelligibility is defined here as the proportion of words understood by the listeners. Word-by-word analysis was performed to rate speech intelligibility in single words, sentences, and connected speech samples. Words or utterances intended by the speaker were compared with the words understood by the listener. Two professional speech-language pathologists trained in using International Phonetic Alphabet independently listened to the tapes and transcribed all utterances.
Words having correct transcriptions were considered to be intelligible. Words having at least one phonemic or phonetic error were deemed unintelligible. All listeners had normal hearing and were free of any neurological or psychological disorders. Responses of all clients were played via tapes. Listeners were provided with headphones if they needed increased clarity.
TREATMENT
The main treatment goal was to teach tongue resting postures and lip closure. According to IAOM (2000), the goal of OMT is to create, restore, and maintain a normal balance of orofacial structures. According to
Hanson and Peachey (
1991), change in tongue resting posture facilitates change in functional behaviors. Tongue posture depends on vertical diameter of the lower one-third of the face, width of dental arches, dental occlusion, plane of the palate, and breathing. Three out of six clients who were treated by orthodontists adapted to low-lying tongue postures that resulted in the relapse of orthopedic-orthodontic treatment.
Treatment was provided one day in a week for 45 minutes. Treatment procedures included holding a tongue depressor between lips for 30-45 minutes per day during a silent reading or writing activity. To keep the lips closed, pressure was applied on the corner of each side of the upper lip and was pressed down for 45 seconds to strengthen lip musculature. To learn correct tongue postures, a sugarless mint was kept on the alveolar ridge for 15 minutes per day for three times. Clients were given extensive home assignments. Data were collected in hospital, University clinic, and private work settings. With the help of a behavior chart, the clients kept track of their progress. After six weeks of treatment, posttherapy speech intelligibility data were collected using similar procedures.
RESULTS AND DISCUSSION
Following OMT for six weeks, all clients were able to maintain appropriate lip and tongue postures 70 % of the time with the help of self-cueing strategies. Three subjects with anterior open bite demonstrated measurable progress. This progress may be attributed to clients' motivation (
Zimmerman, 1988). Due to OMT, all of the subjects developed heightened awareness of tongue and lip positions. They also improved their self-monitoring abilities while swallowing and during articulation activities (Bigenzhan et al. 1992;
Keatley & Coulson, 1989; Schievano et al. 1999).
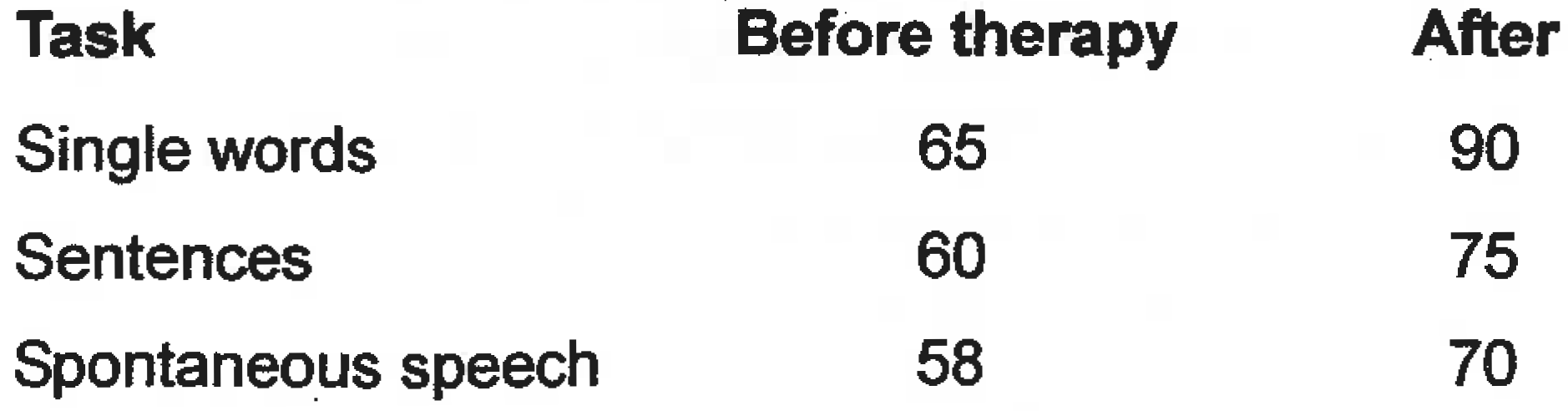
Speech intelligibility, scored by the method of transcription was used to understand precisely the articulatory errors present in various tasks. The rating scale for measuring speech intelligibility was not adapted secondary to increased subjectivity of ratings. Correctly transcribed utterances were counted to be intelligible. 30 words, 10 sentences, and a connected speech sample of 250 words were transcribed both before and after the treatment. Results obtained from five out of six subjects revealed an increase of 25% intelligibility for single words, 15% for sentences, and 12% intelligibility for spontaneous speech (see
Table 1). A qualitative analysis was also performed to understand the nature of deviations of speech sound productions across all the tasks (see
Table 2).
Table 1.
Average speech intelligibility scores in percentage across various speech tasks before and after therapy.
Table 1.
Average speech intelligibility scores in percentage across various speech tasks before and after therapy.
The client with Class III malocclusion and developmental apraxia of speech was excluded from the calculation of average results because the subject failed to perform adequately during the post-treatment measures. The client needed at least three to four attempts for producing each word correctly. The client also needed maximum verbal-visual cues from the clinician to maintain correct production of target words. Based on poor prognostic indicators for progress, the client truly represents the diagnostic terms-"persistent sound system disorders" or "persistent articulatory impairments" (
Powell, 1996;
Shelton, 1993).
The subject with Class III malocclusion did evidence maximum errors with fricatives and affricates. Increased distance between the tongue and mandibular incisors caused the airstream to scatter (
Vallino & Tompson, 1993). In connected speech, intelligibility was compromised because of untreated mandibular prognathism. Lip incompetence was also present that tended to affect intelligibility of bilabial sounds in rapid connected utterances. It was also quite difficult to maintain higher levels of articulatory precision and coordination needed for effective communication. The subject with Class II malocclusion showed lesser amount of articulation errors as compared to clients with Class III malocclusion.
To estimate the intrajudge reliability of speech measures, 25 % of all items were re-transcribed. Intrajudge reliability was found to be 0.99. Interjudge reliability was 0.97 regarding speech intelligibility across all three tasks. Both intrajudge and interjudge reliability were high.
Before therapy, listeners were able to understand an average of 61% of utterances. After therapy the listener was able to understand 78.3% of utterances based on the method of transcription. Transcription scores were noted to vary significantly from pre- to post-therapy status. Listeners perceived that distortion of fricatives, liquids, and affricates decreased drastically during connected speech.
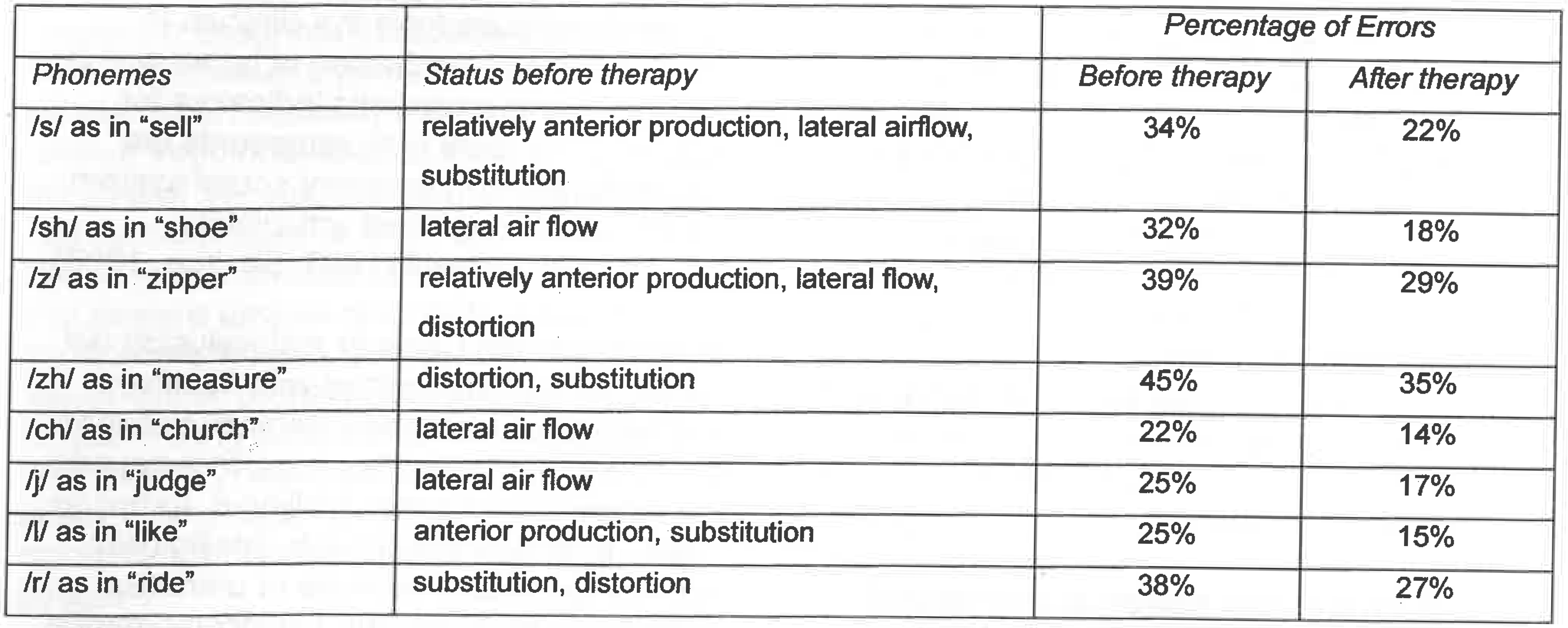
Table 2.
Articulatory/phonological impaiments before and after OMT based on qualitative analysis.
Table 2.
Articulatory/phonological impaiments before and after OMT based on qualitative analysis.
After completion of six weeks of OMT, subjects were informally interviewed to collect information on their perceptions regarding benefits of therapy. All but one subject reported increased understanding of correct tongue resting posture. All but one subject felt that their speech had significantly improved. They felt that their articulatory awareness had increased significantly. Subjects found improvement in swallowing functions and reported of increase in food intake secondary to more appropriate chewing. Besides improvement in speech and swallowing, subjects also felt that their social appearance had improved secondary to close-mouth position. The client with developmental apraxia of speech, which is a type of persistent articulatory impairment however, showed minimal progress.
CONCLUSIONS, CLINICAL IMPLICATIONS, AND FUTURE RESEARCH
The results of this study suggest that OMT is effective in treating individuals with persistent articulatory impairments and occlusion problems. OMT does help in learning desirable oral postures, increasing awareness of the tongue in oral space, and improving articulatory precision and overall speech intelligibility. Learning proper resting postures of tongue and lips may have stimulated self correction of articulation in the clients.
In the recent past the topic of speech intelligibility has been of great interest in the study of OMD and OMT. Speech intelligibility is a functional measure for reporting treatment results, because it provides a good estimate of communicative effectiveness.
The role of orofacial myofunctional therapists is to assess and treat clients with dentofacial disorders to improve cosmetic appearance, orthodontic retention, and speech characteristics (Hale, Kellum, Nason, & Johnson, 1988;
Landis, 1994). Occlusional relapse and mouth breathing are quite possible in clients who had orthodontic intervention (
Hanson, 1988) and were not followed up adequately. Speech language pathologists and other related professionals need to be aware of various oral behaviors, resting postures, dentofacial development, and dental occlusions, and understand precise effects of OMT (Hale et al. 1988) in order to better serve clients with behavioral, medical, dental, and educational needs. In order to derive maximum benefits from speech therapy for individuals with persistent articulatory impairments, speech-language pathologists need to treat underlying orofacial myofunctional variables. In addition to resting postures, they should also work with functional aspects of tongue behavior.
Future research needs to focus on more longitudinal and cross-sectional studies to determine the distinction between normal and abnormal orofacial myofunctional variables associated with persistent articulatory impairments. Retrospective studies are needed to understand efficacy research by documenting articulation remediation with or without OMT. More objective follow-up studies are required to determine the long-term retention of oral postures, articulatory patterns, and swallowing. Finally it would be worthwhile to explore extraneous factors causing relapse of malocclusions and subsequently, leading to resistance to speech remediation.