Why Can Organoids Improve Current Organ-on-Chip Platforms?
Abstract
:1. Introduction
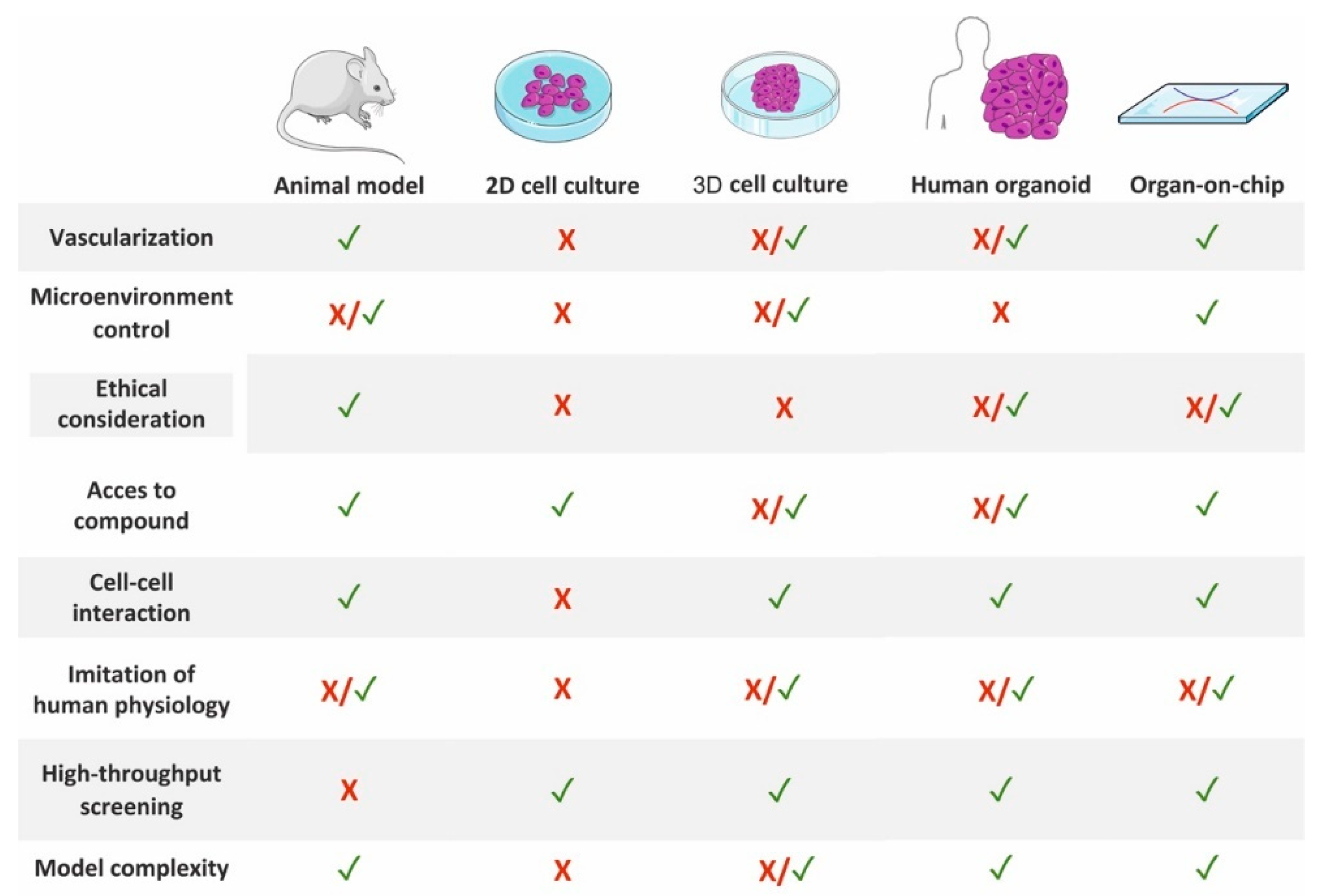
2. Preclinical Models
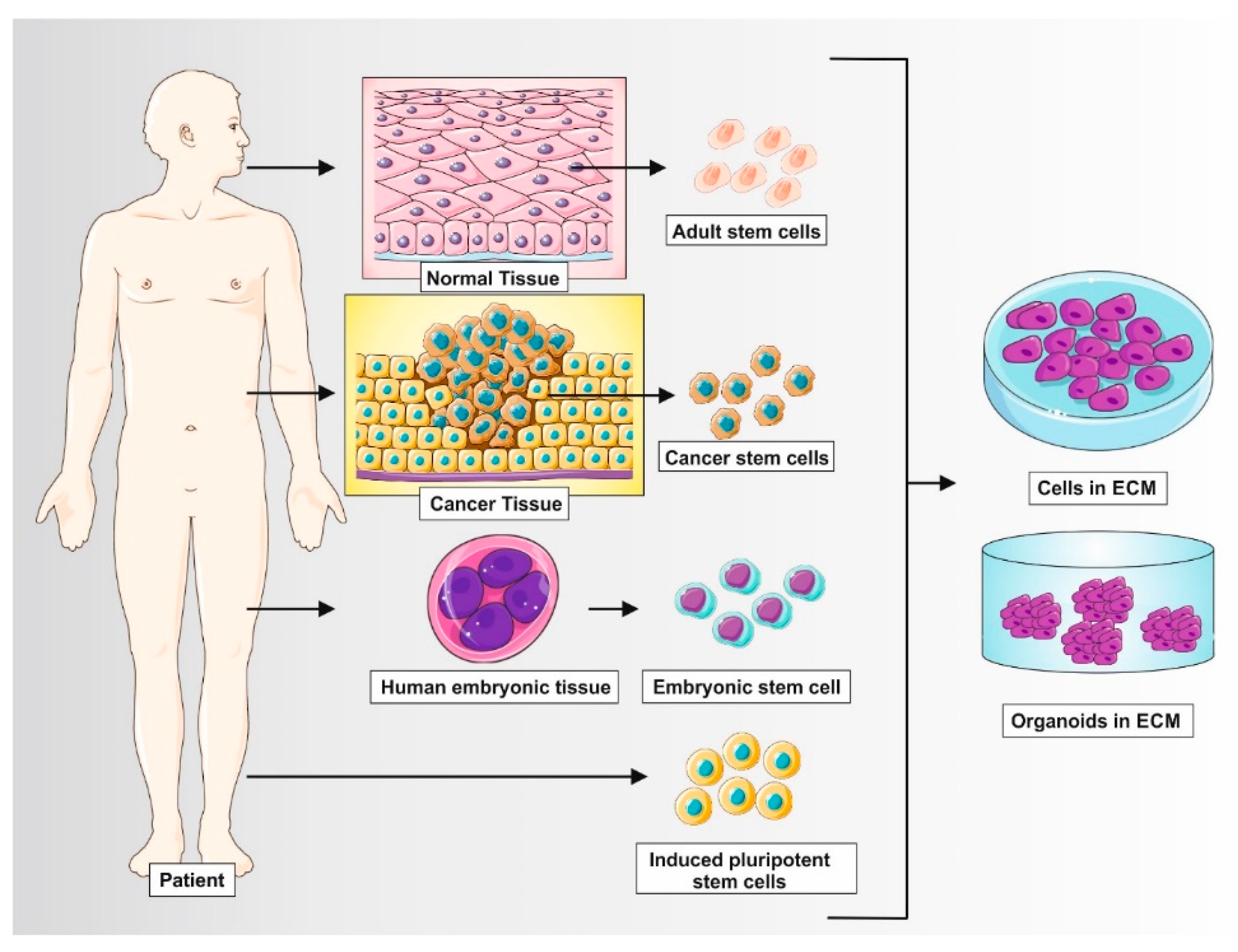
Organoids
3. Organ-on-Chip
3.1. Tumour
3.2. Lung
3.3. Liver
3.4. Heart
3.5. Brain
3.6. Pancreatic
3.7. Others
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brodniewicz, T.; Grynkiewicz, G. Preclinical drug development. Acta Pol. Pharm. Drug Res. 2010, 67, 579–586. [Google Scholar]
- Athar, M.; Back, J.H.; Tang, X.; Kim, K.H.; Kopelovich, L.; Bickers, D.R.; Kim, A.L. Resveratrol: A review of preclinical studies for human cancer prevention. Toxicol. Appl. Pharmacol. 2007, 224, 274–283. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cancer models in Preclinical Research: A Chronicle Review of Advancement in Effective Cancer Research—Sajjad—2021—Animal Models and Experimental Medicine—Wiley Online Library. Available online: https://onlinelibrary.wiley.com/doi/10.1002/ame2.12165 (accessed on 30 March 2022).
- Translating Preclinical Models to Humans. Available online: https://www.science.org/doi/10.1126/science.aay8086 (accessed on 30 March 2022).
- Pusztai, L.; Hatzis, C.; Andre, F. Reproducibility of research and preclinical validation: Problems and solutions. Nat. Rev. Clin. Oncol. 2013, 10, 720–724. [Google Scholar] [CrossRef] [PubMed]
- Frontiers|In Vitro Research Reproducibility: Keeping Up High Standards|Pharmacology. Available online: https://www.frontiersin.org/articles/10.3389/fphar.2019.01484/full (accessed on 30 March 2022).
- Kapałczyńska, M.; Kolenda, T.; Przybyła, W.; Zajączkowska, M.; Teresiak, A.; Filas, V.; Ibbs, M.; Bliźniak, R.; Łuczewski, Ł.; Lamperska, K. 2D and 3D cell cultures—A comparison of different types of cancer cell cultures. Arch. Med. Sci. 2018, 14, 910–919. [Google Scholar] [CrossRef]
- Caleb, J.; Yong, T. Is It Time to Start Transitioning From 2D to 3D Cell Culture? Front. Mol. Biosci. 2020, 7, 33. [Google Scholar]
- Kar, S.K.; Wells, J.M.; Ellen, E.D.; te Pas, M.F.W.; Madsen, O.; Groenen, M.A.M.; Woelders, H. Organoids: A promising new in vitro platform in livestock and veterinary research. Vet. Res. 2021, 52, 43. [Google Scholar]
- Gjorevski, N.; Ranga, A.; Lutolf, M.P. Bioengineering approaches to guide stem cell-based organogenesis. Development 2014, 141, 1794–1804. [Google Scholar] [CrossRef] [Green Version]
- Advances in Development and Application of Human Organoids|SpringerLink. Available online: https://link.springer.com/article/10.1007/s13205-021-02815-7 (accessed on 30 March 2022).
- Nature Reviews Molecular Cell Biology. Human Organoids: Model Systems for Human Biology and Medicine. Available online: https://www.nature.com/articles/s41580-020-0259-3 (accessed on 30 March 2022).
- Lancaster, M.A.; Renner, M.; Martin, C.-A.; Wenzel, D.; Bicknell, L.S.; Hurles, M.E.; Homfray, T.; Penninger, J.M.; Jackson, A.P.; Knoblich, J.A. Cerebral organoids model human brain development and microcephaly. Nature 2013, 501, 373–379. [Google Scholar] [CrossRef]
- Frontiers|Liver Organoids: Recent Developments, Limitations and Potential|Medicine. Available online: https://www.frontiersin.org/articles/10.3389/fmed.2021.574047/full (accessed on 30 March 2022).
- Nishinakamura, R. Human kidney organoids: Progress and remaining challenges. Nat. Rev. Nephrol. 2019, 15, 613–624. [Google Scholar] [CrossRef]
- Mohan, S.C.; Lee, T.-Y.; Giuliano, A.E.; Cui, X. Current Status of Breast Organoid Models. Front. Bioeng. Biotechnol. 2021, 9, 745943. [Google Scholar] [CrossRef]
- Khan, S.; Tiriac, H. Synthetic scaffold for pancreatic organoids. Nat. Mater. 2022, 21, 9–11. [Google Scholar] [CrossRef] [PubMed]
- Lancaster, M.A.; Knoblich, J.A. Organogenesis in a dish: Modeling development and disease using organoid technologies. Science 2014, 345, 1247125. [Google Scholar] [CrossRef] [PubMed]
- Organoids as Model Systems for Human Development, Disease and Clinical Applications|Frontiers Research Topic. Available online: https://www.frontiersin.org/research-topics/8436/organoids-as-model-systems-for-human-development-disease-and-clinical-applications (accessed on 30 March 2022).
- Ingber, D.E. Human organs-on-chips for disease modelling, drug development and personalized medicine. Nat. Rev. Genet. 2022, 1–25. [Google Scholar]
- Clarke, G.A.; Hartse, B.X.; Niaraki Asli, A.E.; Taghavimehr, M.; Hashemi, N.; Abbasi Shirsavar, M.; Montazami, R.; Alimoradi, N.; Nasirian, V.; Ouedraogo, L.J.; et al. Advancement of Sensor Integrated Organ-on-Chip Devices. Sensors 2021, 21, 1367. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Liu, J.; Wang, X.; Feng, L.; Wu, J.; Zhu, X.; Wen, W.; Gong, X. Organ-on-a-chip: Recent breakthroughs and future prospects. BioMed. Eng. OnLine 2020, 19, 9. [Google Scholar]
- Edmondson, R.; Broglie, J.J.; Adcock, A.F.; Yang, L. Three-Dimensional Cell Culture Systems and Their Applications in Drug Discovery and Cell-Based Biosensors. Assay Drug Dev. Technol. 2014, 12, 207–218. [Google Scholar] [CrossRef] [Green Version]
- Hickman, J.A.; Graeser, R.; de Hoogt, R.; Vidic, S.; Brito, C.; Gutekunst, M.; van der Kuip, H. IMI PREDECT Consortium Three-dimensional models of cancer for pharmacology and cancer cell biology: Capturing tumor complexity in vitro/ex vivo. BioTechnol. J. 2014, 9, 1115–1128. [Google Scholar] [CrossRef]
- Ergorul, C.; Levin, L.A. Solving the lost in translation problem: Improving the effectiveness of translational research. Curr. Opin. Pharmacol. 2013, 13, 108–114. [Google Scholar] [CrossRef] [Green Version]
- Future Science OA. Animal Models Are Essential to Biological Research: Issues and Perspectives. Available online: https://www.future-science.com/doi/full/10.4155/fso.15.63 (accessed on 27 April 2022).
- Onaciu, A.; Munteanu, R.; Munteanu, V.C.; Gulei, D.; Raduly, L.; Feder, R.-I.; Pirlog, R.; Atanasov, A.G.; Korban, S.S.; Irimie, A.; et al. Spontaneous and Induced Animal Models for Cancer Research. Diagnostics 2020, 10, 660. [Google Scholar] [CrossRef]
- Robinson, N.B.; Krieger, K.; Khan, F.M.; Huffman, W.; Chang, M.; Naik, A.; Yongle, R.; Hameed, I.; Krieger, K.; Girardi, L.N.; et al. The current state of animal models in research: A review. Int. J. Surg. 2019, 72, 9–13. [Google Scholar] [CrossRef]
- Regenberg, A.; Mathews, D.J.; Blass, D.M.; Bok, H.; Coyle, J.T.; Duggan, P.; Faden, R.; Finkel, J.; Gearhart, J.D.; Hillis, A.; et al. The role of animal models in evaluating reasonable safety and efficacy for human trials of cell-based interventions for neurologic conditions. J. Cereb. Blood Flow Metab. 2009, 29, 1–9. [Google Scholar] [CrossRef] [PubMed]
- The Beginning of the End for Chimpanzee Experiments?|Philosophy, Ethics, and Humanities in Medicine|Full Text. Available online: https://peh-med.biomedcentral.com/articles/10.1186/1747-5341-3-16 (accessed on 27 April 2022).
- Humane Society International. Available online: https://www.hsi.org/ (accessed on 2 March 2022).
- Graham, M.L.; Prescott, M.J. The multifactorial role of the 3Rs in shifting the harm-benefit analysis in animal models of disease. Eur. J. Pharm. 2015, 759, 19–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cukierman, E.; Pankov, R.; Stevens, D.R.; Yamada, K.M. Taking cell-matrix adhesions to the third dimension. Science 2001, 294, 1708–1712. [Google Scholar] [CrossRef] [PubMed]
- Frontiers|3D Tissue Models as an Effective Tool for Studying Viruses and Vaccine Development|Materials. Available online: https://www.frontiersin.org/articles/10.3389/fmats.2021.631373/full (accessed on 27 April 2022).
- Wu, X.; Su, J.; Wei, J.; Jiang, N.; Ge, X. Recent Advances in Three-Dimensional Stem Cell Culture Systems and Applications. Stem Cells Int. 2021, 2021, 9477332. [Google Scholar] [CrossRef]
- Lee, D.; Pathak, S.; Jeong, J.-H. Design and manufacture of 3D cell culture plate for mass production of cell-spheroids. Sci. Rep. 2019, 9, 13976. [Google Scholar] [CrossRef] [Green Version]
- Phung, Y.T.; Barbone, D.; Broaddus, V.C.; Ho, M. Rapid generation of in vitro multicellular spheroids for the study of monoclonal antibody therapy. J. Cancer 2011, 2, 507–514. [Google Scholar] [CrossRef] [Green Version]
- Barrila, J.; Radtke, A.L.; Crabbé, A.; Sarker, S.F.; Herbst-Kralovetz, M.M.; Ott, C.M.; Nickerson, C.A. Organotypic 3D cell culture models: Using the rotating wall vessel to study host–pathogen interactions. Nat. Rev. Microbiol. 2010, 8, 791–801. [Google Scholar]
- Kim, J.B. Three-dimensional tissue culture models in cancer biology. Semin. Cancer Biol. 2005, 15, 365–377. [Google Scholar] [CrossRef]
- Ware, M.J.; Colbert, K.; Keshishian, V.; Ho, J.; Corr, S.J.; Curley, S.A.; Godin, B. Generation of Homogenous Three-Dimensional Pancreatic Cancer Cell Spheroids Using an Improved Hanging Drop Technique. Tissue Eng. Part C Methods 2016, 22, 312–321. [Google Scholar] [CrossRef] [Green Version]
- Ma, P.X. Scaffolds for tissue fabrication. Mater. Today 2004, 7, 30–40. [Google Scholar] [CrossRef]
- Three-Dimensional Porous Scaffolds with Biomimetic Microarchitecture and Bioactivity for Cartilage Tissue Engineering|ACS Applied Materials & Interfaces. Available online: https://pubs.acs.org/doi/abs/10.1021/acsami.9b12206 (accessed on 27 April 2022).
- Sokolowska, P.; Janikiewicz, J.; Jastrzebska, E.; Brzozka, Z.; Dobrzyn, A. Combinations of regenerative medicine and Lab-on-a-chip systems: New hope to restoring the proper function of pancreatic islets in diabetes. Biosens. Bioelectron. 2020, 167, 112451. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.J.; Im, H.; Kim, S.H.; Park, J.W.; Jung, Y. Toward Biomimetic Scaffolds for Tissue Engineering: 3D Printing Techniques in Regenerative Medicine. Front. Bioeng. Biotechnol. 2020, 8, 586406. [Google Scholar] [CrossRef]
- Gao, G.; Schilling, A.F.; Yonezawa, T.; Wang, J.; Dai, G.; Cui, X. Bioactive nanoparticles stimulate bone tissue formation in bioprinted three-dimensional scaffold and human mesenchymal stem cells. BioTechnol. J. 2014, 9, 1304–1311. [Google Scholar] [CrossRef] [PubMed]
- Supramolecular Hydrogelators and Hydrogels: From Soft Matter to Molecular Biomaterials|Chemical Reviews. Available online: https://pubs.acs.org/doi/10.1021/acs.chemrev.5b00299 (accessed on 27 April 2022).
- Chen, F.-M.; Liu, X. Advancing biomaterials of human origin for tissue engineering. Prog. Polym. Sci. 2016, 53, 86–168. [Google Scholar] [PubMed] [Green Version]
- Sultana, N. 1—Mechanical and biological properties of scaffold materials. In Functional 3D Tissue Engineering Scaffolds; Deng, Y., Kuiper, J., Eds.; Woodhead Publishing: Sawston, UK, 2018; pp. 1–21. ISBN 978-0-08-100979-6. [Google Scholar]
- Cui, X.; Hartanto, Y.; Zhang, H. Advances in multicellular spheroids formation. J. R. Soc. Interface 2017, 14, 20160877. [Google Scholar] [CrossRef]
- Engineering Organoids|Nature Reviews Materials. Available online: https://www.nature.com/articles/s41578-021-00279-y (accessed on 30 March 2022).
- Tsuruta, S.; Uchida, H.; Akutsu, H. Intestinal Organoids Generated from Human Pluripotent Stem Cells. JMA J. 2020, 3, 9–19. [Google Scholar]
- Su, X.; Yue, P.; Kong, J.; Xu, X.; Zhang, Y.; Cao, W.; Fan, Y.; Liu, M.; Chen, J.; Liu, A.; et al. Human Brain Organoids as an In Vitro Model System of Viral Infectious Diseases. Front. Immunol. 2022, 12, 792316. [Google Scholar] [CrossRef]
- Heo, I.; Dutta, D.; Schaefer, D.A.; Iakobachvili, N.; Artegiani, B.; Sachs, N.; Boonekamp, K.E.; Bowden, G.; Hendrickx, A.P.A.; Willems, R.J.R.; et al. Modeling Cryptosporidium infection in human small intestinal and lung organoids. Nat. Microbiol. 2018, 3, 814–823. [Google Scholar] [CrossRef]
- Multiorgan-on-a-Chip: A Systemic Approach To Model and Decipher Inter-Organ Communication: Trends in Biotechnology. Available online: https://www.cell.com/trends/biotechnology/fulltext/S0167-7799(20)30309-7 (accessed on 27 April 2022).
- Small Molecule Absorption by PDMS in the Context of Drug Response Bioassays—Science Direct. Available online: https://www.sciencedirect.com/science/article/pii/S0006291X16319179 (accessed on 27 April 2022).
- Ding, C.; Chen, X.; Kang, Q.; Yan, X. Biomedical Application of Functional Materials in Organ-on-a-Chip. Front. BioEng. BioTechnol. 2020, 8, 823. [Google Scholar] [CrossRef]
- Kamei, K.; Mashimo, Y.; Koyama, Y.; Fockenberg, C.; Nakashima, M.; Nakajima, M.; Li, J.; Chen, Y. 3D printing of soft lithography mold for rapid production of polydimethylsiloxane-based microfluidic devices for cell stimulation with concentration gradients. BioMed. Microdevices 2015, 17, 36. [Google Scholar] [CrossRef]
- Carter, S.-S.D.; Atif, A.-R.; Kadekar, S.; Lanekoff, I.; Engqvist, H.; Varghese, O.P.; Tenje, M.; Mestres, G. PDMS leaching and its implications for on-chip studies focusing on bone regeneration applications. Organs-on-a-Chip 2020, 2, 100004. [Google Scholar] [CrossRef]
- Rauti, R.; Ess, A.; Le Roi, B.; Kreinin, Y.; Epshtein, M.; Korin, N.; Maoz, B.M. Transforming a well into a chip: A modular 3D-printed microfluidic chip. APL Bioeng. 2021, 5, 026103. [Google Scholar] [CrossRef] [PubMed]
- Hirama, H.; Satoh, T.; Sugiura, S.; Shin, K.; Onuki-Nagasaki, R.; Kanamori, T.; Inoue, T. Glass-based organ-on-a-chip device for restricting small molecular absorption. J. BioSci. BioEng. 2019, 127, 641–646. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; George, S.M.; Vernetti, L.; Gough, A.H.; Taylor, D.L. A glass-based, continuously zonated and vascularized human liver acinus microphysiological system (vLAMPS) designed for experimental modeling of diseases and ADME/TOX. Lab Chip 2018, 18, 2614–2631. [Google Scholar] [CrossRef] [PubMed]
- Jang, H.; Refatul Haq, M.; Kim, Y.; Kim, J.; Oh, P.; Ju, J.; Kim, S.-M.; Lim, J. Fabrication of Glass Microchannel via Glass Imprinting using a Vitreous Carbon Stamp for Flow Focusing Droplet Generator. Sensors 2018, 18, 83. [Google Scholar] [CrossRef] [Green Version]
- Carvalho, V.; Gonçalves, I.; Lage, T.; Rodrigues, R.O.; Minas, G.; Teixeira, S.F.C.F.; Moita, A.S.; Hori, T.; Kaji, H.; Lima, R.A. 3D Printing Techniques and Their Applications to Organ-on-a-Chip Platforms: A Systematic Review. Sensors 2021, 21, 3304. [Google Scholar] [CrossRef]
- Becker, H.; Gärtner, C. Polymer microfabrication technologies for microfluidic systems. Anal Bioanal Chem. 2008, 390, 89–111. [Google Scholar]
- Schneider, S.; Brás, E.J.S.; Schneider, O.; Schlünder, K.; Loskill, P. Facile Patterning of Thermoplastic Elastomers and Robust Bonding to Glass and Thermoplastics for Microfluidic Cell Culture and Organ-on-Chip. Micromachines 2021, 12, 575. [Google Scholar] [CrossRef]
- Deshmukh, S.S.; Goswami, A. Hot Embossing of polymers—A review. Mater. Today Proc. 2020, 26, 405–414. [Google Scholar] [CrossRef]
- Cvek, M.; Kracalik, M.; Sedlacik, M.; Mrlik, M.; Sedlarik, V. Reprocessing of injection-molded magnetorheological elastomers based on TPE matrix. Compos. Part B Eng. 2019, 172, 253–261. [Google Scholar] [CrossRef]
- Song, S.W.; Kim, S.D.; Oh, D.Y.; Lee, Y.; Lee, A.C.; Jeong, Y.; Bae, H.J.; Lee, D.; Lee, S.; Kim, J.; et al. One-Step Generation of a Drug-Releasing Hydrogel Microarray-On-A-Chip for Large-Scale Sequential Drug Combination Screening. Adv. Sci. 2019, 6, 1801380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, C.Y.; Goral, V.N.; DeRosa, M.E.; Huang, T.J.; Yuen, P.K. A polystyrene-based microfluidic device with three-dimensional interconnected microporous walls for perfusion cell culture. Biomicrofluidics 2014, 8, 046505. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deiss, F.; Mazzeo, A.; Hong, E.; Ingber, D.E.; Derda, R.; Whitesides, G.M. Platform for high-throughput testing of the effect of soluble compounds on 3D cell cultures. Anal Chem. 2013, 85, 8085–8094. [Google Scholar] [CrossRef] [Green Version]
- Quan, Y.; Sun, M.; Tan, Z.; Eijkel, J.C.T.; van den Berg, A.; van der Meer, A.; Xie, Y. Organ-on-a-chip: The next generation platform for risk assessment of radiobiology. RSC Adv. 2020, 10, 39521–39530. [Google Scholar] [CrossRef] [PubMed]
- Huh, D.; Matthews, B.D.; Mammoto, A.; Montoya-Zavala, M.; Hsin, H.Y.; Ingber, D.E. Reconstituting organ-level lung functions on a chip. Science 2010, 328, 1662–1668. [Google Scholar] [CrossRef] [Green Version]
- Reif, R. The body-on-a-chip concept: Possibilities and limitations. EXCLI J. 2014, 13, 1283–1285. [Google Scholar]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef]
- Huang, S.; Yang, J.; Fong, S.; Zhao, Q. Artificial intelligence in cancer diagnosis and prognosis: Opportunities and challenges. Cancer Lett. 2020, 471, 61–71. [Google Scholar]
- Xu, H.; Lyu, X.; Yi, M.; Zhao, W.; Song, Y.; Wu, K. Organoid technology and applications in cancer research. J. Hematol. Oncol. 2018, 11, 116. [Google Scholar] [CrossRef]
- Nagle, P.W.; Plukker, J.T.M.; Muijs, C.T.; van Luijk, P.; Coppes, R.P. Patient-derived tumor organoids for prediction of cancer treatment response. Semin. Cancer Biol. 2018, 53, 258–264. [Google Scholar] [CrossRef]
- Park, S.E.; Georgescu, A.; Huh, D. Organoids-on-a-chip. Science 2019, 364, 960–965. [Google Scholar] [CrossRef] [PubMed]
- Tumor-on-a-Chip Platform to Investigate Progression and Drug Sensitivity in Cell Lines and Patient-Derived Organoids—Szukaj w Google. Available online: https://www.google.com/search?q=Tumor-on-a-chip+platform+to+investigate+progression+and+drug+sensitivity+in+cell+lines+and+patient-derived+organoids&rlz=1C1CHBF_nlNL912NL912&oq=Tumor-on-a-chip+platform+to+investigate+progression+and+drug+sensitivity+in+cell+lines+and+patient-derived+organoids&aqs=chrome.0.69i59j69i61l2.405j0j4&sourceid=chrome&ie=UTF-8 (accessed on 30 March 2022).
- IFlowPlate—A Customized 384-Well Plate for the Culture of Perfusable Vascularized Colon Organoids—Rajasekar—2020—Advanced Materials—Wiley Online Library. Available online: https://onlinelibrary.wiley.com/doi/full/10.1002/adma.202002974 (accessed on 30 March 2022).
- Welp, A.L.; Bomberger, J.M. Bacterial Community Interactions During Chronic Respiratory Disease. Front. Cell Infect. Microbiol. 2020, 10, 213. [Google Scholar] [CrossRef] [PubMed]
- Second-Generation Lung-on-a-Chip with an Array of Stretchable Alveoli Made with a Biological Membrane|Communications Biology. Available online: https://www.nature.com/articles/s42003-021-01695-0 (accessed on 30 March 2022).
- Gkatzis, K.; Taghizadeh, S.; Huh, D.; Stainier, D.Y.R.; Bellusci, S. Use of three-dimensional organoids and lung-on-a-chip methods to study lung development, regeneration and disease. Eur. Respir. J. 2018, 52, 1800876. [Google Scholar] [CrossRef] [PubMed]
- Asrani, S.K.; Devarbhavi, H.; Eaton, J.; Kamath, P.S. Burden of liver diseases in the world. J. Hepatol. 2019, 70, 151–171. [Google Scholar] [CrossRef] [PubMed]
- Kisseleva, T.; Brenner, D. Molecular and cellular mechanisms of liver fibrosis and its regression. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 151–166. [Google Scholar] [CrossRef] [PubMed]
- Collins, S.D.; Yuen, G.; Tu, T.; Budzinska, M.A.; Spring, K.; Bryant, K.; Shackel, N.A. In Vitro Models of the Liver: Disease Modeling, Drug Discovery and Clinical Applications. In Hepatocellular Carcinoma; Tirnitz-Parker, J.E.E., Ed.; Codon Publications: Brisbane, Australia, 2019; ISBN 978-0-9944381-8-8. [Google Scholar]
- Vascularized Liver Organoids Generated Using Induced Hepatic Tissue and Dynamic Liver-Specific Microenvironment as a Drug Testing Platform—Jin—2018—Advanced Functional Materials—Wiley Online Library. Available online: https://onlinelibrary.wiley.com/doi/full/10.1002/adfm.201801954 (accessed on 30 March 2022).
- Wang, Y.; Wang, H.; Deng, P.; Chen, W.; Guo, Y.; Tao, T.; Qin, J. In situ differentiation and generation of functional liver organoids from human iPSCs in a 3D perfusable chip system. Lab Chip 2018, 18, 3606–3616. [Google Scholar] [CrossRef]
- Heart Disease and Stroke Statistics—2022 Update: A Report from the American Heart Association|Circulation. Available online: https://www.ahajournals.org/doi/10.1161/CIR.0000000000001052 (accessed on 30 March 2022).
- Multi-Tissue Interactions in an Integrated Three-Tissue Organ-on-a-Chip Platform|Scientific Reports. Available online: https://www.nature.com/articles/s41598-017-08879-x (accessed on 30 March 2022).
- Yin, F.; Zhang, X.; Wang, L.; Wang, Y.; Zhu, Y.; Li, Z.; Tao, T.; Chen, W.; Yu, H.; Qin, J. HiPSC-derived multi-organoids-on-chip system for safety assessment of antidepressant drugs. Lab Chip 2021, 21, 571–581. [Google Scholar] [CrossRef]
- Kerman, B.E.; Kim, H.J.; Padmanabhan, K.; Mei, A.; Georges, S.; Joens, M.S.; Fitzpatrick, J.A.J.; Jappelli, R.; Chandross, K.J.; August, P.; et al. In vitro myelin formation using embryonic stem cells. Development 2015, 142, 2213–2225. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.U.; Blasiak, A.; Agrawal, D.R.; Loong, D.T.B.; Thakor, N.V.; All, A.H.; Ho, J.S.; Yang, I.H. Subcellular electrical stimulation of neurons enhances the myelination of axons by oligodendrocytes. PLoS ONE 2017, 12, e0179642. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Wang, L.; Zhu, Y.; Qin, J. Human brain organoid-on-a-chip to model prenatal nicotine exposure. Lab Chip 2018, 18, 851–860. [Google Scholar] [CrossRef]
- Cho, A.-N.; Jin, Y.; An, Y.; Kim, J.; Choi, Y.S.; Lee, J.S.; Kim, J.; Choi, W.-Y.; Koo, D.-J.; Yu, W.; et al. Microfluidic device with brain extracellular matrix promotes structural and functional maturation of human brain organoids. Nat. Commun. 2021, 12, 4730. [Google Scholar] [CrossRef] [PubMed]
- Röder, P.V.; Wu, B.; Liu, Y.; Han, W. Pancreatic regulation of glucose homeostasis. Exp. Mol. Med. 2016, 48, e219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heileman, K.; Daoud, J.; Hasilo, C.; Gasparrini, M.; Paraskevas, S.; Tabrizian, M. Microfluidic platform for assessing pancreatic islet functionality through dielectric spectroscopy. Biomicrofluidics 2015, 9, 044125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steiner, D.J.; Kim, A.; Miller, K.; Hara, M. Pancreatic islet plasticity: Interspecies comparison of islet architecture and composition. Islets 2010, 2, 135–145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mohammed, J.S.; Wang, Y.; Harvat, T.A.; Oberholzer, J.; Eddington, D.T. Microfluidic device for multimodal characterization of pancreatic islets. Lab Chip 2009, 9, 97–106. [Google Scholar] [CrossRef] [Green Version]
- Hugill, A.; Shimomura, K.; Cox, R.D. Islet Insulin Secretion Measurements in the Mouse. Curr. Protoc. Mouse Biol. 2016, 6, 256–271. [Google Scholar] [CrossRef]
- Lee, S.H.; Hong, S.; Song, J.; Cho, B.; Han, E.J.; Kondapavulur, S.; Kim, D.; Lee, L.P. Microphysiological Analysis Platform of Pancreatic Islet β-Cell Spheroids. Adv. Healthc. Mater. 2018, 7, 1701111. [Google Scholar] [CrossRef]
- Pflimlin, E.; Bielohuby, M.; Korn, M.; Breitschopf, K.; Löhn, M.; Wohlfart, P.; Konkar, A.; Podeschwa, M.; Bärenz, F.; Pfenninger, A.; et al. Acute and Repeated Treatment with 5-PAHSA or 9-PAHSA Isomers Does Not Improve Glucose Control in Mice. Cell Metab. 2018, 28, 217–227.e13. [Google Scholar] [CrossRef] [Green Version]
- Sokolowska, P.; Zukowski, K.; Janikiewicz, J.; Jastrzebska, E.; Dobrzyn, A.; Brzozka, Z. Islet-on-a-chip: Biomimetic micropillar-based microfluidic system for three-dimensional pancreatic islet cell culture. Biosens. Bioelectron. 2021, 183, 113215. [Google Scholar] [CrossRef]
- Hirano, K.; Konagaya, S.; Turner, A.; Noda, Y.; Kitamura, S.; Kotera, H.; Iwata, H. Closed-channel culture system for efficient and reproducible differentiation of human pluripotent stem cells into islet cells. BioChem. Biophys. Res. Commun. 2017, 487, 344–350. [Google Scholar] [CrossRef]
- Chen, W.-Y.; Evangelista, E.A.; Yang, J.; Kelly, E.J.; Yeung, C.K. Kidney Organoid and Microphysiological Kidney Chip Models to Accelerate Drug Development and Reduce Animal Testing. Front. Pharm. 2021, 12, 695920. [Google Scholar] [CrossRef] [PubMed]
- Xue, Y.; Seiler, M.J.; Tang, W.C.; Wang, J.Y.; Delgado, J.; McLelland, B.T.; Nistor, G.; Keirstead, H.S.; Browne, A.W. Retinal organoids on-a-chip: A micro-millifluidic bioreactor for long-term organoid maintenance. Lab Chip 2021, 21, 3361–3377. [Google Scholar] [CrossRef] [PubMed]
- Kasendra, M.; Tovaglieri, A.; Sontheimer-Phelps, A.; Jalili-Firoozinezhad, S.; Bein, A.; Chalkiadaki, A.; Scholl, W.; Zhang, C.; Rickner, H.; Richmond, C.A.; et al. Development of a primary human Small Intestine-on-a-Chip using biopsy-derived organoids. Sci. Rep. 2018, 8, 2871. [Google Scholar] [CrossRef] [PubMed]

| Materials | Advantages | Disadvantages | Pre-Processing Methods | Ref. |
|---|---|---|---|---|
| PDMS |
|
|
| [57,58,59] |
| Glass |
|
|
| [60,61,62] |
| PMMA |
|
|
| [63,64] |
| Thermoplastic elastomers (TPE) |
|
|
| [65,66,67] |
| Polystyrene (PS) |
|
|
| [68,69] |
| Paper |
|
|
| [70] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sokolowska, P.; Zuchowska, A.; Brzozka, Z. Why Can Organoids Improve Current Organ-on-Chip Platforms? Organoids 2022, 1, 69-84. https://doi.org/10.3390/organoids1010007
Sokolowska P, Zuchowska A, Brzozka Z. Why Can Organoids Improve Current Organ-on-Chip Platforms? Organoids. 2022; 1(1):69-84. https://doi.org/10.3390/organoids1010007
Chicago/Turabian StyleSokolowska, Patrycja, Agnieszka Zuchowska, and Zbigniew Brzozka. 2022. "Why Can Organoids Improve Current Organ-on-Chip Platforms?" Organoids 1, no. 1: 69-84. https://doi.org/10.3390/organoids1010007
APA StyleSokolowska, P., Zuchowska, A., & Brzozka, Z. (2022). Why Can Organoids Improve Current Organ-on-Chip Platforms? Organoids, 1(1), 69-84. https://doi.org/10.3390/organoids1010007






